NMB monitoring and emergence from GA
1/53
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
54 Terms
_________- prevents overdosing NMB agents and reduces the chance of persistent post-operative weakness by how much %?
Weakness increases the potential for ____________
•Routine NMB monitoring prevents overdosing NMB agents and reduces the chance of persistent post-operative weakness
(35% incidence)
•Weakness increases the potential for airway complications, reintubation, and aspiration in PACU
Reasons to Monitor Neuromuscular Function Under Anesthesia
•To facilitate the timing of intubation
•To provide an objective measurement of relaxation during surgery and the degree of recovery before extubation
•To titrate dosages according to patient response
•To monitor for the development of phase II block
•To permit early recognition of patients with abnormal plasma cholinesterase
Neuromuscular Stimulator-
define and list the 3 factors ‘response’ depends on:
•A stimulator is an electrical device that delivers a series of shocks to the patient through electrodes applied to the skin near a nerve
•Muscle contraction is visible in the absence of NMB administration
•Response depends on 3 factors:
•Current applied
•Duration of the current
Position of the electrodes
Stimulating a Muscle Contraction- set up and MOA
•Stimulator is placed over a peripheral nerve
•Electrical current applied to the skin electrodes
•Electrical current stimulates voltage gated sodium channels which depolarizes the membrane and activating calcium channels on presynaptic neuron to open
•Calcium triggers release of AcH into the synaptic cleft
•AcH binds to nicotinic (N-m) receptors and opens sodium channel
•Sodium moving into muscle causes an action potential
•Action potential triggers muscle contraction
What is fade?
•The inability to sustain a response to repetitive nerve stimulation
•Is a sign of drug induced muscle paralysis
•Occurs because the nondepolarizing drugs block presynaptic acetylcholine receptors in addition to their classic antagonistic effect at postsynaptic ACh neuromuscular junction sites
•The function of presynaptic ACh receptors is to facilitate the release of Ach from the nerve terminal
•The facilitated ACh release is blocked by muscle relaxants and is detected as “fade”
Fade is best assessed with ________
Double-burst stimulation
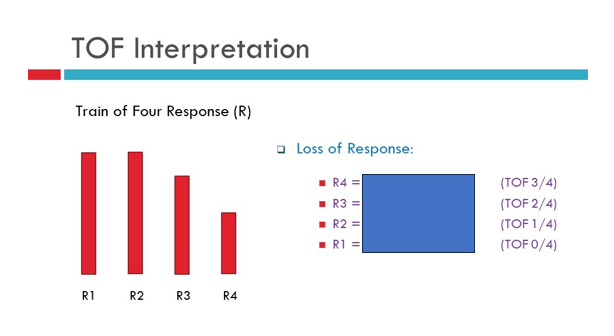
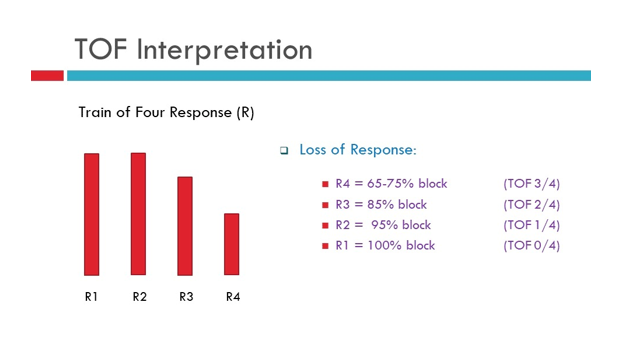
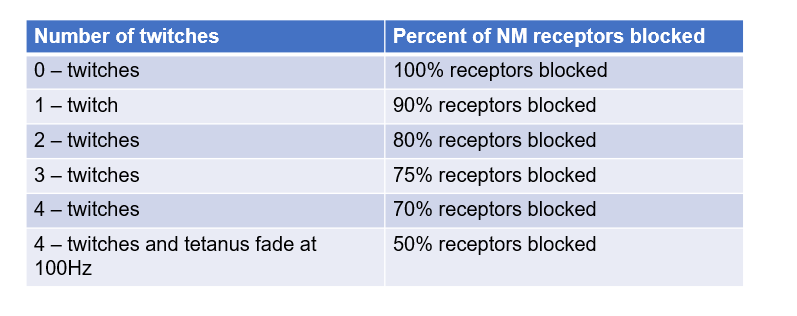
what is the % of block associated with these TOF twitches?
