313 Cardio Flashcards
0.0(0)
Card Sorting
1/115
Earn XP
Description and Tags
Last updated 3:49 PM on 12/16/22
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
116 Terms
1
New cards
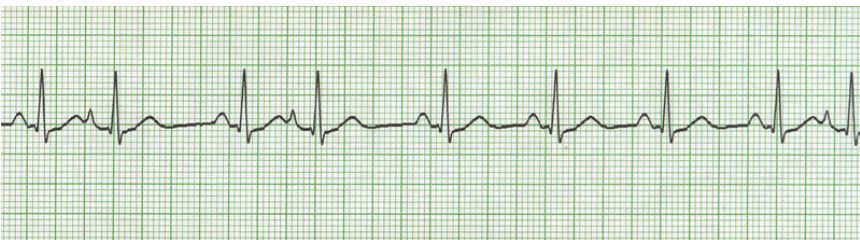
ECG Monitoring
Graphic tracing of electrical impulses produced by the heart. Waveforms of ECG represent activity of charged ions across membranes of myocardial cells
2
New cards
Telemetry monitoring
Continuous observation of HR and rhythm in real time, may be at a distant site from the patient such as a centralized monitoring system
3
New cards
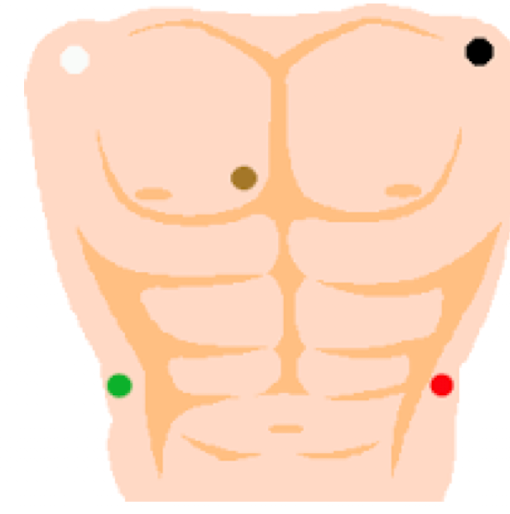
Lead placement of telemetry
Clouds over grass, smoke over fire, brown in the middle
4
New cards
Patient preparation for telemetry
Clip excessive hair on chest wall, rub skin with dry gauze, may need to use an alcohol wipe on oily skin. Apply electrodes
5
New cards
Artifact
results from leads unsticking, muscle or electrical activity like movement.
6
New cards
How many seconds is one strip on an ECG?
6 seconds
7
New cards
Assessment of cardiac rhythm
Must make accurate interpretation and immediately evaluate consequence of findings for individual patient. Assess the patient not the monitor, assess hemodynamic status
8
New cards
Steps in ECG interpretation
1: Rate
2: Rhythm
3: Are P waves present
4: Is the QRS complex present
5: Are intervals WNL
6: is there a P wave for every QRS
7: Is there a QRS for every P wave
2: Rhythm
3: Are P waves present
4: Is the QRS complex present
5: Are intervals WNL
6: is there a P wave for every QRS
7: Is there a QRS for every P wave
9
New cards
Calculating Heart Rate
The best way to calculate HR is to count the number of QRS complexes in 1 minute
10
New cards
Normal Sinus Rhythm
Sinus node 60-100 BPM, follows normal conduction pattern
11
New cards
Dysthymias
Abnormal cardiac rhythms. Due to disorders of impulse formation or disorders of conduction impulses
12
New cards
Which node is the normal pacemaker of the heart
SA node
13
New cards
Common assessment findings with dysrhythmias
Abnormal rate, irregular rhythm, changes in BP, decreased O2, chest, neck, shoulder, back, jaw pain, dizziness, syncope, anxiety, decreased LOC, feeling of doom, numbness, cold clammy skin, diminished pulses, pallor, palpitations, weakness, N/V
14
New cards
Emergent interventions in dysrhythmias
Ensure ABCs, admin O2, obtain baseline VS and O2 sat, obtain 12 lead EKG, hook up telemetry, identify underlying rate and rhythm, establish IV line
15
New cards
Sinus bradycardia
regular rhythm, rate < 60bpm
16
New cards
Cases of sinus bradycardia
normal rhythm in aerobically trained athletes during sleep, occurs in response to valsalva maneuver, vagal stimulation, hypothermia, admin of certain drugs
17
New cards
S+S of sinus bradycardia
hypotension, pale, cool skin, weakness, angina, dizziness, syncope, confusion, SOB
18
New cards
Treatment of sinus bradycardia
atropine 0.5 mg push, pacemaker may be required
19
New cards
Pacemaker
used to pace the heart when the normal conduction pathway is damaged or diseased, consists of power source, one or more conducting leads, myocardium
20
New cards
Temporary pacemaker
pacemaker used temporarily with a power source outside the body
21
New cards
Transvenous pacemaker
leads threaded transvenously to right atrium and/or right ventricle and attached to external power source. Used as a bridge until permeant pacemaker can be inserted or the bradycardia is resolved
22
New cards
Transcutaneous pacemaker
noninvasive temporary procedure, used until transvenous pacemaker is inserted or definitive therapy is available, power source and rate/voltage control device attaches to 2 electrode pads
23
New cards
Placement of transcutaneous pacemaker
attach one pad to the anterior chest and the other pad on the back between the spine and the left scapula at the level of the heard
24
New cards
pt care of a temporary pacemaker
always use lowest current capable of causing a ventricular contraction to minimize pt discomfort. Tell patient what to expect, reassure patient that it is only temporary, whenever possible provide analgesia and sedation
25
New cards
Permanent pacemaker
pacemaker implanted totally within the body. Power source placed subcutaneously, usually over the pectoral muscle on patients non dominant side. Pacer leads are thread transvenously to the right atrium and attached to power source
26
New cards
failure to capture
electrical charge to myocardium is insufficient to produce atrial or ventricular contraction, can result in serious bradycardia or asystole
