L20: Fractures Trauma II
1/88
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
89 Terms
How much body mass does the MSK system make up
70% of body mass
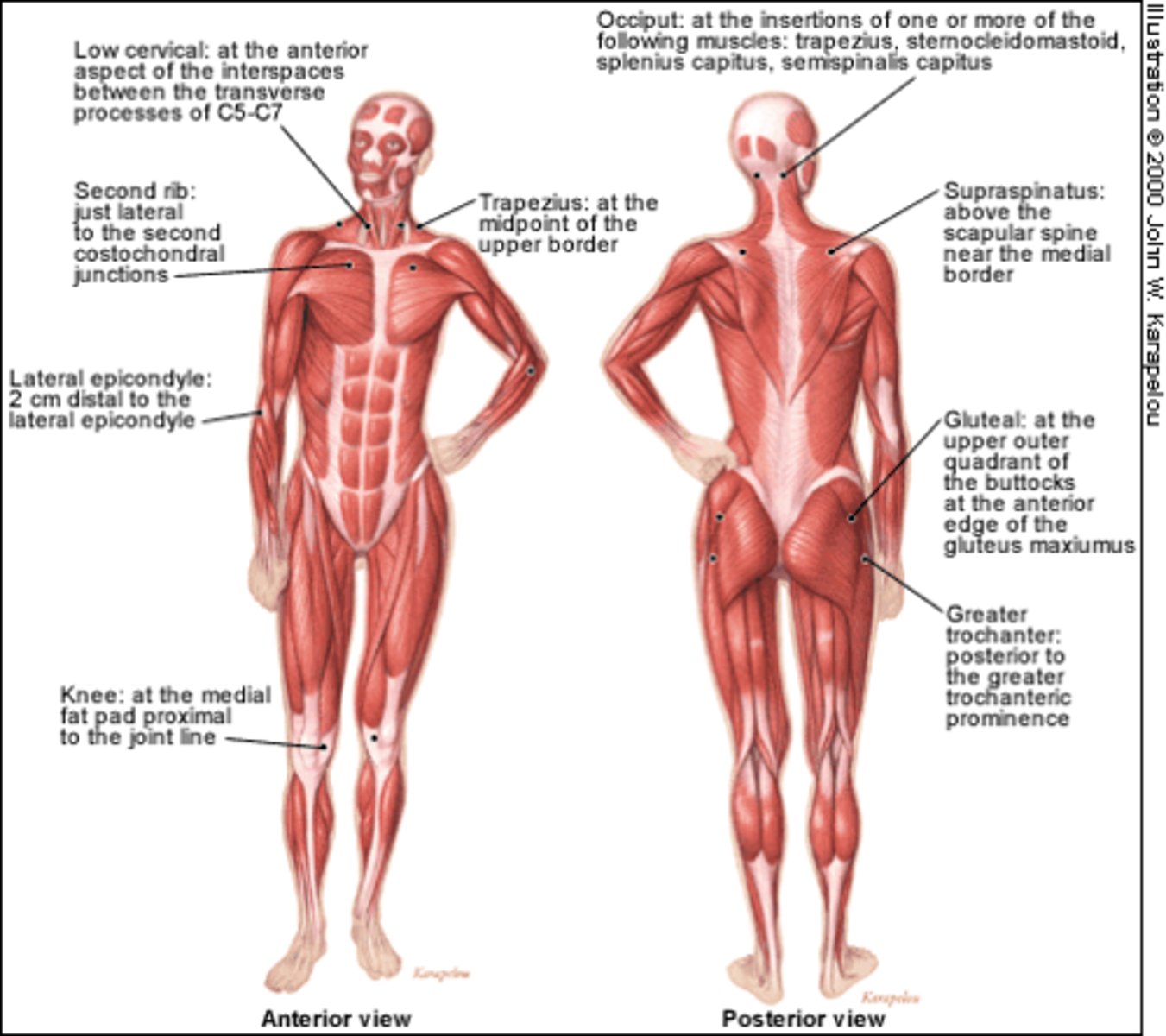
What does the MSK system include
- bones
- cartilage (at articulating surface)
- soft tissue in: MUSCLE, articulations (joints => weakest link), ligaments (bone-bone connection; attach articulating ends together), tendons (muscle-bone connection; join muscle to bone periosteum)
What are considered 'acute' MSK injuries
acute (sudden force) => includes:
- fractures
- contusions (soft tissue)
- articulation injuries: strains, sprains, dislocations
*note: in peds, a strain or sprain force can cause a fracture

What are considered 'chronic' MSK injuries
chronic (caused by overuse) => includes:
- stress fractures (no time to heal from acute injury)
- strains & sprains with no time to heal adequately

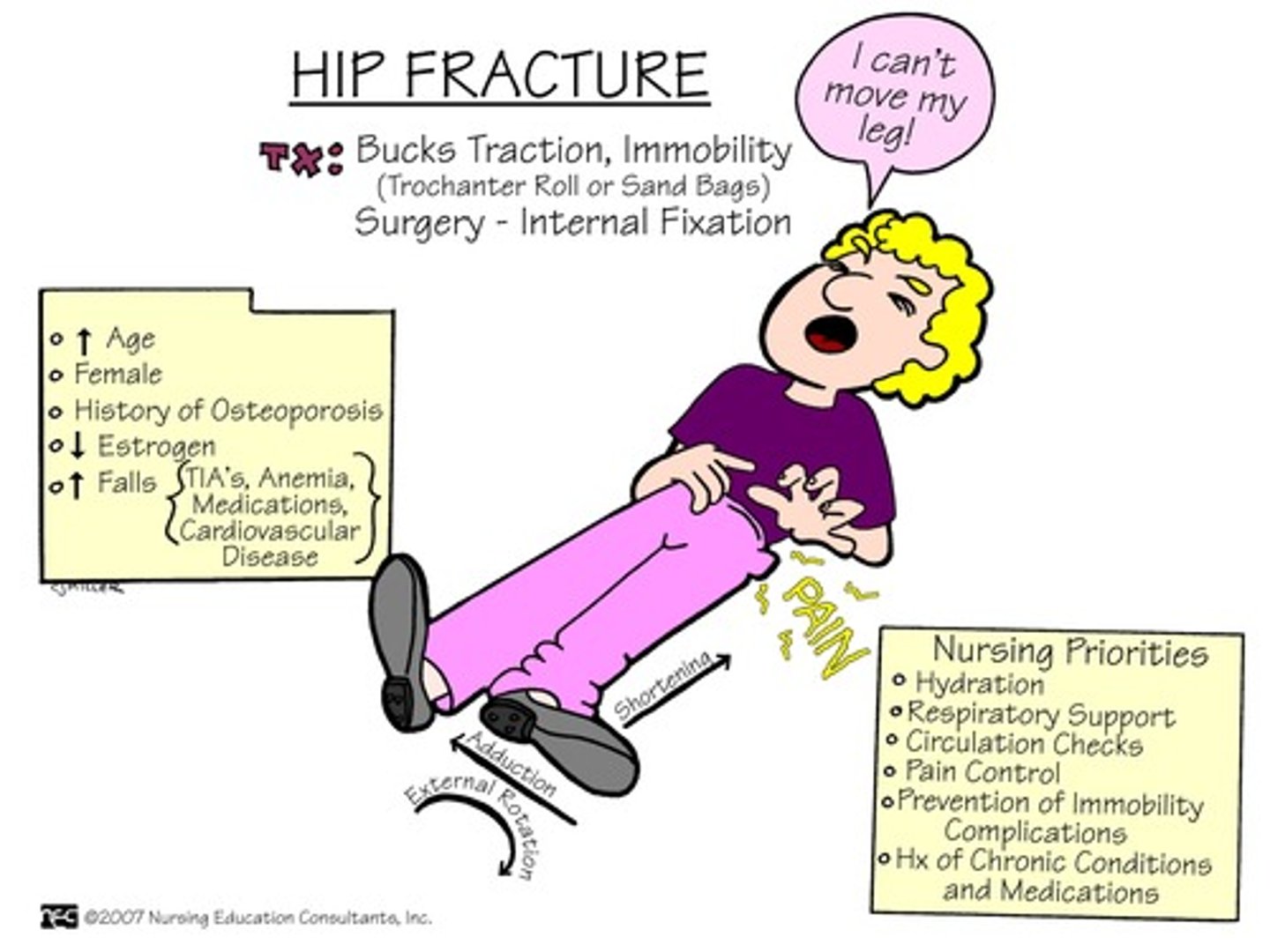
What are fractures overall in different age groups (peds, adults, elderly)
- most are unintentional
- peds: athletic (hockey, soccer) , falls, bicycle, motor-vehicle (eg. clavicle, femur)
- adults: motor-vehicle, motorcycle; athletic (eg. clavicle, femur, radius, head)
- elderly: falls (eg. hip fractures, spinal disk)
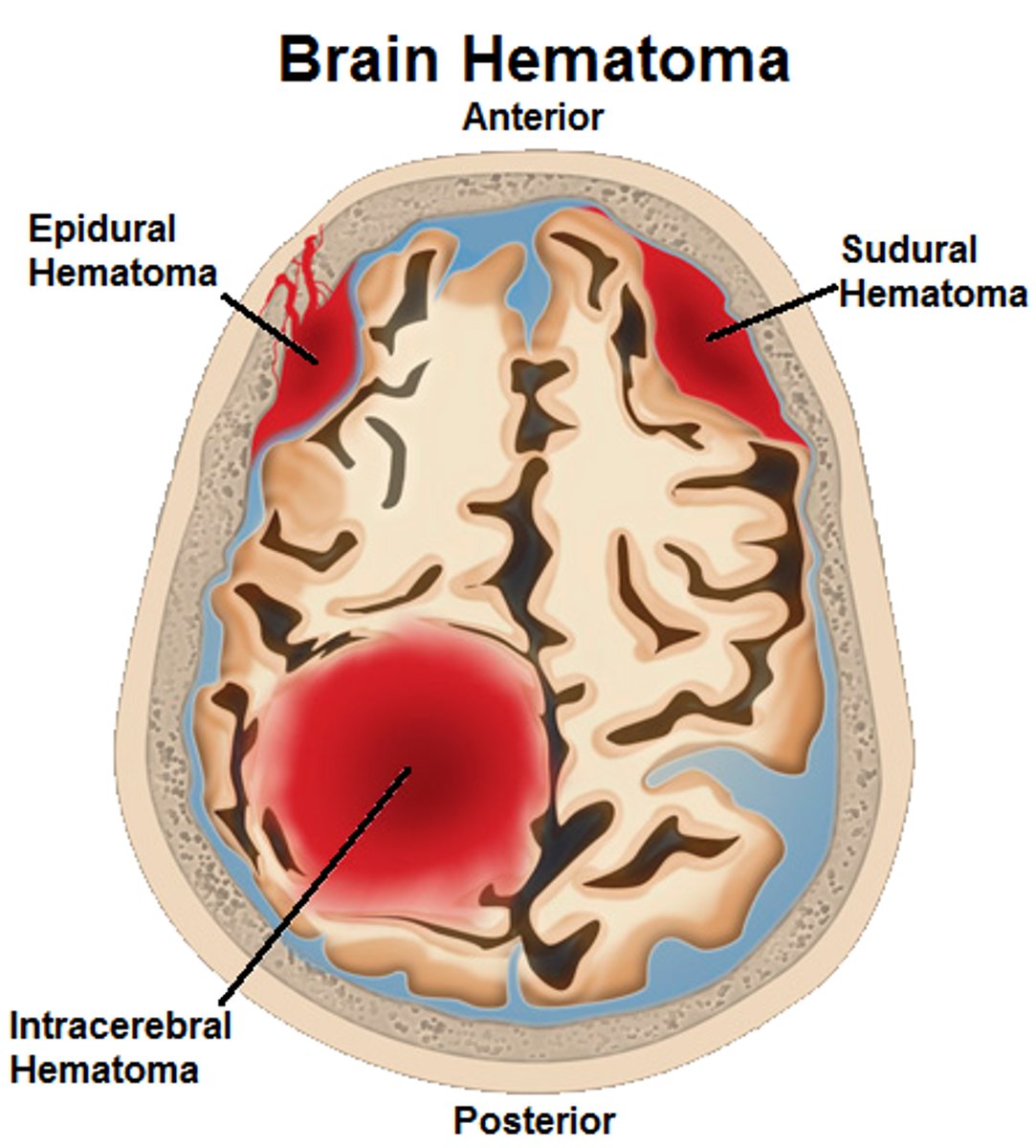
note* always assess for brain injury!

What are the s&s of a fracture
- severe pain => initial numbness maybe present aka 'local shock'
- inflammation
- hematoma (tissue hemorrhage)
- deformity or loss of function
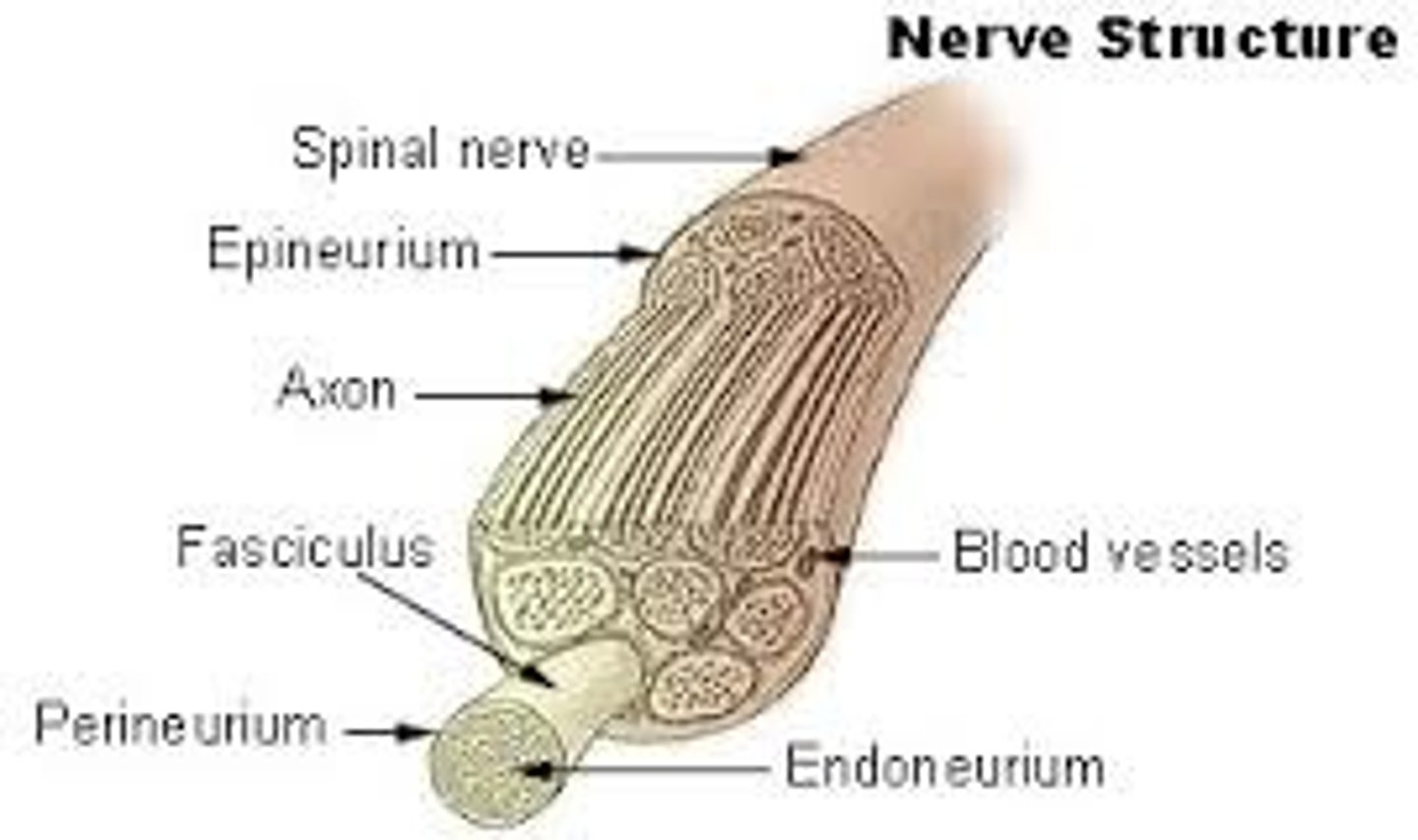
- injury to surrounding tissues/blood vessels/nerves
What is 'local shock' seen in fractures
- massive vasoconstriction to decrease blood flow (and decrease hemorrhage risk) => decreases nerve perfusion => decrease sensation (note: sensation could come back at any moment = severe pain)
How do we get best imaging of a fracture
Xray assessment

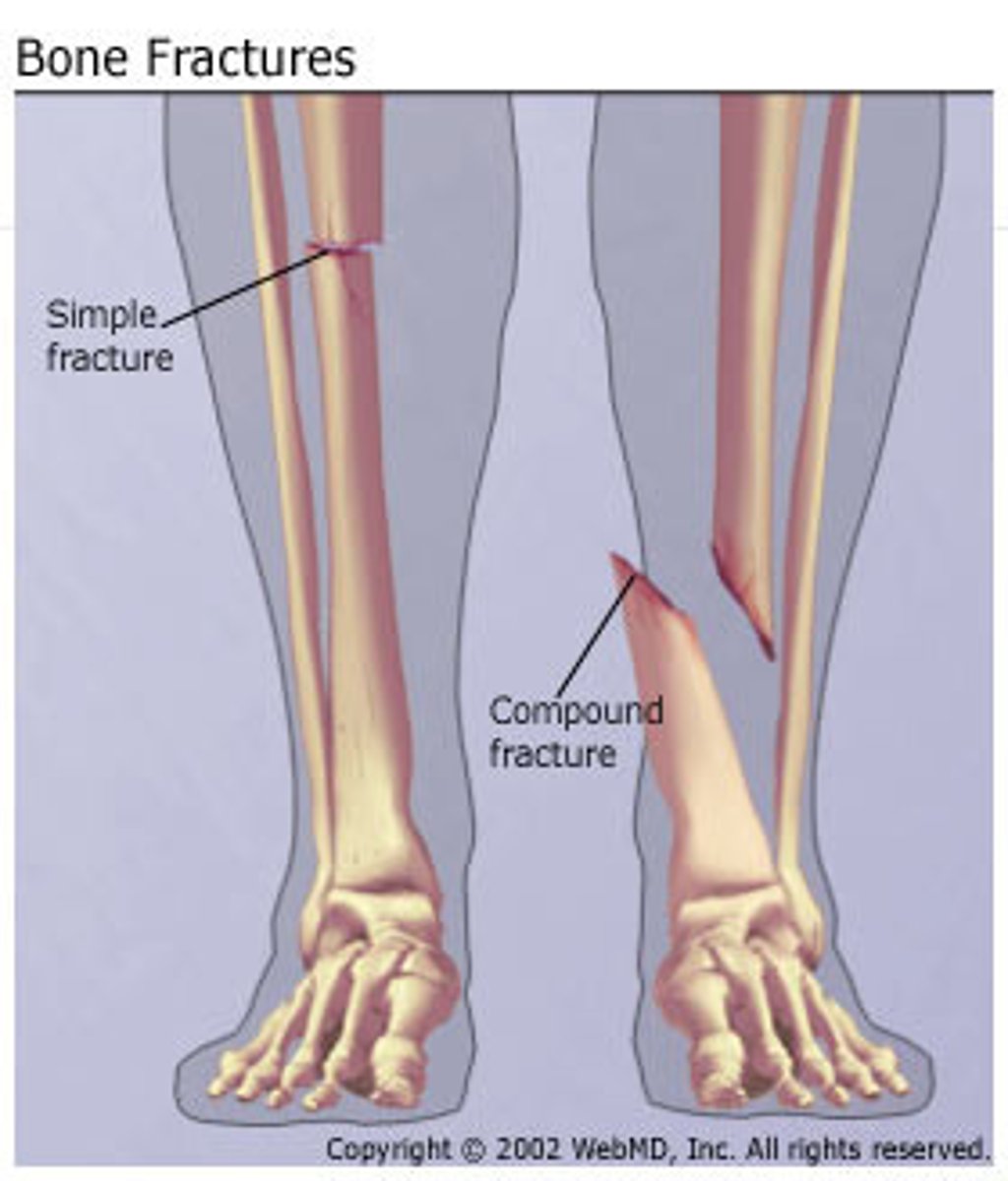
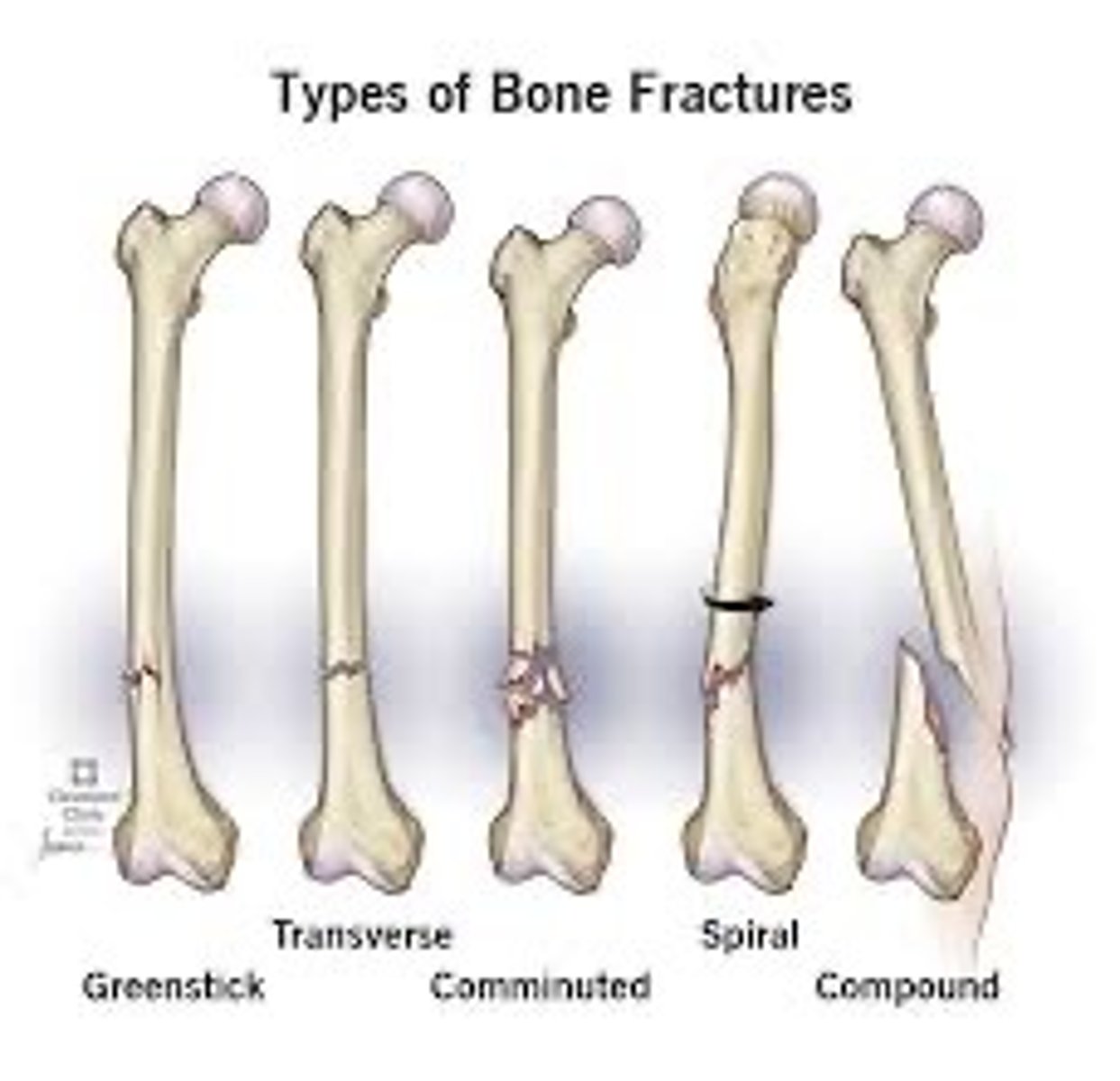
What is an open/compound fracture
- skin break
- fracture is piercing skin, exposing bone
What is a compression fracture
2 bones crushed together, collapse of vertebra

