Cdiff/Osteomyelitis
1/15
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
16 Terms
Cdiff Organism and Pathophysiology
gram neg hardy spore-forming anaerobic rod
hand washing > hand sanitizer
gastric acid, bile acid, healthy flora keeps Cdiff in check
active infection produces toxins A and B that disrupt epithelial barrier and causes inflammation and pseudomembrane
Cdiff Risk Factors
age>65
hospital duration
antibiotics (carbapenems, ciprofloxacin, clindamycin, cephalosporins, etc)
IBD/CKD/ESRD
chemotherapy/immunosuppressants
GI surgery/manipulation/tube feeds
acid suppression (PPI)
complications/mortality risk factors- older age, leukocytosis, renal failure, comorbidities, etc
Cdiff S/S
non bloody watery diarrhea (>3/day), abdominal pain, leukocytosis, fever
complications toxic megacolon, rCDI, mortality
only test if s/s and confident Cdiff since part of normal flora (diagnostic stewardship), do not treat if no need to test
do not use antidiarrheals
Cdiff Classification
non severe
WBC=<15k
SCr =<1.5
hemodynamically stable
severe (just one of following)
WBC not 4-15k,
SCr>1.5 or 50% increase
fulminant (just one of following)
toxic megacolon
ileus
shock
Cdiff Dx Testing
NAAT high sensitivity tests for toxin gene
GDH high sensitivity tests for Cdiff prescence
toxin moderate specificity tests toxin A and B
GDH and toxin test (both positive or negative treat or do not treat)
If GDH positive but toxin negative do NAAT (treat if NAAT positive)
Cdiff Treatment Options
fidaxomicin- more specific, less dosing, reduces rCDI, $$ (no clinical difference in treatment)
vancomycin- must be PO because IV does not get to colon
metronidazole- ileus only
fecal microbiome transplant (FMT)
Cdiff Treatment Algorithm
initial Cdiff
fidaxomicin 200mg BID PO x 10days
alternative vancomycin 125mg QID PO x10 days
fulminant
