Pancreatic and Bile Secretions
1/18
Earn XP
Description and Tags
13, 15, 16
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
19 Terms
What organ produces the highest amount of proteins?

Pancreas has the highest rate of protein synthesis throughout the body
→ this is reflected in the structure of a pancreatic acinus, which has lots of RER stacked on top of one another
What is the signal transduction pathway in the pancreatic acinus?
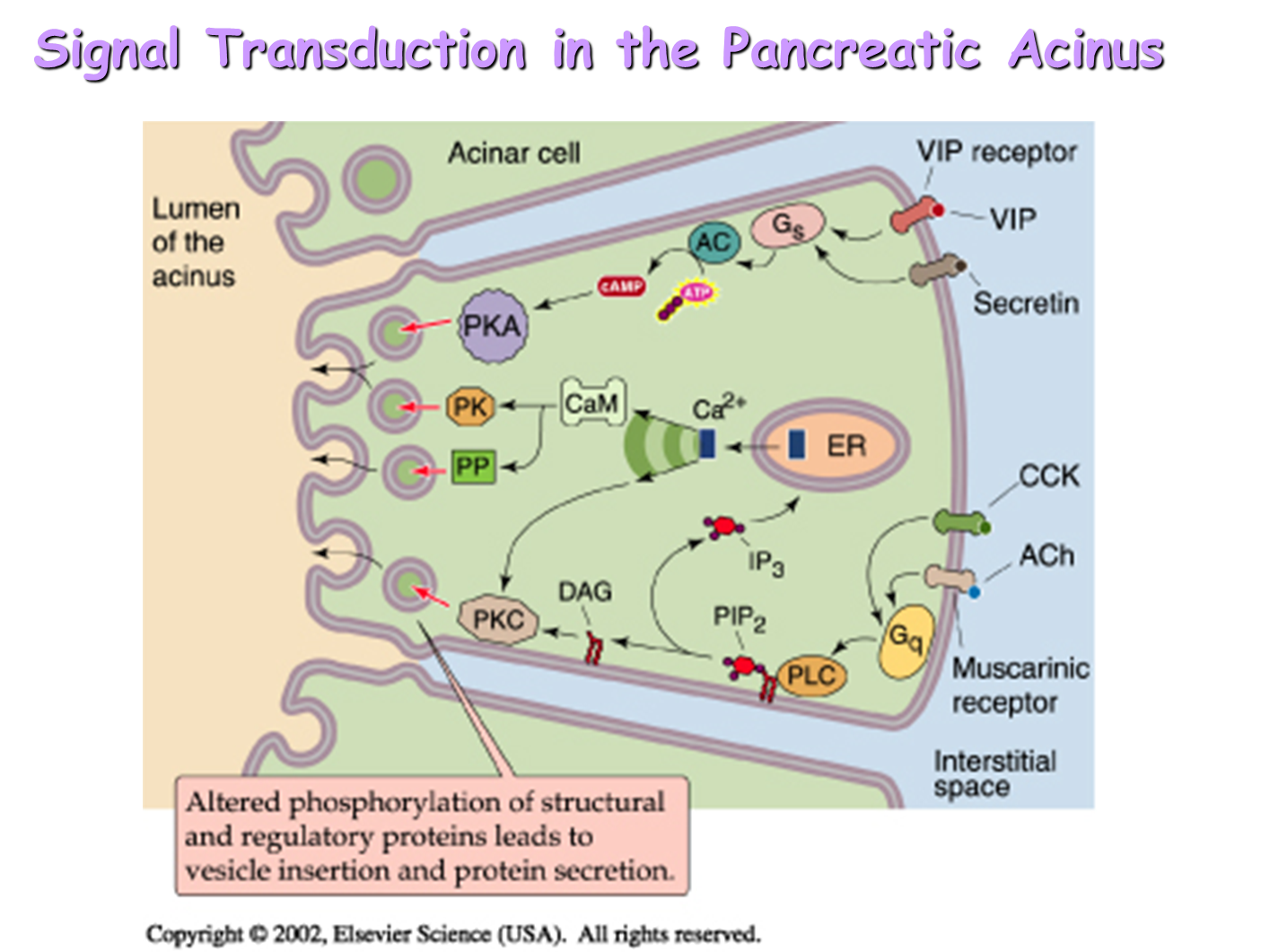
1) CCK Receptor and Acetylcholine Receptor
→ binding at the receptor activates the Gq protein leading to increased levels of IP3, DAG, and calcium
→ triggers release of fluid primarily and enzymes and is considered the principal hormone for secretion
2) VIP Receptor and Secretin (Vasoactive Intestinal Peptide)
→ coupled to adenylate cyclase pathway, increasing cAMP which triggering the secretion of primarily enzymes and a small amount of fluid
What are the active enzymes secreted by the pancreatic acinar cells
The majority of enzymes secreted from the pancreas are in the form of zymogens or inactive enzymes. However, the pancreas does secrete five active enzymes
→ alpha-Amylase
→ Carboxyl ester lipase
→ Lipase
→ RNAse
→ DNAse
Which organs secrete the most bicarbonate?
while forty percent of bicarbonate secretion comes from the Brunner’s glands in the mucosal cells of the duodenum, the other 60 percent is secreted by the pancreas
What is the rate of bicarbonate secretion in the pancreas as related to flow rate?
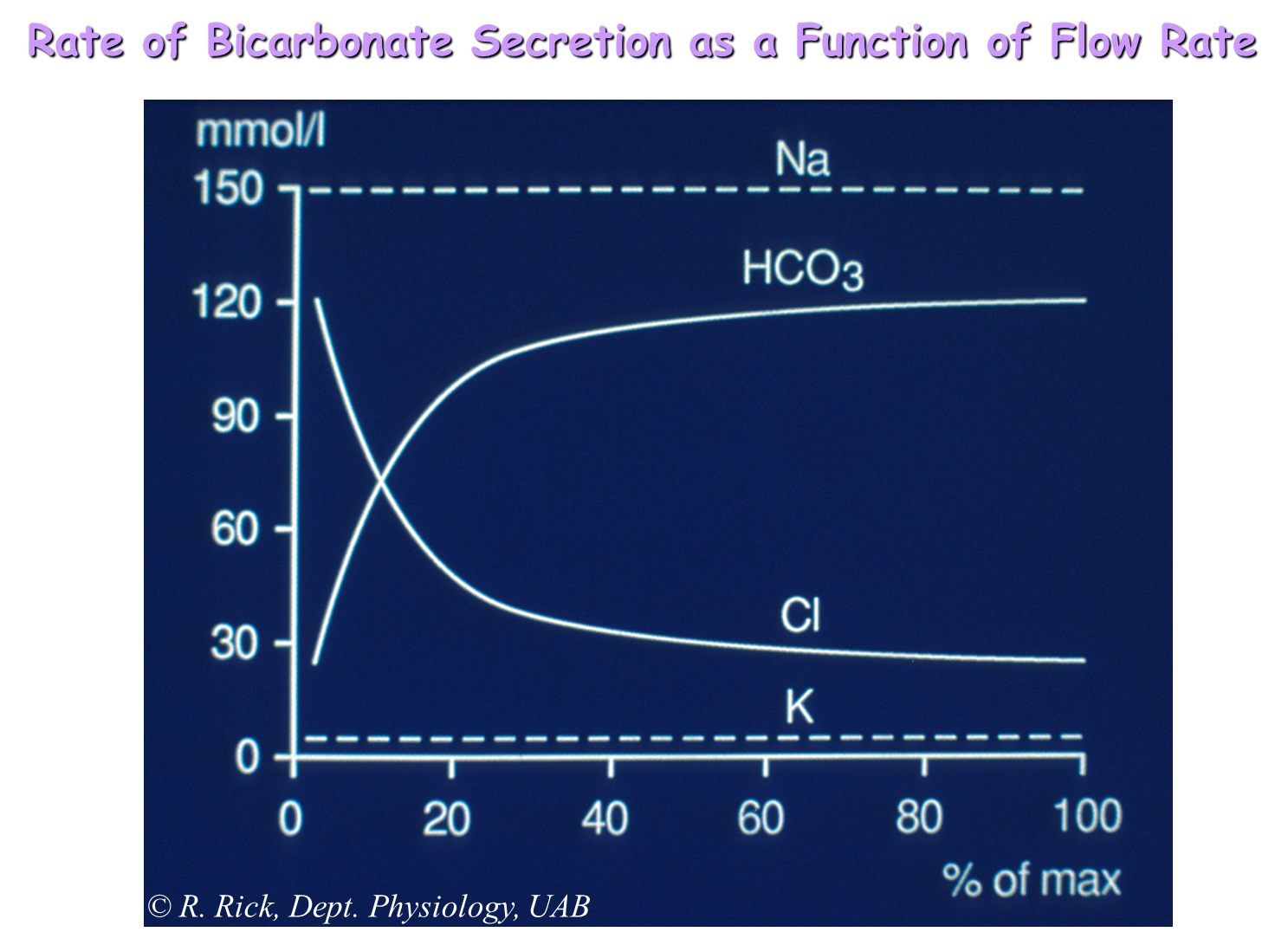
Flow Rate
→ at low flow rates, the predominant secretion in the pancreas is NaCl
→ as flow rates increase, bicarbonate secretions will increase while chloride secretions decrease, leading to majority sodium bicarbonate secretion
What is the Mechanism of Ion Secretion from Pancreatic Acinar Cells?
