Heart Failure and PE
1/29
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
30 Terms
What is heart failure?
means the heart can’t pump enough blood to meet the body’s needs. Blood backs up, Organs don’t get enough oxygen. and Fluid builds up in lungs or body
Inadequate cardiac output
Inadequate tissue perfusion
increased diastolic filling pressure → increased in pulmonary capillary filling
It’s not that the heart stops — it’s that it works too hard and too poorly.
Why does heart failure happen? Common cause
Long-standing high blood pressure
Coronary artery disease (CAD)
Heart attack (MI)
Valve problems (mitral/aortic)
Cardiomyopathy
Pulmonary hypertension
Pericarditis
Think: anything that increases workload or damages the heart muscle.
How it work and result too much work load? What is cardiac output?
The heart struggles with:
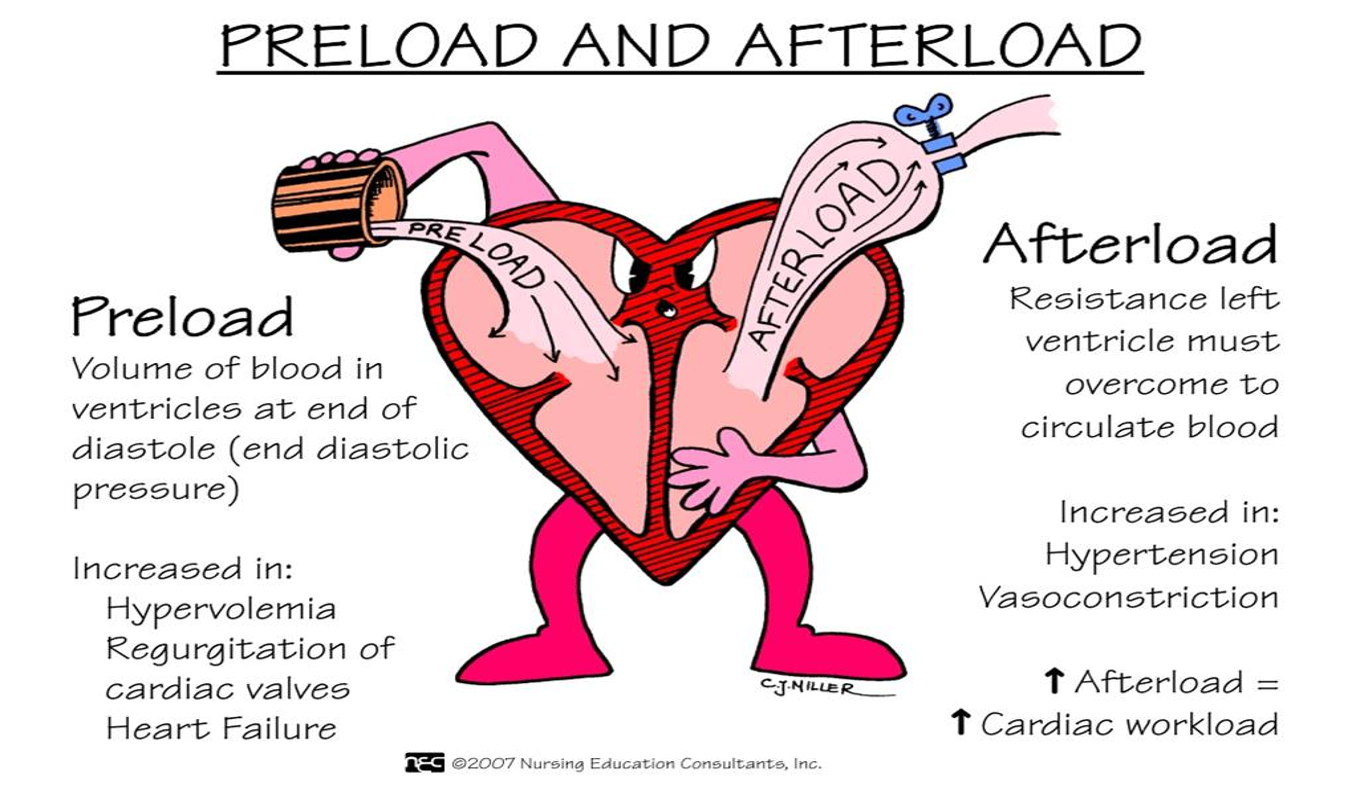
Preload → how much blood fills the heart
Afterload → how hard the heart has to pump against pressure
In HF:
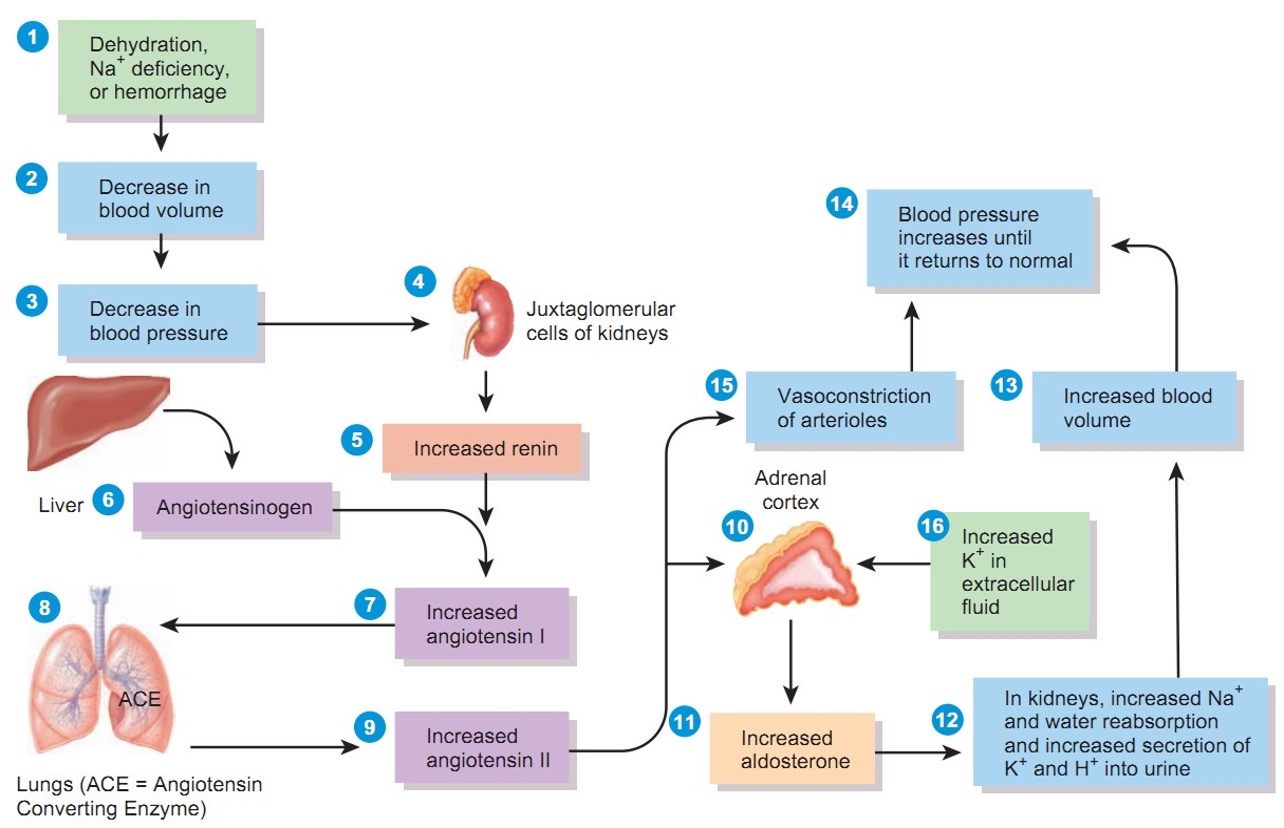
Kidneys think blood flow is low
They retain sodium & water
This increases preload
More fluid = more stress on the heart
Cardiac output- the volume of blood pumped from each ventricle per minute
increased preload and afterload can result to?