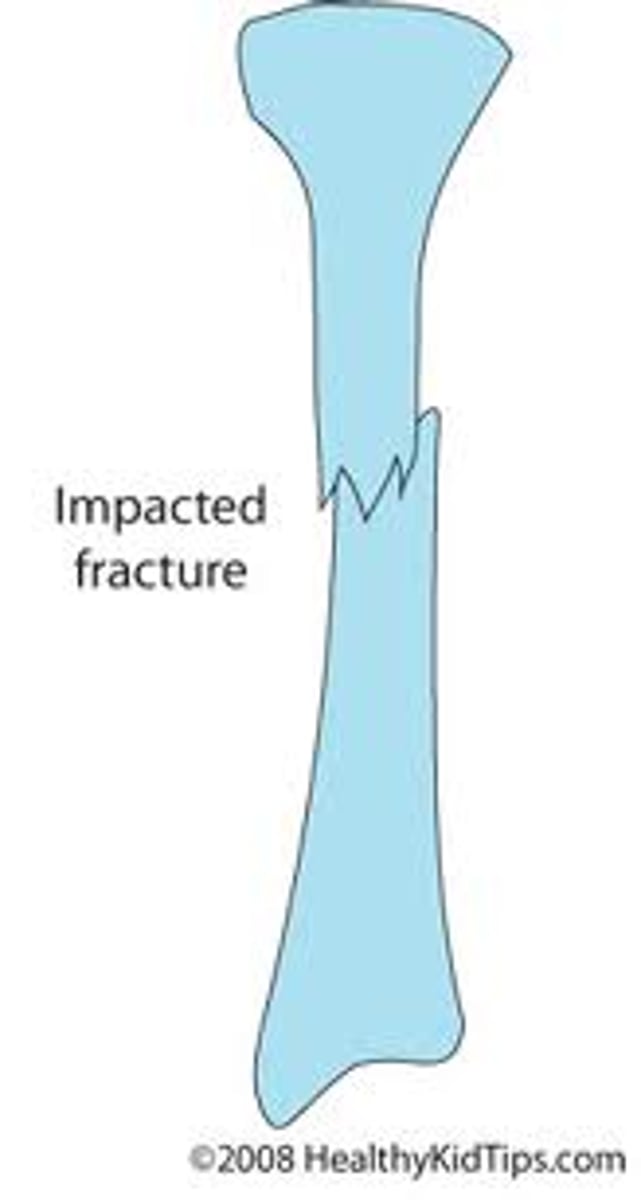
What is an impacted fracture
fracture fragments crushed together (broken bones are driven into each other)
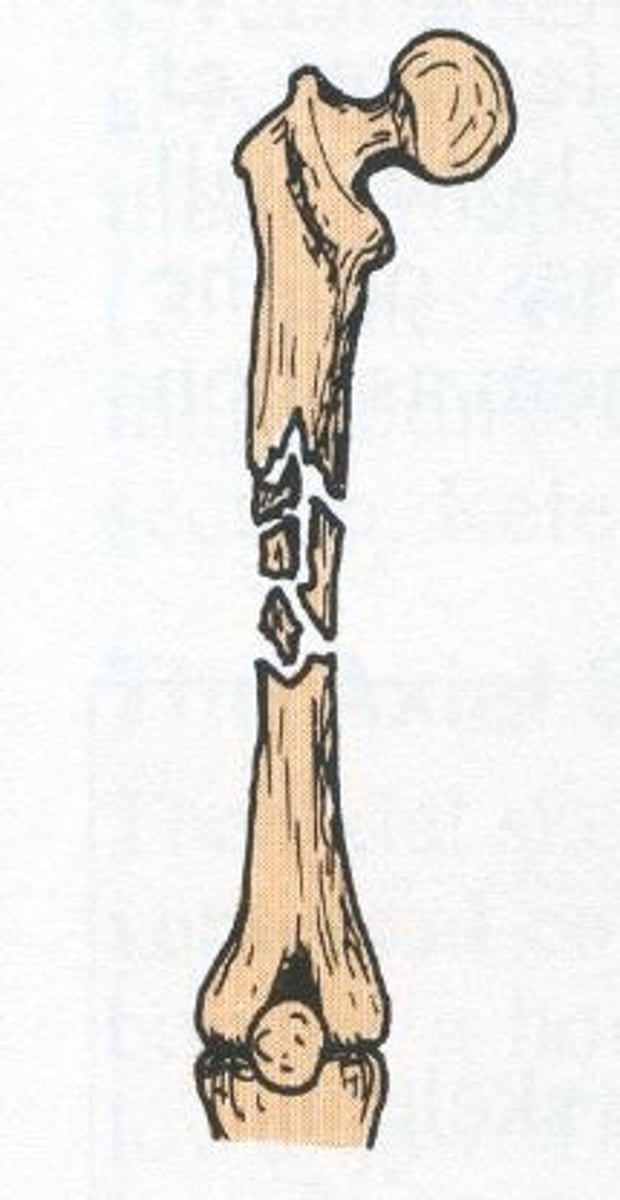
What are the types of unstable fractures
- oblique
- spiral
- comminuted (fragmented/cracked & compressed bone)
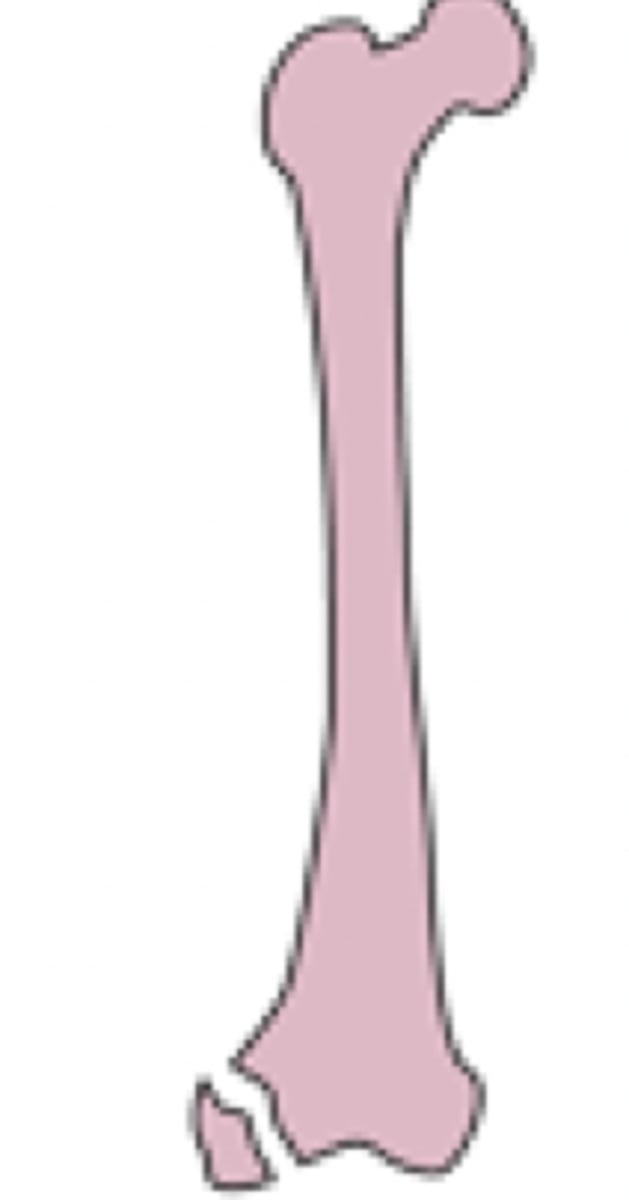
What is an avulsed fracture
- fragment of bone is separated from the rest
- smaller SA, fragment needs to be rehealed to original bone structure
- longer healing time
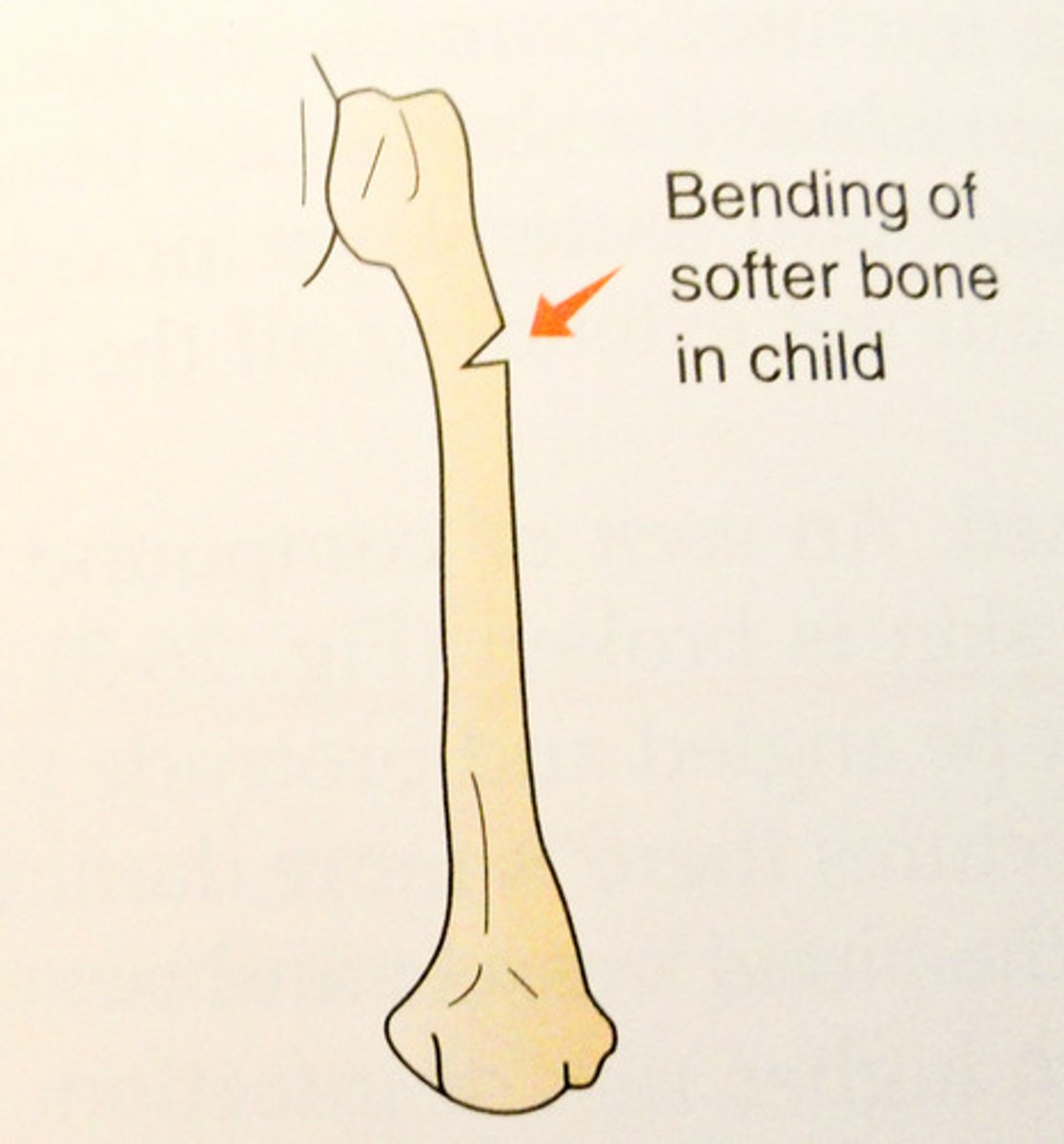
What is a greenstick fracture
- bone breaks partially
- heals very well
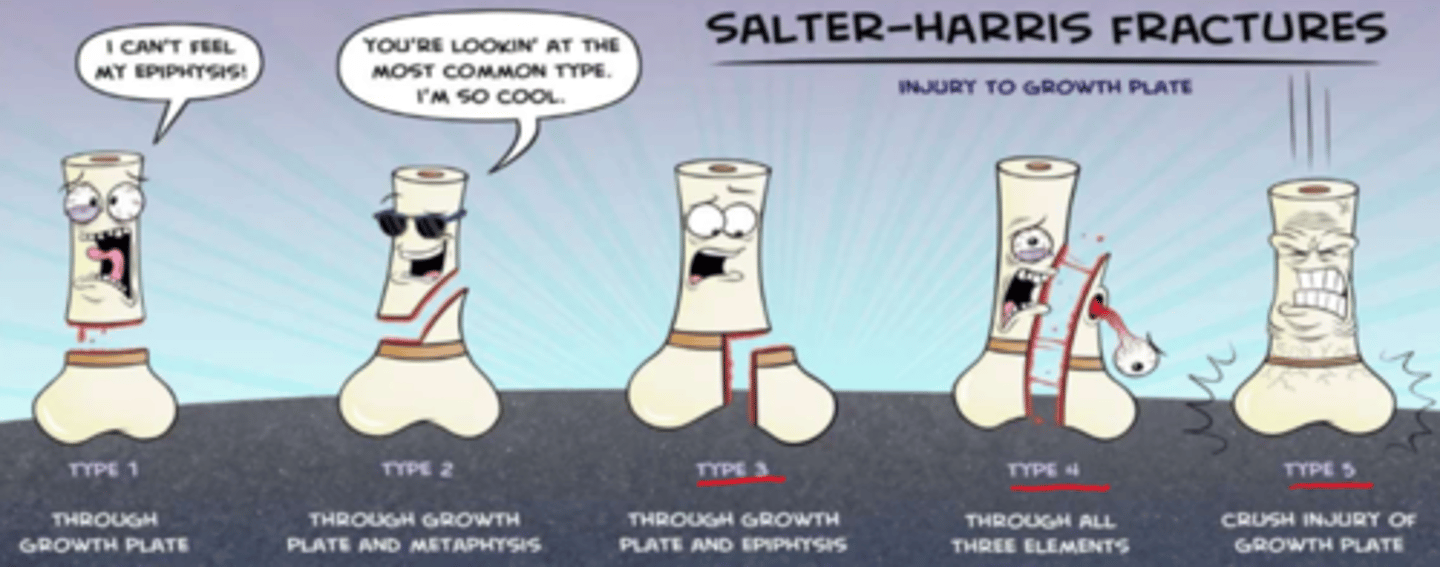
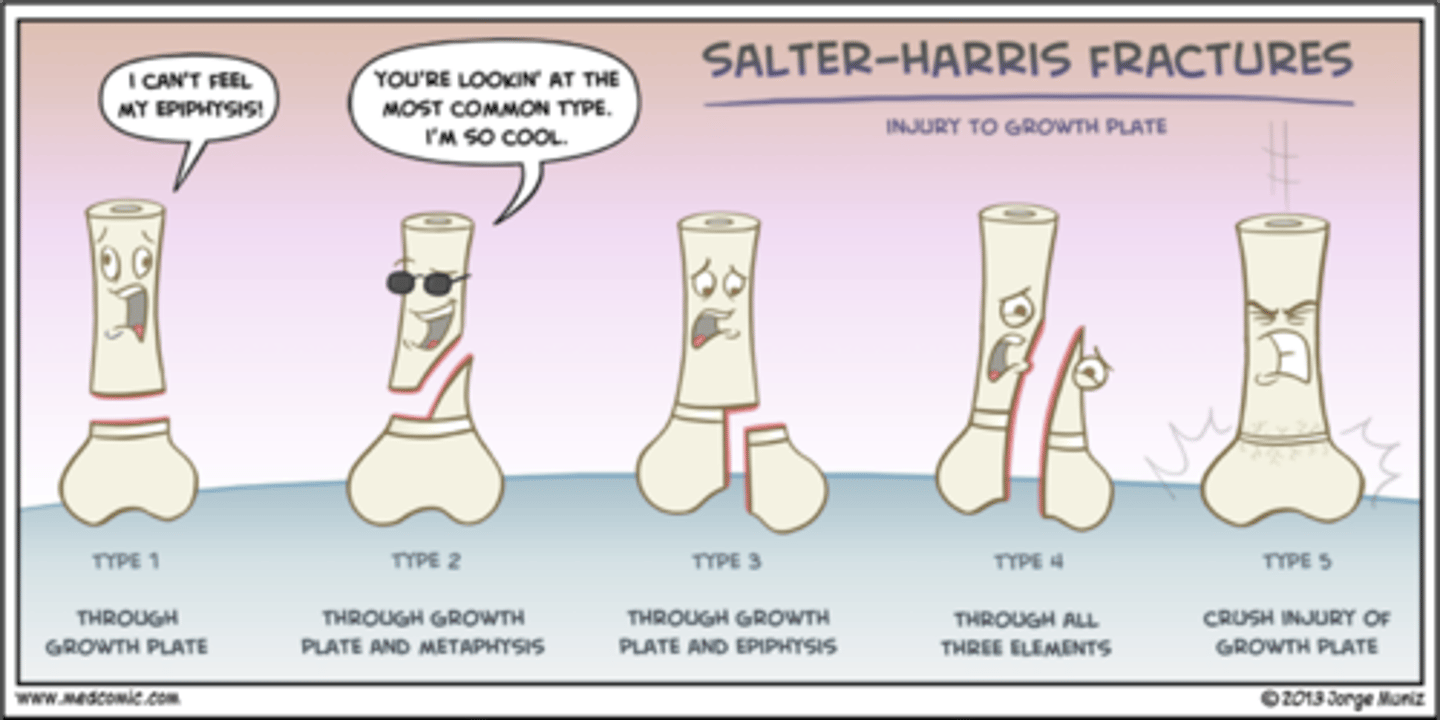
What is an epiphyseal fracture
- injury to growth plate (types 3-5; type 1-2 not likely to affect bc above growth plate)
- risk of growth compromise in peds
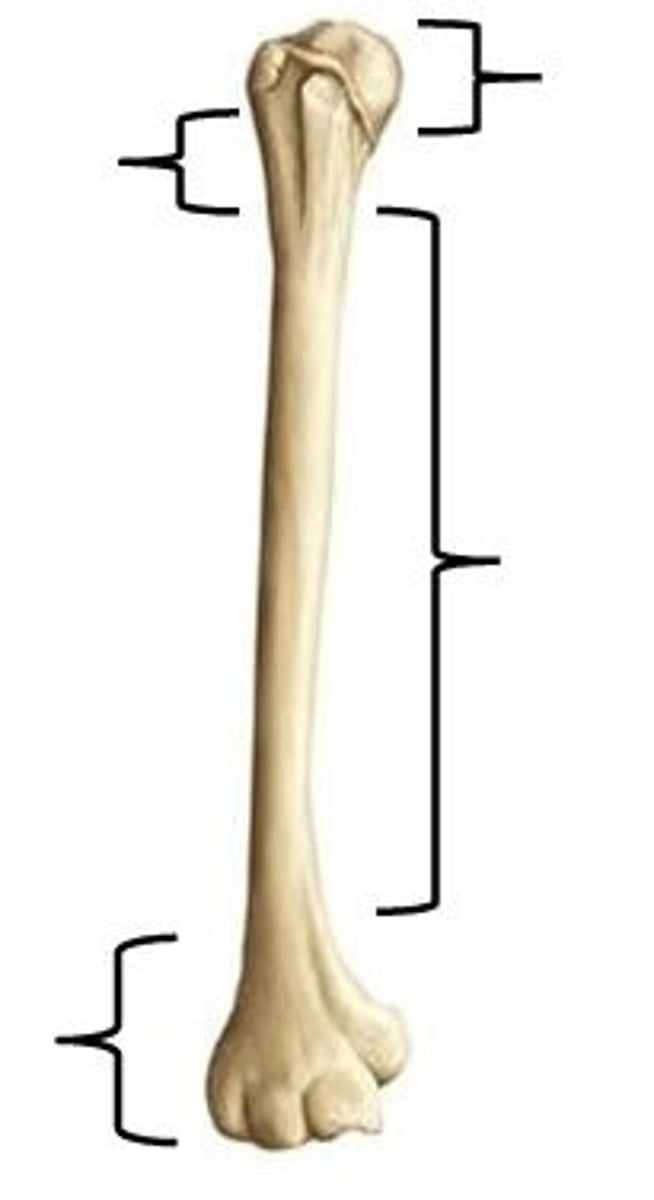
What are the anatomical parts of a long bone
- epiphysis: head/top of the bone
- diaphysis: shaft/neck of the bone - middle
- epiphysis: end/bottom of the bone
What are the 5 types of epiphyseal fractures in peds (salter harris classification)
Type 1: through the growth plateType 2: through growth plate & metaphysis (most common)
Type 3: through growth plate and epiphysis
Type 4: through all long bone elements
Type 5: crush/comminuted injury of growth plate
What are our overall tx goals in fractures
- pain management (may even give during local shock)
- inflammation management
- reduction of the fracture (if applicable)
- immobilization
- complications management
- restoration of function

What meds would we give during fracture tx
- analgesics (opioids, Tylenol or synergy)
- NSAIDs
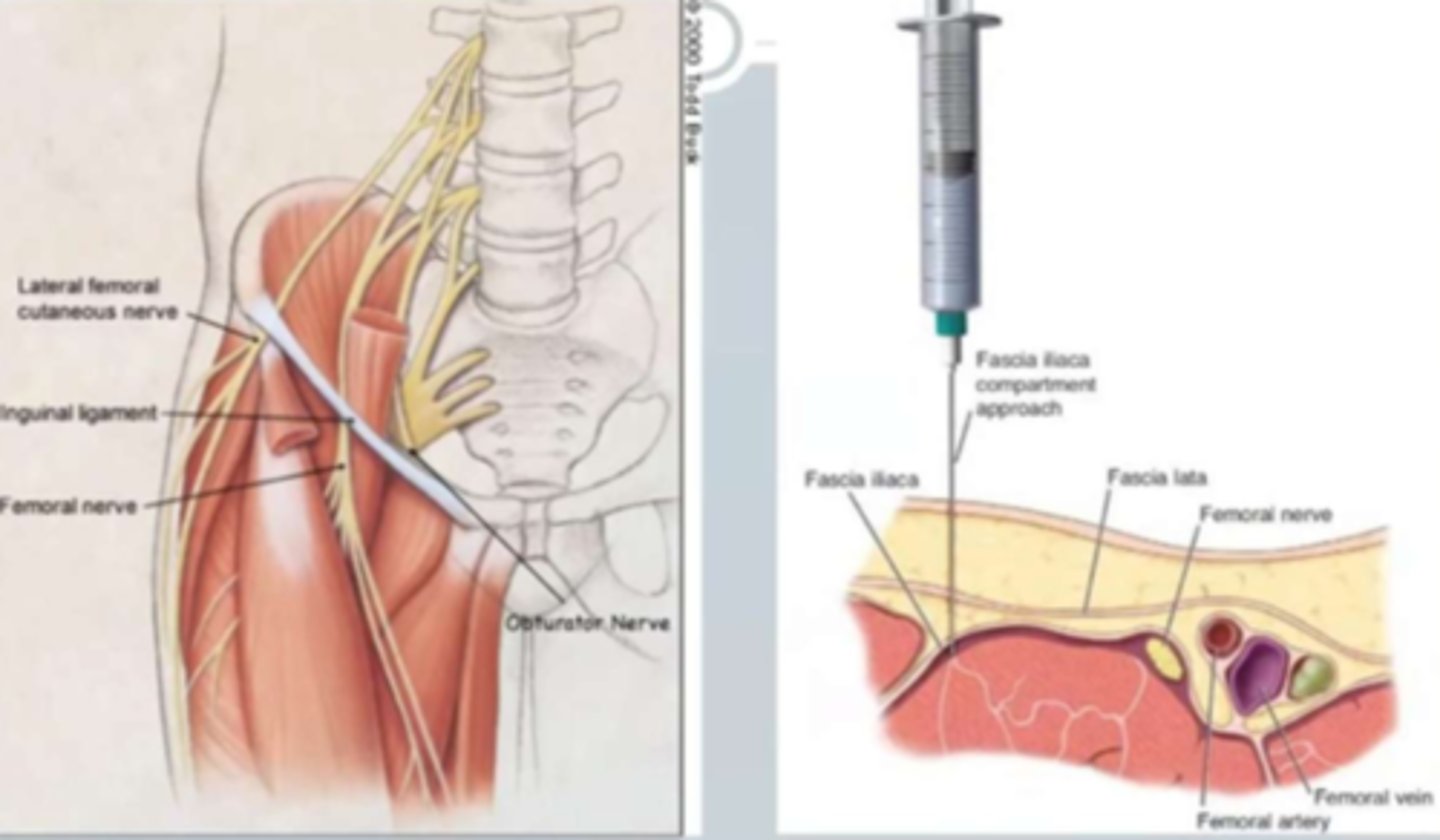
- anesthesia: local (nerve block under ultrasound guidance => eg. hip fractures, or spinal) or general
(note: nerve block for elderly hip fracture good bc they're at risk for opioid toxicity)
What is 'reduction' of a fracture
- reduction - restoration of alignment
- goal is to straighten the fracture
- 2 types: external traction OR surgical reduction
What is external traction of a fracture (reduction)
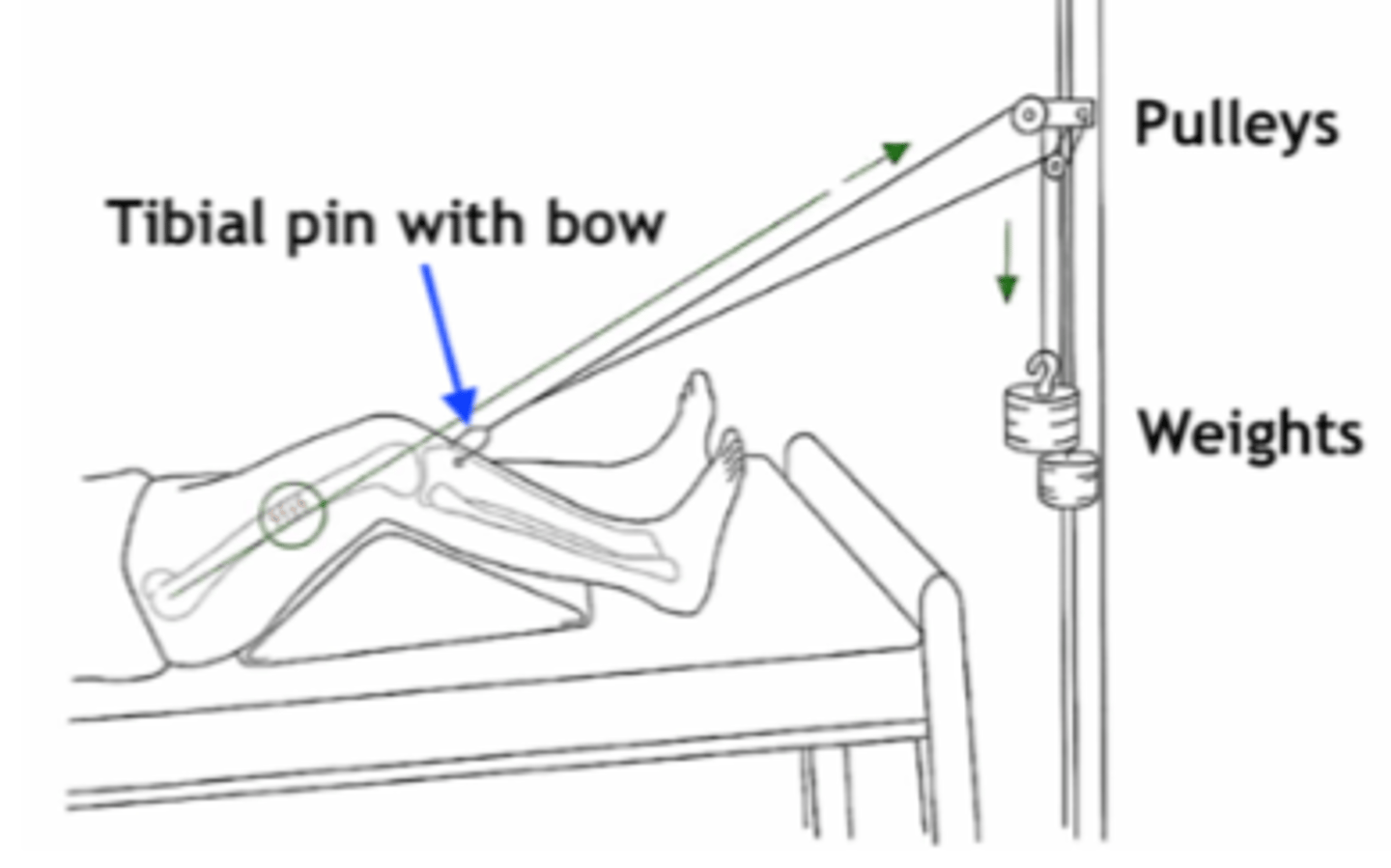
- reduces fracture into place. can be through:
- manual pulling
- skeletal traction (via pins/wires/pulleys to pull the bone & straighten it)

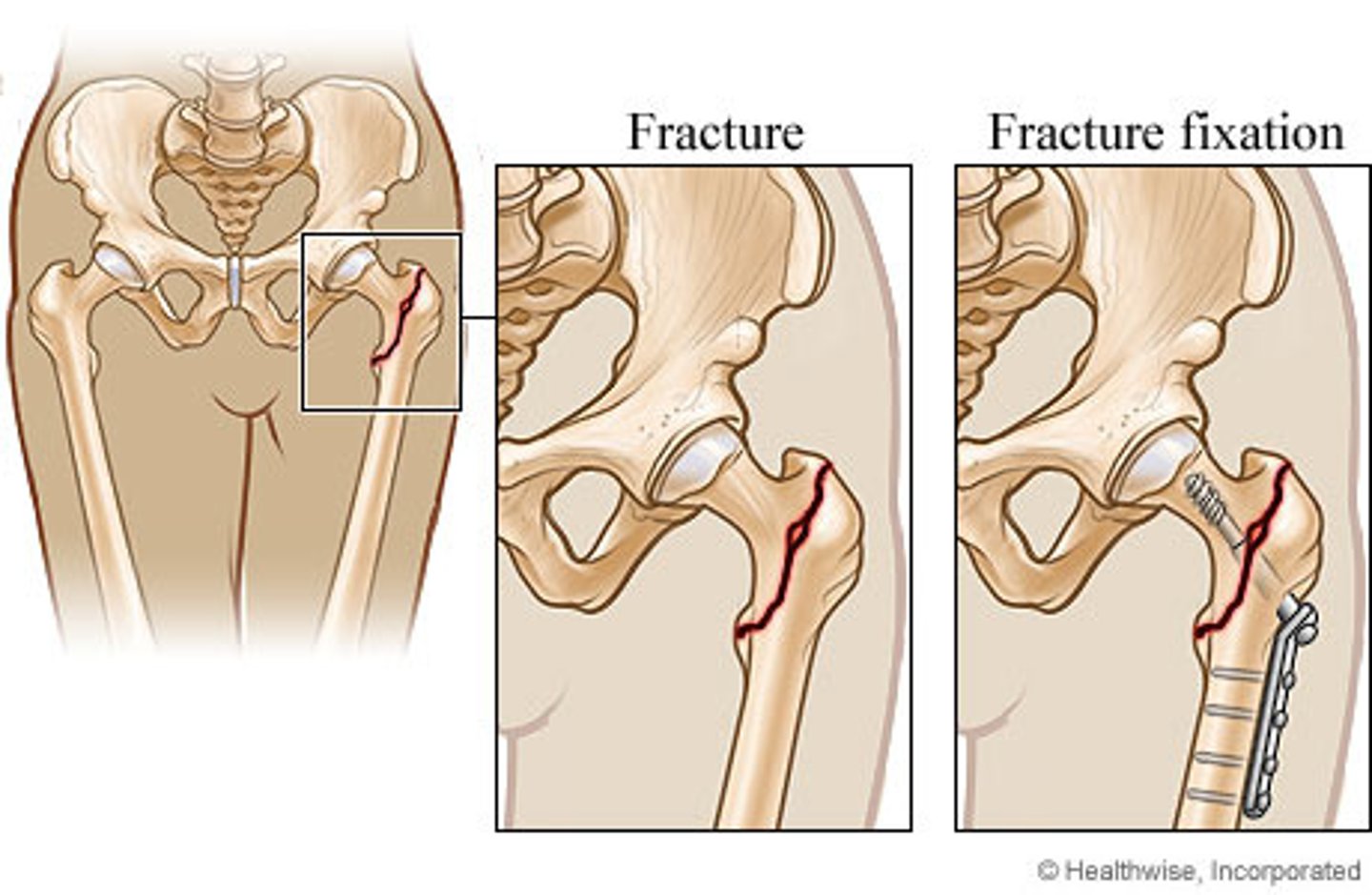
What is 'fixation' of a fracture
- fixation - maintenance of alignment (after reduction)
- reduce level of traction & keep it in place to allow for healing
- can either be permanent or temporary depends on effects on pt