27
New cards
Failure to sense
failure to recognize spontaneous atrial or ventricular activity and pacemaker fires inappropriately. Fires during excitable period in cardiac cycle can result in VT
28
New cards
Complications of pacemakers
Infection, hematoma formation, pneumothorax, failure to sense or capture, perforation of atrial or ventricular septum, battery failure
29
New cards
Post insertion care of pacemakers
prophylactic antibiotics, post insertion CXR, close observation of insertion site for infection or bleeding, continuous telemetry, limit arm and shoulder movement
30
New cards
Patient education of pacemakers
regular pacer function checks, report signs of infection, avoid lifting arm on pacer side above shoulder, environmental control
31
New cards
Sinus tachycardia
regular rhythms, rate > 100 bpm
32
New cards
Clinical associations sinus tachycardia
Vagal inhibition or sympathetic stimulation, exercise, fever, pain, anxiety, hypovolemia, drugs, caffeine
33
New cards
S+S sinus tachycardia
Dizziness, Dyspnea, hypotension, increased myocardial O2 consumption, increased HR, angina,
34
New cards
Treatment sinus tachycardia
Determined by underlying cause, treat hypotension, fever, or pain. Vagal maneuvers and carotid massage, beta blockers, CCB
35
New cards
Atrial dysrhythmias
caused by pacemaker cells not firing from the SA node but from somewhere else in the atria
36
New cards
Premature atrial contraction
contraction originating from ectopic focus in the atria and not the SA node
37
New cards
Manifestation of PAC
non life threatening dysrhythmia can be seen in NSR, travals across atria by abnormal pathway and creates a distorted P wave,
38
New cards
Causes of PAC
in normal heart it can result from emotional stress or fatigue, caffeine, tobacco, alcohol
39
New cards
Clinical significance of PAC
isolated PAC are not significant in those with healthy hearts, may be warning of more serious dysrhythmia in those with heart disease
40
New cards
Treatment of PAC
monitor frequency and eliminate cause, Beta blockers
41
New cards
Atrial fibrillation
total disorganization of atrial electrical activity due to multiple ectopic foci, resulting in loss or atrial contraction
42
New cards
Manifestations of A fib
atrial rate 300-600bpm, irregular rate and rhythm, no P wave, narrow QRS
43
New cards
Rate of a fib with controlled ventricular response
normal (60-100)
44
New cards
rate of a fib with rapid ventricular response
over 100
45
New cards
rate of a fib with slow ventricular rate
under 60
46
New cards
Cause of A fib
often occurs with underlying cardiac disease
47
New cards
Complications of A fib
loss of CO, loss of atrial kick, thrombi formation as a result of blood stasis, may lead to stroke
48
New cards
Treatment of A fib
decrease the ventricular rate to within normal limits, anticoagulation to prevent thrombus, electric cardioversion
49
New cards
drugs for ventricular rate control
Digoxin, Beta blockers, calcium channel blockers
50
New cards
Drugs to improve cardioversion
amiodarone
51
New cards
Radiofrequency catheter ablation
electrode tipped ablation catheter burns areas of conduction system responsible for irregular rhythm. Definitive treatment for tachycardic dysrhythmias
52
New cards
Synchronized cardioversion
considered for a fib after adequate anticoagulation has been attained, synchronized circuit delivers a counter-shock on the R wave of the QRS complex on the ECG
53
New cards
treatment for complex a fib
anticoagulation therapy needed for a fib not responding to cardioversion
54
New cards
atrial flutter
dysrhythmia produced by pacemaker other than the SA node,
55
New cards
manifestations of atrial flutter
atrial rate 250-350 bpm, ventricular rate will vary, no P waves, flutter waves, QRS narrow
56
New cards
causes of atrial flutter
acute MI, severe mitral valve disease, thyrotoxicosis, COPD, patient who have had thoracic surgery, digoxin toxicity
57
New cards
Clinical significane atrial flutter
high ventricular rates and loss of the atrial kick can decrease CO, risk for stroke due to risk of thrombus formation from blood stasis
58
New cards
Treatment of atrial flutter
primary goal is to control the ventricular rate until SA node can take over. Medication therapy, antiarrhythmatic drugs
59
New cards
Medication therapy for A flutter
CCBs, beta blockers, digoxin
60
New cards
Superventricular tachycardia
any narrow QRS complex with a rhythm over 100 BPM, originates above bundle of his, usually PAC triggers a run of repeated premature beats,
61
New cards