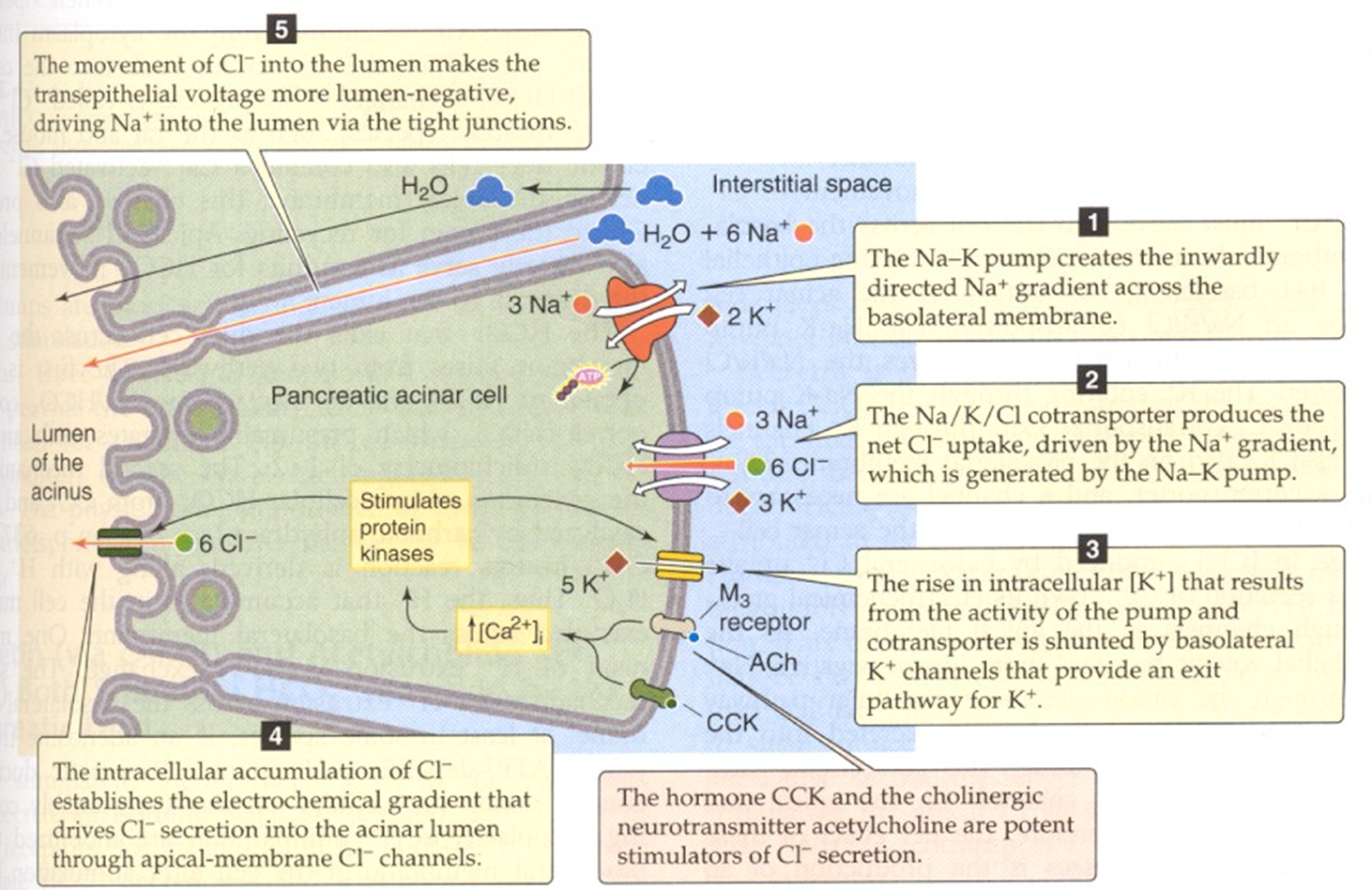
1) Sodium-Potassium pump will pump two potassium inward and three sodium outward
→ this creates an inward sodium gradient across the basolateral membrane
2) NaKCl cotransporter will uptake Chloride, driven by the gradient created by the Sodium Potassium Pump
3) rise in intracellular potassium from the activity of both NaKCl cotransporter and the sodium potassium pump is handled by a K+ channel on the basolateral end, letting K+ exit from the cell
4) Accumulated Chloride travels out from the acinar cell to the lumen of the acinus via a Chloride channel on the apical membrane
5) movement of Chloride outward into the lumen, makes the lumen more negative, allowing for sodium to travel into the lumen along with water via the tight junctions
How does ion transport in the pancreatic duct occur?
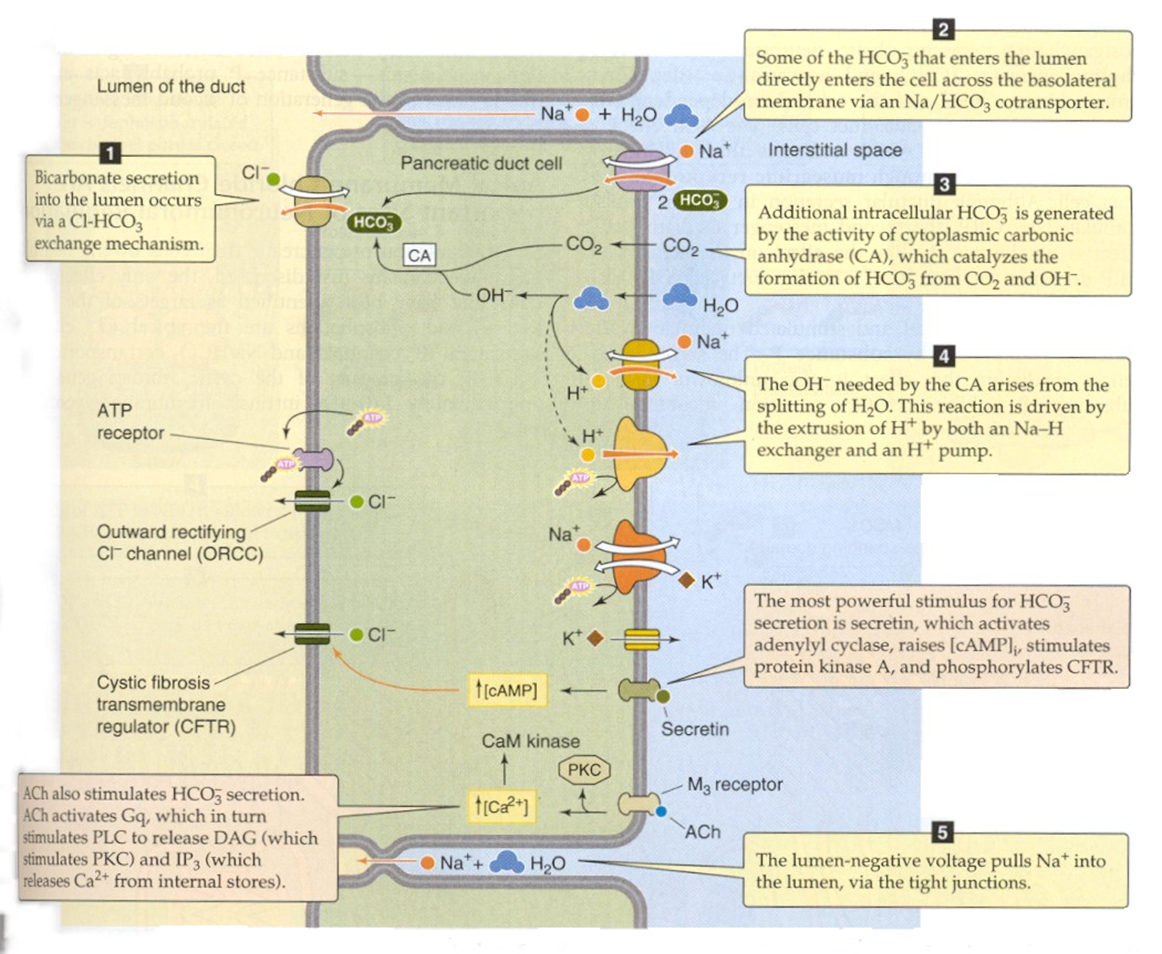
Stimulation of acetylcholine and secretin will be the main hormones responsible for fluid secretion
1) Bicarbonate secretion into the lumen will be performed by a Cl-HCO3 exchanger