_______-is the preferred site of monitoring to determine level of NMB
How do you set it up?
what response are you looking for ?
Ulnar nerve -(Adductor pollicis muscle)
•Distal (negative) electrode is placed over the proximal flexor crease of the wrist
•Proximal (positive-red) electrode is placed over and parallel to the carpi ulnaris tendon
•Elicited response→ adduction of the thumb
Facial Nerve Monitoring-
what is the nerve that is being stimulated ?
what is the muscle being stimulated?
elicited reponse?
•Temporal branch of facial nerve
•Stimulates the orbicularis oculi muscle or orbicular muscle
• Illicited response → contraction of muscle around the eye or contraction of the lip
*Most common site if you do not have access to the Ulnar nerve
________ muscles are usually first to be lost and last to return
•Best site to monitor onset- intubating conditions b/c it Mirrors ________ relaxation
_________are more sensitive to NMB and will indicate full return of upper airway muscles
•Best site to monitor reversal – extubating conditions
Eye
larynx and diaphragm
Adductor pollicis [ulnar nerve]
onset of paralysis- muscles from 1st-last
eyes → extremities → Trunk [neck to intercostals] → abdominal muscles → Diaphragm
Recovery from paralysis - 1st - last
Diaphragm → abd muscles → trunk → extremities → Face → protective reflexes of pharynx and upper esophagus
________ time from drug administration to maximum effect
_________ time from drug admin to 25% recovery of the twitch response
__________ time from drug admin to 90% recovery of twitch response
___________: compares the 4th twitch to the 1st twitch; recovery is indicated when the 4th twitch is ____% of the first
•Onset time:
•Clinical duration:
•Total duration of action
Train-of-four ratio
90% TOFr- 0.9!!
•Pulse length of NM monitoring usually set to allow __________ before next twitch can occur
•Usually_________[length of time]
•Set by manufacturer
repolarization of nerve
0.1-0.2 msec
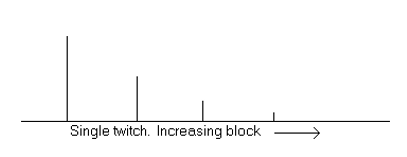
Single Twitch
•A single supramaximal electrical stimulus ranging from 0.1-1 Hz with a 10 second delay between twitches
•Generally used as a qualitative rather than quantitative measure
•Used to determine onset of NMB
As block is starting to work the degree of response decreases!
Train-of-Four (TOF)
•A series of four twitches at ___ Hz every half-second for ___ seconds
•Monitored visually or manually [can feel the twitches]
•Reflects blockade from ______%
•Useful during ___________
2
2
70-100
onset, maintenance, and emergence
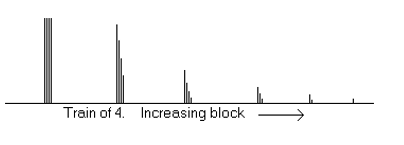
just because we have 4/4 twitches does not mean we are ‘ready’ to extubate!
