The Temporomandibular Joint
1/177
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
178 Terms
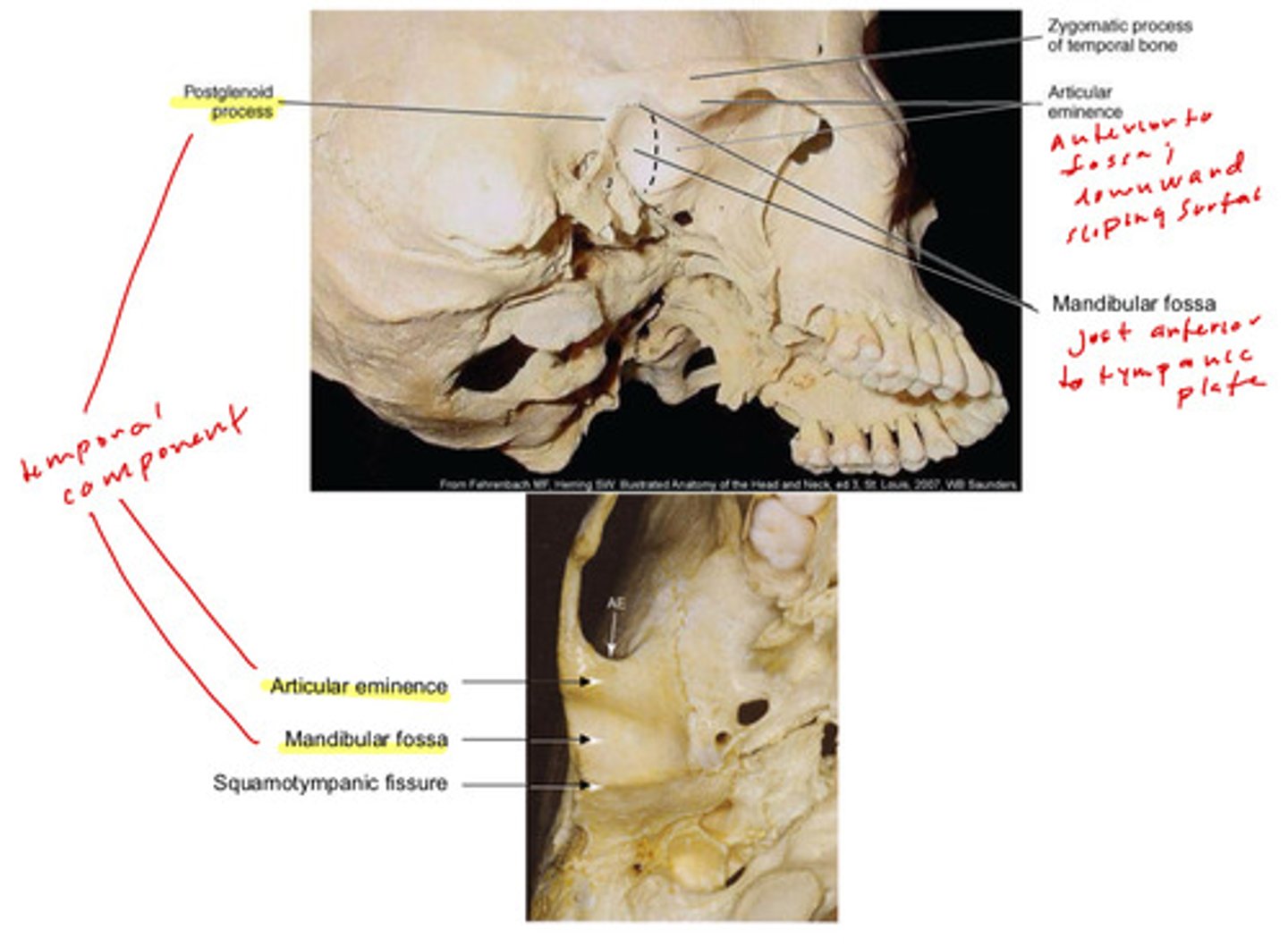
what are the temporal components of the TMJ (5)
1) postglenoid process
2) articular eminence
3) mandibular fossa
4) squamotympanic fissure
5) zygomatic process of temporal bone
what are the notable mandibular components of the TMJ (5)
1) articulating surface of condyle
2) condyle of mandible (head and neck)
3) medial pole of condylar process
4) lateral pole of condylar process
5) mandibular notch
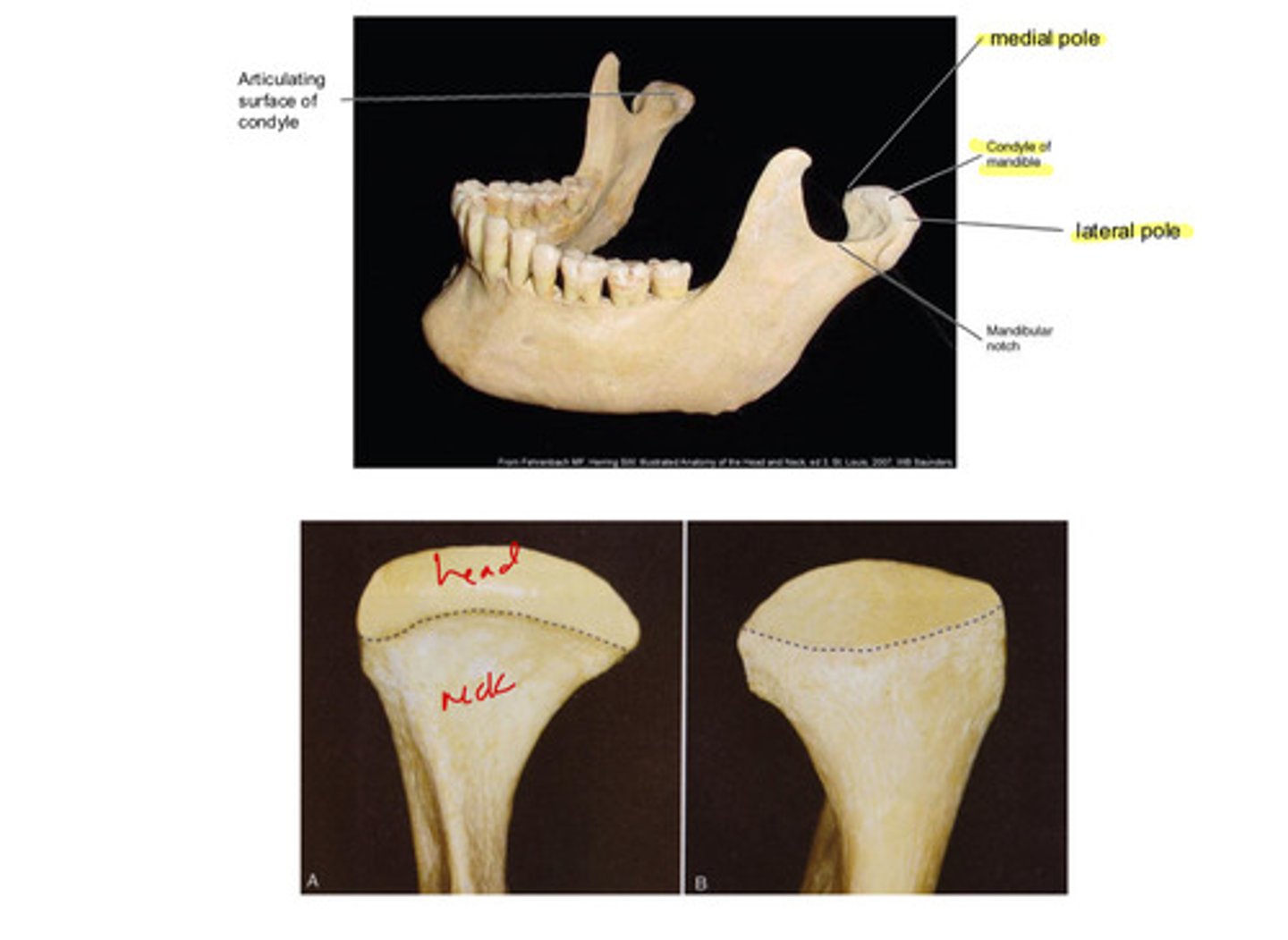
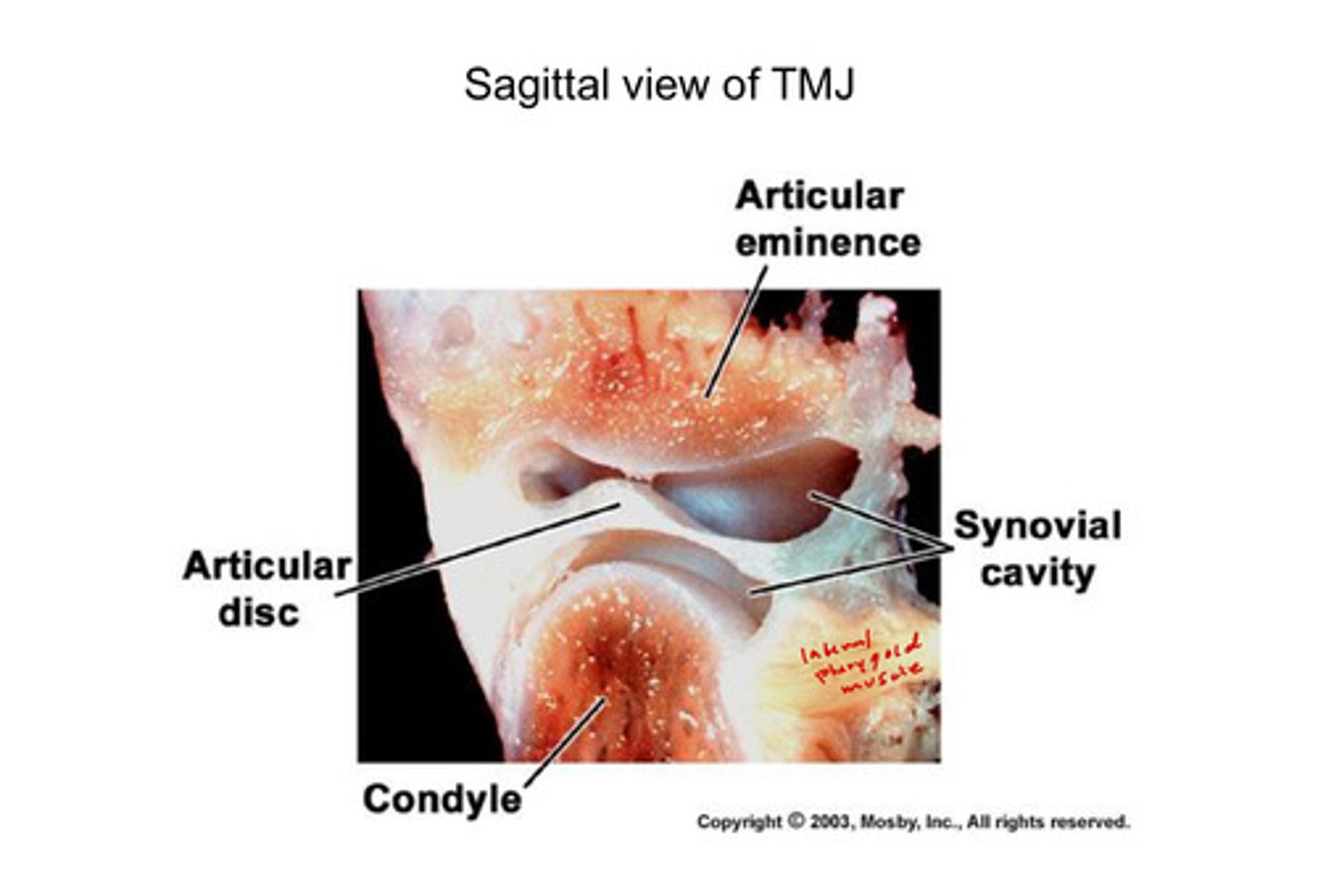
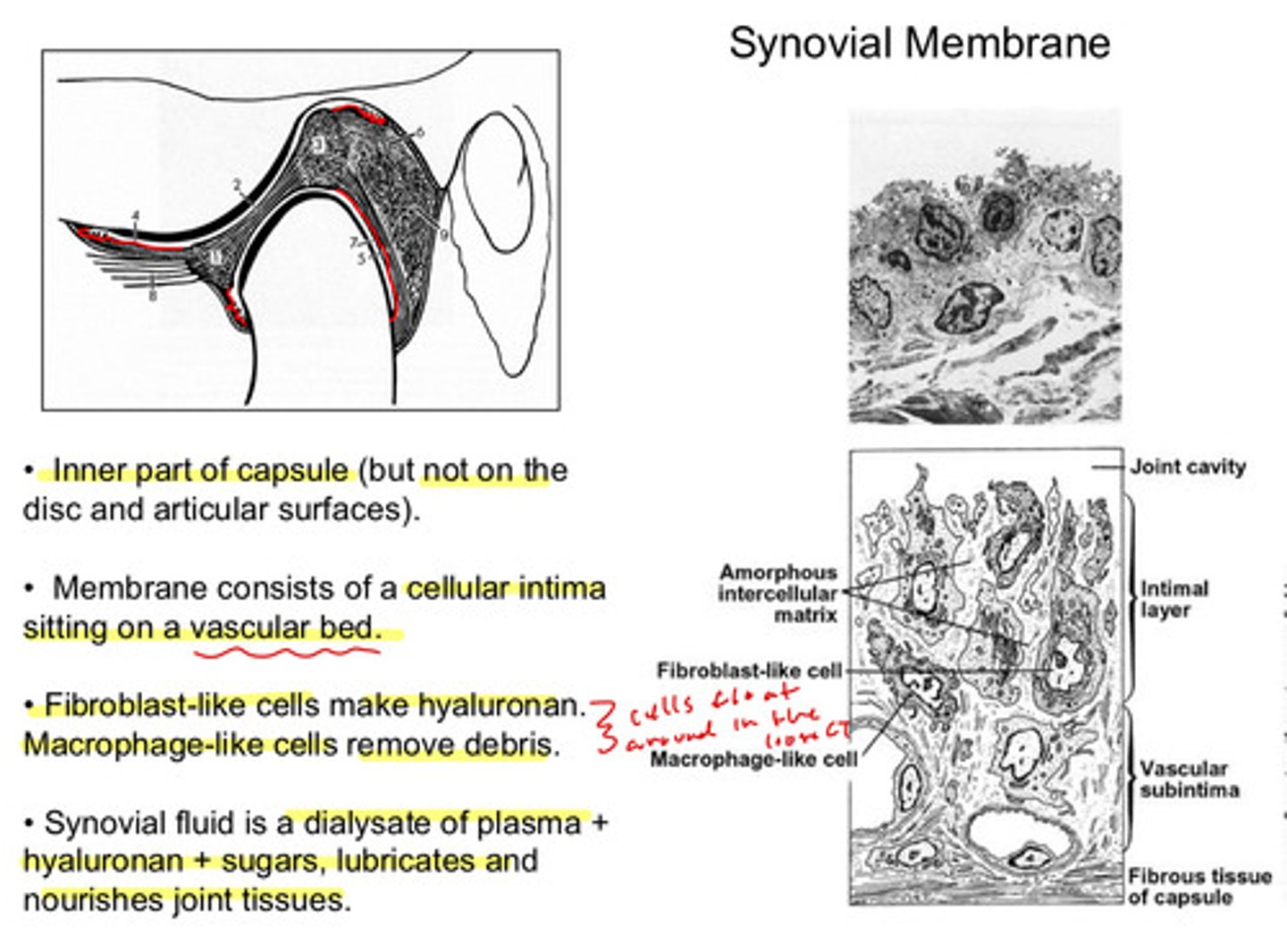
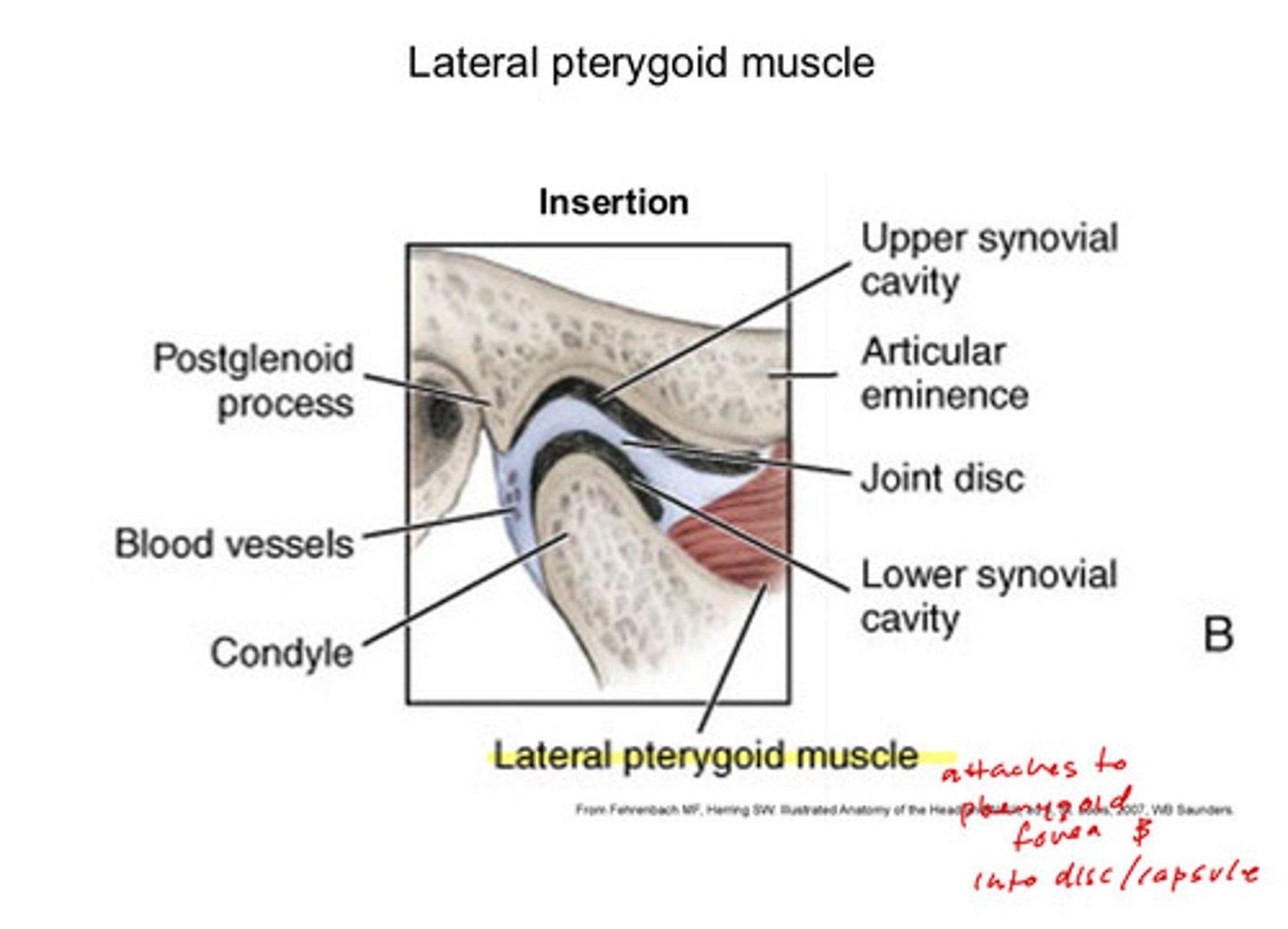
image of sagittal view of TMJ
note that you can see the superior and inferior synovial cavities; the lateral pterygoid muscle is also visible
in the middle of the TMJ, what are the 4 zones that you can see of the adult mandibular condyle?
first you see the articular disk with the inferior joint cavity underneath
1) articular zone: fibrous; adjacent to joint cavity; composed of dense fibrous CT
2) proliferative zone: mainly cellular; has many undifferentiated cells but in an adult, it is inactive
3) fibrocartilaginous zone: chondrocytes embedded in fibrous matrix
4) calcified cartilage: partially mineralized cartilage
and underneath is the subarticular bone
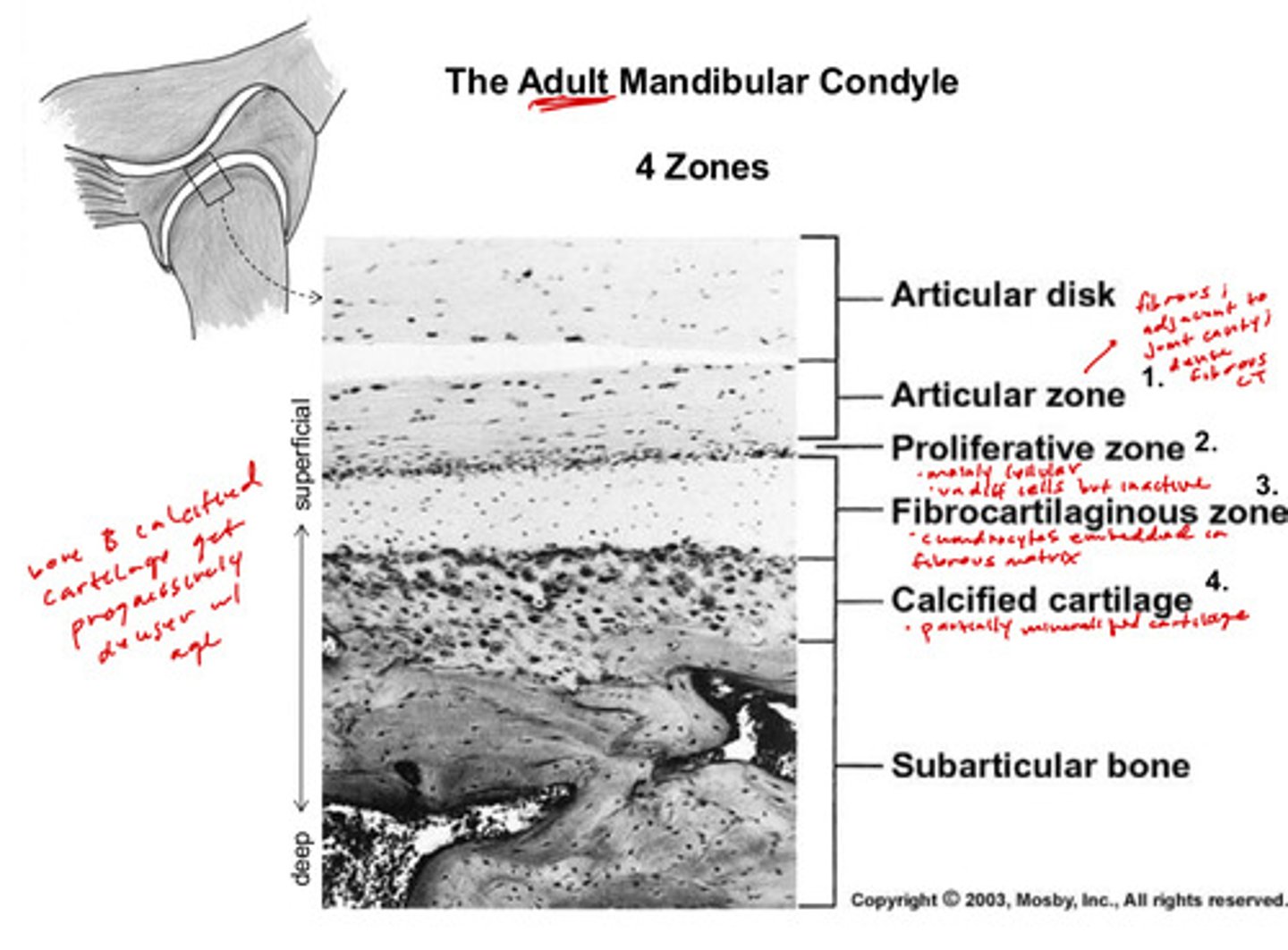
in the TMJ, the bony and calcified cartilage zones get progressively _______ with age
denser!
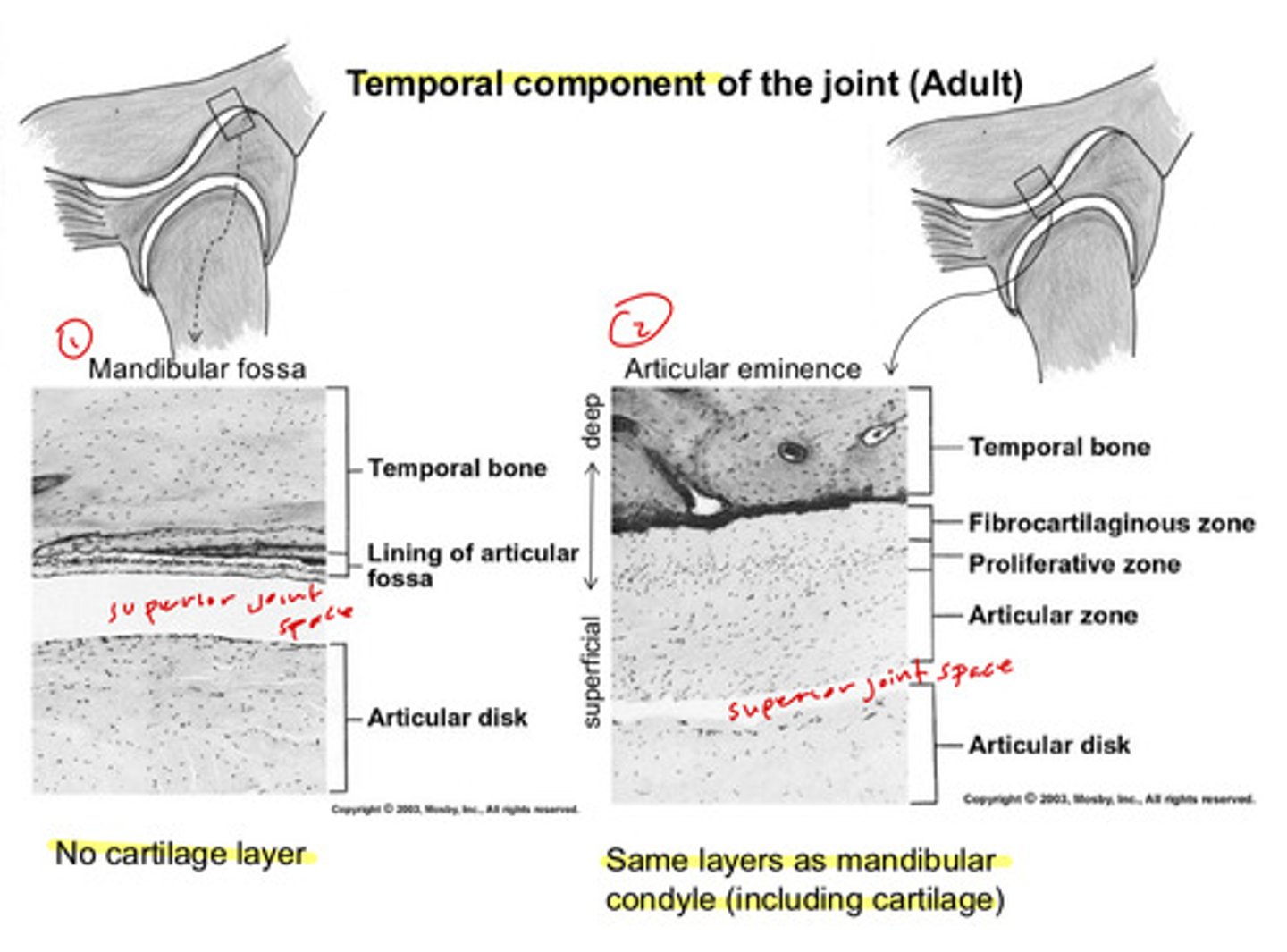
at the most posterior portion of the TMJ (at the mandibular fossa), what are the 3 areas that you can see of the temporal component of the adult joint
1) temporal bone
2) lining of articular fossa
superior joint space in between
3) articular disk underneath
there is no cartilage layer
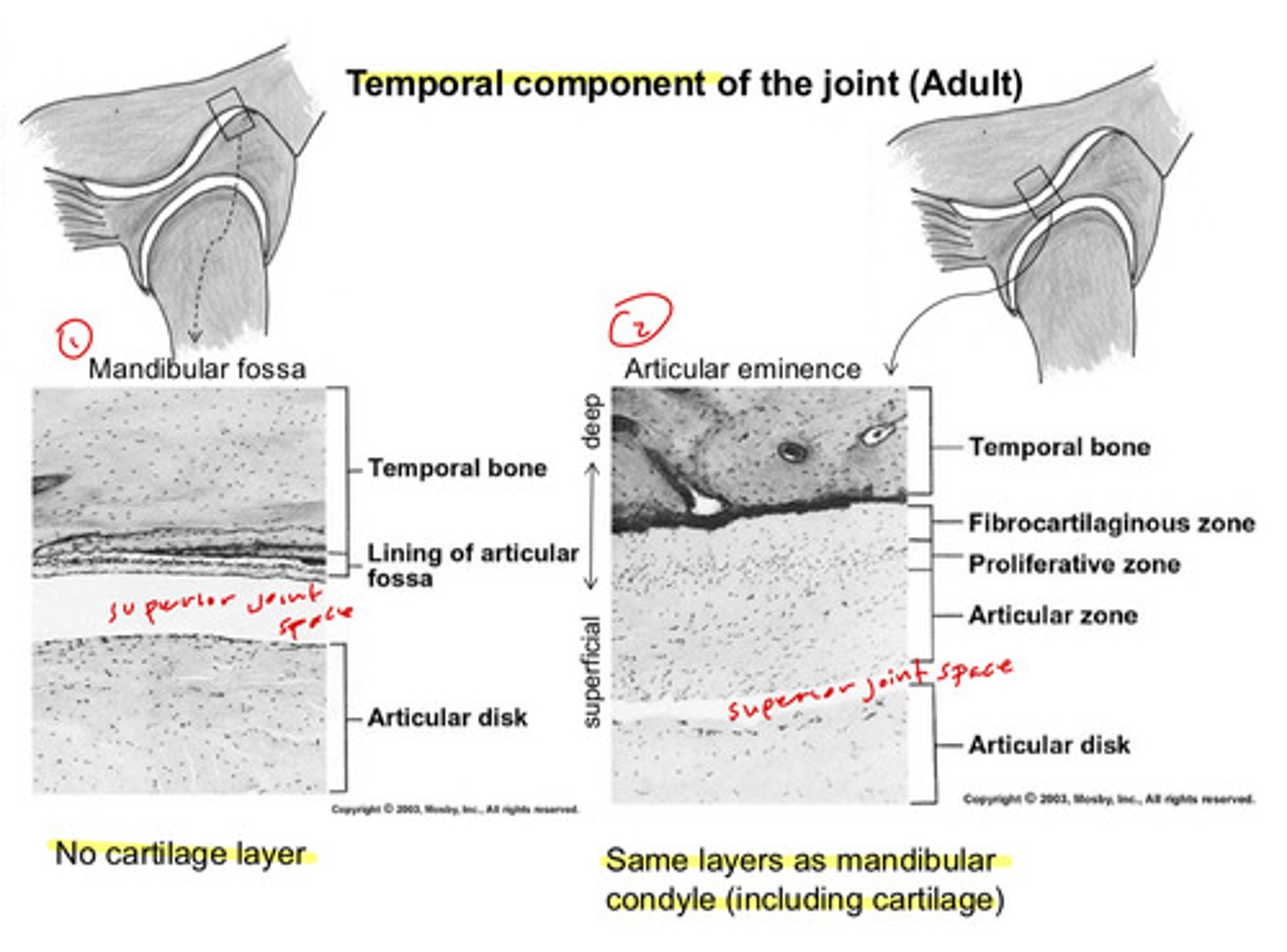
in the middle portion of the TMJ (at the articular eminence), what are the 5 areas/zones that you can see of the temporal component of the adult joint
1) temporal bone
2) fibrocartilaginous zone
3) proliferative zone
4) articular zone (again, adjacent to the joint cavity, but this time the superior joint space)
superior joint space in between
5) articular disk underneath
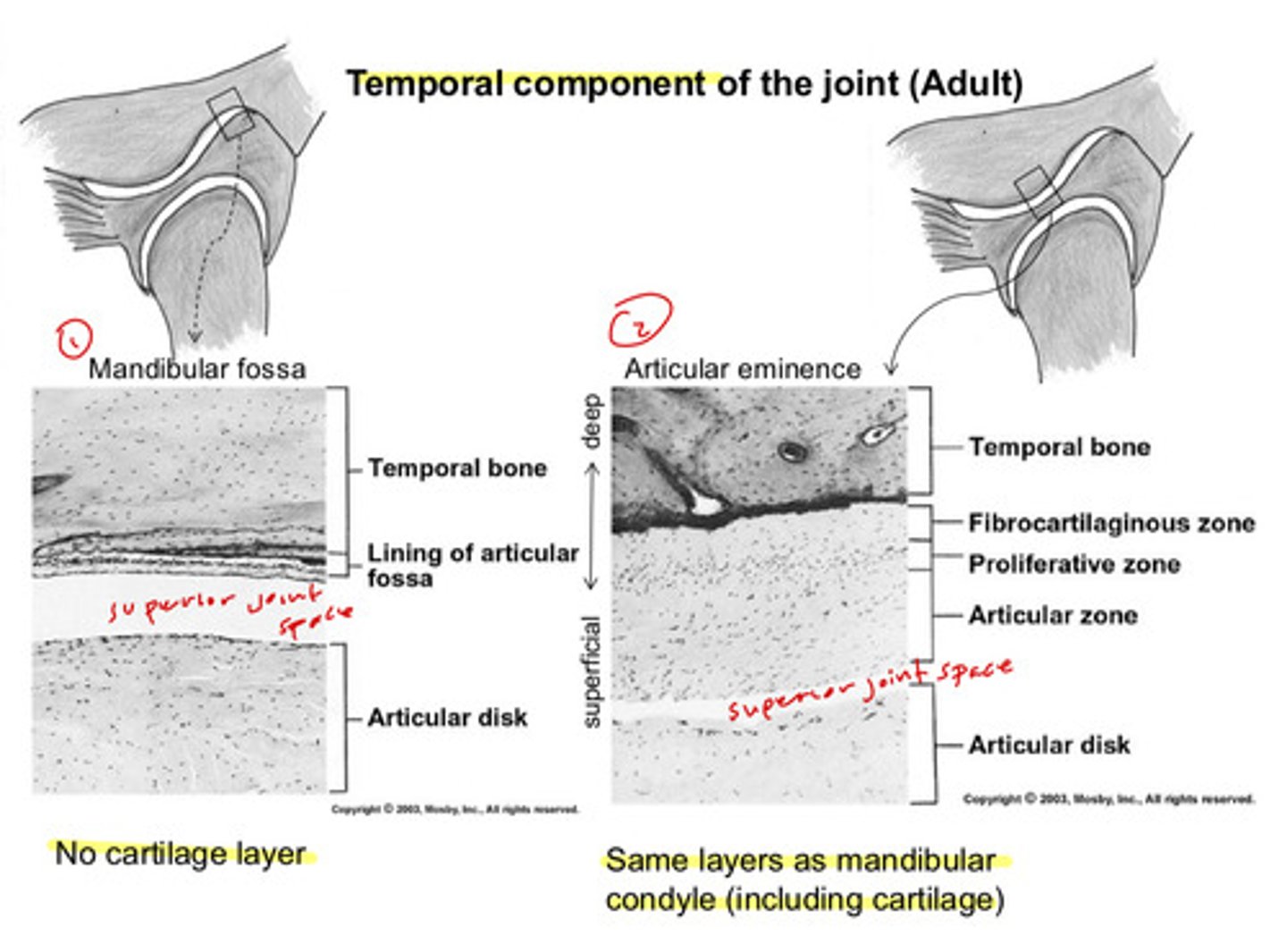
at the articular eminence of the temporal component of the adult joint, we see the _____ layers as the mandibular condyle, just in _______ orientation
same layers; opposite orientation
starting from whichever joint space (whether you are going in a superior orientation or an inferior orientation), the order is as follows:
1) articular zone closest to joint
2) proliferative zone next
3) fibrocartilaginous zone after
4) calcified cartilage zone adjacent to fibrocartilaginous zone
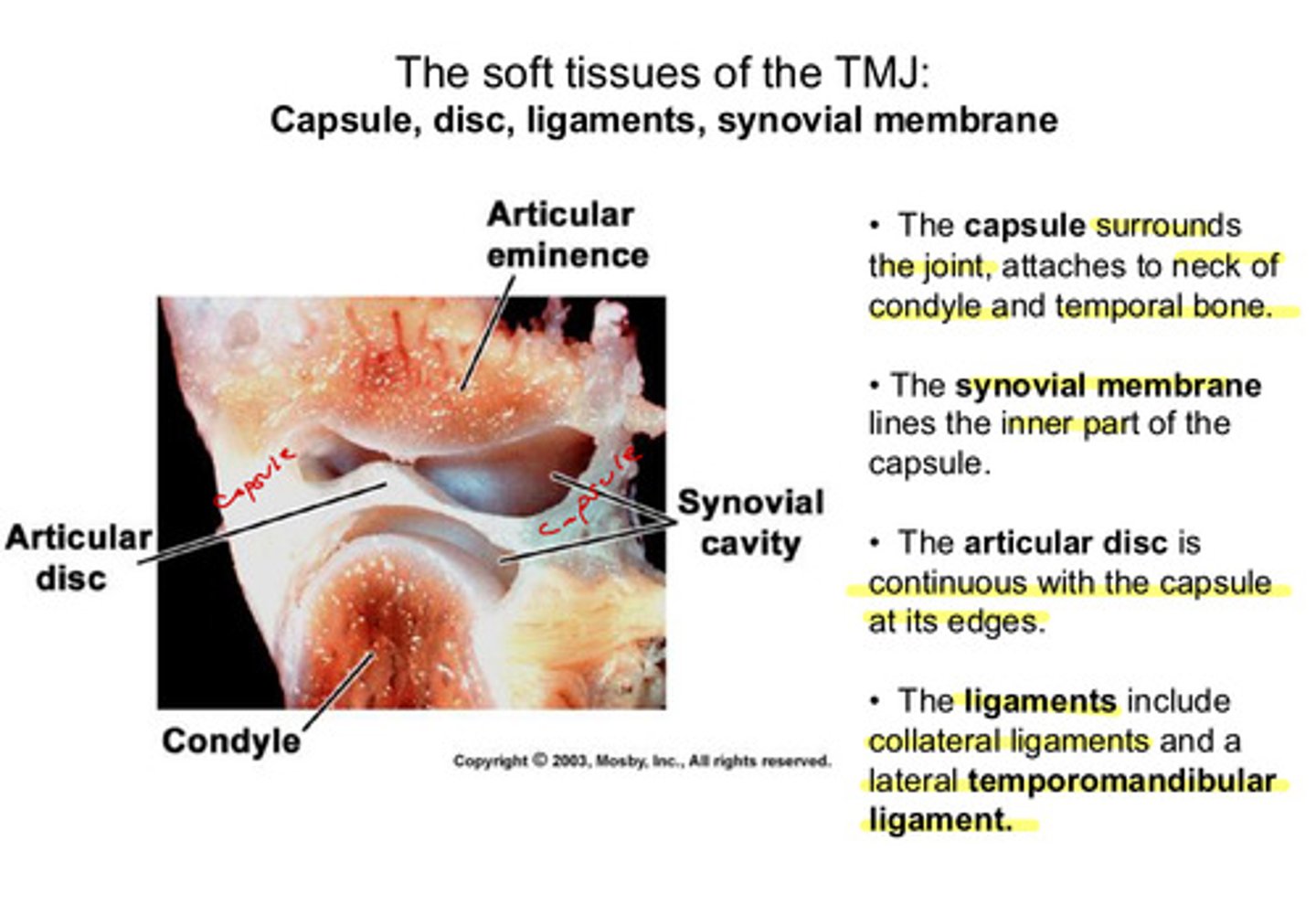
what are the 4 soft tissues of the TMJ
1) capsule
2) disc
3) ligaments
4) synovial membrane
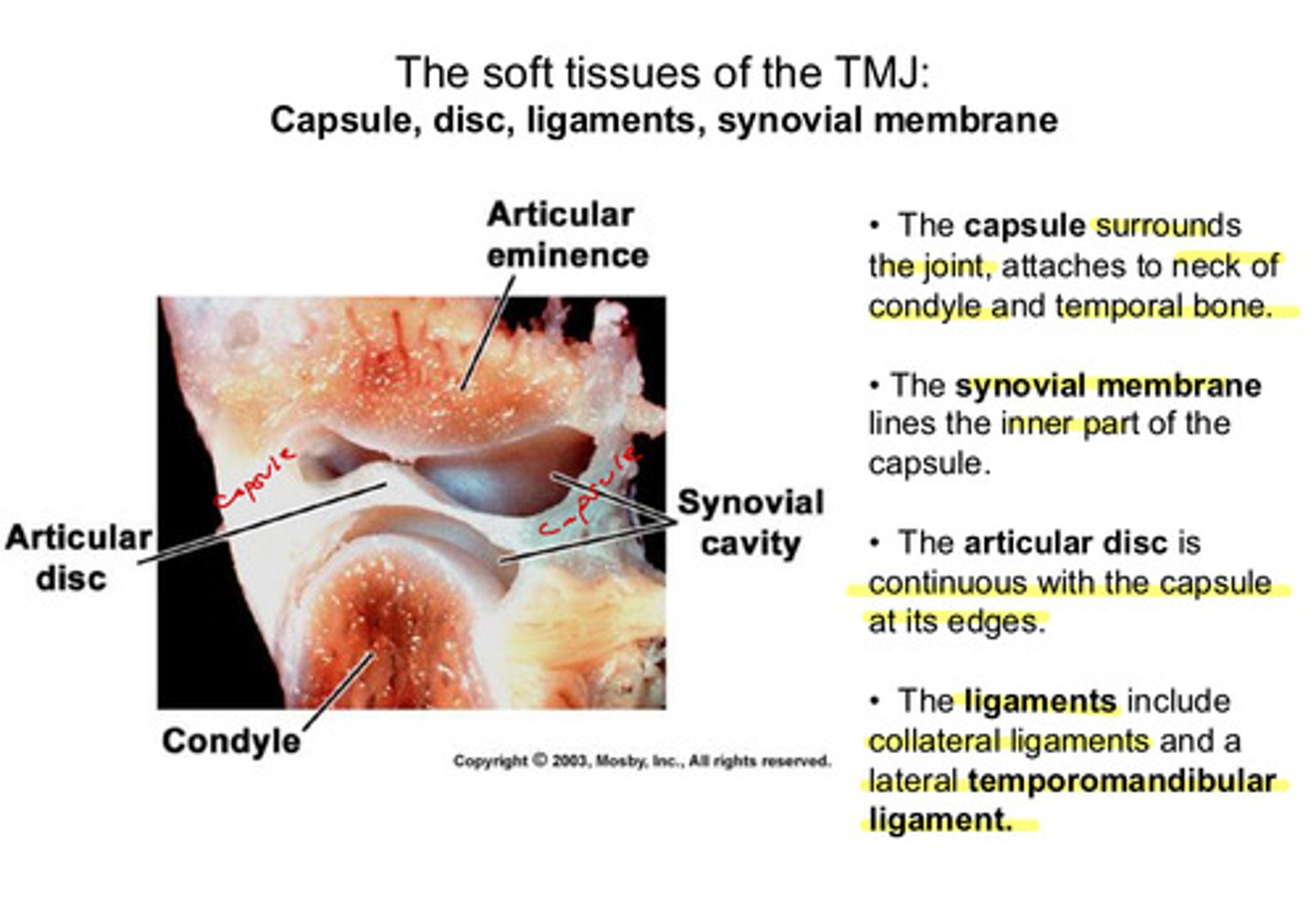
describe the location of the capsule
surrounds the joint, attaches to neck of condyle and temporal bone
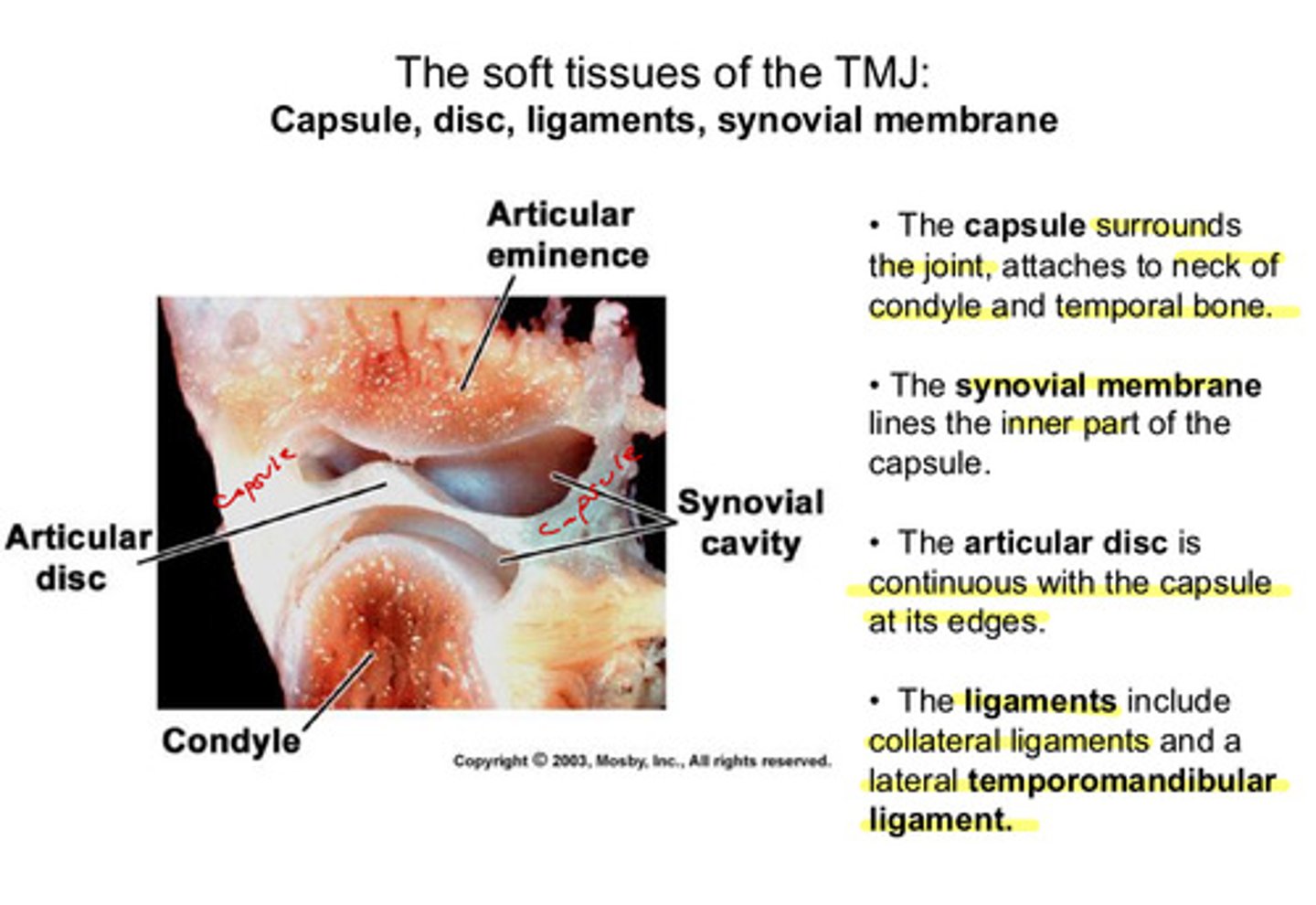
describe the location of the synovial membrane
lines the inner part of the capsule
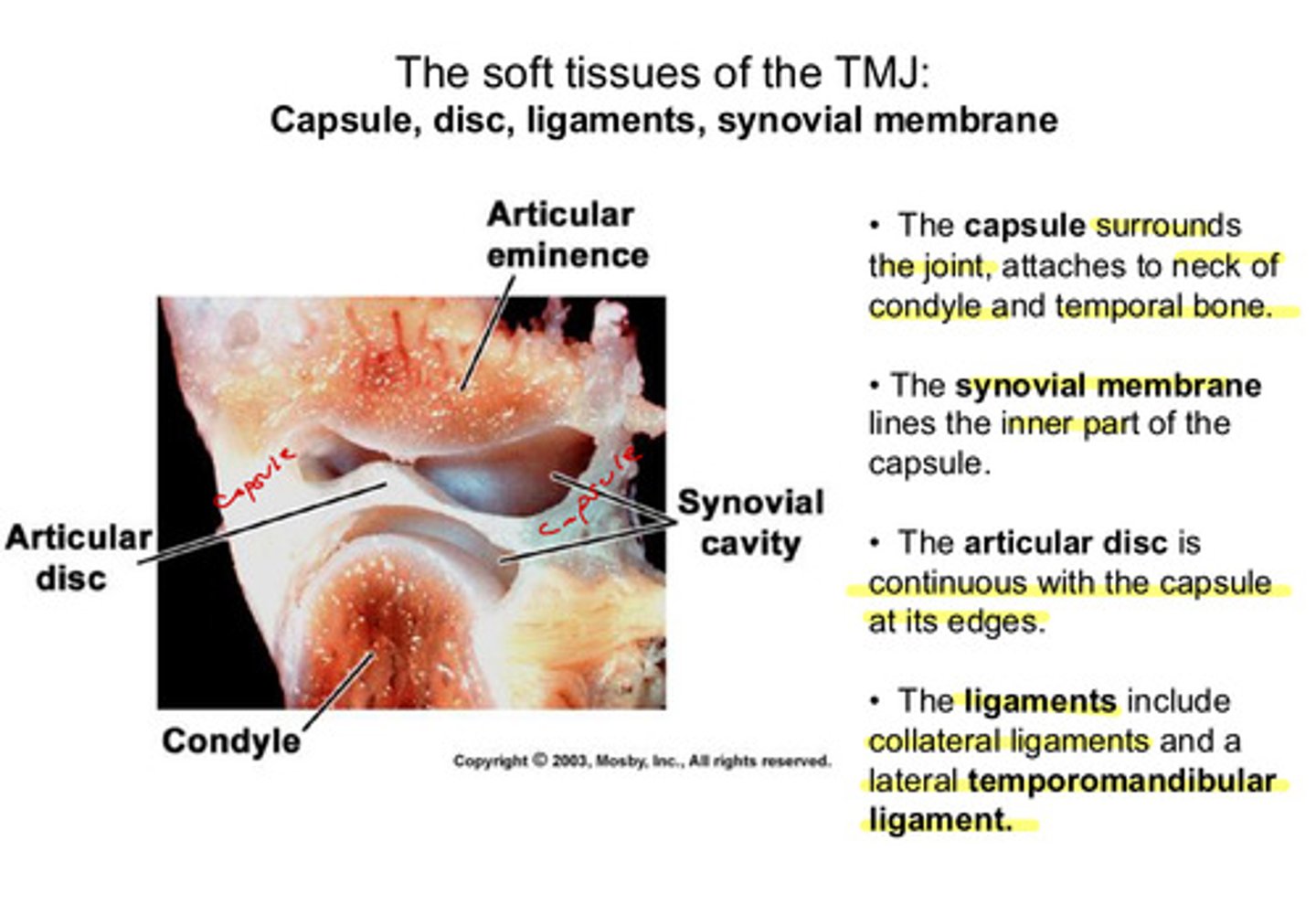
describe the location of the articular disc
continuous with the capsule at its edges; between the eminence and the condyle
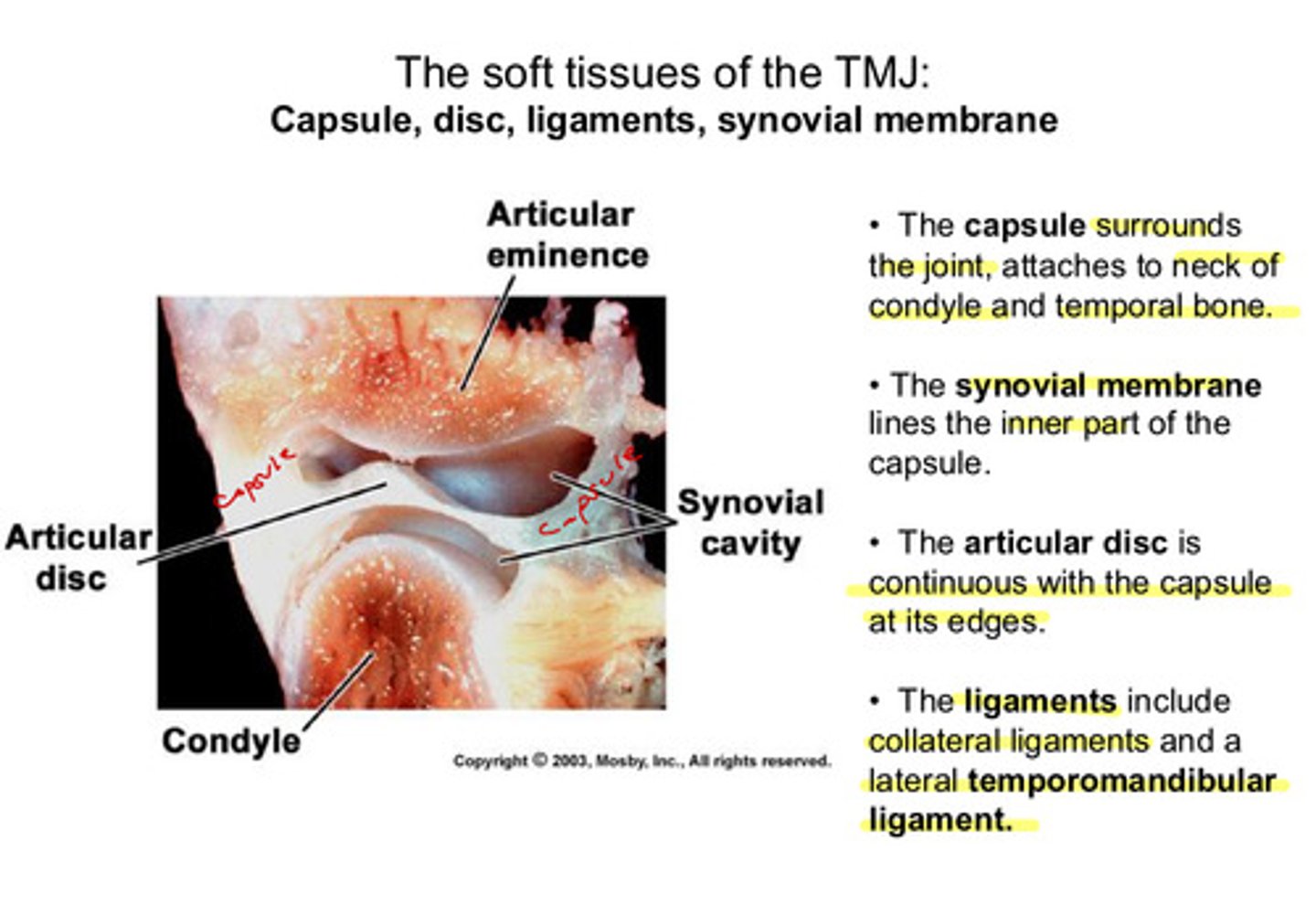
what are the ligaments involved in the TMJ (considered soft tissue)
collateral ligaments & a lateral temporomandibular ligament
the collateral ligaments (medial and lateral) attach where?
on the medial pole and lateral pole of the condyle, respectively
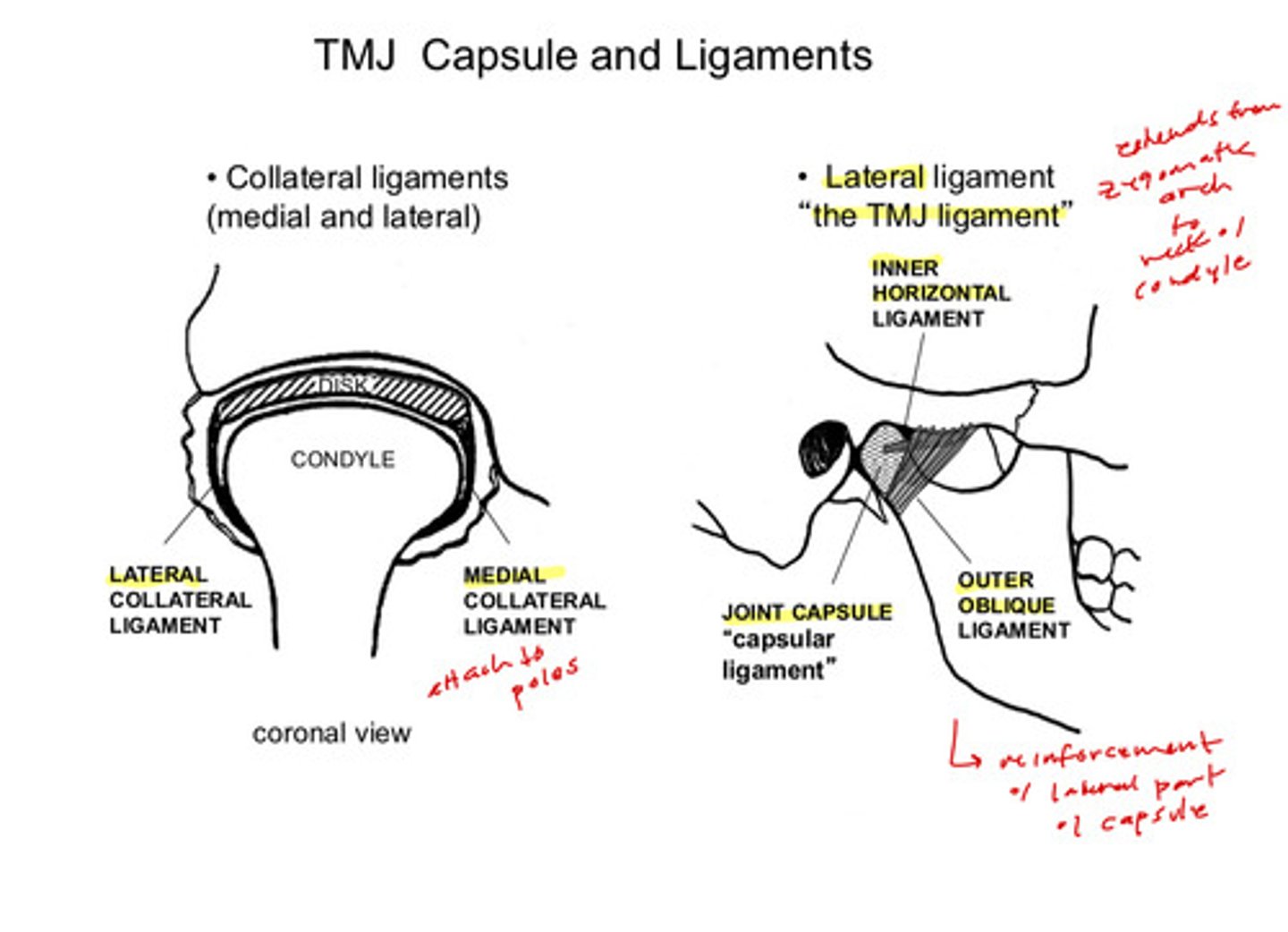
where does the lateral TMJ ligament attach and what does it help do?
extends from the zygomatic arch to the neck of the condyle; helps reinforce the lateral part of the capsule
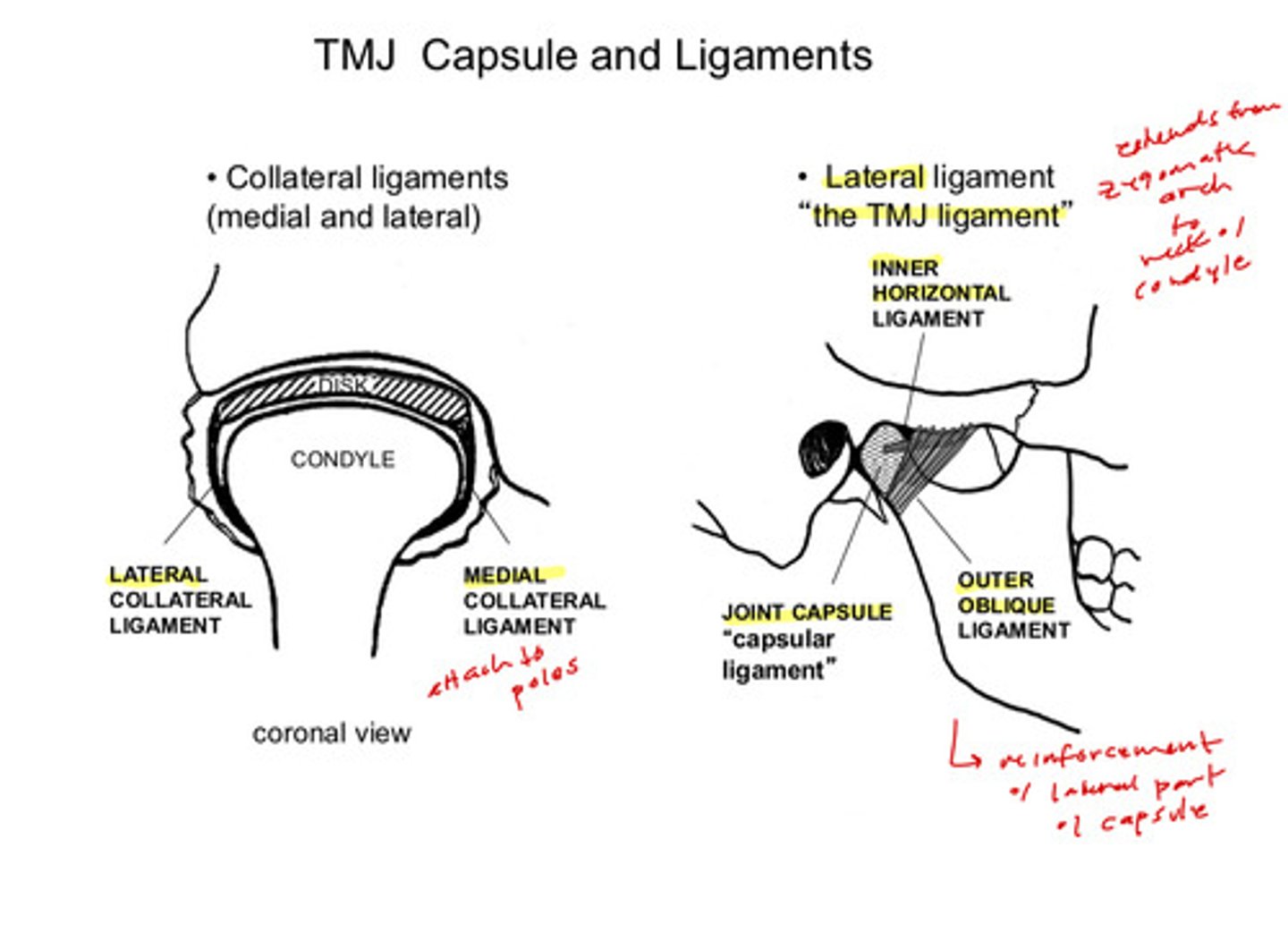
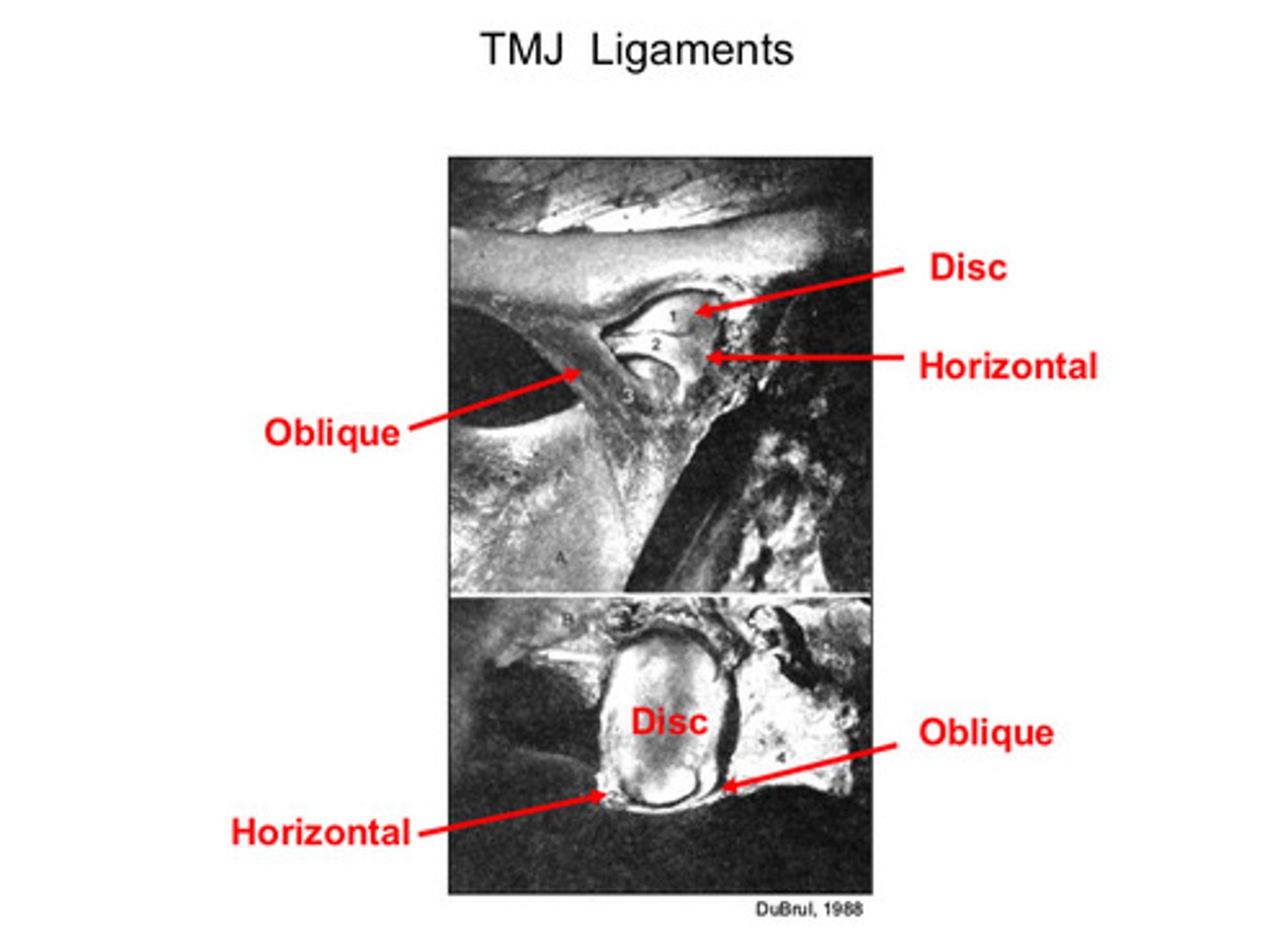
the TMJ ligament has 2 parts, what are they and which is larger
has an outer oblique ligament (larger) and an inner horizontal ligament (smaller)
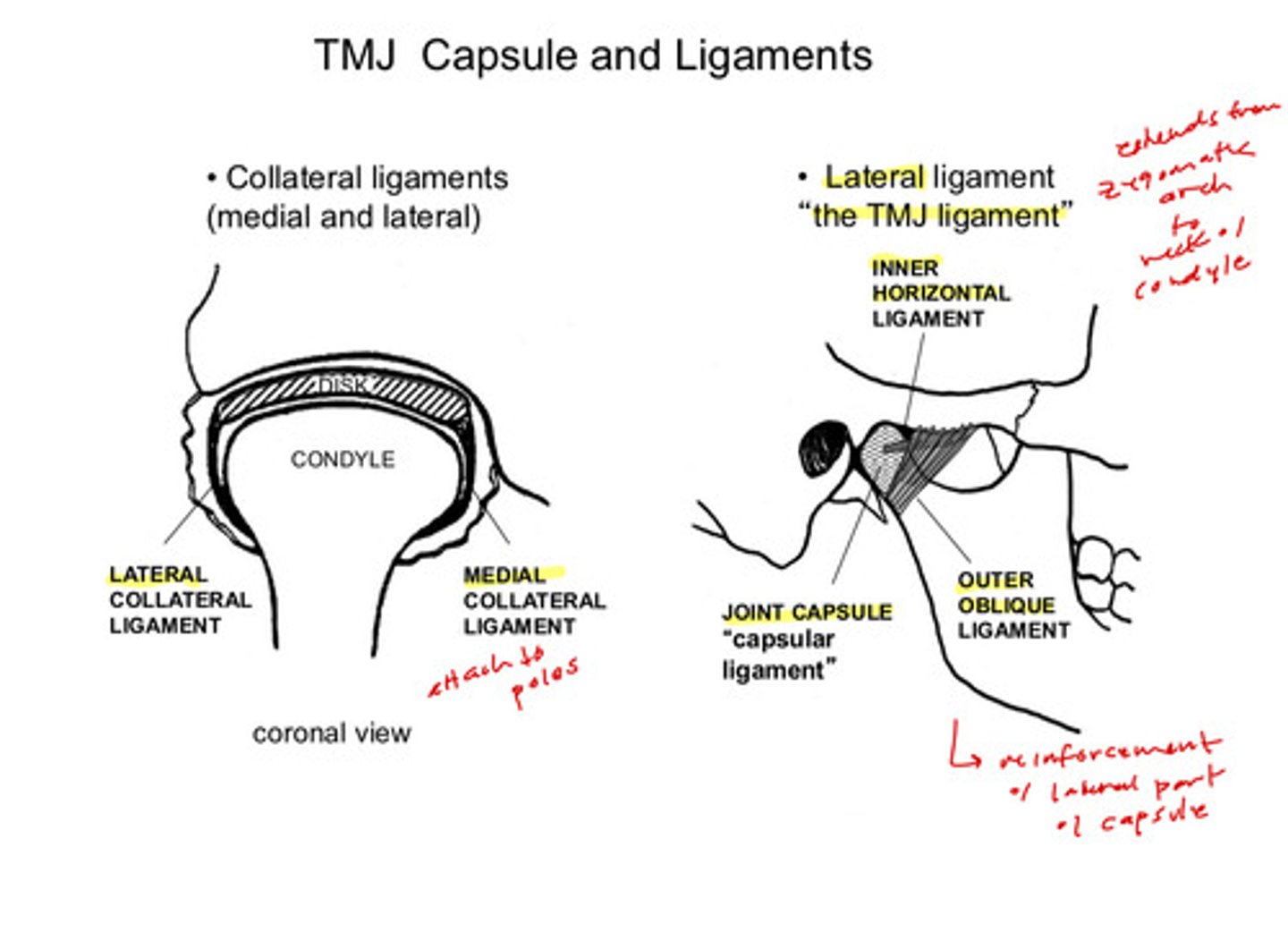
imaging of the TMJ ligaments
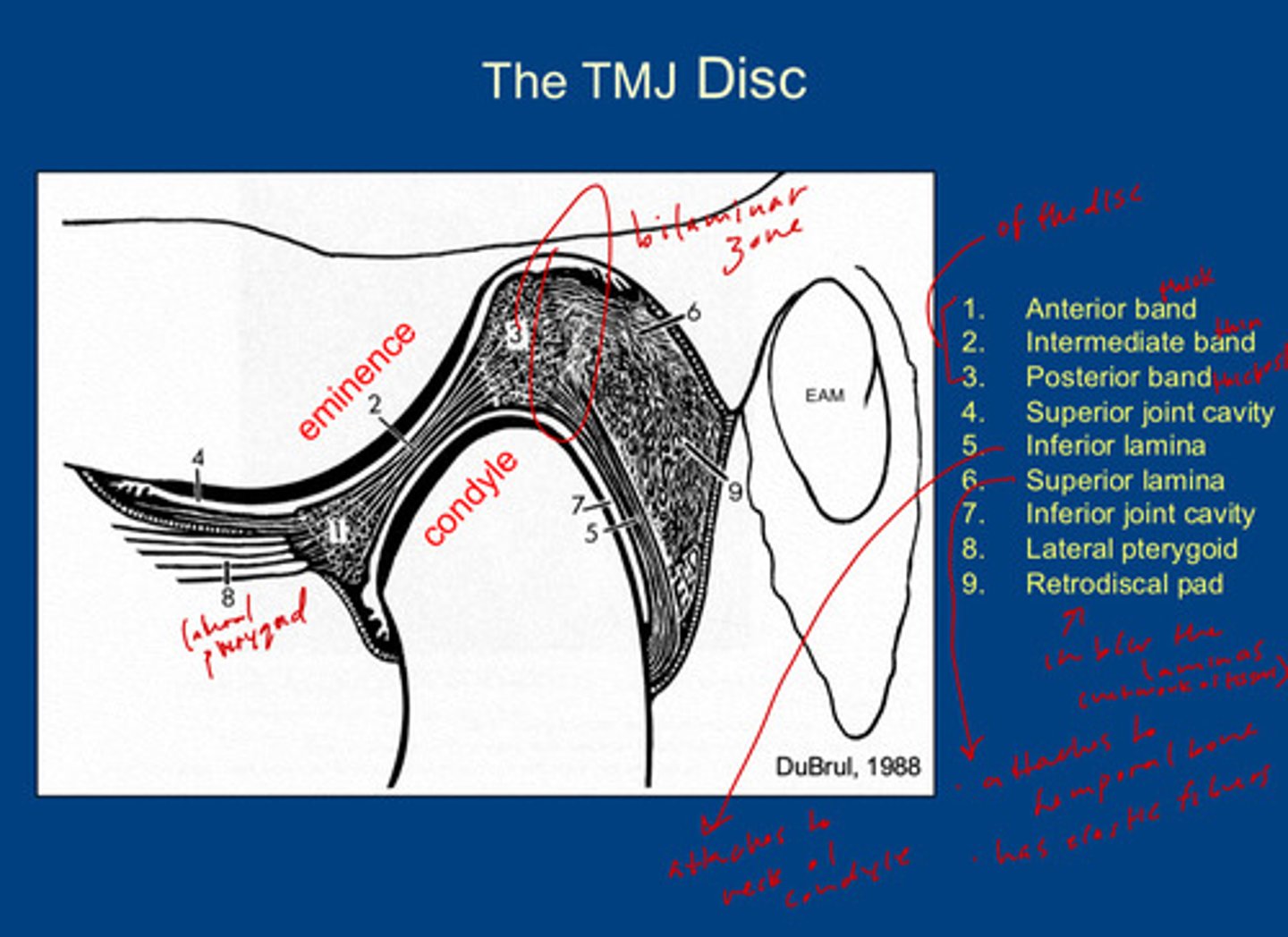
what are the 9 landmarks of the TMJ disc
1) anterior band of the disc (thick)
2) intermediate band of the disc (thinnest)
3) posterior band of the disc (thickest)
4) superior joint cavity
5) inferior lamina: attaches to the neck of the condyle
6) superior lamina: attaches to temporal bone; has elastic fibers
7) inferior joint cavity
8) lateral pterygoid muscle
9) retrodiscal pad: located between the inferior and superior lamina; acts as a network of tissues
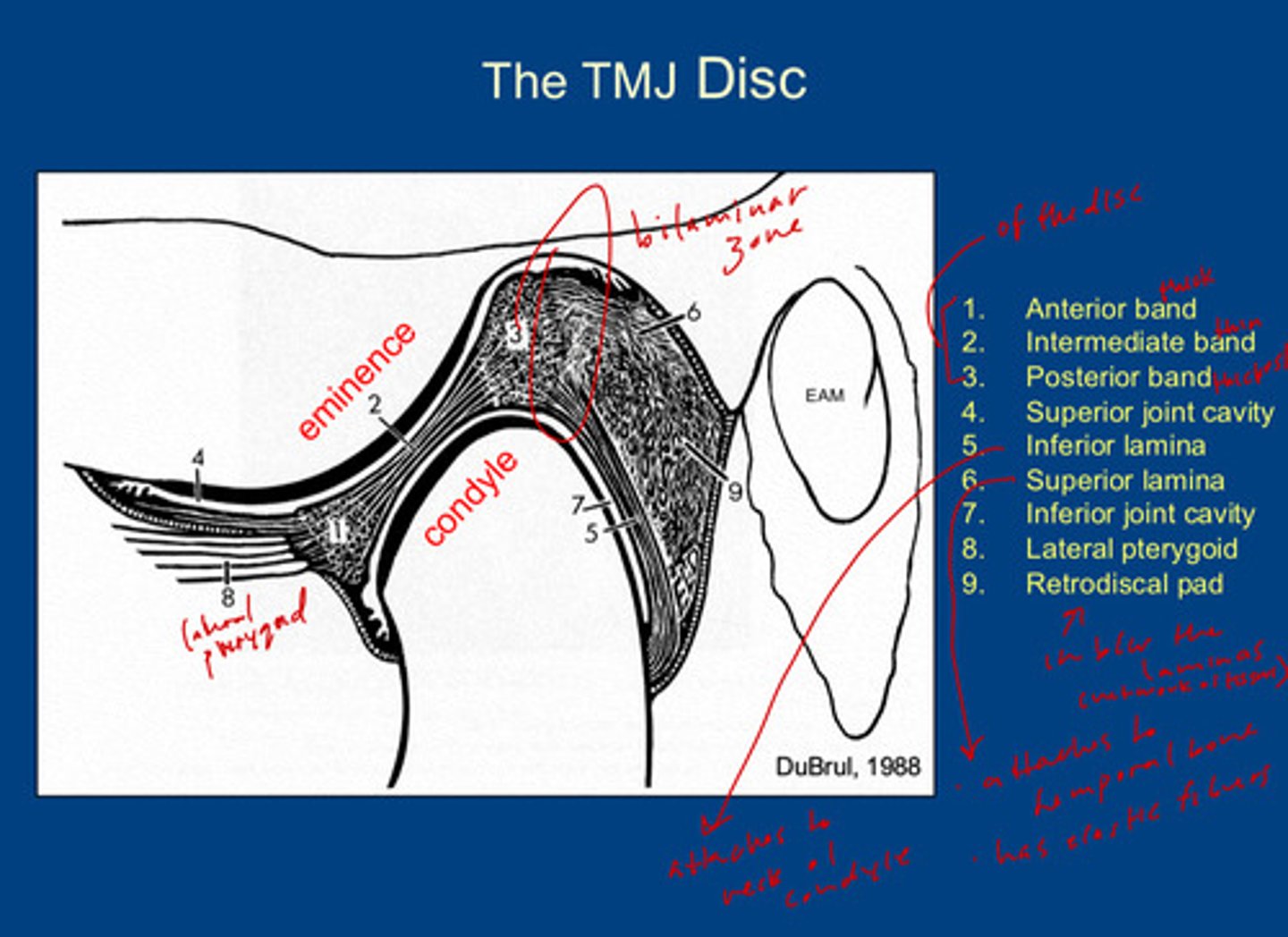
where is the bilaminar zone in the TMJ disc
the zone of transition between the posterior band and the superior and inferior laminas (posteriorly to the posterior band)
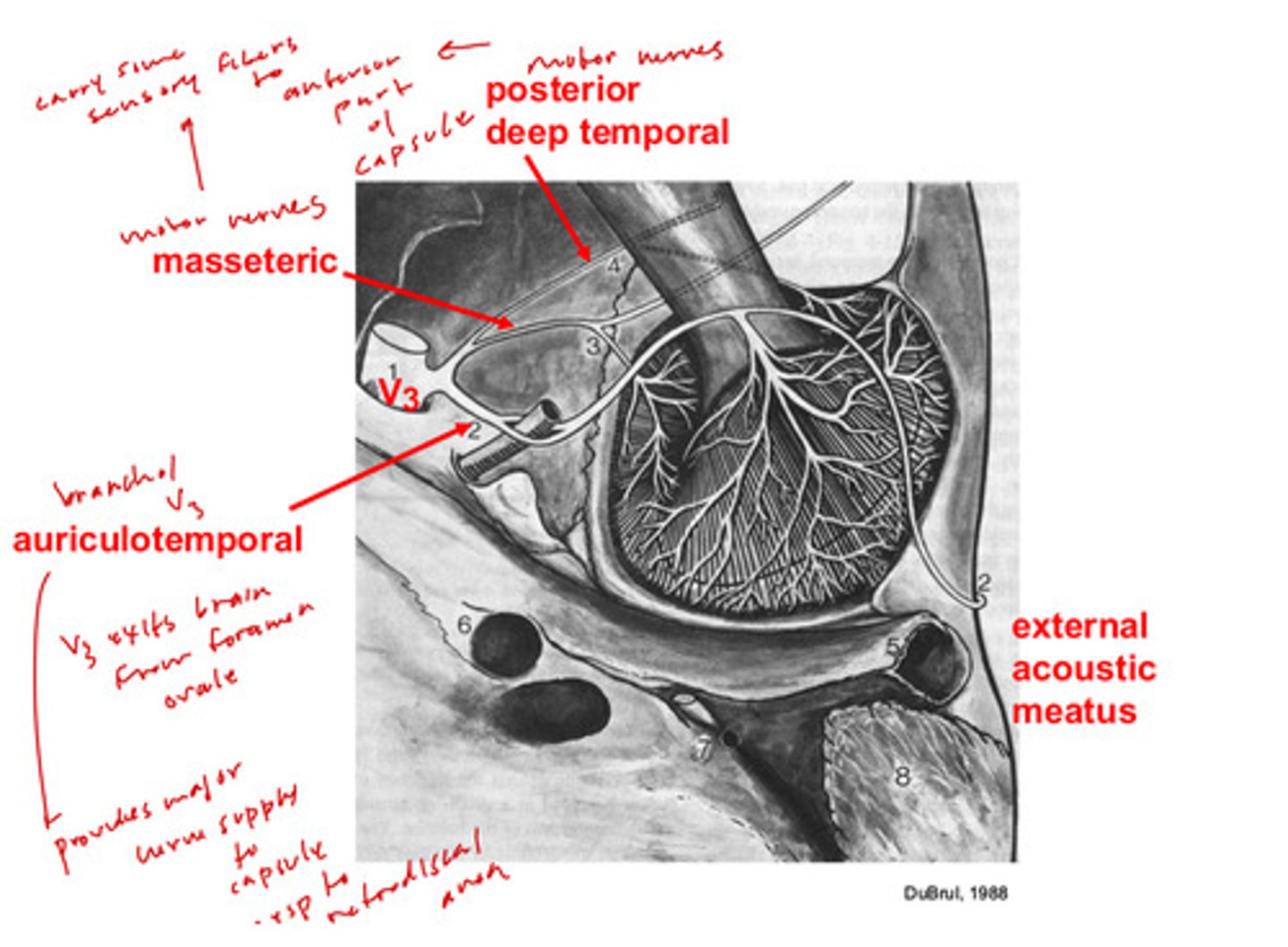
what are the 3 nerves that contribute to the innervation of the TMJ
1) auriculotemporal: branch of V3 (mandibular branch of trigeminal)
2) masseteric: branch of V3
3) posterior deep temporal: branch of V3
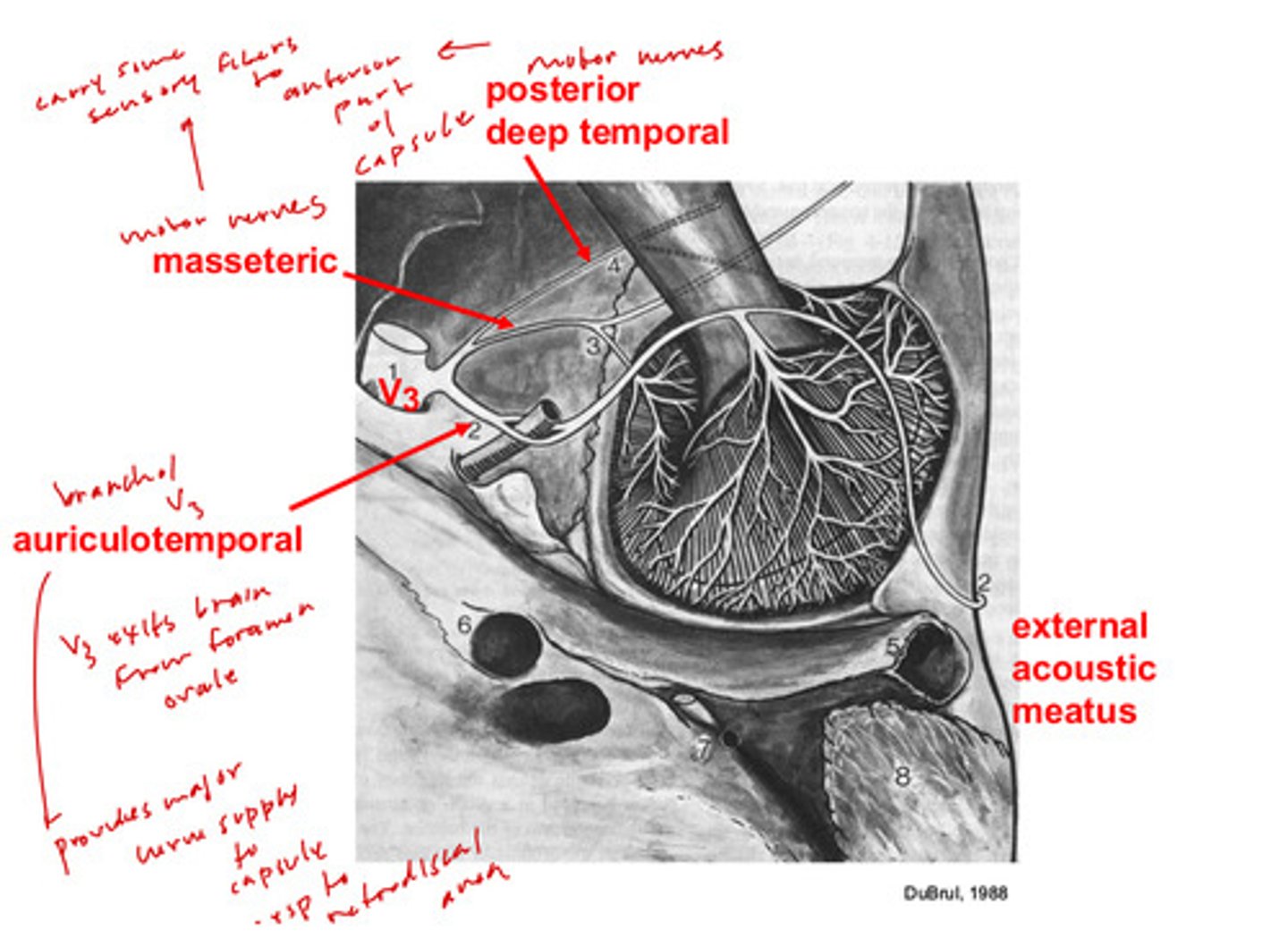
where does V3 exit the cranial cavity from?