→ the main transport of bicarbonate out into the lumen
2) Bicarbonate travels across from the interstitial space to the pancreatic duct cell via the Na/HCO3 cotransporter
3) Additional intracellular HCO3 is generated by carbonic anhydrase in the cytoplasm, transforming HCO3 from CO2 and OH-
4) CFTR Channel
→ CFTR channel sits on the apical membrane and allows for secretion of Chloride down its gradient into the lumen
→ makes sure that there is always enough chloride present in the lumen to exchange for Cl-HCO3 (see 1)
What is the difference between the cephalic, gastric and duodenal phase of digestion
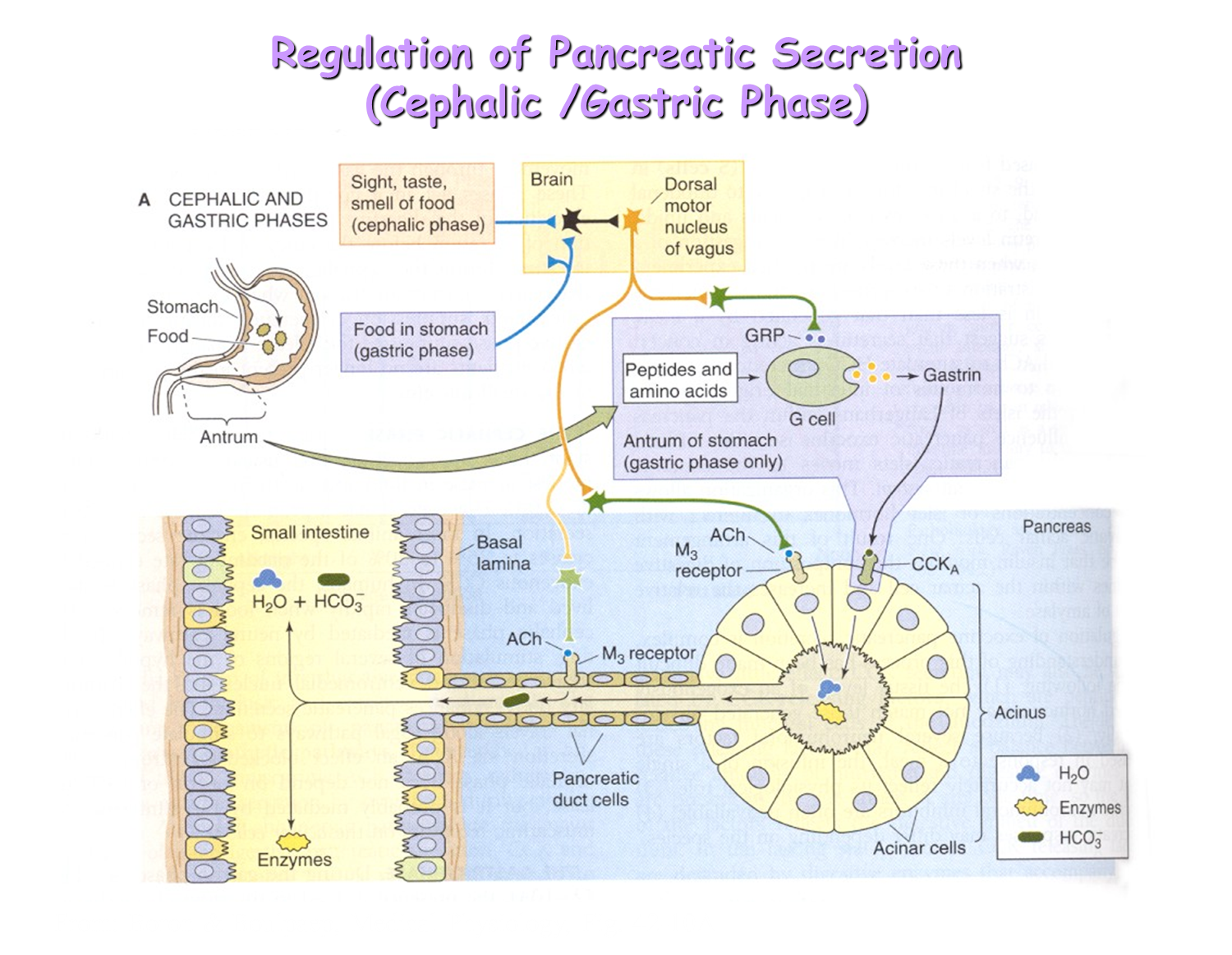
Cephalic Phase
→ purely neural phase that involves a reaction from the brain in response to the sight/smell/taste of food
→ leads to vagus stimulation causing the secretion of acetylcholine and gastrin
→ Acetylcholine binds to the M3 receptors while the Gastrin binds weakly to the CCKA receptor allowing for small amounts of fluid and enzyme release
Gastric Phase