Tetanus
•Consists of rapid delivery of a ________Hz stimulus for ___ seconds
•Should be used sparingly for _________
•Do not perform on a _______
30, 50, or 100
5
deep block assessment
fully alert patient- painful
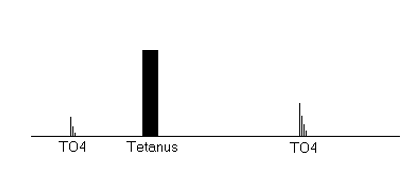
Post-Tetanic Count- describe
•Useful when the_____________ response is absent
A PTC of ______indicates a reversal in less than 10 mins
•50-Hz tetanus for 5 seconds, followed by a 3 second pause then single twitches of 1 Hz
•Because you have 100% paralysis, the value of the PTC is to attempt to give a time estimate as to when recovery may occur
•Useful when the TOF or double-burst stimulation response is absent
•The number of twitches elicited is counted
•The higher the count, the less intense the block
A PTC of 6-8 indicates a reversal in less than 10 mins
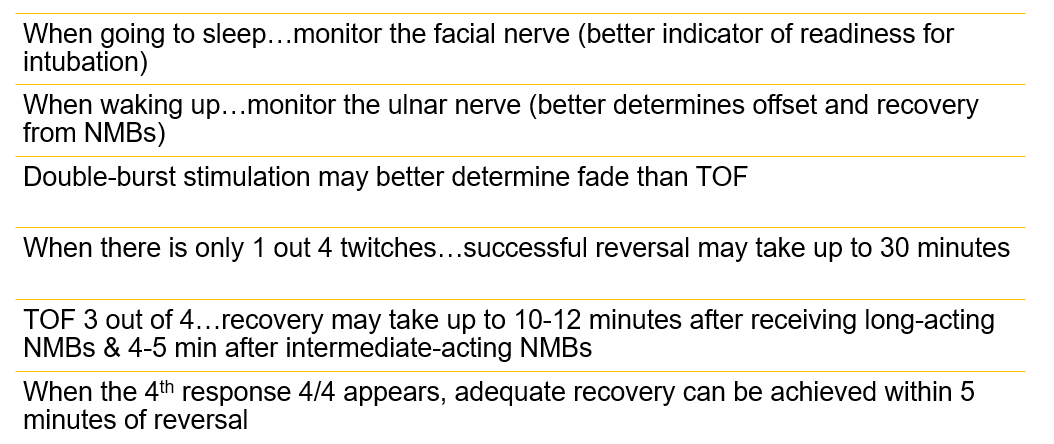
Double-Burst Stimulation
•2 short bursts of ____ tetanus separated by ____ seconds
•The use of DBS improves the ability to detect________during recovery
•Evaluate second response to first response which facilitates detection of ____
•Useful during all phases of care
•Correlates closely with _____
•Easier to detect ____ when compared to TOF
50Hz
0.75
residual paralysis during recovery
fade
TOF
fade
Depolarizing (Phase I) Block [Succ]
•Block antagonized by prior administration of ______ as pretreatment (approx. ____% more succ. required)
•Block potentiated by ____________ drugs
•Succinylcholine mimics the action of ACh by depolarizing the motor endplate, but is different from ACh because it is hydrolyzed by plasma cholinesterase
•Muscle fasciculation precedes the onset of NMB
•Sustained response to tetanic stimulation (no fade)
•Absence of post-tetanic potentiation, stimulation, or facilitation
•Lack of fade of TOF or double-burst stimulation
•Block antagonized by prior administration of non-depolarizer as pretreatment (approx. 20% more succ. required)
