MCAT Biology - The Musculoskeletal System
1/117
Earn XP
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
118 Terms
rhabdomyolysis
Extreme physical trauma to muscles, namely, compression, destroys skeletal muscle tissue; products of skeletal muscle destruction, some of which are toxic, circulate in the blood until they are filtered out
(rhabdo– “striation”, myo– “muscle”, –lysis “breakdown”)
Skeletal muscle
essential for supporting the body and facilitating movement; responsible for voluntary movement and innervated by the somatic nervous system; striated; multinucleated, formed as individual muscle cells fuse into long rods during development
striated
striped
Red fibers / slow-twitch fibers
occur predominantly in muscles of support; high myoglobin content and primarily derive their energy aerobically; contain many mitochondria to carry out oxidative phosphorylation
Myoglobin
oxygen carrier that uses iron in a heme group to bind oxygen, imparting a red color; secondary supplemental energy reserve in muscle
White fibers / fast-twitch fibers
predominantly in muscles for short bursts of motion; contain less myoglobin;
Smooth muscle
responsible for involuntary action, controlled by the autonomic nervous system; respiratory tree, digestive tract, bladder, uterus, blood vessel walls, etc.; single nucleus located in the center of the cell; actin and myosin, but not as well organized; capable of more sustained contractions
tonus
constant state of low-level contraction, as may be seen in the blood vessels
myogenic activity
respond to nervous input, but do not require external signals to undergo contraction; exhibited in smooth and cardiac muscle
Cardiac muscle
involuntary and innervated by the autonomic nervous system; appears striated; primarily uninucleated, but cells may contain two nuclei
intercalated discs
microscopic identifying features of cardiac muscle; major portal for cardiac cell-to-cell communication via gap junctions for rapid and coordinated depolarization of muscle cells and efficient contraction of cardiac muscle
gap junctions
connections between the cytoplasm of adjacent cells, allowing for the flow of ions directly between cells
sinoatrial (SA) node
where depolarisation begins
atrioventricular (AV) node
depolarization spreads using conduction pathways here from the SA node
bundle of His
transmits the electrical impulses from the atrioventricular node to the point of the apex of the fascicular branches
Purkinje fibers
allow the heart's conduction system to create synchronized contractions of its ventricles
vagus nerve
parasympathetic outflow to the heart and slows the heart rate
Norepinephrine / epinephrine
binds to adrenergic receptors in the heart, causing an increased heart rate and greater contractility; increasing intracellular calcium levels within cardiac myocytes
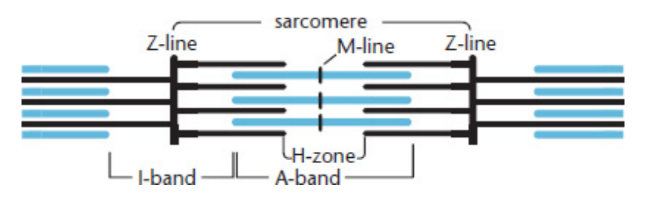
sarcomeres
basic contractile unit of skeletal muscle; thick and thin filaments
thick filaments
organized bundles of myosin
myosin
motor proteins best known for their roles in muscle contraction and in a wide range of other motility processes in eukaryotes; ATP-dependent and responsible for actin-based motility
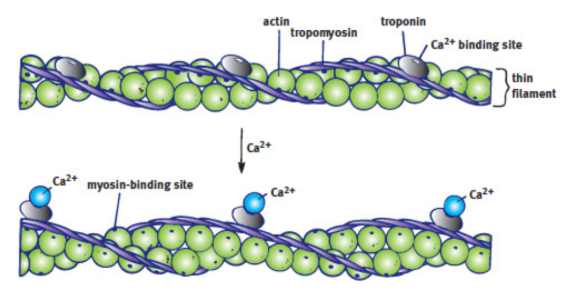