What is baroreceptor?
This is the body’s EARLY response when cardiac output drops (like in Heart Failure).
The body is trying to save blood pressure and perfusion.
Signals are sent to the CNS → SNS increases heart activity → SNS causes vasoconstriction → SNS increases preload → Kidneys release renin
What happens in the body?
Heart pumps poorly → ↓ cardiac output
Body panics
Activates:
Sympathetic Nervous System (SNS) release epinephrine and norepinephrine→ ↑ HR, vasoconstriction, contractility, and conduction ← B1 receptor stimulated
RAAS system → In kidney; retain sodium & water
Short-term help (B1 help the heart to pump more) → long-term harm
Fluid overload + worsening HF
What induces excretion of sodium by the kidney?
Natriuretic Peptide
Atrial natriuretic (ANP)
–Increases sodium excretion – secreted by muscle cells in the atria.
Brain natriuretic peptide (BNP)*
–Hormone secreted by the cardiomyocytes in the ventricles in response to an increase ventricular blood volume.
Key indicator to diagnosis of HF?
Brain natriuretic peptide (BNP)*
> 100 = HF
Heart failure is a chronic (long-term) process where the heart is stuck in a loop it can’t escape. What are those?
1⃣ Afterload on the Left Ventricle increases
Afterload = how hard the LV must push to eject blood.
In HF:
Blood vessels are constricted
Blood pressure is higher
The LV must work harder to pump forward
🧠 Think: pumping against a tight hose
2⃣ Cardiac workload increases
Because afterload is high:
LV uses more energy
LV needs more oxygen
Muscle gets tired and stiff
The heart is overworking every beat.
3⃣ Stroke volume decreases
Stroke volume = blood pumped per beat
Because the LV is weak or stiff:
Less blood leaves the heart
More blood stays behind
Ejection fraction drops
This is the failure part of heart failure.
Why this becomes a vicious cycle
↓ Stroke volume → ↓ cardiac output
Body senses poor perfusion
SNS + RAAS activate
↑ Vasoconstriction → ↑ afterload
↑ Fluid retention → ↑ preload
Heart stretches and weakens
➡ And the cycle continues.
LV ejection fraction of HF patient
The percentage of blood pumped out of the LV with each beat.
