Pathology
0.0(0)
Card Sorting
1/200
Earn XP
Description and Tags
Last updated 9:21 PM on 3/30/23
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
201 Terms
1
New cards
2
New cards
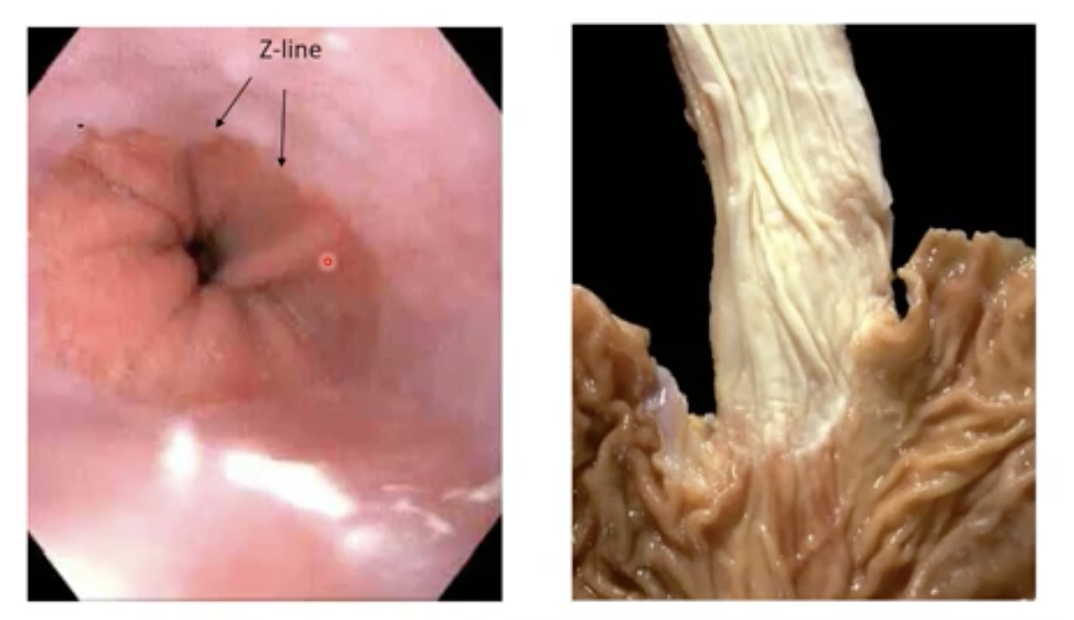
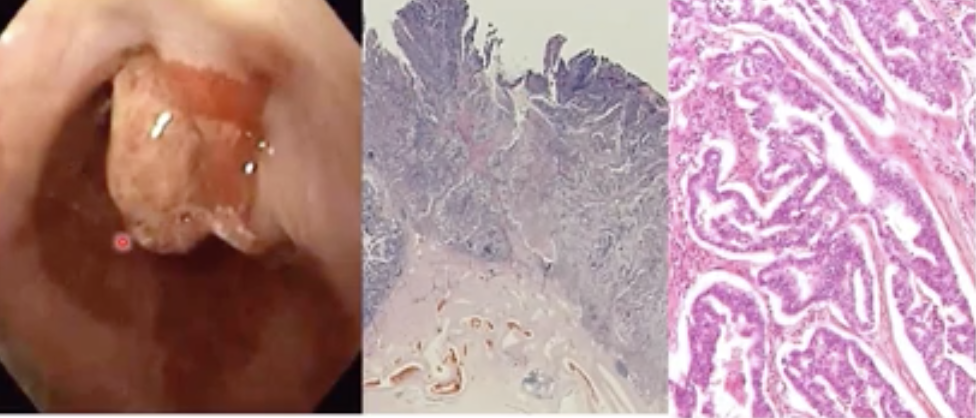
What does a normal esophagus look like?
Note the different epithelial lining between the oesophagus and the stomach on the left
On the right, the pale part is oesophagus and darker is stomach
On the right, the pale part is oesophagus and darker is stomach
3
New cards
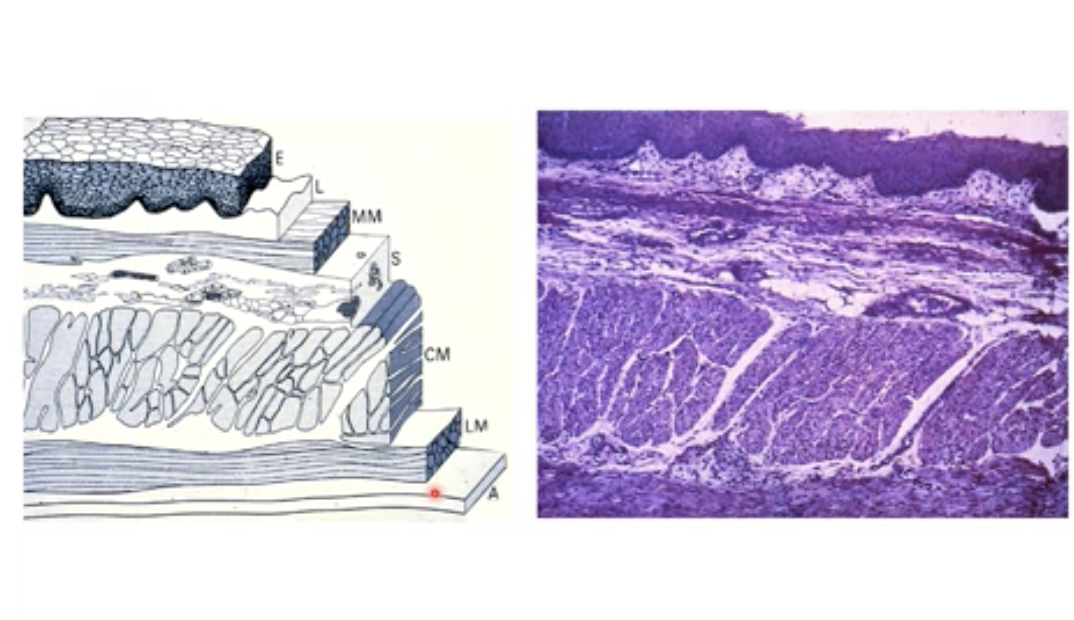
What kind of cell type is the oesophagus made of?
* Squamous (top) + Fibroblasts / Lamina propria
+ Muscular Mucosa = Mucosa (1st layer formed from three layer)
* Fatty tissue + Veins = Submucosa
* Smooth muscle fibers (thick layer in the middle)
* Fatty tissue
\
\
+ Muscular Mucosa = Mucosa (1st layer formed from three layer)
* Fatty tissue + Veins = Submucosa
* Smooth muscle fibers (thick layer in the middle)
* Fatty tissue
\
\
4
New cards
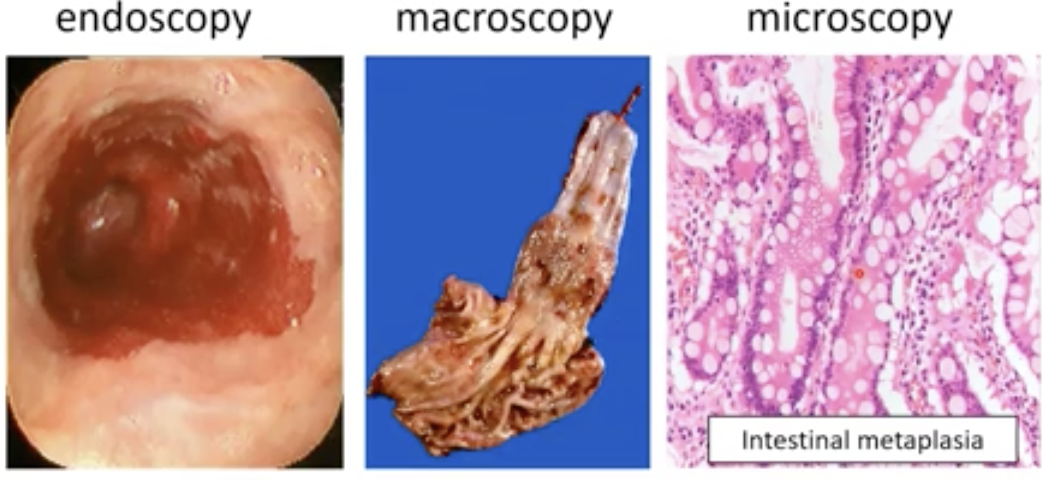
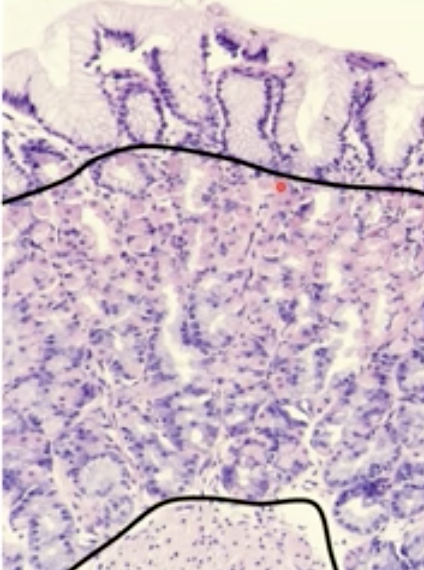
What are the first 2 phases in dev of oesophageal carcinoma steps:
Phase 1: Inflammation due to content of stomach goes up to throat (too acidic) (Reflux oesophagitis) → hyperaemia, granulocytes and in severe cases ulceration
Phase 2: Metaplasia (intestinal) and CHRONIC inflammation (replacing normal squamous epithelia with intestinal type epithelium) aka Barett esophagus
Phase 2: Metaplasia (intestinal) and CHRONIC inflammation (replacing normal squamous epithelia with intestinal type epithelium) aka Barett esophagus
5
New cards
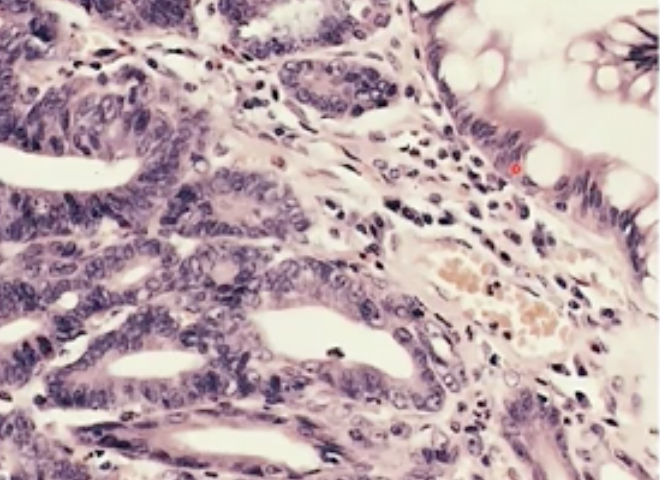
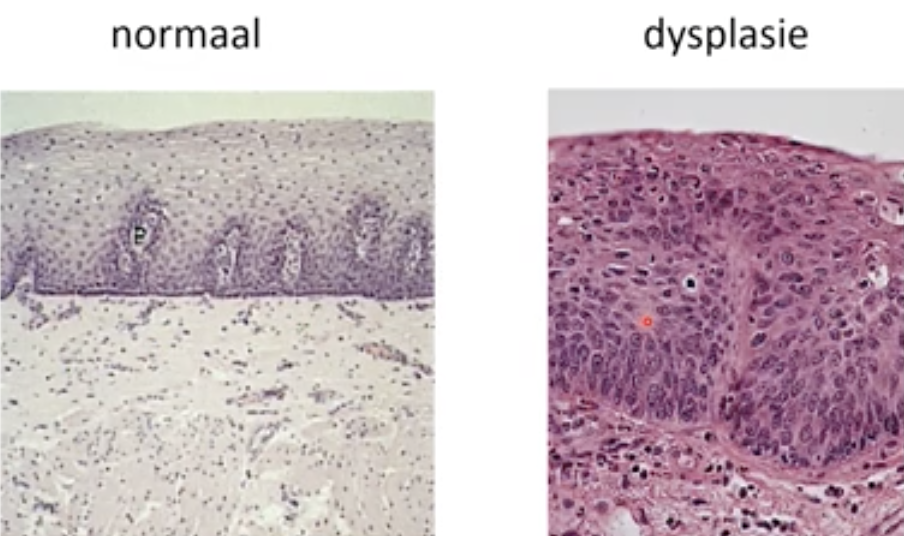
If intestinal metaplasia stays, we see molecular changes. Explain?
Dysplasia occurs, cytonucleur atypia = large nuclei, irregular shape and coarse chromatin pattern.
6
New cards
Having cytonucleur atypia increases the risk of what ?
Adenocarcinoma, when the cells penetrate the muscular layer
7
New cards
Squamous cell carcinoma is caused by what?