•Block potentiated by anti-cholinesterase drugs (Acetylcholinesterase inhibitors)
Phase II Block
•Occurs after repeated or continuous administration of Succinylcholine
•May occur with dosages of 2-5 mg/kg in conjunction with inhaled anesthetics or in higher doses 8-12 mg/kg with N20-opioid anesthesia
•Is characterized by:
•Fade after tetanic or TOF stimulation
•Post tetanic potentiation (facilitation)
•Partial or complete reversal with anticholinesterases
•Resembles nondepolarizing block
high doses will inhibit presynaptic Ach receptors so that is why you will see fade with phase 2
Guidelines for Successful NM Monitoring- summary
Factors that may prolong paralysis:
•Myasthenia gravis *
if you are not optimized→ give a anticholinesterase
•Motor neuron disease
•Muscular dystrophy
•Guillain-Barre’ syndrome
•Amyotrophic lateral sclerosis
•Steroid myopathy
•Clindamycin
•Tetracycline
•Cyclosporine
•Volatile anesthetics
•Magnesium
•Lithium
•Increased age
•Pregnancy
Atypical Plasma Cholinesterase is also known as:
•pseudocholinesterase deficiency, atypical butyrylcholinesterase (BuChE)
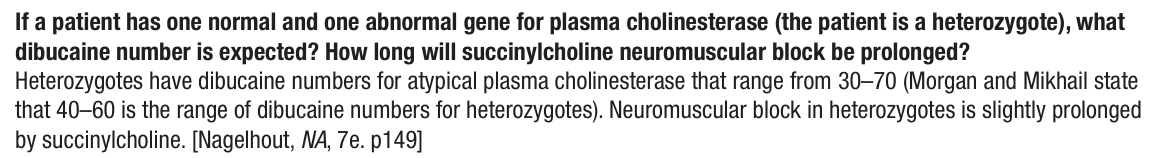
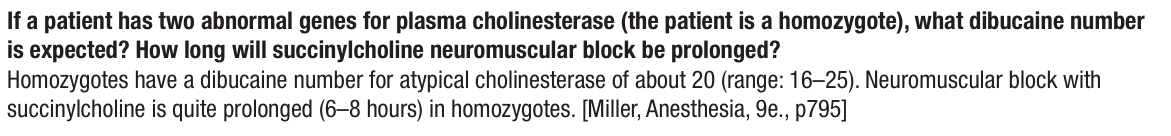
Atypical Plasma Cholinesterase- characteristics and dx
•Characterized by insufficient plasma cholinesterase levels
•Results in prolonged block (8+ hrs) after administration of the depolarizing NMB succinylcholine (SCh)
•Atypical plasma cholinesterase levels are determined by the Dibucaine Number Test
•Patients with a Dibucaine Number LESS THAN 80 have atypical plasma cholinesterase activity (should not receive SCh)
•NORMAL DIBUCAINE NUMBER=80
•Patients with a Dibucaine Number LESS THAN ______ have atypical plasma cholinesterase activity (should not receive ____)
•NORMAL DIBUCAINE NUMBER=_________
<80 [thoughts? might be 20?]
Succ
80
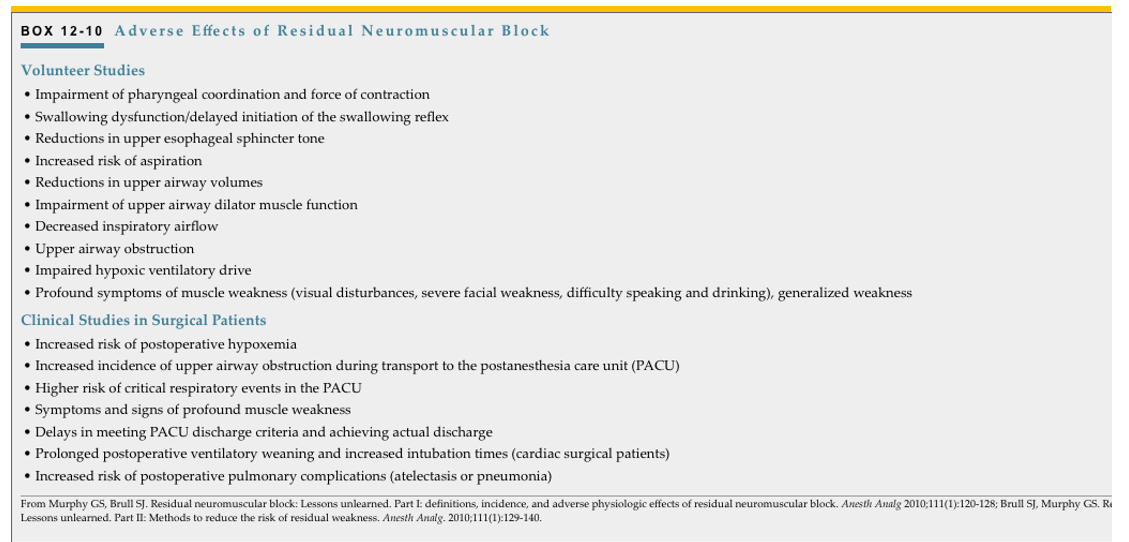
Reversal of Neuromuscular Blockade
•Studies have indicated that the incidence of residual paralysis may be as high as ______%