the foramen ovale
what does the masseteric nerve contribute to the TMJ
they are motor nerves, but carry some sensory fibers to anterior part of the capsule
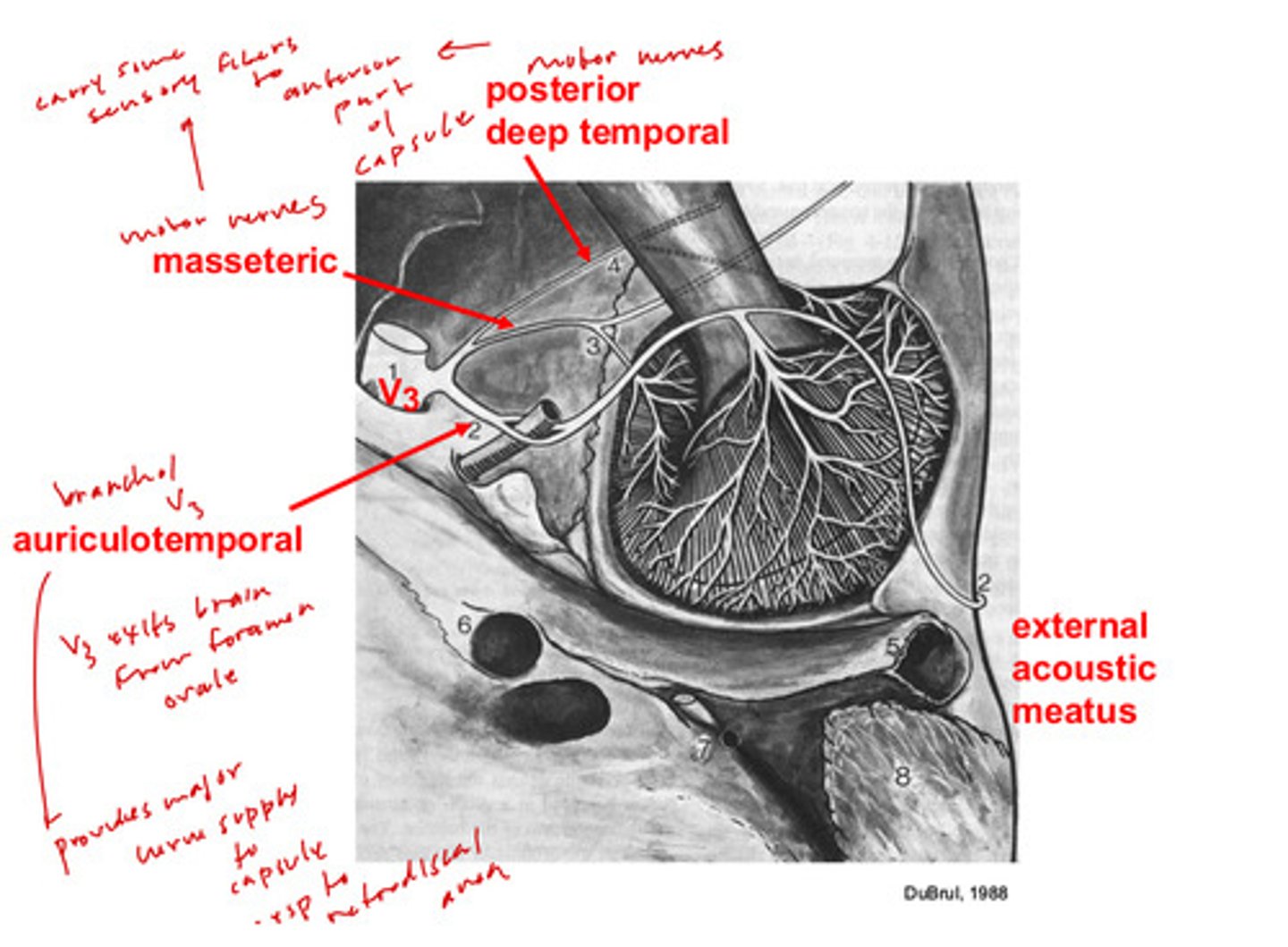
what does the auriculotemporal nerve contribute to the TMJ
provides major nerve supply to the capsule, especially to the retrodiscal area
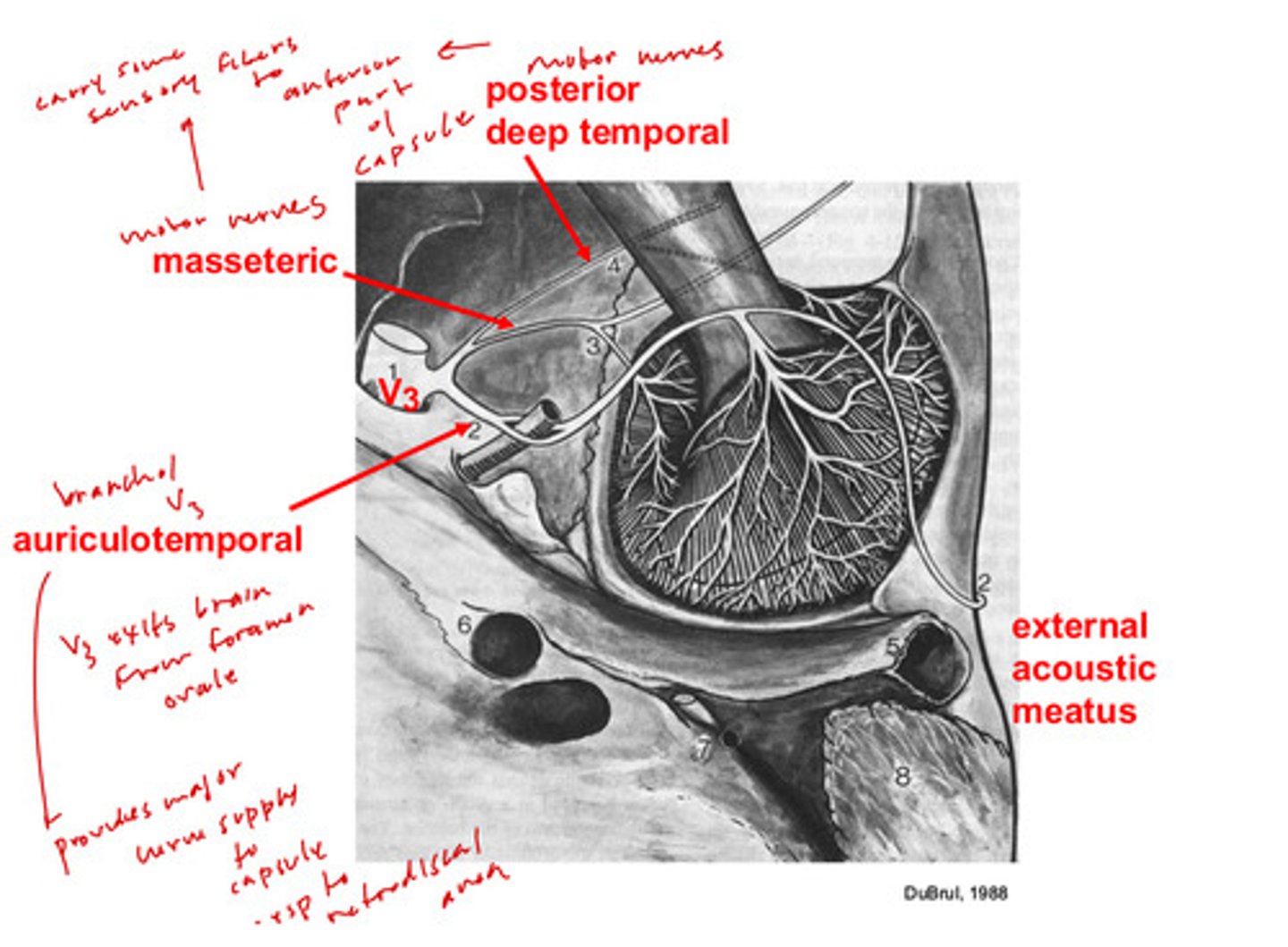
what does the posterior deep temporal nerve contribute to the TMJ
they are motor nerves, but carry some sensory fibers to anterior part of capsules
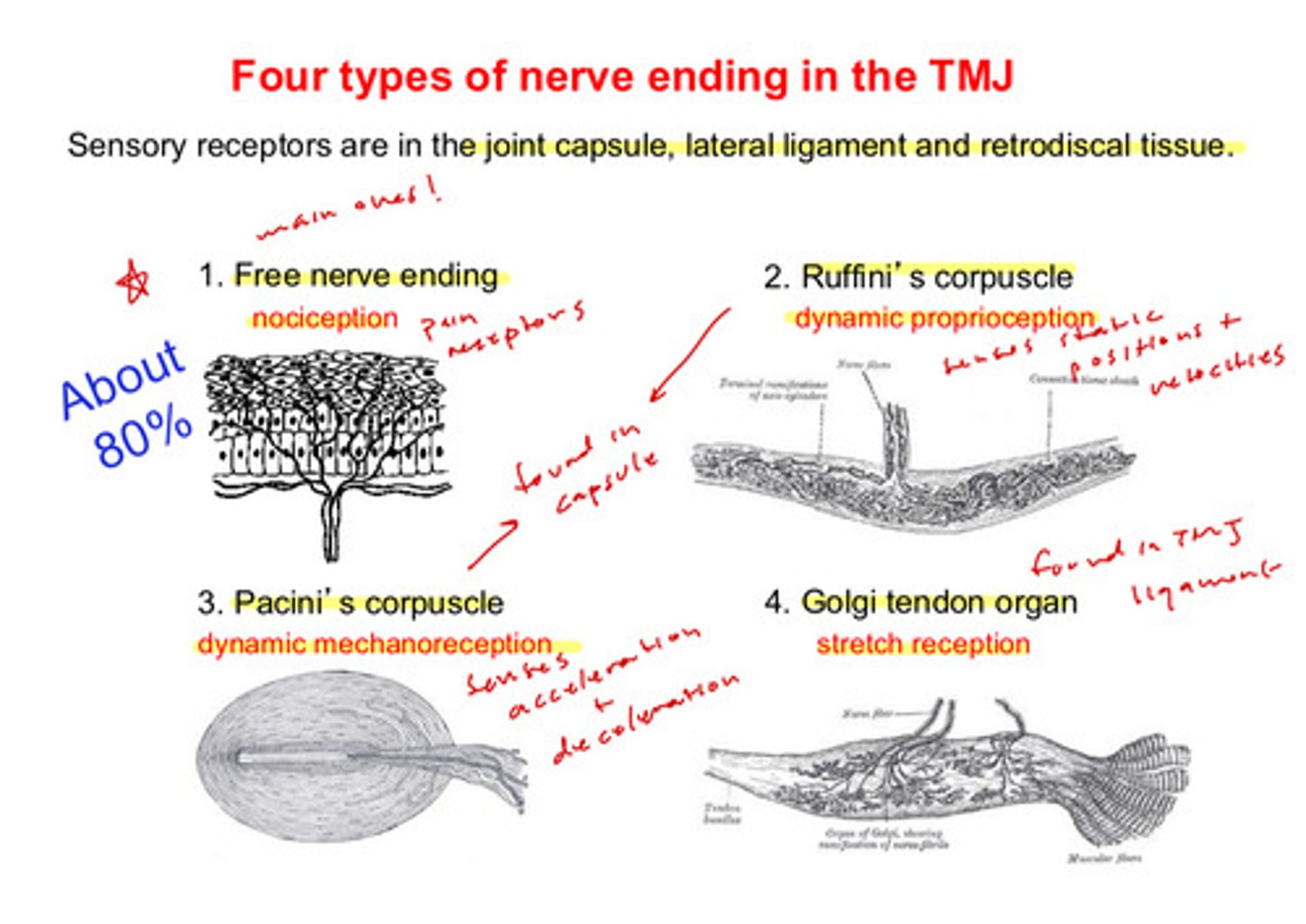
what are the 4 types of nerve endings in the TMJ
1) free nerve endings: nociception
2) ruffini's corpuscle: dynamic proprioception
3) pacini's corpuscle: dynamic mechanoreception
4) golgi tendon organ: stretch reception
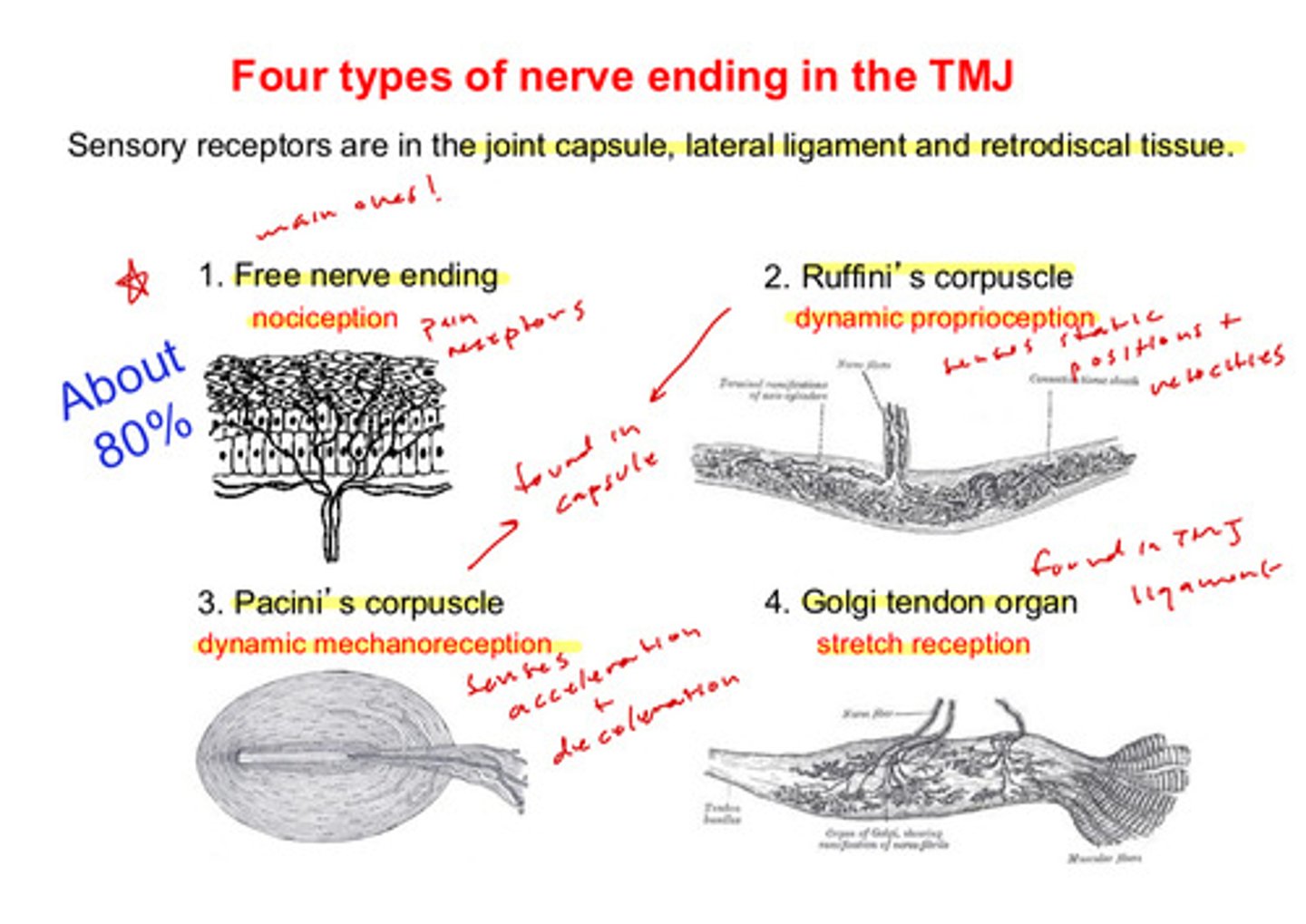
which is the major type of nerve endings in the TMJ?
free nerve endings: nociception (pain receptors) —> about 80%
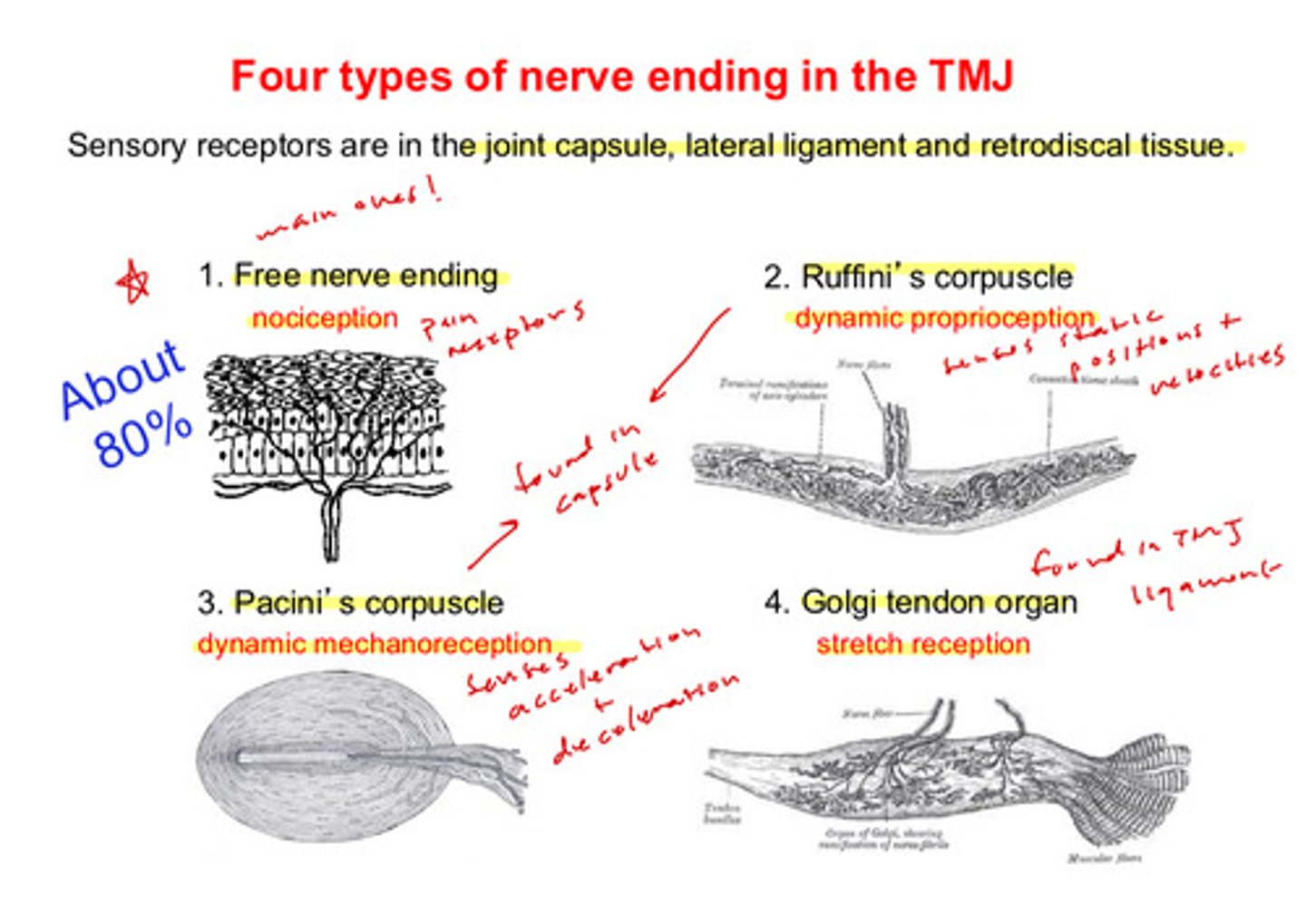
where are the ruffini's corpuscle nerve endings located and what does it sense?
found in the capsule; dynamic proprioception —> senses static positions and velocities
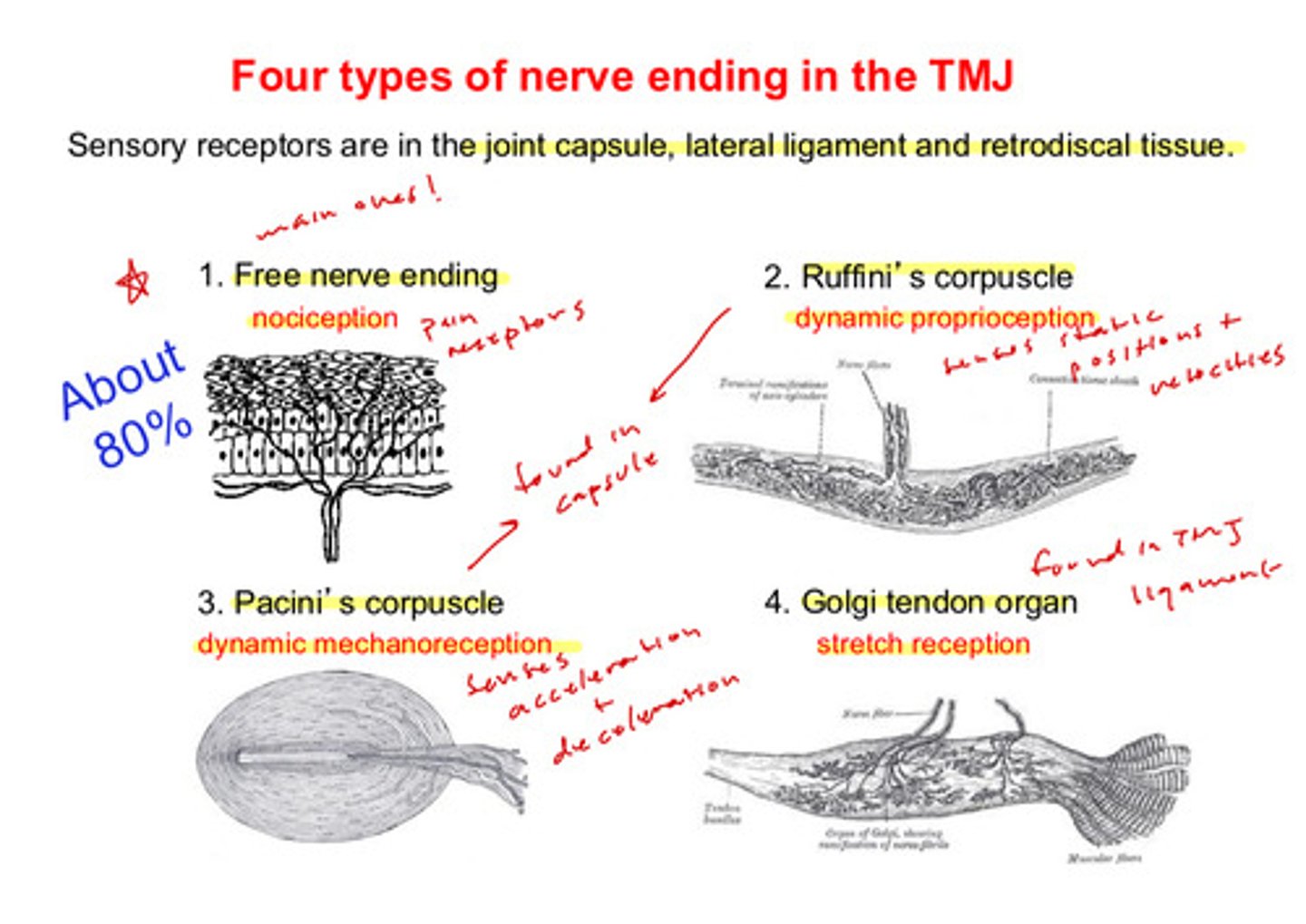
where are the pacini's corpuscle nerve endings located and what does it sense?
found in the capsule; dynamic mechanoreception —> senses acceleration + deceleration

where are the golgi tendon organ nerve endings located?
found in the TMJ ligament
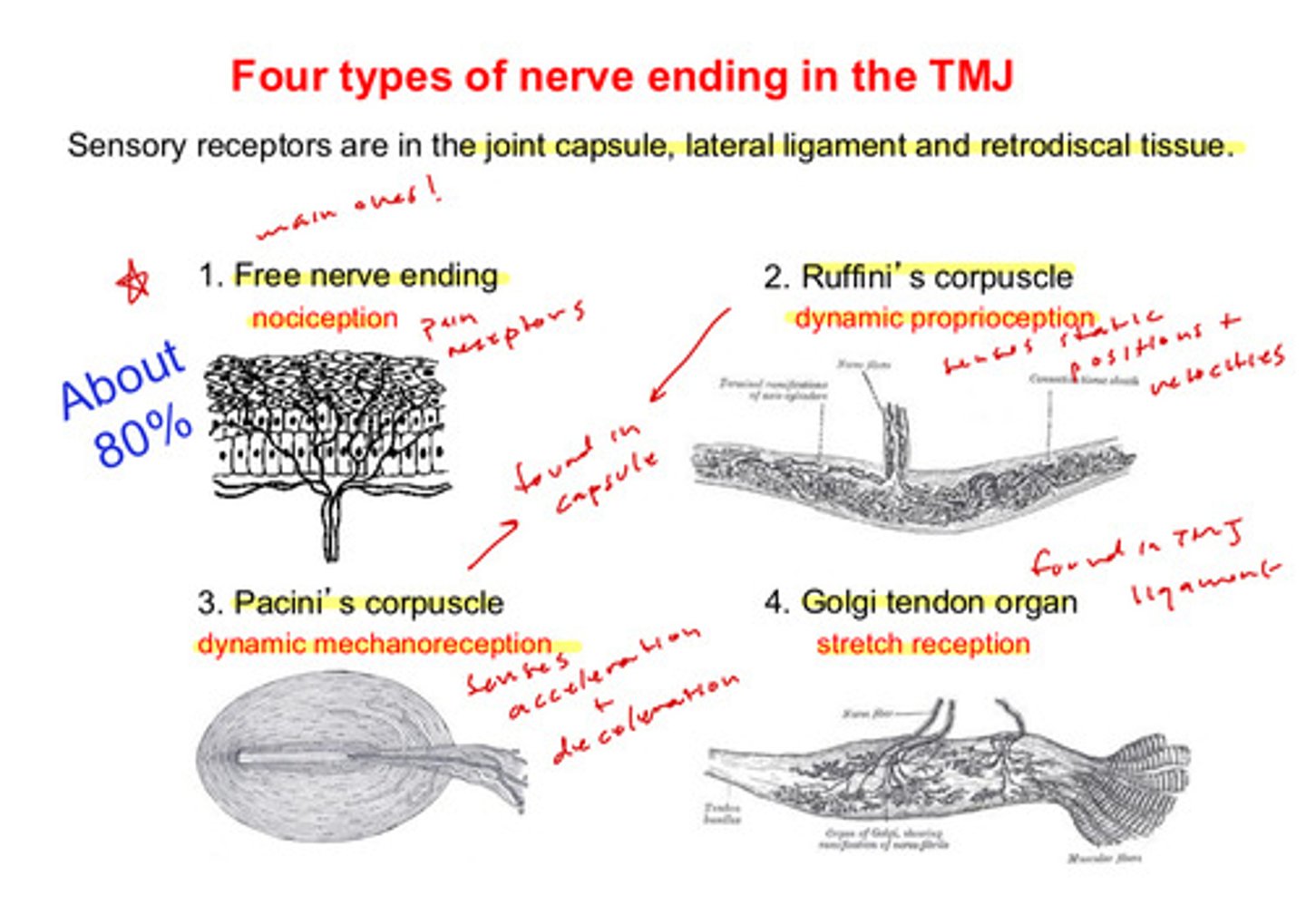
what 3 areas are the sensory receptors of the TMJ found?
the joint capsule, the lateral ligament, and the retrodiscal tissue
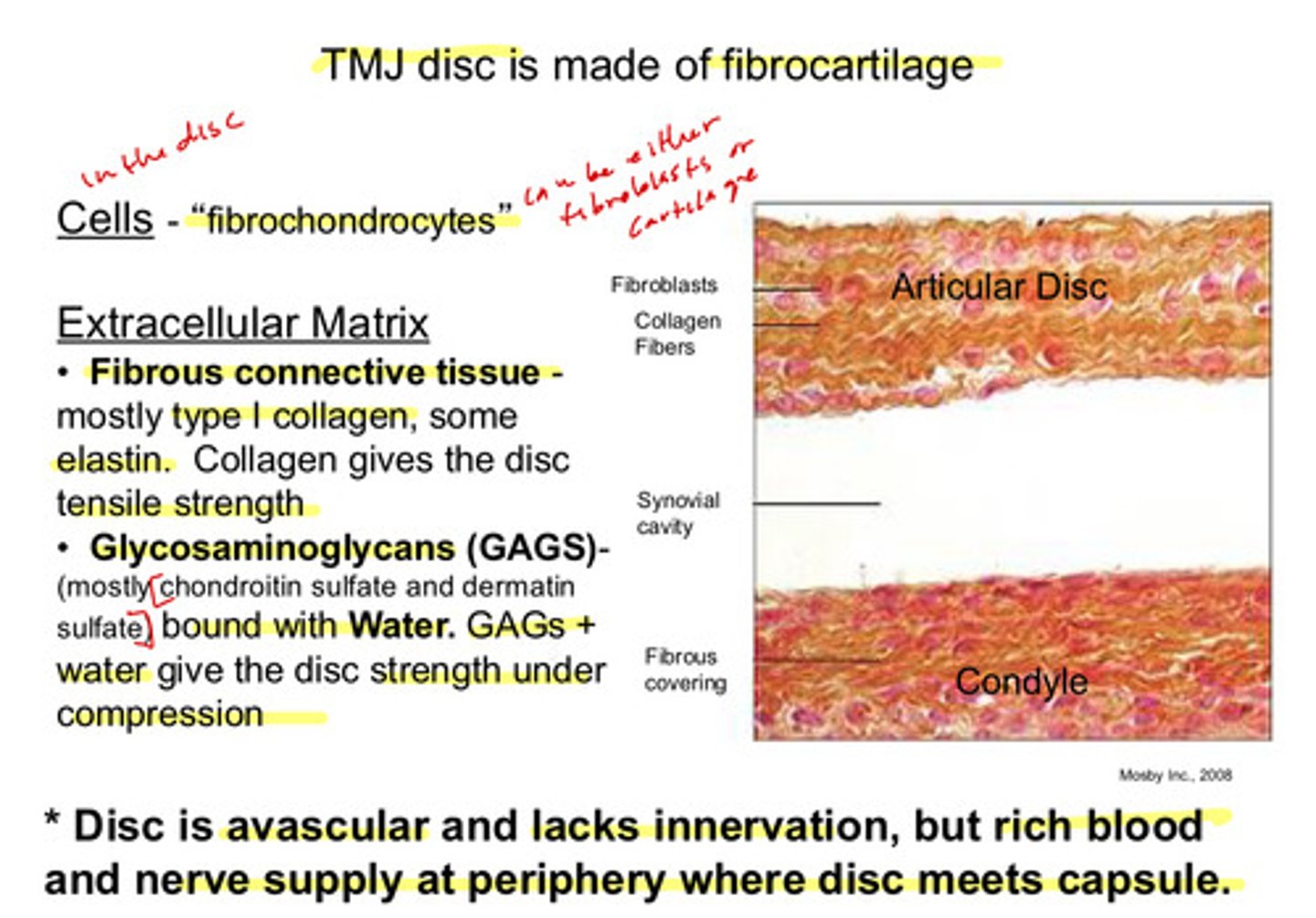
the TMJ disc is made of what kind of tissue and what kinds of cells are found in this tissue
made of fibrocartilage; fibrochondrocytes are found in the disc —> these are capable of acting either as fibroblasts or chondrocytes
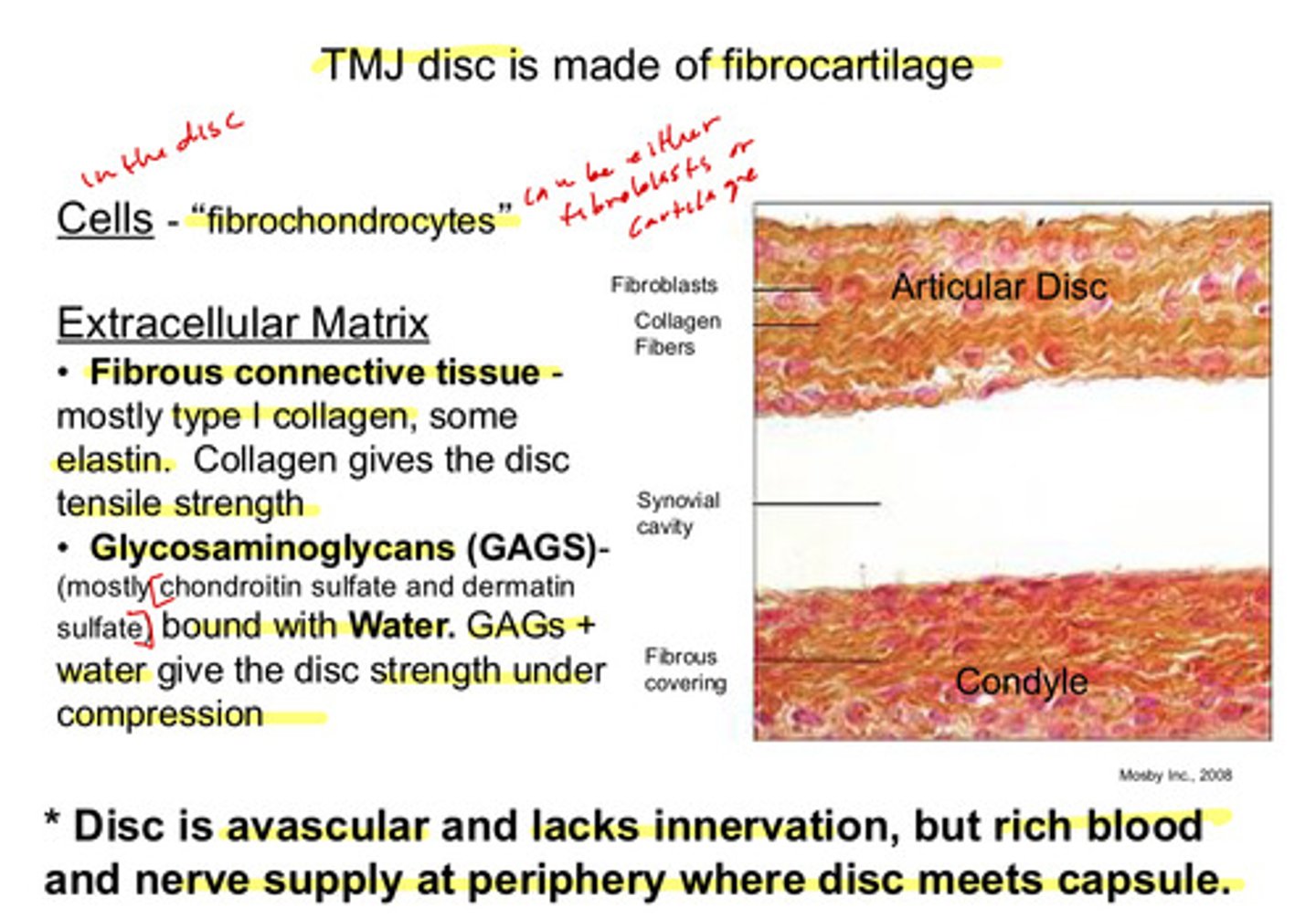
what are the 2 main components of the extracellular matrix of the TMJ disc and what property do they contribute to the disc?