→ distension induces vasovagal reflex from the stomach wall to the pancreas, causing the same things as the cephalic phase
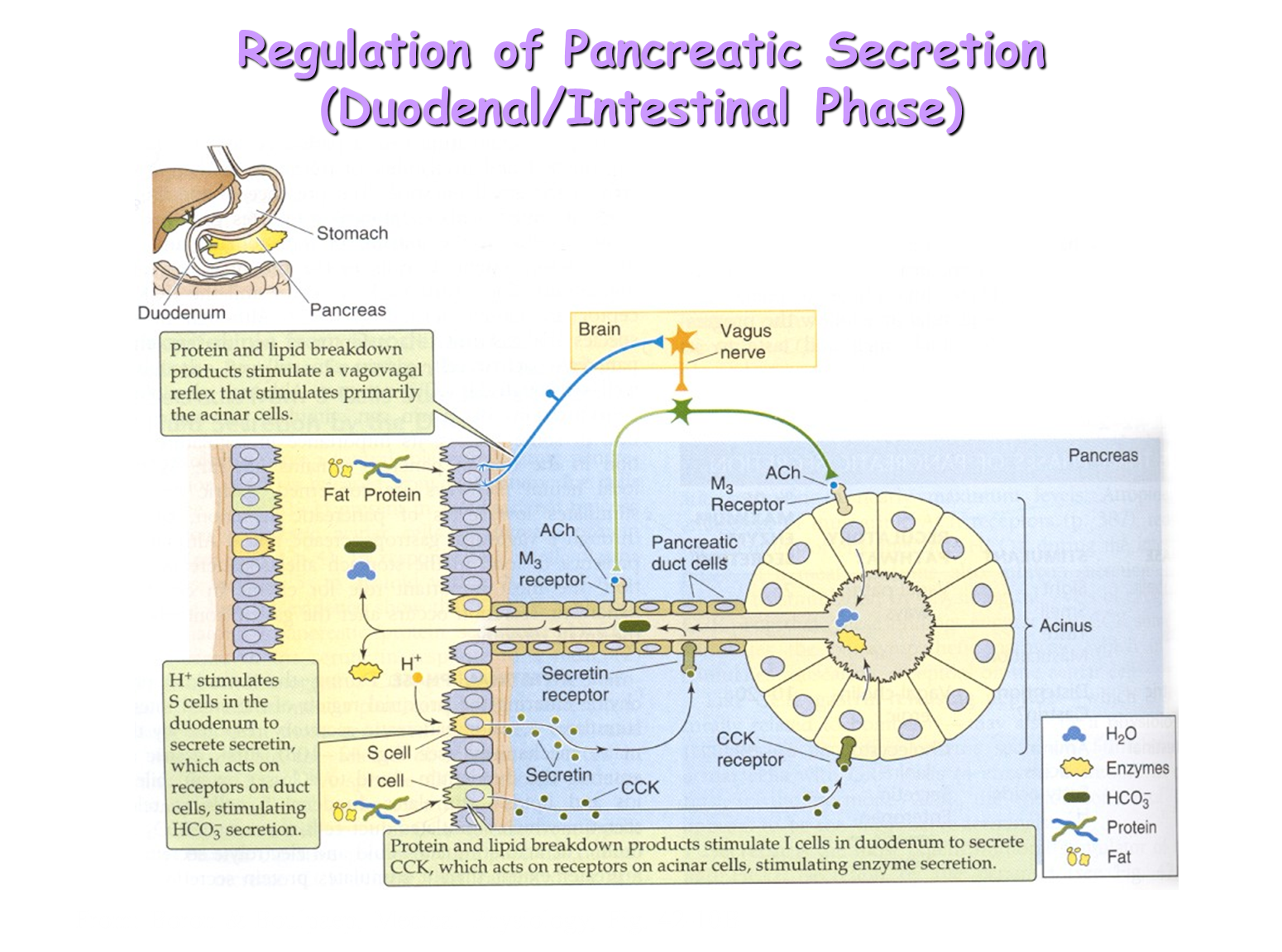
Duodenal/Intestinal Phase
→ presence of food emptying into the duodenum will activate the enteroendocrine cells of the intestine (S-cells and I-cells secretion of Secretin and CCK respectively)
→ increased levels of Secretin and CCK allow for a greater amount of enzyme and fluid release into the duodenum
How is the rate of bicarbonate secretion related to pH
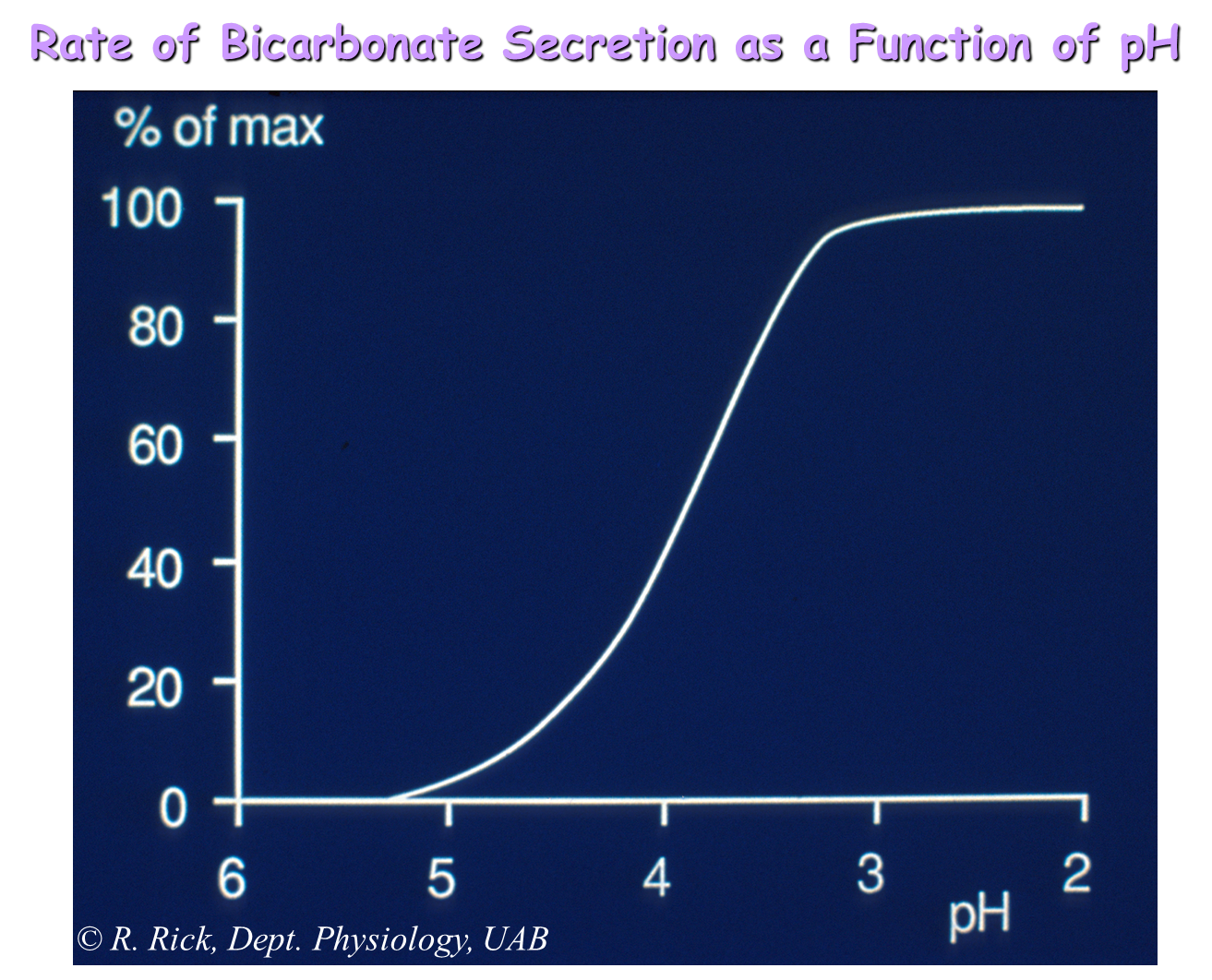
pH lowering will cause activation of the S-cells in the duodenum leading to secretin secretion and fluid secretion from the pancreas as a result
→ the duodenum however, will never reach an acidic point enough where pH will not have a major effect on the secretion of secretin
→ the pH of the duodenum lays around 5-6
→ because of this the primary activator of secretin secretion is controlled by interaction with food and the S-cells
What are Bile Acids and Salts?