vancomycin 500mg QID PO and add IV metronidazole 500mg q8hr if ileus present, can also add rectal vanc
rCdiff
try something new (standard vanc, pulsed vanc, standard fidaxomicin, eventually fecal microbiota transplant FMT)
long term suppression for patients who are not candidates for FMT, relapsed after FMT, or require ongoing frequent antibiotics
oral vanc 125mg PO QD
Osteomyelitis Pathogens
S. aureus (main pathogen)
Salmonella (Sickle cell pts)
fungi (immunocompromised pts)
can cover empirically but culture for specific coverage
Osteomyelitis Types
hematogenous (through bloodstream)
pediatric AHO
NVO in older patients
worsening back/neck pain, fever, inflammatory markers, obtain blood cultures/aspiration biopsy before antibiotics unless sepsis or extremely ill
contiguous (adjacent soft tissue infection and vascular insufficiency)
acute vs chronic with sequestrum less systemic signs but easier to visualize
dx DFO through Xray/MRI, inflammatory markers, and BeBoP, 3O not systemic 4O systemic
direct inoculation
DFO MRSA Risk Factors
hx of MRSA
antibiotic exposure
invasive procedures
open wounds
HIV infection
hospitalization/ICU
hemodialysis
DFO Pseudomonas Risk Factors
soacking feet
macerated ulcer
failed previous antibiotic therapy w/o coverage
severe infection
DFO Anaerobic risk factors
chronic foot ischemia leading to necrosis
DFO Patient Populations
adults cover S. auerus
PWID cover S. auerus and Pseudo
post-op/trauma/vascular insufficiency cover pos and neg
necrosis cover anaerobes
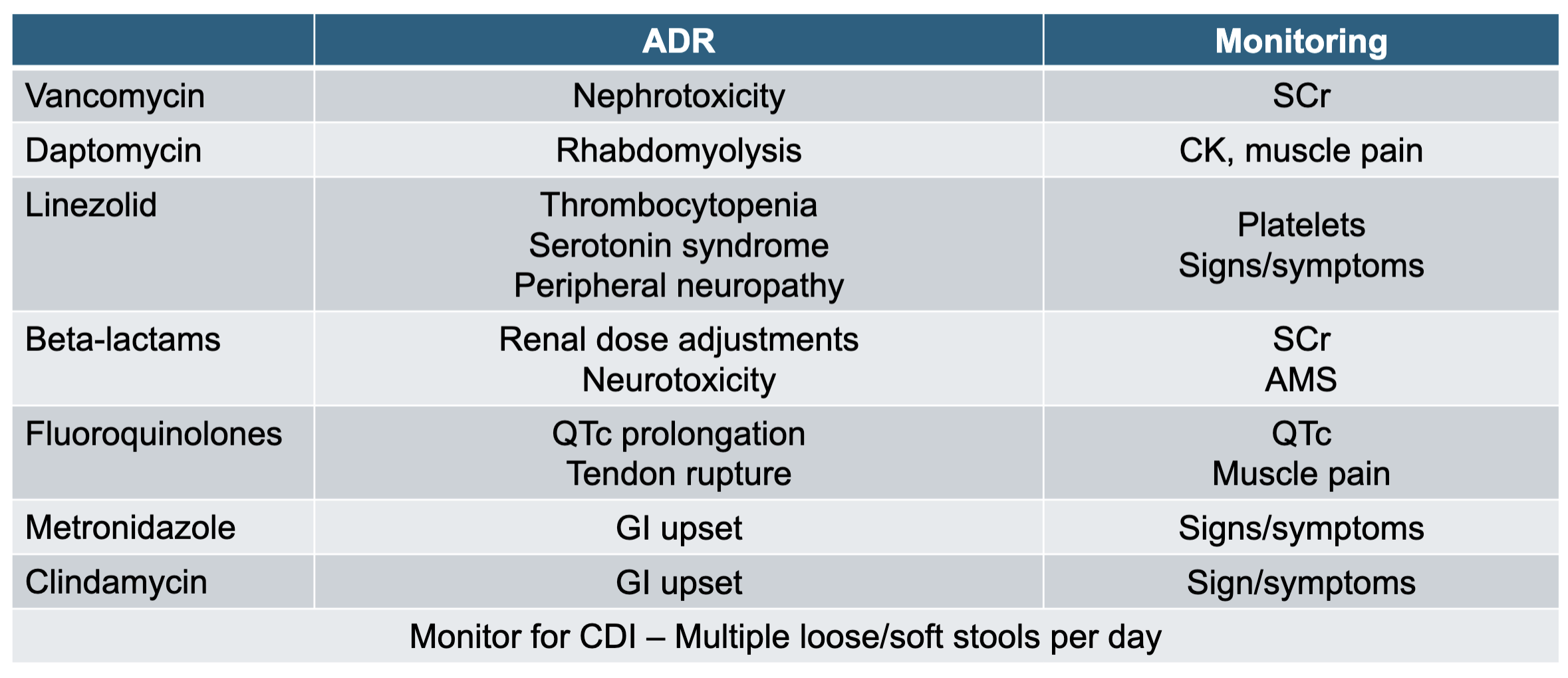
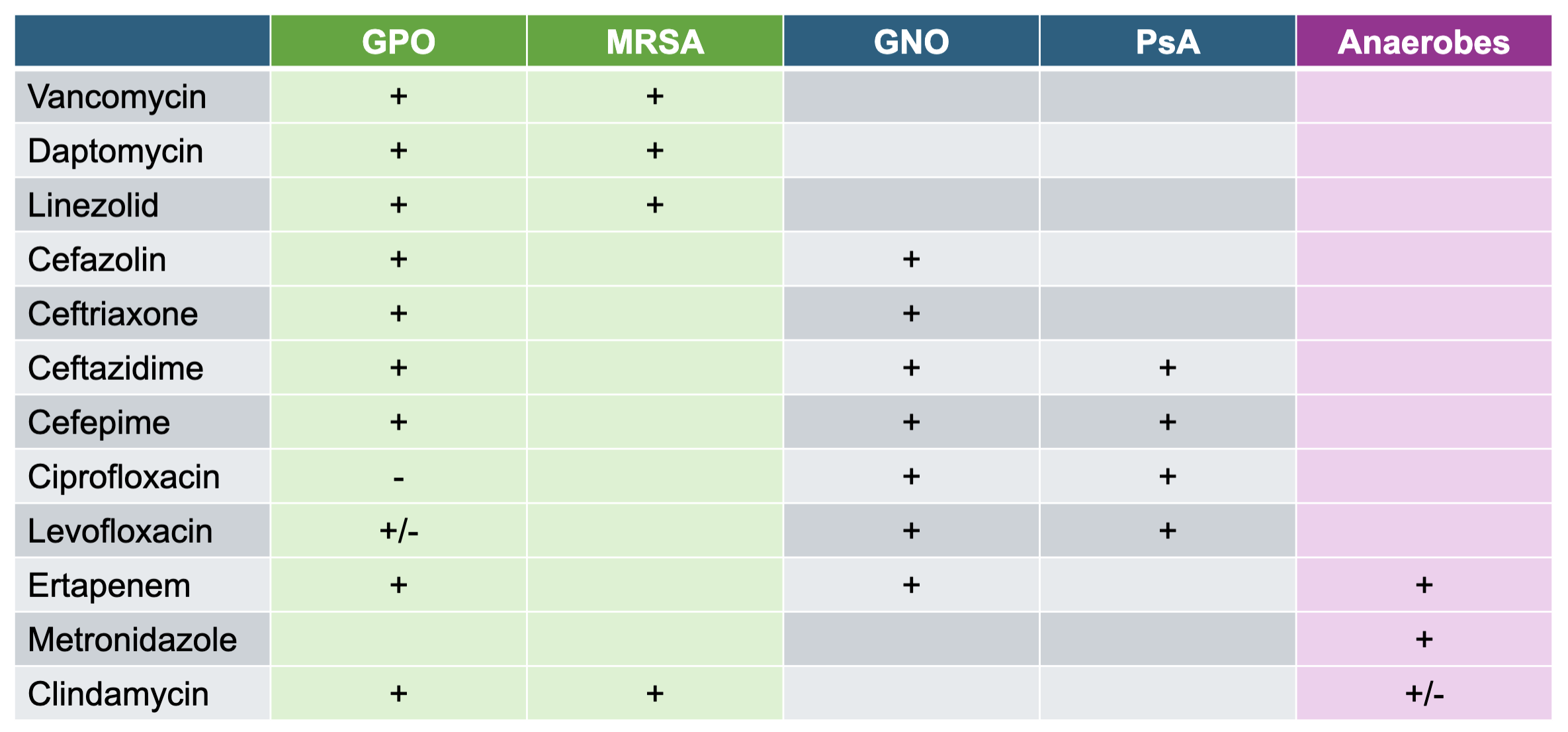
Antibiotics
MEMORIZE +/- TABLE and MONITORING TABLE
Duration of Therapy
usual course 4-6 wks, if completely debrided with margins after bone resection can do 3 wks
OPAT
IV at home, check for insurance, patient ability/comfort, electricity/refrigeration, and no concerns for misuse