•Residual paralysis has occurred up to 4hrs after use of an intermediate relaxant this is called —> __________
45%
“re-curarization”
Reversal should not be attempted unless spontaneous recovery of _______ twitches of the TOF has occurred (Unless using sugammadex)
A TOFR of ______ along with clinical signs like: ________ were criteria for many years
A TOFR of ≥ ____ should be attained because even small degrees of residual block increase the incidence of adverse outcomes and morbidity
1-2
0.7
strong hand grip and 5 second head lift
0.9
Best indication of NMBA reversal is TOFR ≥
0.9

reversal considerations when return of muscle strength is incomplete in clinical practice
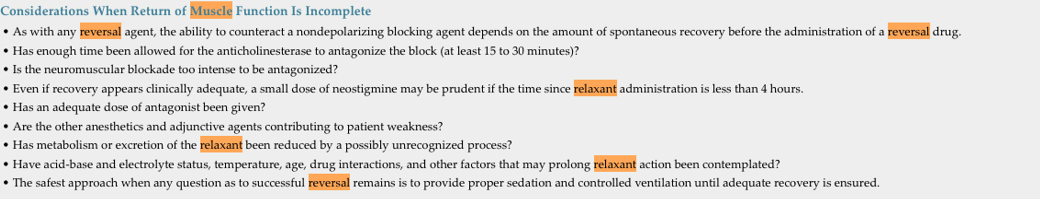
Cholinesterase Inhibitors
MOA
provides 2 mechanisms in the reversal of NM blockade:
•Inhibit AChE, thereby increasing the concentration of endogenous ACh around the receptors
•Provides 2 mechanisms in the reversal of NM blockade:
Increases the concentration of ACh at the junctional cleft, which increases the likelihood that the ACh will reoccupy the receptor site once occupied by the NM blocker
Because the concentration of ACh is increased, the life of the ACh within the cleft is increased
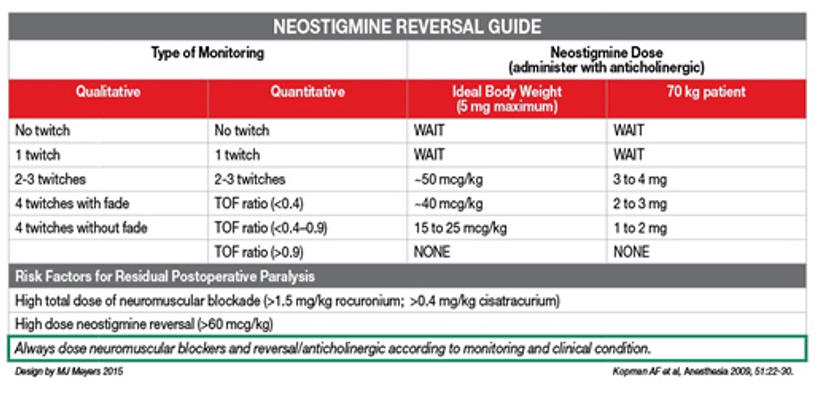
Most common reversal agents with onest and DOA
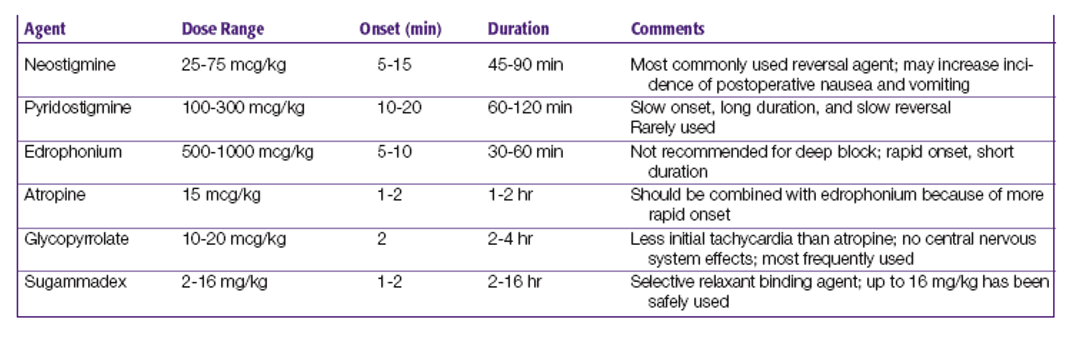
neostigmine reversal guide and risk factors for residual postop paralysis
Sugammadex
•Cyclodextrin that encapsulates rocuronium or vecuronium
•With a moderate block, 2 mg/kg provides recovery of TOF ratio of 0.9 within 100 seconds
•Dose depends on the degree of NM blockade
4-8 mg/kg for a more profound block
16 mg/kg will immediately reverse rocuronium
•Does not inhibit acetylcholinesterase, so it avoids the need for antimuscarinics
•Low volume of distribution (12-15 L)
•75-90% is eliminated unchanged in the urine
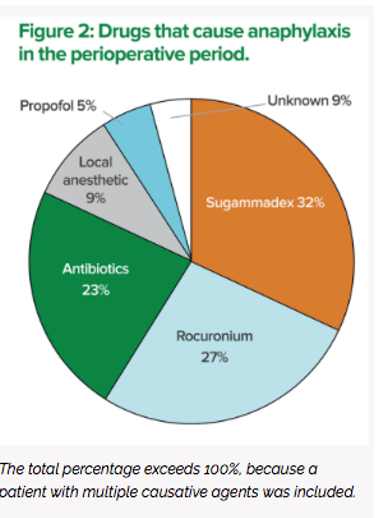
•Risk for anaphylaxis-
drugs that cause anaphylaxis in the perioperative period