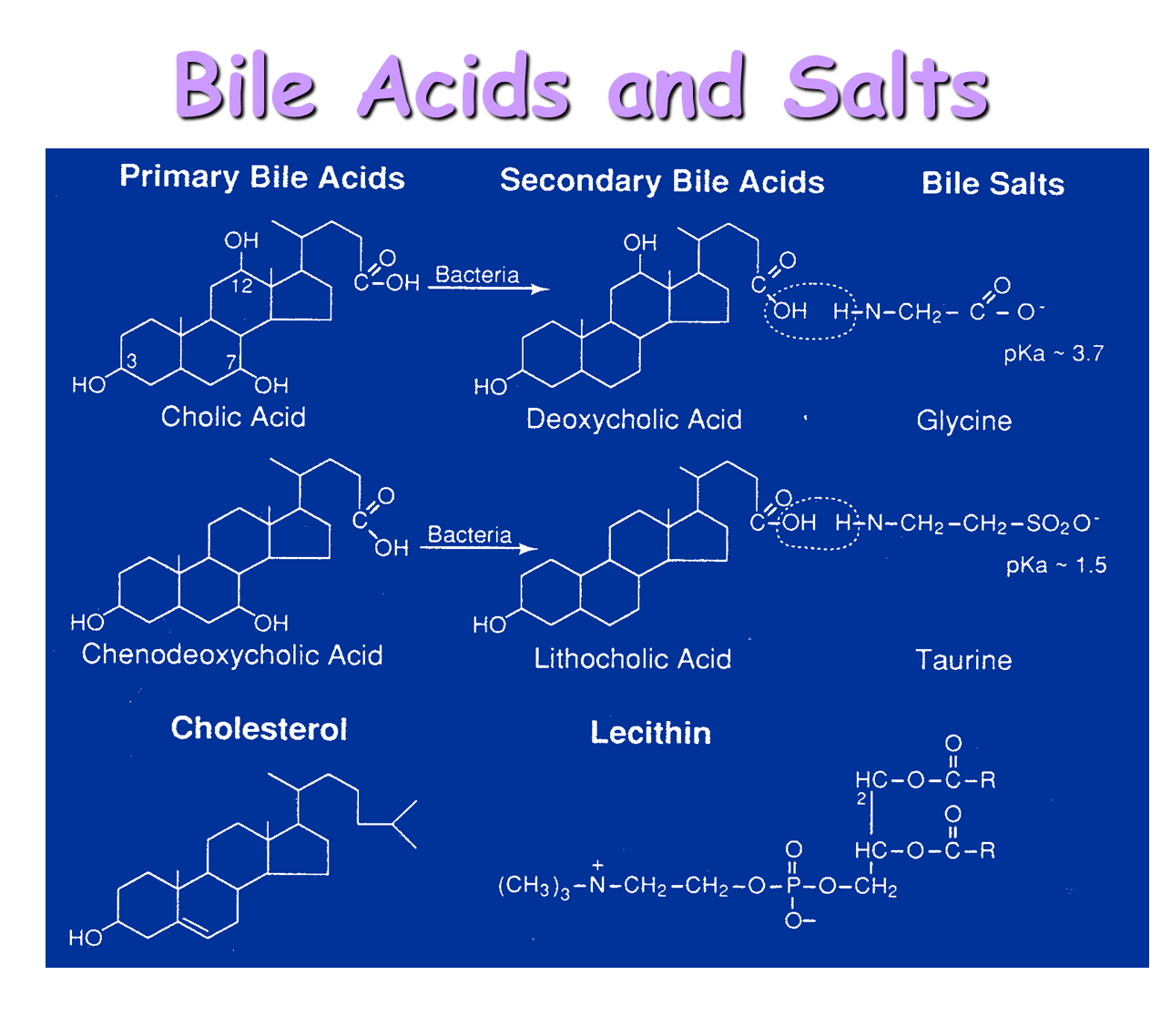
Bile Acids are derivatives of cholesterols and come in two main forms
1) Primary Bile Acids: Cholic Acid and Chenodeoxycholic Acid
→ when they are made by the liver, they are conjugated and have an added amino acid on it - this helps to make it more soluble
→ when put into the gut will be introduced to bacteria which will strip off its 7OH group and amino acid
2) Secondary Bile Acids: Deoxycholic Acid and Lithocholic Acid
→ has had its 7OH group and amino acid stripped off by bacteria in the gut, making it a secondary bile acid
What are the Bile Duct Transporters (bicarbonate)
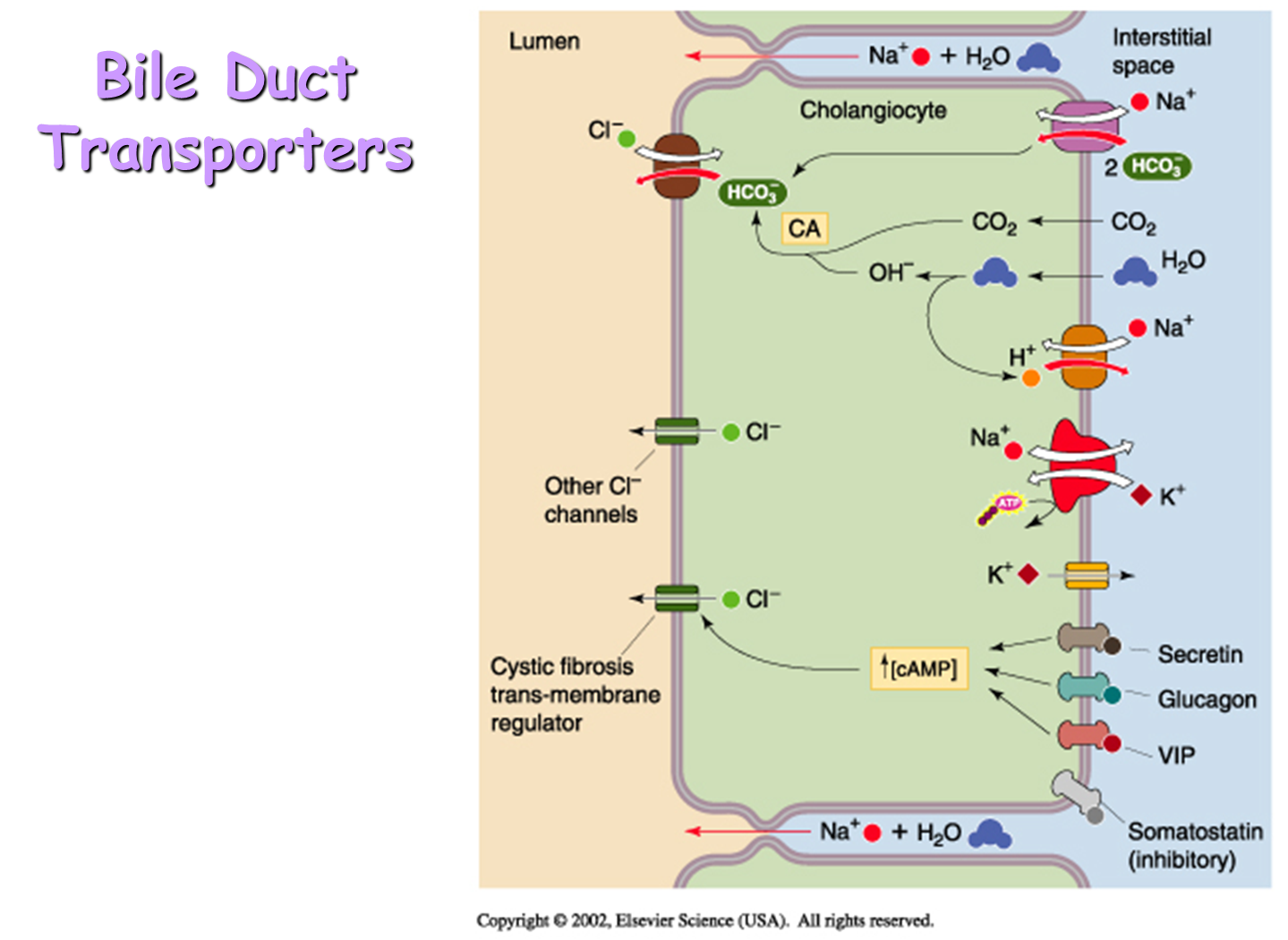
function the exact same as the pancreatic duct - coupled to Secretin, Glucagon, VIP, and Somatostatin (only inhibitory)
1) Bicarbonate secretion into the lumen will be performed by a Cl-HCO3 exchanger
→ the main transport of bicarbonate out into the lumen
2) Bicarbonate travels across from the interstitial space to the pancreatic duct cell via the Na/HCO3 cotransporter
3) Additional intracellular HCO3 is generated by carbonic anhydrase in the cytoplasm, transforming HCO3 from CO2 and OH-
4) CFTR Channel
→ CFTR channel sits on the apical membrane and allows for secretion of Chloride down its gradient into the lumen
→ makes sure that there is always enough chloride present in the lumen to exchange for Cl-HCO3 (see 1)
What is Enterohepatic Circulation?