What are the different forms of fixation (in fractures)
- external traction (skeletal) (same as skeletal reduction just reduced amount)
- external fixation (implants placed outside of the skin)
- internal fixation (implants placed under the skin)
What is the goal of 'immobilization' in fractures
- maintains alignment until the fracture is healed
- same methods as reduction & fixation however prolonged time (fixation & traction)
- other methods used here: splint, cast, boot, brace

How do we initiate restoration of fx in fracture tx
- rehab exercises
- physiotherapy
- occupational therapy
- note: early mobility prevents clot formation

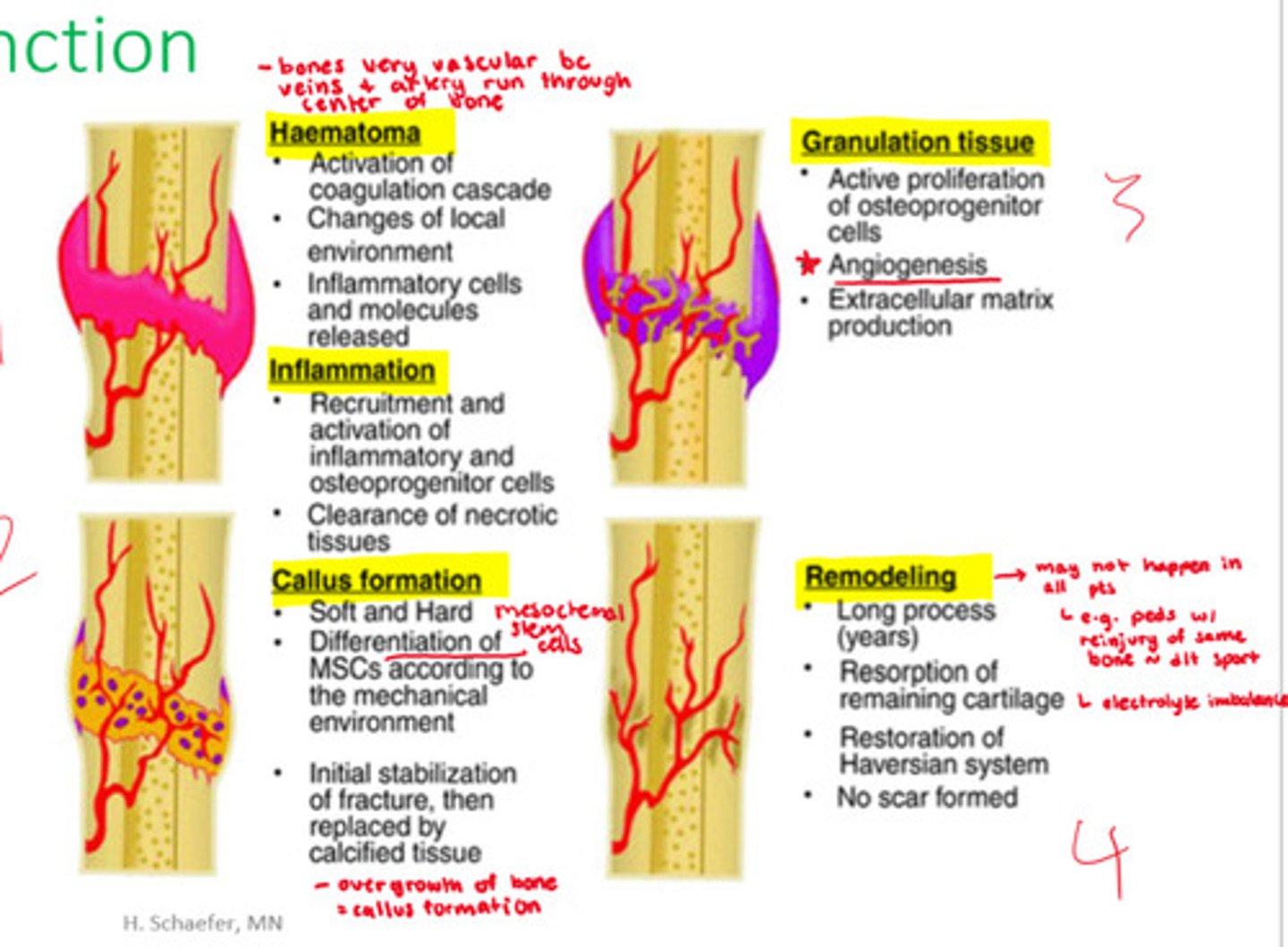
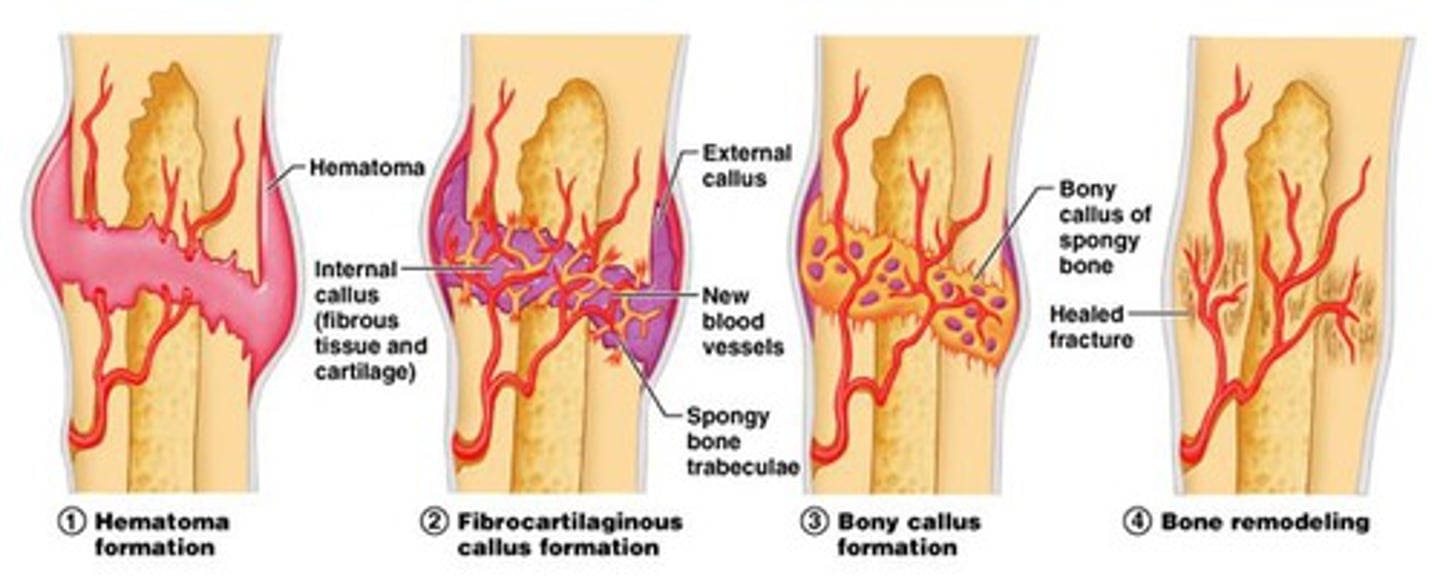
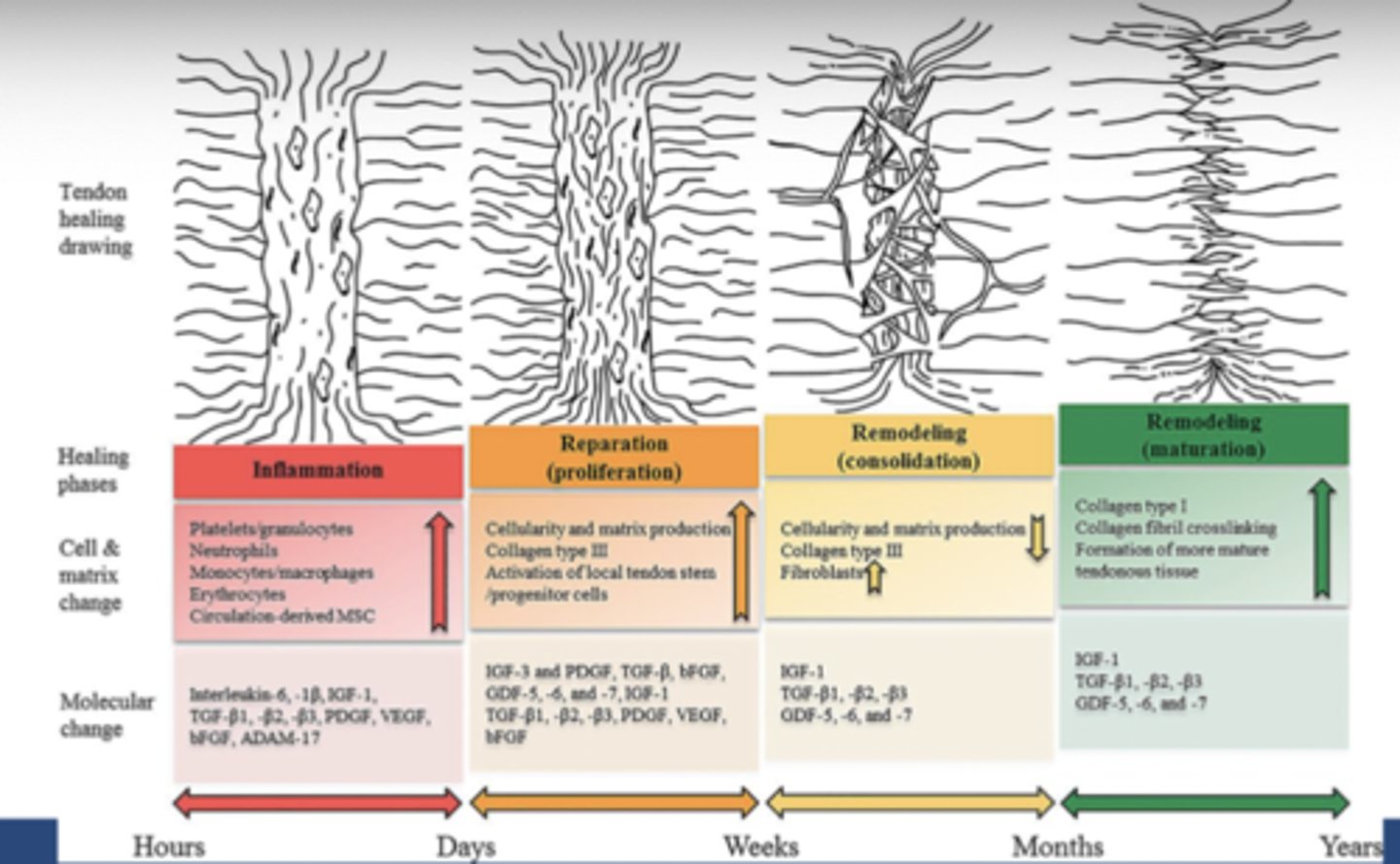
stages of restoring function in fractures
- hematoma, inflammation, callus formation, granulation tissue, remodeling
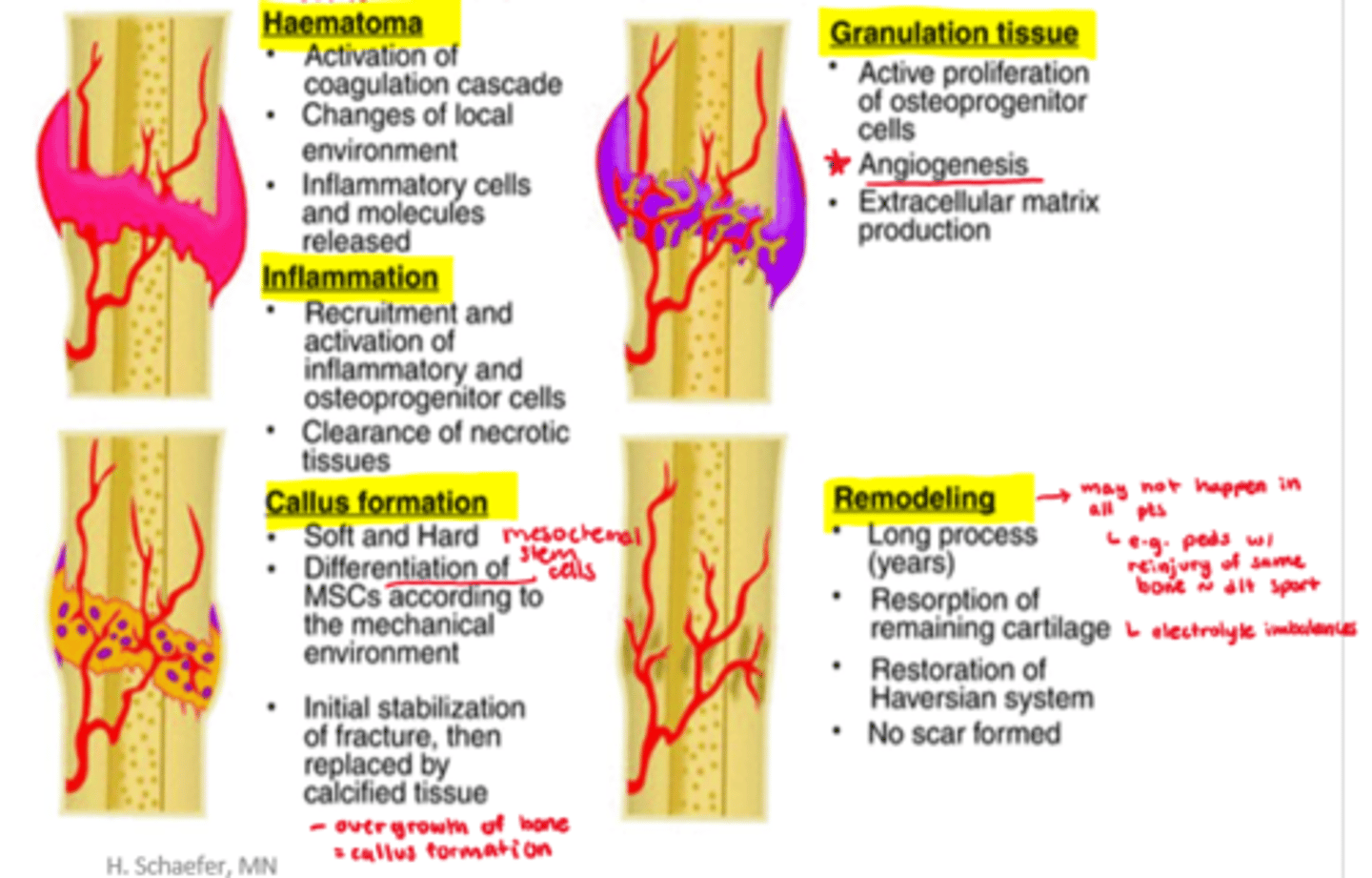
What happens in the hematoma stage of healing fractures
- activation of coagulation cascade
- changes of local environment
- inflammatory cells and molecules released
- (note: bones are very vascular)
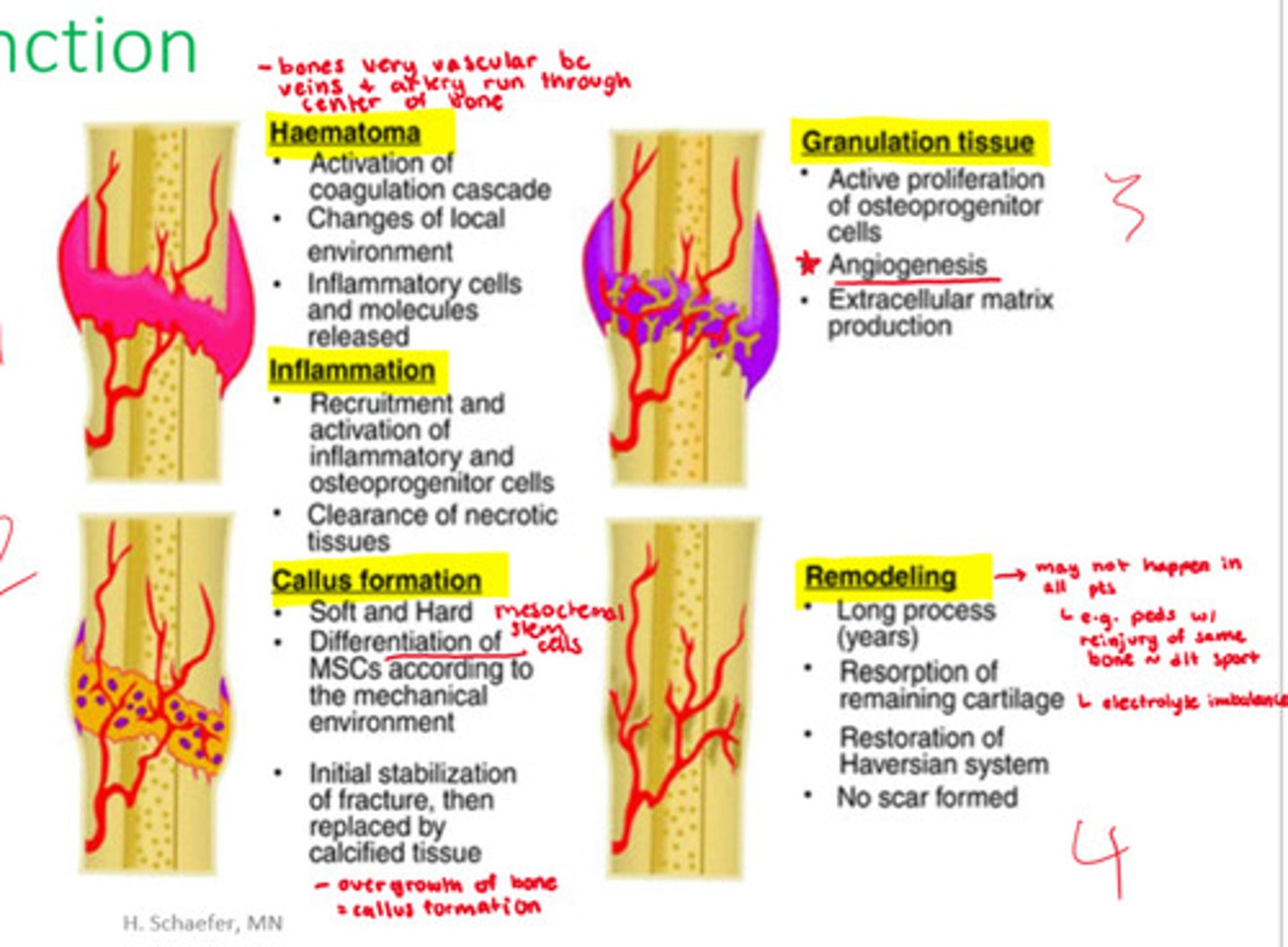
What happens in inflammation stage of fracture healing?
- recruitment and activation of inflammatory and osteoprogenitor cells
- clearance of necrotic tissues
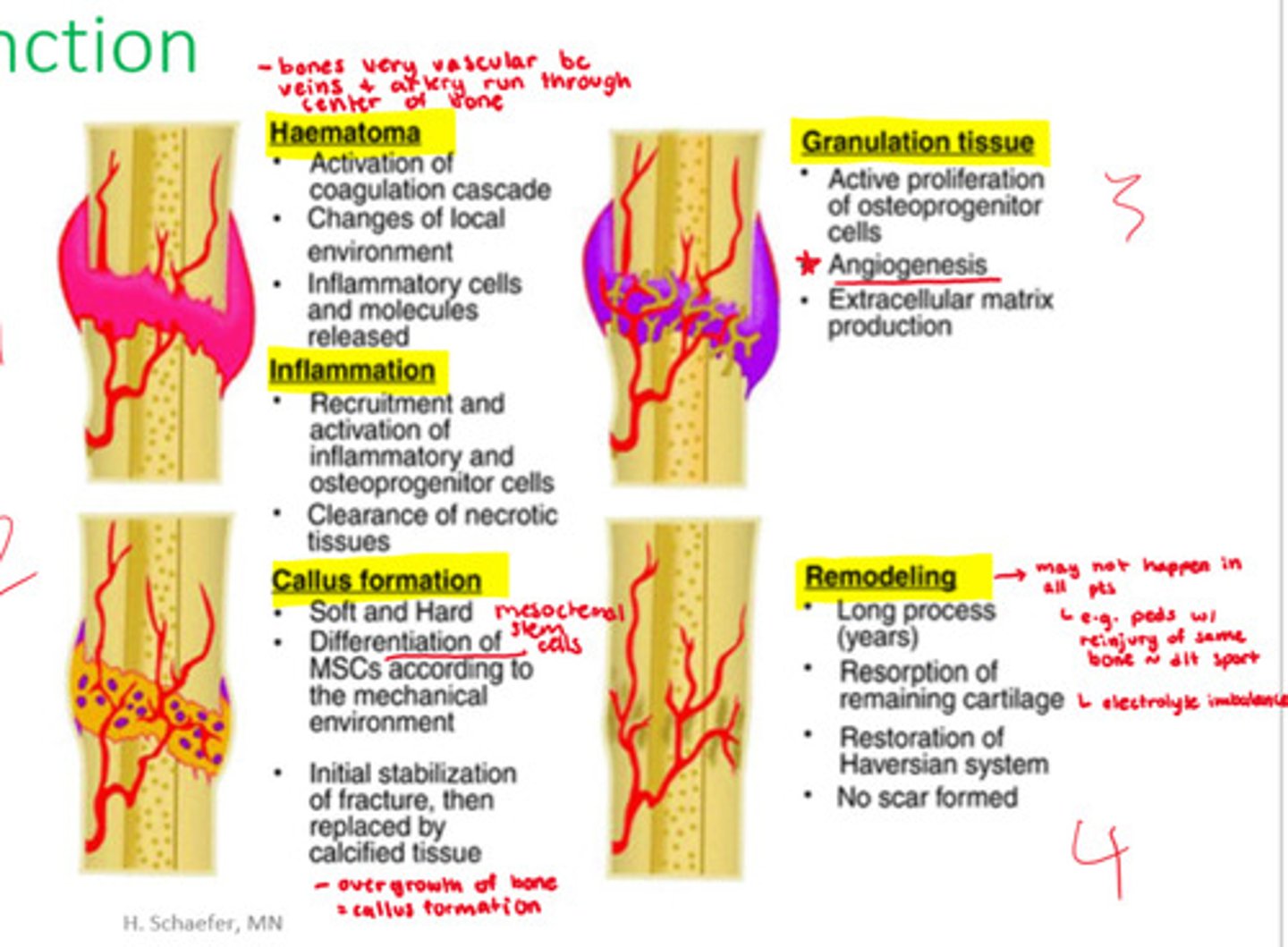
What happens in callus formation (overgrowth of bone) stage of fracture healing?
- soft and hard
- differentiation of mesenchymal stem cells d/t mechanical environment
- initial stabilization of fracture then replaced by calcified tissue
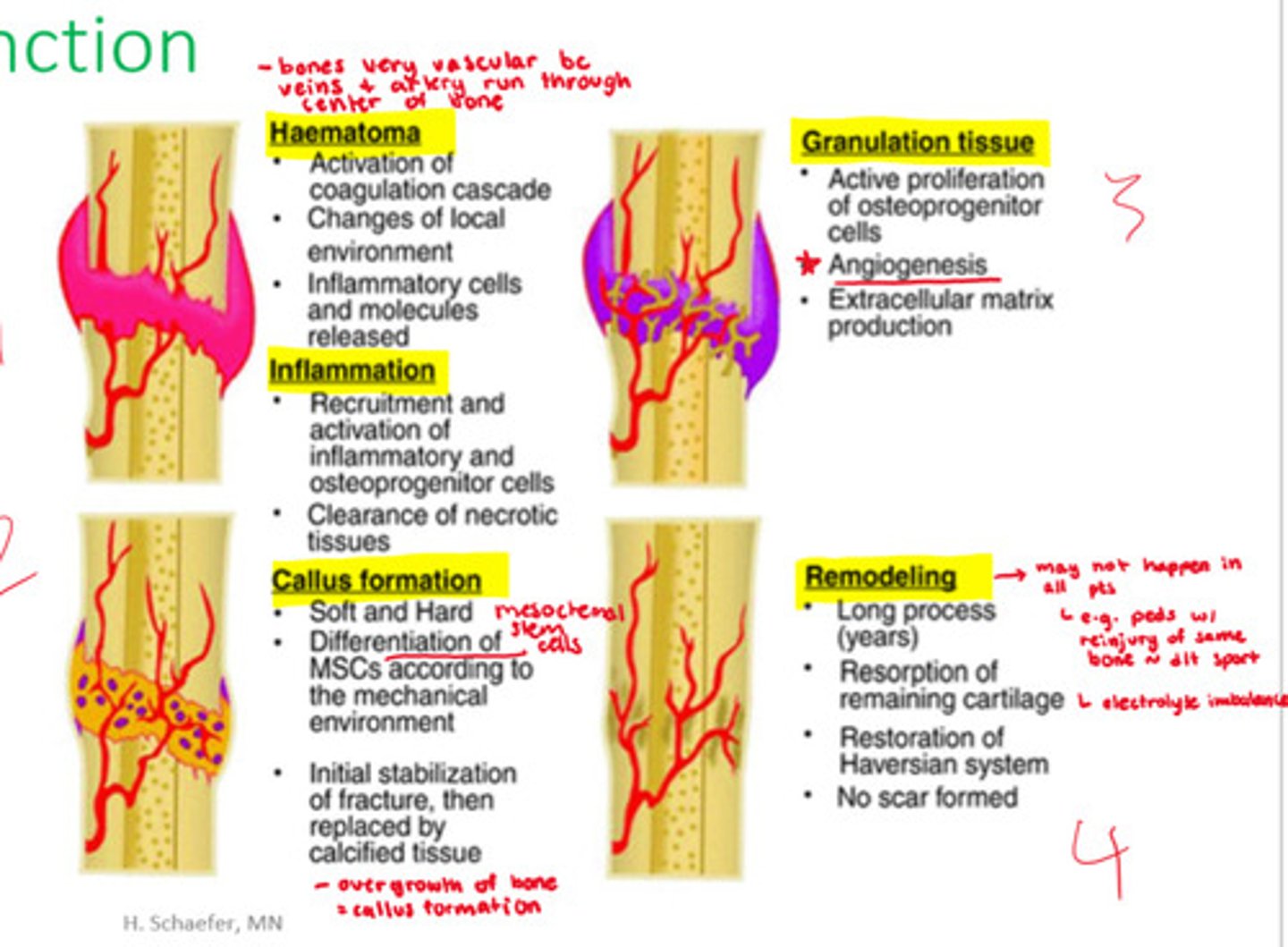
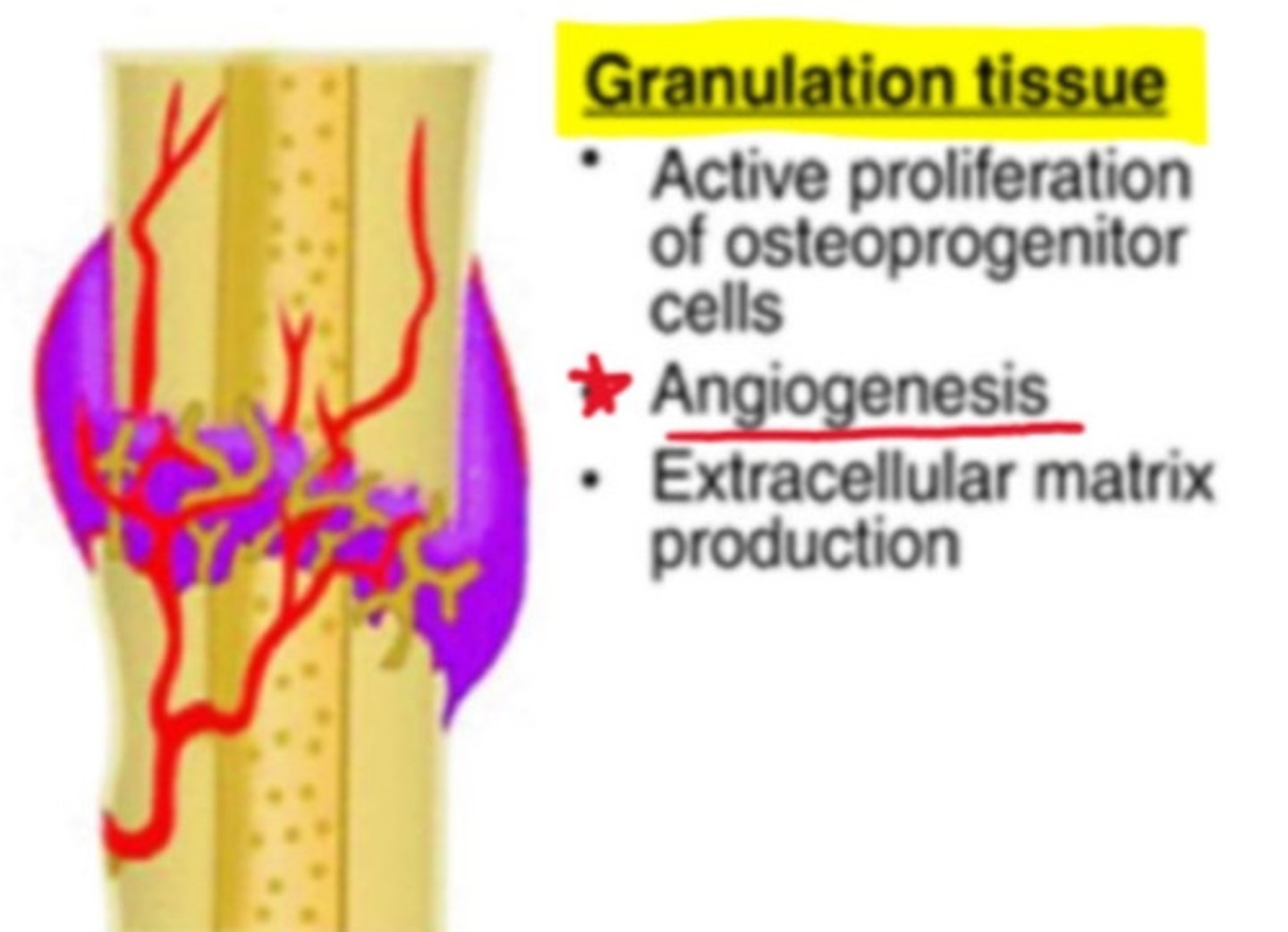
How does granulation tissue help restore function in fractures?
- active proliferation of osteoprogenitor cells
- angiogenesis
- extracellular matrix production
How does remodeling help restore function in fractures?
- long process (years)
- restoration of remaining cartilage
- restoration of Haversian system
- no scars formed
- note: may not happen in all patients => e.g. electrolyte imbalances or peds pts with reinjury of bone d/t sport
What are the potential complications of fractures
- vascular damage (hemorrhage => risk of hypovolemic shock)
- infection
- associated injuries (eg. pneumothorax, CNS injury)
- thromboembolism
- compartment syndrome
What are additional, less common complications of fractures
- fat embolism syndrome (FES)