thin filaments
made of actin, troponin and tropoamyosin
actin
globular multi-functional proteins that form microfilaments in the cytoskeleton, and the thin filaments in muscle fibrils
troponin
complex of three regulatory proteins that are integral to muscle contraction in skeletal muscle and cardiac muscle
tropomyosin
works in conjunction with troponin to regulate muscle contraction; present in smooth and striated muscle tissues
titin
acts as a spring and anchors the actin and myosin filaments together, preventing excessive stretching of the muscle
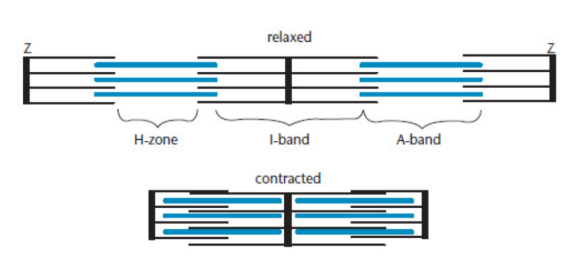
Z-lines
define the boundaries of each sarcomere (end of alphabet/sarcomere); distance between shrinks during contraction
M-line
runs down the center of the sarcomere, through the middle of the myosin filaments; distance between shrinks during contraction
I-band
the region containing exclusively thin filaments; shrinks during contraction
H-zone
region containing only thick filaments; shrinks during contraction
A-band
contains the thick filaments in their entirety, including any overlap with thin filaments; size remains constant during contraction
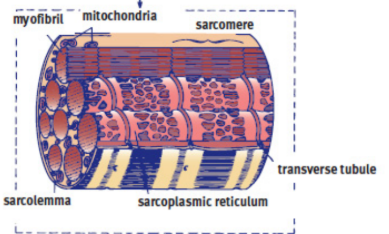
myofibrils
rod-like organelle of a muscle cell; arrangement of many sarcomeres in series; arranged in parallel in myocyte
sarcoplasmic reticulum (SR)
covering of myofibrils; modified endoplasmic reticulum that contains a high concentration of Ca²⁺ ions; tightly controls intracellular calcium concentrations so that muscles are contracted only when necessary; releases Ca2+ to contract; resorbs to relax
sarcoplasm
modified cytoplasm of myocytes; located just outside the sarcoplasmic reticulum
sarcolemma
cell membrane of a myocyte; capable of propagating an action potential and can distribute the action potential to all sarcomeres in a muscle using a system of transverse tubules
transverse tubules (T-tubules)
oriented perpendicularly to the myofibrils; distribute the action potential to all sarcomeres in a muscle
myocyte / muscle fiber
muscle cell; multinucleated at the periphery; exhibit an all-or-nothing response
neuromuscular junction,
where the nervous system communicates with muscles via motor (efferent) neurons and contraction begins
nerve terminal / synaptic bouton / motor end plate
end of (motor) neuron; releases acetylcholine into the synapse
motor unit
a nerve terminal and the myocytes it affects
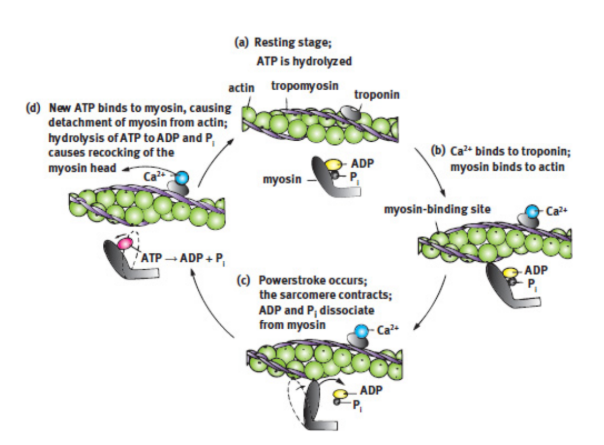
Regulation of Contraction with Calcium
Calcium binds to troponin, leading to a conformational change in tropomyosin, which exposes the myosin-binding sites of actin
Shortening of the Sarcomere / sliding filament model
free globular heads of the myosin molecules move toward and bind with the exposed sites on actin and allow myosin to pull on actin, which draws the thin filaments toward the M-line
The Actin–Myosin Cross-Bridge Cycle
myosin carrying hydrolyzed ATP (ADP and an inorganic phosphate, Pi) is able to bind with the myosin-binding site.
The release of the inorganic phosphate and ADP in rapid succession provides the energy for the powerstroke to slide the actin filament over the myosin filament.
ATP binds to the myosin head, releasing it from actin.