35% or less
Reduced EF which causes an increase in residual end-systolic volume
*The more a myocardial fiber is stretched during filling, the more it shortens during systole and the greater the force of the contraction
Left and right HF Overview
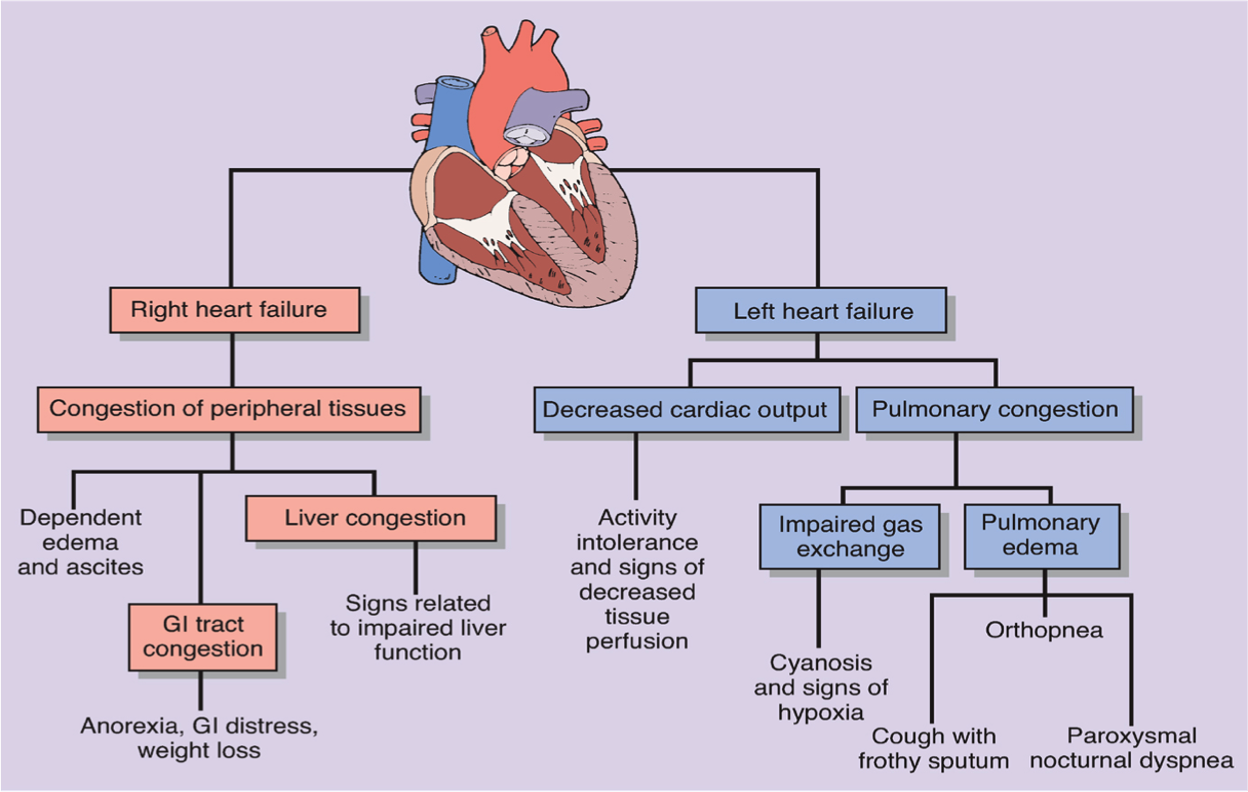
What is left HF?
Heart does not “pump” effectively
Accumulates in the pulmonary (backward)
Hydrostatic pressure builds
Fluid is forced from the capillaries into the interstitial and alveolar spaces causing edema.
Sign and Symptoms of left HF
Left HF: Lungs- blood backs up
•Mnemonic: "DO CHaP"
•D → Dyspnea
•O → Orthopnea
•C → Cough/Crackles
•H → Hemoptysis (frothy sputum)
•a → Adventitious lung sounds (Crackles)
•P → Pulmonary congestion
Paroxysmal nocturnal dyspnea- severe shortness of breath that wakes individuals from sleep
What is right HF?
Pulmonary disorders increase pulmonary vascular resistance, raising afterload on the right ventricle and leading to right ventricular hypertrophy and failure (cor pulmonale).
What happens to the BODY when right-sided heart failure backs blood up into the systemic circulation?
Liver -- Hepatocytes atrophy and necrosis because of high pressure.
Portal system will have an increase in hydrostatic pressure = Ascites.
Enlarged spleen and GI tract
Kidneys and decreased glomerular filtration
Fluid retention – aldosterone not metabolized
Superior Vena Cava cannot drain
Management of Heart Failure
Nutrition Management
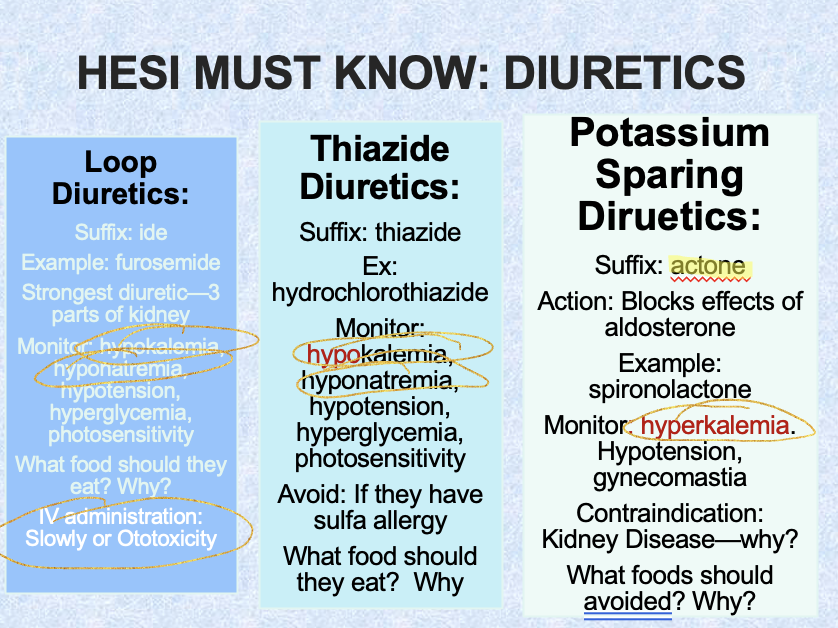
Thiazide Diuretic (if not acute for older adults to prevent dehydration)
CPAP in patients with sleep apnea
Ventricular assist devices
Pacer – biventricular pacing
Medication Management of left and right HF
Left HF
CE inhibitors / ARBs / ARNIs (CORE meds)
Beta blockers
Diuretics
Aldosterone antagonists
Digoxin (selected patients)
Right HF
Diuretics (MOST IMPORTANT for RHF)
Treat pulmonary cause
ACE inhibitors & beta blockers
What is ACE inhibitor? (action, Contraindication, and s/e)
Suffix: pril
–Examples (Captopril, Lisinopril, Enalapril, Ramipril)
ACTION: Suppress the RAAS system and prevent activity of ACE
