Platelets, Viscosity, and Hemostasis
1/19
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
20 Terms
Where do platelets originate from?
They originate from megakaryoblasts from the myeloid lineage
Megakaryoblasts break into hundreds of fragments, which are the platelets
What are the platelets function?
They are involved in the clotting of blood
What is viscosity? What is the viscosity of blood determined by?
Viscosity is the resistance to flow
The viscosity of blood is determined by:
The number of erythrocytes (RBCs)
The amount of albumins (proteins)
What is Hemostasis? (not homeostasis)
The reduction and stoppage of blood loss from a damaged blood vessel
What are the three mechanisms of Hemostasis?
Three Mechanisms of Hemostasis:
Vascular spasm
Platelet plug formation
Blood clotting (coagulation)
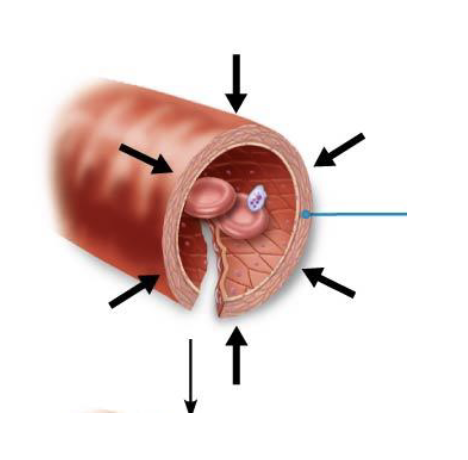
Describe the Vascular Spasm mechanism
The first response to a damaged blood vessel
The smooth muscle contracts in response to a cut in the blood vessel, which reduces blood flow loss (short term)
This helps prevent excessive blood loss until the other longer term mechanism takes effect
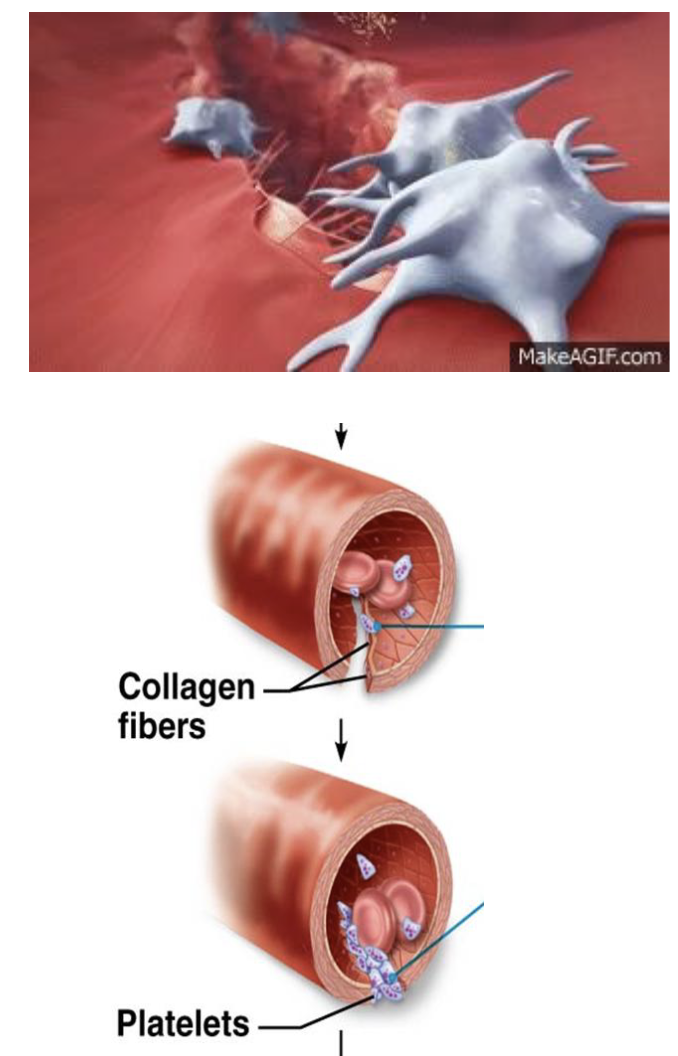
Describe the Platelet Plug Formation mechanism
Broken tissue releases chemicals that attracts platelets
Platelets change shape and extend projections to stick onto the broken tissue, forming a platelet plug
This mechanism is also short term, stopping blood for a few hours
Describe the Blood Clotting Mechanism Pathways
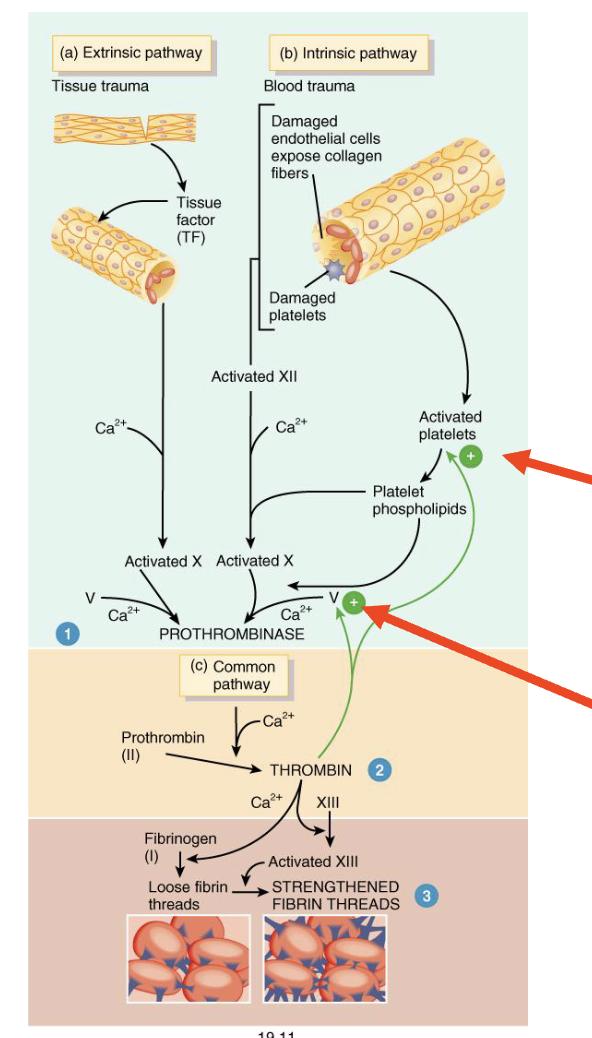
Blood clotting has two pathways:
Extrinsic Pathway: the tissue is damaged externally, with blood leaving the blood vessel (faster process)
Intrinsic Pathway: the tissue is damaged internally, with blood not leaving the blood vessel
Describe the Extrinsic Pathway Steps
Tissue damage with bleeding has occurred
Damaged tissues & platelets collect at the wound site and releases “tissue factor” (thromboplastin)
Thromboplastin converts a plasma protein into factor X (clotting factor)