1) fibrous connective tissue: mostly type I collagen, some elastin. collagen gives the disc tensile strength
2) glycosaminoglycans (GAGs) bound with water: mostly chondroitin sulfate and dermatin sulfate. GAGs and water give the disc strength under compression
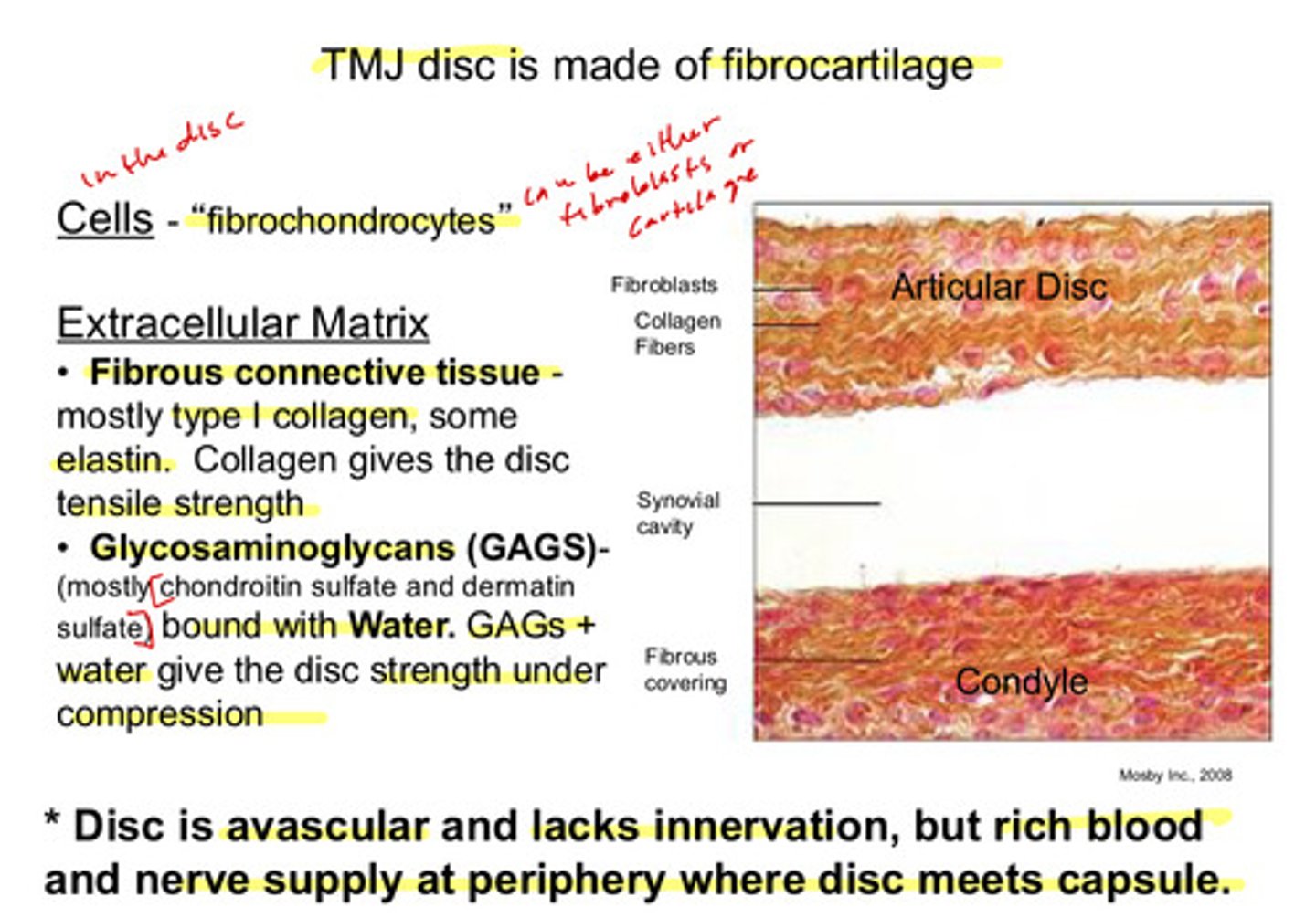
the disc itself is avascular and lacks innervation, but there is a rich blood and nerve supply located at ?
the periphery where the disc meets the capsule
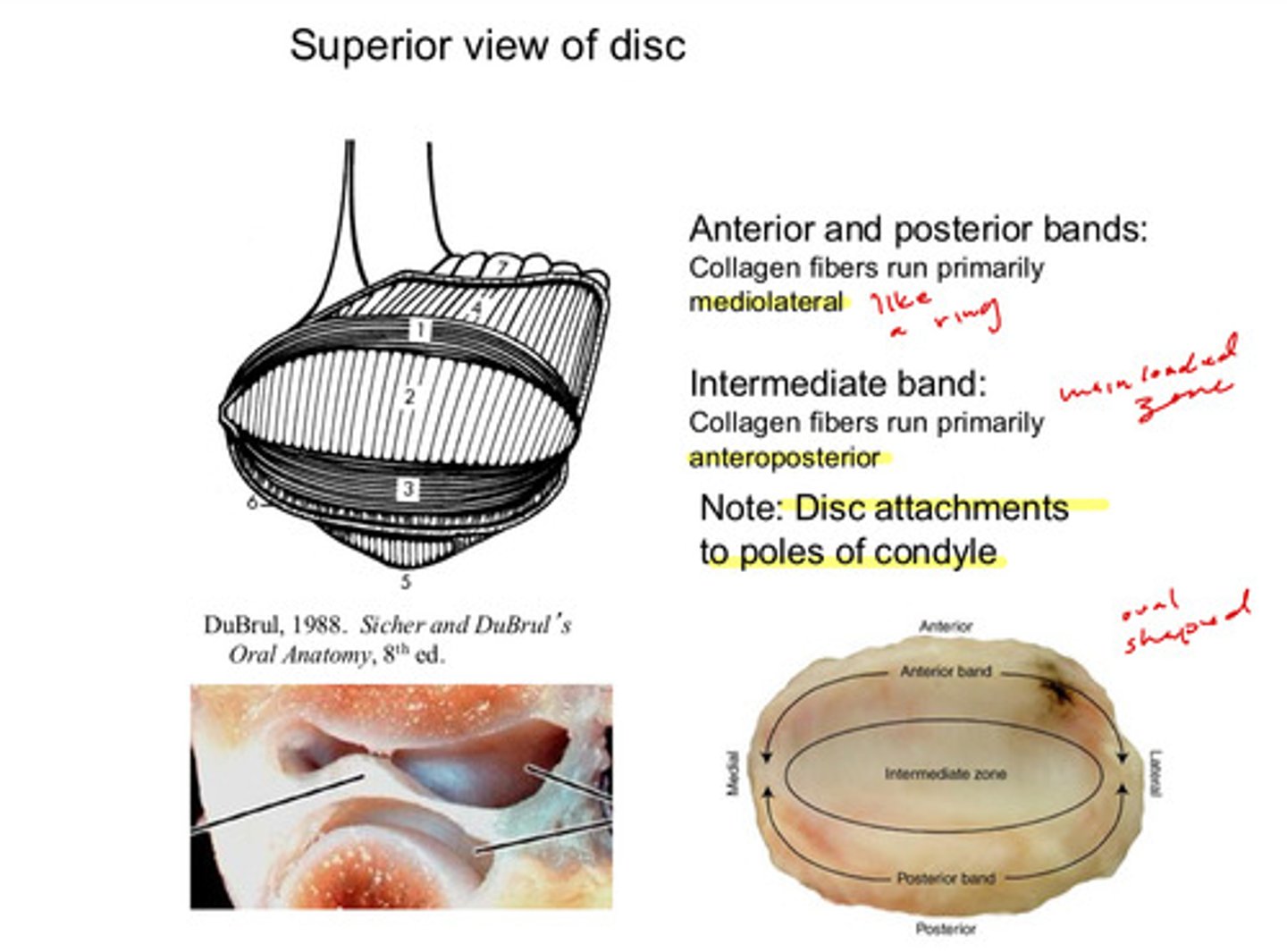
describe the orientation in which the collagen fibers of the anterior and posterior bands of the TMJ disc run
run primarily mediolateral like a ring
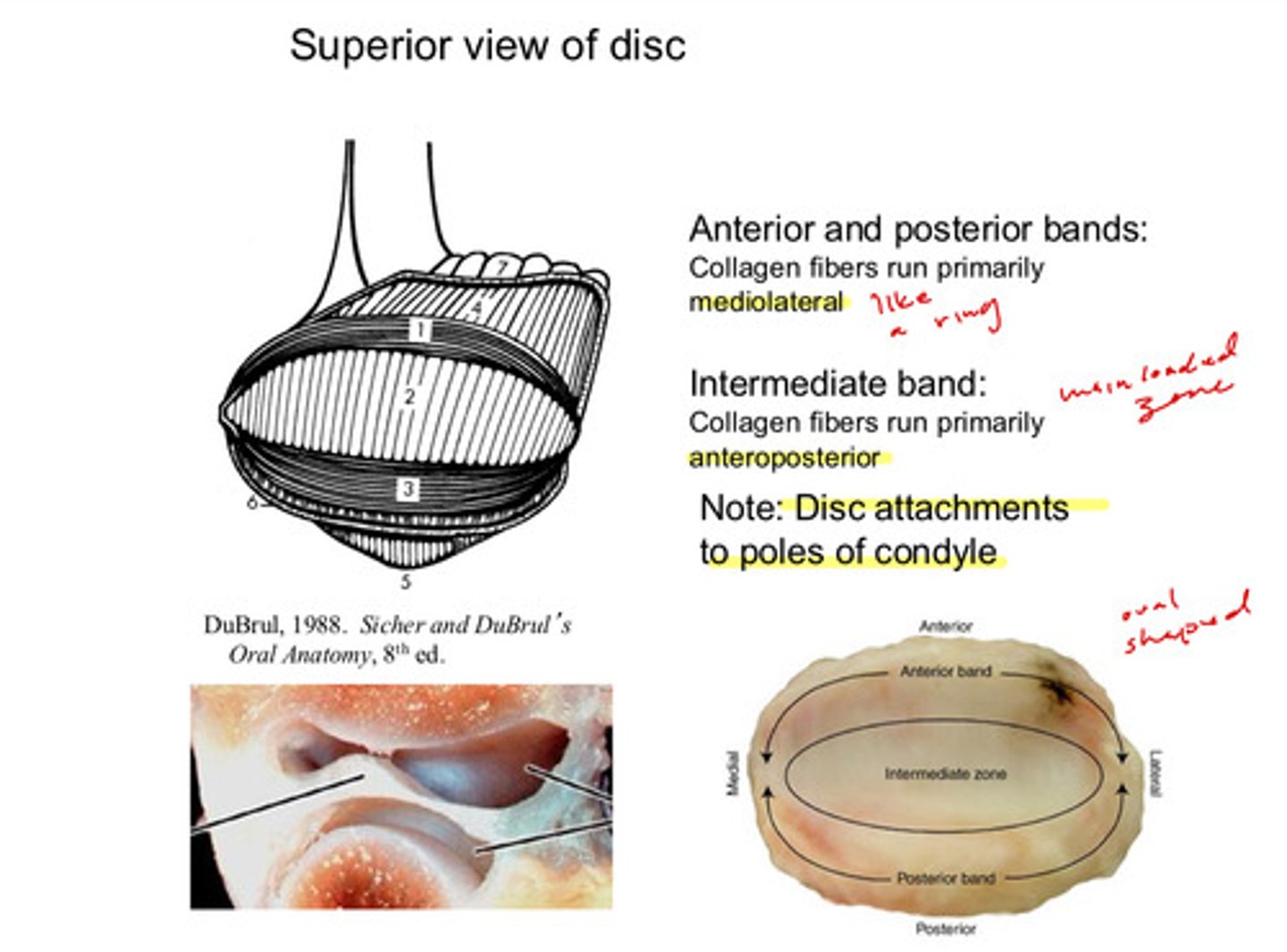
describe the orientation in which the collagen fibers of the intermediate band of the TMJ disc run
run primarily anteroposterior (this is the main loaded zone)
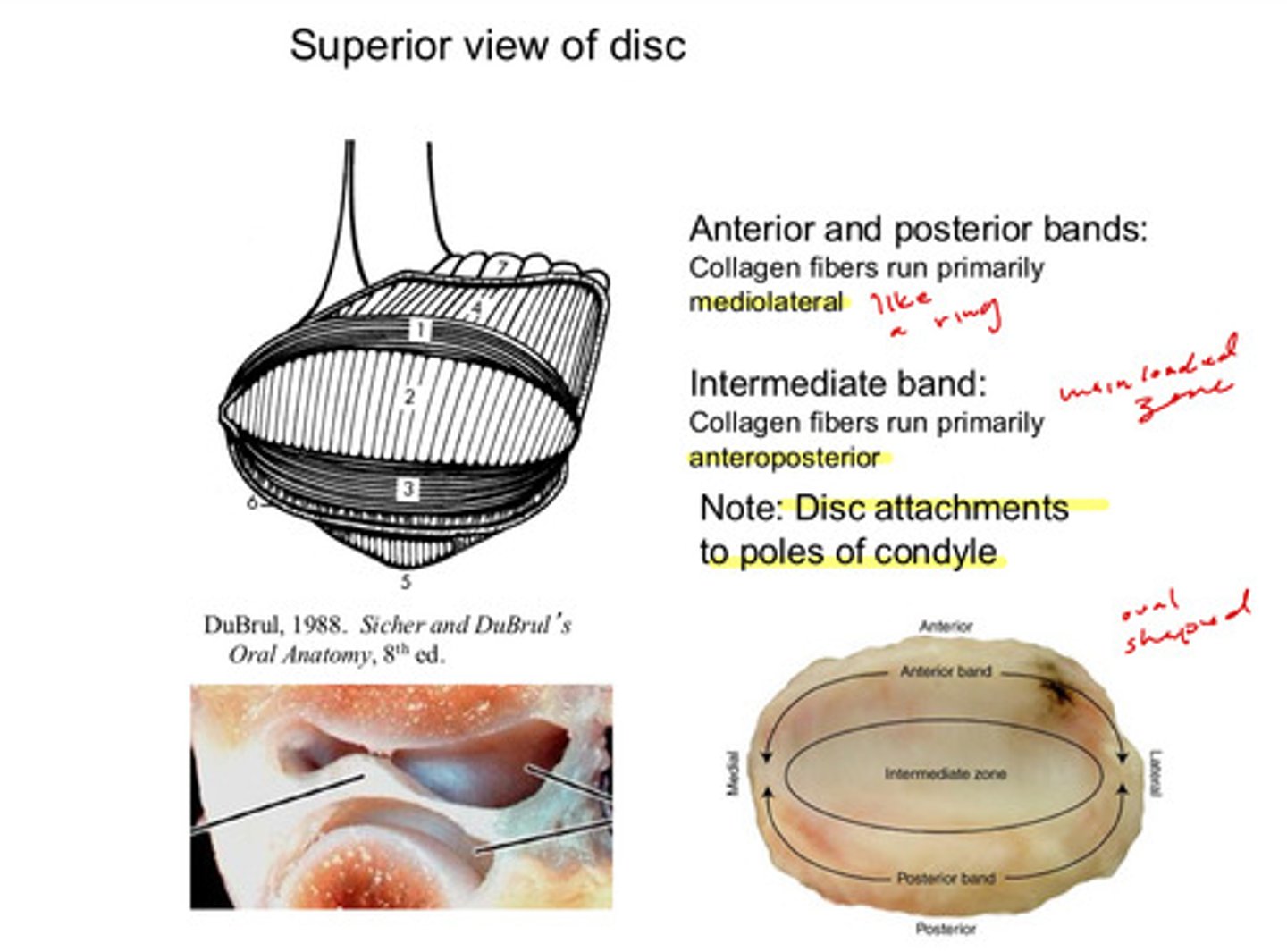
note that the disc is attached to the pole of the condyle via the ?
the collateral ligaments
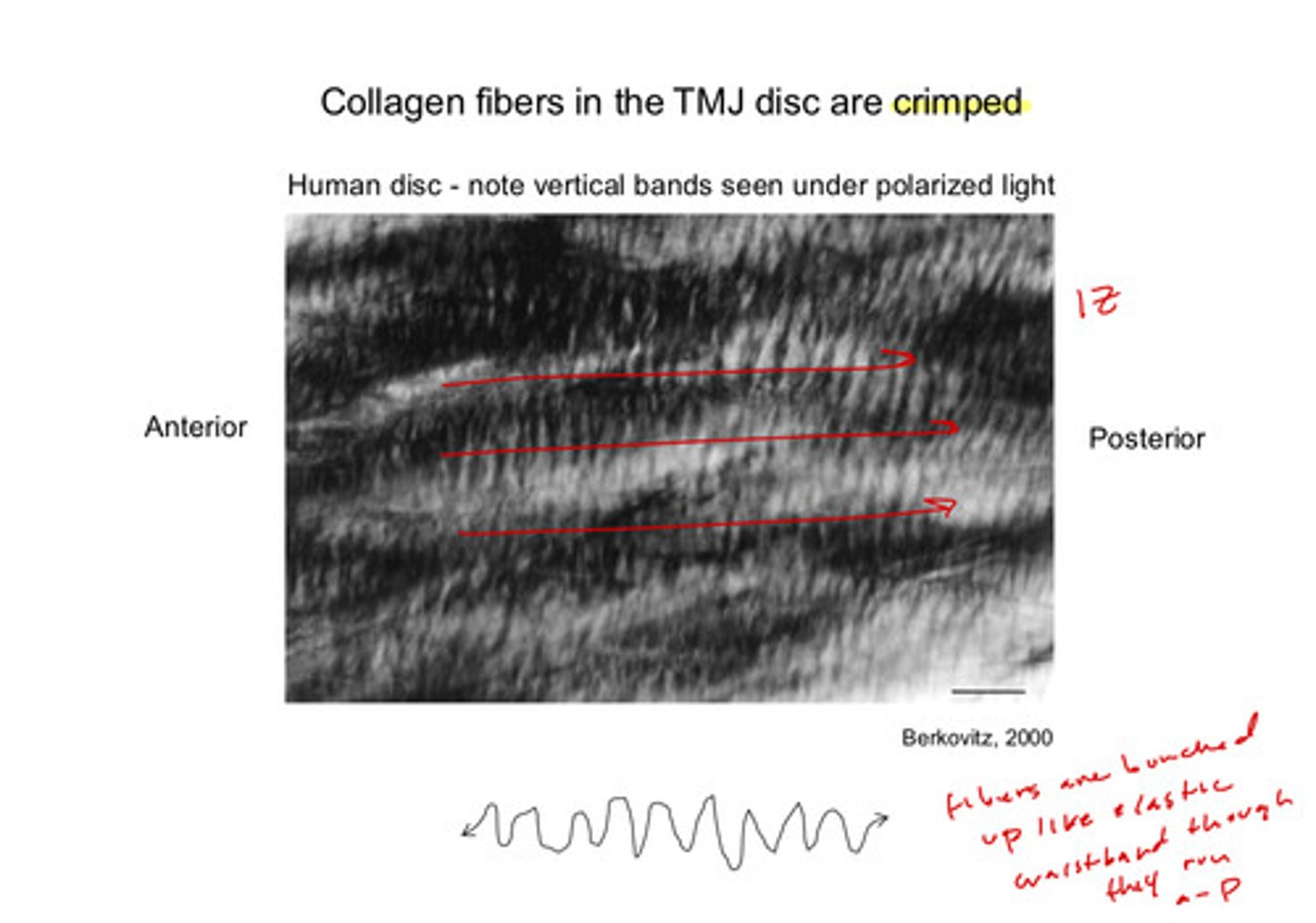
the collagen fibers in the TMJ disc are ?
crimped! the fibers are bunched up like an elastic waistband, giving it a crimped look despite running mainly anterioposterior (in the central TMJ disc/intermediate zone)
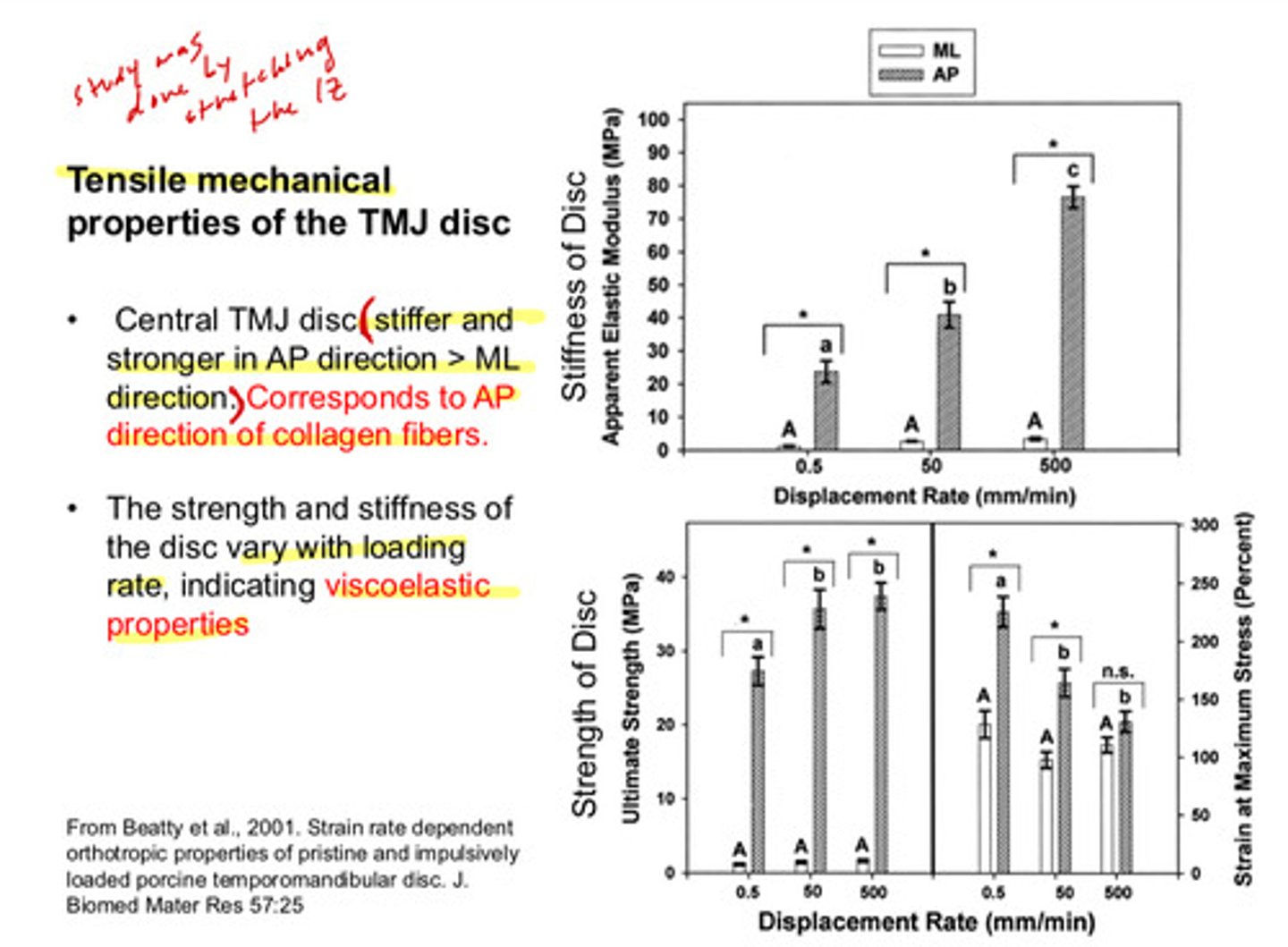
the central TMJ disc is stiffer and stronger in the AP direction > ML direction. this corresponds to?
the AP direction of the collagen fibers
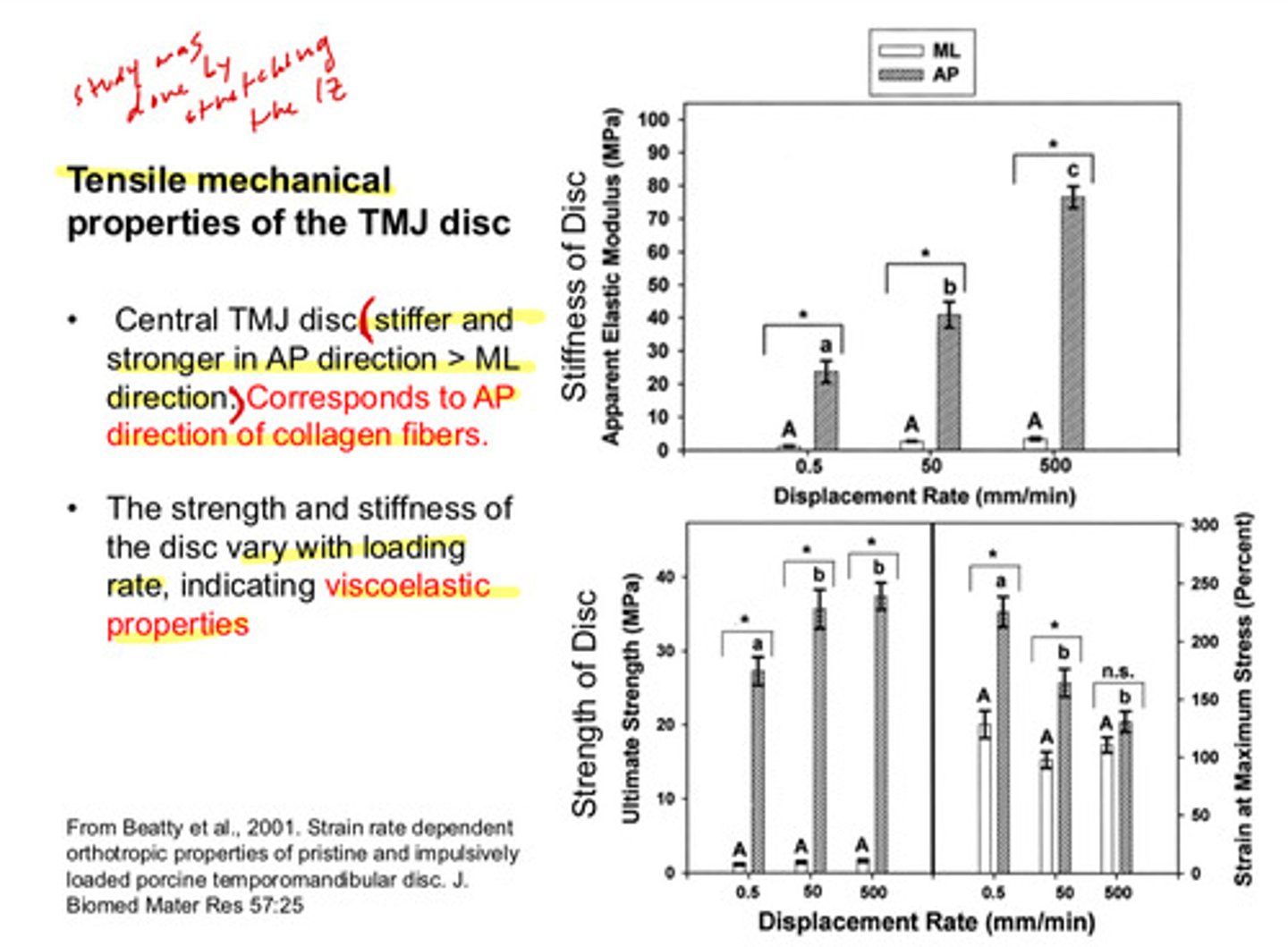
the strength and stiffness of the disc vary with ________ rates, indicating ___________ properties
loading rates, indicating viscoelastic properties
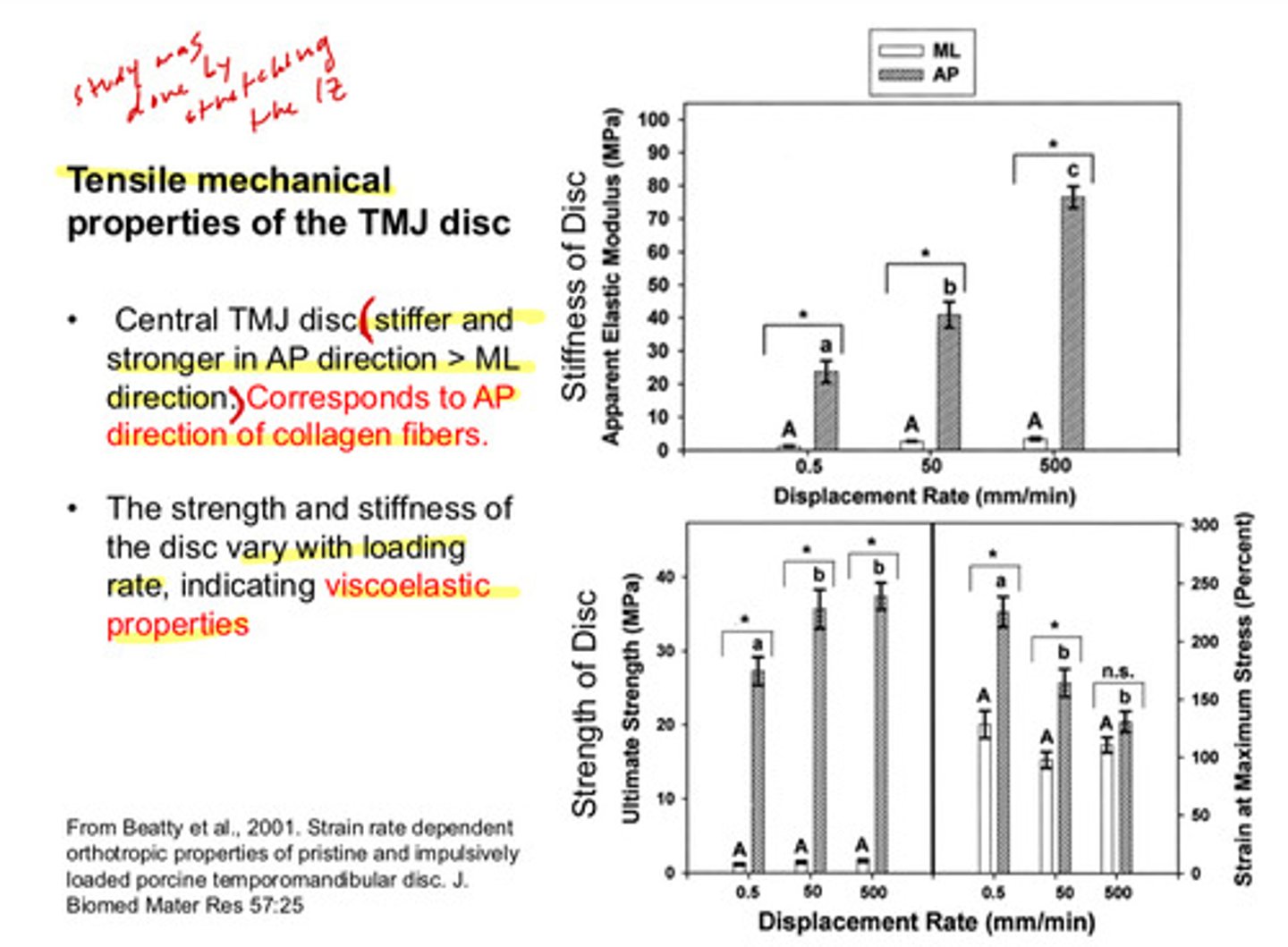
the first table shows the stiffness of the disc in ML and AP directions at various displacement rates
AP is much stiffer than ML, and increases in stiffness as displacement rate increases
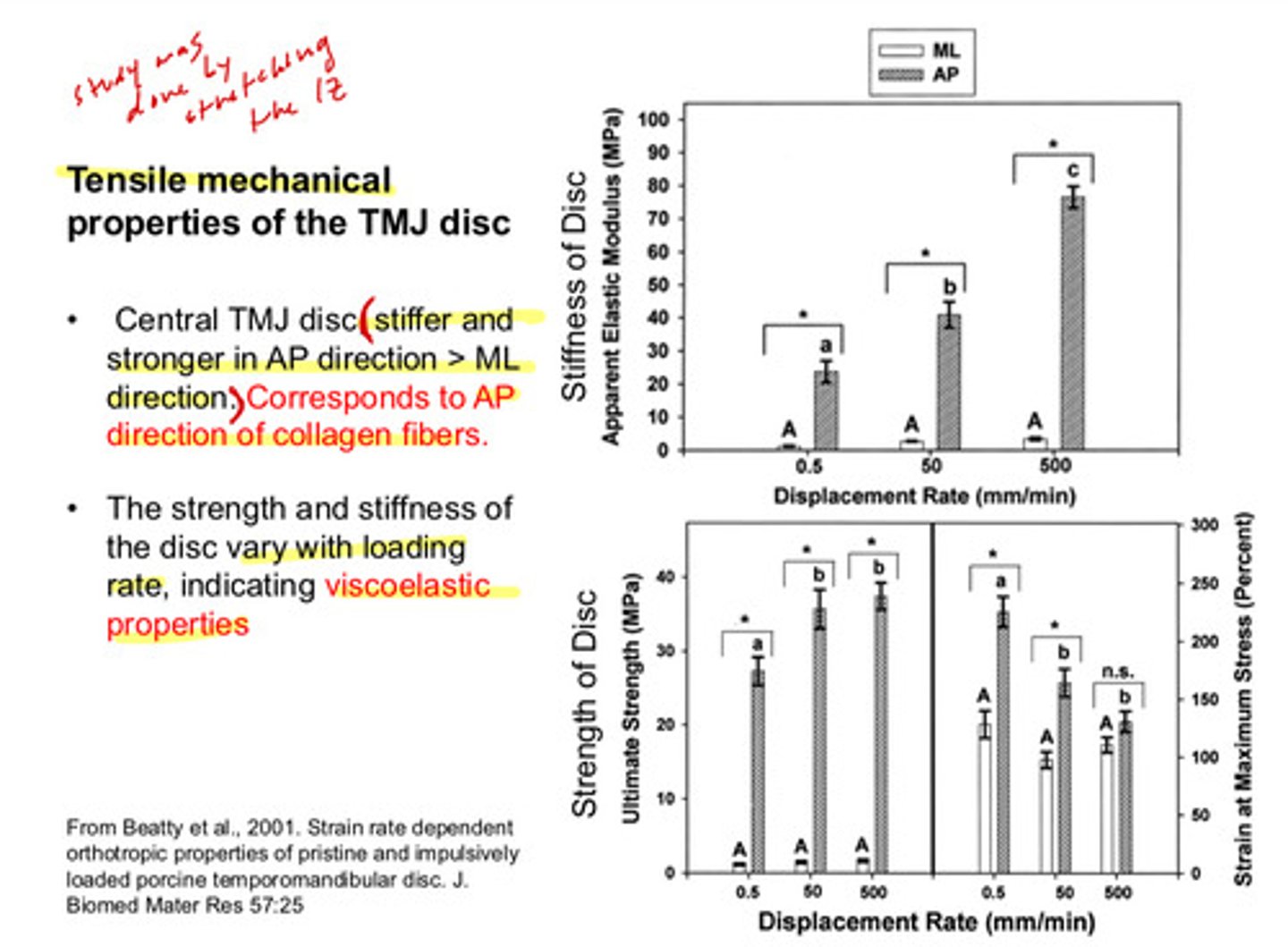
the second table shows the strength of the disc and the % strain inflicted on the disc in ML and AP directions at various displacement rates
AP is again much stronger than ML; its strength increased with increased displacement rates, and % strain decreased with increased displacement rates (the ML oriented fibers varied with % strain)
recall: what does it mean to be viscoelastic
- material will deform under load but will not instantly bounce back
- ^ depending on the rate and duration of the load
- material will show time-dependent strain and stress relaxation
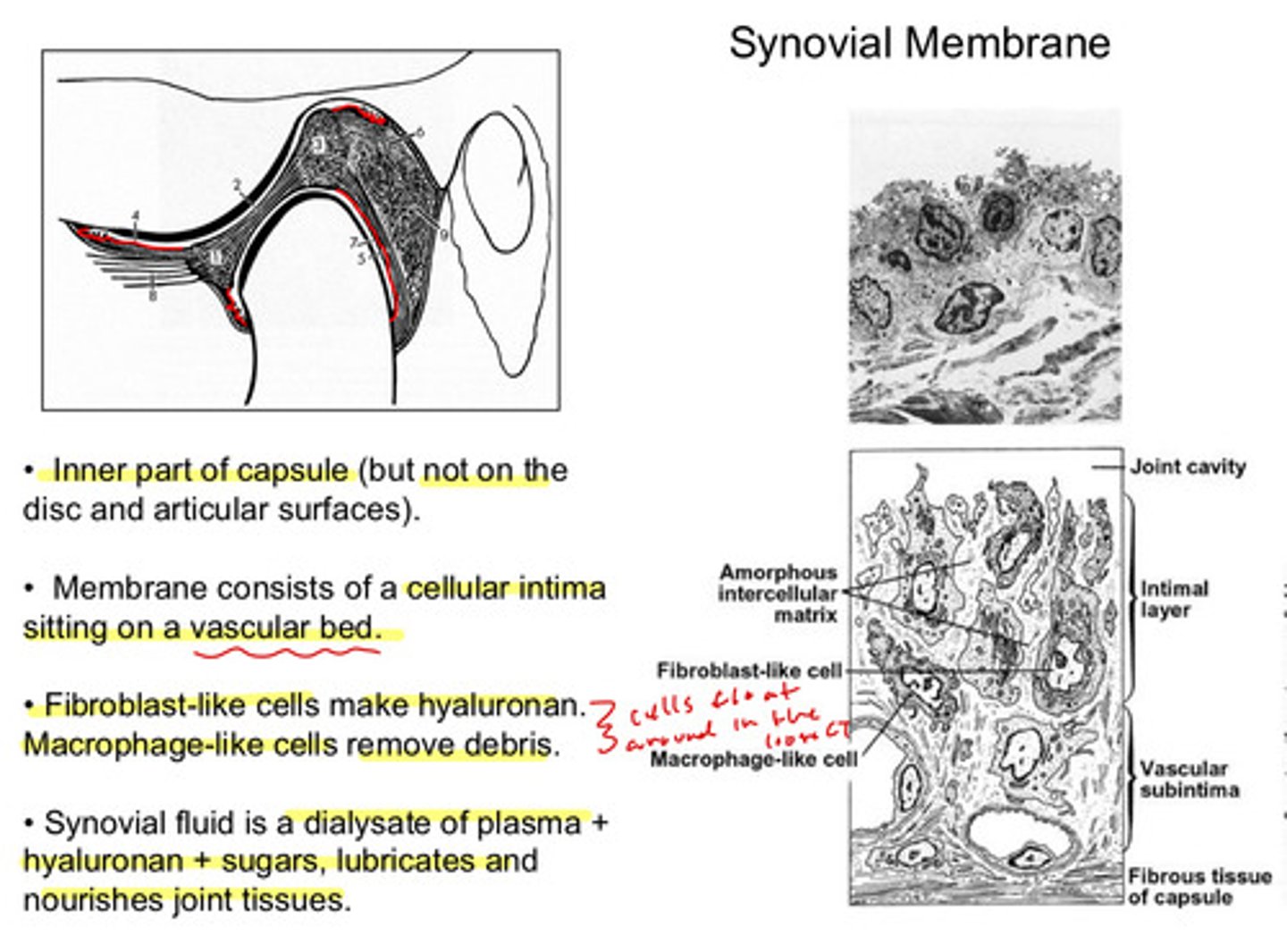
where is the synovial membrane located
inner part of the capsule (but not on the disc and articular surfaces)
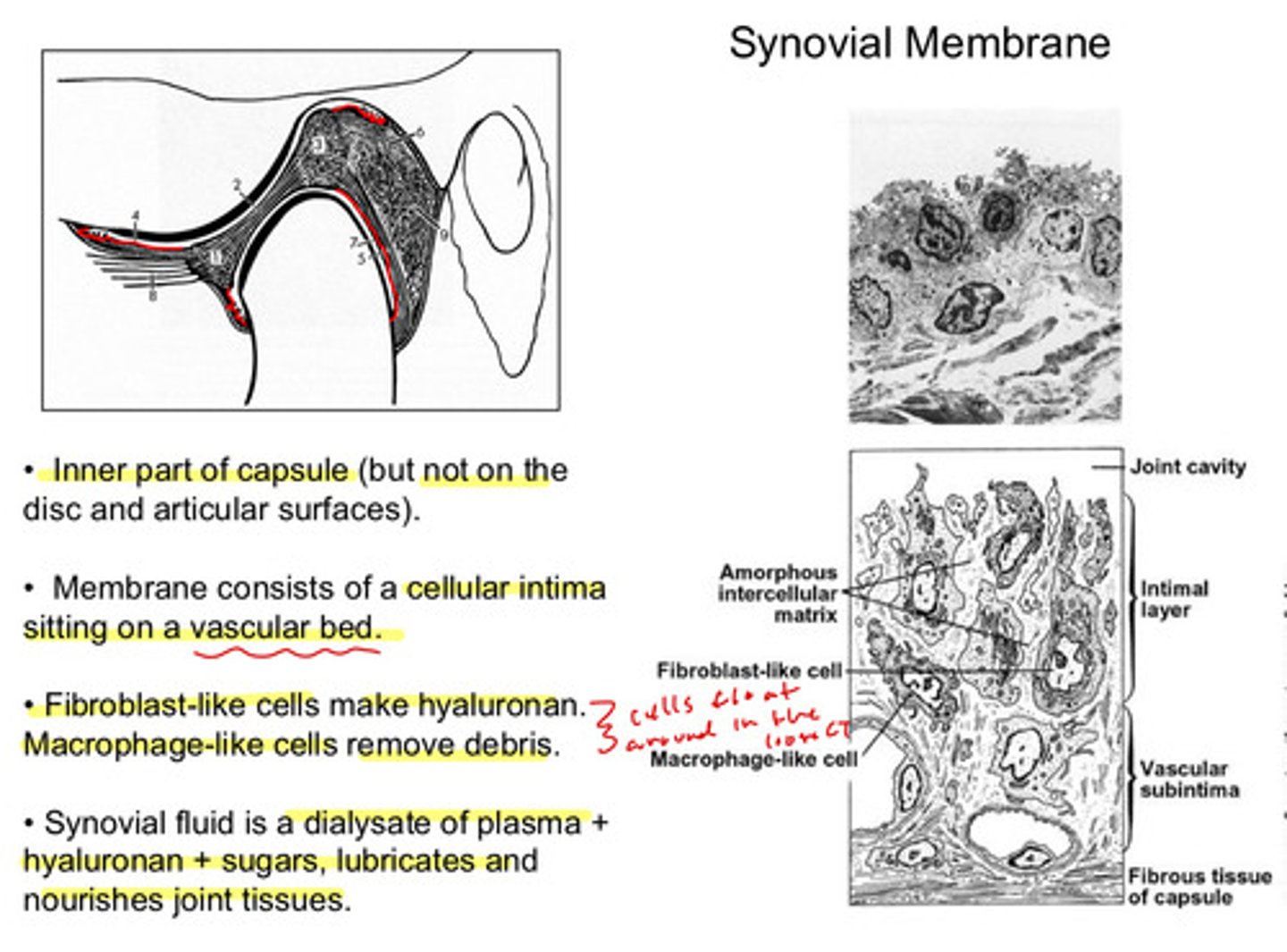
the synovial membrane consists of a _______ _______ layer sitting on a ?
cellular intima layer sitting on a vascular bed
what kinds of cells are present in the synovial membrane and what are their actions
fibroblast like cells: make hyaluronan
macrophage like cells: remove debris
these cells float around in the loose CT of the membrane
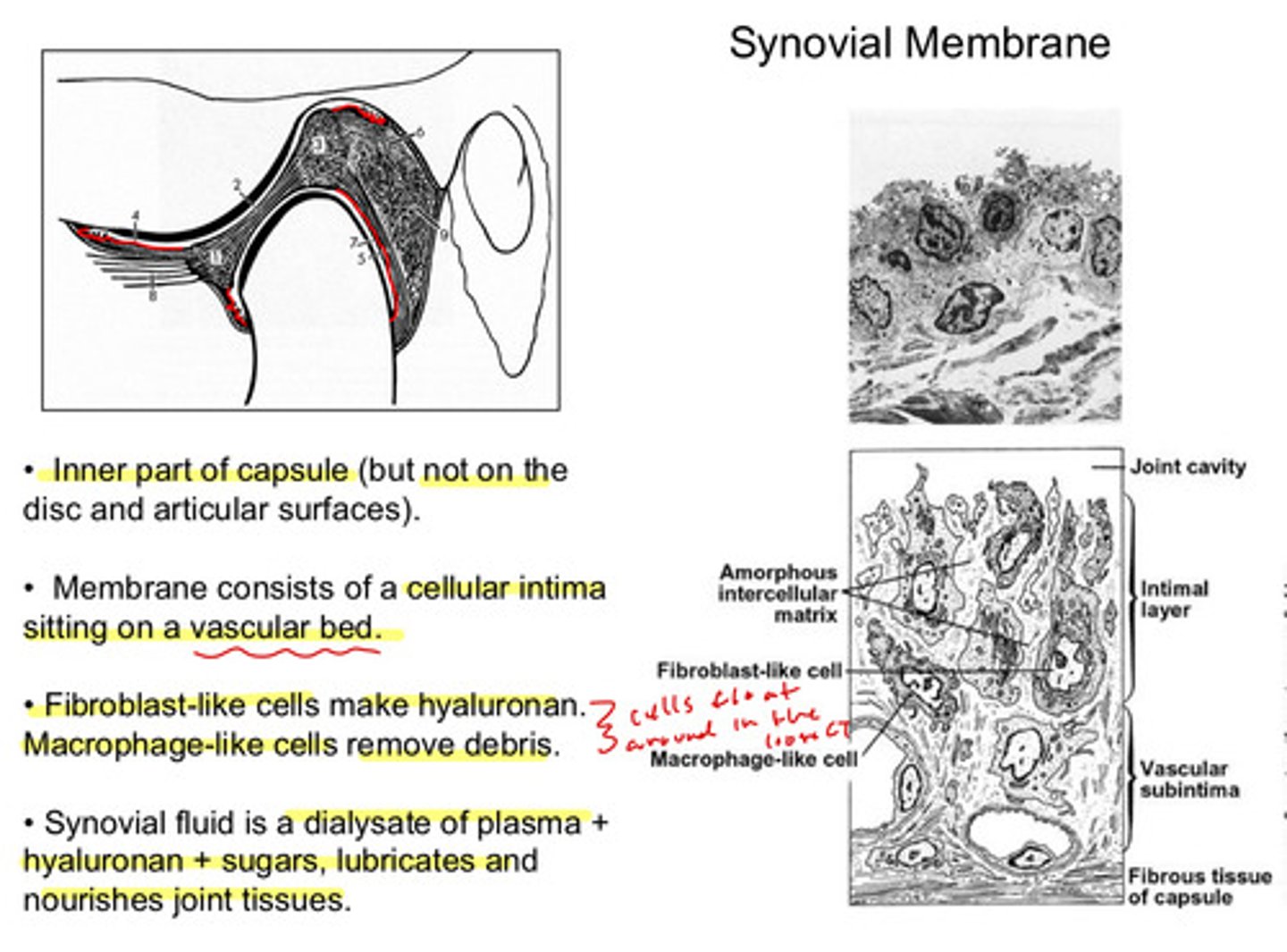
the synovial fluid is a dialysate (fluid used in dialysis to remove waste products) of what 3 things?