–This causes Na and H2O to not be retained so sodium and BP will decrease; also dilates blood vessels
Contraindications
–Renal failure—can worsen renal failure—what should you monitor
S/E: and AE
–Angioedema-
–Cough—annoying but normal
–Elevated K+
Key teaching for ACE
–Avoid potassium containing foods/meds
•Don’t forget to teach about salt substitutes usually containing high potassium levels
–Monitor weight and assess for s/s of heart failure
–First Dose hypotension effect—change positions slowly, ask for assistance
What is ARBS?
Suffix: sartan
•Examples: Valsartan, Losartan
Similar to ACE inhibitors in use, patient education and nursing considerations but some key differences:
Action: Inhibits angiotensin II verses Ace inhibitors which inhibit ACE conversion of Angiotensin I to Angiotensin II
Produce fewer side effects
Does not have cough SE
Less risk for angioedema
ACE inhibitors do not impact HR but ARBs decrease HR
What is Digoxin? (Action, s/e, what to monitor?)
•Allows heart muscles to contract more efficiently
Side effects include bradycardia, visual disturbances (diplopia, halo around lights, blurred vision, yellow vision, photophobia)
•Monitor serum digoxin levels
Therapeutic range 0.5 -2.0 ng/dL
•Monitor apical pulse for 1 minute
•If <60 bpm, withhold med and notify physician
Digoxin toxicity (s/s, toxic level, monitor, antidote)
S/S
–Early: Gi manifestations (anorexia, nausea, vomiting, diarrhea) then heart rate abnormalities, visual disturbances
Toxic Level:
–Greater than 2.0
Risk Factors for Toxicity
–Hypokalemia—
Monitor levels
•Pt’s taking loop and thiazide diuretics
•Teach pts to eat foods high in potassium
Antidote
–Digibind
HESI MUST KNOW: DIURETICS
Key teaching management of HF
Daily weights (MOST IMPORTANT teaching)
How is it done?
Tell the patient to:
Weigh every morning
After urinating
Before eating or drinking
Same scale
Same clothes (or no clothes)
Same time every day
Consistency is EVERYTHING.
When should the patient notify the HCP?
Call the provider if:
Gain of 2–3 lb in 1 day
OR 5 lb in 1 week
This usually means fluid retention, not fat gain.
How do you confirm a patient’s report of weight gain?