Factor X becomes Prothrombinase
Describe the Intrinsic Pathway Steps
Tissue is damaged internally
This damage exposes the connective tissue of blood vessel
Platelets collect at the wound site then break down, releasing Platelet Factor 3
Platelet Factor 3 activates Factor XII, which converts Factor X into prothrombinase
What is the Common pathway and describe the steps
Past prothrombinase, the pathway is the same
5. Prothrombinase converts Prothrombin into thrombin
6. Thrombin converts fibrinogen into fibrin
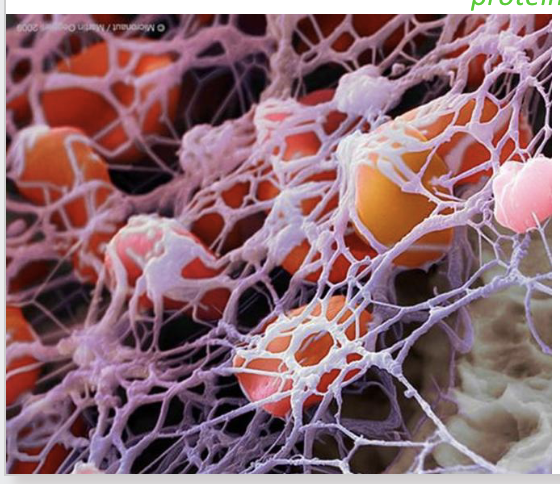
7. Fibrin forms a net like structure across the wound, which traps platelets and red blood cells, forming a clot
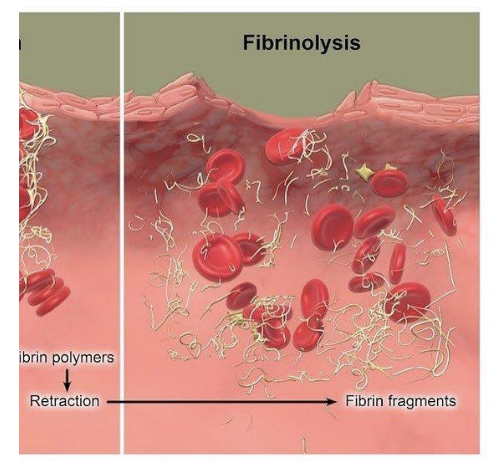
What is Clot Retraction?
As the clot retracts, it pulls the edges of the damaged blood vessel closer together
The Disorders of Hemostasis (Haemostasis)
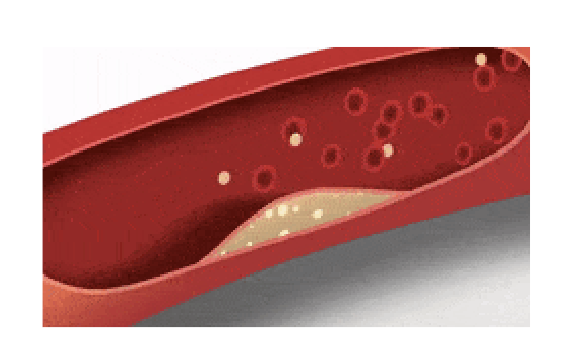
Thrombus: a blood clot forms in an unbroken blood vessel, which can potentially obstruct blood flow
Embolus: a detached mass that flows through the blood (ex: thrombus)
Hemophilia (haemophilia): a genetic condition where blood does not clot
How does our body prevent blood clotting?
Our body has chemical inhibitors to avoid blood clots called Anticoagulants
Antithrombin & Heparin (examples)
What type of feedback is blood clotting?
Positive Feedback
Why doesn’t blood clotting spread?
Once the clot forms, almost all thrombin is bound to the fibrin it forms, preventing it from being released into the blood stream
How do we get rid of blood clots?
Through fibrinolysis
The enzyme plasmin degrades fibrin, which breaks down the blood clot
Why is Vitamin K important for blood clotting?
It stimulates the liver to produce prothrombin and other clotting factors
What are Anticoagulent drugs?
Used to delay or prevent undesirable blood clots
Examples include: Heparin & Aspirin
What are Thrombolytic Agents?
Substances that dissolve formed blood clots
Works by turning plasminogen into plasmin
Plasmin then breaks down the blood clot through fibrinolysis