plasma + hyaluronan + sugars
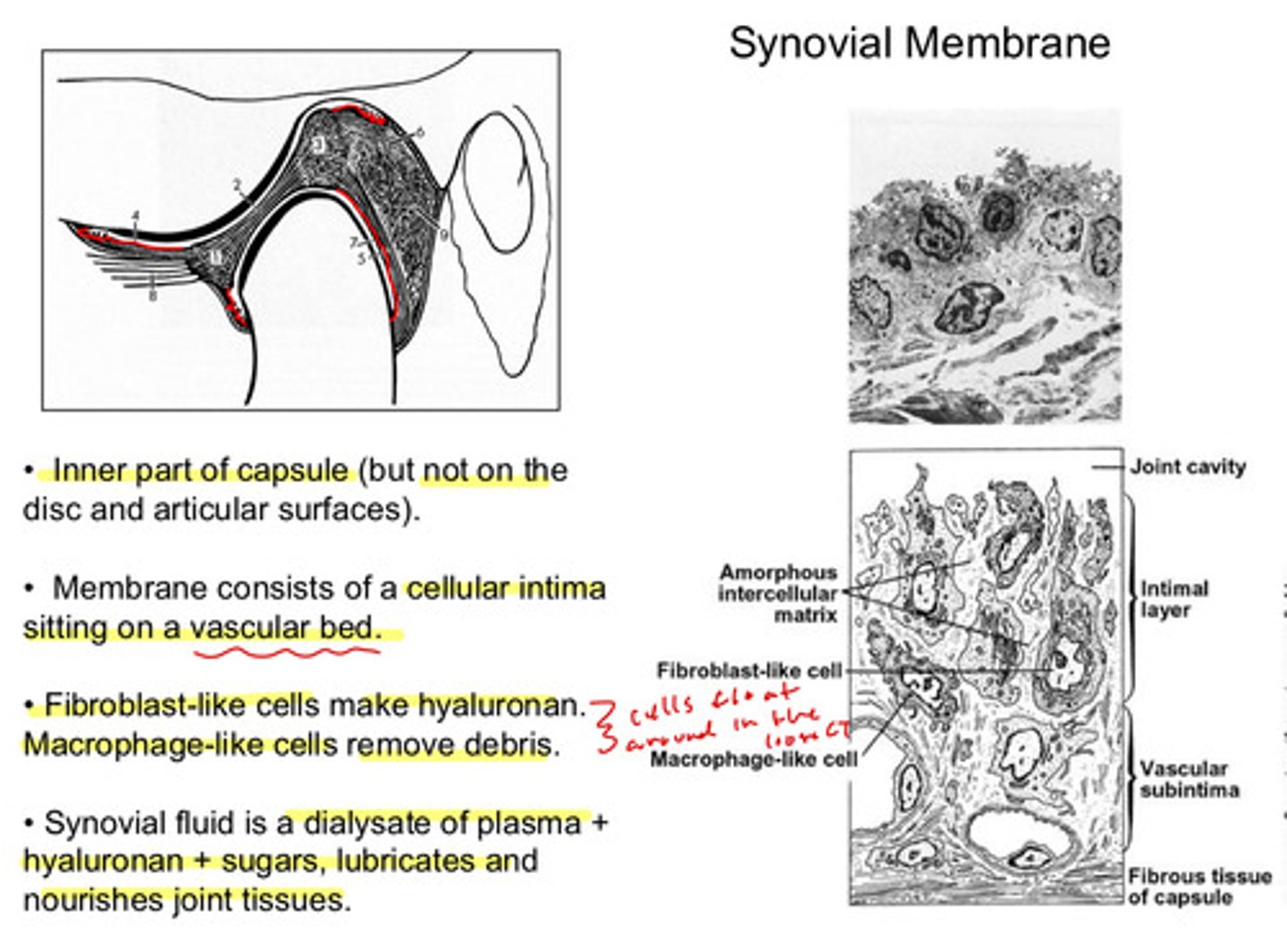
the synovial membrane has what action?
lubricates and nourishes joint tissues
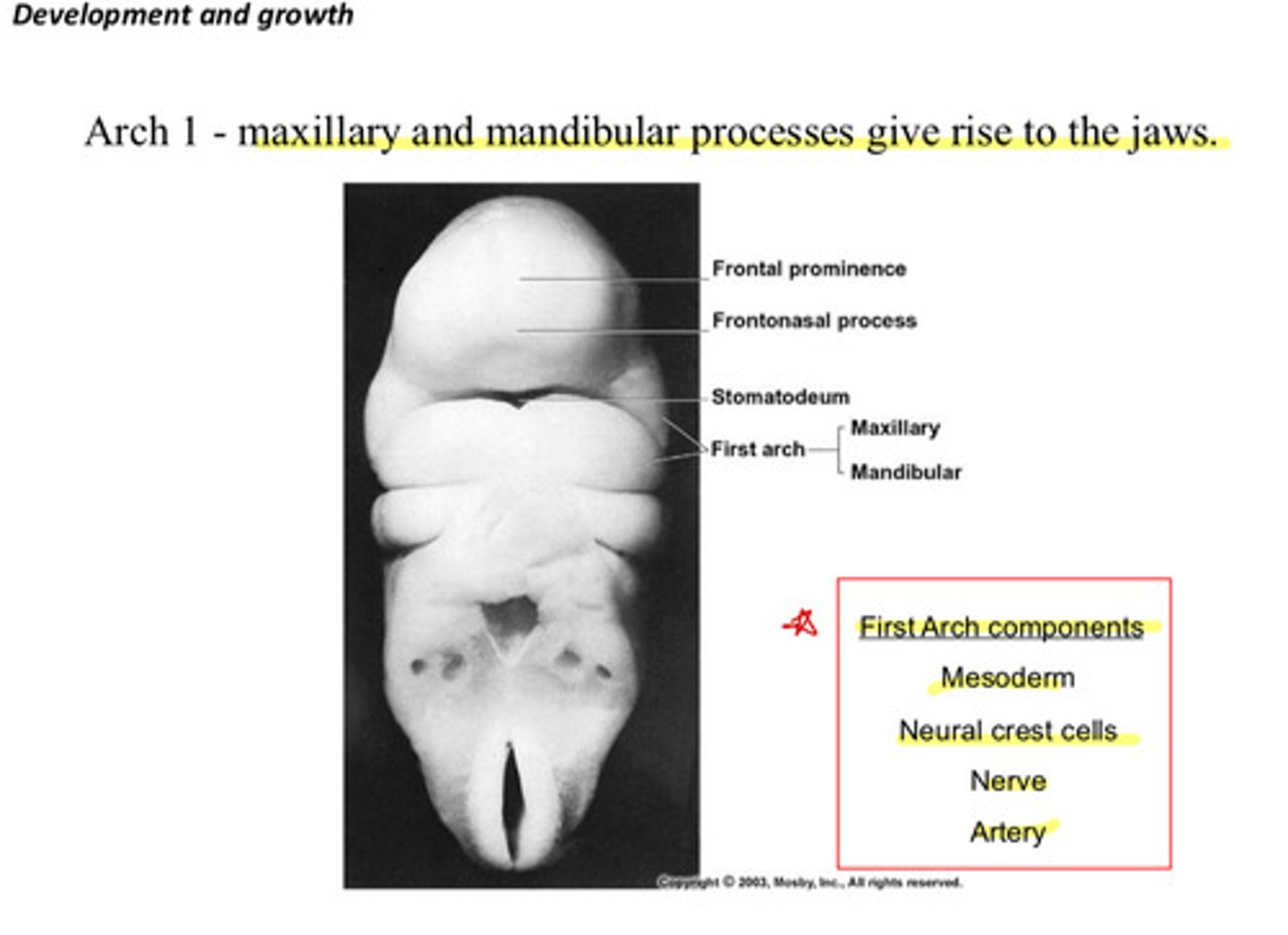
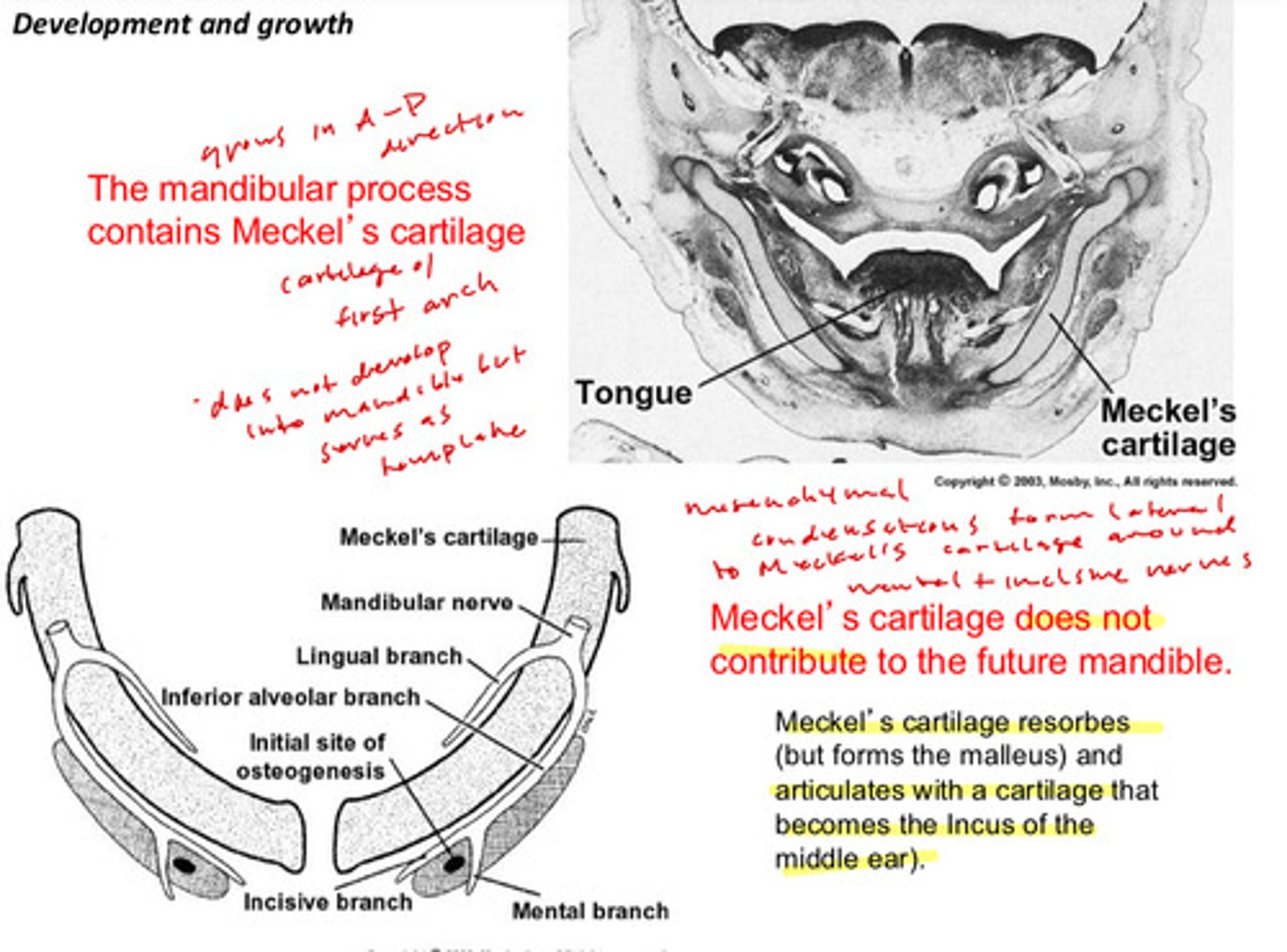
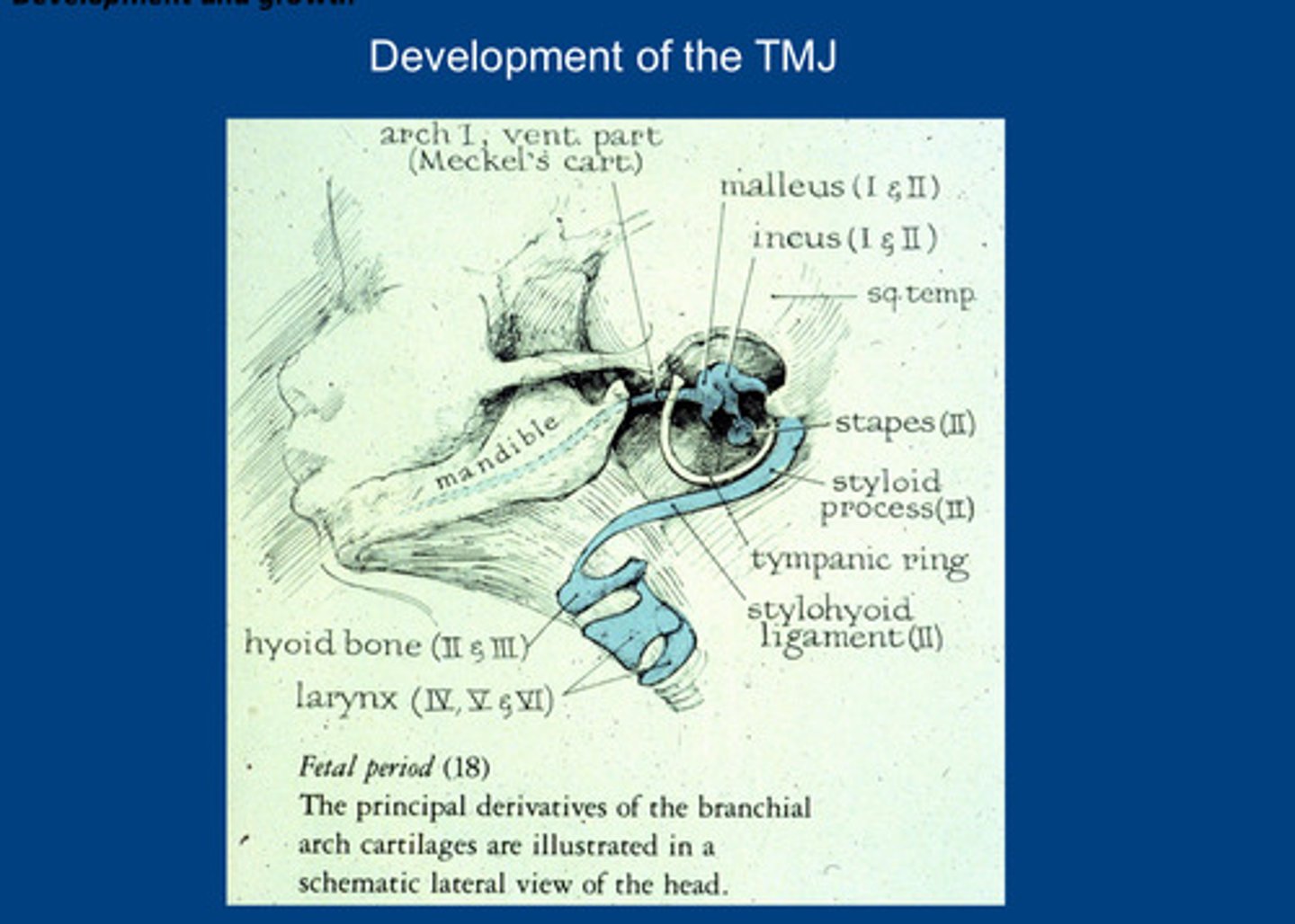
which embryological arch contributes to the jaws? (and what processes of this arch)
arch 1 (pharyngeal): maxillary and mandibular processes give rise to the jaws
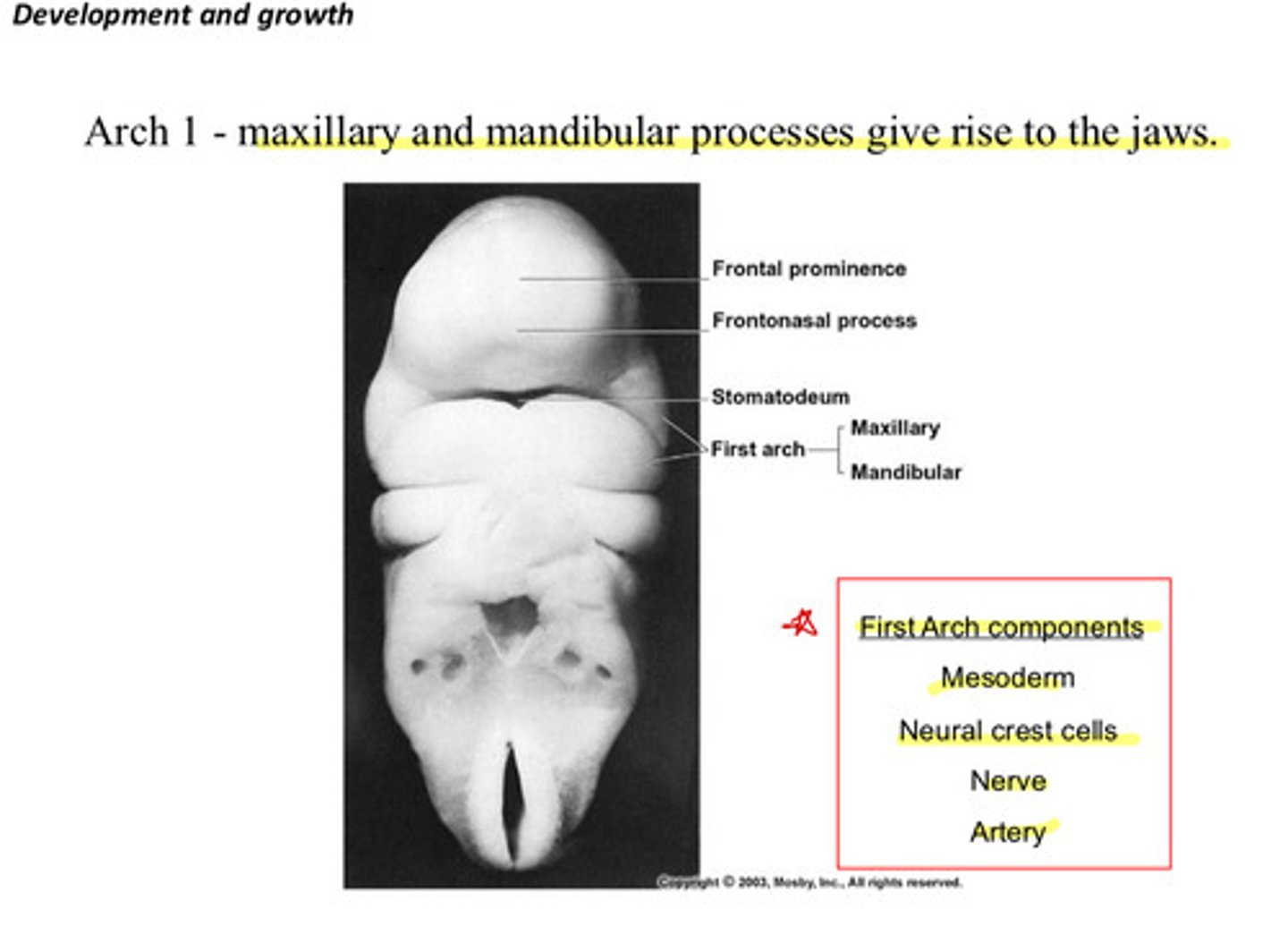
recall the 4 tissue components of the first pharyngeal arch
mesoderm, neural crest cells, nerve, artery
the mandibular process contains what cartilage that does NOT develop into the mandible but serves as a template
meckel's cartilage
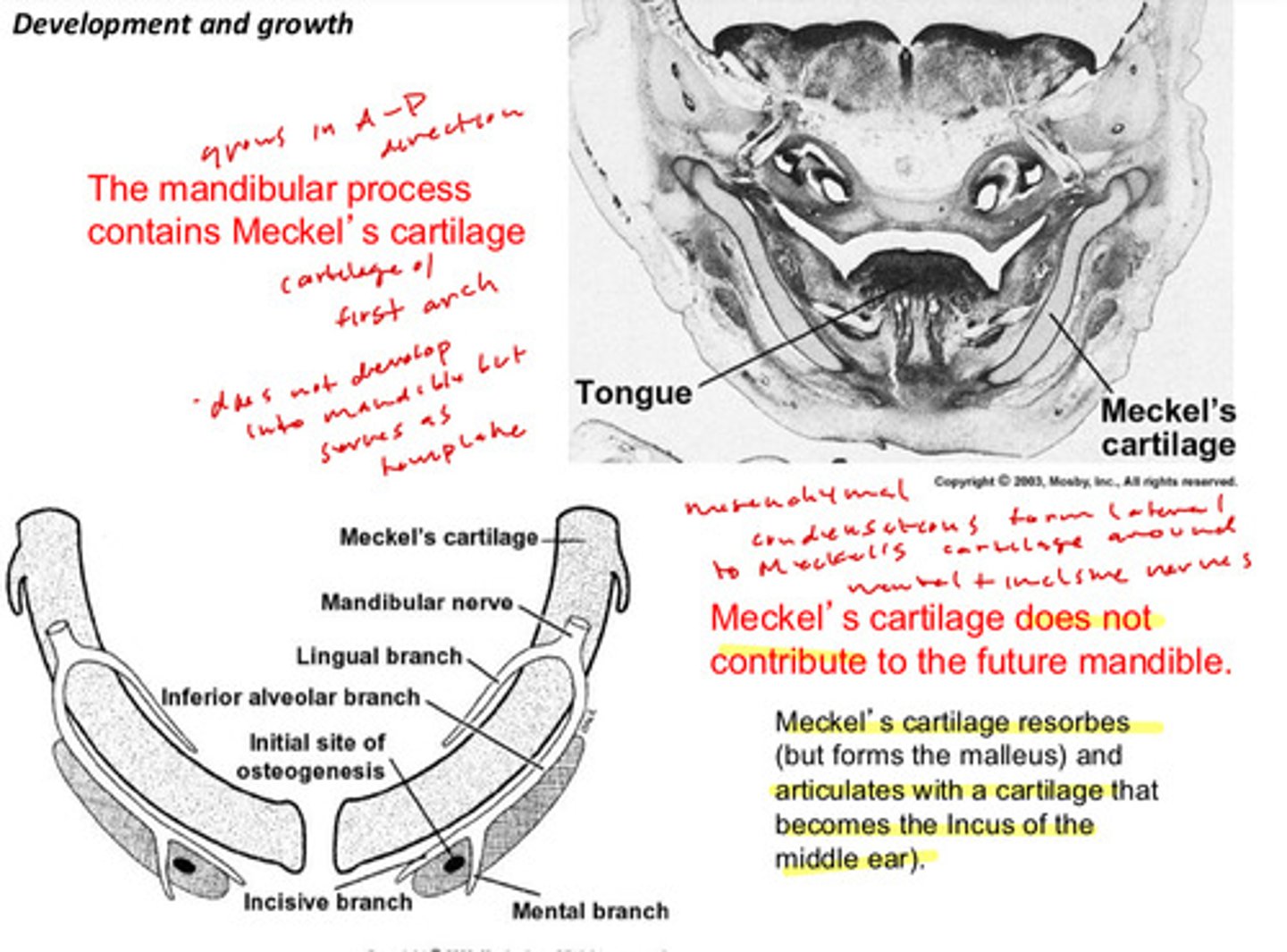
meckel's cartilage does not contribute to the future mandible, what does it end up becoming?
the cartilage resorbs, but forms the malleus and articulates with a cartilage that becomes the incus of the middle ear
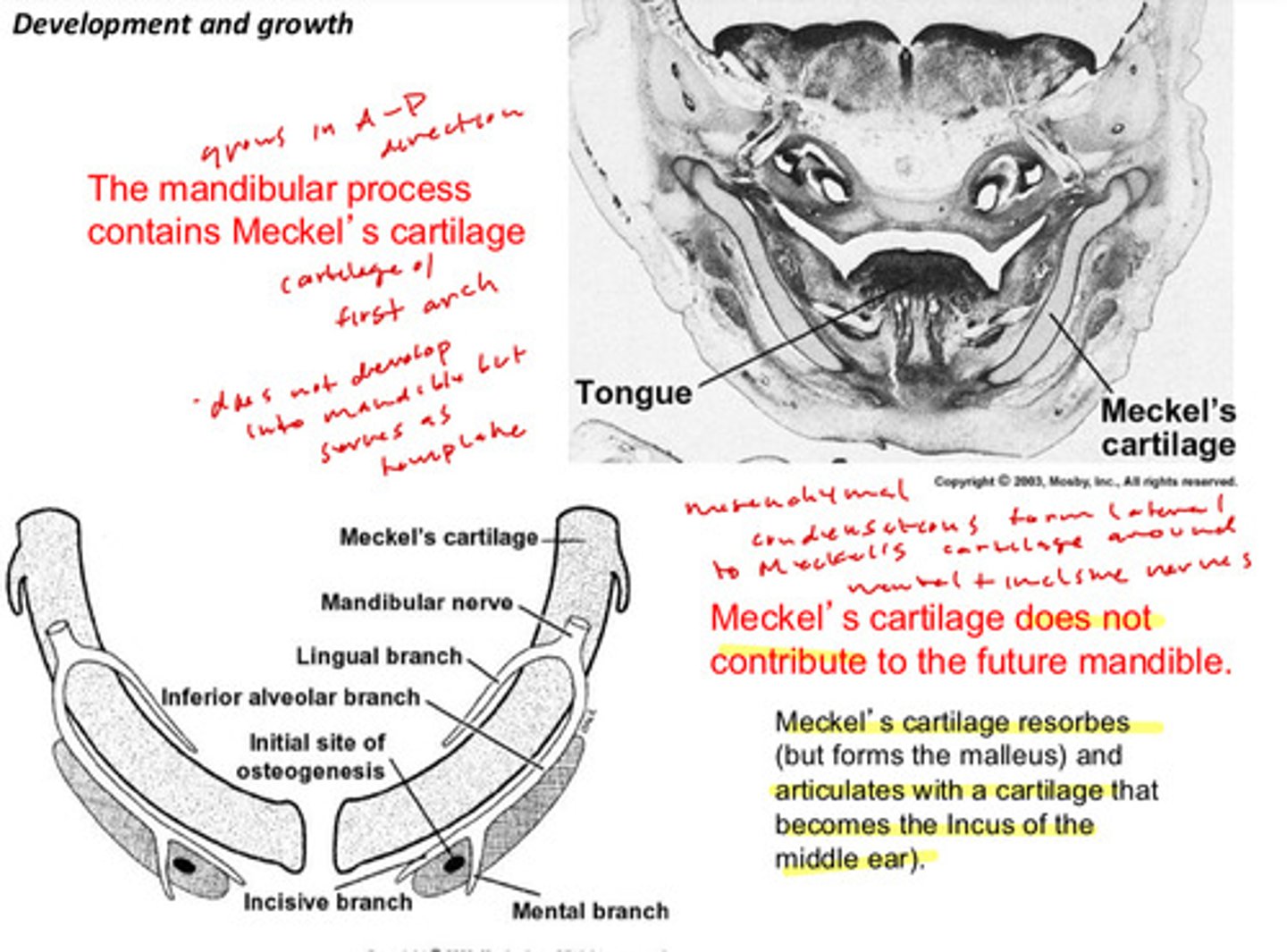
how does meckel's cartilage serve as a template for the mandible
mesenchymal condensations form lateral to meckel's cartilage around the mental and incisive nerves
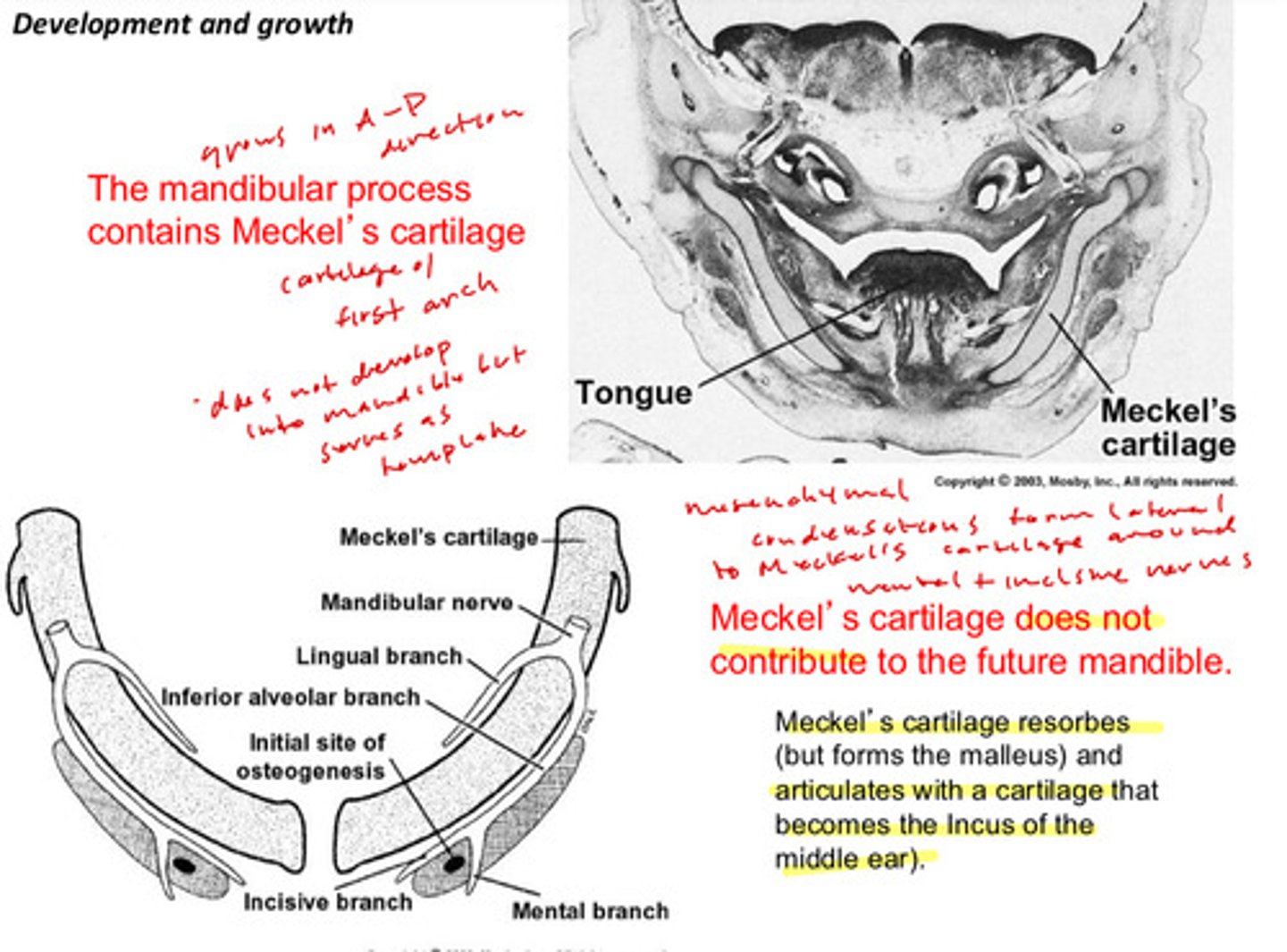
the mandibular process grows in which direction?