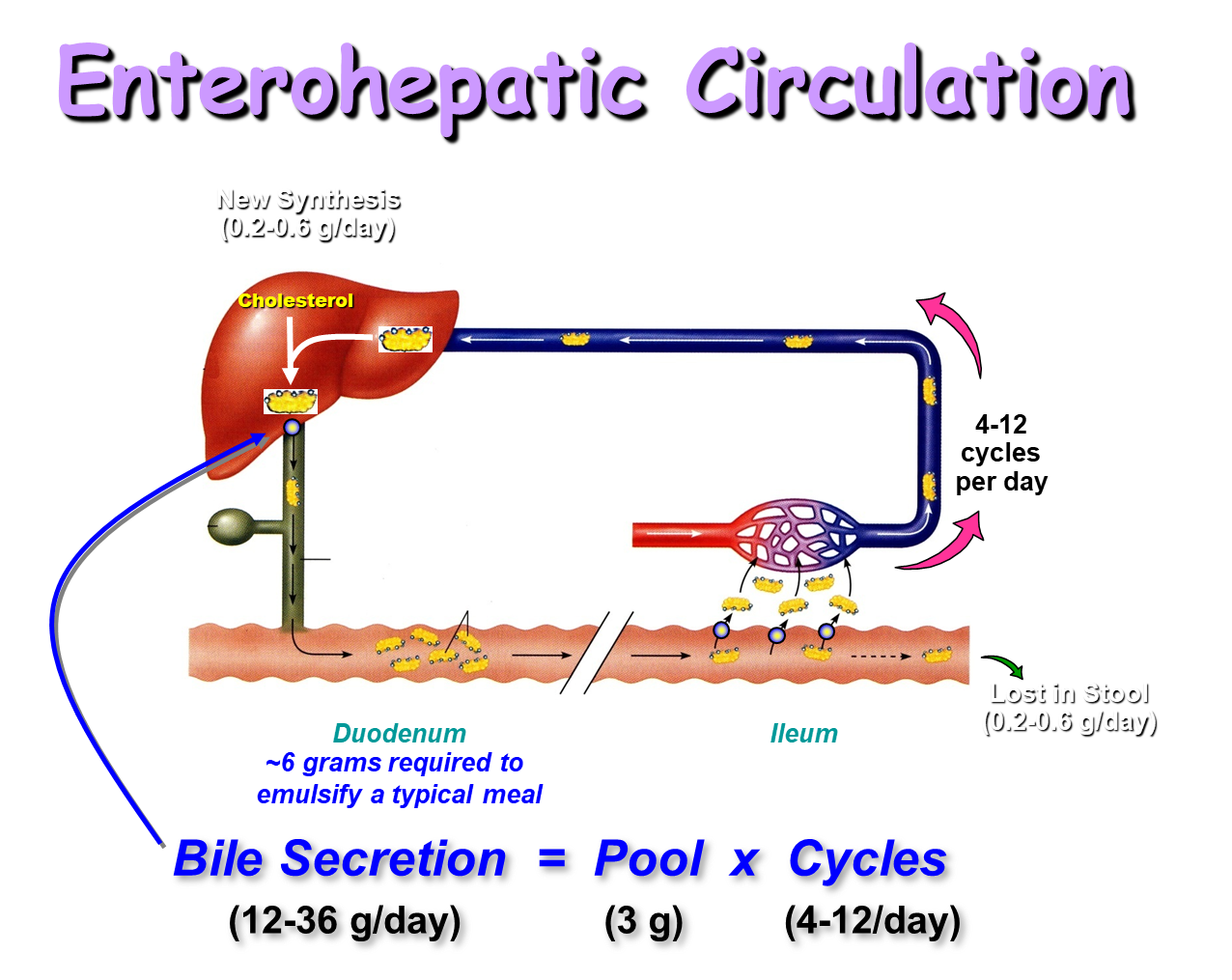
Bile Acids will be secreted into our duodenum from the liver/gall bladder
1) they will travel down to the terminal ileum, where if they are still a primary bile acid (still have their amino acid and their 7OH group) will be transported back to the liver
→ primary bile acids are not lipid soluble, and are hydrophilic, so will have transporters that pick them up
→ recycled back to the liver for reuse
2) secondary bile acids are more hydrophobic and can diffuse directly across the enterocyte - do not need a special transporter
→ will also be cycled back to the liver where they are reconjugated in the liver
this is done because bile acids are energetically costly to make
How does Bile Acid Transport Occur in the Hepatocytes
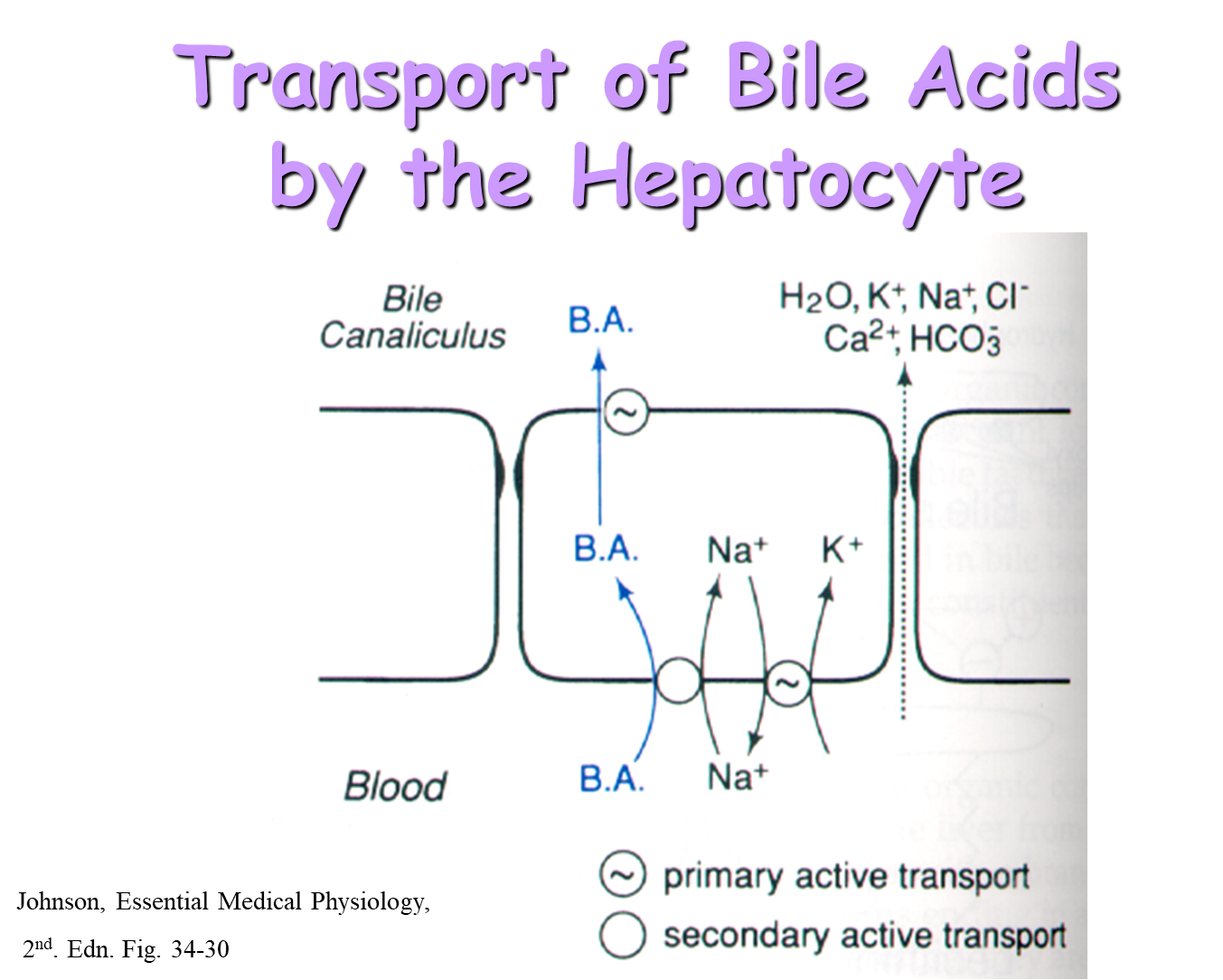
Bile Acids can be taken up from the hepatocytes from the blood via secondary active transport
→ the bile acids are then secreted out into the bile canaliculus via active transport
Why do we need a gall bladder
Bile Acids
→ powerful detergents that break apart membranes and are toxic to enterocytes
→ they are secreted constantly by the liver and are modified readily by bacteria
Because of this we have a dedicated organ, the gall bladder, to store the bile acids when we aren’t using them as well as helping to concentrate bile acids
What is the model for water absorption by the gall bladder?