Dysplasia of squamous epithelium
8
New cards
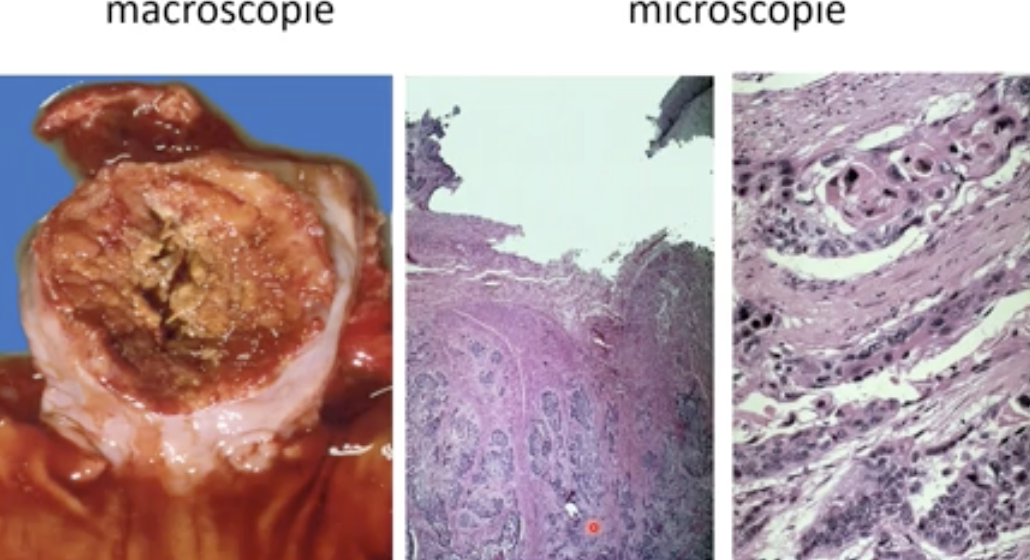
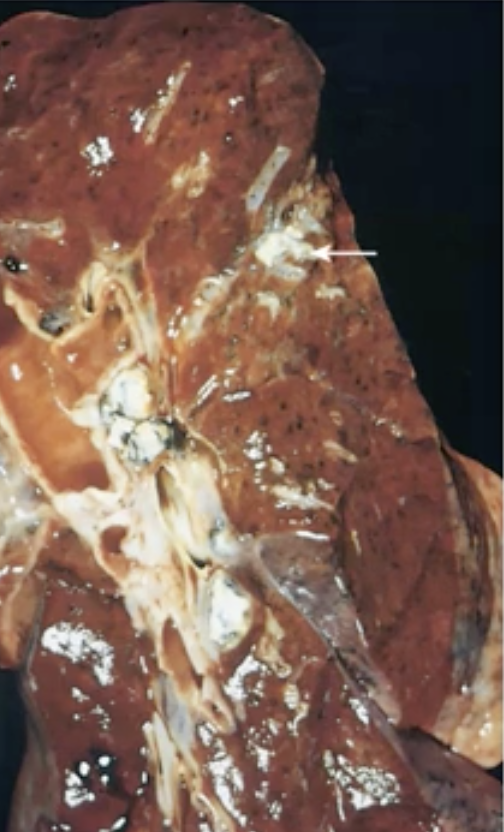
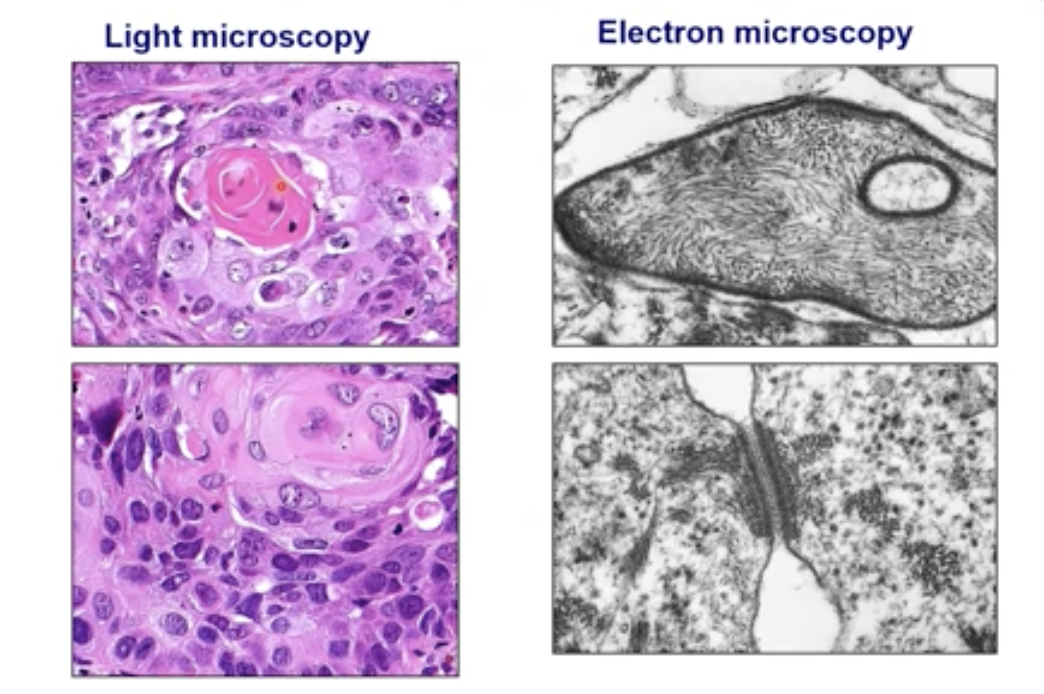
What does squamous cell carcinoma look like?
9
New cards
What does a healthy stomach look like ?

10
New cards
The gastric mucosa is made of three layer, what are they?
Foveolar (cells that make mucous) - glandular - Smooth muscle (in to out)
11
New cards
What are the two most important types of cells found in the glandular layer of the gastric mucosa?
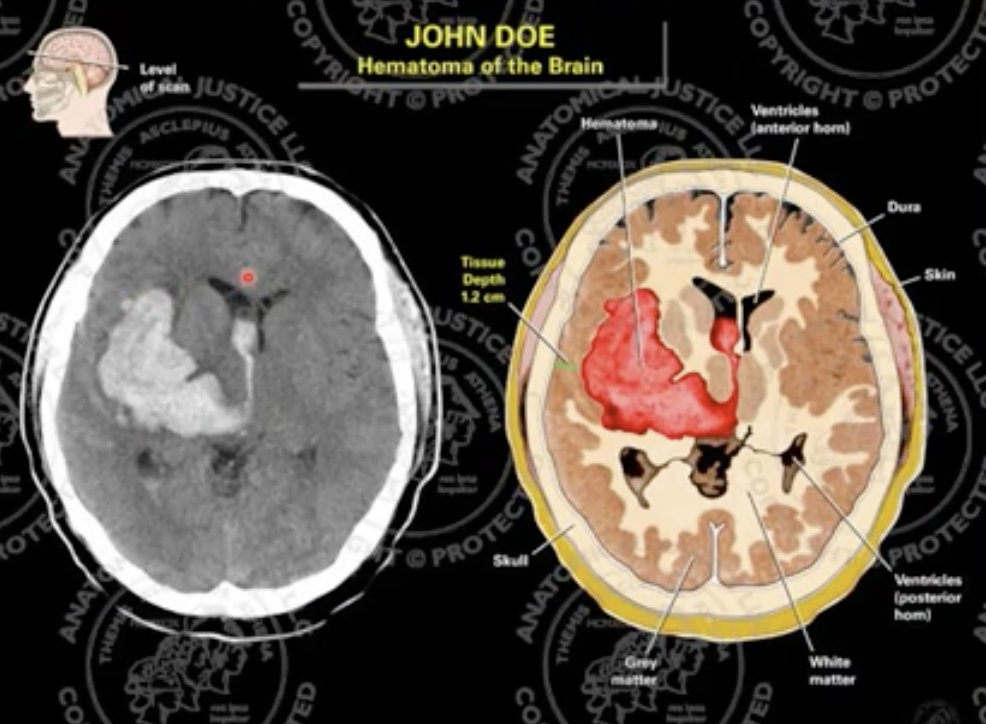
Parietal cells → produce acid and intrinsic factor (important protein for uptake of B12)
Chief cells → make pepsinogen (when in contact with acid it breaks down into smaller molecules to digest food)
These two types are not present in the antrum
Chief cells → make pepsinogen (when in contact with acid it breaks down into smaller molecules to digest food)
These two types are not present in the antrum
12
New cards
The antrum of the stomach houses important hormone producing cells, what hormone and what is its function?
Gastrin → stimulates prod of acidic fluid by the parietal cells and regulates it.
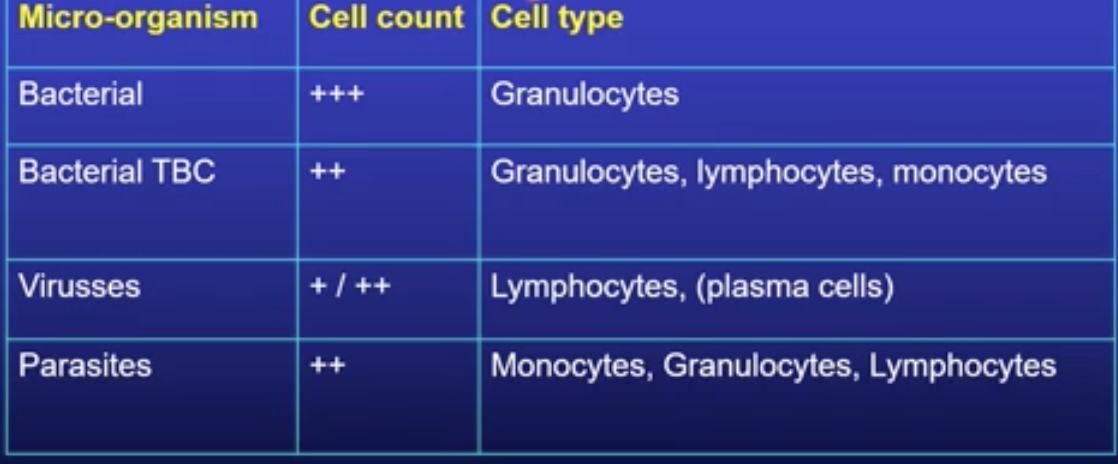
13
New cards
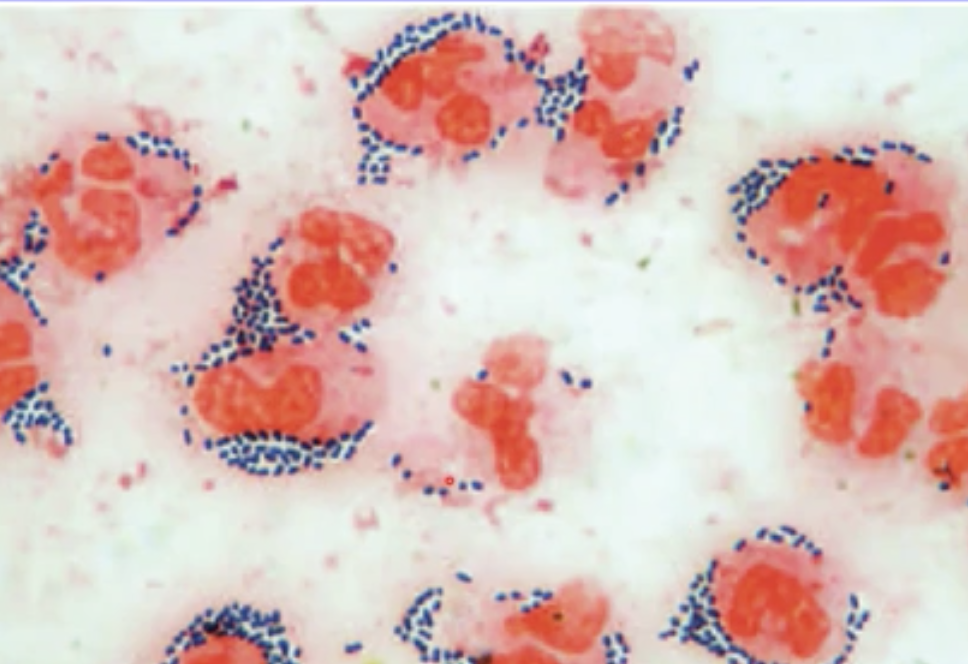
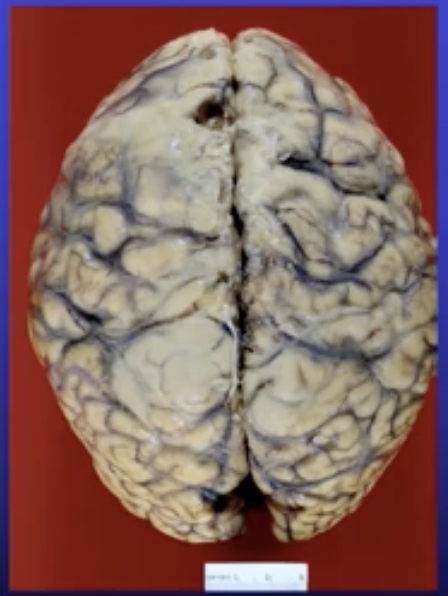
What is H.pylori?
A bacteria that causes inflammation of the stomach → acute gastritis
14
New cards
Auto-immune gastritis, what causes it and what happens?