manifestations of superventricular tachycardia
rate 150-200 bpm, rhythm is regular or slightly irregular, P wave often hidden in proceeding T wave, PR is shortened, QRS normal
62
New cards
Causes of superventricular tachycardia
overexertion, emotional stress, stimulants(caffeine, tobacco)
63
New cards
Clinical significance of superventricular tachycardia
prolonged episode and increased HR may precipitate decreased CO, palpitations, hypotension, dyspnea, angina
64
New cards
Treatment of superventricular tachycardia
vagal maneuvers, valsalva, cardioversion, drug therapy
65
New cards
medications for superventricular tachycardia
beta blockers, CCBs, amiodarone
66
New cards
Ventricular rhythms
rhythms that originate somewhere in the ventricles. No P wave, wide QRS complex
67
New cards
Premature ventricular contraction
contraction originating in ectopic focus of the ventricles, premature occurrence of wide distorted QRS complex. No P wave because it originates in the ventricle, compensatory pause
68
New cards
manifestations of PVC
rate varies, irregular rhythm, no P wave, distorted QRS
69
New cards
unifocal PVC
all PVCs look the same
70
New cards
multifocal PVC
multiple PVCs that look different
71
New cards
Couplet PVC
PVCs occur in twos
72
New cards
Triplet PVC
PVCs occur in threes
73
New cards
Ventricular bigeminy
PVC occurs every other beat
74
New cards
Ventricular trigeminy
PVC occurs every third beat
75
New cards
Causes of PVC
stimulants(caffeine, alcohol, nicotine, epinephrine,) fever, exercise, recreational drug use
76
New cards
Clinical significance of PVC
is normal heart, usually benign, pulse deficit may exist
77
New cards
Treatment of PVC
based on cause of PVC, O2 therapy, electrolyte replacement, assess hemodynamic status, drug therapy
78
New cards
Medications for PVC
beta blockers, procainamide, amiodarone, lodocaine
79
New cards
Ventricular tachycardia
run of three or more PVCs, considered life threatening because of decreased CO and the possibility of deterioration to V fib, will cause death if prolonged or untreated
80
New cards
Manifestations of V tach
rate > 150 BPM, regular or irregular rhythm, P wave independent of QRS complex, QRS is distorted
81
New cards
Causes of V tach
hypokalemia, hyperkalemia, MI
82
New cards
Treatment of VT with a pulse
Maintain BP and pulse with or without symptoms, amiodarone, replace electrolytes, cardioversion (usually for symptomatic pts)
83
New cards
Treatment pulseless VT
patient is in cardiac arrest, preform CPR and defibrillation
84
New cards
Defibrillation
most effective method of terminating VF and pulseless VT, passage of DC electrical shock through the heat to depolarize the cells of the myocardium to allow the SA node to resume the role of pacemaker
85
New cards
Clinical significance V tach
treatment for VT must be rapid, may recur is prophylactic treatment is not initiated, V fib may develop
86
New cards
Ventricular fibrillation
Lethal dysrhythmia requiring immediate treatment, most frequent seen rhythm in cardiac arrest occurring outside the hospital, Ventricle has multiple chaotic impulses rapidly firing
87
New cards
manifestation V fib
no effective CO or contraction occurs, no measurable rate, irregular rhythm, no identifiable P waves or QRS complexes, ECG is shaky
88
New cards
Causes of V fib
MI, coronary reperfusion, hypokalemia, hyperkalemia, electric shock
89
New cards
clinical significance
unresponsive, pulseless, apneic state, death will result quickly
90
New cards
treatment for V fib
immediate initiation of CPR and advanced cardiac life support measure with use of defibrillation and drug therapy
91
New cards
Medications for V fib
Vasopressor-epinephrine, amiodarone
92
New cards
Idioventricular rhythm
SA node and AV node fail to function and the rhythm is generated in the ventricle
93
New cards
Agonal rhythm
dying heart, rate under 20 bpm
94
New cards
accelerated idioventricular rhythm
rate between 40-100 bpm,
95
New cards
Causes of idioventricular rhythm
MI, cardiac arrest, mediactions, electrolyte imbalances, myocarditis, congenital heart disease
96
New cards
Treatment of IVR
is patient is symptomatic, correct the cause, pacing, atropine
97
New cards
Asystole
no measurable electrical activity originating from the heart, straight or flat line is seen on cardiac monitor. Should be assessed with second monitor lead
98
New cards
Treatment asystole
compressions should be started immediately, epinephrine, treat cause defibrillation not indicated
99
New cards
Premature Atrial Contraction
100
New cards

Sinus Bradycardia