- chronic pain: complex regional pain syndrome (CRPS)
- fracture blisters
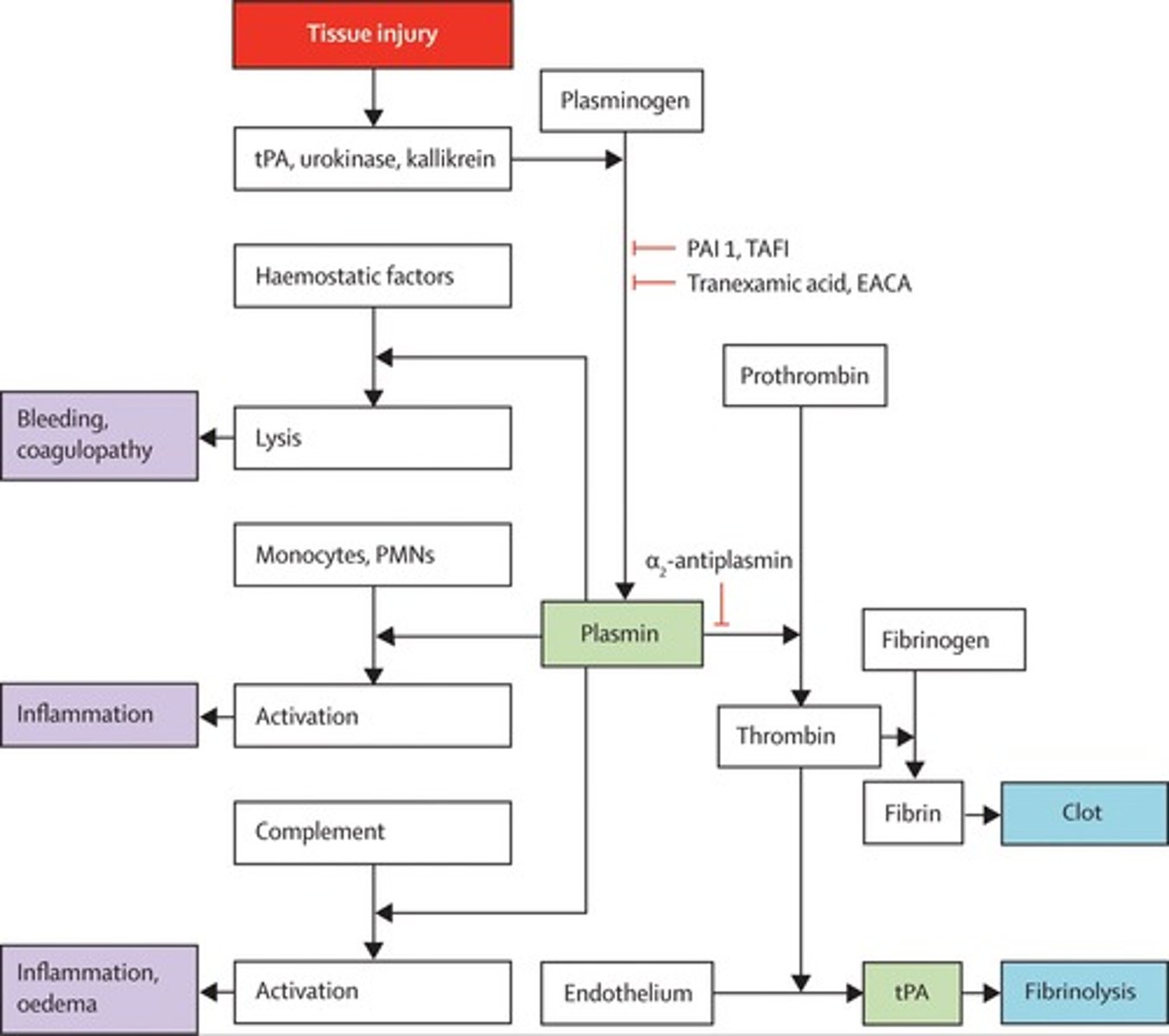
What is tranexamic acid
- antifibrinolytic (stops breakdown of clots)
- interferes with plasminogen during synthesis (breaking down clots)
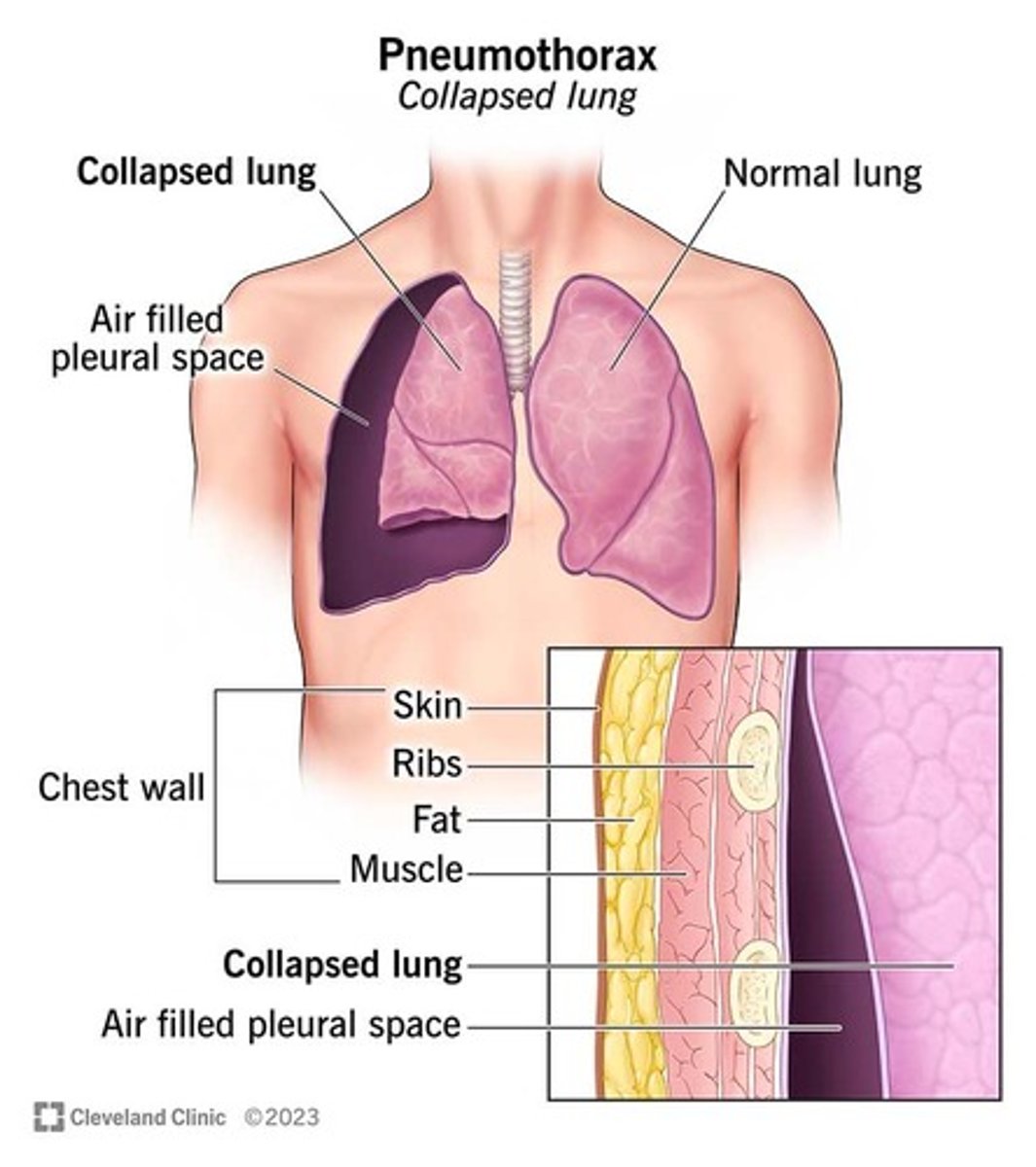
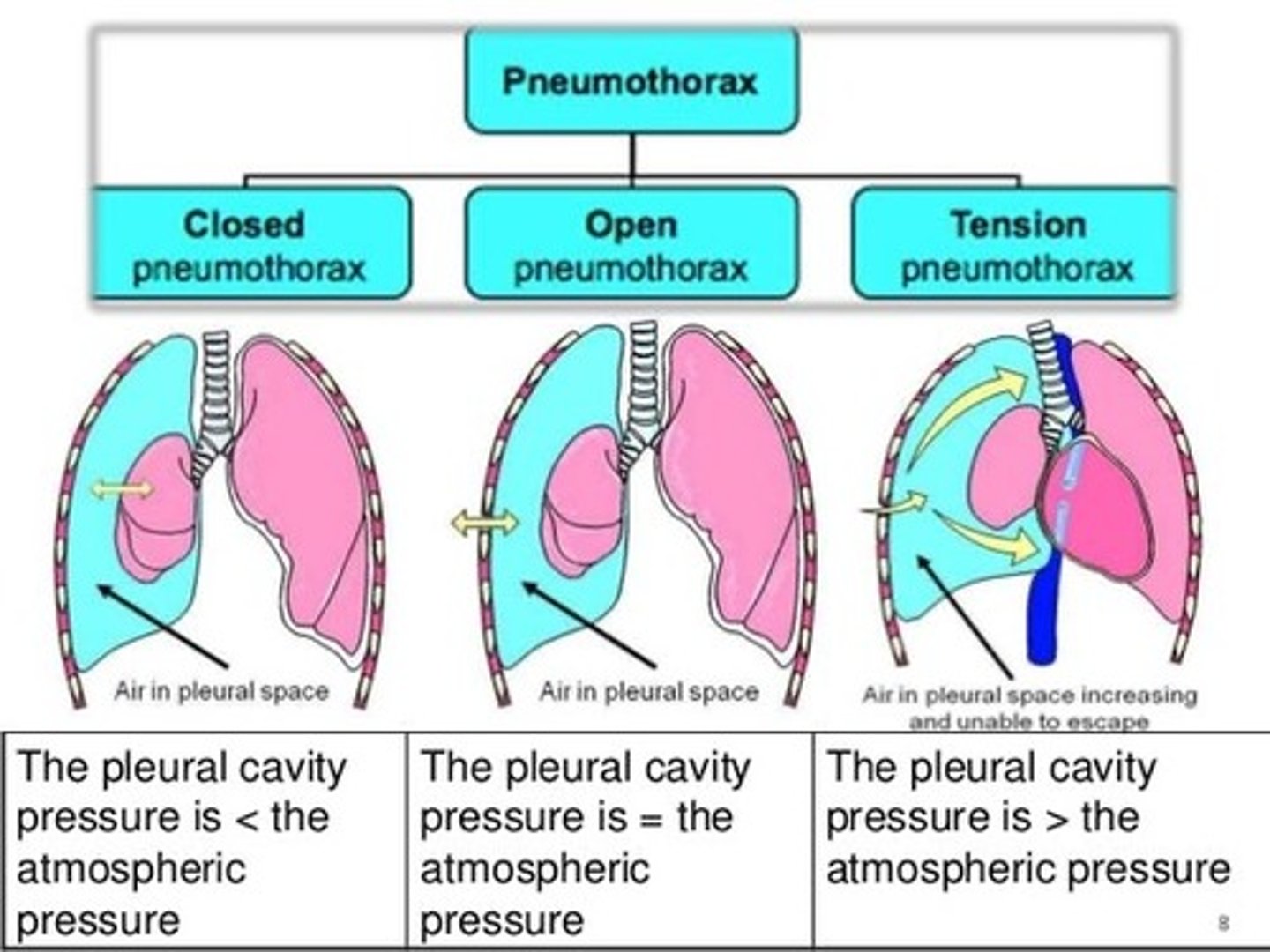
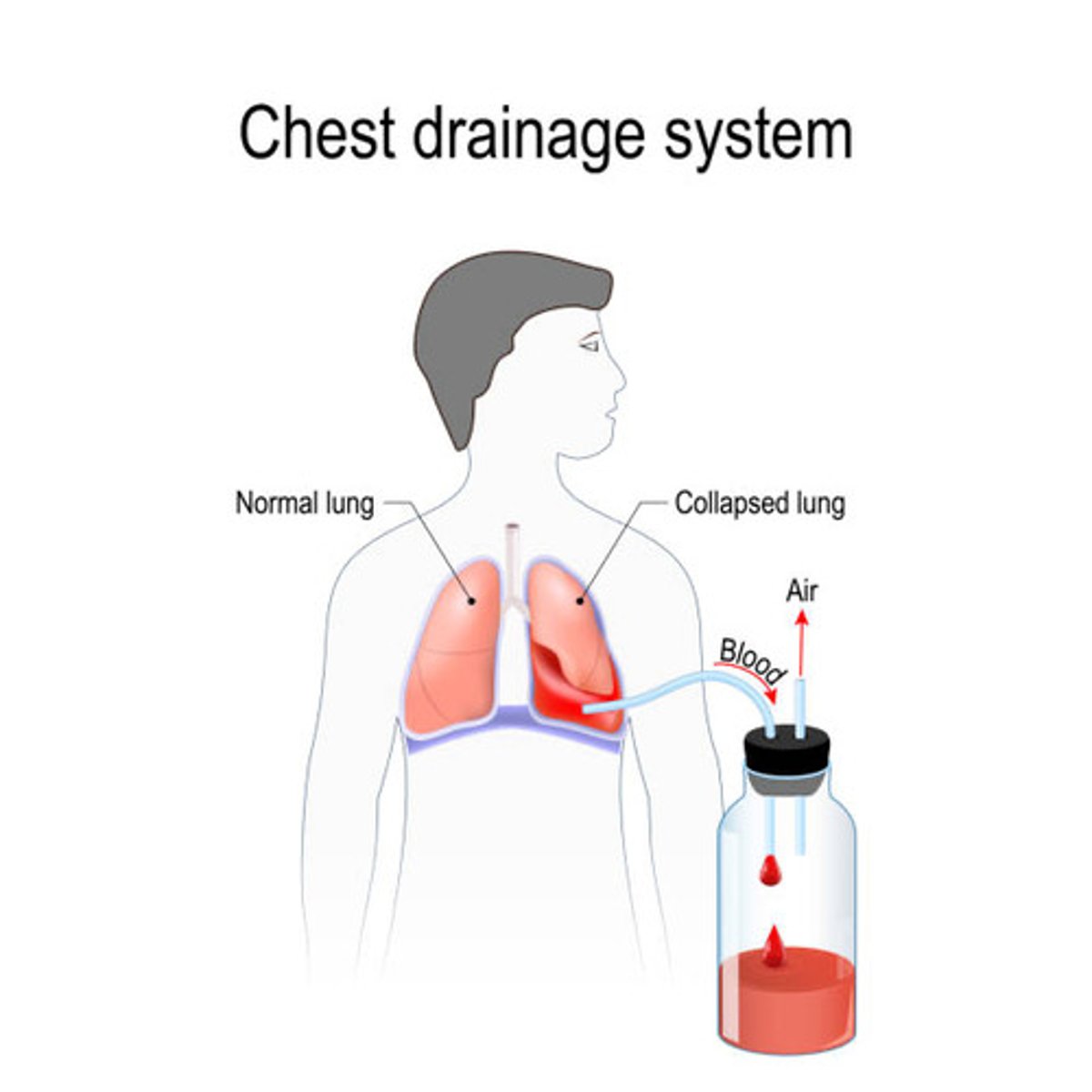
What is meant by pneumothorax overall
- air in the pleural space, compressing the lung as a result
- many classifications: tension vs pneumothorax
=> tension pneumo is an emergency!
What is a right-sided pneumothorax
- pressure within the lung is equal to atmospheric pressure
- reabsorption of air is still possible
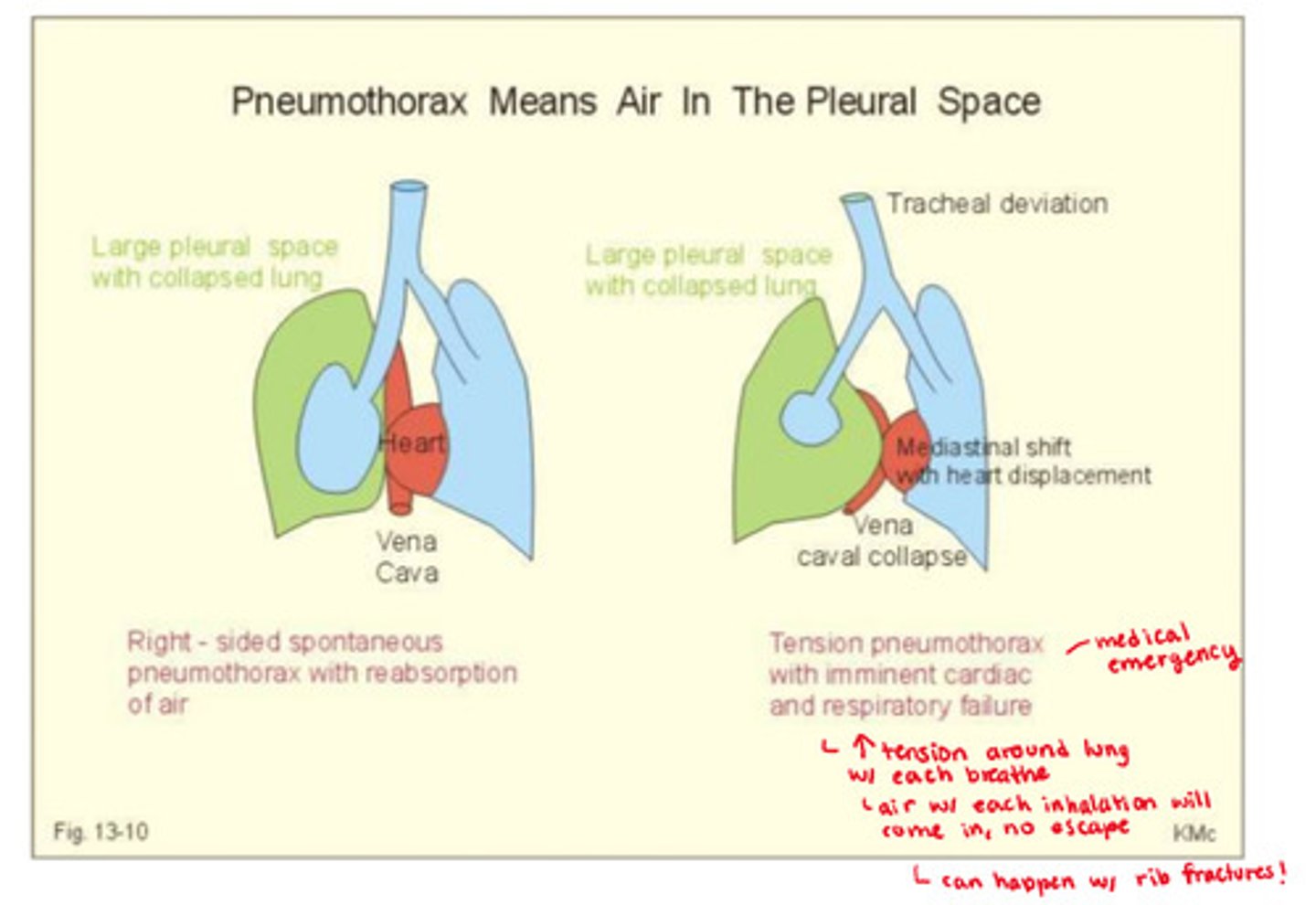
what are the pressure levels in the lungs during a tension pneumothorax
- increased tension around the lungs with each breathe, pleural cavity pressure is greater than atmospheric pressure
What are the cellular level damages that tension pneumothorax causes
- risk of hypoxemia
- compresses the myocardium, affecting CO
- risk of obstructive shock
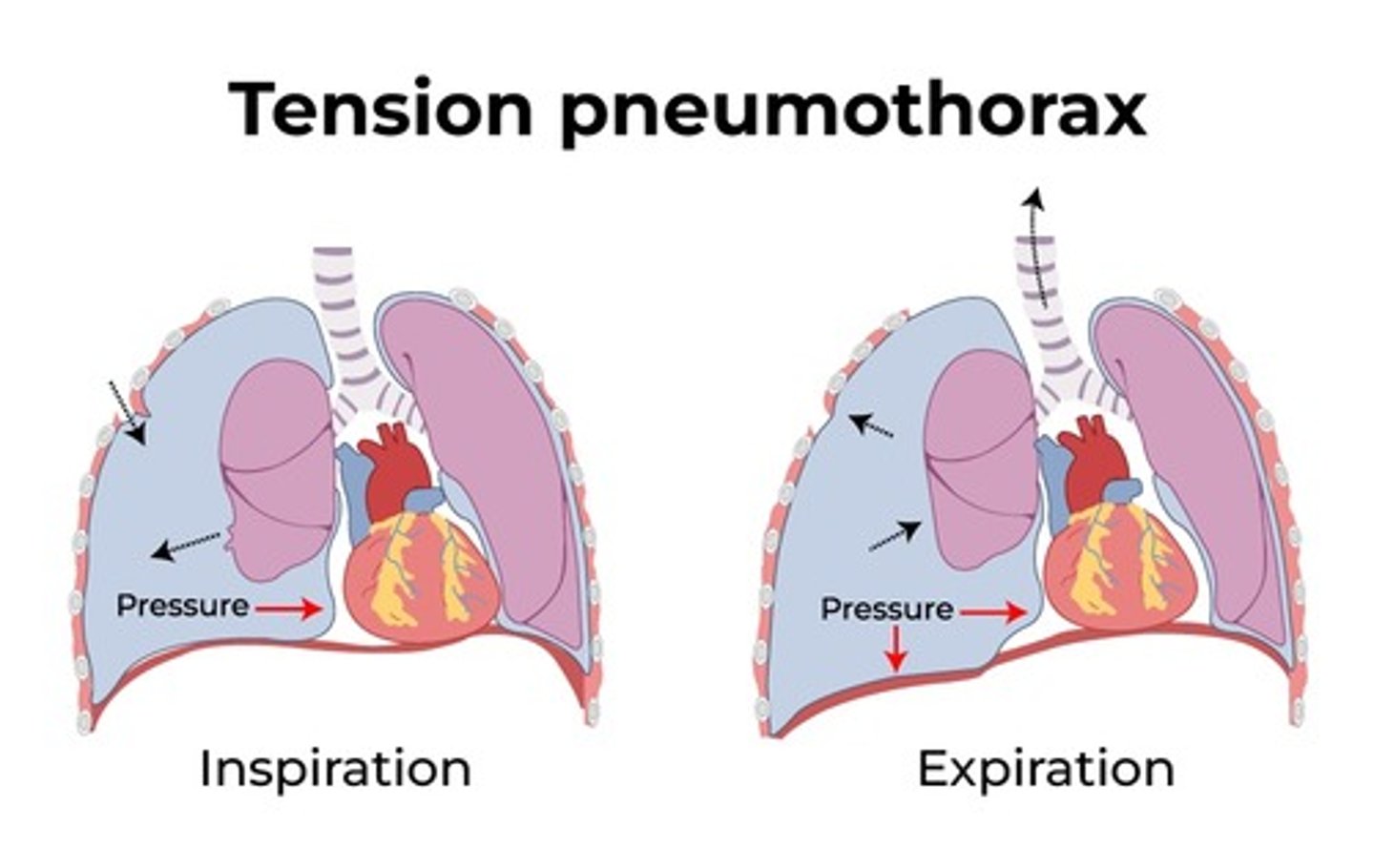
What are the s&s of a tension pneumothorax
- SOB
- declining O2 sats
- tracheal shift,
- signs of obstructive or cardiogenic shock
- may include cyanosis
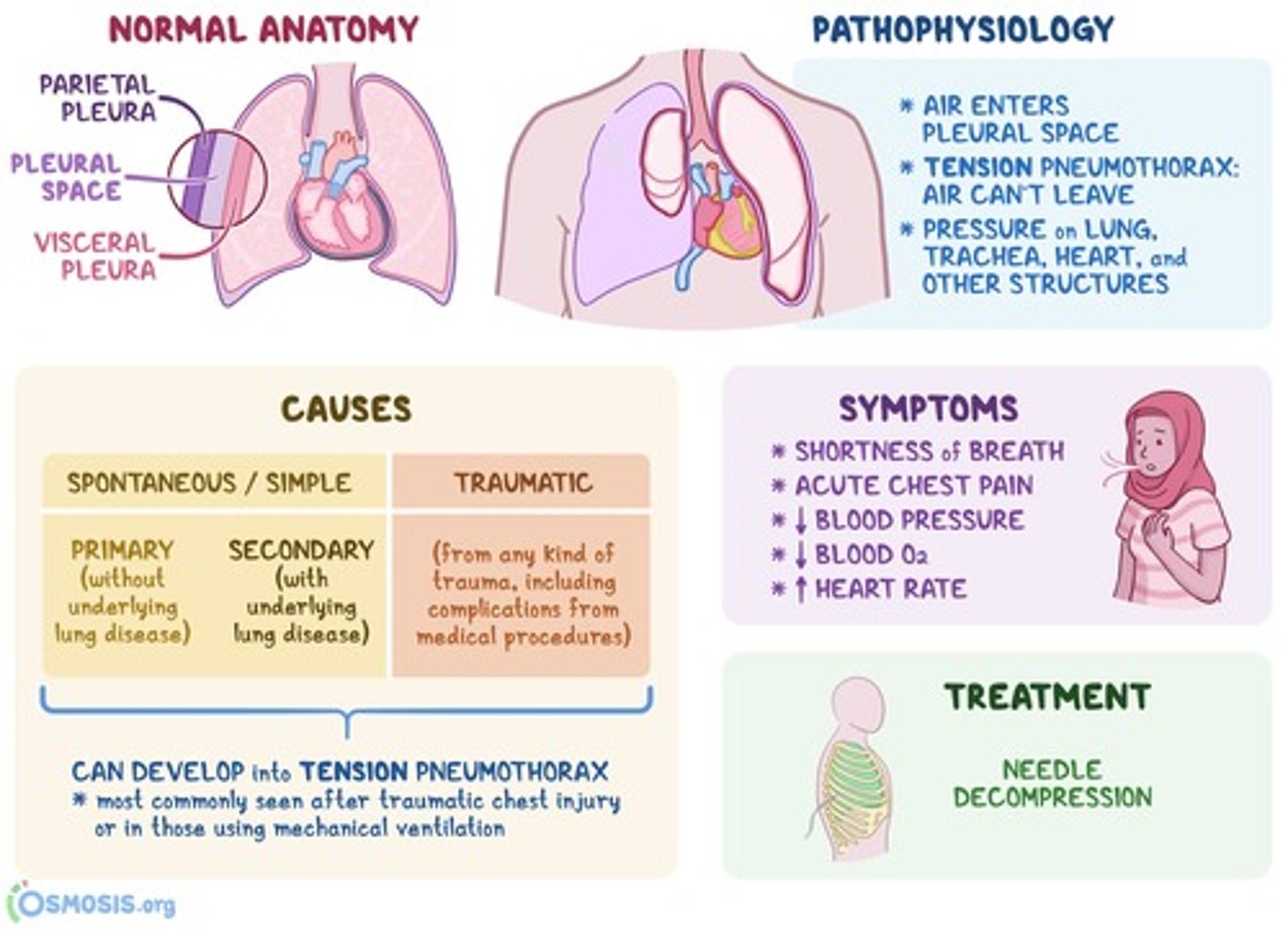
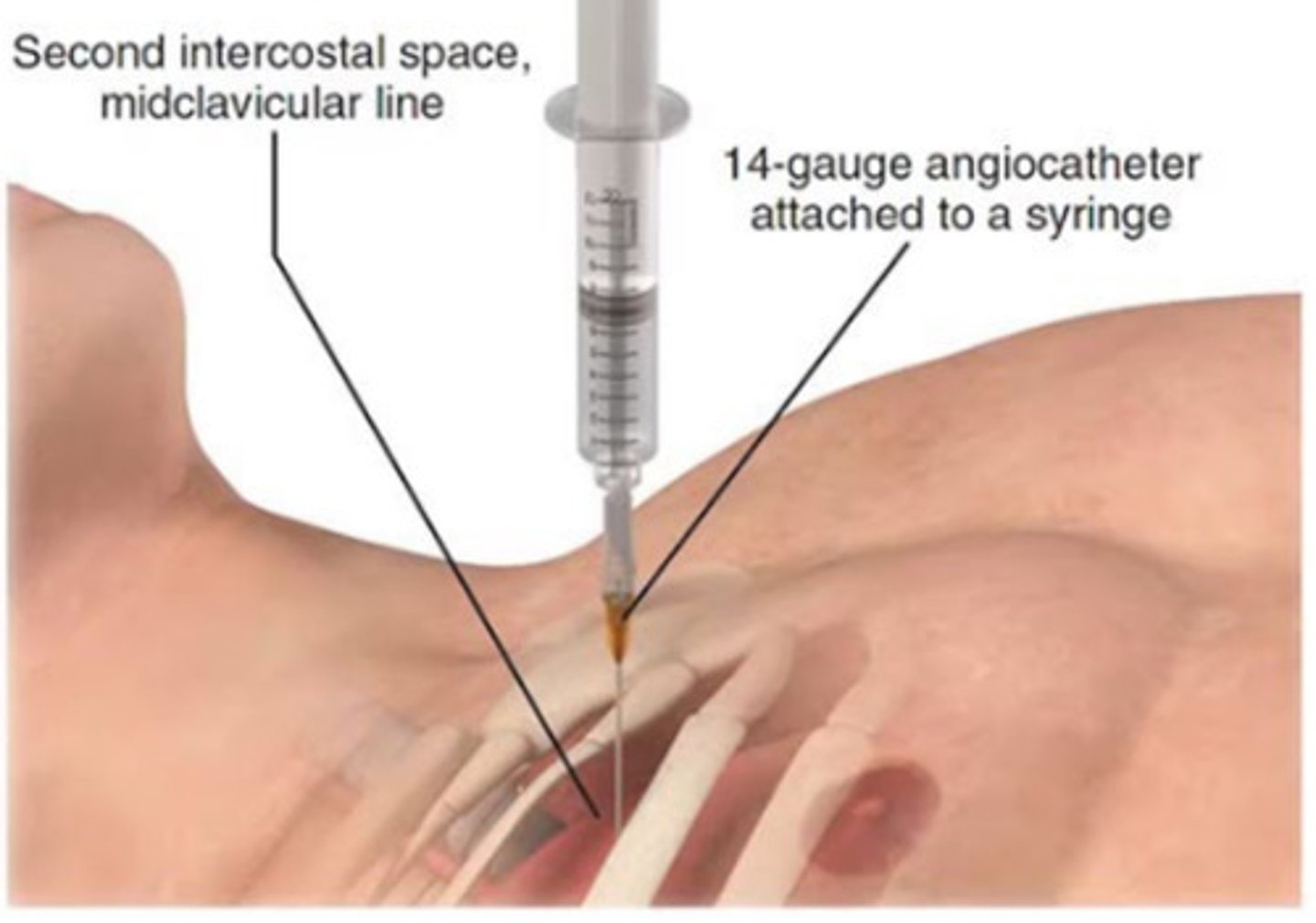
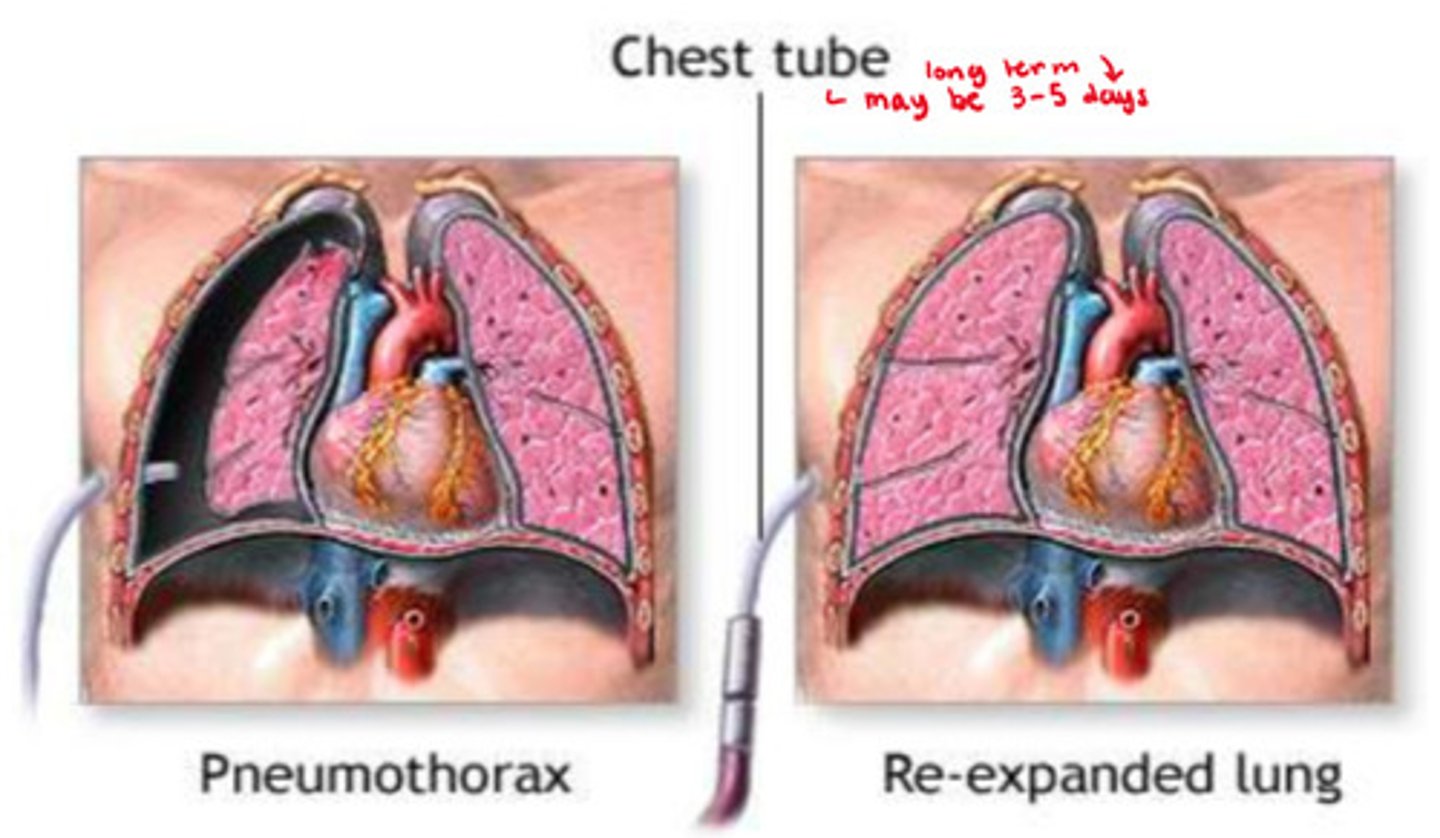
How do we tx a tension pneumothorax
- O2
- one-way valve seal
- chest tube = large needle into 2nd ICS to decompress air & allow for reinflation
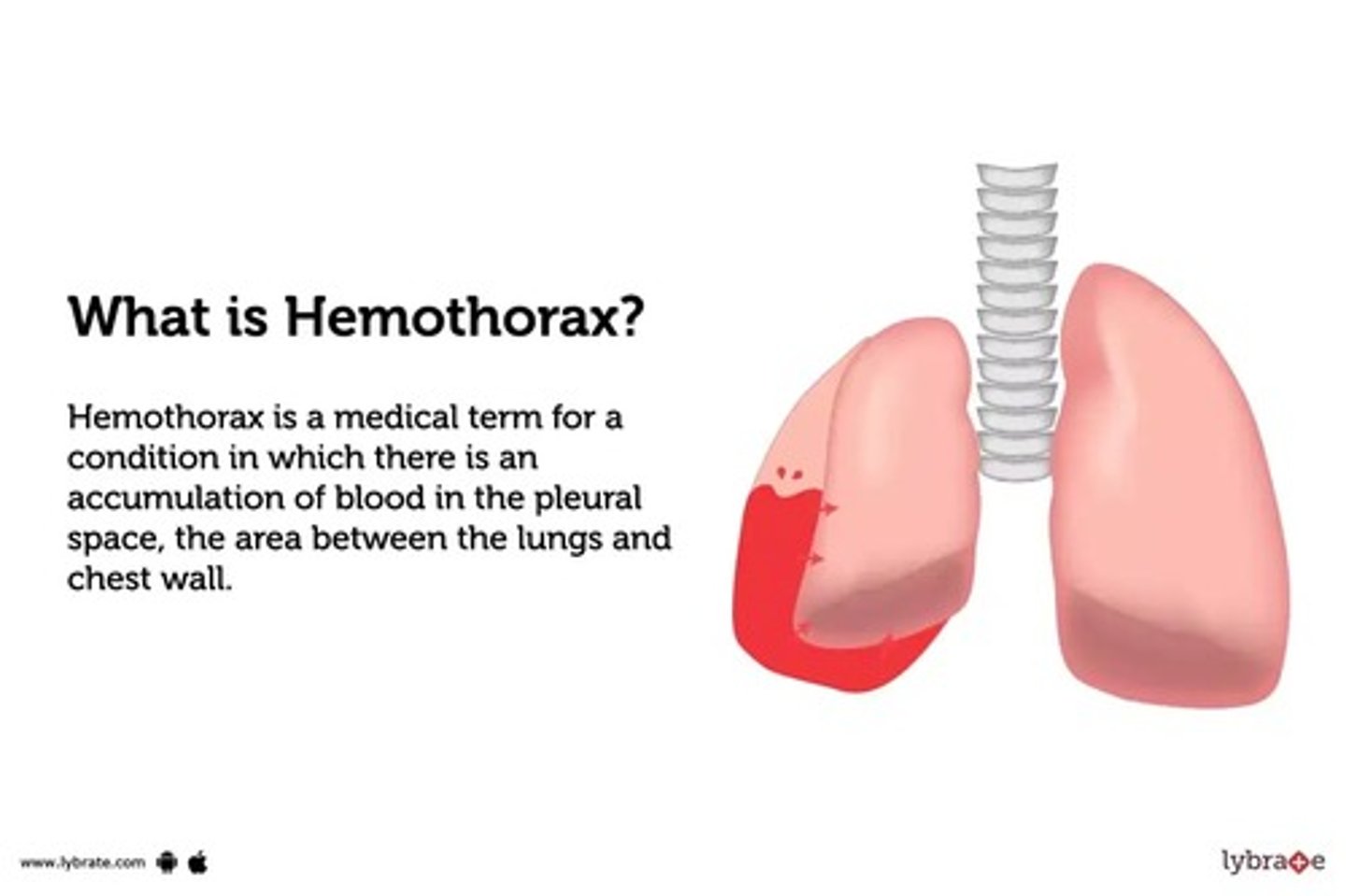
What is a hemothorax
- blood in the pleural space caused by bleeding (hemorrhaging)
- risk of hypovolemia & hypovolemic shock
- risk of low CO & cardiogenic shock
What is is a traumatic tension pneumothorax
- injury to the chest wall causes air to enter the pleural space but not to exit it
=> increase in pressure within the pleural space, compresses the lungs, causes lung collapse (always a medical emergency)
How would we tx a hemothorax
- chest tube into 8-9th ICS (INSTEAD OF 2nd)
- blood settles with gravity in the lower lung regions, why we need lower needle/chest tube placement
What are the clotting risks in fractures
- thromboembolism (DVT, PE)
- high risk in hip fractures, trauma (up to 60% of hip fracture patients)
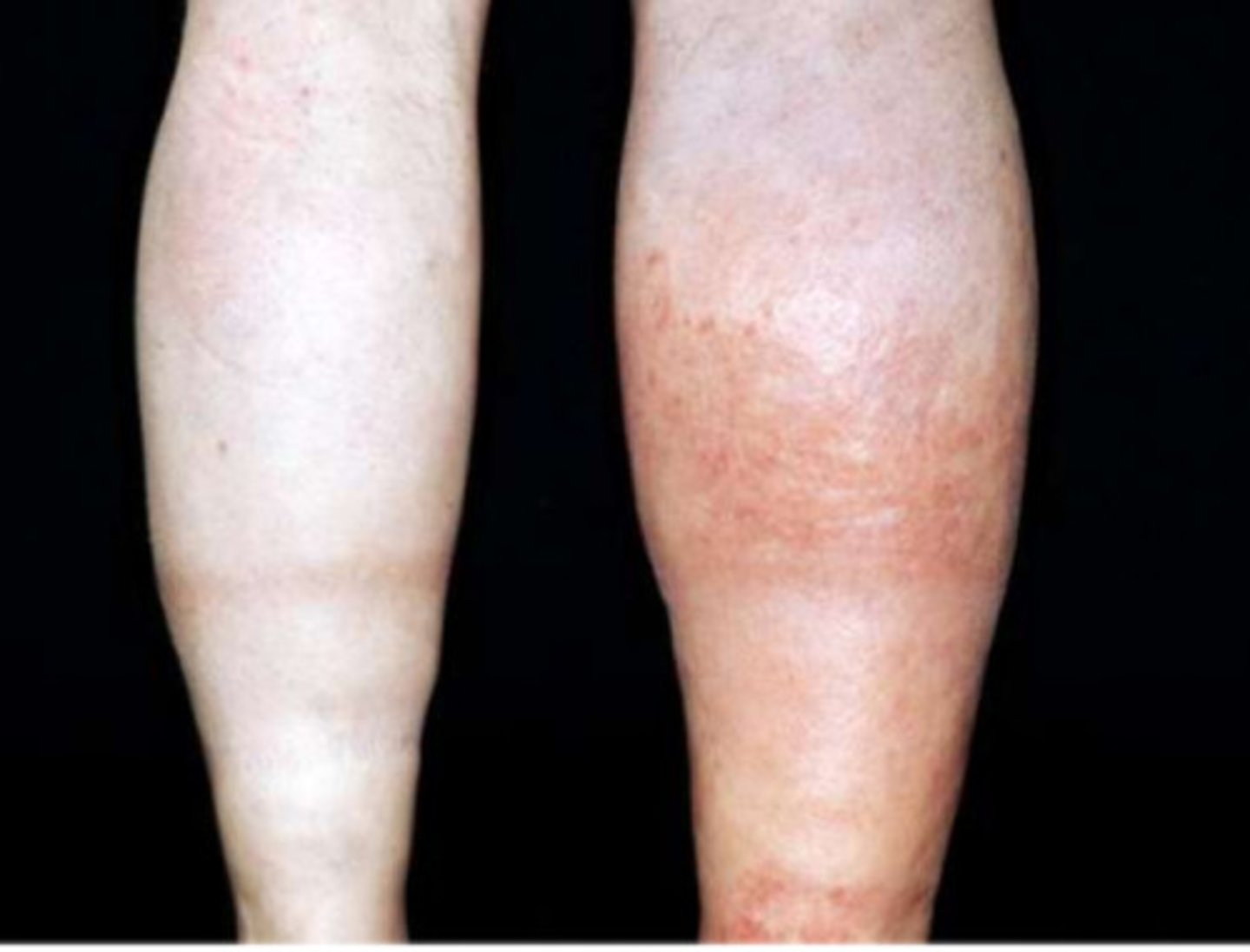
What are the DVT s&s & how to dx
- s&s: edema, erythema, pain; unilateral
- dx: ultrasound