ATP is hydrolyzed to ADP and Pi, which recocks the myosin head so that it is in position to initiate another cross-bridge cycle
acetylcholinesterase
degrades acetylcholine in the synapse, ending the signal at the neuromuscular junction; allows the sarcolemma to repolarize
rigor mortis
after death. myosin heads cannot detach from actin because ATP production ceases, making it impossible for muscles to relax and lengthen
simple twitch
response of a single muscle fiber to a brief stimulus at or above threshold; latent period, contraction period, and relaxation period
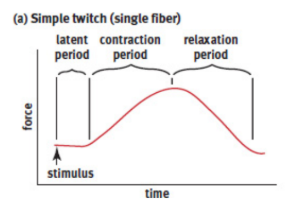
latent period
time between reaching threshold and the onset of contraction; action potential spreads along the muscle and allows for calcium to be released from the sarcoplasmic reticulum
frequency summation
muscle fiber is exposed to frequent and prolonged stimulation with insufficient time to relax; contractions will combine, become stronger and more prolonged
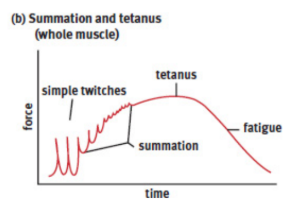
tetanus (symptom)
contractions become so frequent that the muscle is unable to relax at all; will result in muscle fatigue; caused by C. tetani infection but also normal multiple simple twitches
tetanus (disease)
caused by a bacterium called Clostridium tetani that releases the toxin tetanospasmin that blocks the release of GABA from the neurons that inhibit motor neurons, making the motor neurons overexcitable; leads to constant contraction of muscles (tetanus the symptom), which can be so strong as to fracture bones
can usually be prevented after exposure by administration of a tetanus immunoglobulin
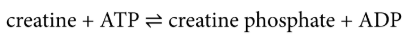
Creatine phosphate
created by transferring a phosphate group from ATP to creatine during times of rest; first supplemental energy reserve in muscle
oxygen debt
difference between the amount of oxygen needed by the muscles and the actual amount present; when even red muscle fibers must switch to anaerobic metabolism and produce lactic acid; after exercise; body must metabolize all of the lactic acid it has produced, using oxygen to convert it to pyruvate
skeleton
the structural frame that supports the body of most animals
Exoskeletons
encase whole organisms in structural frame; protect the soft tissue structures; must be shed and regrown to accommodate growth
ex. arthropods, such as crustaceans and insects
endoskeletons
internal structural frame covered by other structures (muscle, connective tissue, and vasculature); not able to protect the soft tissue structures as well as exoskeletons; much better able to accommodate the growth of a larger organism
ex. Vertebrates, including humans
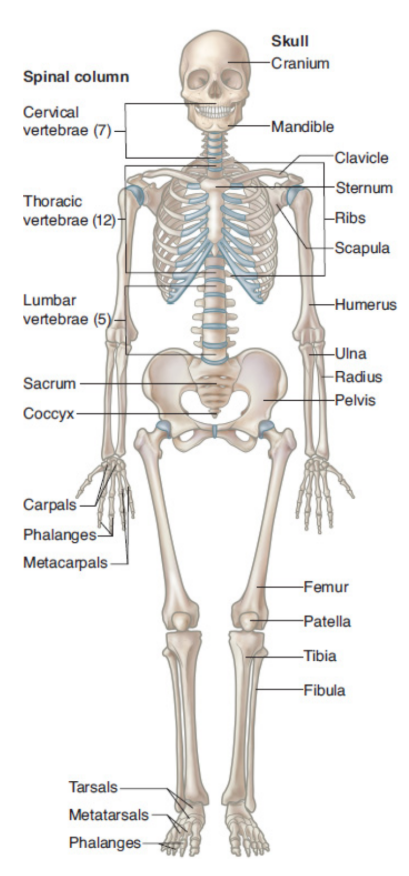
axial skeleton
consists of the skull, vertebral column, rib cage, and hyoid bone; provides the basic central framework for the body
hyoid bone
small bone in the anterior neck used for swallowing
appendicular skeleton
consists of the bones of the limbs, the pectoral girdle (scapula and clavicle); and pelvis
bones of the upper limbs
humerus
radius
ulna
carpals
metacarpals
phalanges
bones of the lower limbs
femur
tibia
fibula
tarsals
metatarsals
phalanges
Bone Composition
connective tissue derived from embryonic mesoderm; much harder than cartilage, but is relatively lightweight; vascular
long bones
characterized by cylindrical shafts
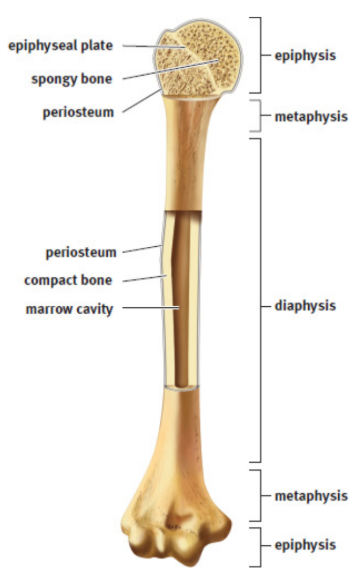
diaphyses
cylindrical shafts of long bones; full of marrow
metaphyses
point of swelling in a long bone; full of marrow
epiphyses
rounded terminal of long bone; spongy cores for more effective dispersion of force and pressure at the joints
compact bone
dense and strong; outermost portion of long bone
spongy / cancellous bone
lattice structure; consists of trabeculae; inner portion of long bone
bone marrow
fills cavities between trabeculae
Red marrow