* ABs against parietal cells and intrinsic factor
* Intestinal metaplasia because cells try to replace the missing ones but differentiate into intestinal cells instead
* Neuronal-endocrine cell hyperplasia because G cells keeps stimulating production of acid
* Loss of intrinsic factor = No uptake of B12 = Anemia
* Increased risk for adenocarcinoma and neuroscience-endocrine tumour
* Intestinal metaplasia because cells try to replace the missing ones but differentiate into intestinal cells instead
* Neuronal-endocrine cell hyperplasia because G cells keeps stimulating production of acid
* Loss of intrinsic factor = No uptake of B12 = Anemia
* Increased risk for adenocarcinoma and neuroscience-endocrine tumour
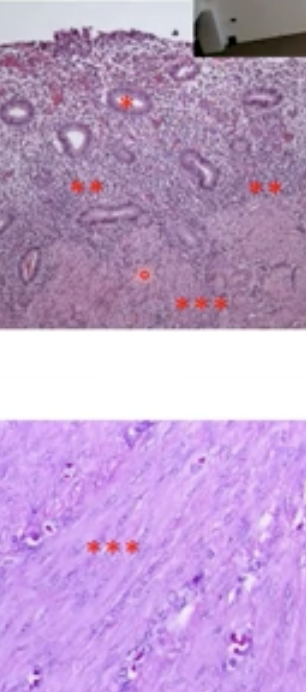
15
New cards
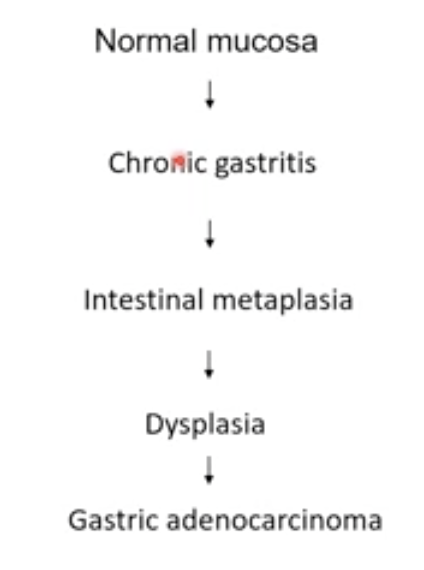
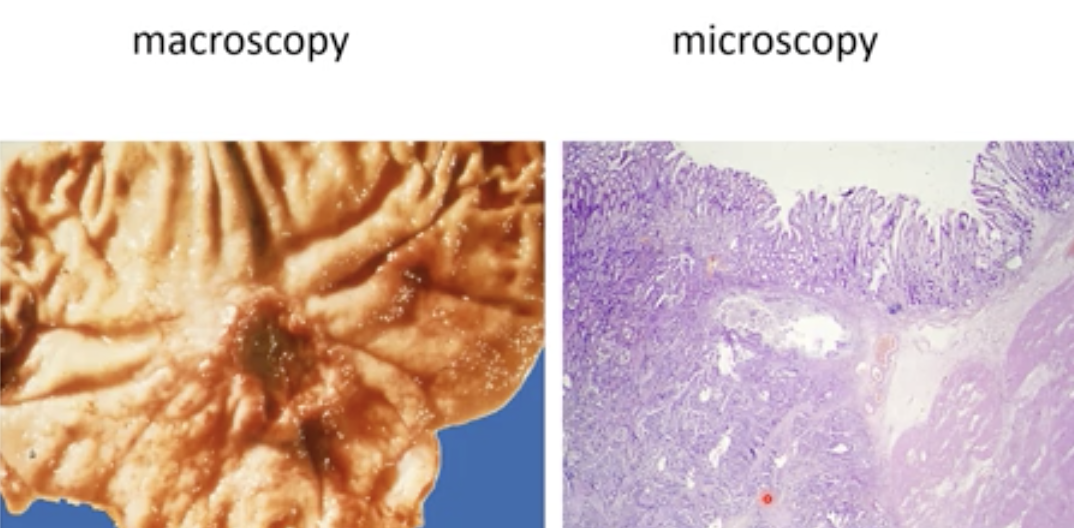
What does gastric adenocarcinoma (intestinal type) look like?
“Intestinal type” just because the precursor is intestinal metaplasia → but it is not in the bowel its in the stomach
16
New cards
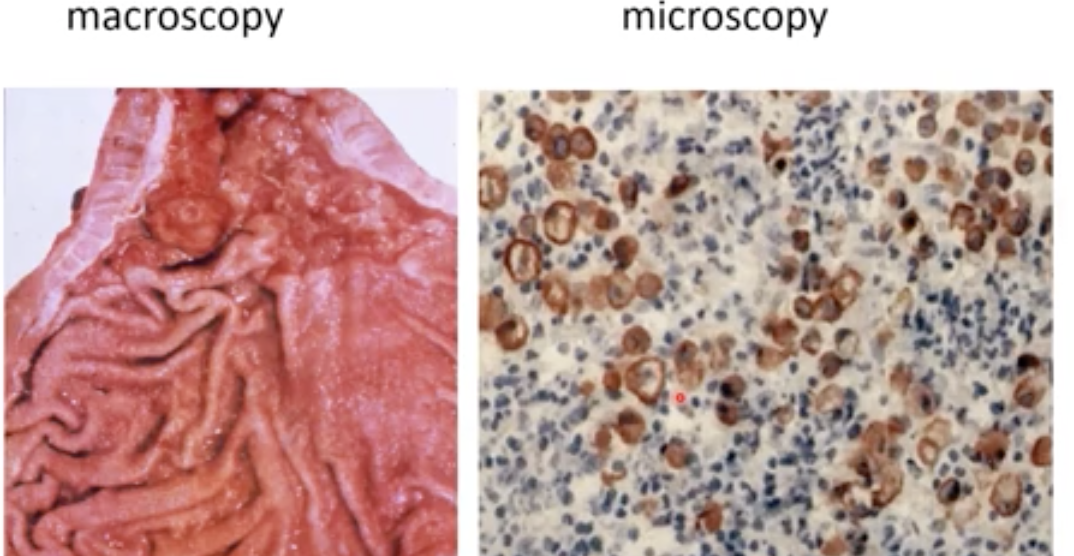
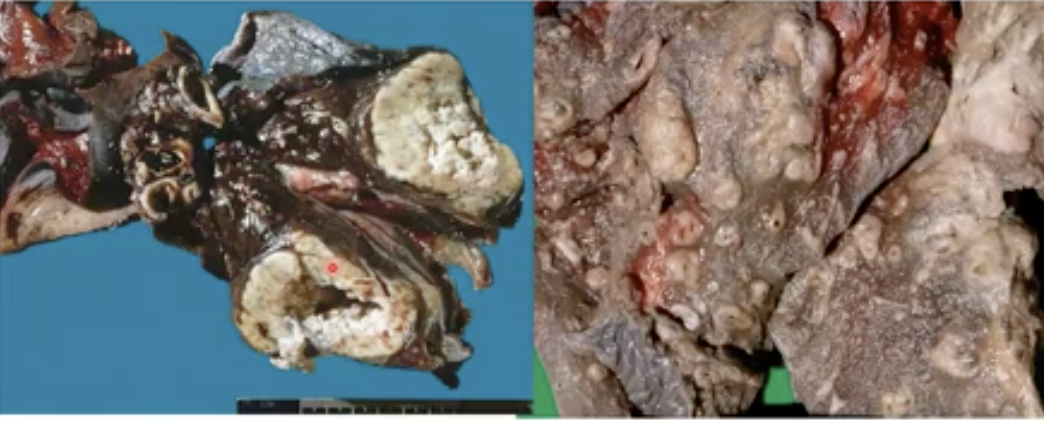
What does gastric adenocarcinoma (diffuse type) look like?
The tumour is everywhere so the organ looks the same but the wall thickens. By blowing air into the stomach we can see if the wall is stiff → bad sign
* The brown cells are tumour cells even if they are individual → why we call it diffuse type
* They are associated with pertineal metastasis (abdominal wall)
* The brown cells are tumour cells even if they are individual → why we call it diffuse type
* They are associated with pertineal metastasis (abdominal wall)
17
New cards
What are the three forms of cancer prevention?
Etiology → Primary prevention (avoidance)
Pathogenesis → Secondary prevention & diagnostics (discovery and removal of small cancers before they develop)
Tumour biology → Therapy
Pathogenesis → Secondary prevention & diagnostics (discovery and removal of small cancers before they develop)
Tumour biology → Therapy
18
New cards
Which form of cancer prevention does the “Population based screening for colorectal cancer” fall under and why?
Secondary prevention
* Identifying high risk subjects (55yr to 80yrs)
* Early detection
Because late stage → poor prognosis
* Identifying high risk subjects (55yr to 80yrs)
* Early detection
Because late stage → poor prognosis
19
New cards
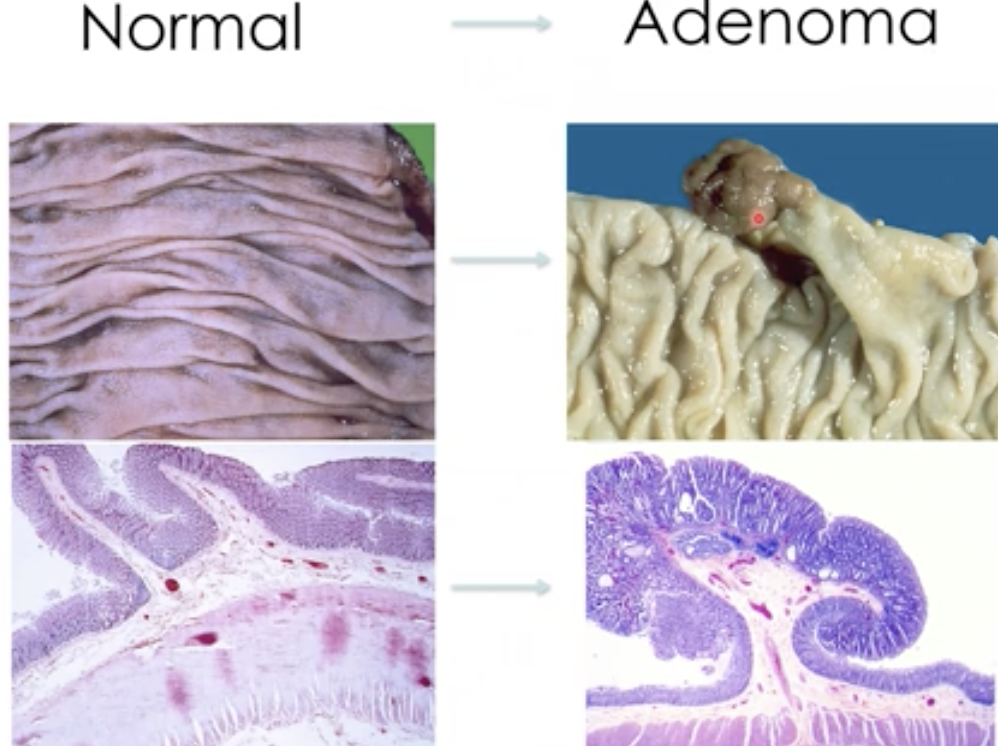
What is an adenoma ?
A type of polyp that is caused by dysplasia and results in adenocarcinoma - A precursor to colorectal cancer
20
New cards
95% of adenomas do not progress to CRC, what is the issue then?
We do not know which polyps COULD progress so we have to remove all of them - the progression could take from 10-15yrs which gives enough time for removal
21
New cards
What are the characteristics of an adenoma that is likely to progress to CRC? aka an advanced adenoma
* High grade dysplasia (the more irregular the cells)
* size > 10mm
* Villous component (fingerlike structure → higher risk of progression)
* size > 10mm
* Villous component (fingerlike structure → higher risk of progression)
22
New cards
How does a carcinoma arise in an adenoma?
Adenoma → Malignant polyp → Carcinoma

23
New cards
85% of CRC cases are caused by chromosomal instability, explain?
* Abnormal number of chromosomes (usually three copies of a chromosome)
* Translocations between chromosomes
* Translocations between chromosomes
24
New cards
15% of CRC cases are caused by microsatellite instability, explain?
* An accumulation of point mutations
25
New cards
Mutations and chromosomal abnormalities are not the only clues for CRC, what else can be intervened with for better detection in the screening program?
* Epigenentic changes ex. methylation
* Mutations in the mRNA, miRNA, Protein
* Abnormal proteins = mutations somewhere in the translation or transcription of the DNA or RNA
* Mutations in the mRNA, miRNA, Protein
* Abnormal proteins = mutations somewhere in the translation or transcription of the DNA or RNA
26
New cards
What is the hallmark of interstitial lung disease?
Stiffening of the lung
27
New cards
Give an example of a restrictive lung disease?
Asbestosis
28
New cards
What does a healthy trachea look like?
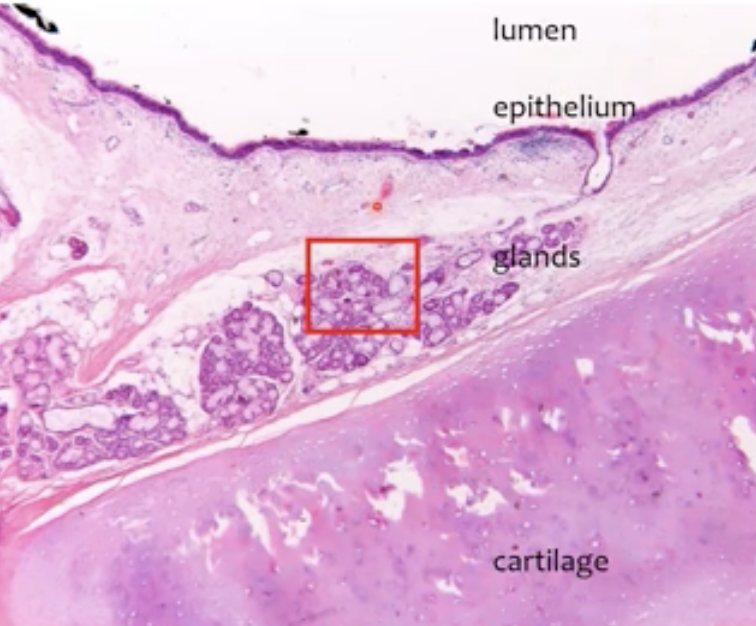
29
New cards
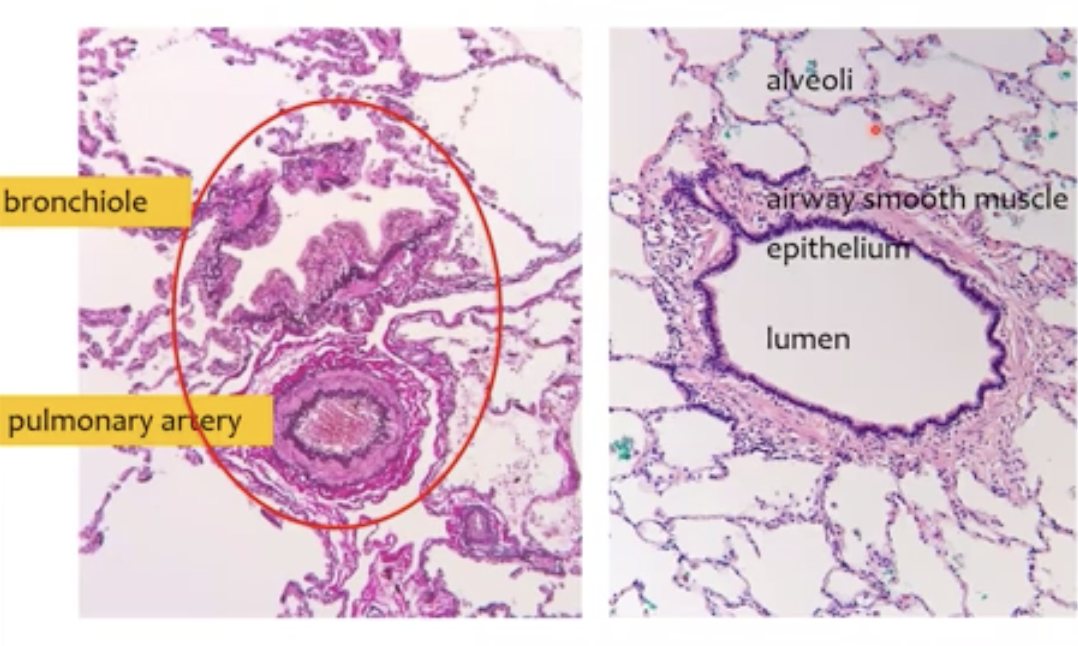
What does a bronchiole look like?