What are the PE s&s and how to dx
- s&s: chest pain, SOB, low O2 sat (or low normal range)
- dx: CT scan
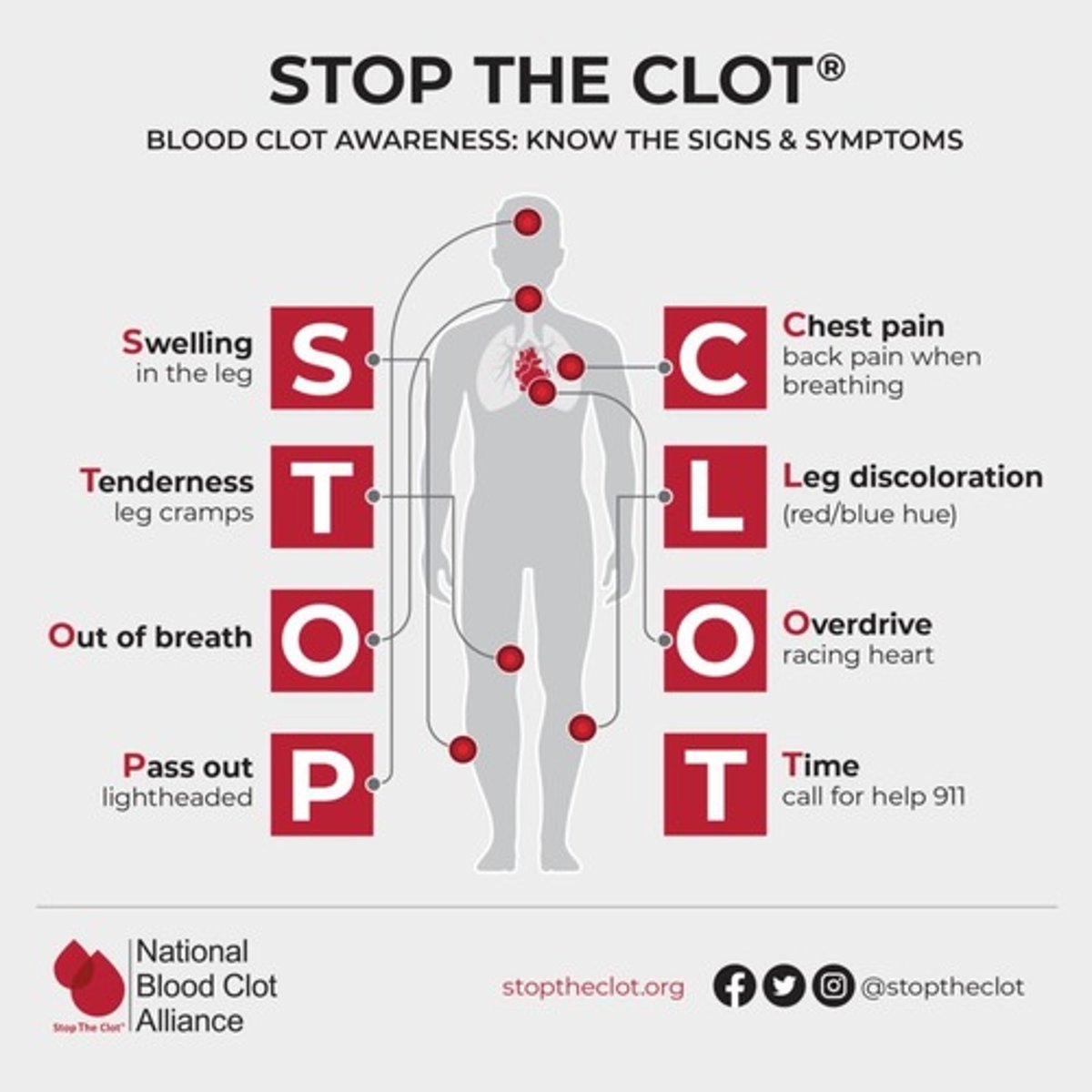
How to tx thromboembolisms
- anticoagulants: tPA, heparin; enoxaparin
- pneumatic compression devices
- early ambulation