Common Clinical Signs of Recovery from NMBs
•Adequate Vt and RR
•Respirations smooth and unlabored
•Pt opens eyes widely on command
•Effective swallow, gag, cough
•Head lift >5 seconds; strong knee to chest movement is equivalent in small children
•Adequate vital capacity of 15ml/kg
•Negative inspiratory force (NIF) -25 to -30 cm H20
•Sustained tetanic response to 50 Hz for 5 seconds
No fade to double burst stimulation
Avoiding Residual Postoperative Block if Equipment Is Not Available:
•Do not use long-acting NM blocking agents
•Antagonize the block at the end of the procedure
•If a nerve stimulator is not available
•Do not initiate reversal before spontaneous muscle activity is present
•Adhere meticulously to the rules for clinical evaluation of residual block
IF a nerve stimulator is available
•Do not initiate reversal before at least______responses to TOF stimulation are present
•During recovery, tactile evaluation of response to ______ is preferred over tactile evaluation of the response to TOF stimulation
•easier to feel ____ in ____ stimulation than in the TOF response
2 (preferably 3 or 4)
double burst stimulation
fade
DB stimulation
•Surgical stimulation diminishes as the procedure nears completion and__________ is reduced, enabling rapid emergence
•Residual ________ is reversed
•The patient should start to breathe________
_______ requirements should be addressed before awakening
•The OR should be __________
•The patient should be returned to the _______ position before extubation
anesthetic depth
muscle relaxant
spontaneously
•Analgesic
warmed, warm blankets placed on the patient, with noise and conversation minimized
supine
remember not to extubate during phase ____ of anesthesia for risk of __________
II
laryngospasm
Awake extubation -
indicated for what patients?
criteria to meet for awake extubation:
may give lido b/c of ETT irritation- what is the dose:
lidocaine suppresses what?