\
30
New cards
What are the disease that arise from ciliary malfunction in the airway?
* Ciliary dyskinesia syndrome
* Kartagener syndrome
* Smoking can also cause malfunction
* Kartagener syndrome
* Smoking can also cause malfunction
31
New cards
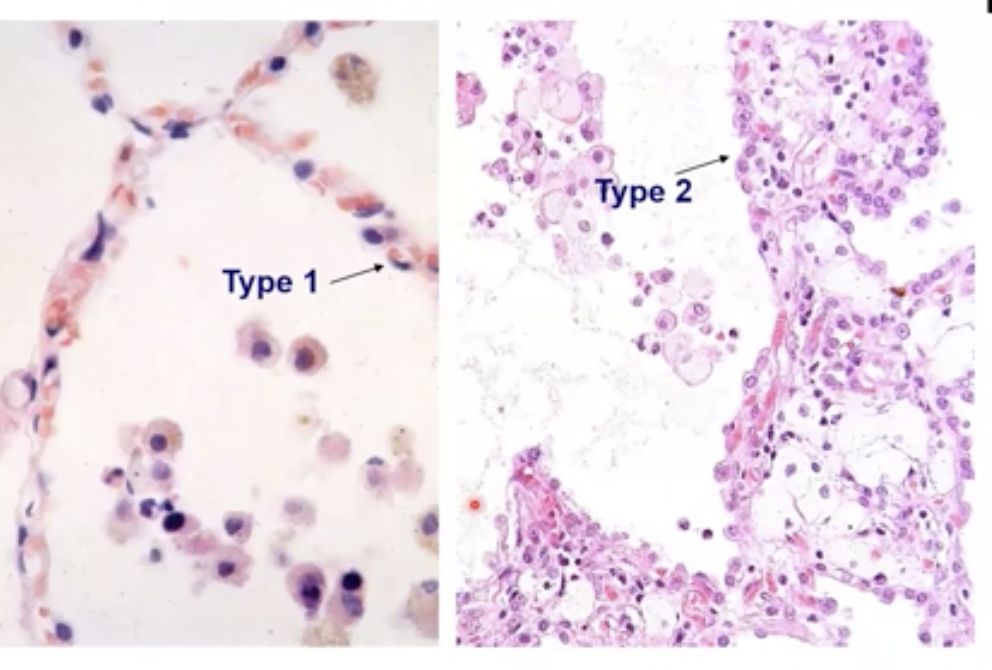
What substance do type 2 pneumocystis and Clara cells produce?
Surfactant
32
New cards
The pulmonary circulation is low flow, high pressure system. True or False ?
False, its high flow, low pressure
33
New cards
What is atelectasis ?
Collapse of the lung
34
New cards
Diffuse alveolar damage is also knows as __ __and is caused by__ ___
Aka ARDS or Adult respiratory insufficiency (clinical name) it is caused by:
* Hypoxemia (not enough O2)
* Pulmonary oedema
* Multi-organ failure (not enough O2)
* Poor prognosis
* Hypoxemia (not enough O2)
* Pulmonary oedema
* Multi-organ failure (not enough O2)
* Poor prognosis
35
New cards
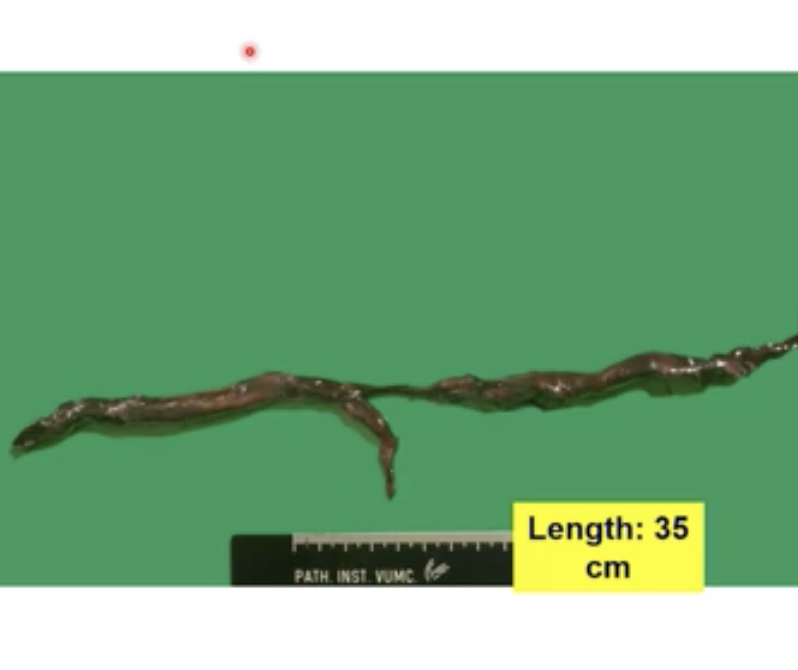
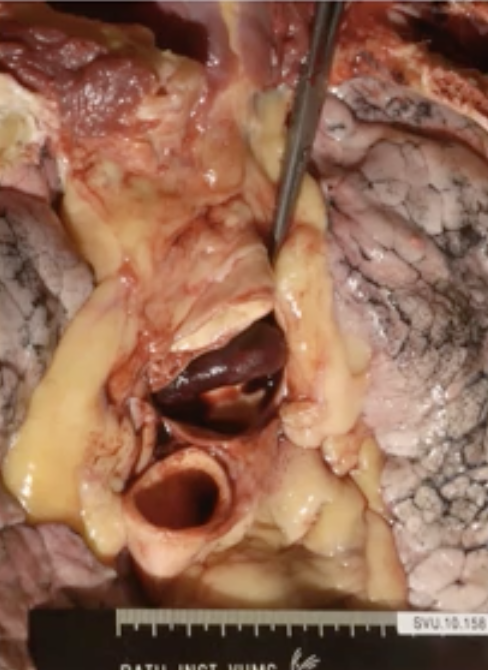
What causes a saddle pulmonary embolism?
When someone sits still for a long time they could develop a thrombus in the leg, when they stand up and the circulation is fast again this thrombus travels to the heart and to the lungs → this is what causes a Saddle pulmonary embolism (when the thrombus is big). The saddle is where the thrombus is trapped. LETHAL
36
New cards
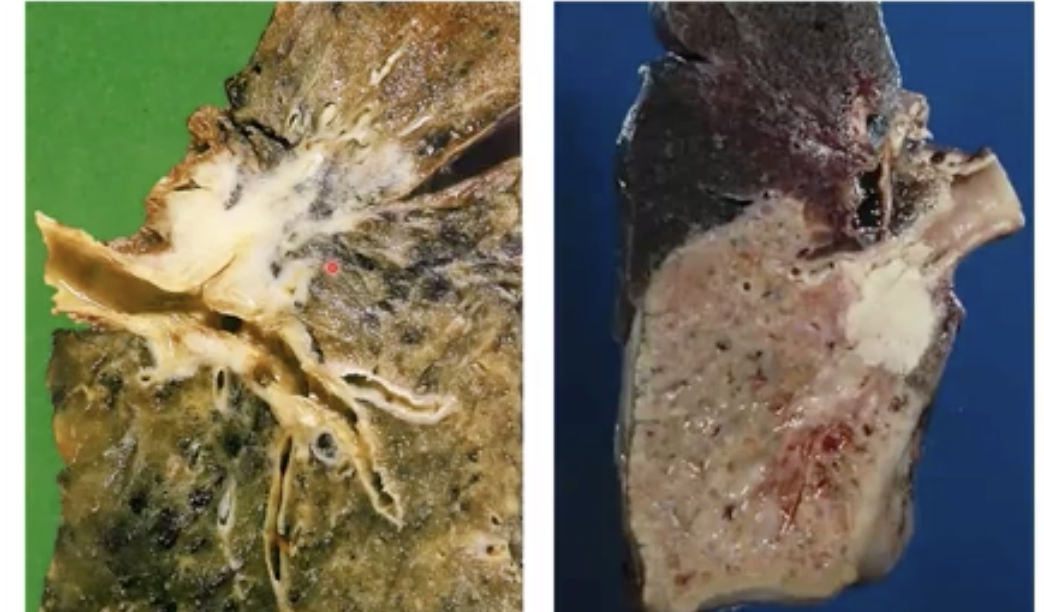
What can the thromboembolism cause? What does it look like?
Lung infarction → Not enough supply of O2 to the lung tissue
\
\
37
New cards
What is the main difference between instructive and restrictive lung disease?
Obstructive → Difficulty exhaling
Restrictive → Difficulty inhaling
Restrictive → Difficulty inhaling
38
New cards
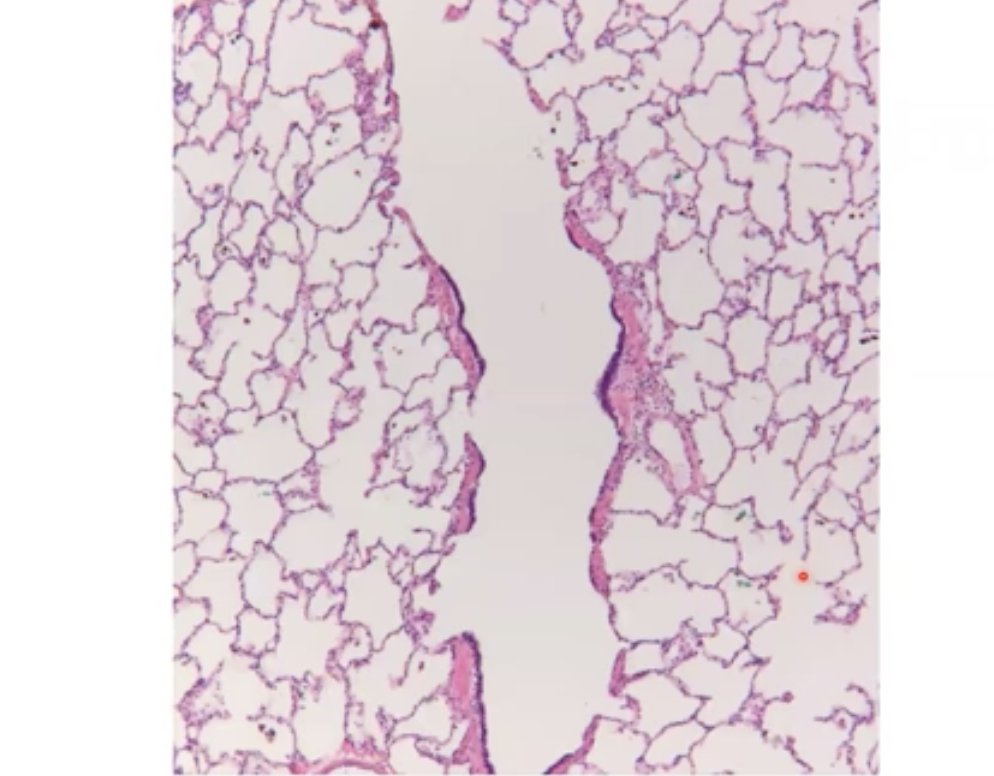
If normal lung tissue looks like this →
How does emphysema look?
How does emphysema look?