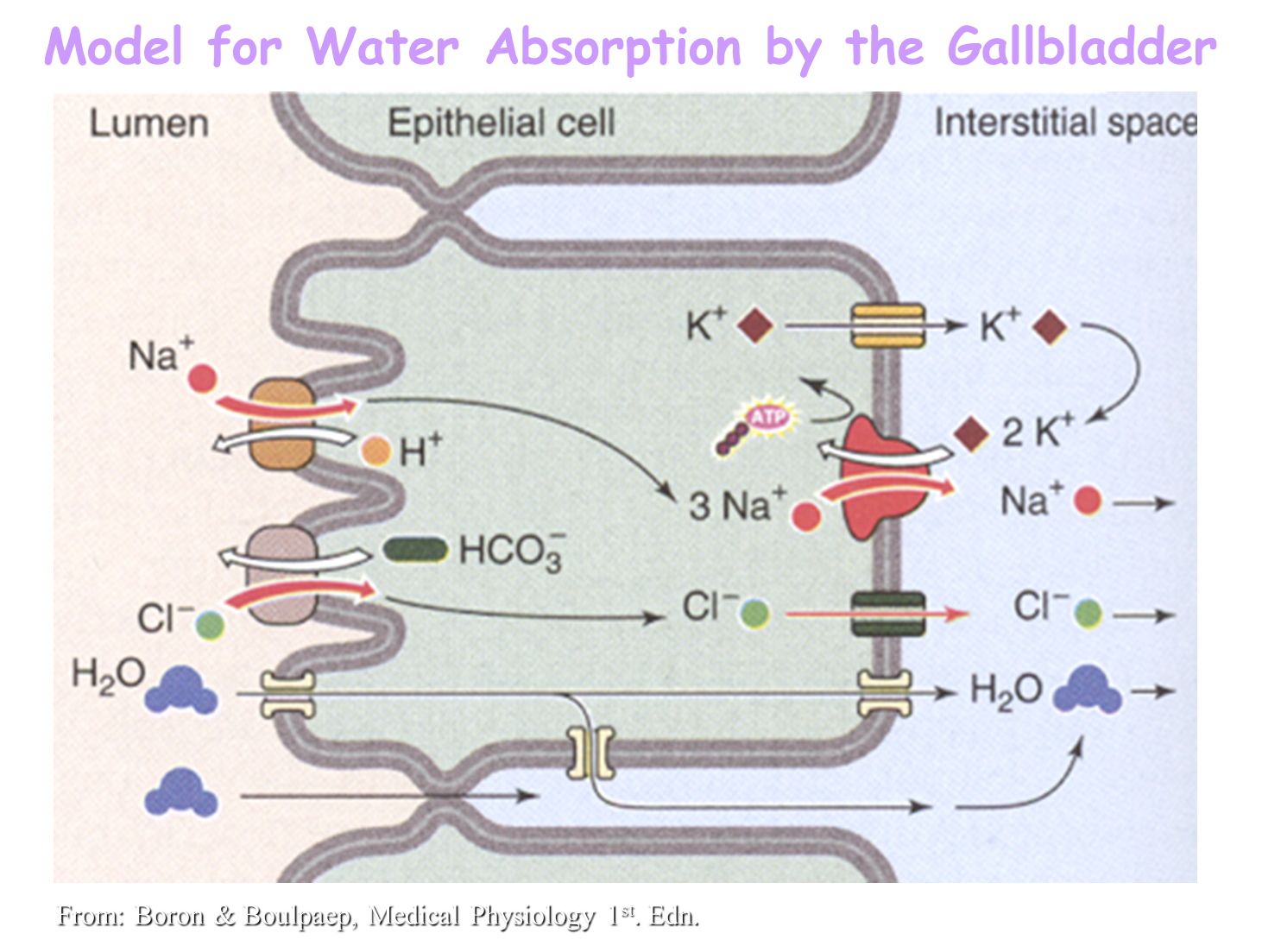
1) Pulling in sodium and chloride at the lumen of the gall bladder via the Sodium-proton exchanger and the Chloride-bicarbonate exchanger
→ the net movement of salt into the gall bladder allow for water to move through the gall bladder via the tight junctions into the interstitial space
What is the difference between bile in between meals and after meals
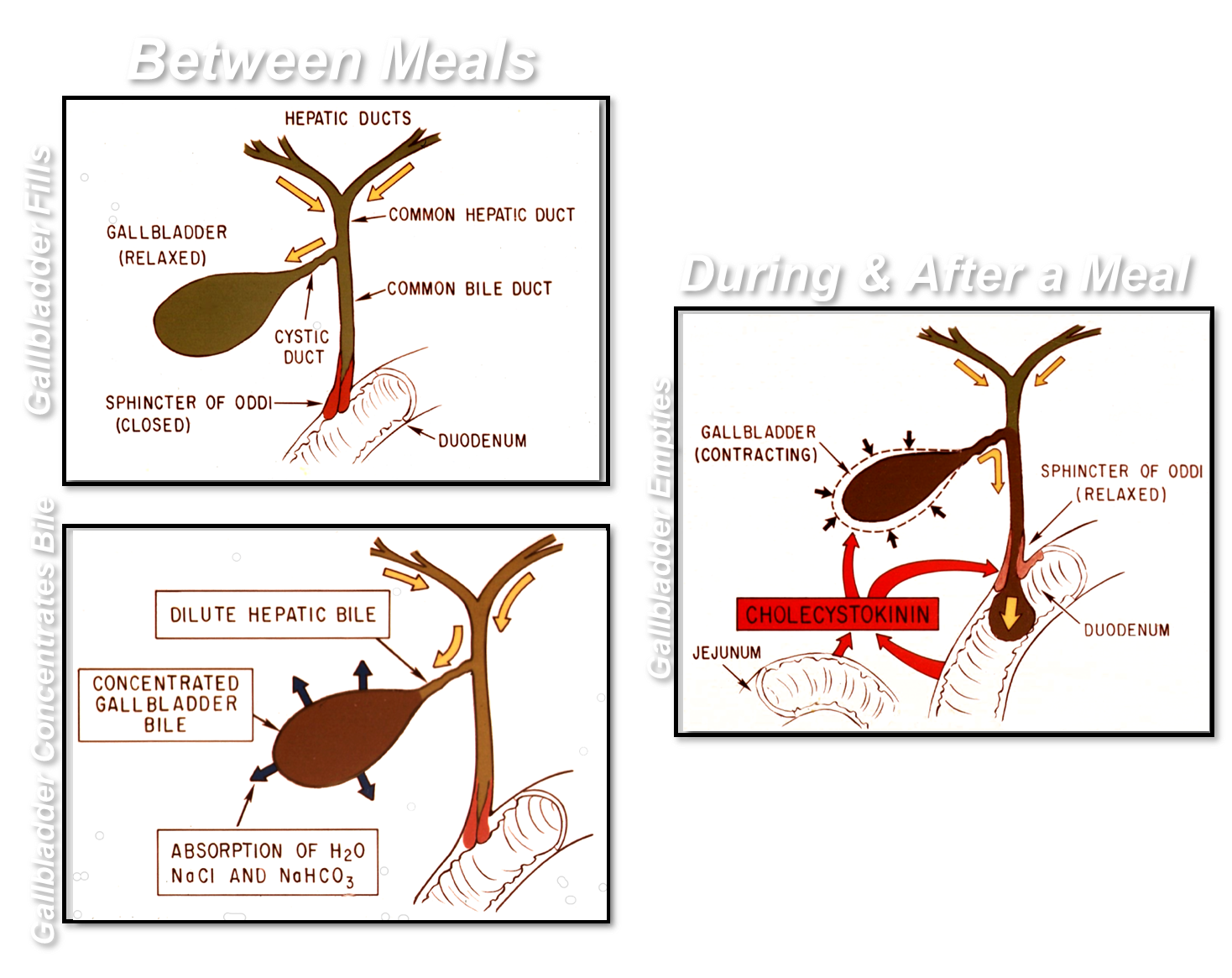
1) In Between Meals
→ the Sphincter of Oddi is contracted, causing the bile secreted by hepatic ducts to enter into a relaxed Gall Bladder via the Cystic Duct
→ The bile will become concentrated by the gall bladder by absorbing water and salt from the dilute bile
2) During and After Meal
→ release of CCK will contract the gall bladder, pushing bile outward into the duct and relaxation of the sphincter of Oddi
→ causes bile secretion into the second portion of the duodenum
What are Gall Stones?