A-P
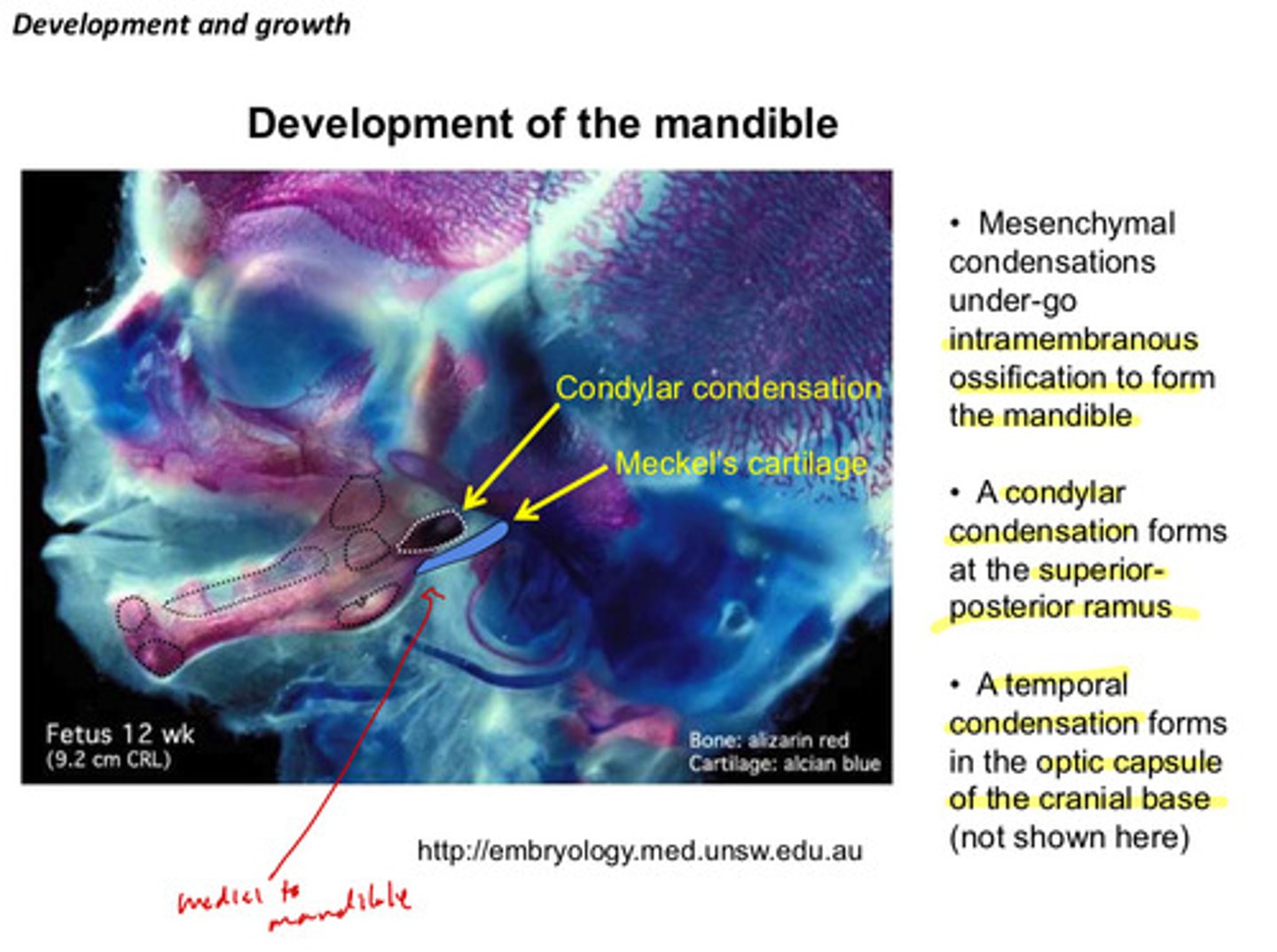
mesenchymal condensations under go what kind of ossification to form the mandible
intramembranous ossification
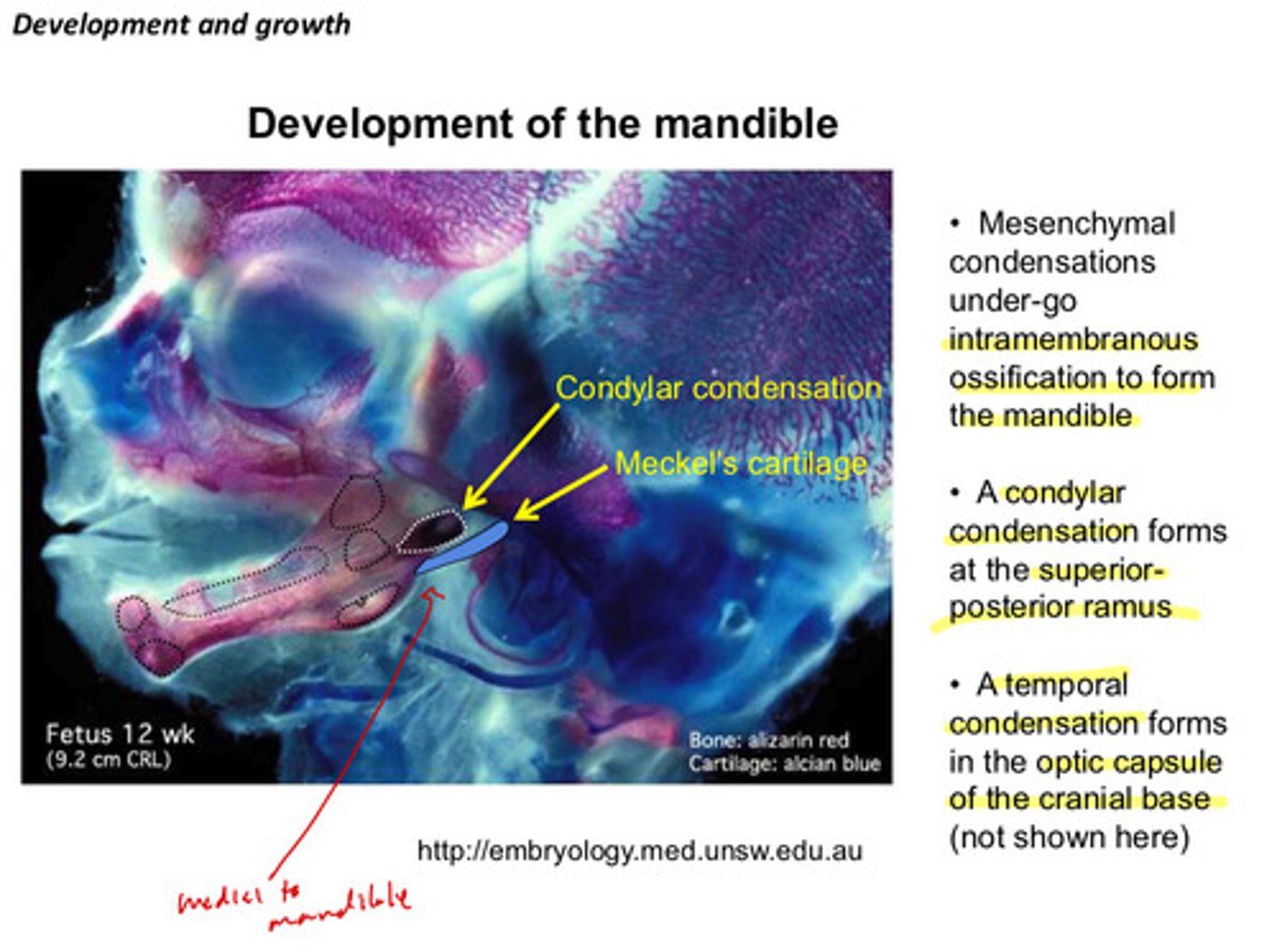
a condylar condensation forms at what structure
at the superior posterior ramus
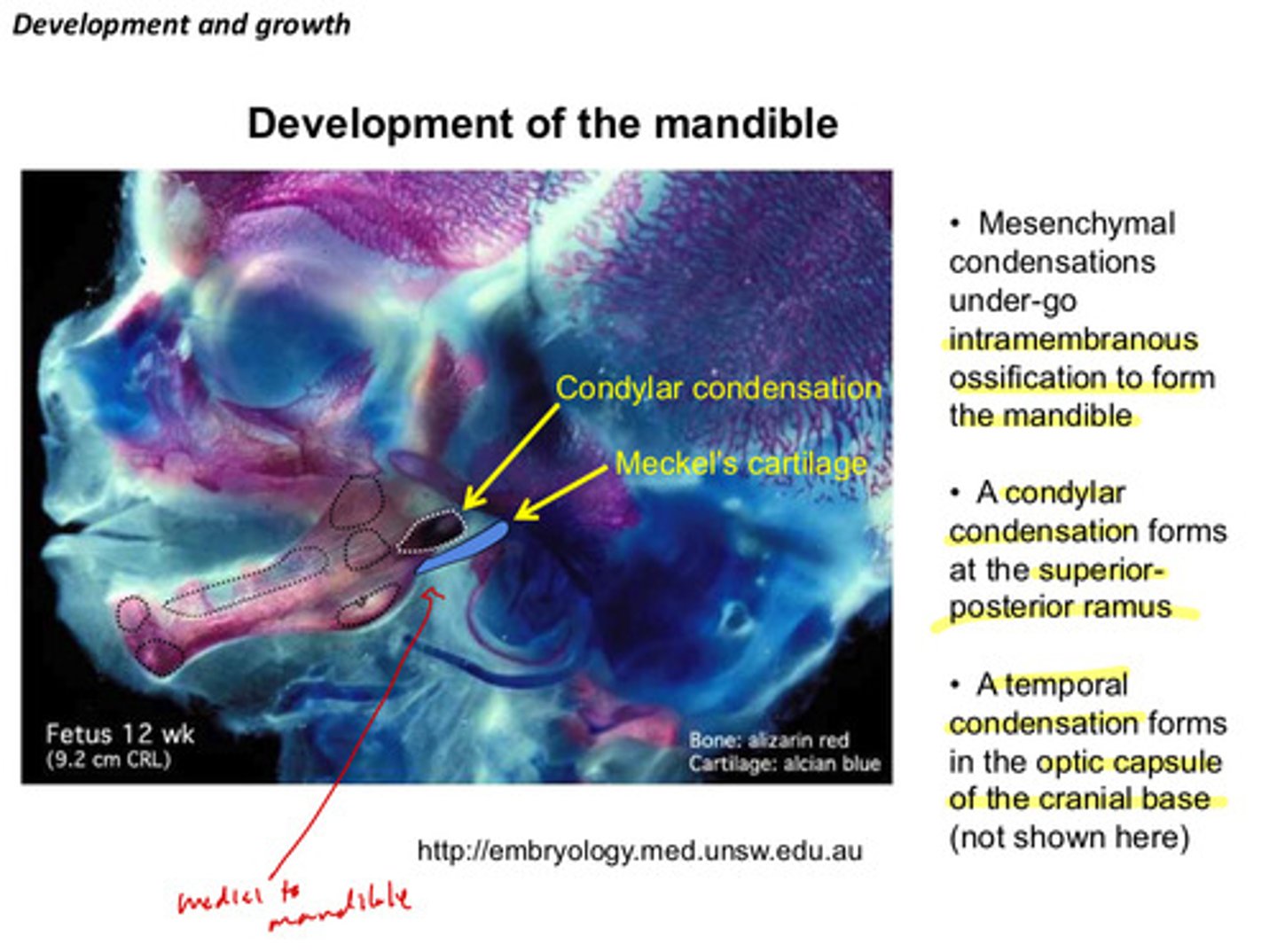
a temporal condensation forms in which structure of the cranial base
in the optic capsule
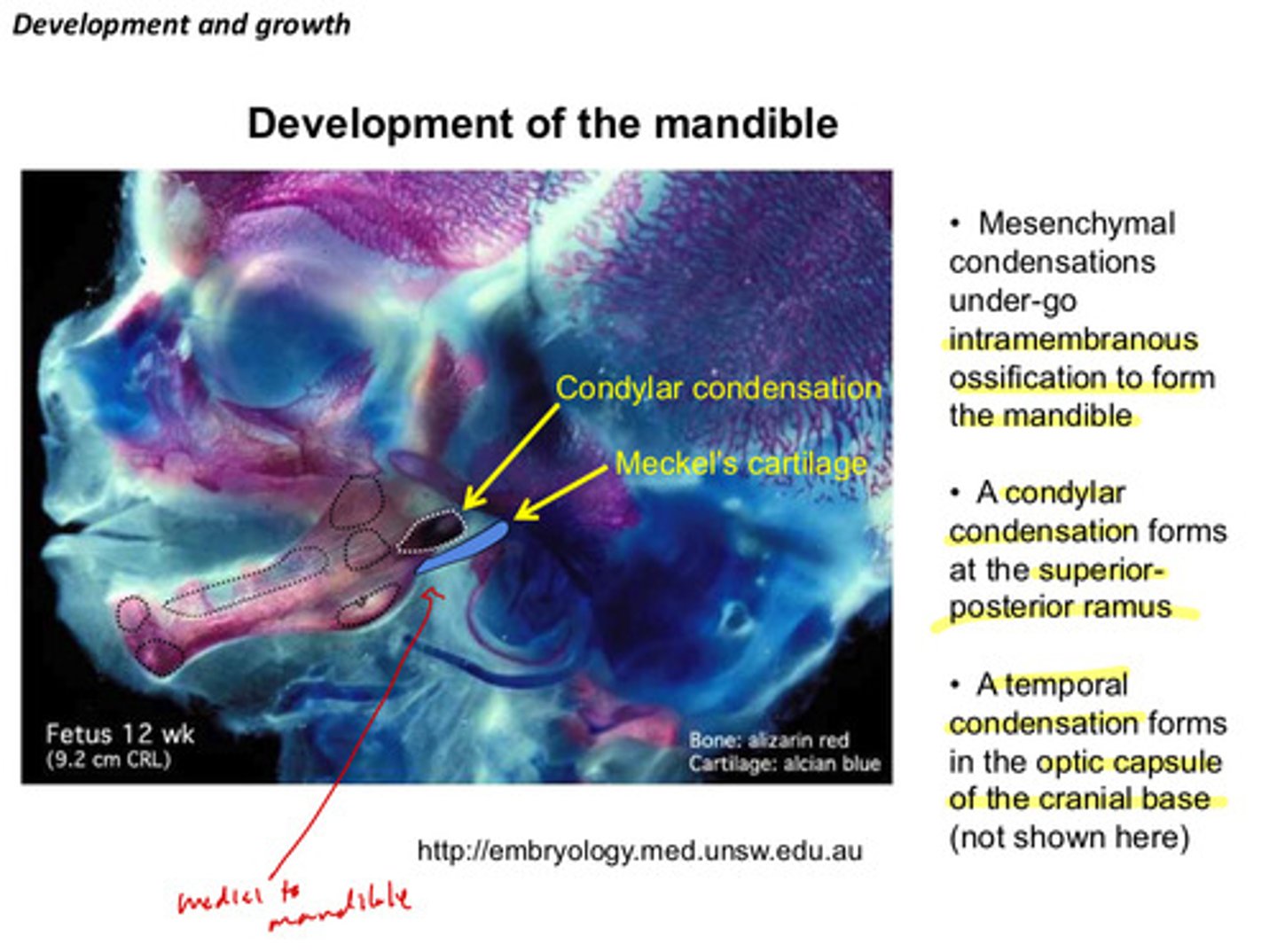
recall: where is meckel's cartilage before it resorbs in relation to the developing mandible
medial to mandible
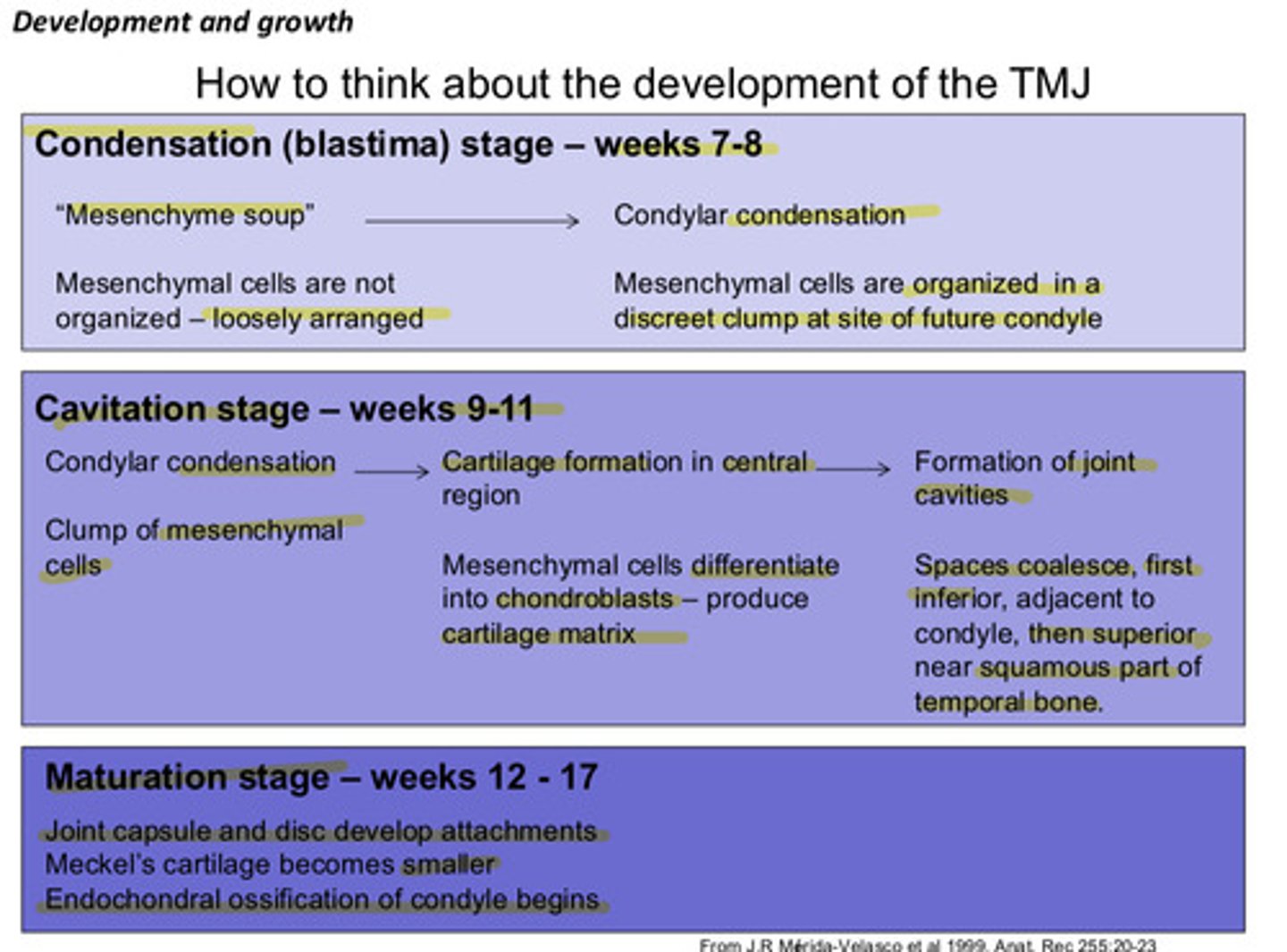
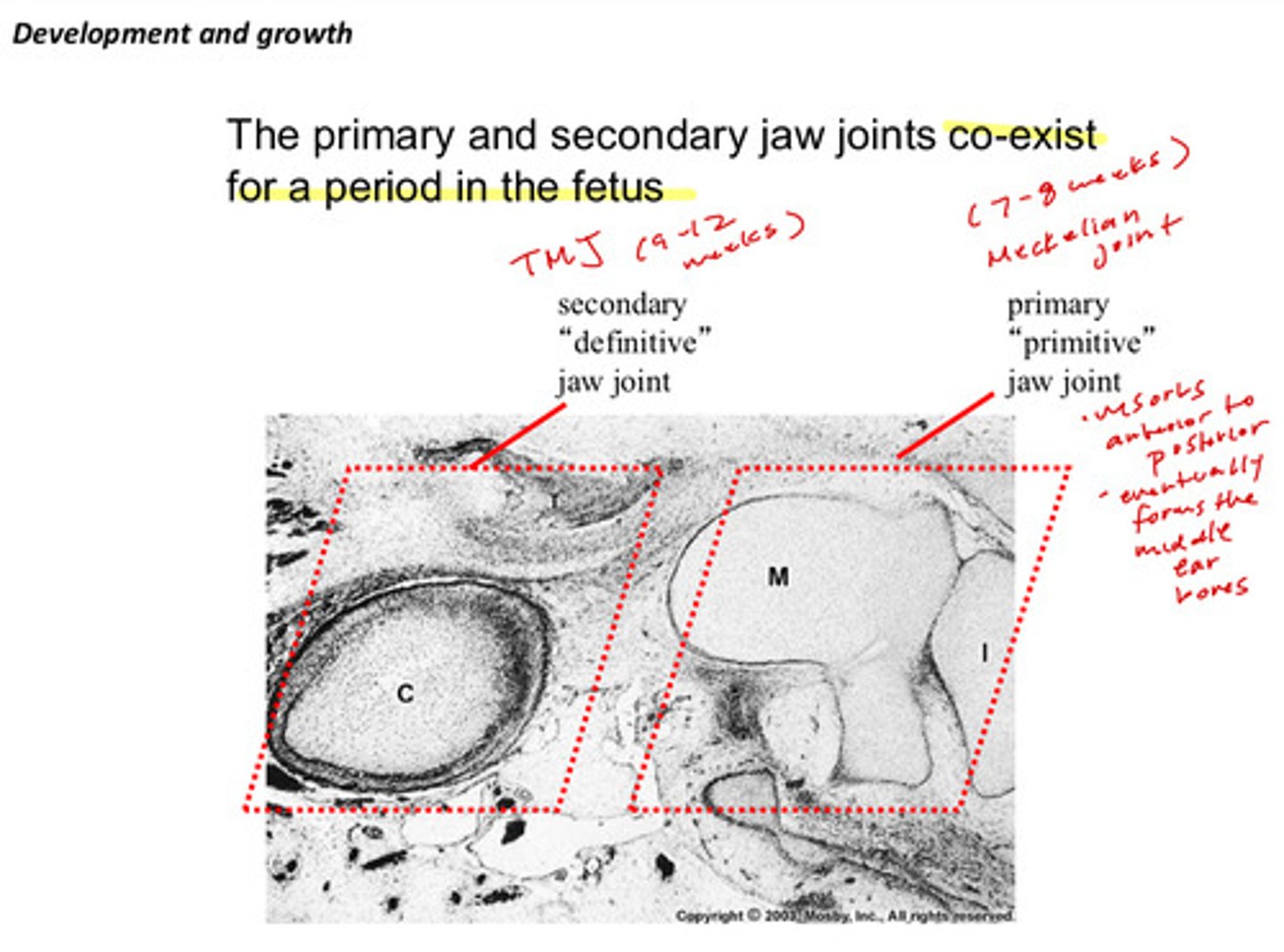
what are the 3 main stages of the development of the TMJ and during which weeks of development do they occur?
1) condensation (blastima) stage: weeks 7-8
2) cavitation stage: weeks 9-11
3) maturation stage: weeks 12-17
describe the condensation stage and what we see (2)
1) "mesenchyme soup": mesenchymal cells are not organized - loosely arranged
2) condylar condensation: mesenchymal cells are organized in a discreet clump at site of future condyle
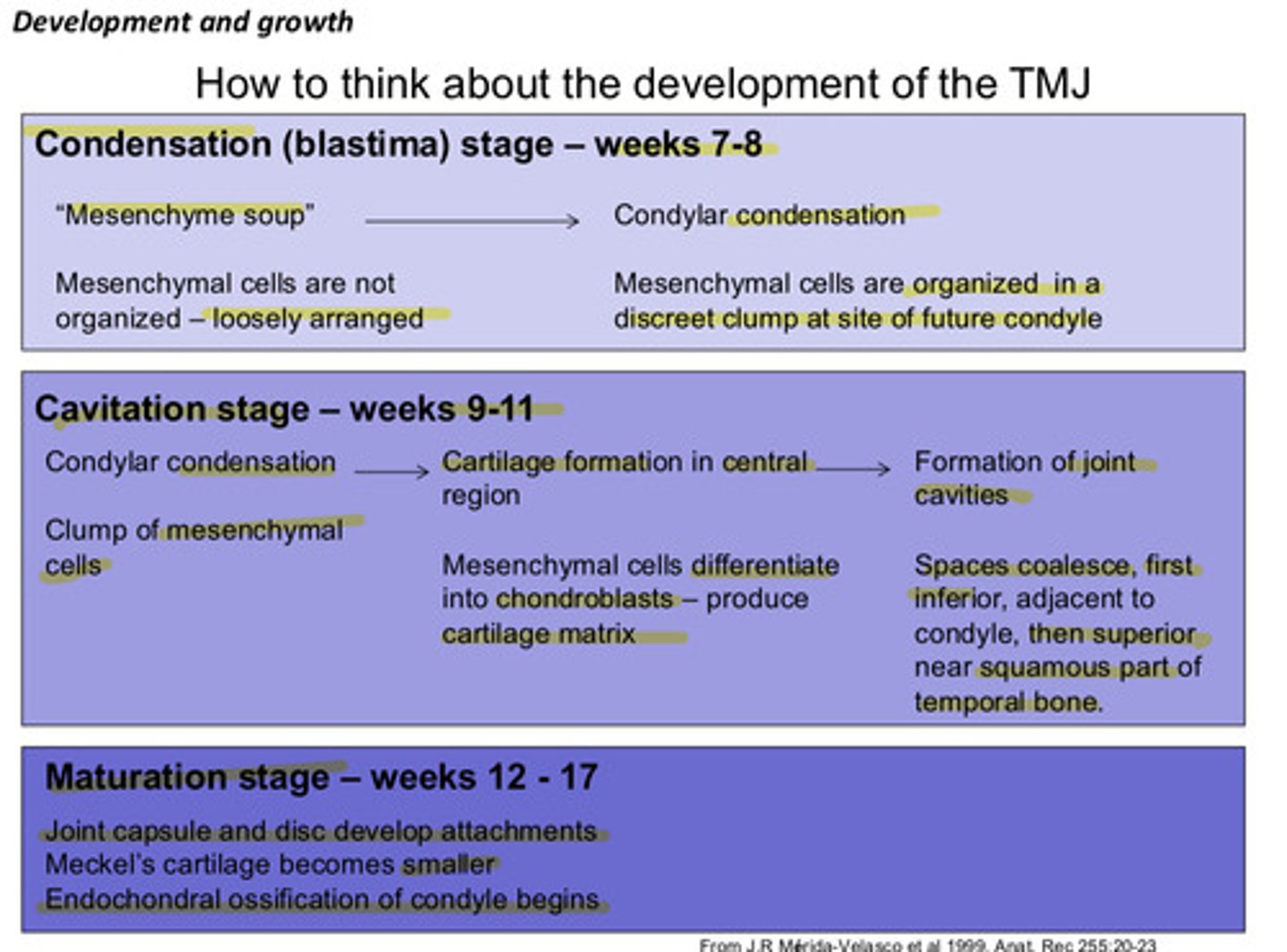
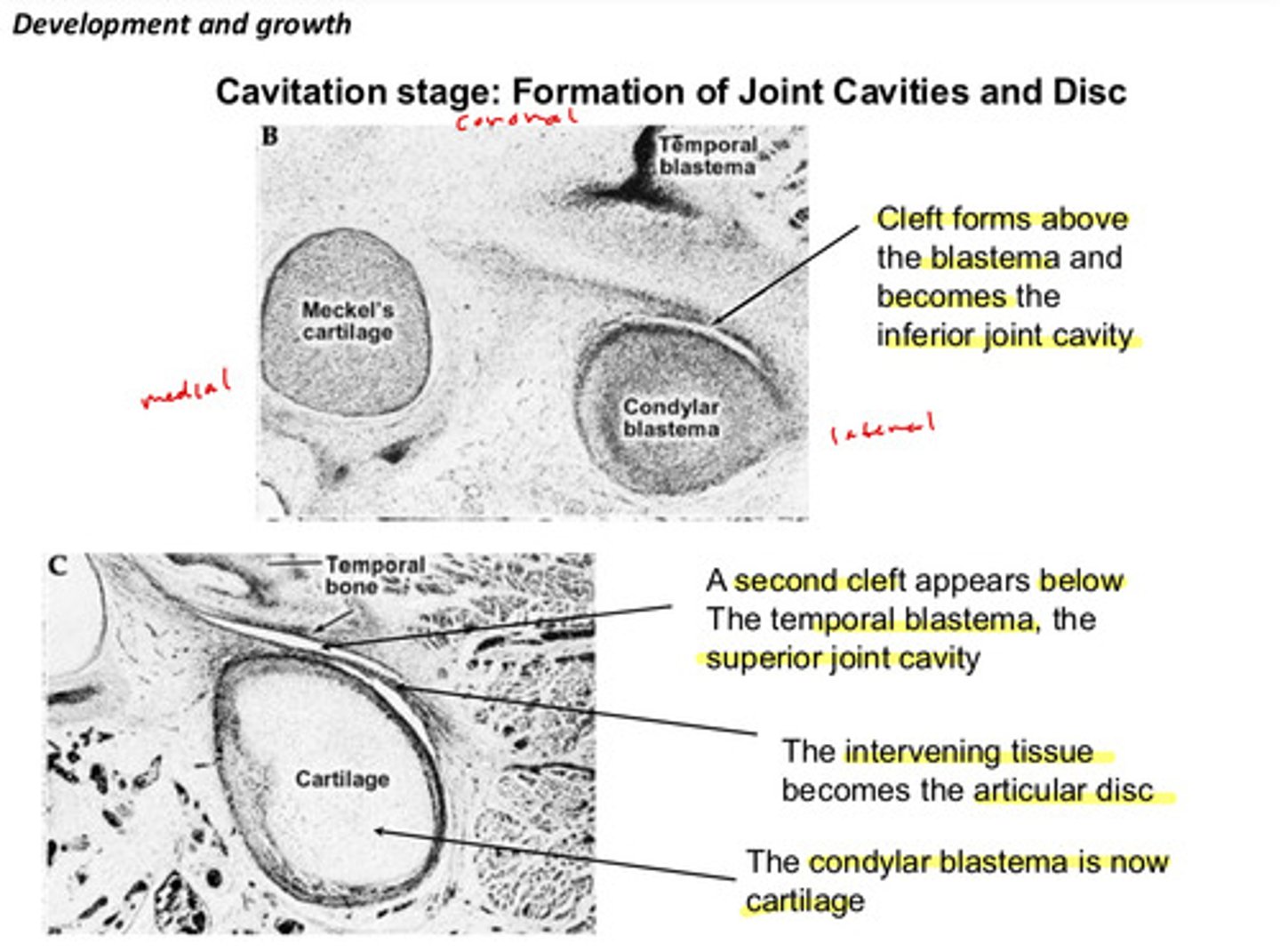
describe the cavitation stage and what we see (3)
1) condylar condensation: clump of mesenchymal cells
2) cartilage formation in central region: mesenchymal cells differentiate into chondroblasts — produce cartilage matrix
3) formation of joint cavities: spaces coalesce, first inferior, adjacent to condyle, then superior near squamous part of temporal bone
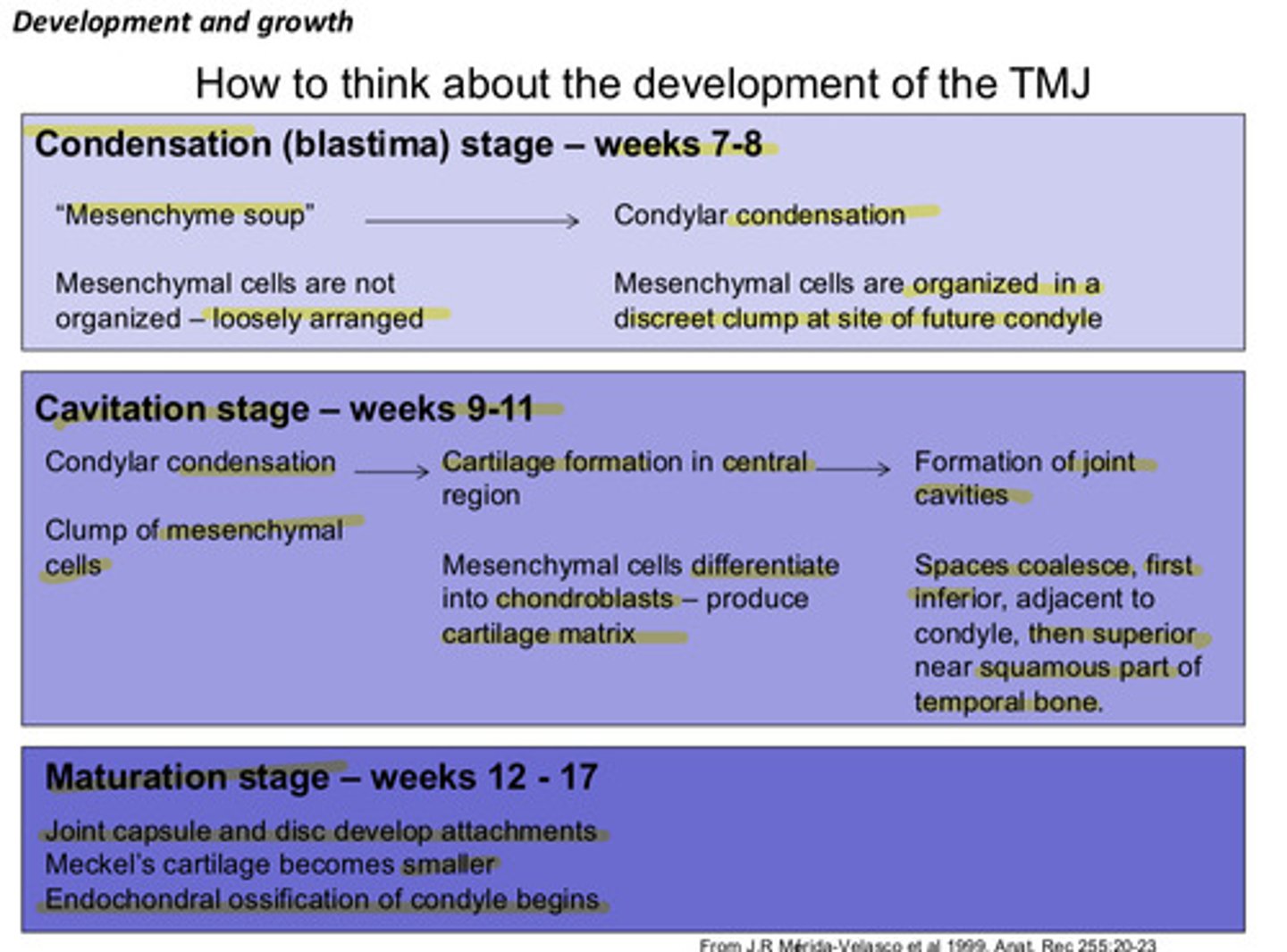
describe the maturation stage and what we see (3)
1) joint capsule and disc develop attachments
2) meckel's cartilage becomes smaller
3) endochondral ossification of condyle begins
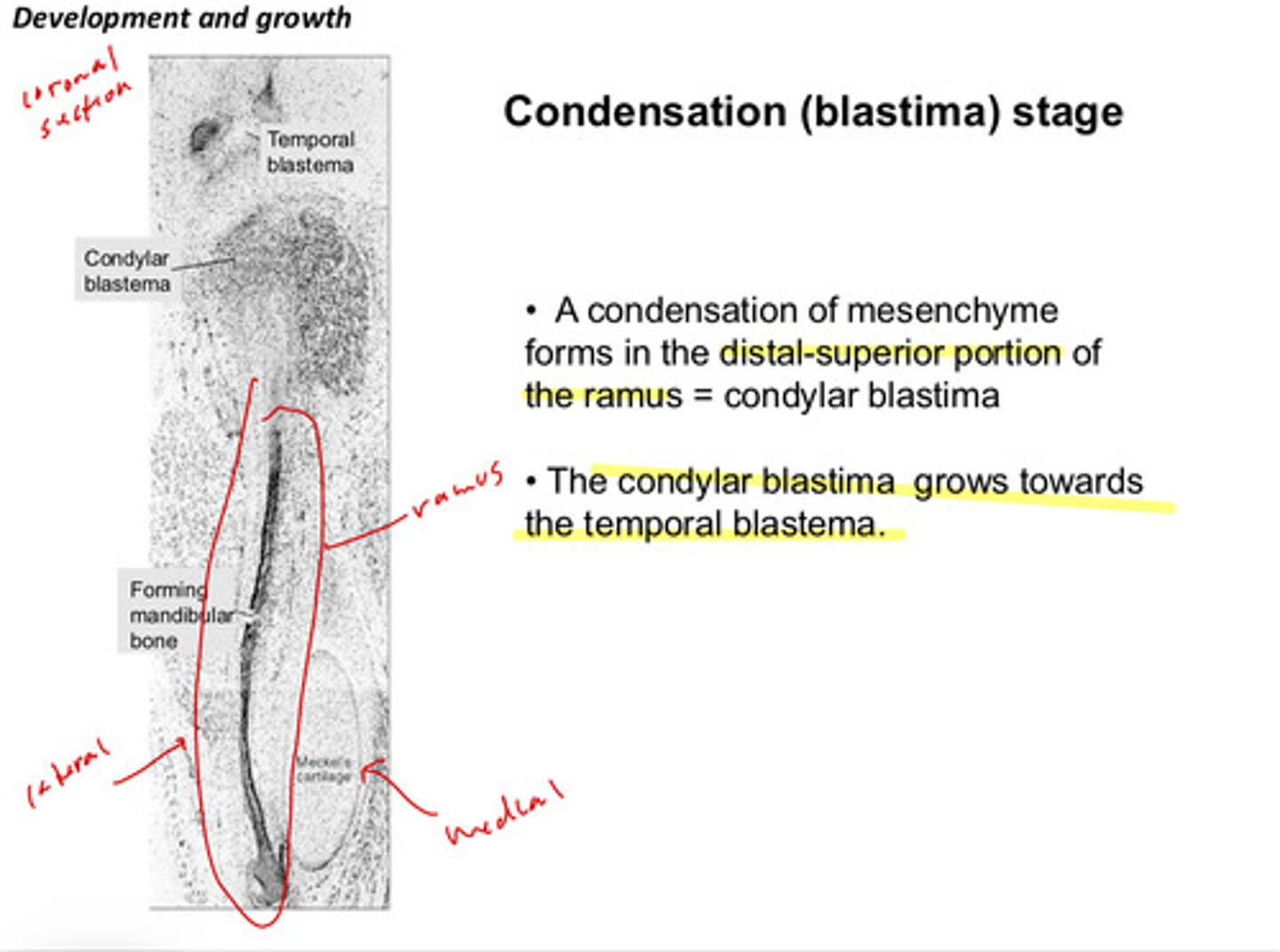
in the condensation (blastima) stage: a condensation of mesenchyme forms in the distal superior portion of the ramus, what is this condensation called?
condylar blastima
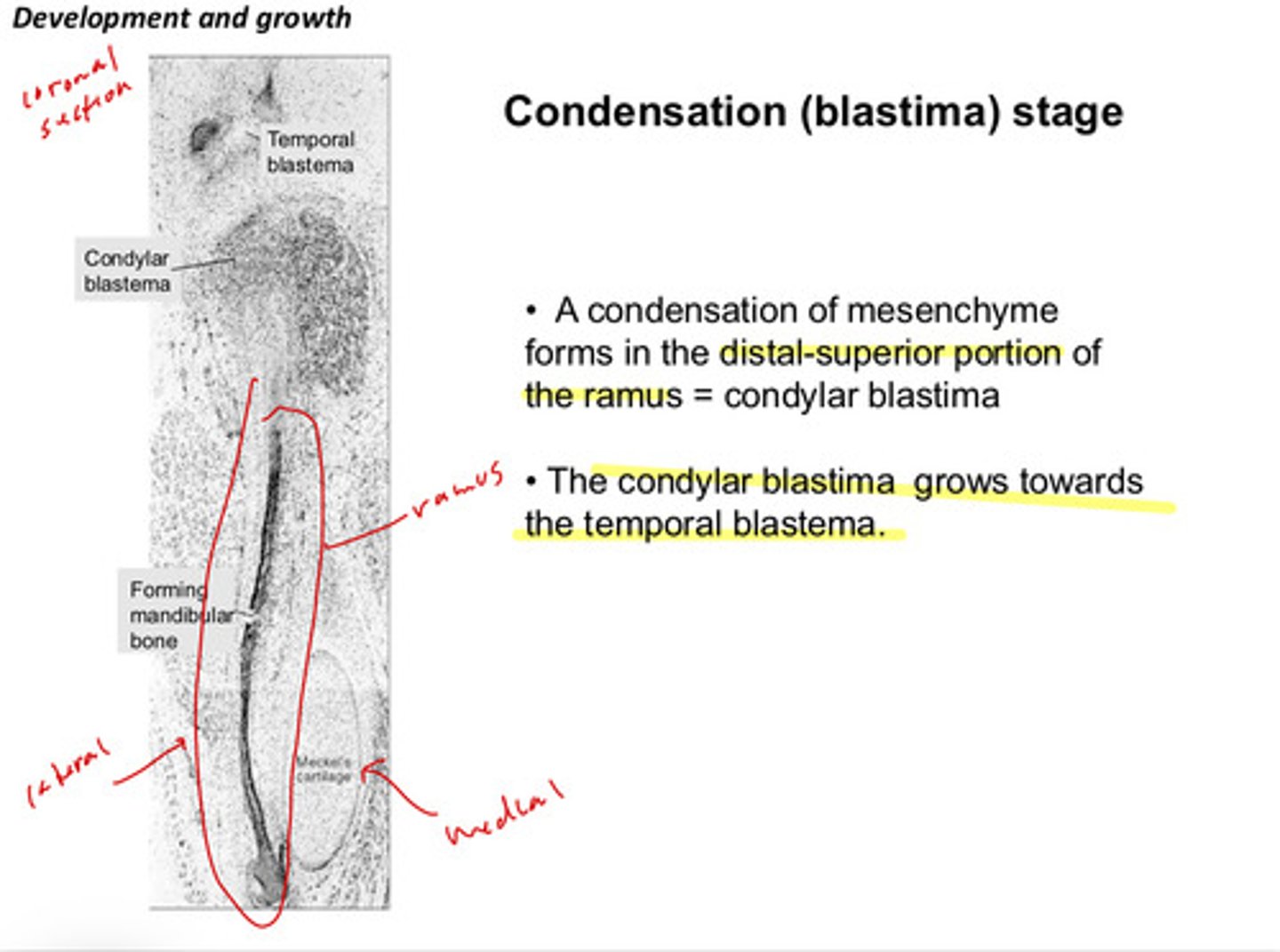
in the condensation stage: the condylar blastima grows toward the ________ blastima
temporal blastima
in the cavitation stage, we see the formation of the joint cavities and the disc. the first cleft forms above the condylar blastima and becomes what
the inferior joint cavity
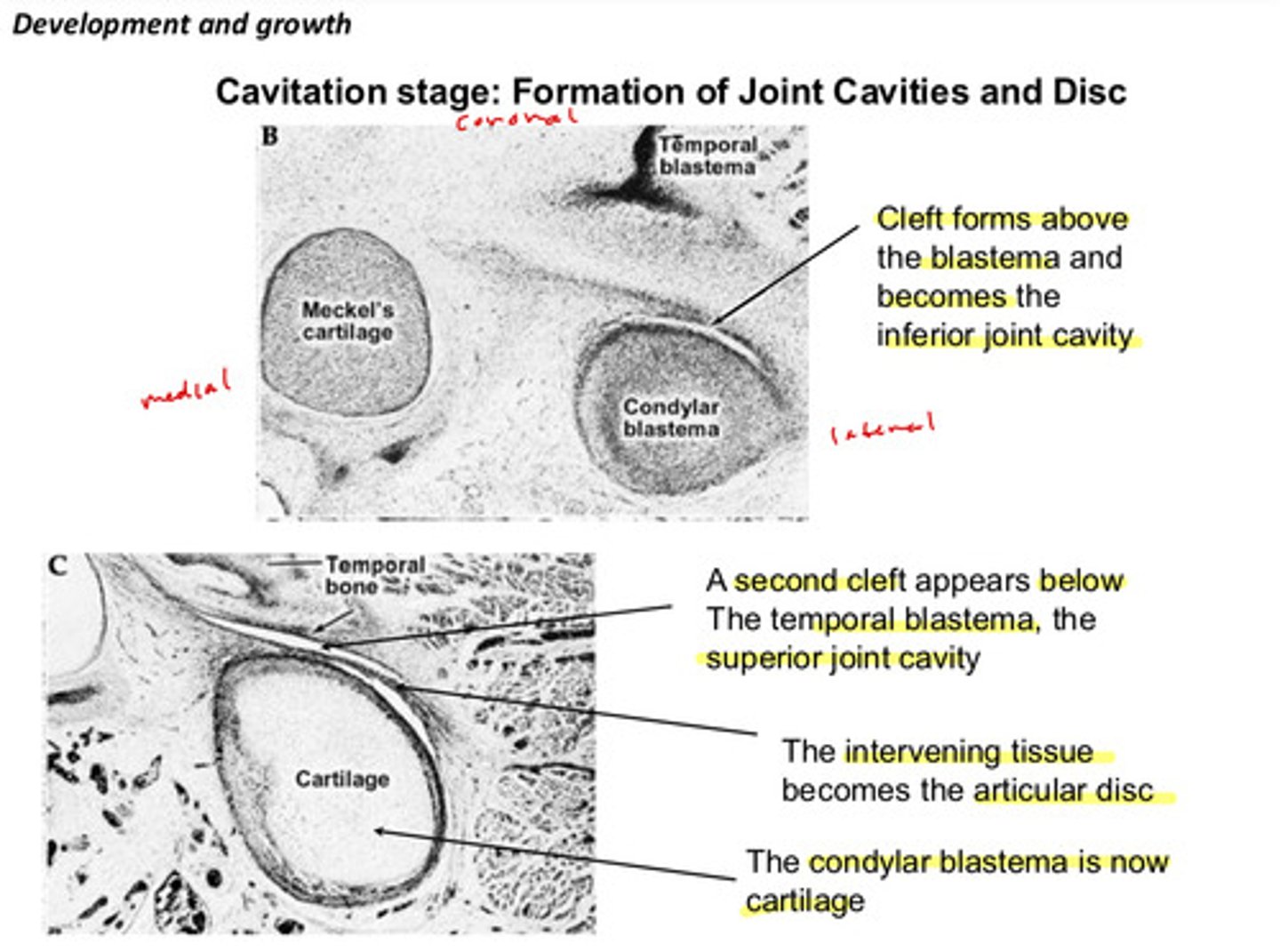
in the cavitation stage: a second cleft appears below the ______ blastima and becomes what?
the temporal blastima, becomes the superior joint cavity
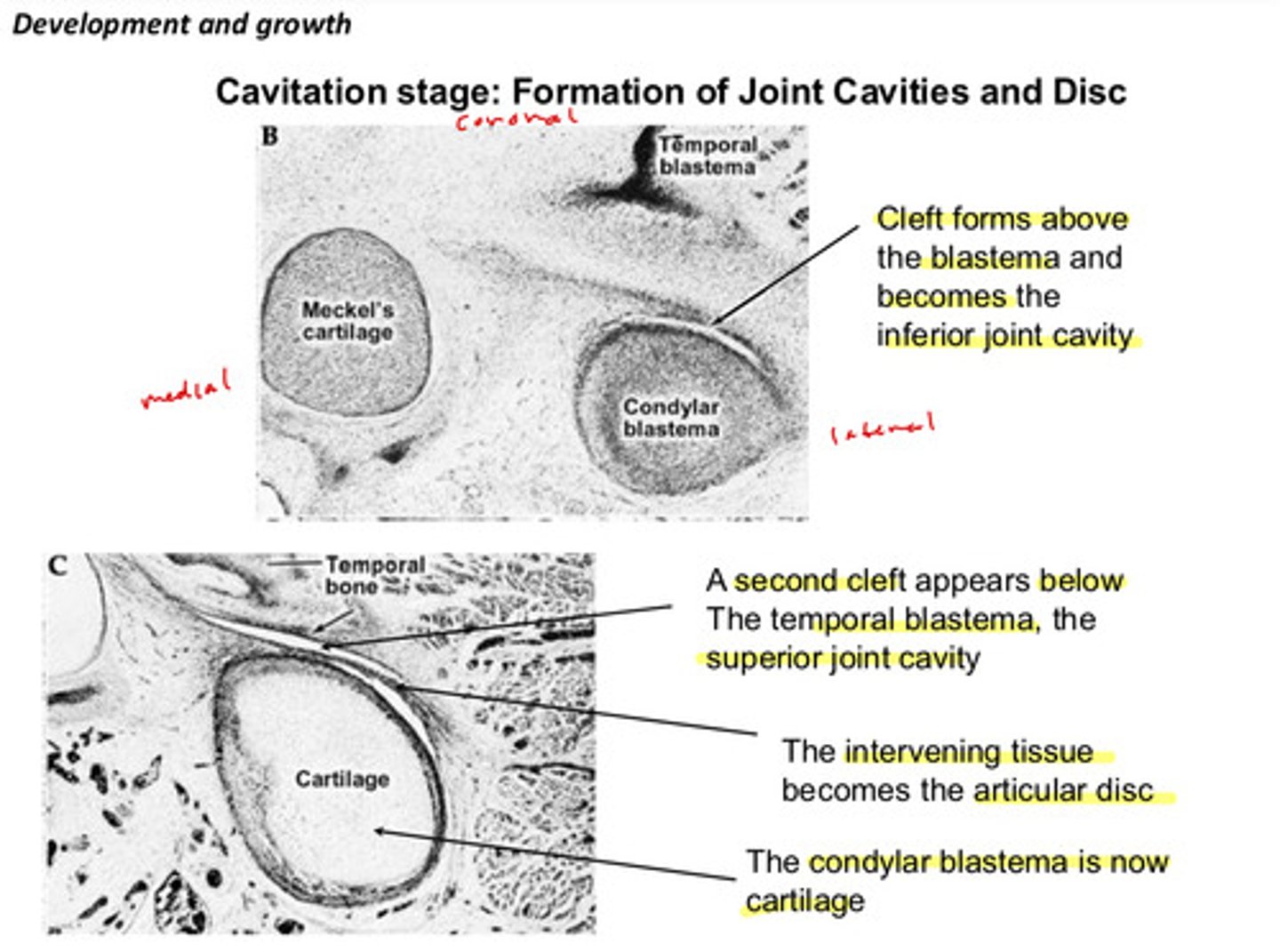
in the cavitation stage: the tissue between the 2 formed clefts becomes what
the articular disc
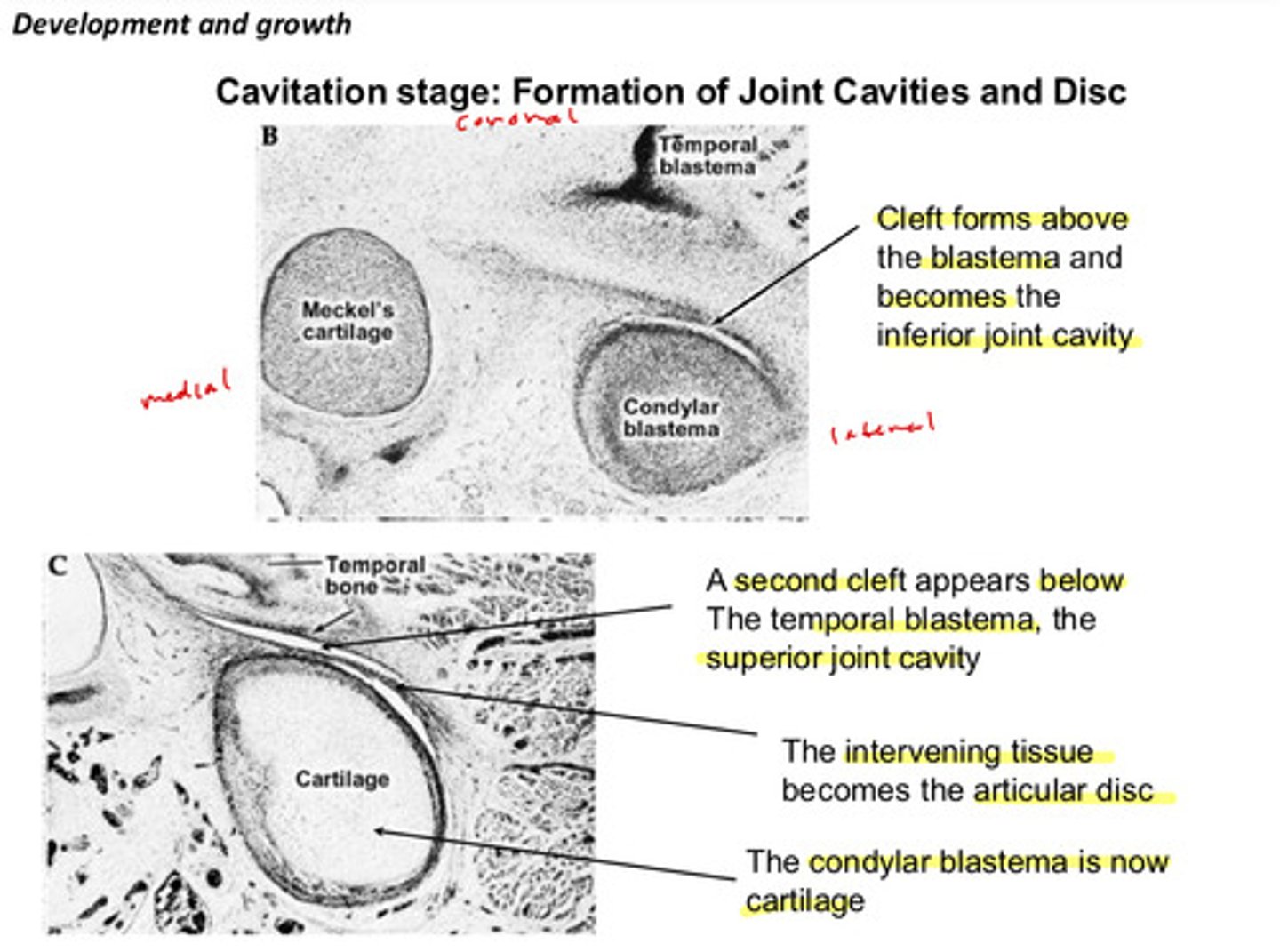
in the cavitation stage: after the second cleft forms becoming the superior joint cavity, the condylar blastima is now ?