Gas exchange is not efficient because the surface area now is a lot smaller, typically happens in smokers
39
New cards
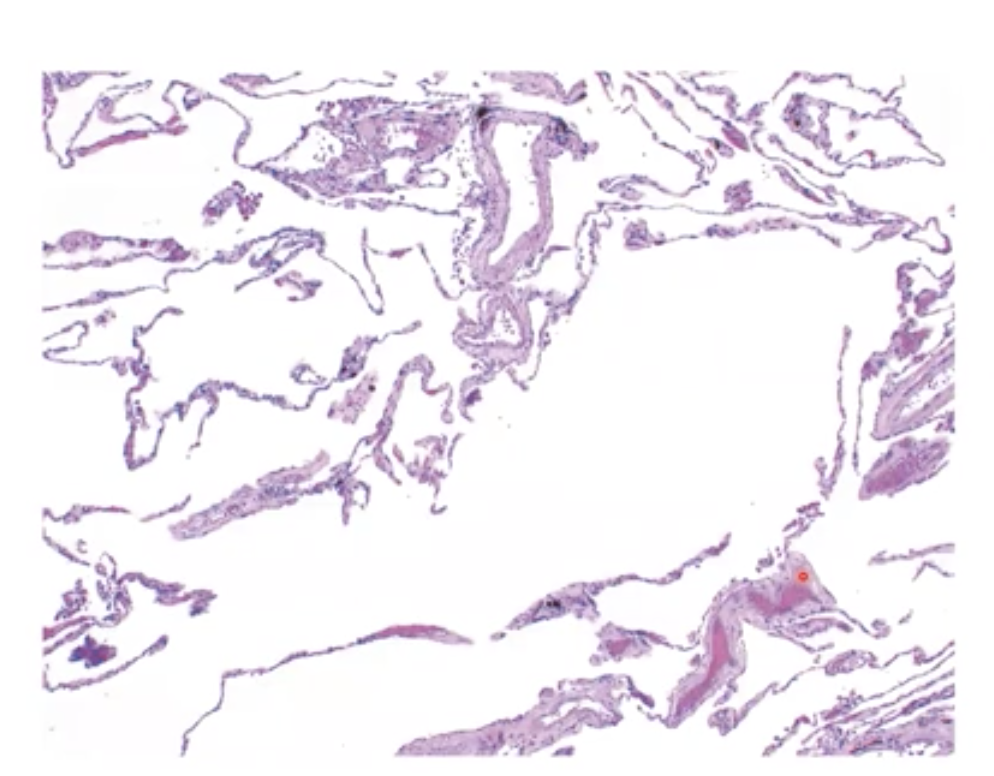
Emphesyma on gross examination of the lungs look like __it is a__ ____ lung disease
The dar smooth part is normal but the white parts are expanded alveoli
Emphesyma is an example of obstructive lung disease
Emphesyma is an example of obstructive lung disease
40
New cards
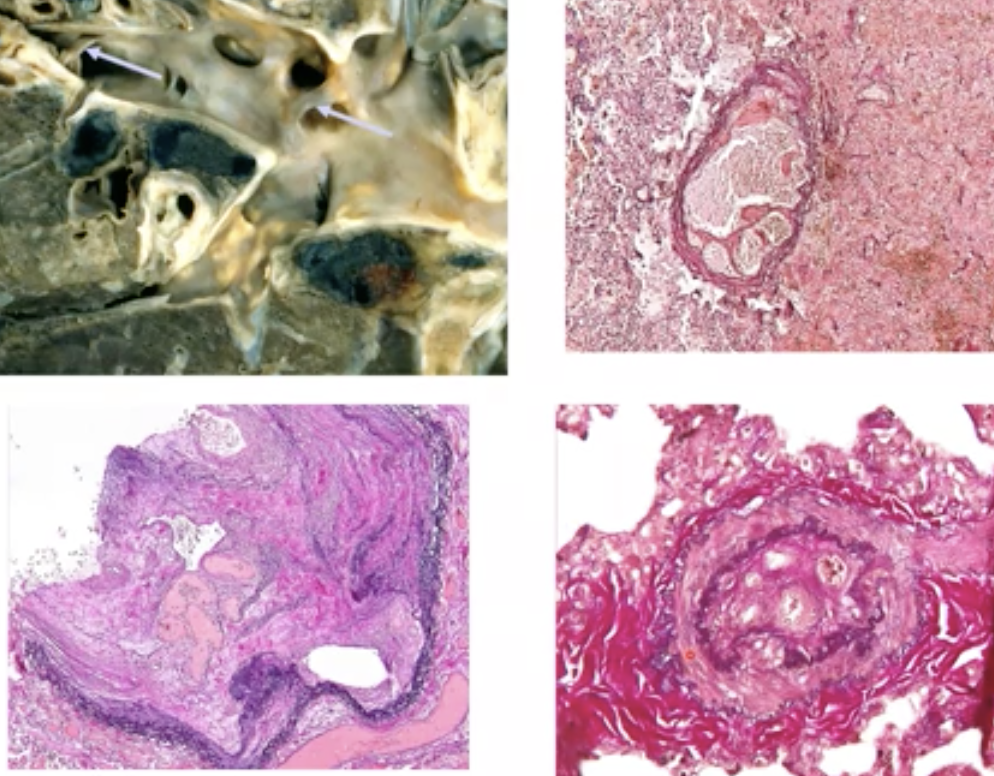
What is silicosis and what causes it?
Occurs in miners, causes stiffening of the lung tissue
41
New cards
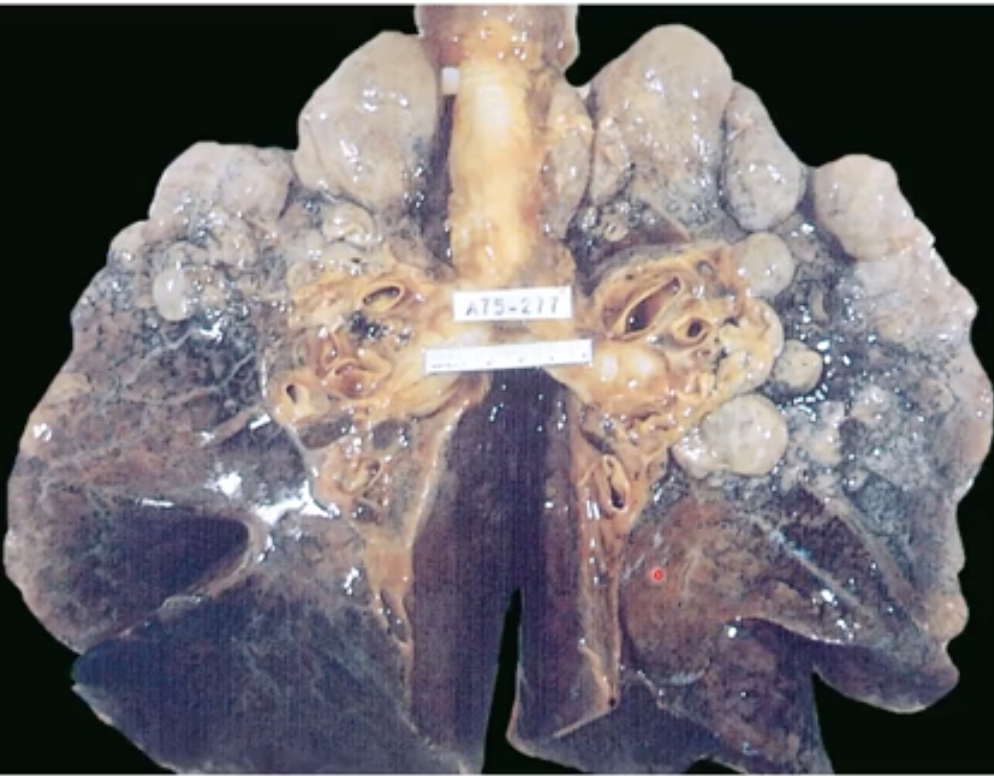
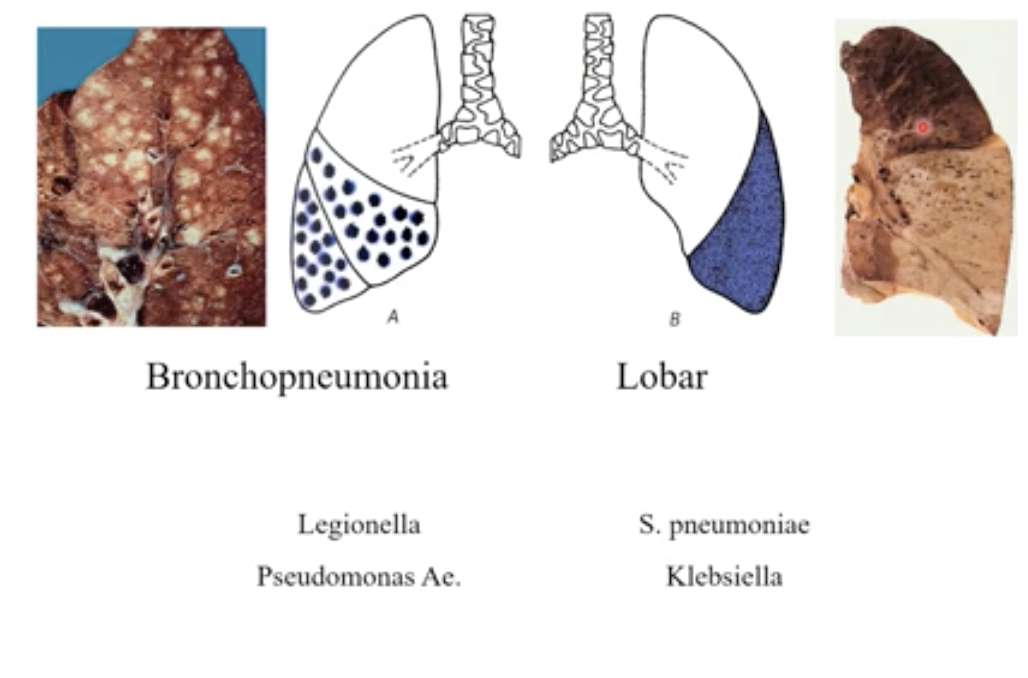
What are the two types of pneumonia? Explain their causes and symptoms
Bronchopneumonia → when the bacteria go into the bronchioles and alveoli and eat at the tissue (can be seen outside the lung
Lobar → the whole lobe is filled with bacteria
Lobar → the whole lobe is filled with bacteria
42
New cards
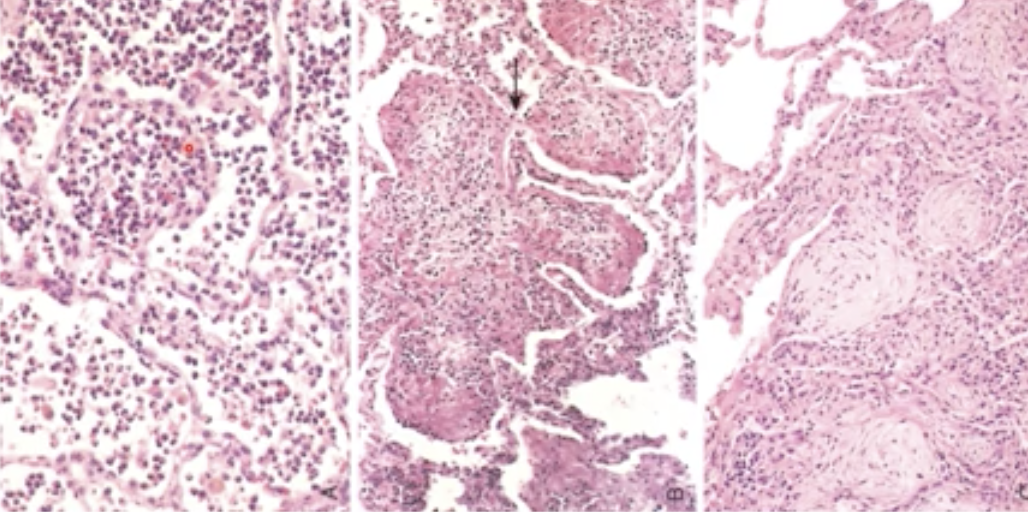
What does acute pneumonia look like over time?
Diffuses on its own
43
New cards
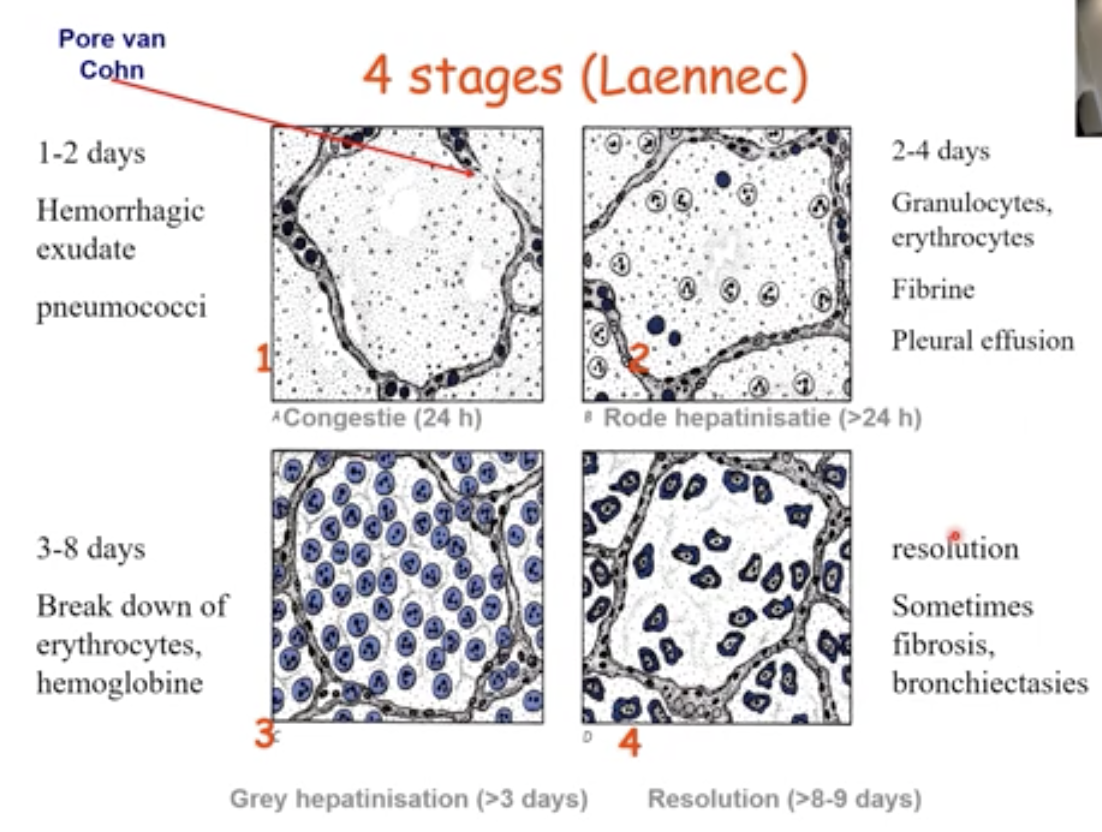
There are 4 stages of pneumonia, what are they characterised by?