filled with hematopoietic stem cells, which are responsible for the generation of all the cells in blood
yellow marrow
composed primarily of fat, relatively inactive
epiphyseal (growth) plate
cartilaginous structure at the internal edge of the epiphysis; site of longitudinal growth; filled with mitotic cells that contribute to growth from childhood to puberty
periosteum
fibrous sheath that surrounds the long bone to protect it as well as serve as a site for muscle attachment
Tendons
attach muscle to bone
ligaments
pieces of fibrous tissue that hold bones together at joints; consist of a synovial capsule, which encloses the actual joint cavity
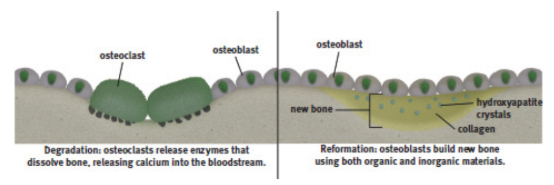
bone matrix
organic matrix of protein, polysaccharides and minerals, secreted by osteoblasts, that becomes bone after mineralization; responsible for strength of compact bone
organic components of bone matrix
collagen, glycoproteins, and other peptides
inorganic components of bone matrix
hydroxyapatite crystals and minerals like sodium, magnesium, and potassium
hydroxyapatite crystals (Ca10(PO4)6(OH)2)
calcium, phosphate, and hydroxide ions, which harden together
osteons / Haversian systems
structural units of bone matrix
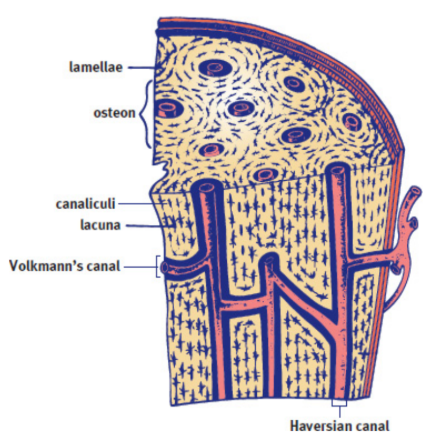
lamellae
concentric circles of bony matrix surrounding a central microscopic channel that contains the blood vessels, nerve fibers, and lymph vessels that maintain the health of the bone
Haversian canals
Longitudinal channels with an axis parallel to the bone
Volkmann’s canals
transverse channels with an axis perpendicular to the bone
lacunae
small spaces which house mature bone cells between the lamellar rings; interconnected by canaliculi
canaliculi
tiny channels that connect lacunae allow for the exchange of nutrients and wastes between osteocytes and the Haversian and Volkmann’s canals
Osteoblasts
cells that builds bone using essential ingredients such as calcium and phosphate obtained from the blood
osteoclasts,
polynucleated resident macrophages that resorb bone; release calcium and phosphate back into the bloodstream
Bone remodeling
occurs in response to stress in such a way as to accommodate the repetitive stresses faced by the body
Parathyroid hormone
peptide hormone released by the parathyroid glands in response to low blood calcium, promotes resorption of bone, increasing the concentration of calcium and phosphate in the blood
Vitamin D
activated by parathyroid hormone, also promotes the resorption of bone; encourages the growth of new, stronger bone
calcitonin
peptide hormone released by the parafollicular cells of the thyroid in response to high blood calcium, promotes bone formation, lowering blood calcium levels
Osteoporosis
most common bone disease in the United States; thought to be the result of increased osteoclast resorption and some concomitant slowing of bone formation, leading to loss of bone mass
Estrogen is believed to help prevent osteoporosis by stimulating osteoblast activity
Cartilage
softer and more flexible than bone; consists of chondrin; vascular
chondrin
firm but elastic matrix secrted by chondrocytes that makes up cartilage
chondrocytes
makes chondrin for cartilage
Fetal skeletons
mostly made up of cartilage; advantageous because fetuses must grow and develop in a confined environment and then must traverse the birth canal
Adult cartilage
only in body parts that need a little extra flexibility or cushioning
ex. external ear, nose, walls of the larynx and trachea, intervertebral discs, and joints
endochondral ossification
hardening of cartilage into bone; responsible for the formation of most of the long bones
intramembranous ossification
mesenchymal tissue is transformed into, and replaced by, bone
ex. skull
mesenchymal tissue
undifferentiated embryonic connective tissue
Immovable joints
Fixed joints between bones held together by dense, fibrous tissue
ex. skull