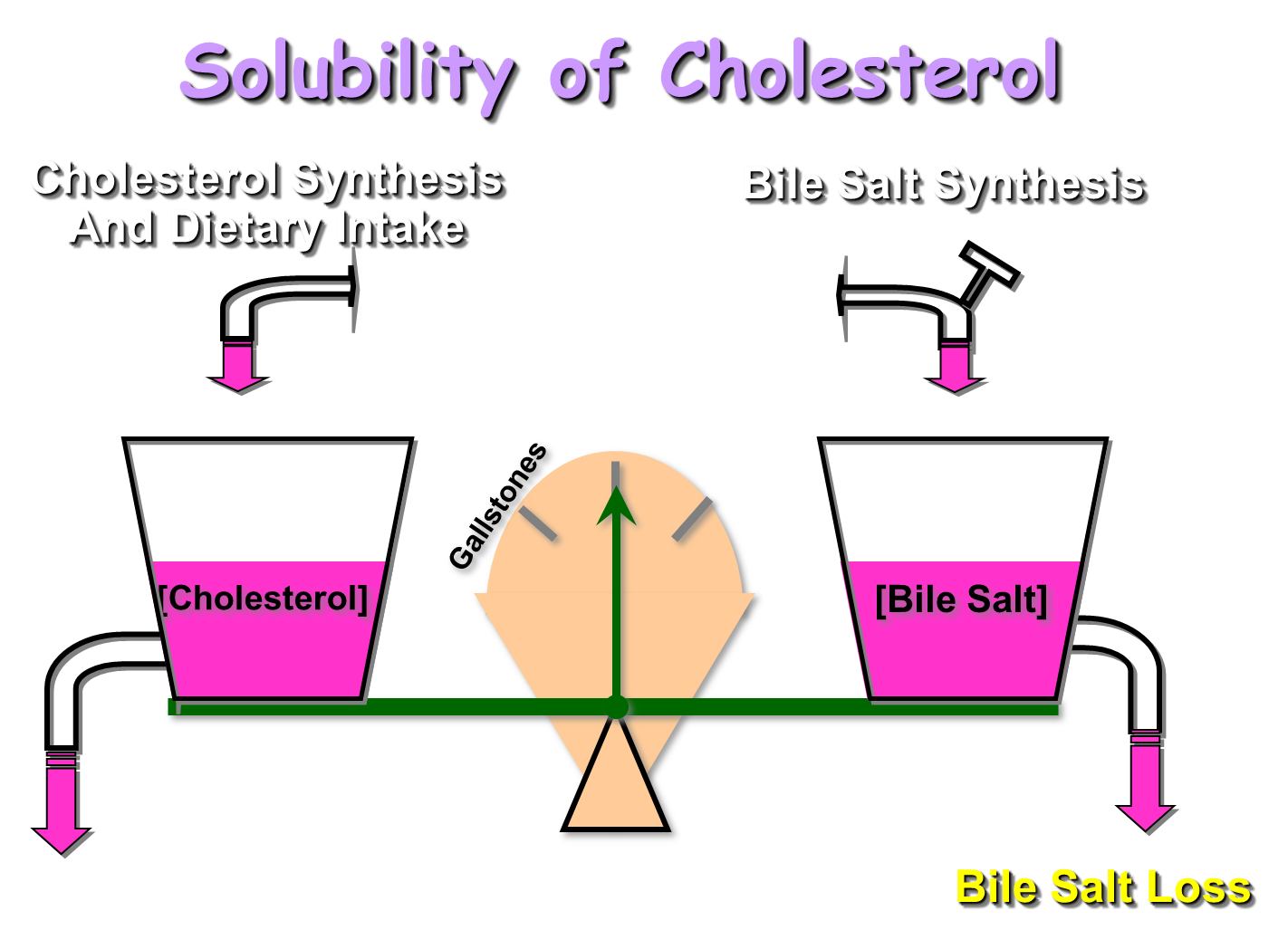
Stones that can be made of cholesterol (excessive cholesterol) or pigment (excessive bilirubin)
1) Pigment stones can be seen in people with elevated levels of bilirubin and is associated with people who are shedding red cells rapidly such as in sickle cell
2) Cholesterol stones are created from either excessive cholesterol or loss of bile salts (or both)
What is Bilirubin?
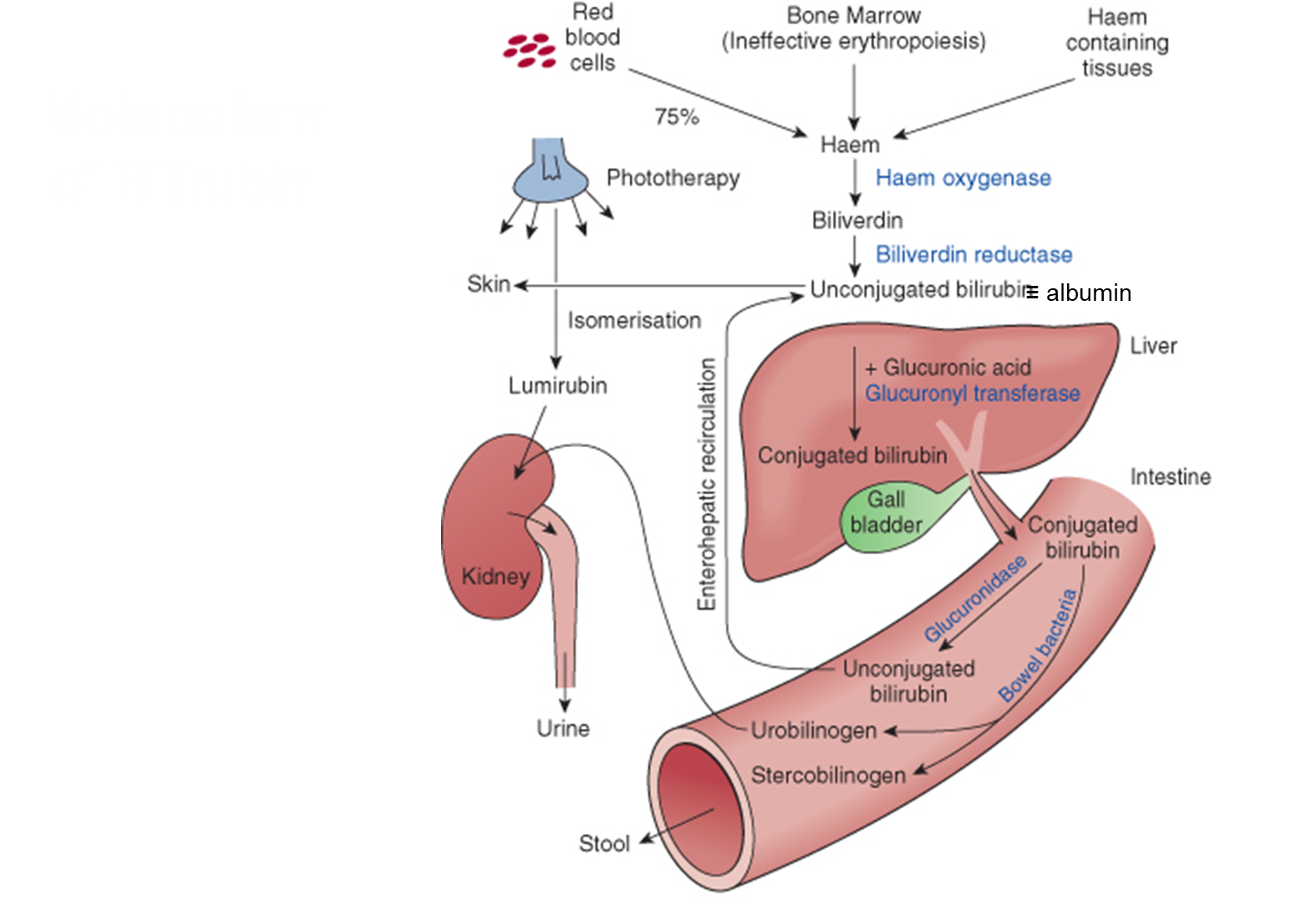
Bilirubin is a byproduct formed from the degradation of hemoglobin (destruction of red blood cells)
→ Bilirubin prefers to be conjugated, in the blood it will be with albumin and at the liver it will become conjugated with glucuronic acid
→ Bilirubin conjugated to glucuronide can be secreted into bile where it can be deconjugated to urobilinogen by bacteria
→ urobilinogen can escape into the blood and filtered into the kidneys - giving pee its characteristic color
→ urobilinogen can also be oxidized to urobilin and stercobilin which is then excreted in our poop which gives its characteristic color
what are the three kinds of jaundice
Three kinds of jaundice
1) Pre-hepatic jaundice - creating more bilirubin than you can get rid of
→ often seen in patients who are rapidly shedding red blood cells like sickle cell
2) Intra-hepatic jaundice - failure to conjugate bilirubin or failure to uptake it
→ seen in patients with hepatitis or cirrhosis
3) Post-hepatic jaundice - obstruction of the bile duct
→ causes bilirubin to back up through the liver and leading to bilirubin spilling outward into circulation