1: 1-2 days Congestion
2: 2-4 days Red hepatization
3: 3-8 days Grey hepatization
4: Resolution (immune cells clear the infection)
2: 2-4 days Red hepatization
3: 3-8 days Grey hepatization
4: Resolution (immune cells clear the infection)
44
New cards
What causes tuberculosis and what are the symptoms ?
* Infection of the lung caused by mycobacteria
* the first infection is not severe but results in remnants in the lung
* the first infection is not severe but results in remnants in the lung
45
New cards
What is the hallmark of tuberculosis ? And where is it shown on the picture
* Epitheloid Granulomas and mutinucleated macrophages + necrosis are all hallmarks of tuberculosis
* The red dots
* The red dots
46
New cards
What is the mechanical form of protection against lung infections?
Mucociliairy transport + Coughing reflex
47
New cards
What is the immunological form of protection against lung infections?
* IgA secretion in bronchial mucus
* Humoral and cellular immune response
* Humoral and cellular immune response
48
New cards
What cells are responsible for phagocytosis of bacteria that causes lung infections?
* Alveolar macrophages
* Neutrofilic granulocyte
* Neutrofilic granulocyte
49
New cards
What defines an adenocarcinoma?
A cancer that starts in mucus producing (glandular) cells which a lot of organs house so it can happen in almost any organ.
50
New cards
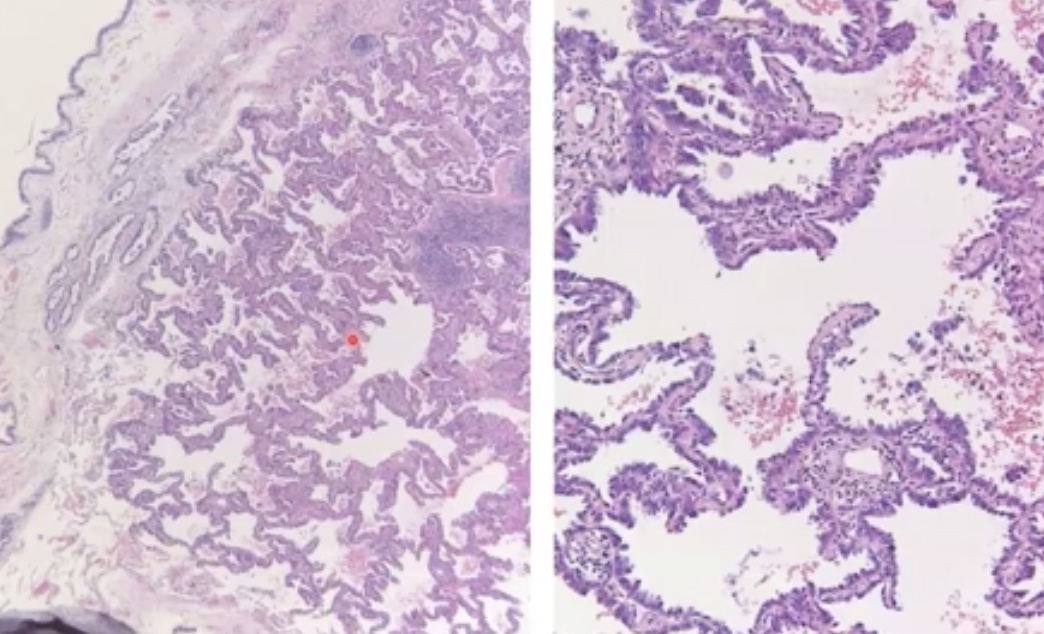
The histology of an adenocarcinoma in the lungs looks like this, how do it look on the organ itself ? What category of carcinoma does it fall under?
Non-small cell carcinoma
51
New cards
What does squamous cell carcinoma look like in the lung and what is the major cause ? What category of carcinoma does it fall under?
98% of cases are smoker
Non-small cell carcinoma
Non-small cell carcinoma
52
New cards
An important form of neuroendocrine carcinoma is the _____ where the cartilage below the trachea is affected
Small cell carcinoma - mean survival without treatment is only 2-4 months.
Responds well to chemo but only at first
Responds well to chemo but only at first
53
New cards
What is the gefitinib ?
A tyrosine kinase inhibitor for cases where the mutation is found on the EGFR gene (the mutation = increased growth factor signalling) - Screening for this mutation is important to identify patients who will response well to Gefitinib
54
New cards
Why are checkpoint inhibitor therapy useful for cancer treatment?
Checkpoint PDL1 molecules are present to prevent T cell from attacking own cells, which can include tumour cells.
Checkpoint inhibitor inhibit this function and allow the T cells to kill the antigen presented by the tumour cell
Checkpoint inhibitor inhibit this function and allow the T cells to kill the antigen presented by the tumour cell
55
New cards
what is the main difference between neuroglia and non neuroglia cells?
Neuroglia cells are derived from the neural tube while the non neuroglia cells migrate from outside the neural tube to the developing central nervous system
56
New cards
Give 3 examples of non neuroglia cells?
Fibroblasts, smooth muscle cells, endothelium, microglia
57
New cards
What cells are considered neuroglia cells?
Neurons, Astrocytes and oligodendrocytes
58
New cards
How do oligodendrocytes work?
Their cell body wraps around the axon to make the myelin sheaths. They also interact with the axon by providing it with nutrients, especially long axons that would lose energy transporting it from one side to the other.
59
New cards
What are the functions of astrocytes?
* they maintain the blood brain barrier when interacting with vessels
* they uptake neurotransmitters lost in the synaptic cleft and participate in synaptic communication
* they control ion-water homeostasis
* they release energy substrates
* orchestrate remyelination and myelin maintainance
* React to injury
* they uptake neurotransmitters lost in the synaptic cleft and participate in synaptic communication
* they control ion-water homeostasis
* they release energy substrates
* orchestrate remyelination and myelin maintainance
* React to injury
60
New cards
What do the microglia do?
Immune response of the brain together with the astrocytes. They can become phagocytic microglia that eat up debris from injury which is important for recovery
61
New cards
A stroke is what type of injury? what is it caused by?
It is considered a cerebrovascular accident and ischemic
because the brain is very sensitive to lack of O2 (prevented via the Circle of Willis)
because the brain is very sensitive to lack of O2 (prevented via the Circle of Willis)
62
New cards
What causes a lack of O2 in the brain and therefore a stroke?
* Arterial Obstruction due to vessel wall disease such as atherosclerosis or vasculitis
* Arterial obstruction due to an embolus (piece of thrombus that clogs a small enough vessel)
* Reduced perfusion due to hypotension, heart infarct or severe bleeding in the body
* Reduced O2 uptake due to suffocation or CO intoxication
* Arterial obstruction due to an embolus (piece of thrombus that clogs a small enough vessel)
* Reduced perfusion due to hypotension, heart infarct or severe bleeding in the body
* Reduced O2 uptake due to suffocation or CO intoxication
63
New cards
What are the 4 afferent arteries in the brain?
2 carotid and 2 vertebral that create an anastomosis in the base of the brain → CoW
64
New cards
What are the arteries that depart from the CoW?
* 3 terminal
* 2 Anterior cerebral
* 2 Medial Cerebral
* 2 Posterior cerebral
* Very few anastomosis except the CoW
* 2 Anterior cerebral
* 2 Medial Cerebral
* 2 Posterior cerebral
* Very few anastomosis except the CoW
65
New cards
Why do some stroke survivors lose the abilitiy to speak or understand language?
Stroke in Broca or Wernickes (in the left side of the brain)
66
New cards
What is characteristic of an ischemic cerebrovascular accident?
Little blood, brain becomes necrotic in that area and creates a hole from the affected tissue. Caused by an occlusion of a vessel
67
New cards
Haemorrhagic cerebrovascular accidents are characterised by?
A broken blood vessel and lots of blood in that area which compresses the vessels around it → lack of O2 → Necrosis in area of ischemia
Main cause is hypertension, malformations of blood vessels (ex artery-venous malformations where the artery and the vein are directly connected)
\
Main cause is hypertension, malformations of blood vessels (ex artery-venous malformations where the artery and the vein are directly connected)
\
68
New cards
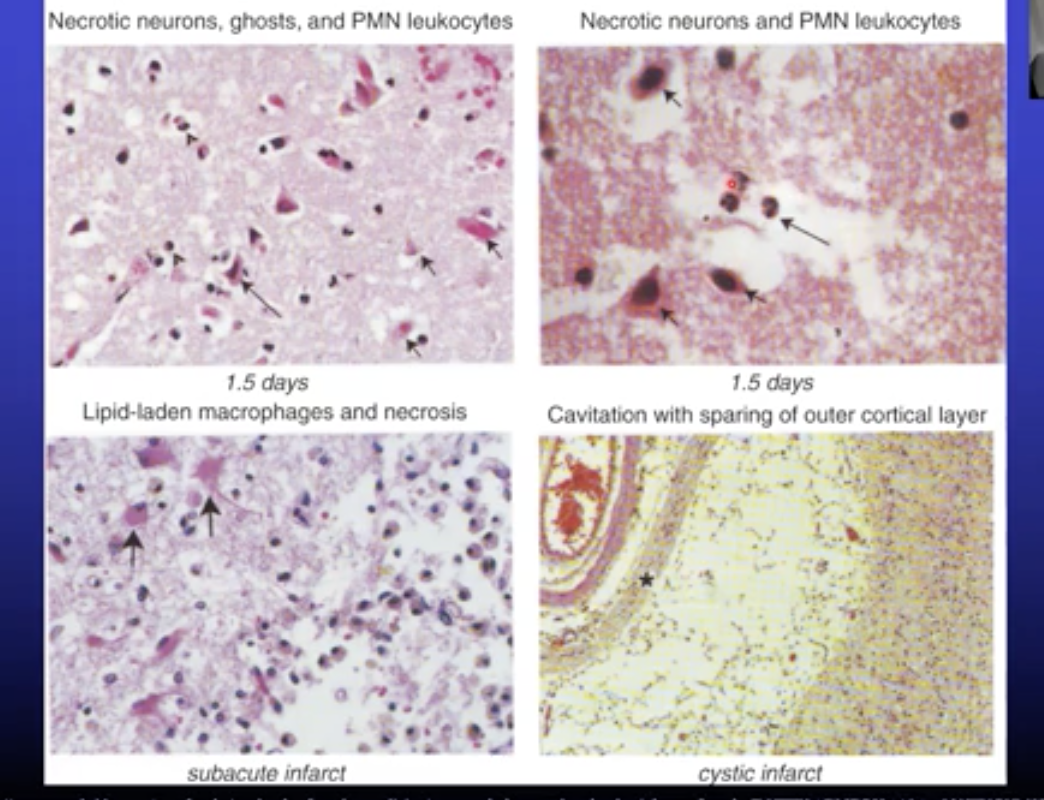
What are the cellular consequences of ischemia ?
* Neuronal damage and death → neurons becomes red
* Loss of myelin (oligodendrocyte loss of function)
* Death of glia cells
* Loss of tissue with clearing reaction via influx of granulocytes and macrophages (colliquation, when the damaged tissue becomes liquid)
* Cavitation (a hole)
* Loss of myelin (oligodendrocyte loss of function)
* Death of glia cells
* Loss of tissue with clearing reaction via influx of granulocytes and macrophages (colliquation, when the damaged tissue becomes liquid)
* Cavitation (a hole)
69
New cards
Simply defined, ischemia is a lack of __*and causes*__
lack of blood, causes hypoxia
70
New cards
Name the types of extra axial cerebral hemorrhages
Epidural (between skull and dura)
Subdural (between dura and arachnoid)
Subarachnoidal (between arachnoid and Pia)
Subdural (between dura and arachnoid)
Subarachnoidal (between arachnoid and Pia)
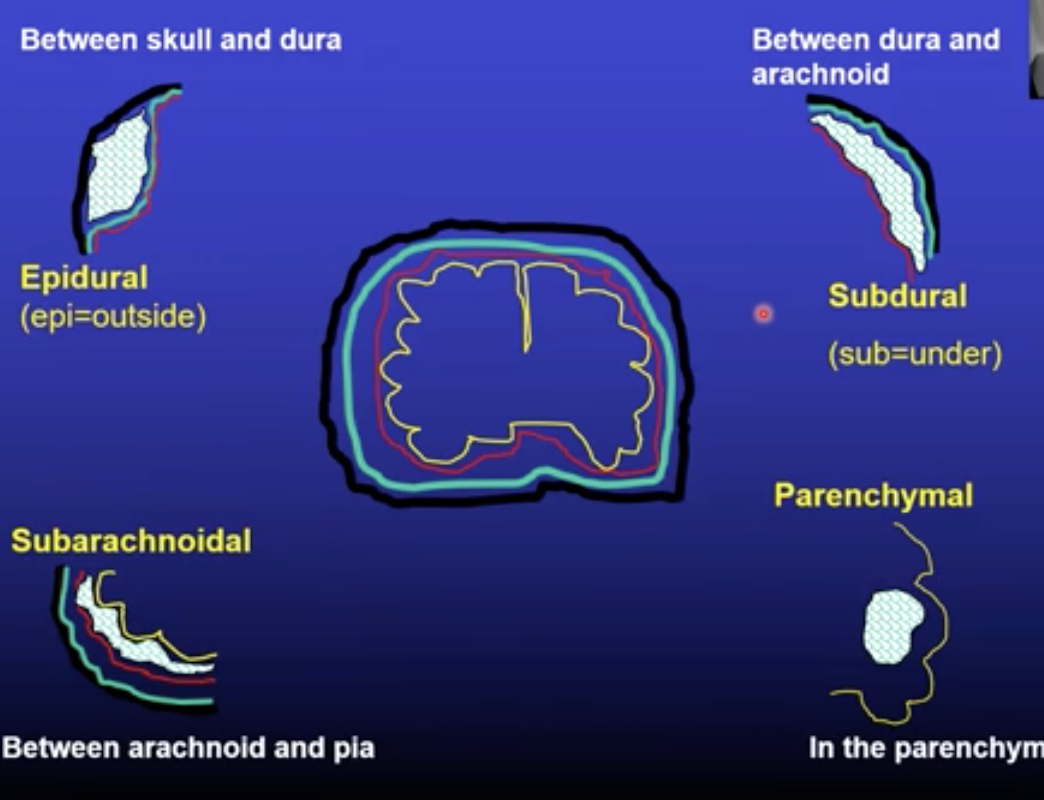
71
New cards
What is the only intra-axial (in the brain) type of haemorrhage called ?