If the patient says,
“I gained 6 pounds in 3 days”
You confirm by:
Reviewing documented daily weights
Comparing today’s weight to baseline
Assessing for:
Edema
JVD
Crackles
Shortness of breath
Objective daily weights > patient feelings
Diet: Heart-Healthy / DASH DietMain goals:
↓ Sodium
↓ Fluid retention
↓ Blood pressure
↓ Cardiac workload
Limit sodium to ~2 g/day
Avoid salt substitutes if on ACE inhibitors or aldosterone antagonists (high potassium!).
Discharge to Home in Heart Failure
Indications of poor perfusion
Examples from your slide:
Fatigue
Angina (chest pain)
Activity intolerance
What does this mean?
Poor perfusion = organs aren’t getting enough oxygenated blood.
This tells the nurse:
Cardiac output is still limited
Patient may not tolerate normal activity
Risk for falls, injury, worsening HF
Nursing implications (assessment & interventions)
You should:
Assess vital signs with activity
Monitor for:
SOB
Dizziness
Chest pain
Excessive fatigue
Adjust activity level
Teach energy conservation
Coordinate home support if needed
NCLEX clue: Fatigue = ↓ cardiac output
Assess ability to perform ADLs
ADLs = bathing, dressing, toileting, cooking, walking.
What are you looking for?
Ask:
“Can you shower without stopping?”
“Do you get short of breath getting dressed?”
“Can you walk to the bathroom safely?”
If patient cannot perform ADLs independently:
They may need:
Home health nursing
Physical therapy
Assistive devices
Family support
Safety + independence = discharge readiness
Energy conservation strategies (VERY TESTABLE ⭐)
Teach the patient to:
Plan & pace
Schedule activities with rest periods
Do hardest tasks in the morning
Sit instead of stand when possible
Reduce energy use
Keep frequently used items within reach
Avoid unnecessary trips up/down stairs
Use shower chair, raised toilet seat if needed
Control breathing
Stop activity if SOB
Use pursed-lip breathing
Avoid rushing
Memory trick: “Do less, rest more, breathe better”
Assess nutritionWhat are you looking for?
Excess sodium intake
Poor appetite or early satiety
Unintentional weight gain or loss
Understanding of DASH / low-sodium diet
Ask:
“What did you eat yesterday?”
“Do you read food labels?”
“Who prepares your meals?”
Red flags 🚩:
Processed foods
Fast food reliance
No understanding of sodium limits
Assess home environment
You’re looking for:
Stairs (can patient manage them?)
Bathroom safety
Access to scale for daily weights
Transportation to appointments
Ability to obtain medications
Unsafe home = ↑ risk of:
Falls
Non-adherence
Readmission
Assess understanding of disease
Ask teach-back questions:
“What symptoms should make you call your provider?”
“Why do you weigh yourself daily?”
“What foods should you avoid?”
You want to see:
Understanding of:
Daily weights
Medication purpose
Diet
Symptom reporting
If they can’t explain it → teaching isn’t done.
What is pulmonary edema?
Pulmonary edema happens when fluid leaks into the lungs (alveoli) instead of staying in blood vessels.
➡ Oxygen can’t move well
➡ Gas exchange fails
➡ The patient feels like they’re drowning in air
What causes PE?
Fluid overload
Too much fluid in circulation
Often from heart failure, renal retention, or excess IV fluids
The heart can’t handle the volume → blood backs up into lungs.
Acute MI
Sudden loss of left ventricular pumping ability
Blood backs up into pulmonary circulation
Pressure forces fluid into alveoli
Heart suddenly fails → lungs pay the price
Mitral valve disease
Blood leaks backward from LV → LA → lungs
Pulmonary pressure rises
Fluid shifts into lung tissue
What nurses must assess EARLY for PE?
Key early assessment findings:
Crackles (especially bases)
Dyspnea at rest
Disorientation or confusion
Restlessness
Anxiety
Confusion = low oxygen to the brain (late sign!)
If PE is left untreated what’s gonna happen?
Severe hypoxia
Pink, frothy sputum
Respiratory failure
Cardiac arrest
This is why crackles + SOB at rest = act NOW
Nursing priority for PE
Airway and breathing FIRST
Sit patient upright
Apply oxygen
Call provider / rapid response