•Occurs after the patient fully regains protective reflexes
•Is indicated in patients at risk of aspiration, difficult airways, and patients who may be difficult to mask ventilate
The patient should be:
awake
hemodynamically stable,
regained full muscle strength,
follow simple commands (lift head)
breathe spontaneously with adequate oxygenation and ventilation
•The presence of an ETT may be irritating to patients emerging from anesthesia: Lidocaine 0.5-1.0mg/kg IV
•Suppresses coughing but may prolong emergence
sequence to extubation :
•The patient breathes 100% O2
•Oropharynx is suctioned
•Mild positive airway pressure (20cm H20) is applied via the ETT [APL valve]
•ETT cuff is deflated and tube is removed
•100% O2 administration via face mask
•Attention should remain focused on the patient until the patient’s ability to ventilate, oxygenate and protect their airway is confirmed
•The extubated patient may become unconscious again and lose protective airway reflexes when stimulation decreases
Deep Extubation
reduces risk of _______ and good for ______ surgeries
useful for ___& ___ Pt
other factors to consider:
•Stimulation of airway reflexes by the ETT during emergence can be avoided by extubating the patient while the patient is still deeply anesthetized (stage III MAC >1.3)
•Reduces the risk of laryngospasm and bronchospasm
•Avoids the coughing and bucking that is undesirable after middle ear surgery, open eye surgeries, and abdominal or inguinal hernias
•Useful for smokers, asthmatics
•Avoids the coughing and bucking that is undesirable after middle ear surgery, open eye surgeries, and abdominal or inguinal hernias
•Consider contraindications
•Anesthesia depth must be sufficient to avoid responses to airway stimulation
•Anesthesia may be deepened with a short acting IV anesthetic (propofol) or brief inhalation of a high concentration of volatile agent
w/ deep extubation have airway equipment and meds ready in case you need to reintubate
*Deflate cuff- if NO response→ extubate!
since they were ‘deep’ you might need to help them breathe for a little bit after extubation w/ APL and 100% O2
Emergence Delirium
•Severe agitation is occasionally seen on emergence from GA, especially in adolescents
•Physiologic causes:
Hypoxia
Hypercarbia
Airway obstruction
Full bladder
Pain: treated with cautious titration of opioids (Fentanyl 25mcg IV)
Delayed Awakening
ABG will tell you what?
consider Xray/CT for ___
_____ is the most frequent cause of delayed awakening in PACU
•Evaluate vital signs: BP, SaO2, EKG, temp
•ABG will detect problems of oxygenation, ventilation, electrolyte imbalance, metabolic disorders (glucose)
•Consider XRay/CT for evaluation of intracranial or intrathoracic abnormalities
•Residual sedation is the most frequent cause of delayed awakening in the PACU
•If residual effects of opioids are a possible cause, consider Narcan
•IF inadequate reversal of NM blockade is a possible cause, consider additional dose of reversal agent
Consider other causes
possible causes for delayed awakening:
•Residual drug effects
Opioids
NM Blockade
Benzodiazepines
Anticholinergics
Alpha agonists
•Hypothermia
•Hypoglycemia
•Electrolyte disturbances
•Hypoxemia
•Increased ICP- Cerebral hemorrhage
•Air embolism
Transport to PACU
•Remain at the head of the bed during transport to PACU, and continuously observe the patient’s airway, ventilation, and overall condition
•Monitor BP, SpO2, EKG- if travelling farther distances
•Consider supplemental O2
•Consider recovery in lateral position (prevent aspiration, and upper airway obstruction)
•Medications and airway equipment should be available during transport if the patient is unstable or if transport is a long distance
•Upon handoff to PACU RN, provide a concise, thorough summary of the patient’s medical history, intraoperative course, postop condition, and current therapy
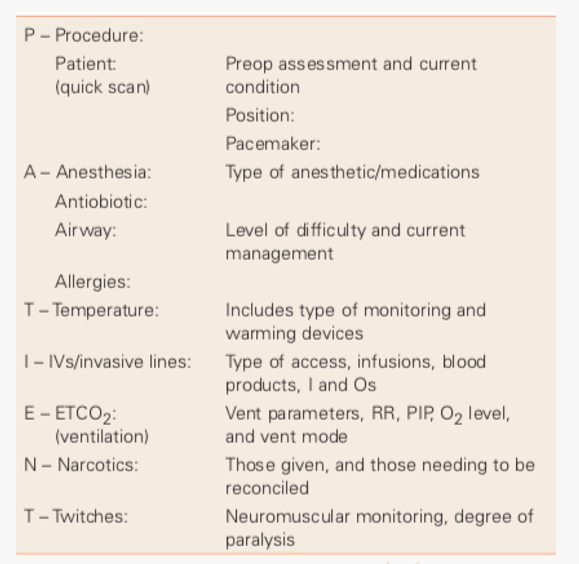
PATIENT mnemonic for hand off to PACU