Intra parenchymal
72
New cards
What are the causes and consequences of sub (venous) and epi (arterial) dural haemorrhages?
Trauma
Progressive deterioration of consciousness → death
Therapy : decompression via a hole in the skull to let the blood flow out
Progressive deterioration of consciousness → death
Therapy : decompression via a hole in the skull to let the blood flow out
73
New cards
What are the causes and consequences of subarachnoid haemorrhages?
cause behind aneurysms (damage and wearing of blood vessels)
Severe headache and sudden loss of consciousness
Therapy : Insert a coil and clog it to stop the bleeding
Severe headache and sudden loss of consciousness
Therapy : Insert a coil and clog it to stop the bleeding
74
New cards
What is the most severe type of haemorrhage and what causes it ?
**Intraparenchymal**
causes fast increase in intracranial pressure, 80% mortality rate.
caused by **hypertension**, blood thinners / anticoagulants, trauma
causes fast increase in intracranial pressure, 80% mortality rate.
caused by **hypertension**, blood thinners / anticoagulants, trauma
75
New cards
What is the difference between meningitis and Encephalitis ?
Meningitis is when the infection occurs in the meninges of the brain (most often bacterial
Encephalitis is when the infection starts in the meninges and extends to the brain or directly starts in the brain (most often viral)
Encephalitis is when the infection starts in the meninges and extends to the brain or directly starts in the brain (most often viral)
76
New cards
Evaluation of CSF is important, why?
Because observing what kind of cells are most prominent can give an idea on what kind of infection is in the brain (Bacterial, Viral or Parasitic)
77
New cards
What will a typical picture of bacterial meningitis look like?
78
New cards
What happened here?
The bacteria in the meninges stimulate the recruitment of neutrophils aka white blood cells which are white so it shows on the surface of the brain
79
New cards
How does herpes virus affect the brain?
Causes encephalitis, haemorrhage in temporal lobe. The virus uses the vessel to spread around the brain and find more host cells.
80
New cards
What is PML?
Its a virus infection via the JC virus and is most frequent in HIV patients before the current treatment - now its more commonly found in people who are immunocompromised (ex ppl who take immusuppressive treatment for MS) - Very severe and lethal
81
New cards
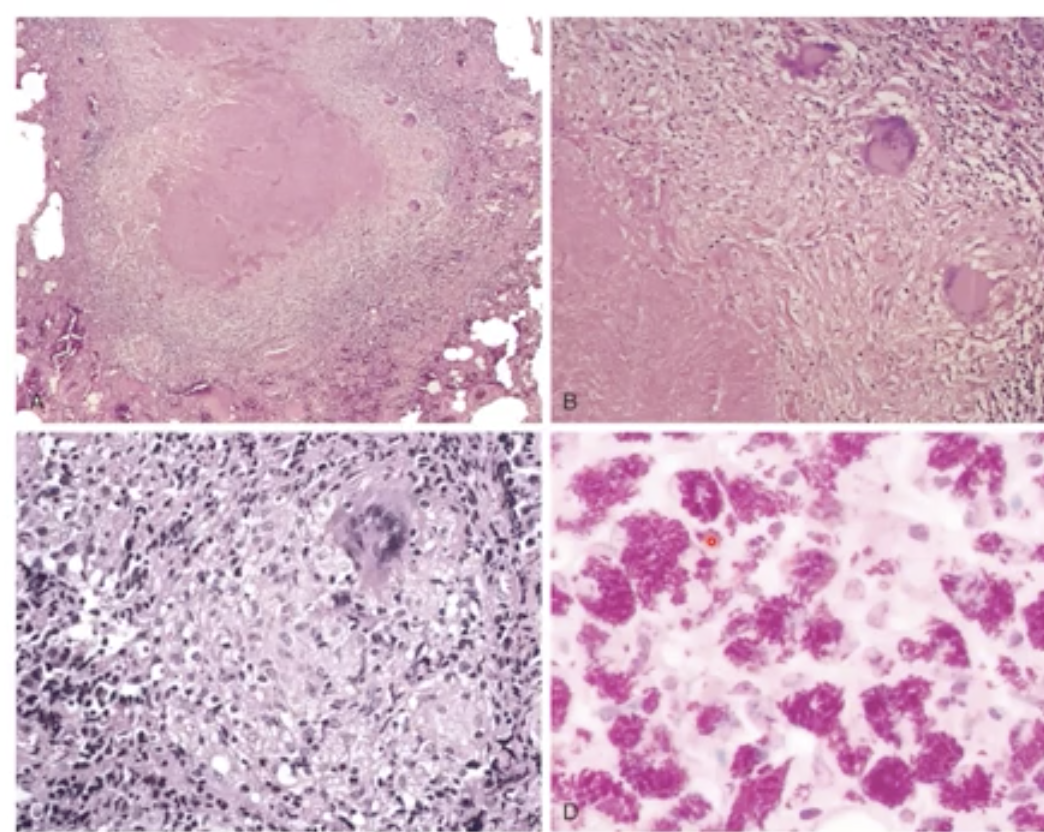
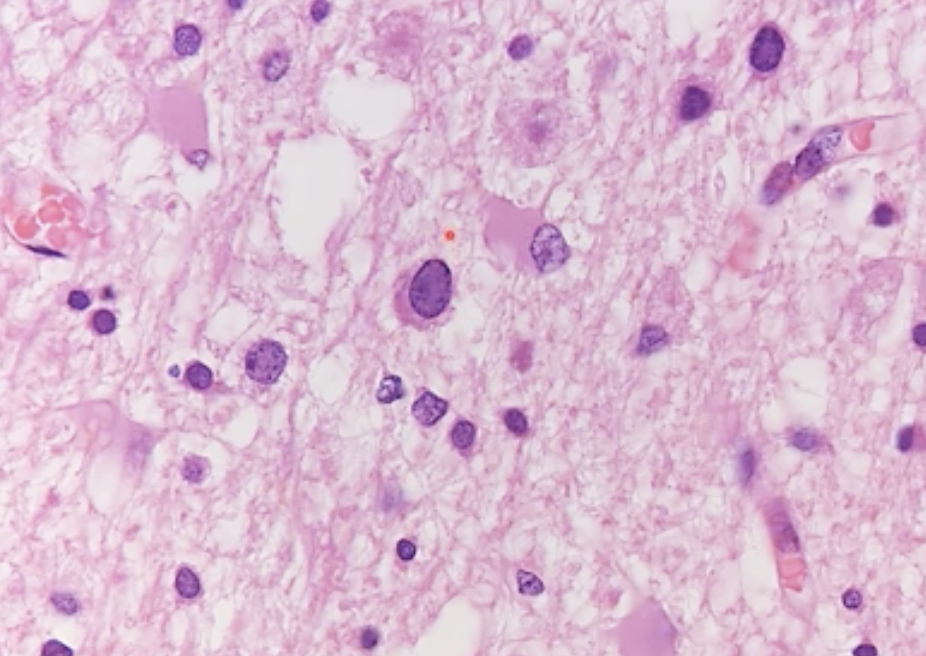
What does PML look like under the microscopic ?
The giant oligodendricite in the middle by the pointer has been infected by the JC virus. Astrocytes are also seen here because they are very actively trying to get rid of the infection
82
New cards
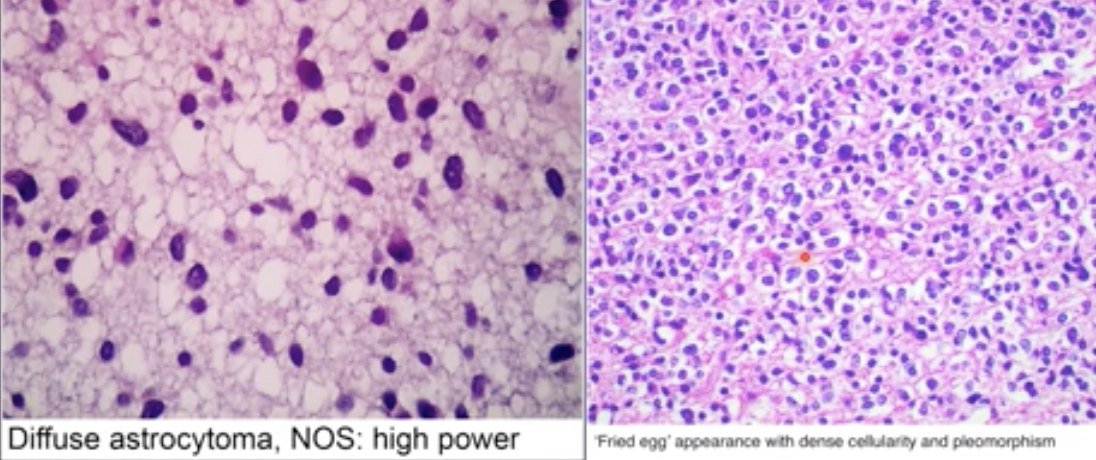
What are the most common types of CNS tumours?
Metastases (started in other organs and reached the brain)
83
New cards
Primary CNS tumours include what two types?
Gliomas → Astrocytomas, Oligodendrogliomas, Ependymomas..etc
Primitive Neuroscience Epithelial Tumours → Medulloblastoma (Children)
Primitive Neuroscience Epithelial Tumours → Medulloblastoma (Children)
84
New cards
What is the most common lung tumour that spreads to the CNS?
Pulmonary adenocarcinoma
85
New cards
What complications do gliomas usually present?
* They are very infiltrative and impossible to remove completely via surgery
* They never metastasise outside the CNS
* Presence/ Number of mitosis, Endothelial proliferation, Necrosis are all useful for prognosis grading
* Highest grade (WHO IV) → survival of only 1 year
* They never metastasise outside the CNS
* Presence/ Number of mitosis, Endothelial proliferation, Necrosis are all useful for prognosis grading
* Highest grade (WHO IV) → survival of only 1 year
86
New cards
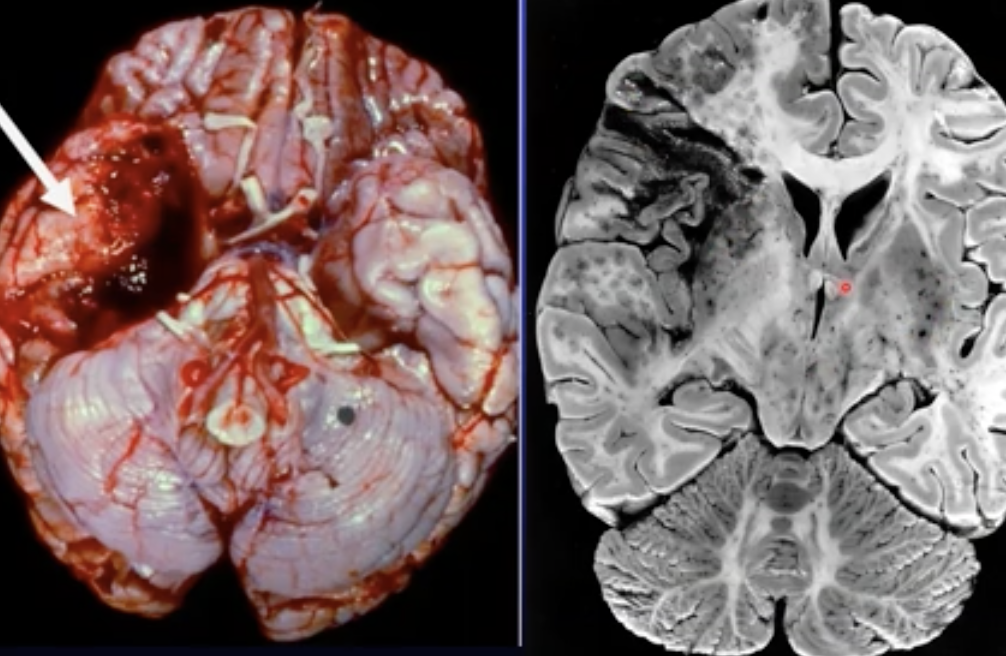
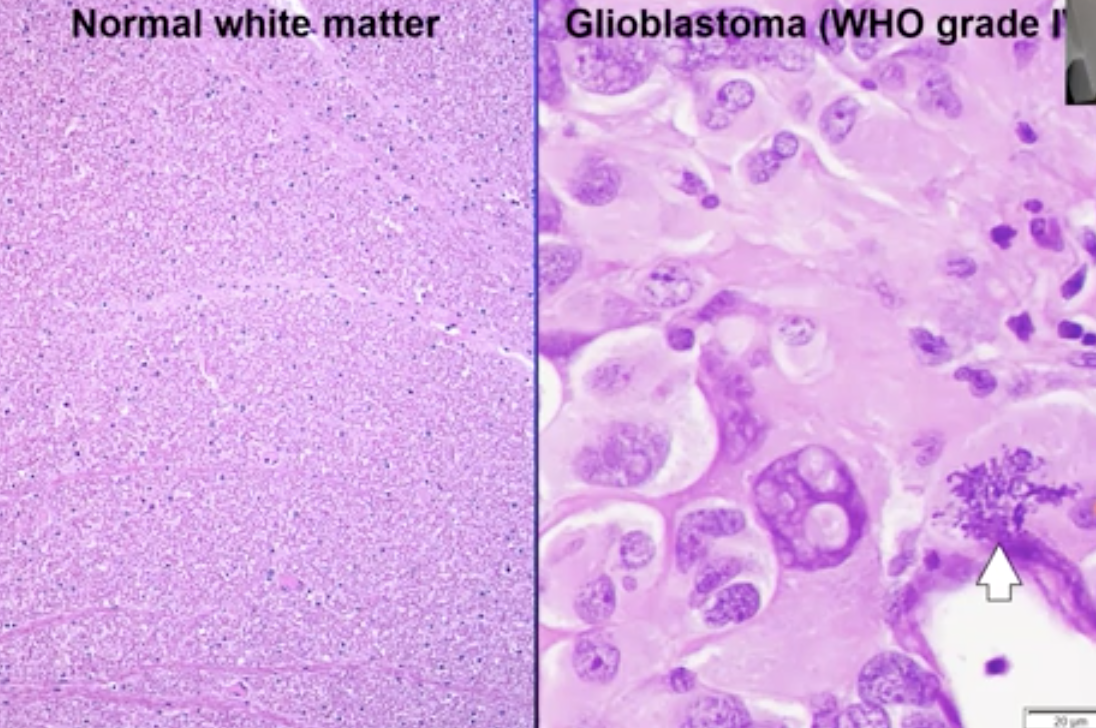
What is the most severe glioma ?