What are the thrombus risk factors
- venous stasis (eg. decreased mobility, arrhythmias eg. Afib)
- high viscosity (eg. dehydration)
- tissue injury (eg. surgery, inflammatory diseases, atherosclerosis, infection)
- smoking (eg. cytotoxic => endothelial injury, oxidation of LDLs)
- drug induced
- inherited disorders
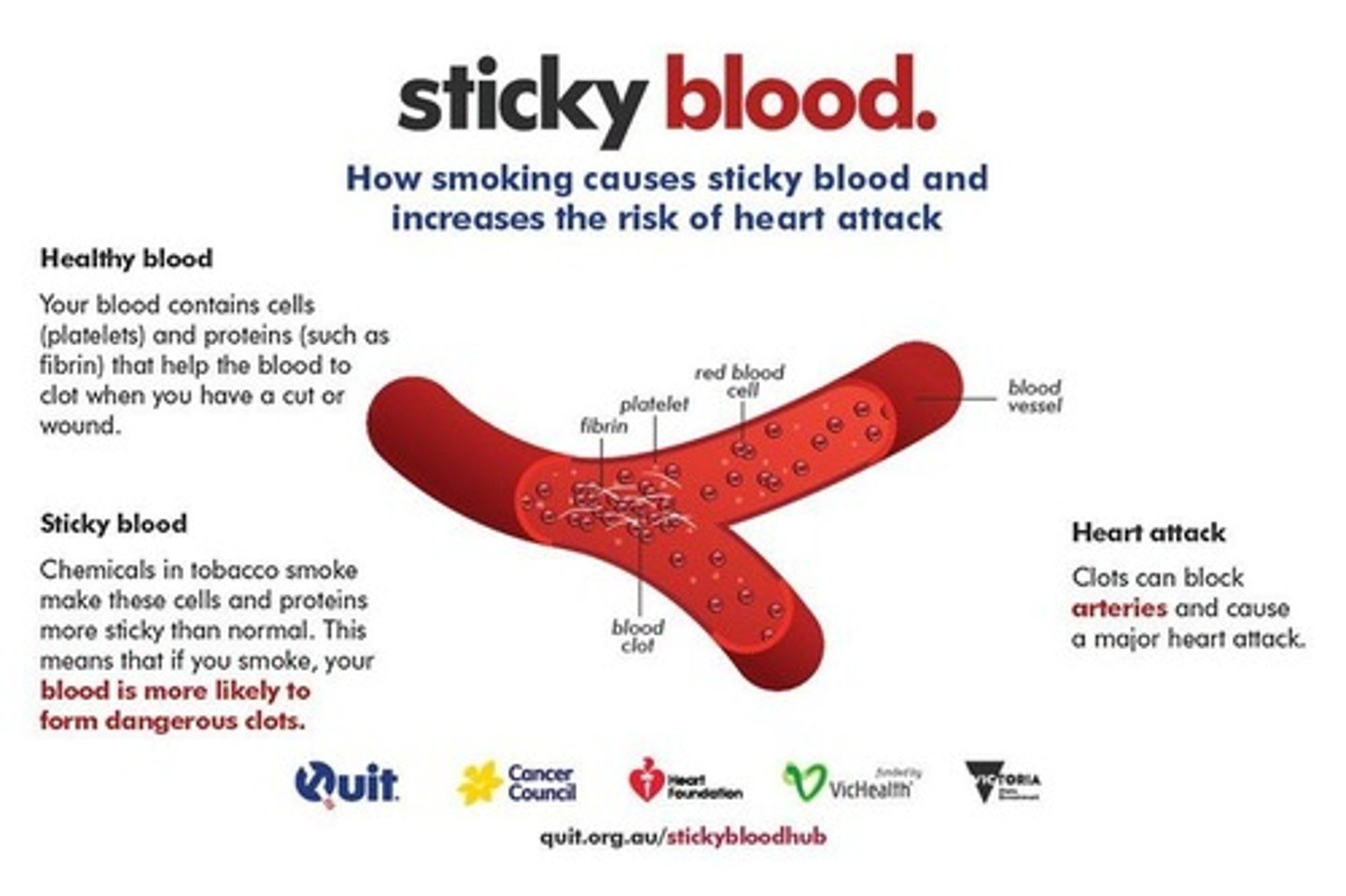
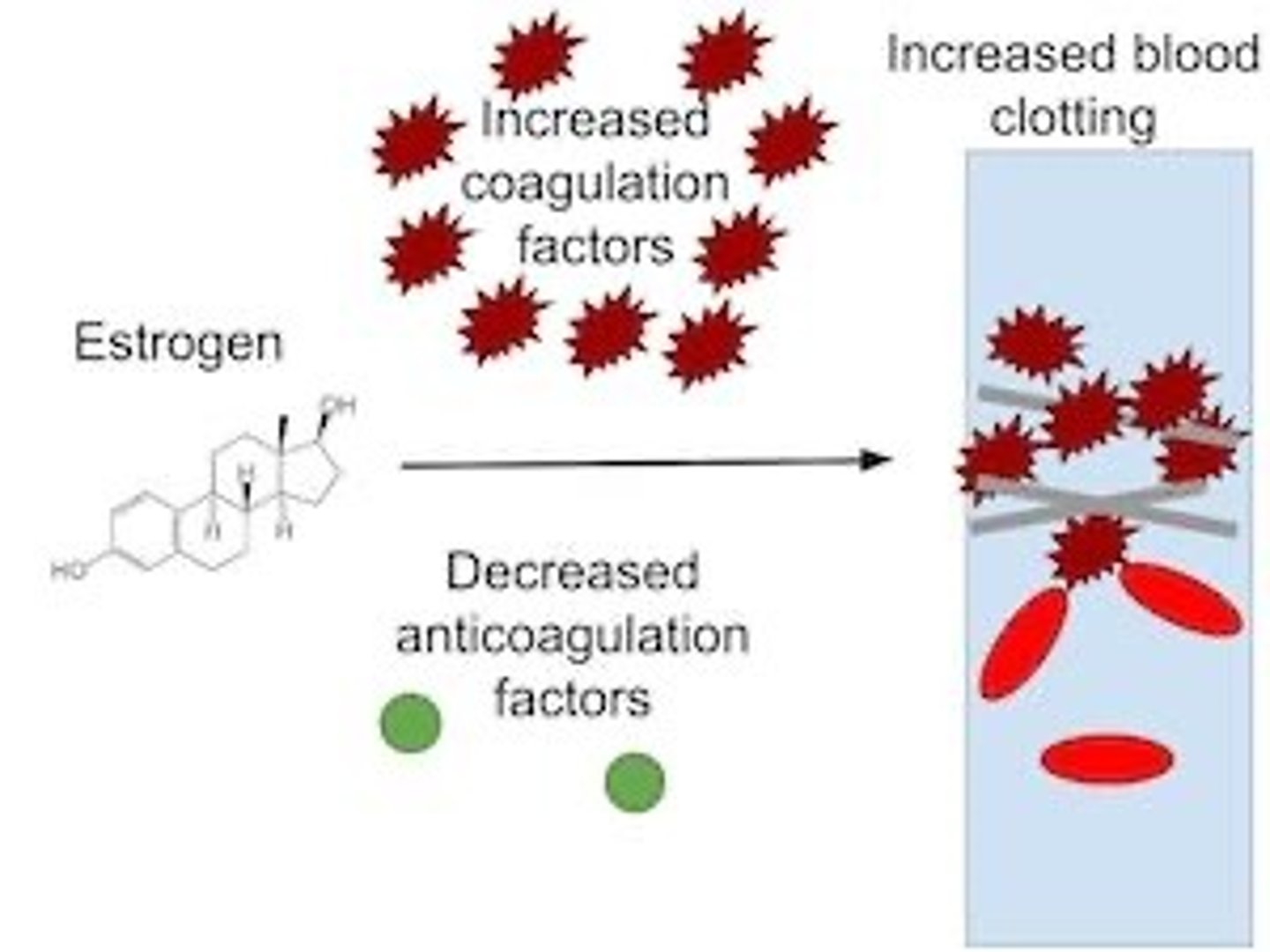
What are drug induced thrombosis risk factors
- Heparin HITT
- birth control (high estrogen) => increased hepatic coagulation factor synthesis & decreased clot lysis
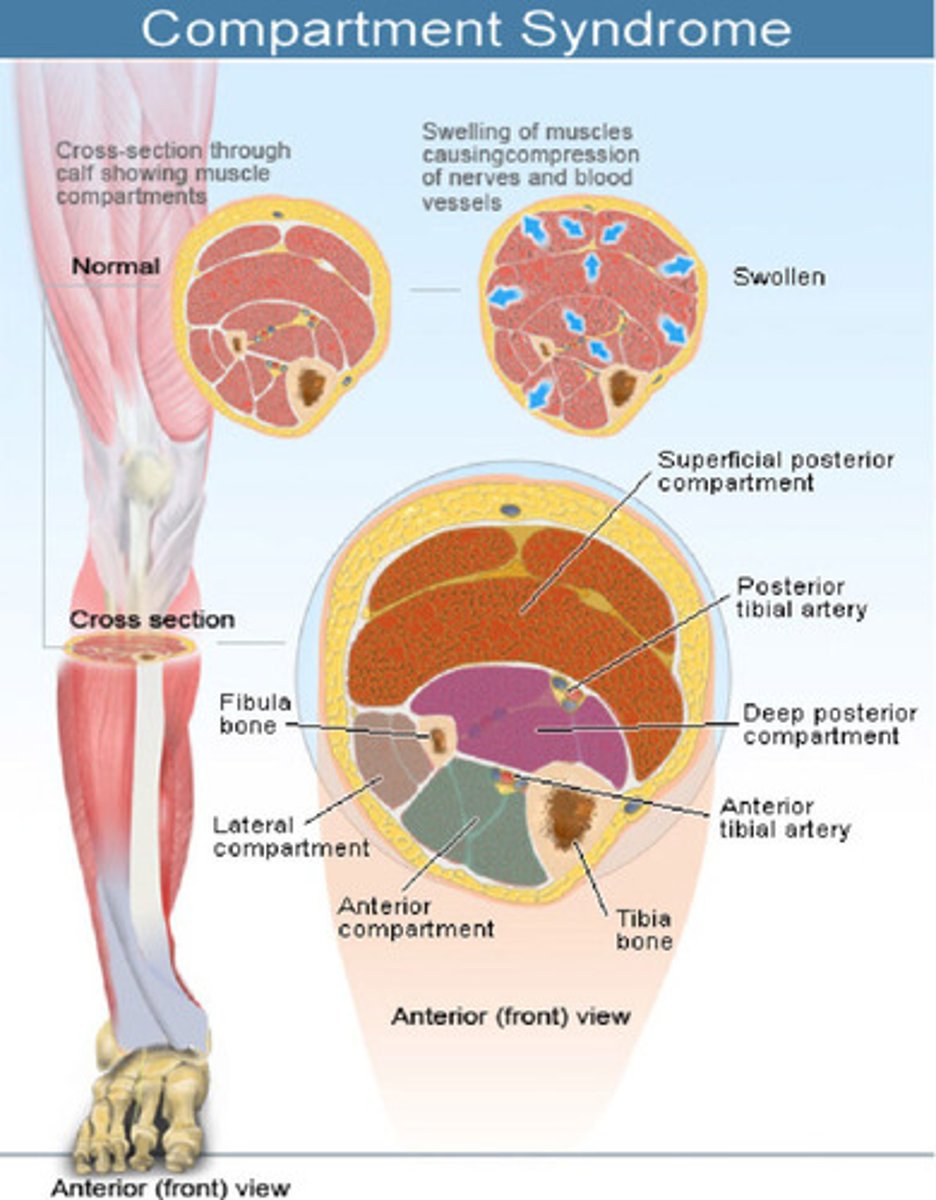
What is compartment syndrome (acute)
- high pressure within a body compartment (fascia - contains muscles, nerves & vessels)
- due to injury's inflammatory sequelae causing increase in volume
- emergency! risk of total loss tissue/extremity/necrosis
increased pressure => ischemia & hypoxia => tissue damage
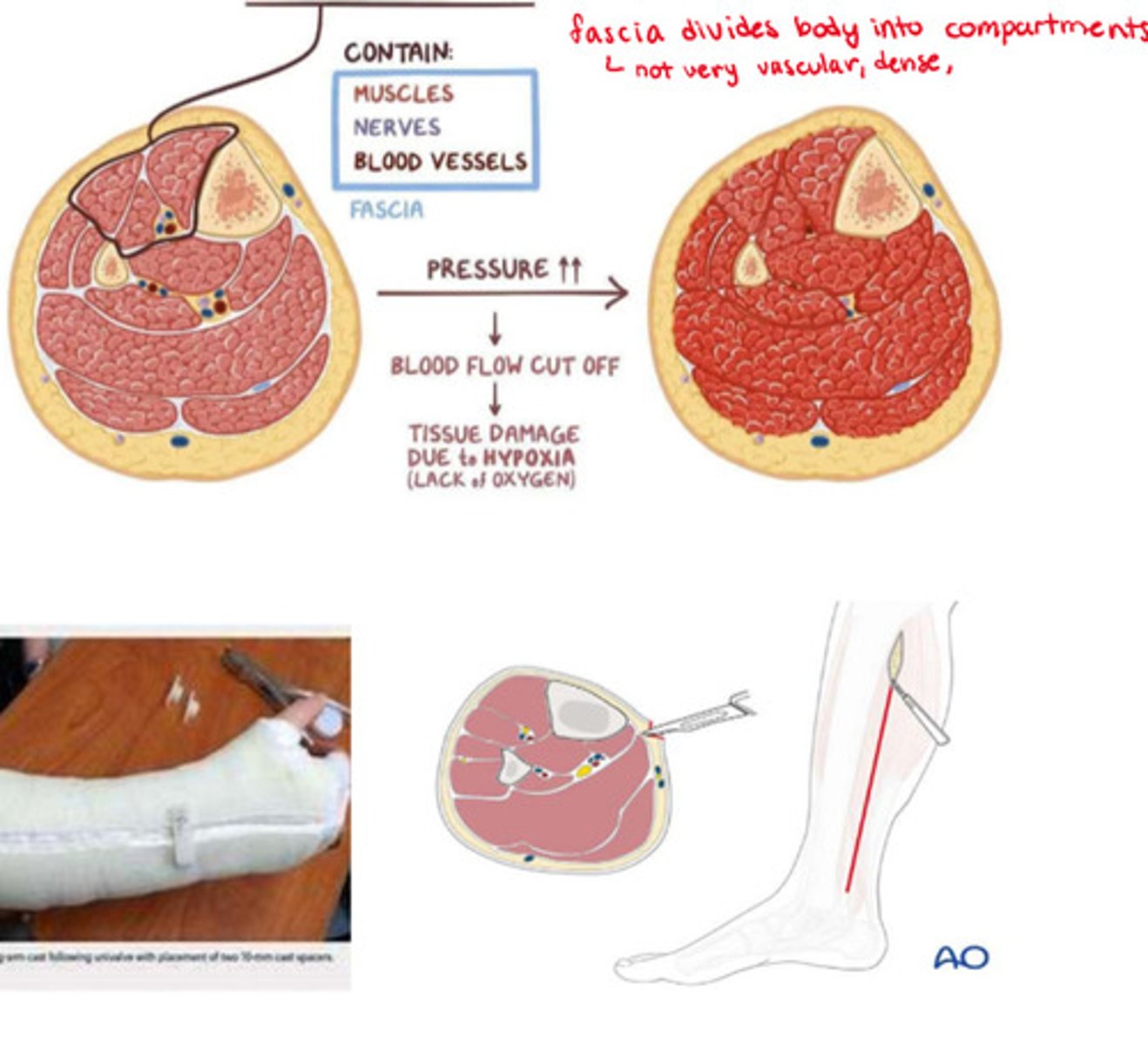
What is the etiology of compartment syndrome
- post injury
- common with immobilization devices (d/t swelling after insertion of an eg. cast)
- may take hours to days onset

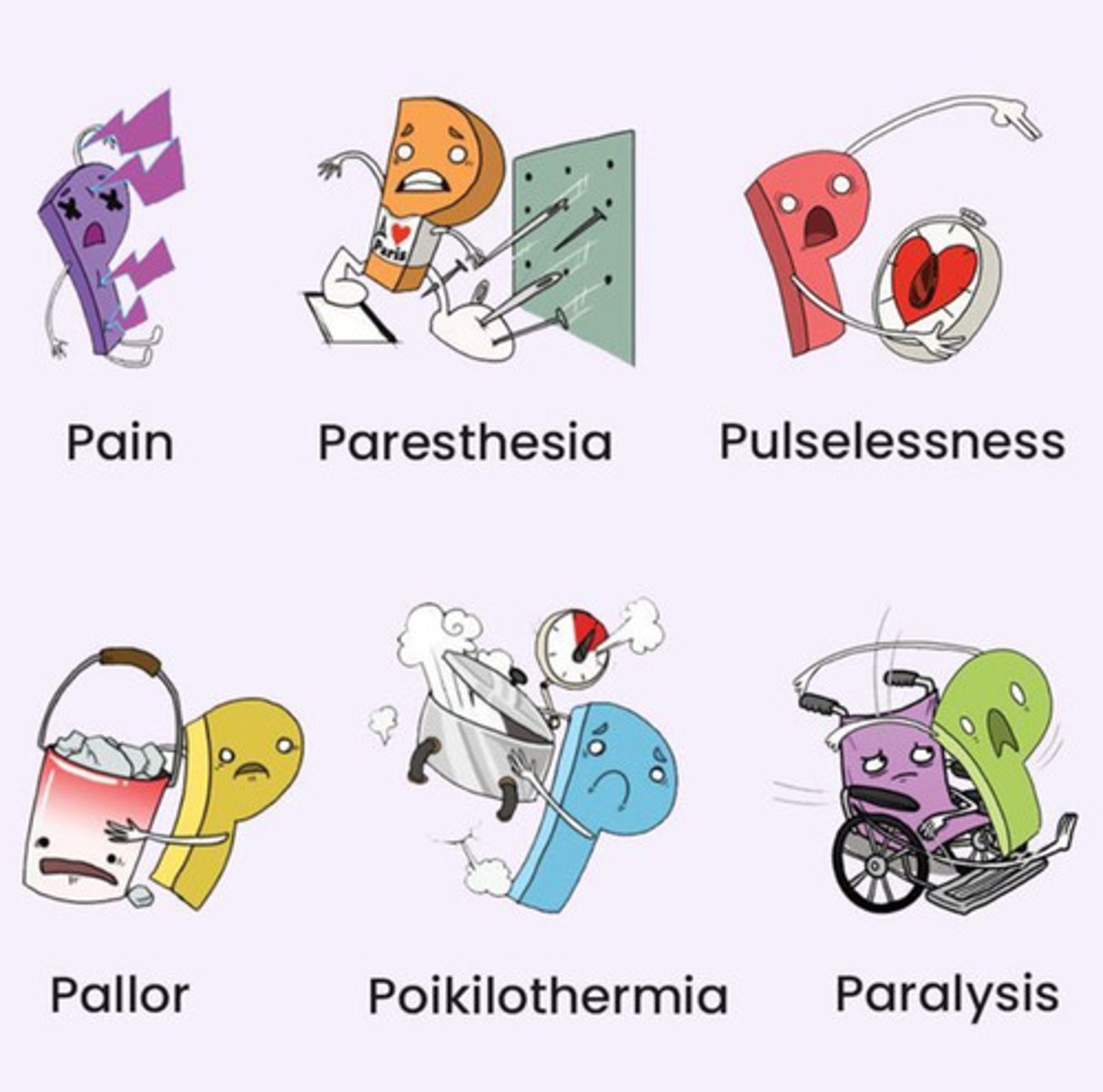
What are the s&s of compartment syndrome
The "6 P's"
- worsening pain (sudden)
- pallor
- paresthesia (pins & needles, nerve supply is impacted)
- puffy (edema)
- paralysis (of distal segments)
- pulses are usually normal!!!
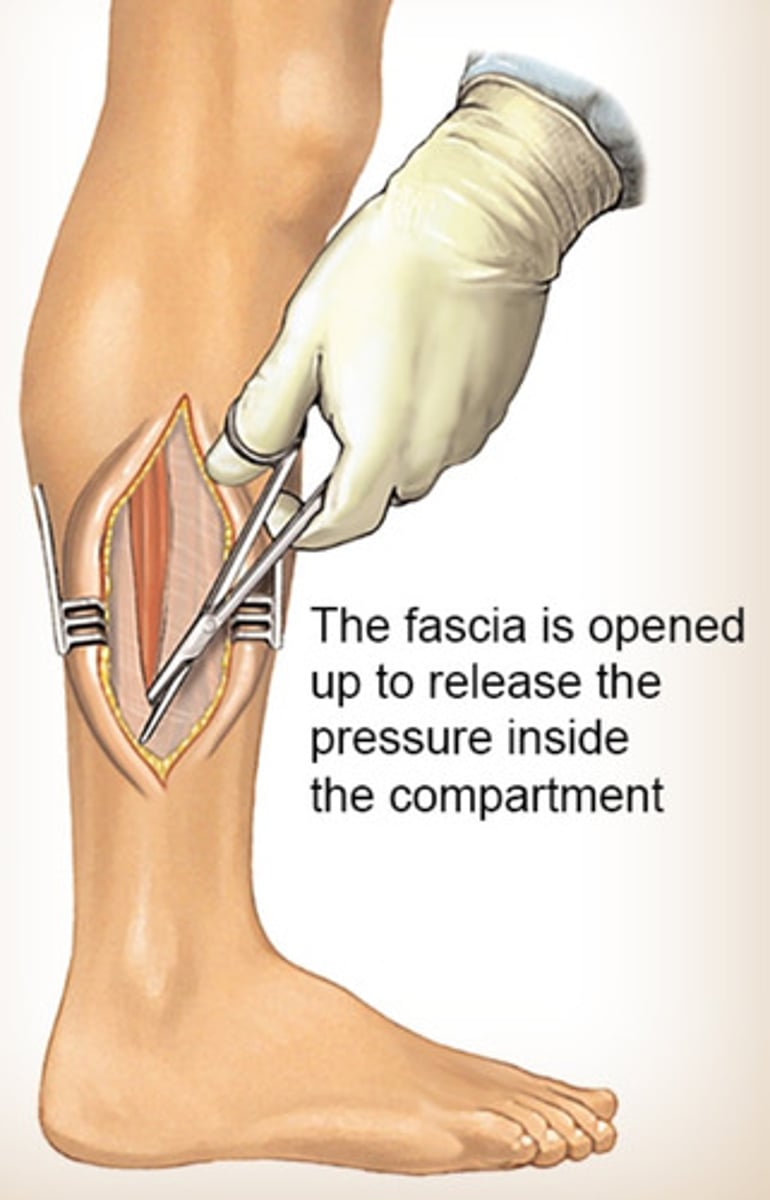
How do we tx compartment syndrome
relieve pressure immediately!!
- elevate
- relieve cast/dressing ('bivalve' cast => spilt the cast open to relieve pressure)
- fasciotomy => slicing fascia open surgically to relieve pressure
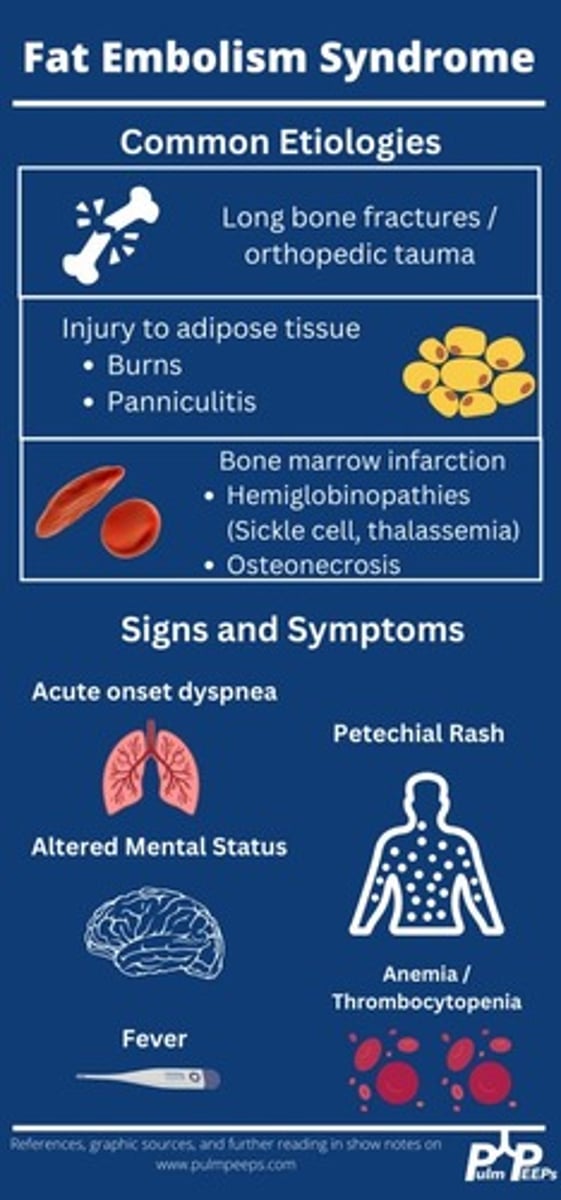
What is fat embolism syndrome (FES)
- adipose tissue or bone marrow tissue migration into circulation
- with diffuse (widespread/non-localized) symptomology of interrupted perfusion
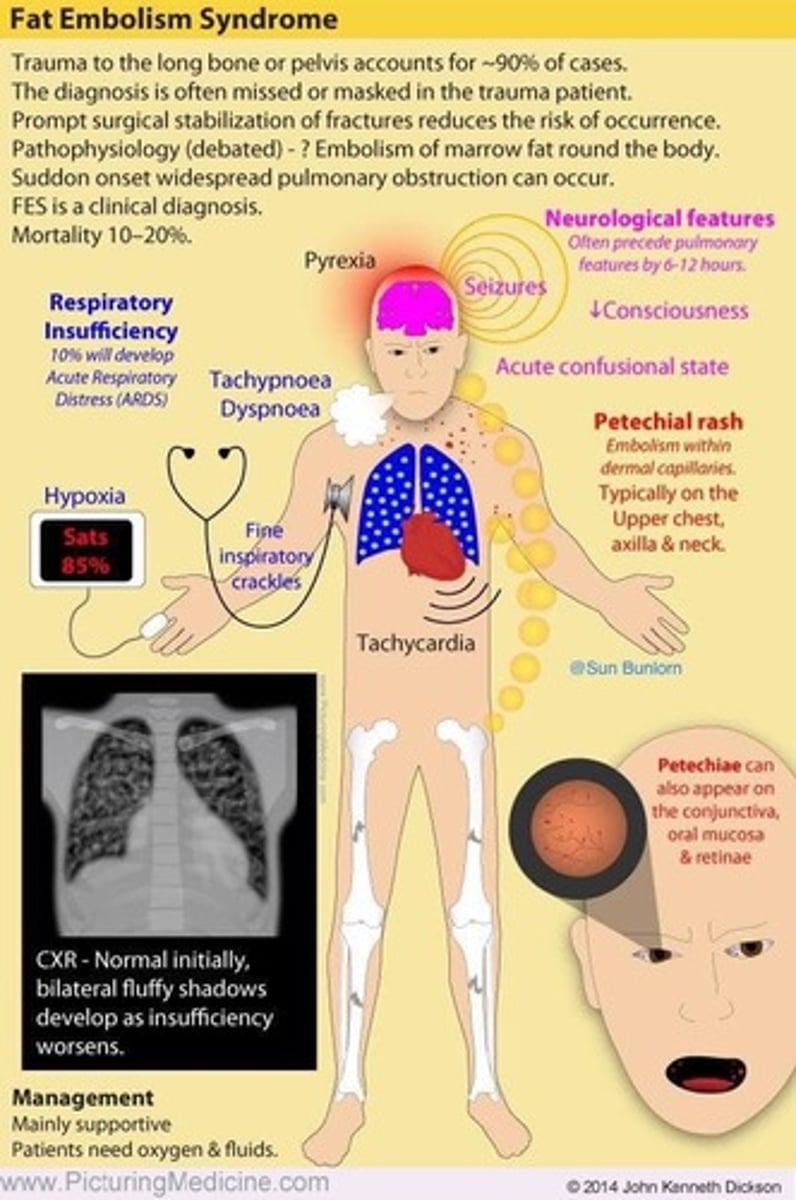
What is the etiology of FES
- long bone fractures
- range of onset => 3 hours-3 days post injury
What are the S&S of FES
- PE signs, CVA signs, skin rash
- chest pain, SOB, decreased O2 sats, cyanosis, pallor
- LOC (slight at first - disorientation), seizures
- diffuse (aka petechial) rash: usually over upper body, oral cavity, conjunctiva

What is a diffuse (petechial) rash
Micro-hemorrhaging into tissues, usually seen at distal sites of injury

How to tx FES
- prevention is best - early stabilization (eg. reduction, immobilization) of fractures
- O2
- glucocorticoids

What is complex regional pain syndrome (CRPS) & its etiology
- higher pain than injury warrants
- etiology: can be associated with poor analgesia in acute pain (could be weeks post injury)

What are the S&S of CRPS
- pain more extreme than injury
- pain characteristics: severe, burning, aching
- pain elicited by very low stimulus
- physiologic changes to skin (shiny, thin, eczema) & tissue (eg. muscle wasting)