is now cartilage
in the maturation stage, what generally happens?
tissues attain mature morphology
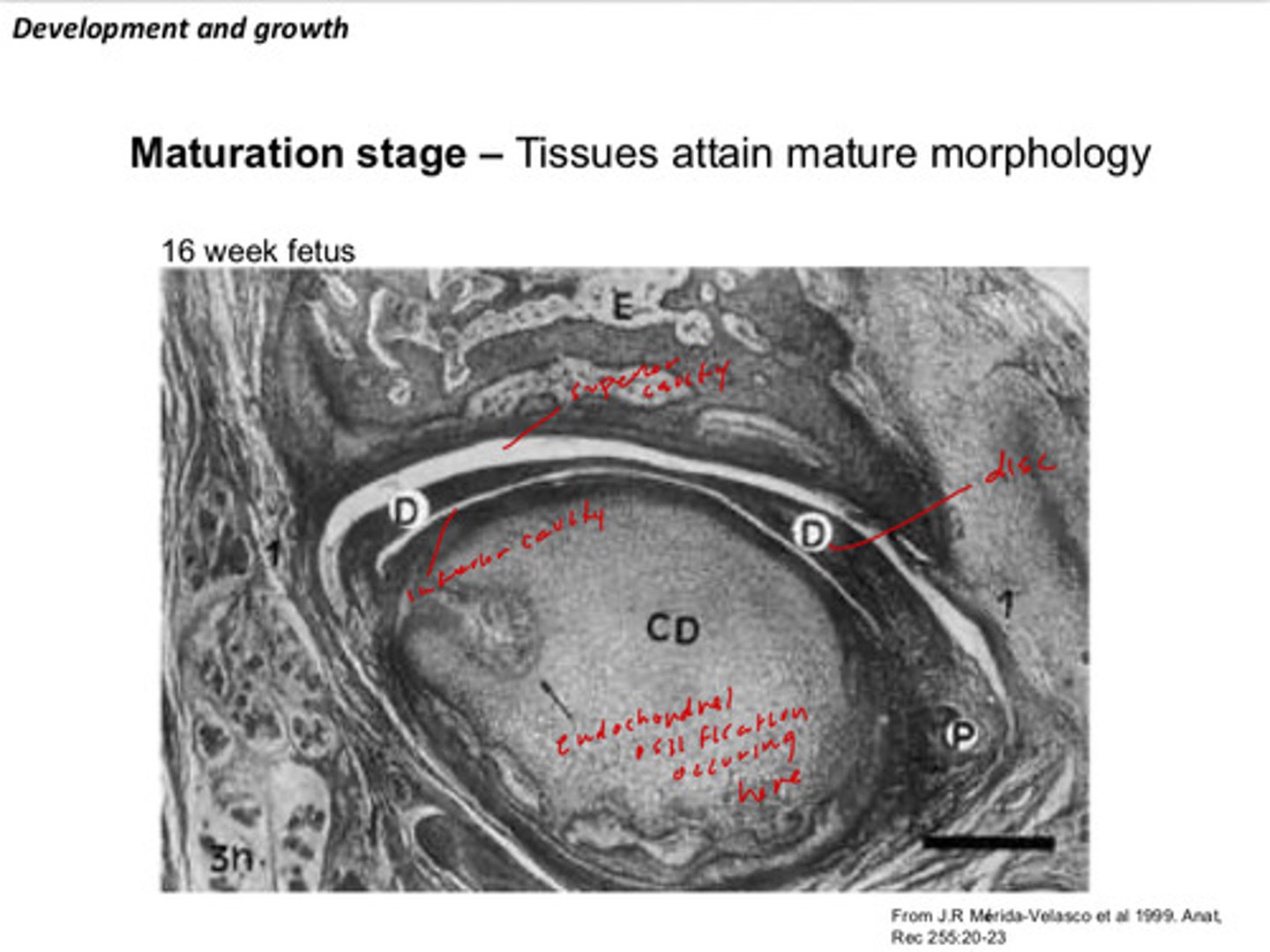
what kind of ossification does the condylar cartilage undergo
endochondral ossification
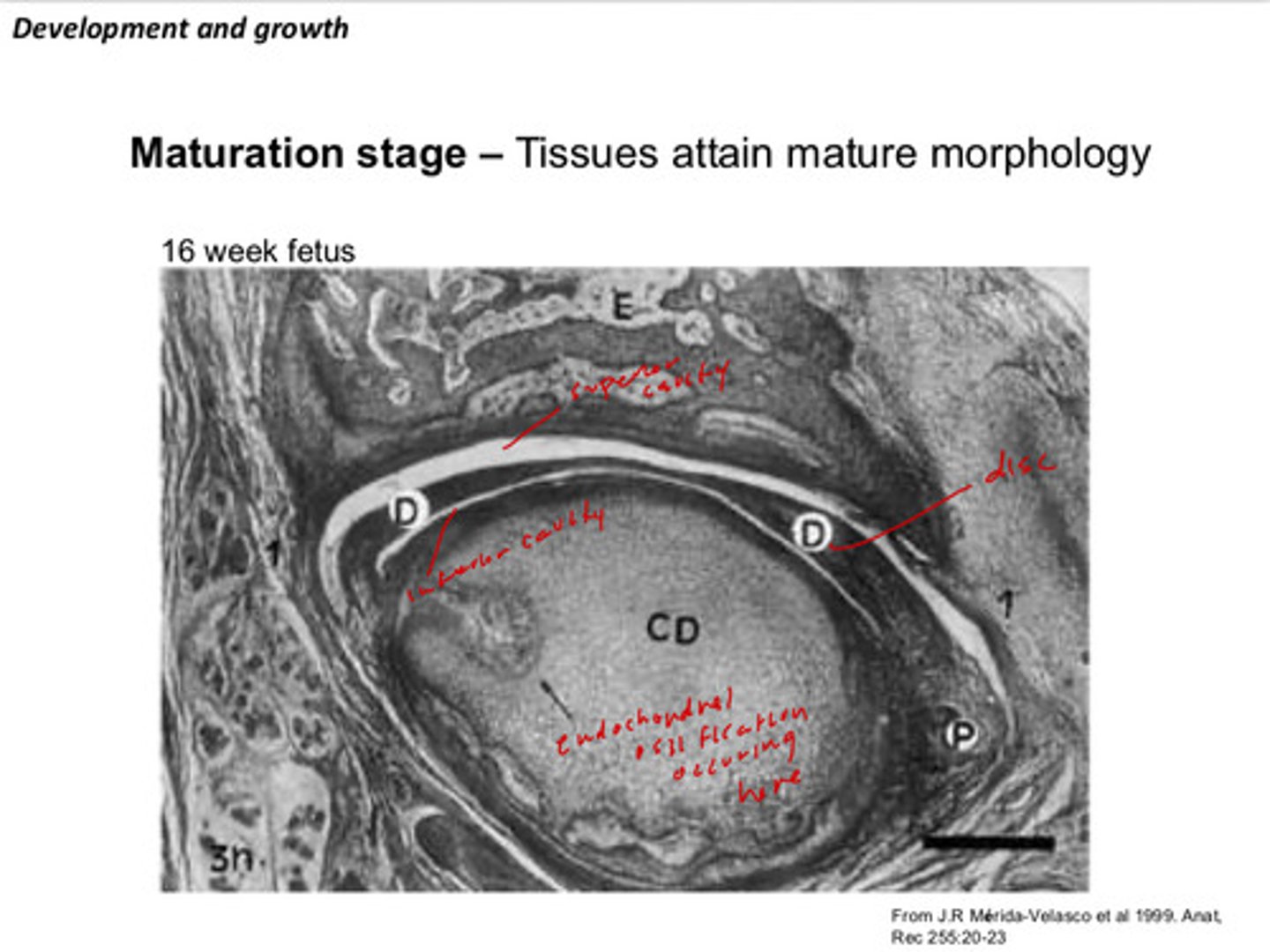
image of the development of the TMJ in relation to the first pharyngeal arch
the primary and secondary jaw joints co-exist for a period in the fetus. describe what this means?
meckel's cartilage/meckelian joint acts as a primary "primitive" jaw joint (this later resorbs anterior to posterior to eventually form the middle ear bones) and the TMJ is the secondary "definitive" jaw joint; they coexist around weeks 10-20 of embryo development
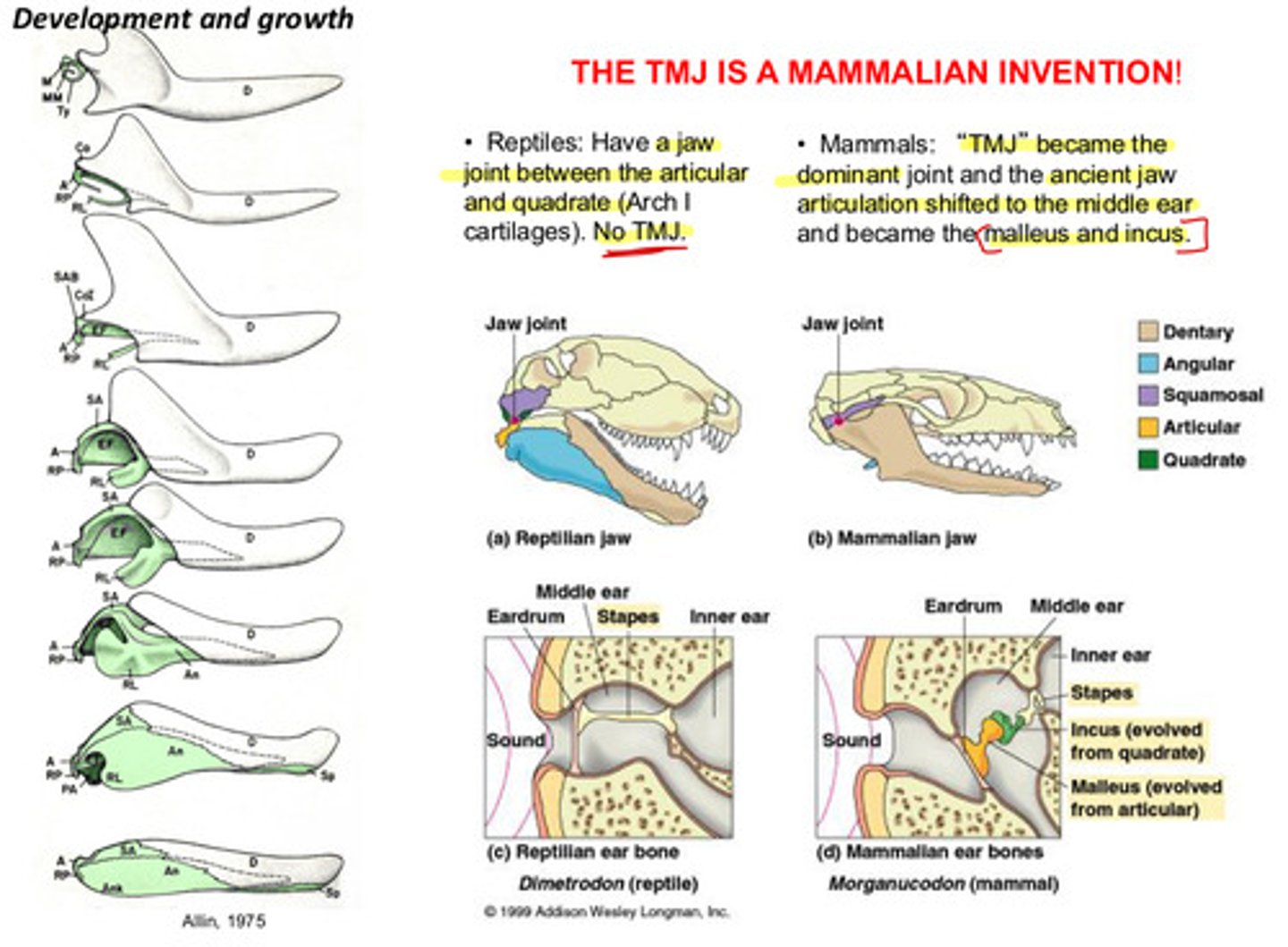
recall: the TMJ is a mammalian invention!
reptiles do NOT have a TMJ, but they do have a jaw joint between the articular and quadrate cartilages
mammals do have a TMJ which became the dominant joint and the ancient jaw articulation shifted to the middle ear bones
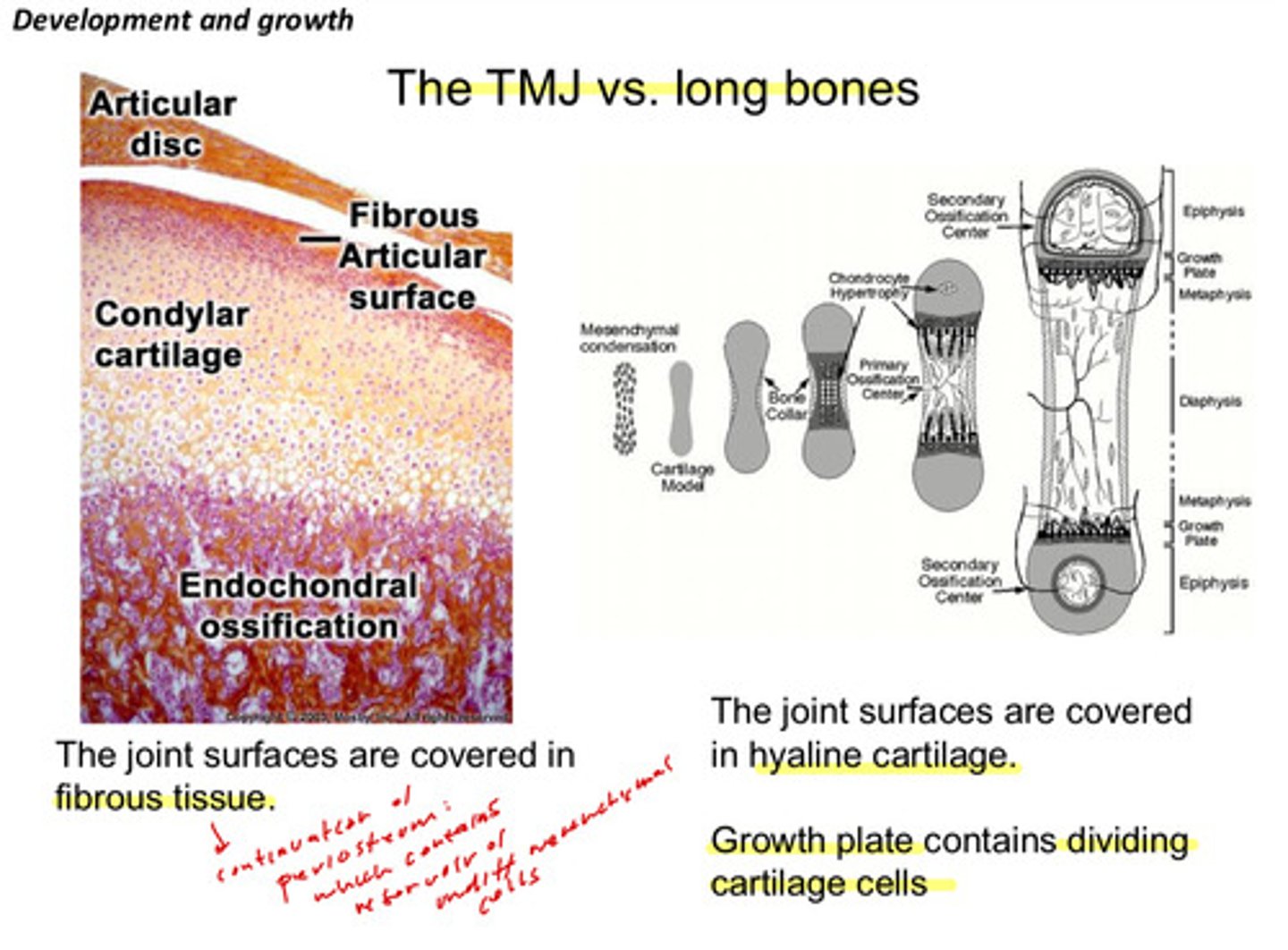
what is the difference between TMJ and long bones?
the TMJ surfaces are covered in fibrous tissue (fibrocartilage) and is a secondary cartilage; long bone joint surfaces are covered in hyaline cartilage and is a primary cartilage (the long bone growth plates contain dividing cartilage cells)
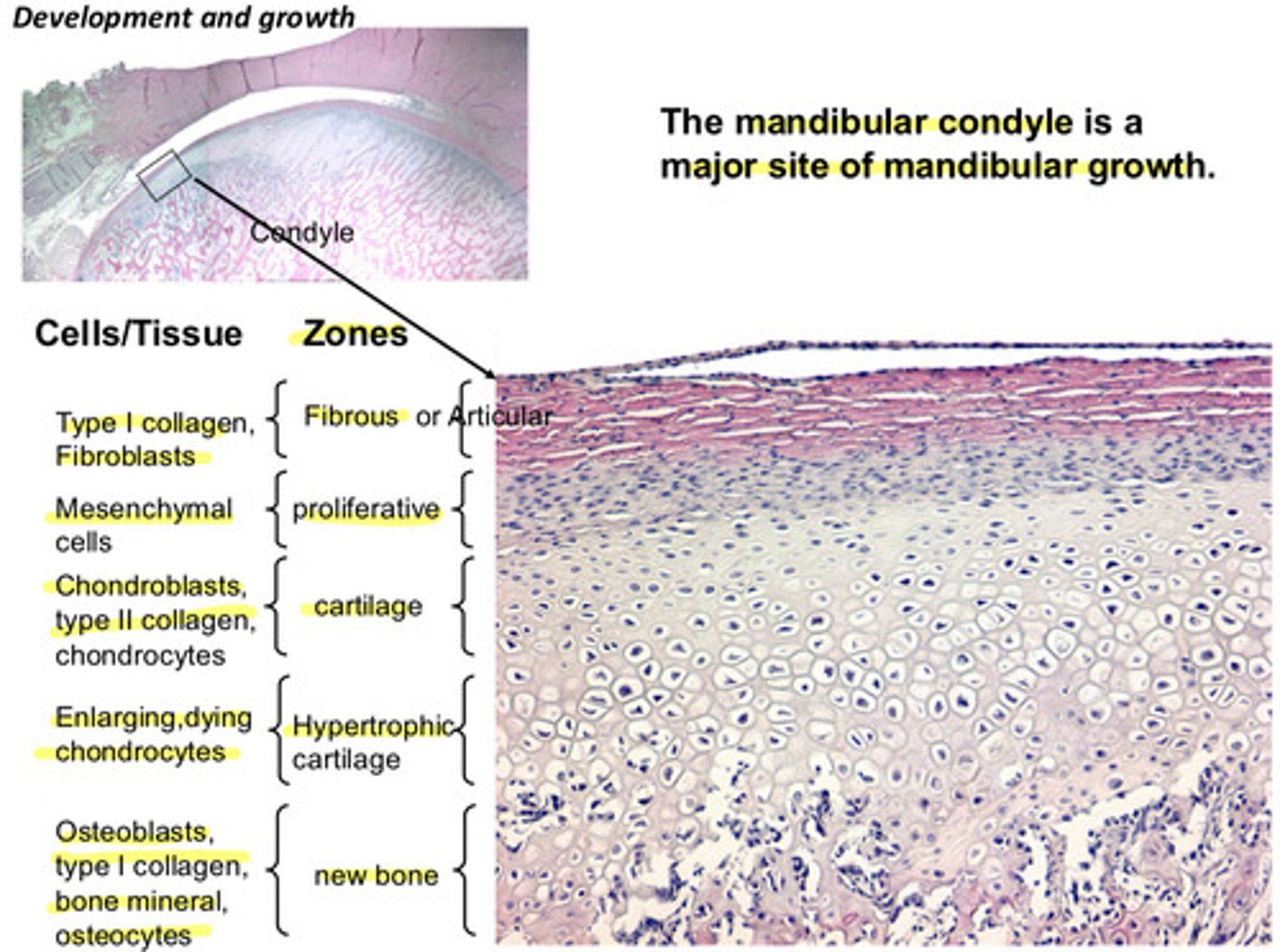
which part of the mandible is the major site of mandibular growth?
the mandibular condyle
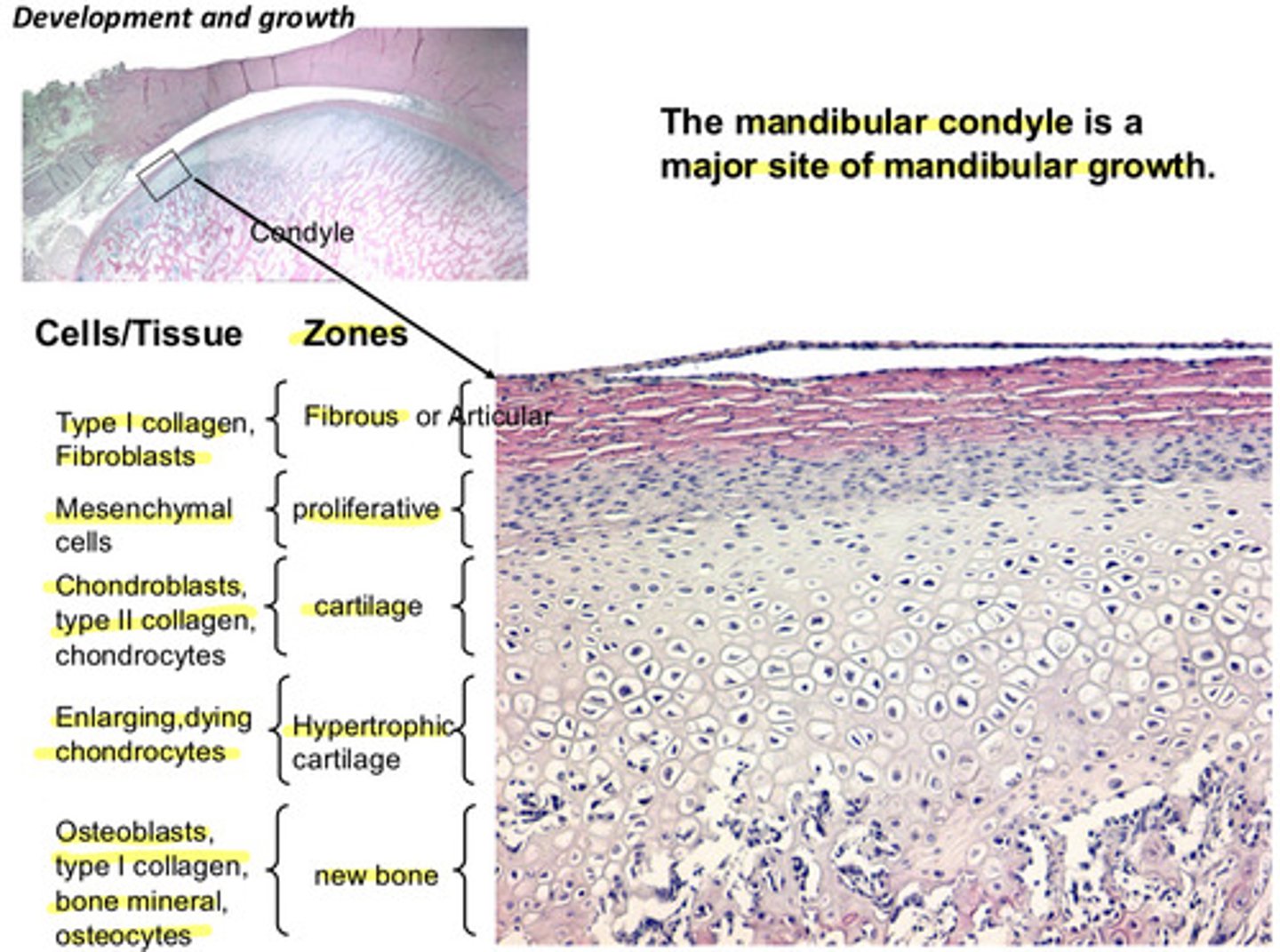
recall the zones of the mandibular condyle and what kinds of cells are present in them? remember that this is still during development, so the cartilage zones are not yet fibrocartilage and there is presence of hypertrophic cartilage which contributes later to bone (becomes calcified)
1) articular or fibrous: type I collagen, fibroblasts
2) proliferative: mesenchymal cells
3) cartilage: chondroblasts, type II collagen, chondrocytes
4) hypertrophic cartilage: enlarging, dying chondrocytes
5) new bone: osteoblasts, type I collagen, bone mineral, osteocytes
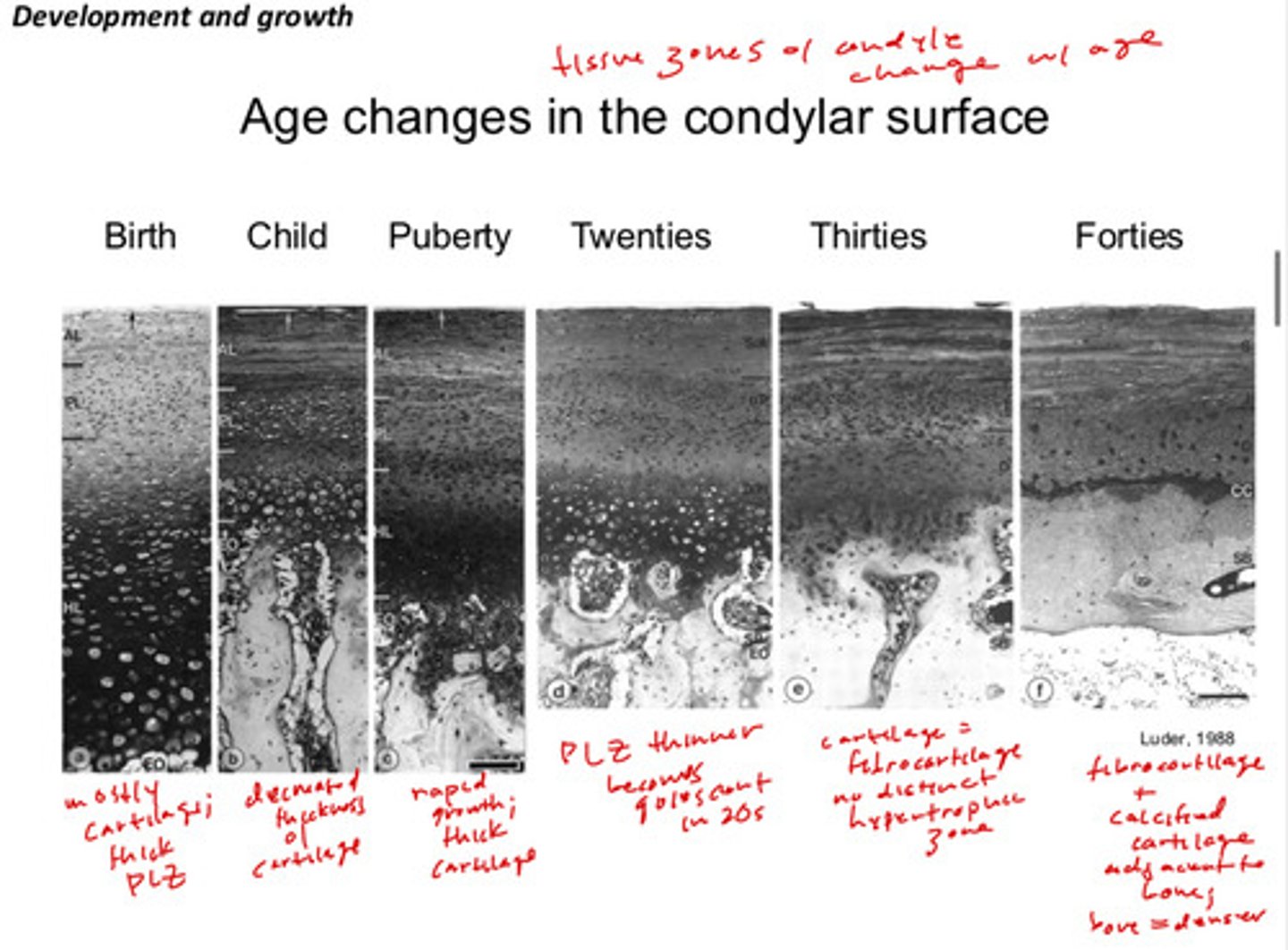
generally, how does age change/affect the condylar surface?
at birth: mostly cartilage, thick proliferative zones
child: decrease of thickness of cartilage
puberty: rapid growth; thick cartilage again
twenties: proliferative zones becomes thinner and quiescent
thirties: cartilage transitions to more fibrocartilage; there is no distinct hypertrophic zone at this point
forties: distinct fibrocartilage + calcified cartilage adjacent to the bones; bone is also denser
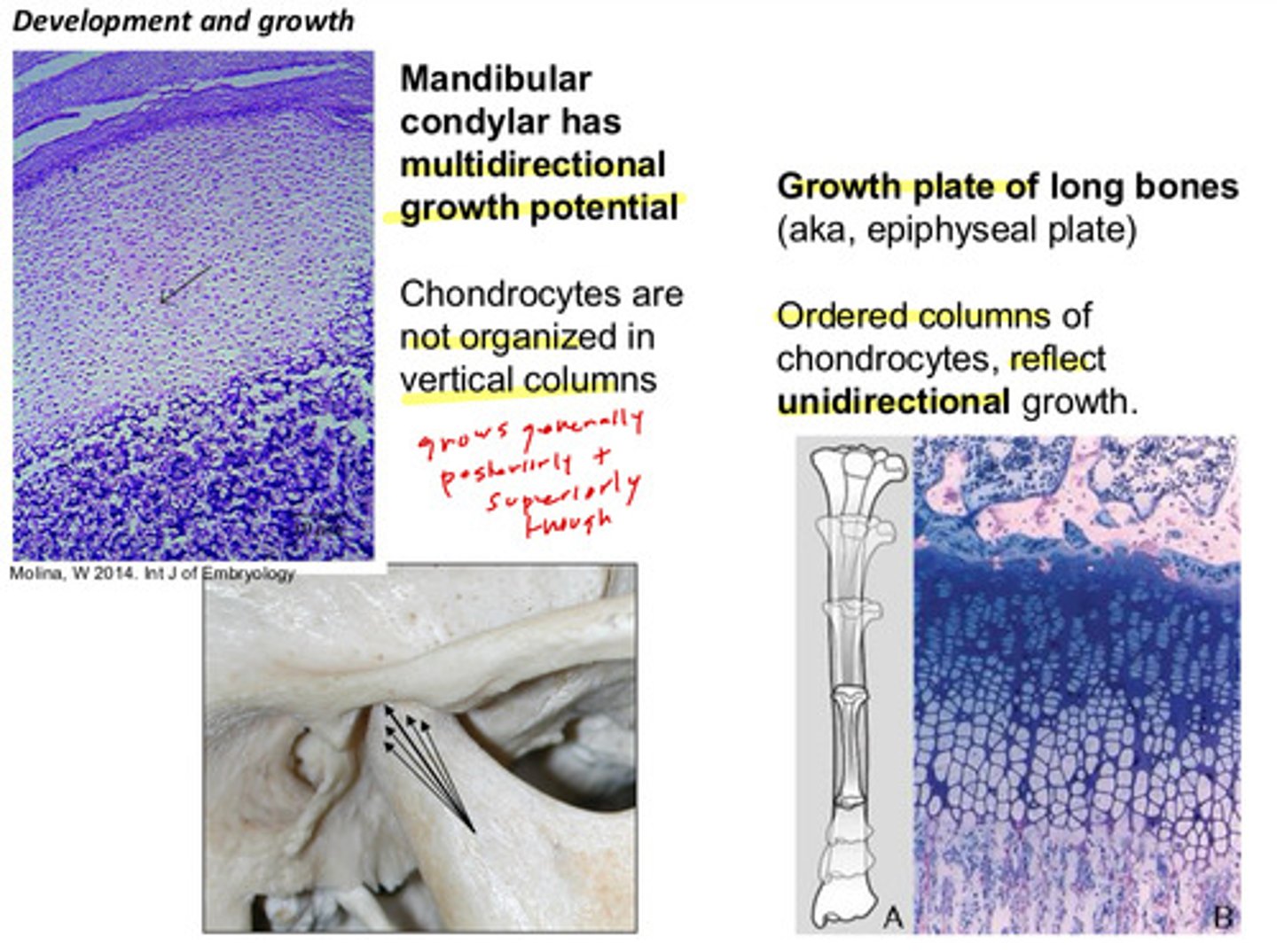
the mandibular condyle has ______________ growth potential; how are the chondrocytes organized?
multidirectional growth potential; chondrocytes are not organized in vertical columns (grows generally posteriorly and superiorly though)
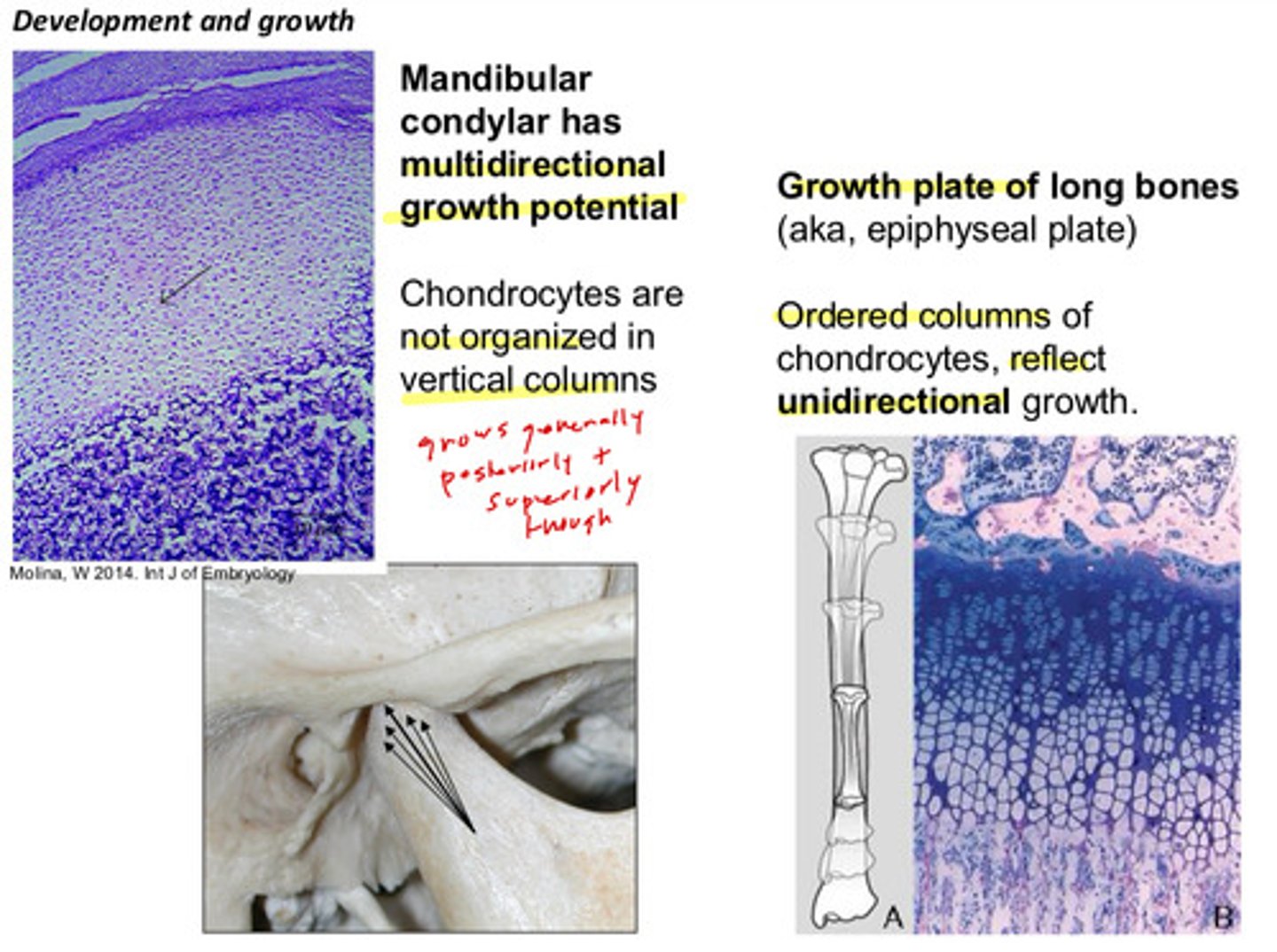
in comparison to the mandibular condyle, the growth plate (epiphyseal plate) of long bones reflect __________ growth and the chondrocytes are in ____________ _________
unidirectional; ordered columns
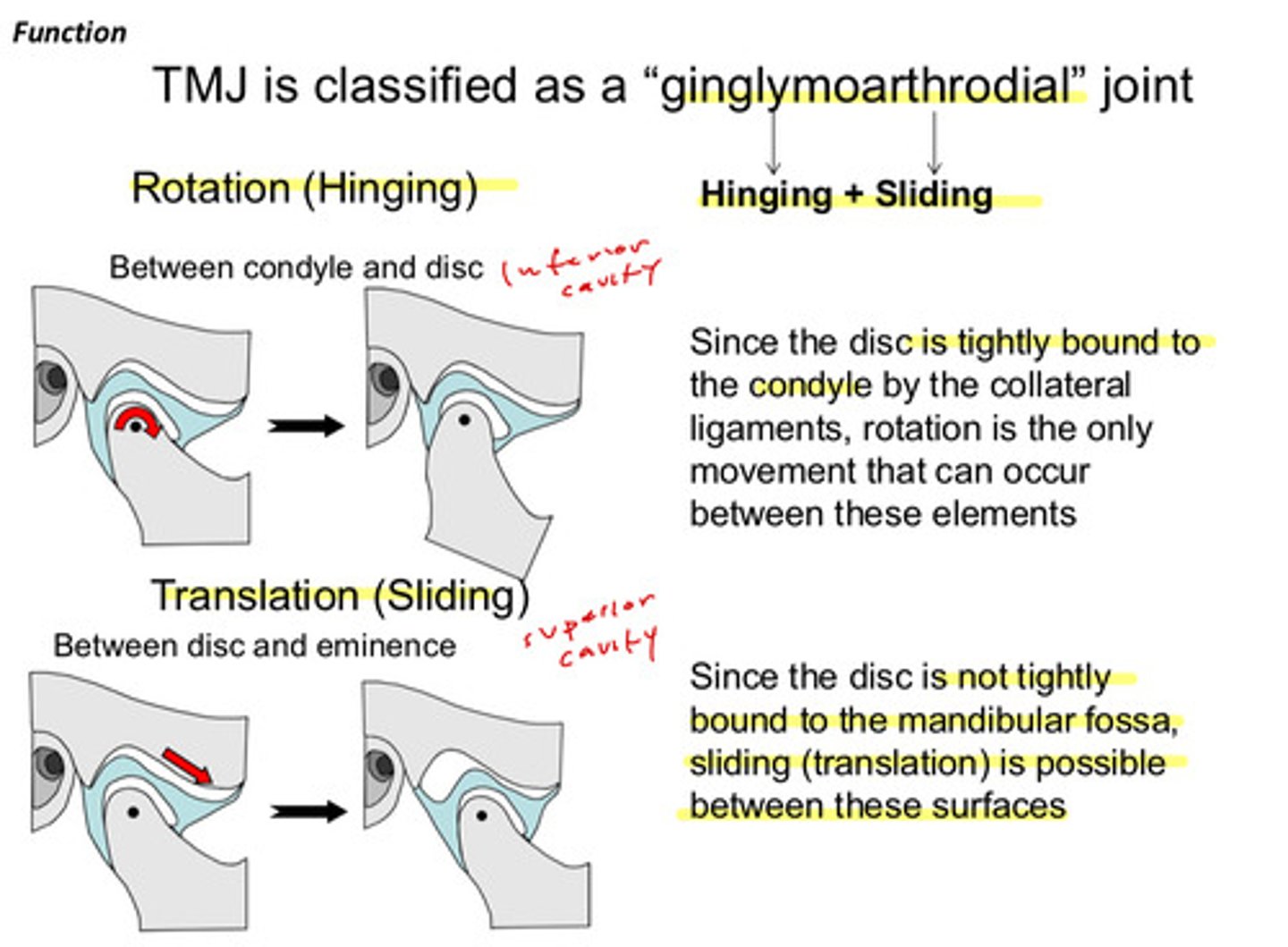
TMJ is classified as a "ginglymoarthrodial" joint, what does this mean?
the TMJ has a rotation (hinging) and a translation (sliding) action!