Glioblastoma (tumour of the precursors of glial cells). Arrow points are multiple mitosis processes happening at the same time in one cell
87
New cards
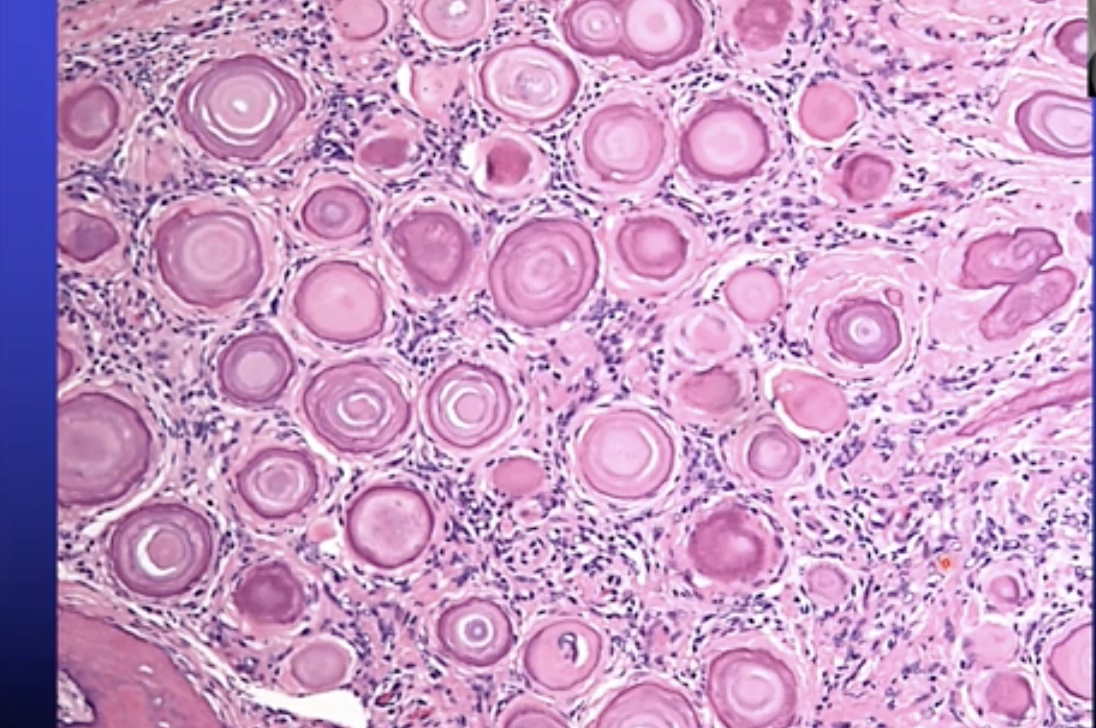
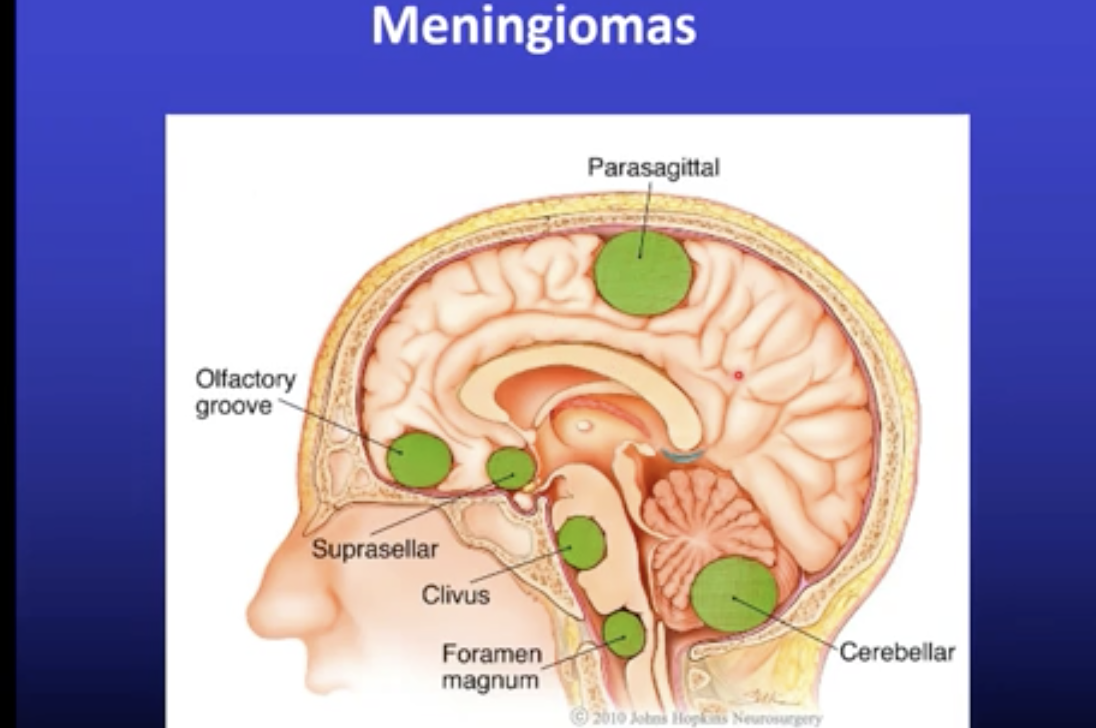
What are the tumours of the meninges called and what are there main characteristics ?
Meningiomas
* Located outside the CNS
* Grow slowly, few symptoms
* Occur more in females because they are sensitive to oestrogen
* Often benign
* Can be removed surgically
* Located outside the CNS
* Grow slowly, few symptoms
* Occur more in females because they are sensitive to oestrogen
* Often benign
* Can be removed surgically
88
New cards
What defines a carcinoma ?
Tumour of epithelial cells
\
\
89
New cards
What defines a sarcoma ?
Tumour of smooth tissue
90
New cards
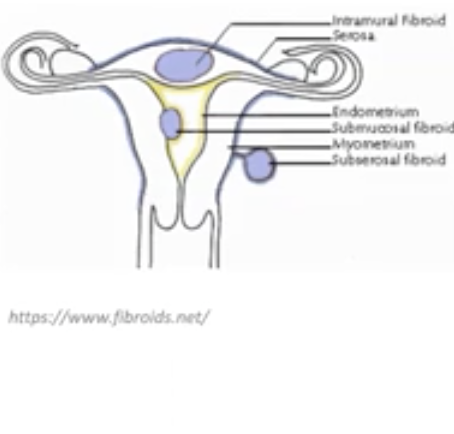
What are the three layers of the uterus? (in to out)
Endometrium / Mucosa : Glandular structures (one dot) and stroma (two)
Myometrium : S. muscle tissue (three)
Serosa : mesothelial lining on the outside of the uterus
Myometrium : S. muscle tissue (three)
Serosa : mesothelial lining on the outside of the uterus
91
New cards
Where does an endometrial polyp usually arise?
Enlargement of the mucosa which can lead to the malignant form called endometrial carcinoma
92
New cards
Where do mesenchymal tumours arise from and what are they called when they’re benign / malignant?
they arise in the myometrium, they are called leiomyomas (most common form of uterus tumours) and can become sarcomas (can originate from s.muscle and also stroma)
93
New cards
What is the histology of a leiomyoma? How do people know they have it?
* No histology because there is no atypia or mitosis or necrosis
* Infertility or pain (in the case of an ischemia)
* Infertility or pain (in the case of an ischemia)
94
New cards
What is the difference between endometriosis and adenomyosis ?
Endometriosis is presence of endometrium outside the uterus (ie ovaries, ligs, peritoneal pelvis, from c section scar..etc)
Adenomyosis is presence of endometrium in the uterus (about 0.2 to 0.3 cm from pre-existent endometrium
Adenomyosis is presence of endometrium in the uterus (about 0.2 to 0.3 cm from pre-existent endometrium
95
New cards
What are the risk factors of an endometrial polyp ?
Obesity
Late menopause
Use of tamoxifen
Late menopause
Use of tamoxifen
96
New cards
What does atypical hyperplasia lead to ?
Endometrial intraepithelial neoplasia which can be caused by long term oestrogen stimulation
97
New cards
What is the most common malignant tumour in endometrial carcinoma ?
endometriosis adenocarcinoma - 80%
98
New cards
What are the risk factor of endometrial carcinoma ?
* Obesity
* Diabetes
* Hypertension
* Infertility
* Estrogen exposure
* Minority
* Germline mutations
* PTEN abnormality
* DNA mismatch repair genes (Lynch Syndrome)
* Diabetes
* Hypertension
* Infertility
* Estrogen exposure
* Minority
* Germline mutations
* PTEN abnormality
* DNA mismatch repair genes (Lynch Syndrome)
99
New cards
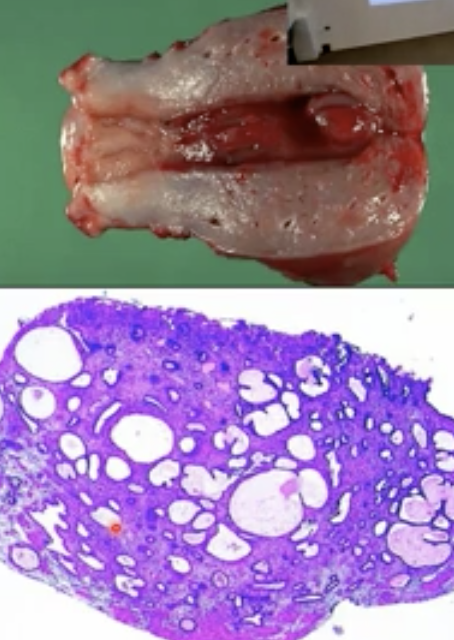
How are endometrial carcinomas graded?
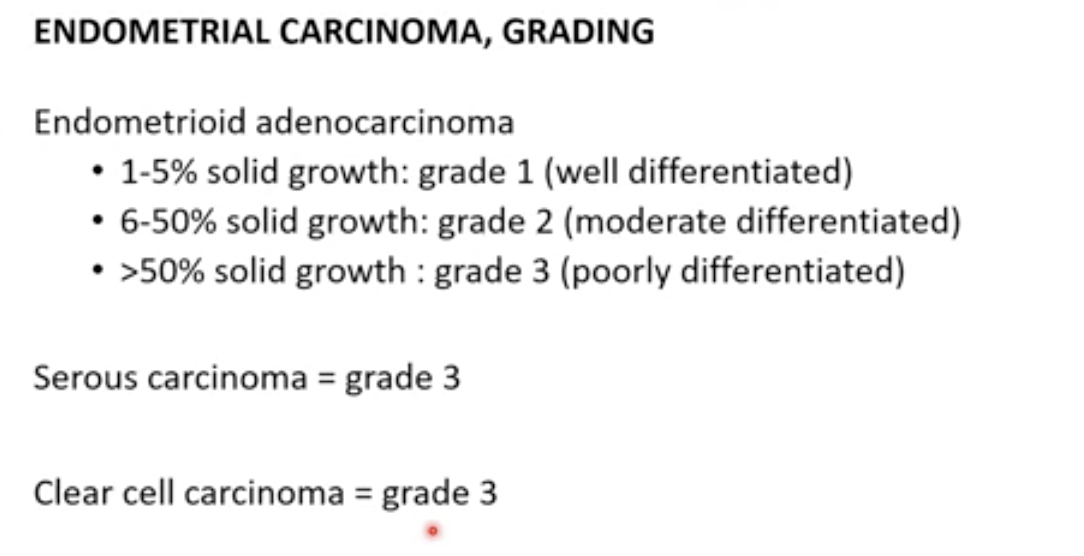
100
New cards
What are the main characteristics of endometroid carcinoma?
* Often grade 1
* Looks like endometrium
* Squamous or mutinous differentiation (important because its unique to this kind)
* Low mitotic activity
* Hyperplastic background
* Atypical hyperplasia / EIN
* Looks like endometrium
* Squamous or mutinous differentiation (important because its unique to this kind)
* Low mitotic activity
* Hyperplastic background
* Atypical hyperplasia / EIN