How to tx CRPS
- prevention with adequate acute pain analgesia
- physiotherapy for mobilization
- chronic pain treatment (non-opioid; eg. NSAIDs)
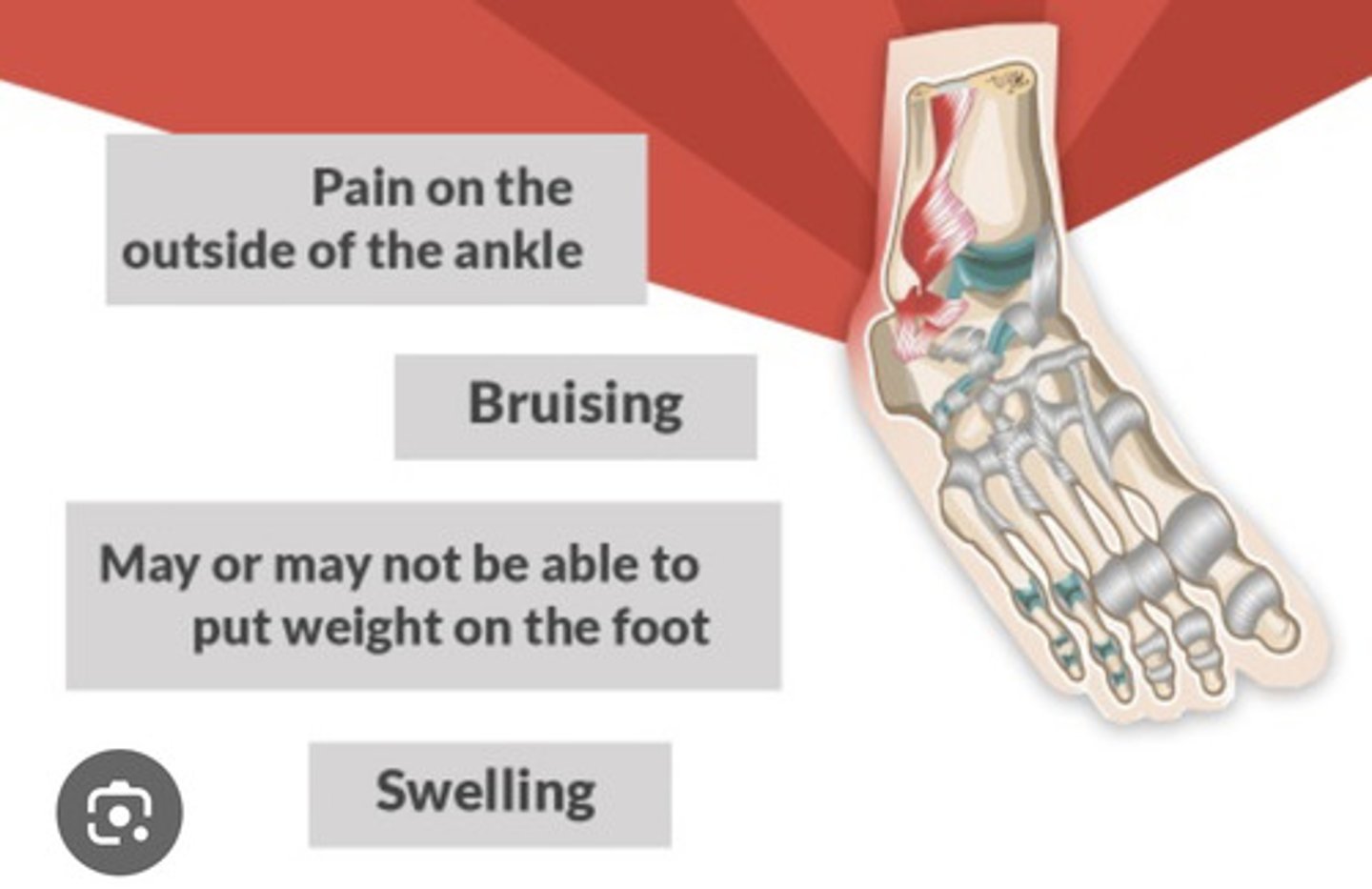
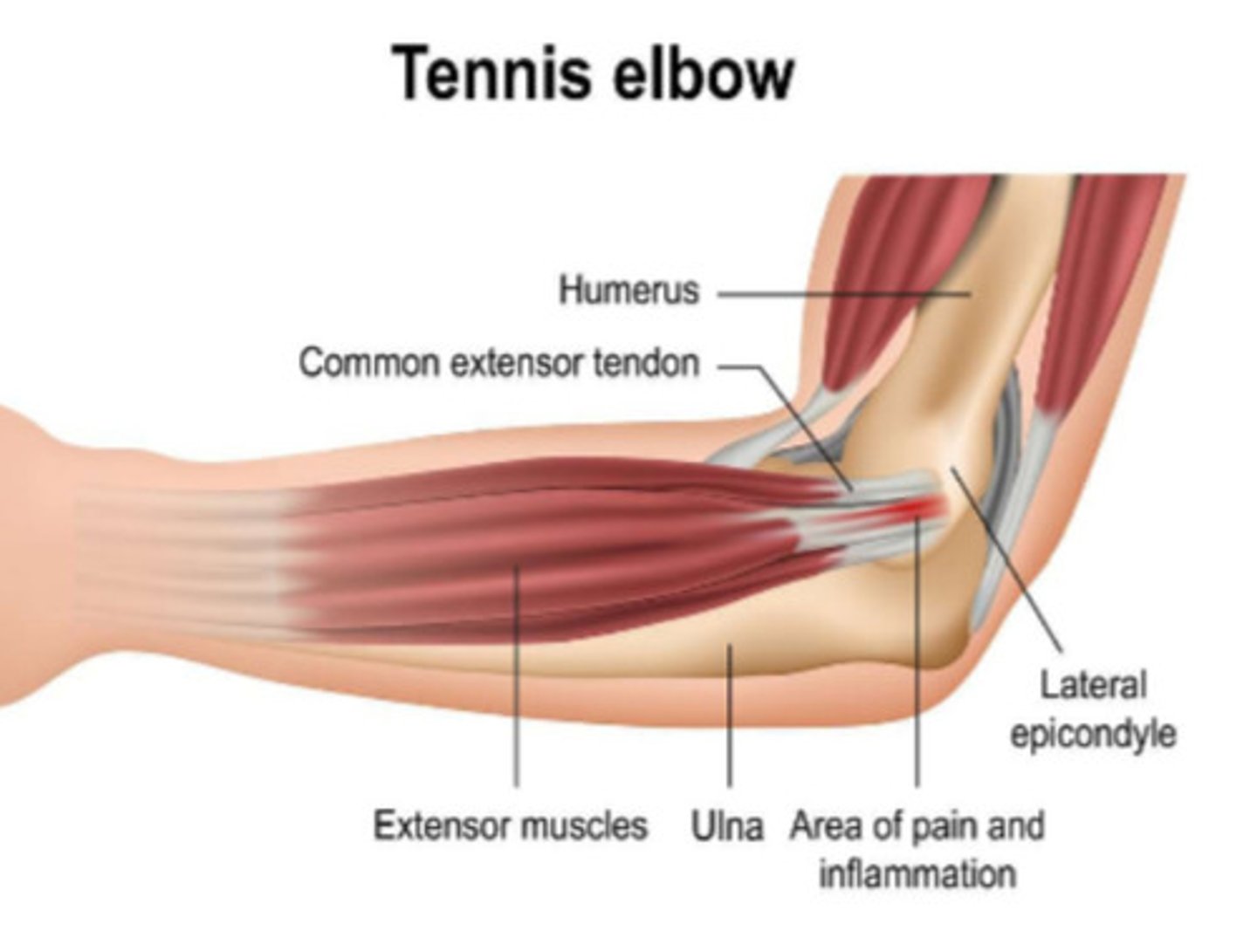
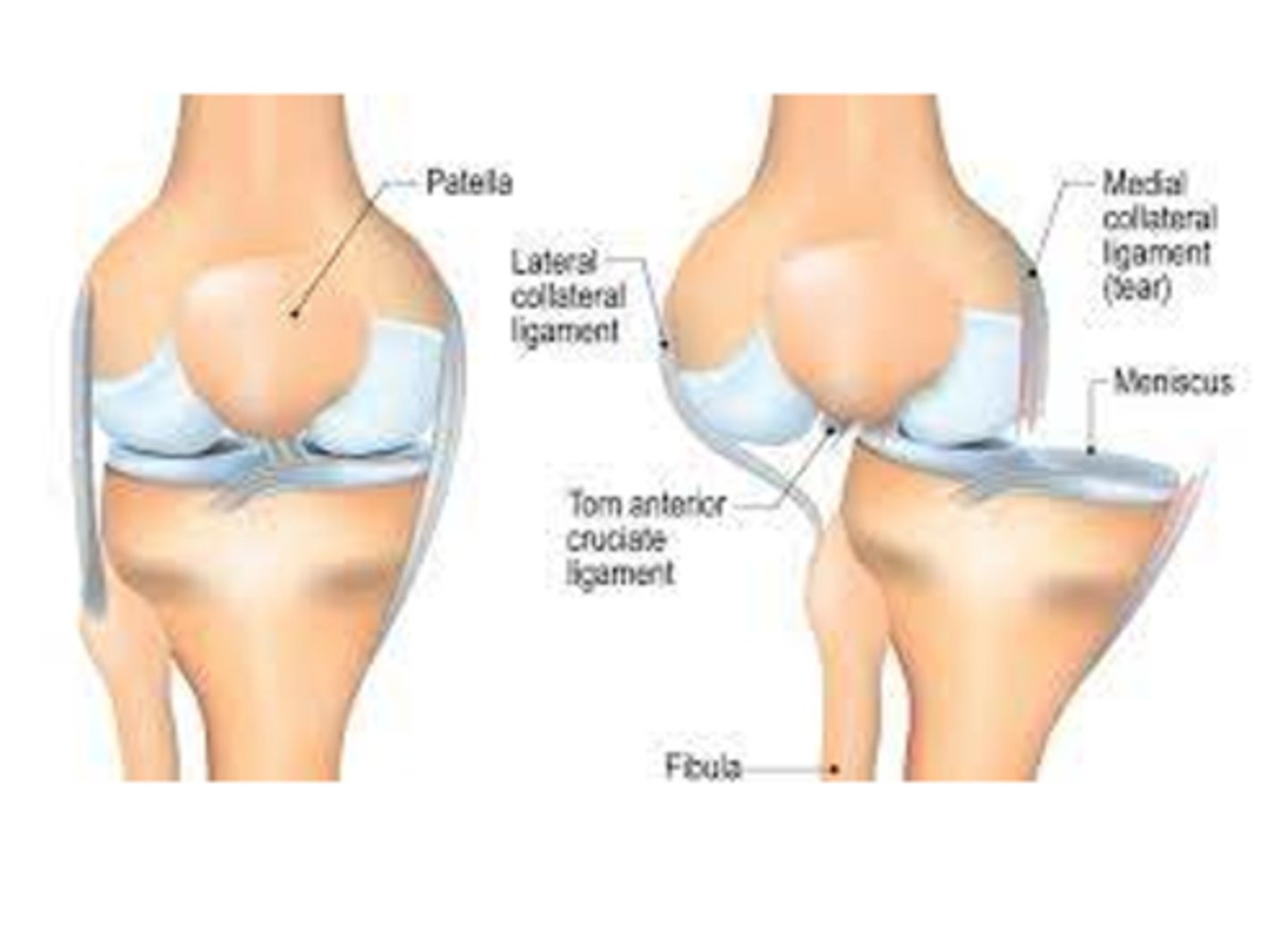
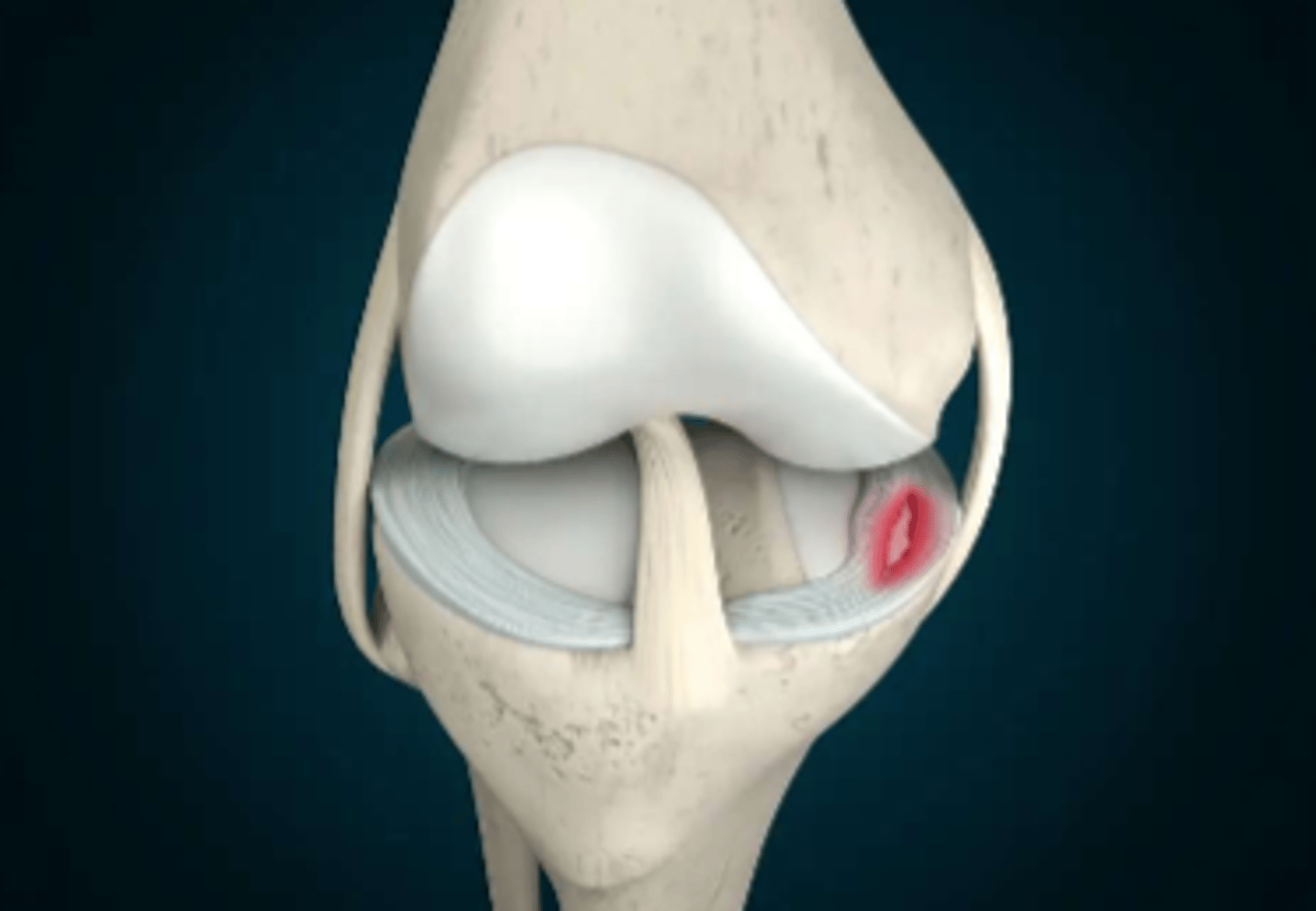
What is a SPRAIN
- mechanical overload of a joint
=> ligament injury = stretch, tear (complete or incomplete), assess for associated bone injury
- common sprains: ankle (inversion); knee (ACL & MCL); elbow; wrist or ligament tear (eg. ACL tear - more dysfunctional)
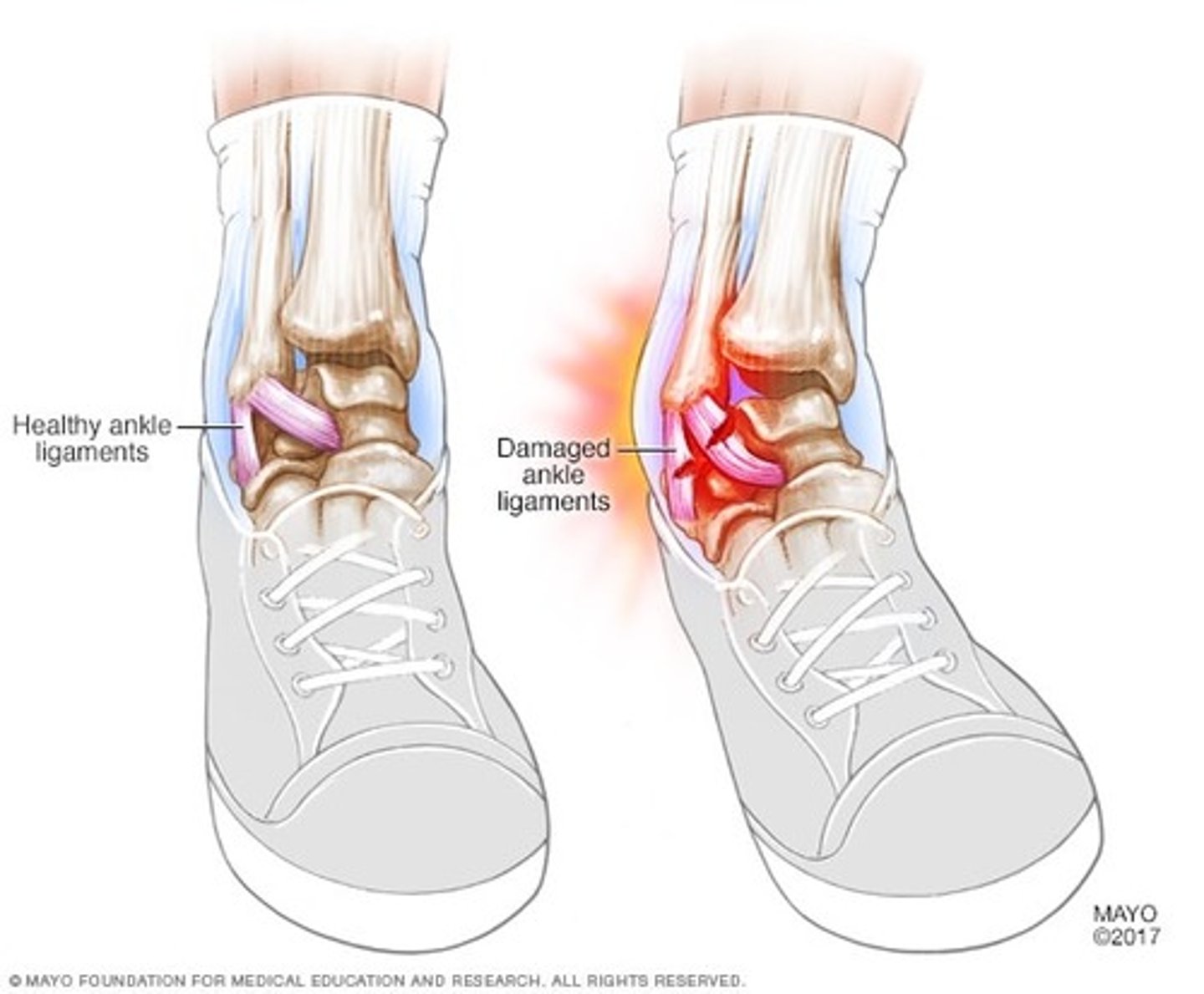
What are the s&s in a sprain
- pain, inflammation
- contusion (bruise)
- decreased function
What is a STRAIN and its etiology
- mechanical overload of a muscle or muscle-tendon complex
- etiology: high risk sports, excessive stretching or contraction => tearing of fascia, muscle, joint structures
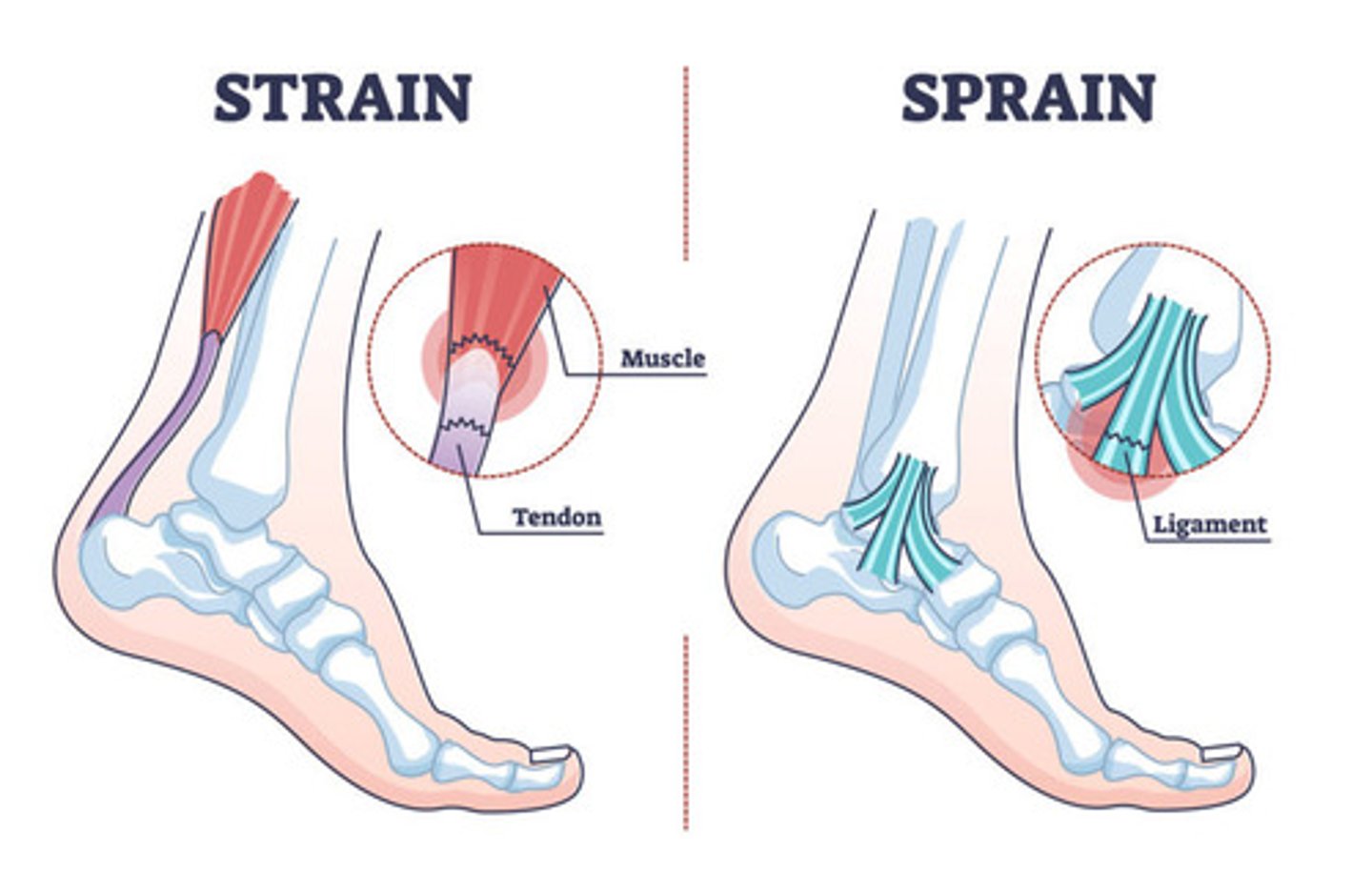
What are the most common types of strains
- muscles: lower back or c-spine
- joints: elbow or shoulder
- tendon tear: achilles tendon, bicep tendon (tendon inflammation is usually chronic in nature)
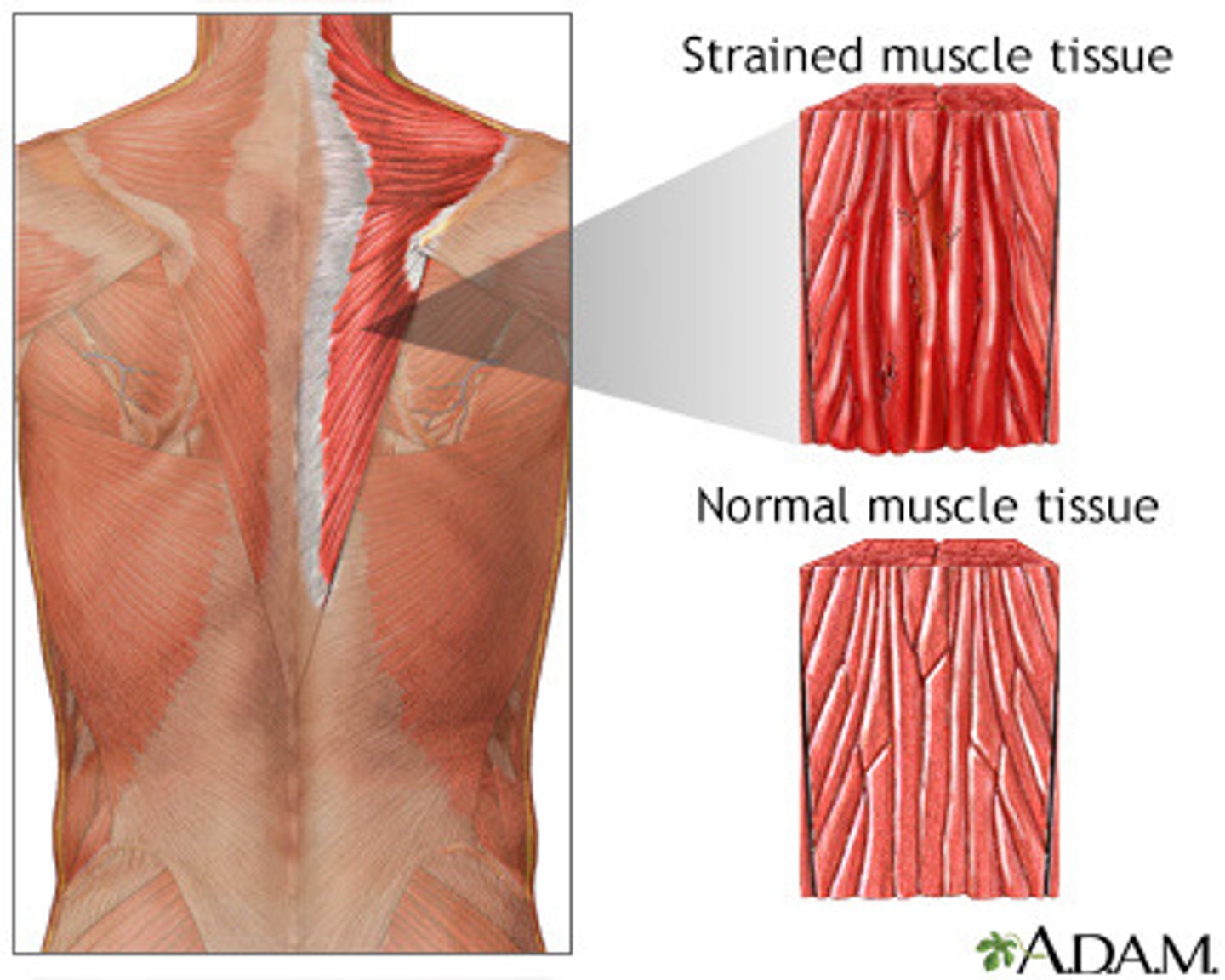
What are the s&s of a strain
- inflammation
- pain, increased pain with aggravating activity
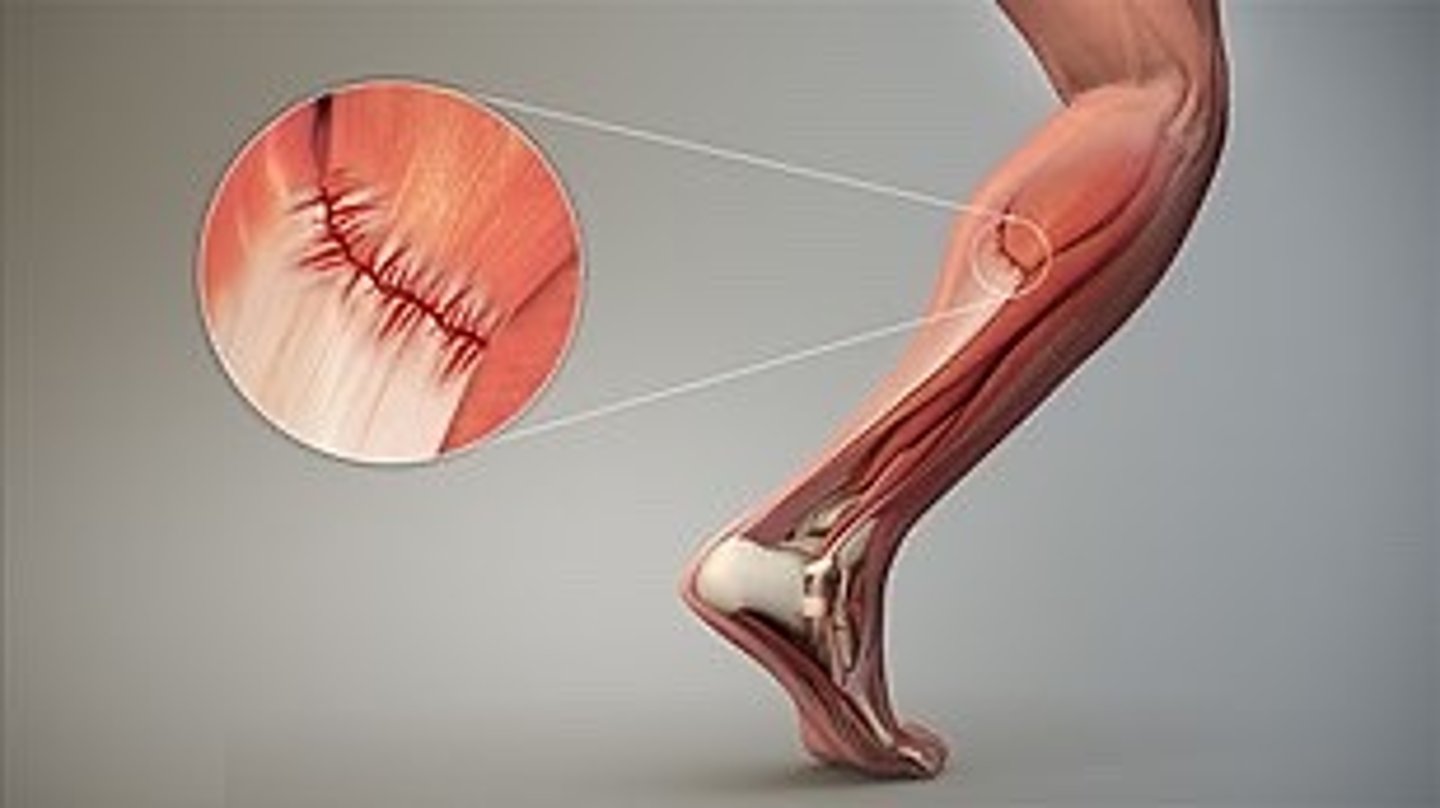
How do we assess for a strain
- assess: area of injury, risk of bigger injury
- Xray not useful only rules out #
How do we treat a sprain or strain at home
dependant on degree of injury
- compresses: cold (ice x 15-20 min, allow for skin temp return to normal, ice again)
- compression of affected area - decrease inflammation; support
*note: immobilization (eg. splint, cast) if support or further damage prevention required

How do we treat a sprain or strain via activity levels
dependent on degree of injury
- rest (weeks)
- rehabilitation - return to function & strength exercises
- surgery
- prevention: posture, exercise mechanics, warm-up & cool-down, limit overuse

Why don't we ice a sprain or strain after 48 hours
ice doesn't usually work after this time period as we no longer have the superficial inflammation anymore and want to optimize perfusion

What drugs would give to treat a sprain or strain
NSAIDS; muscle relaxants (CNS depressant)

What are the different types of muscle relaxant drugs
- Robax (methocarbamol)
- Robaxacet (methocarbamol & acetaminophen)
- Robaxisal (methocarbamol & ASA)

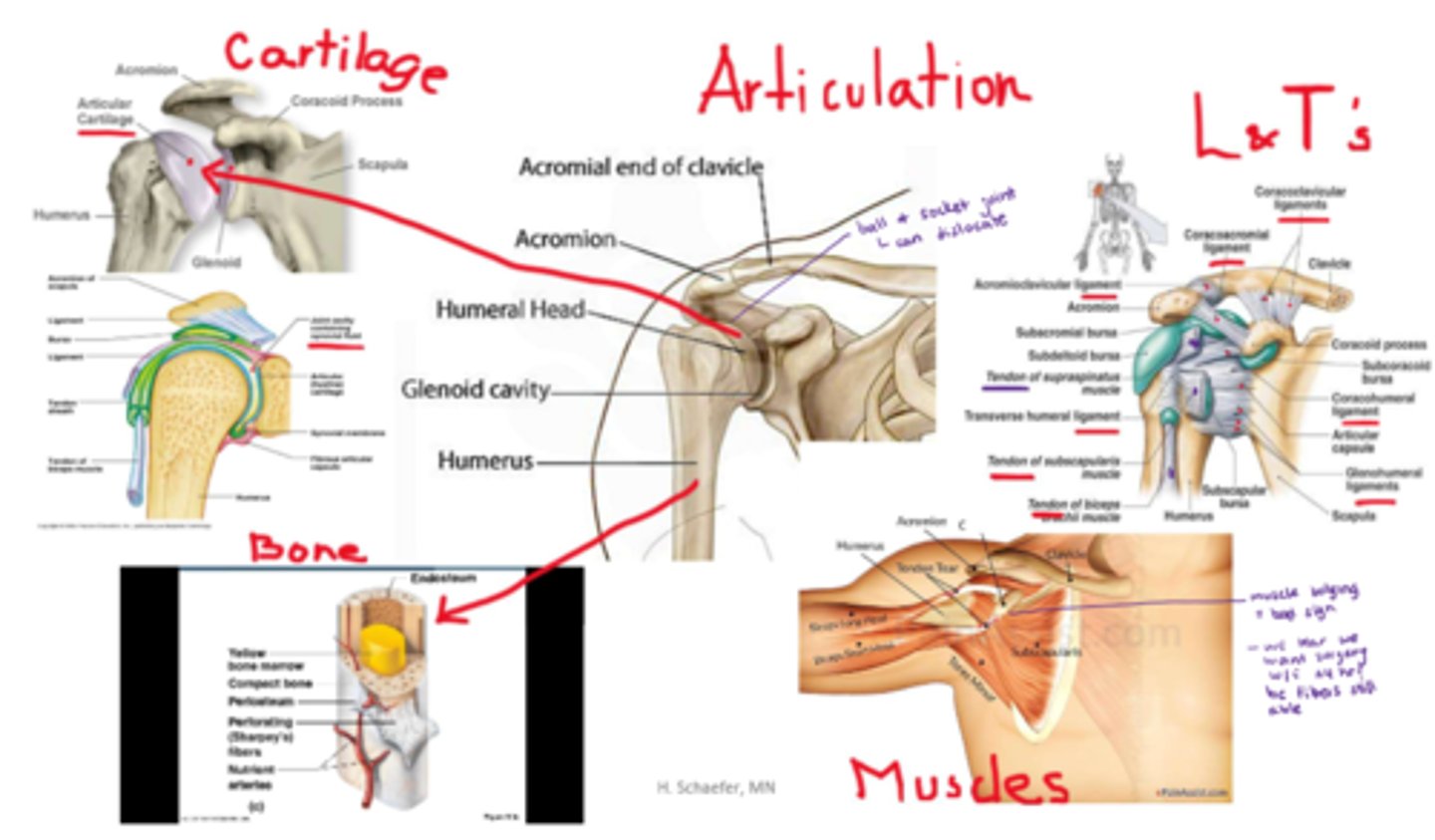
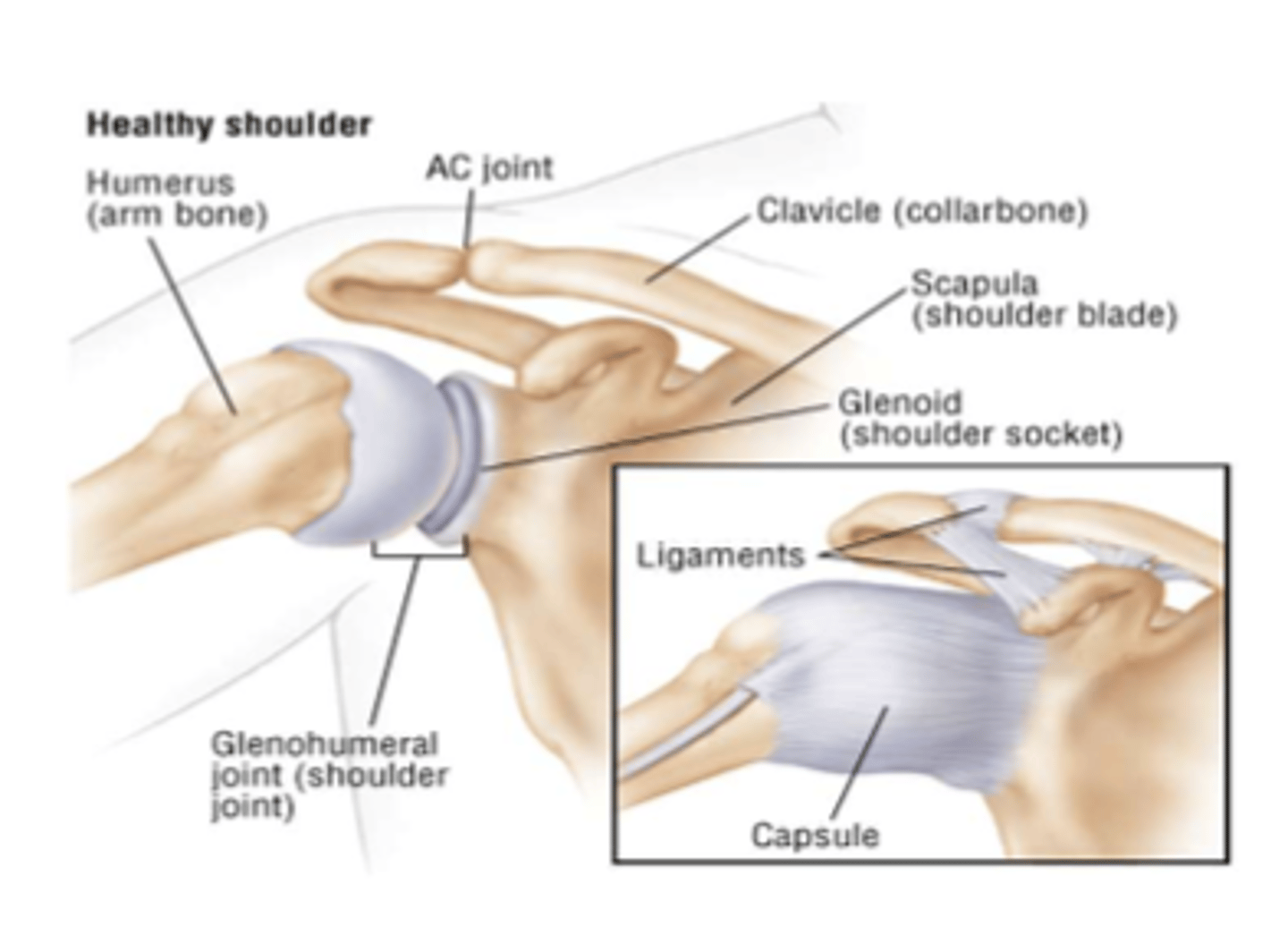
What is a dislocation
- complete joint displacement
- repeat dislocations: likely & easier
- complications: nerve/ blood vessel injury
What usually causes a dislocation
- direct force (traumatic)
- congenital (eg. hip dislocation at birth)
- pathologic (d/t joint disease eg. arthritis)
What is meant by subluxation
incomplete/partial dislocation
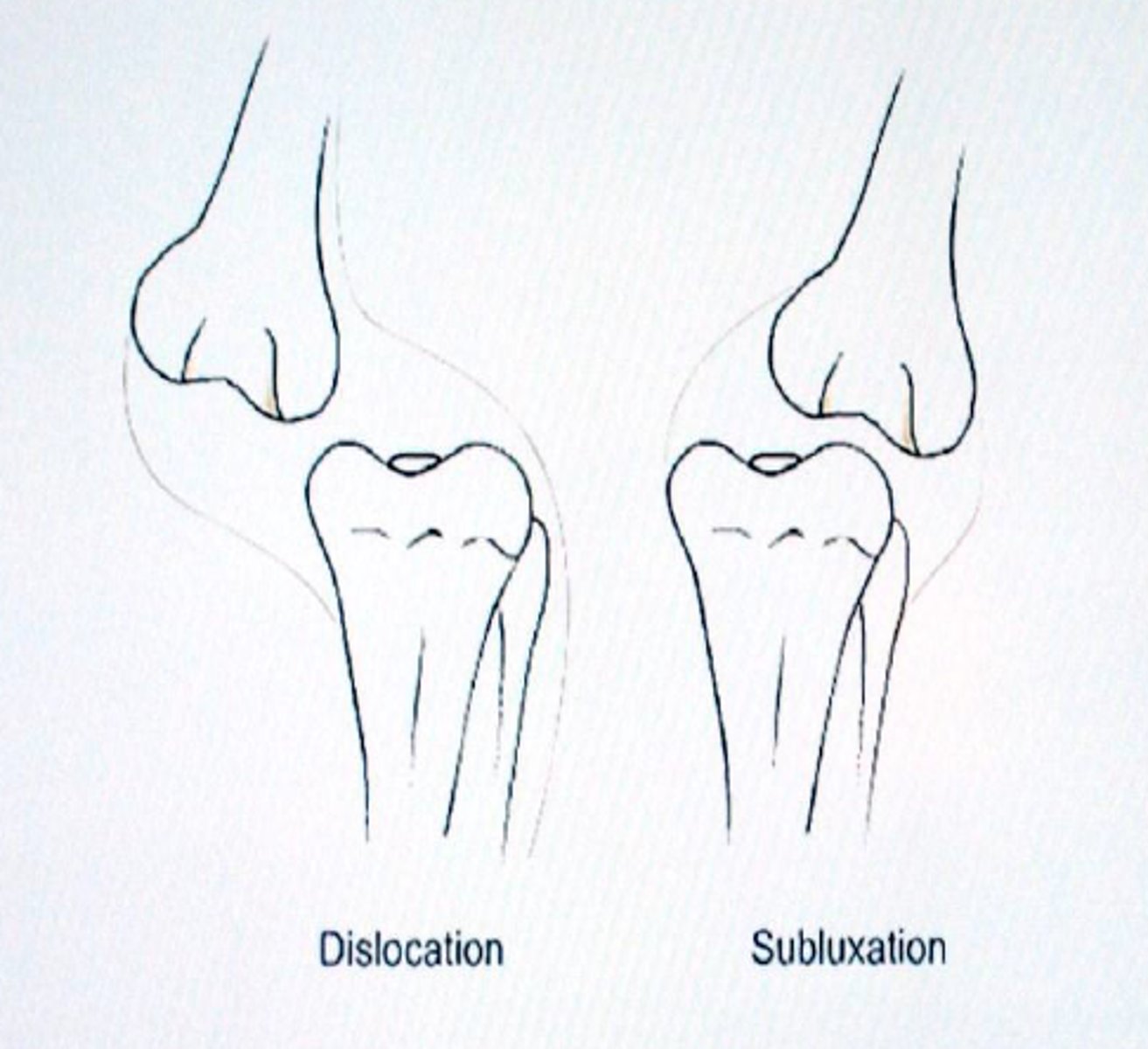
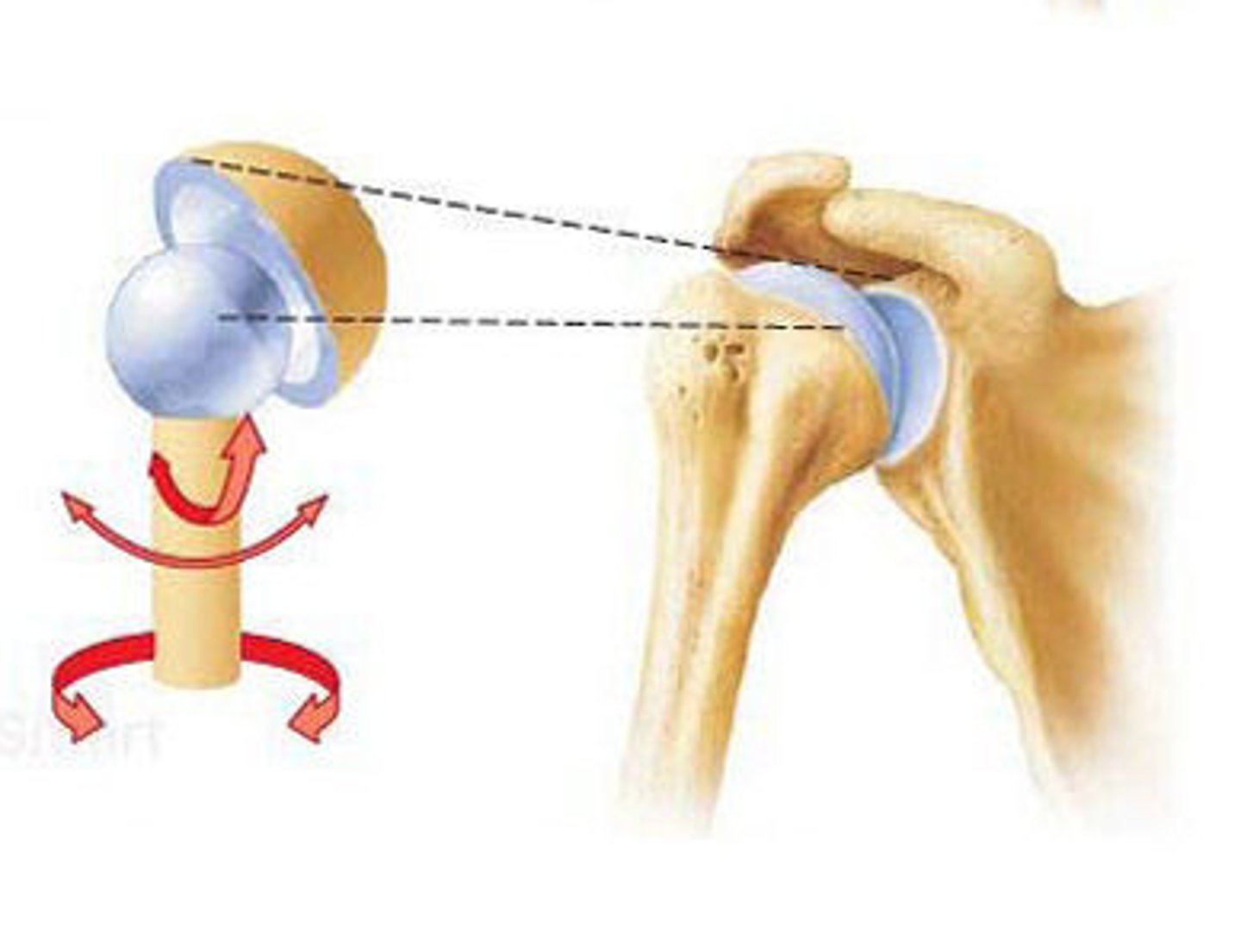
What are the most common dislocations
- ball & socket joints (high mobility)
- eg. shoulder (glenohumeral joint)
How do we tx dislocations
- immobilize with a sling or splint
- manual closed reduction maneuvers
- analgesia

How well do bones heal
excellent blood & nerve supply so they heal well
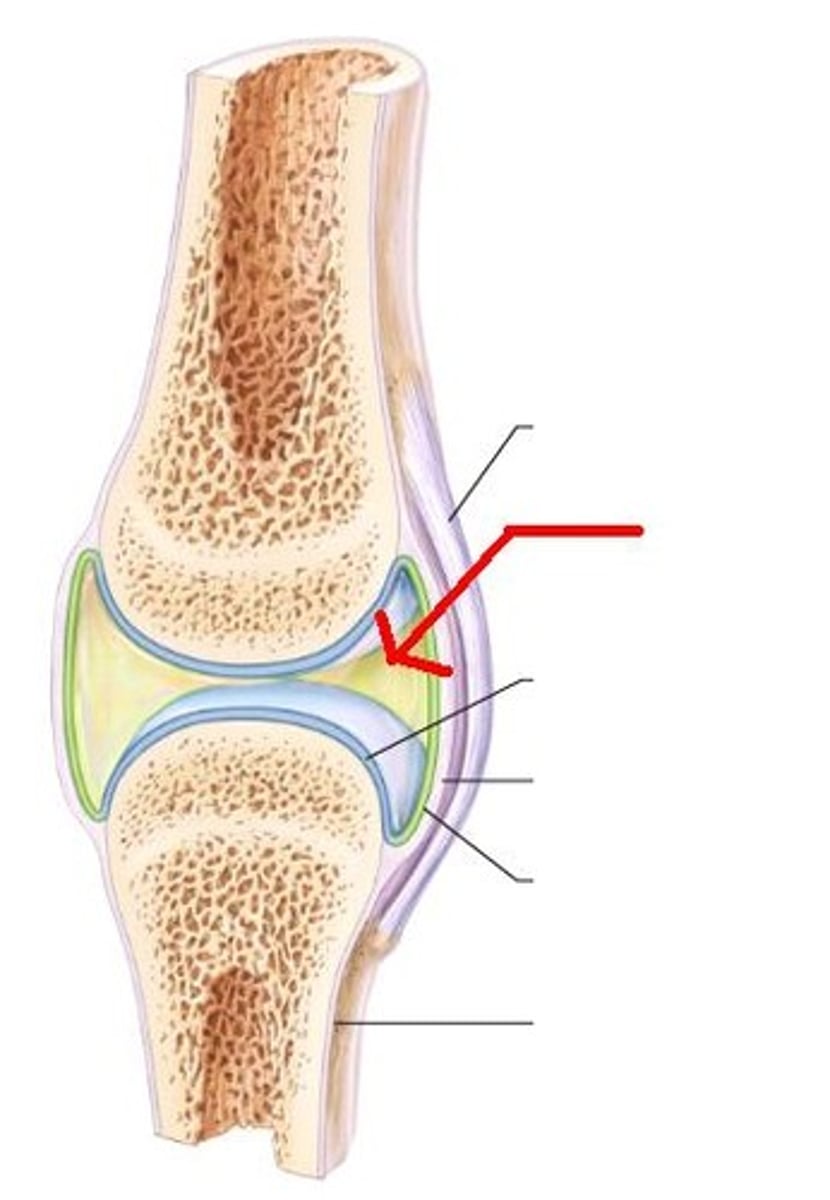
How well do synovial joints heal
- synovial joint: contains blood & nerve supply
- synovial membrane frequently injured - heals well
- synovial joint contains synovial fluid 'sacs' called bursae that cushion the joint (inflammation = 'bursitis')
How does a meniscus (pads of knee joint) tear heal
fibrocartilage, slow healing
How do tendons & ligaments heal
- collagen (fibrous protein) structures
- slow healing, relies on diffusion from surrounding tissue
What is a laceration vs a puncture wound
- both 'integumentary tearing'
- laceration: tear or cut in the skin, often with irregular edges
- puncture wound: much deeper usually with a small opening, caused by a sharp, pointed object
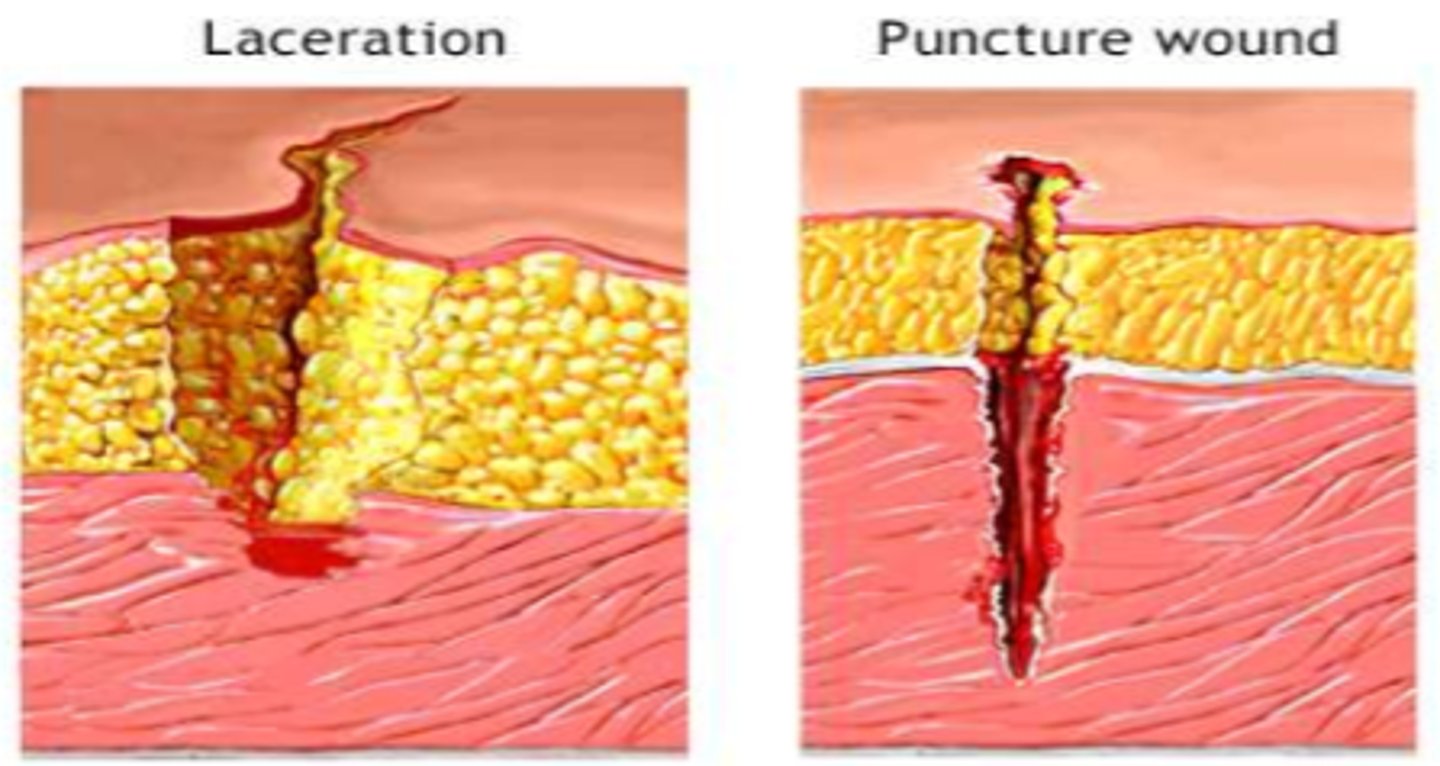
What are our concerns with integumentary tearing
- infection
- soft tissue trauma
- nerve trauma
- bleeding & blood loss (eg. medications increasing clotting time)

What do we assess in a laceration
- size, depth
- deformity
- contusion

How do we tx a laceration
- asepsis, cleansing of wound
- irrigation, decontamination as necessary, debridement
- antimicrobials: abx wash
- prevention: vaccination (tetanus - opportunistic bacteria)
- closure (sutures, staples)

What drugs could we give during wound tx
- local anesthesia
- epinephrine adjunct (vasoconstricts)
- analgesia post (once numbing subsides)

What is a contusion
- aka bruise
- soft tissue injury, skin is intact
- caused by hemorrhaging under the skin
- accompanying issues: pain, inflammation, compartment syndrome

What is the difference between a local & large hemorrhage
- local hemorrhage: 'bruising' (ecchymosis (bleeding under the skin) => reabsorbed)
- large hemorrhage = hematoma
How to tx a contusion
- cold compresses (to decrease bruise from starting/expanding)
- NSAIDs
- needle aspiration