rotating in inferior cavity and translating is superior cavity
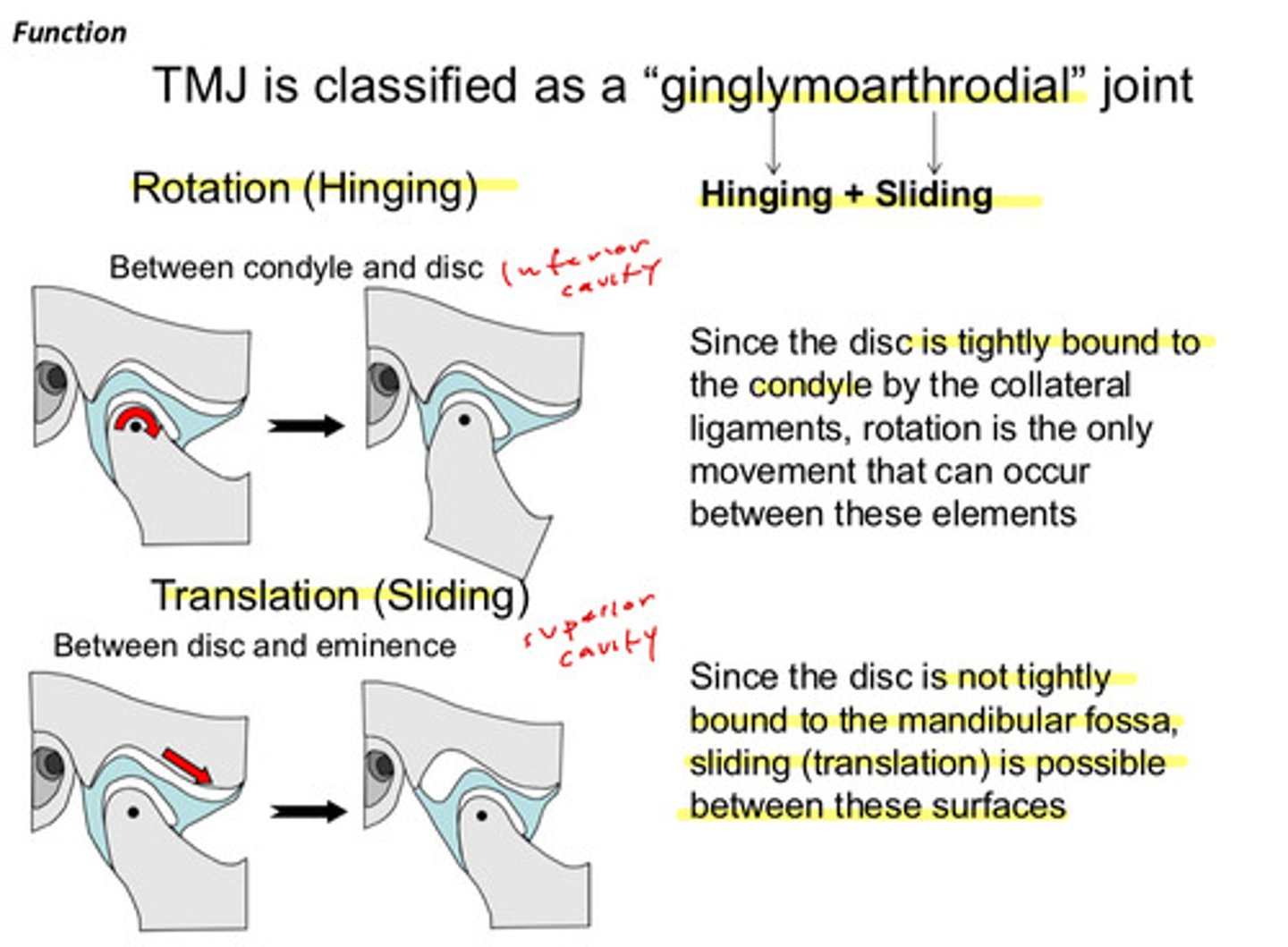
why can rotation only occur in the inferior cavity?
since the disc is tightly bound to the condyle by the collateral ligaments, rotation is the only movement that can occur between these elements
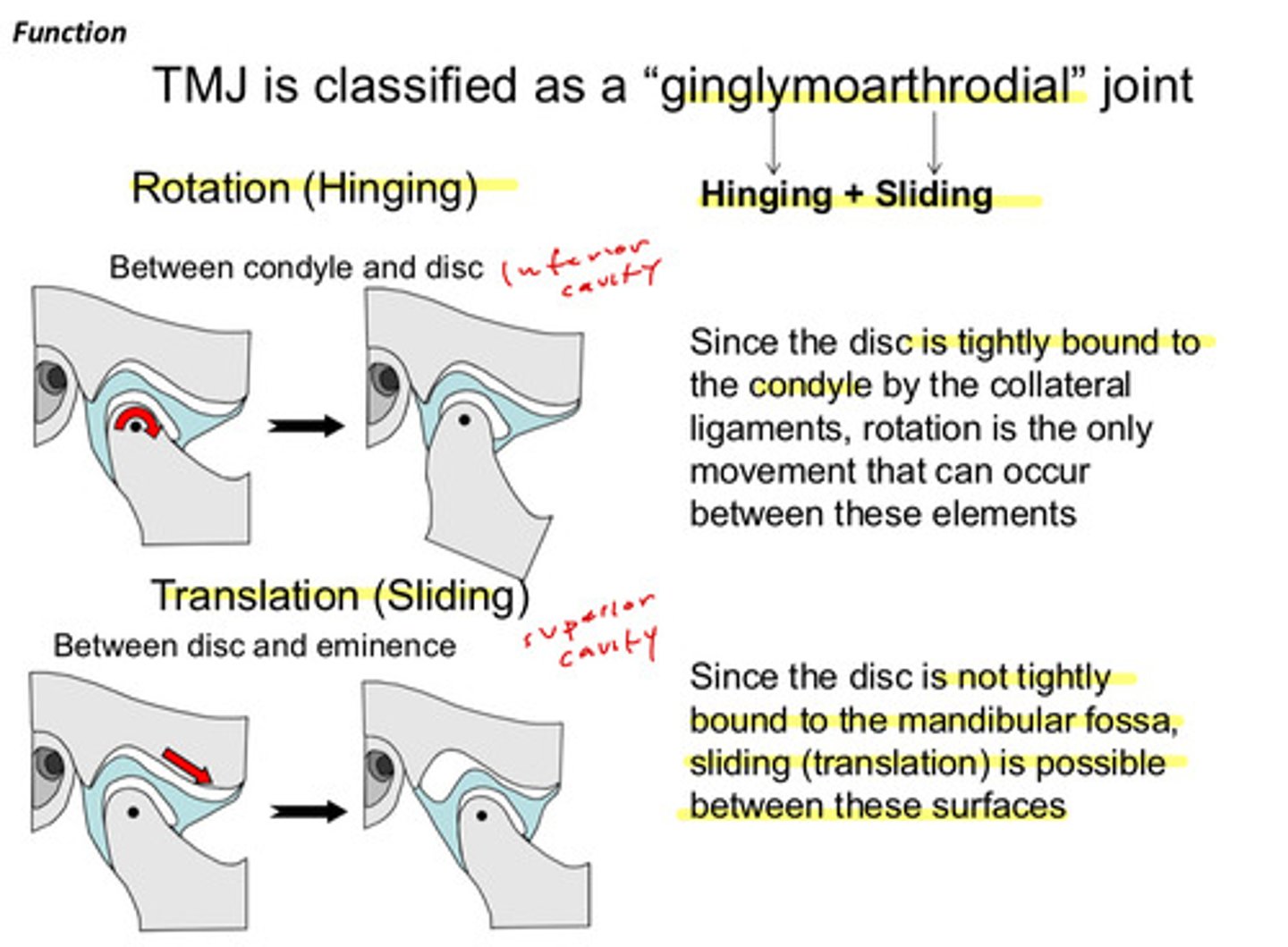
why can translation only occur in the superior cavity?
since the disc is not tightly bound to the mandibular fossa, sliding (translation) is possible between these surfaces
describe the movement of the condyle and disc during mouth opening (3)
1) closed rest position: condyle is seated in fossa
2) disc rotates posteriorly on condyle as condyle moves out of fossa
3) full opening: condyle and disc have translated forward and down eminence
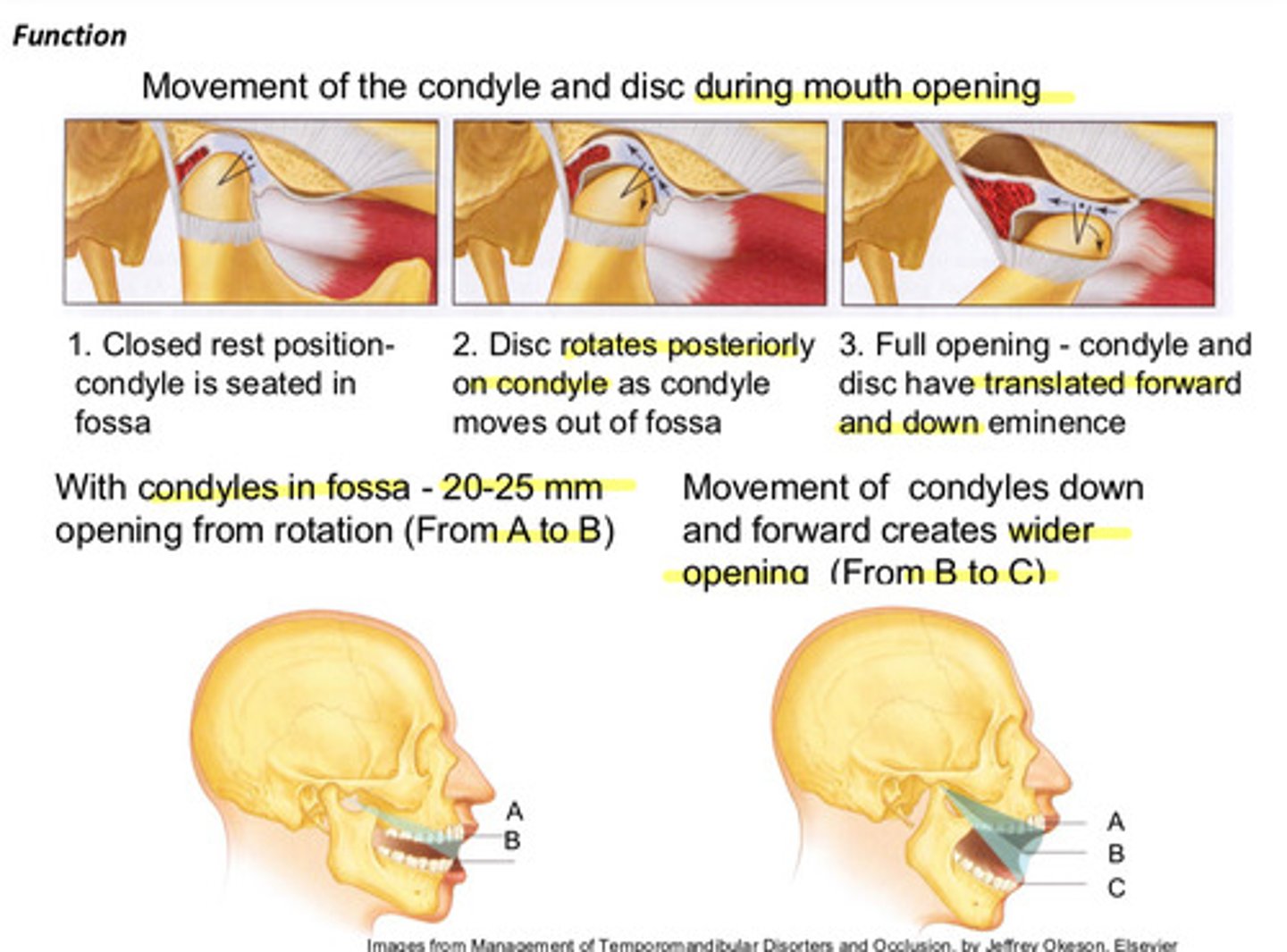
with the condyles in the fossa, what is the amount you can open while still only in rotation
20-25 mm
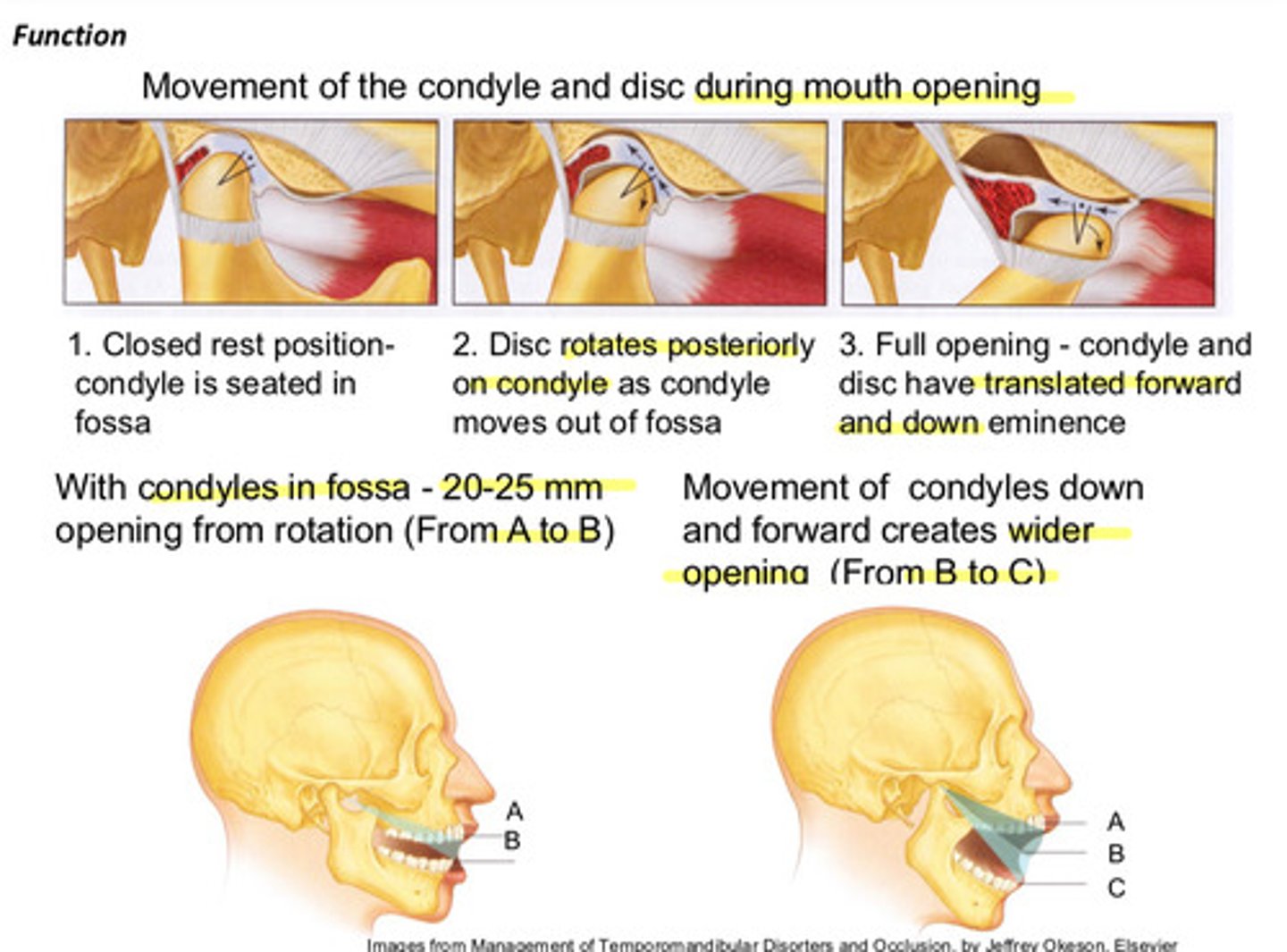
movement of condyles down and forward creates a _______ opening
wider
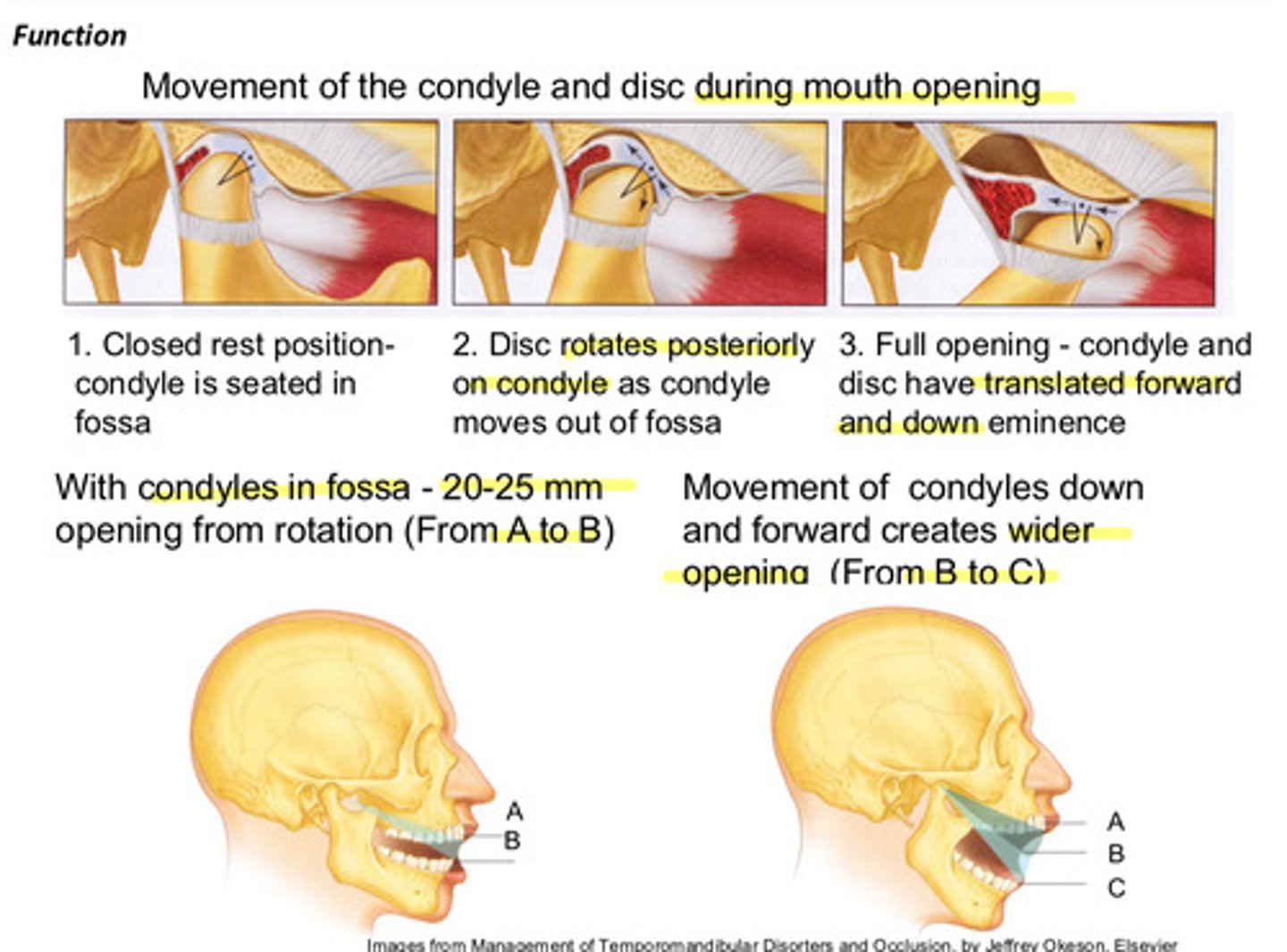
image of opening and closing function
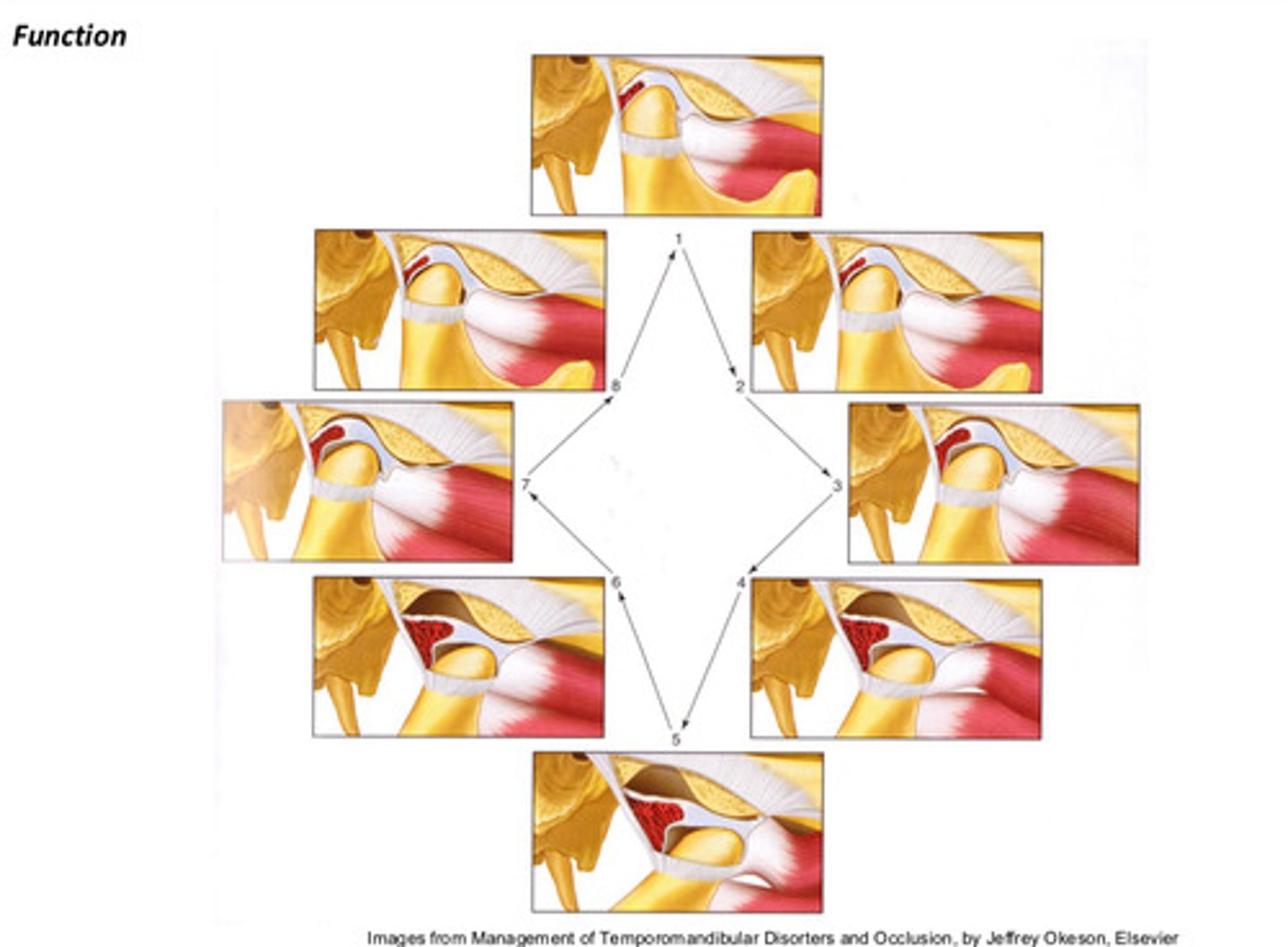
image of TMJ in "normal" position and image of TMJ in a passive opening position (wrenched all the way open)
during TMJ movement, the disc moves WITH the condyle
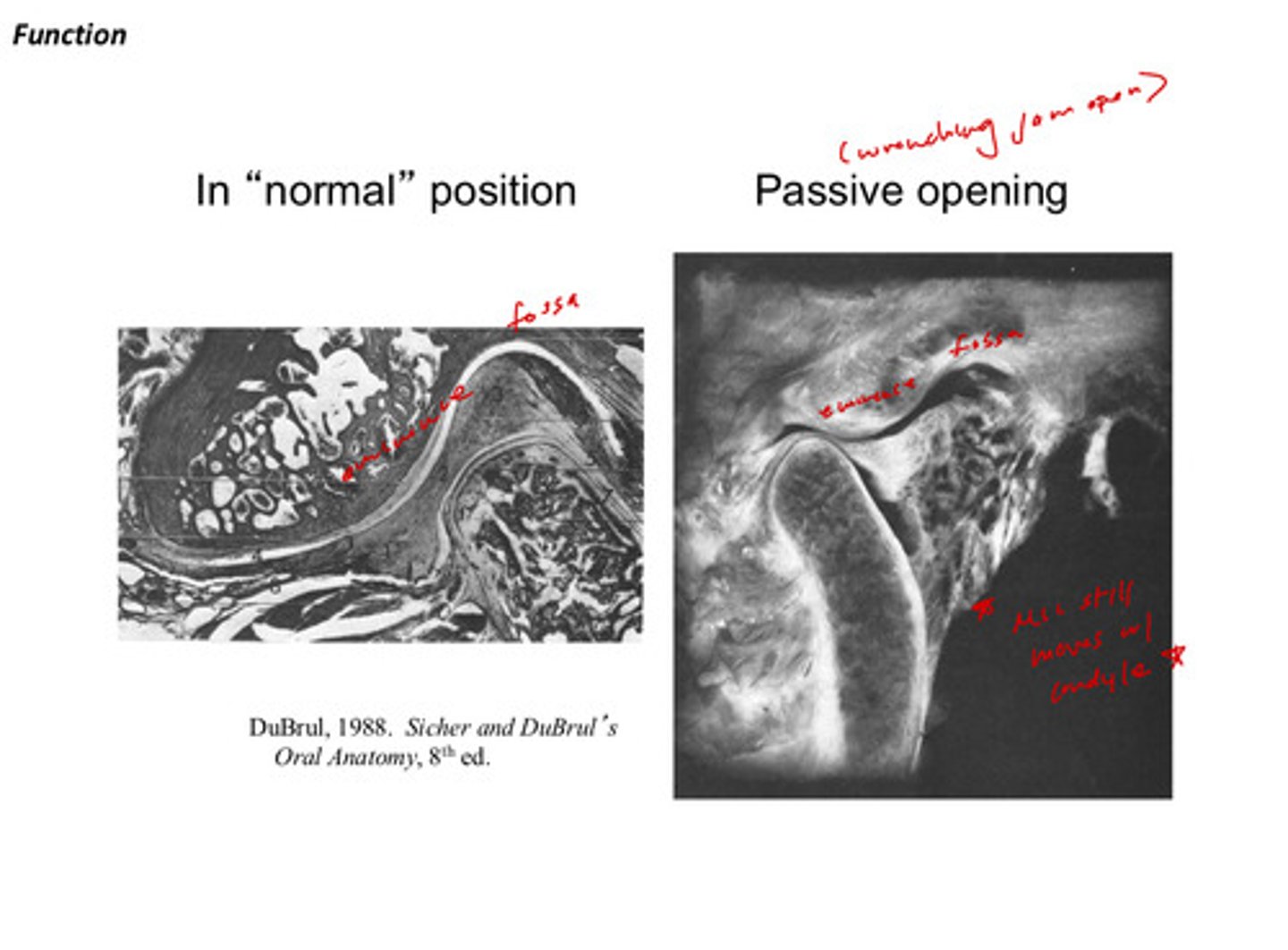
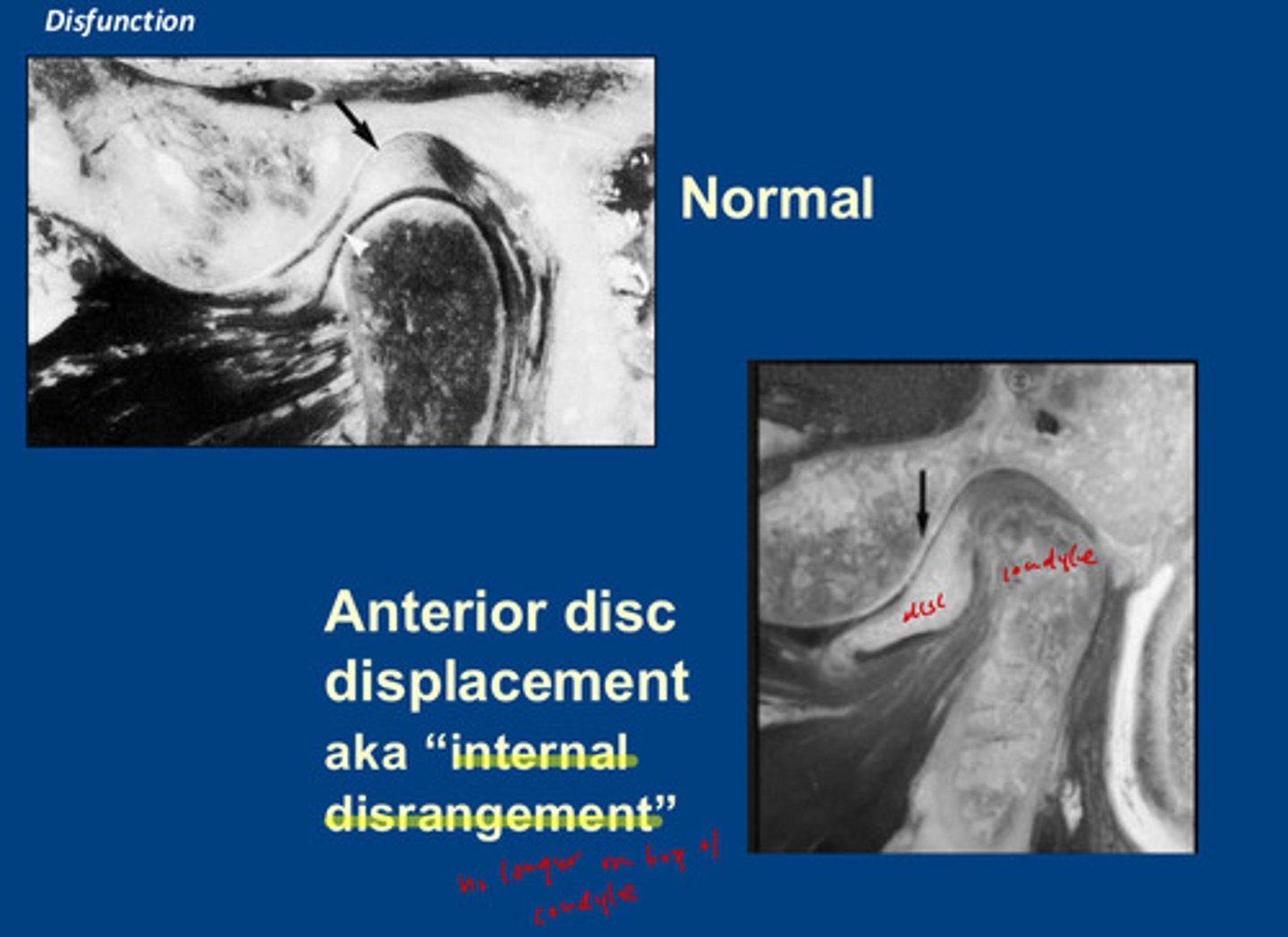
image of anterior disc displacement aka "internal disrangement"; what does this mean?
the disc is no longer on top of the condyle! it is displaced anteriorly in relation to the condyle
describe the difference between anteriorly displaced disc w reduction and anteriorly displaced disc without reduction
with reduction: the disc is displaced anteriorly but the condyle will slide under it during opening and pop under the disc
without reduction: the disc is displaced anteriorly but the disc stays bunched up even when the condyle moves anteriorly
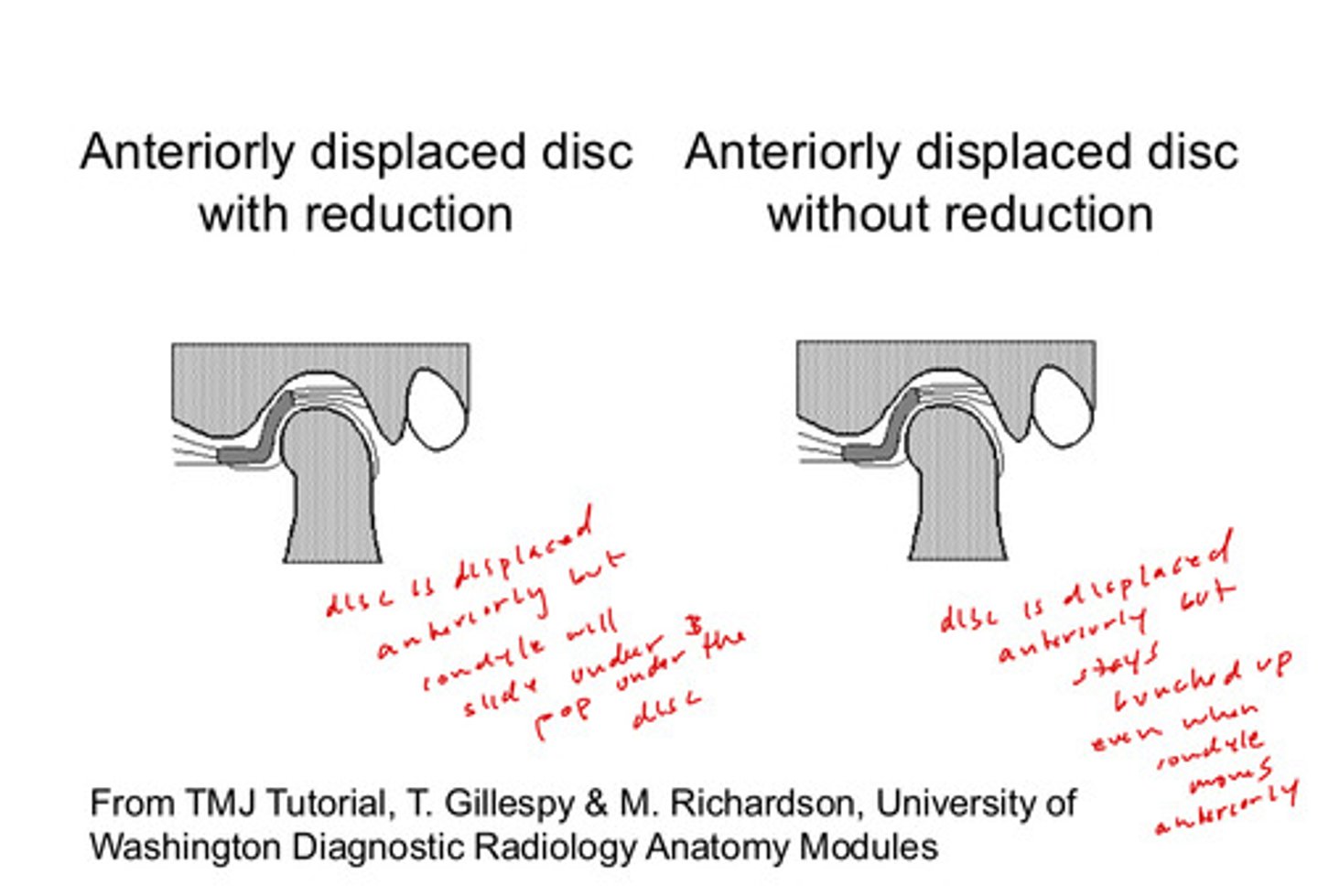
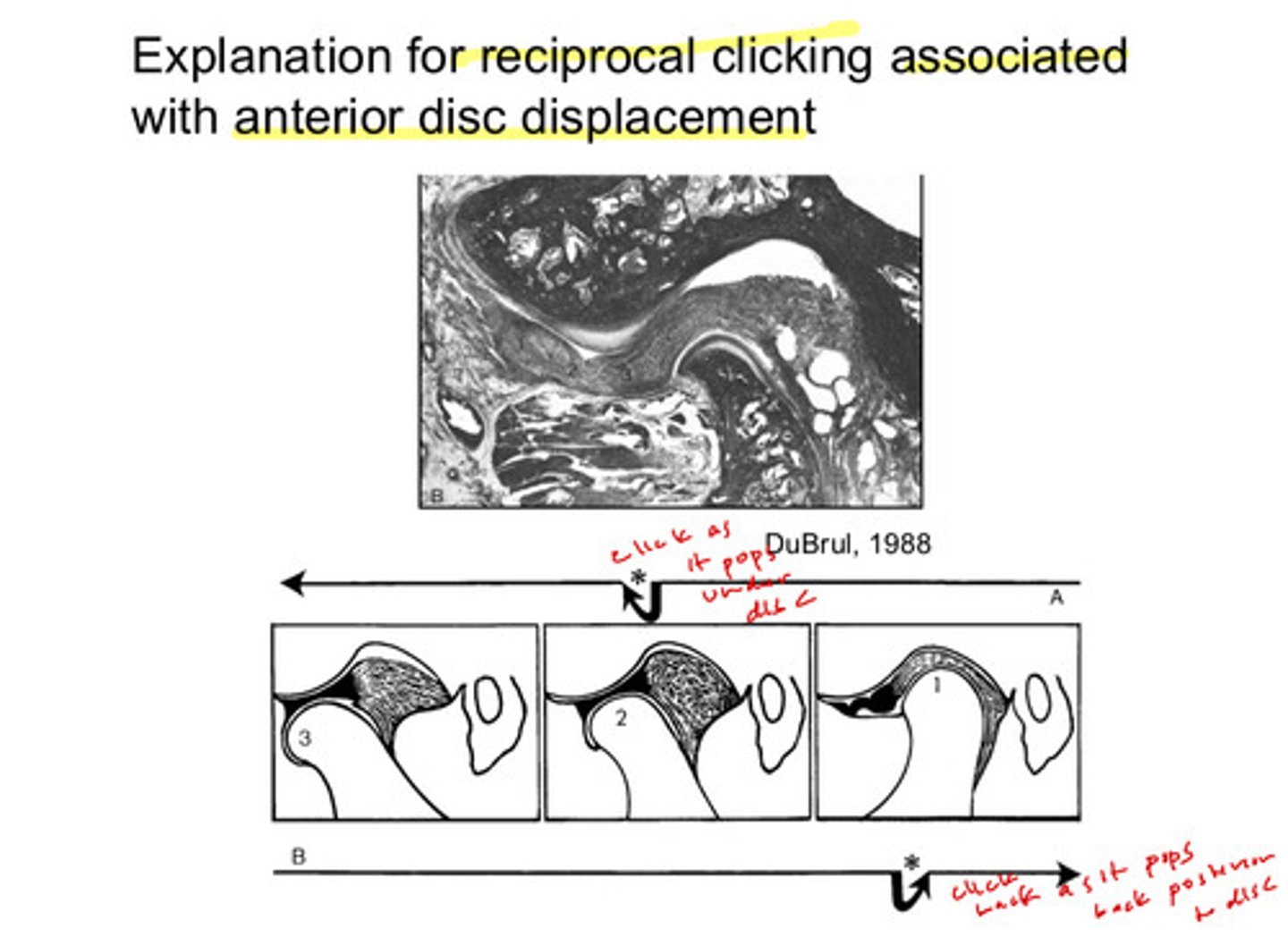
the explanation for reciprocal clicking is associated with ?
the anterior disc displacement: the condyle clicks as it pops under the disc and clicks back as it pops back posterior too the disc
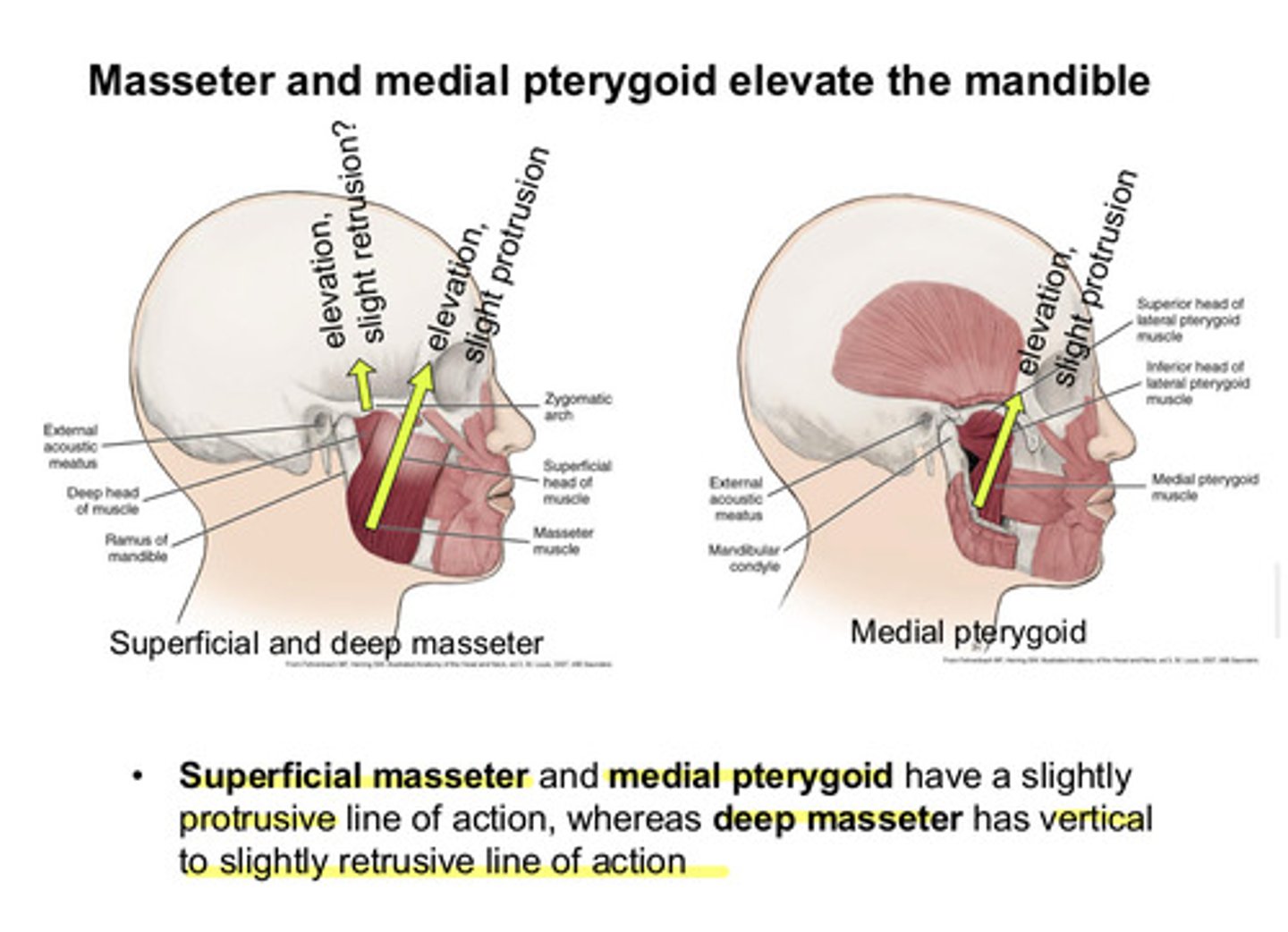
what are the 2 parts of the masseter and what actions does each part have
superficial and deep masseter; superficial has elevation and slight protrusion action, deep has elevation and slight retrusion
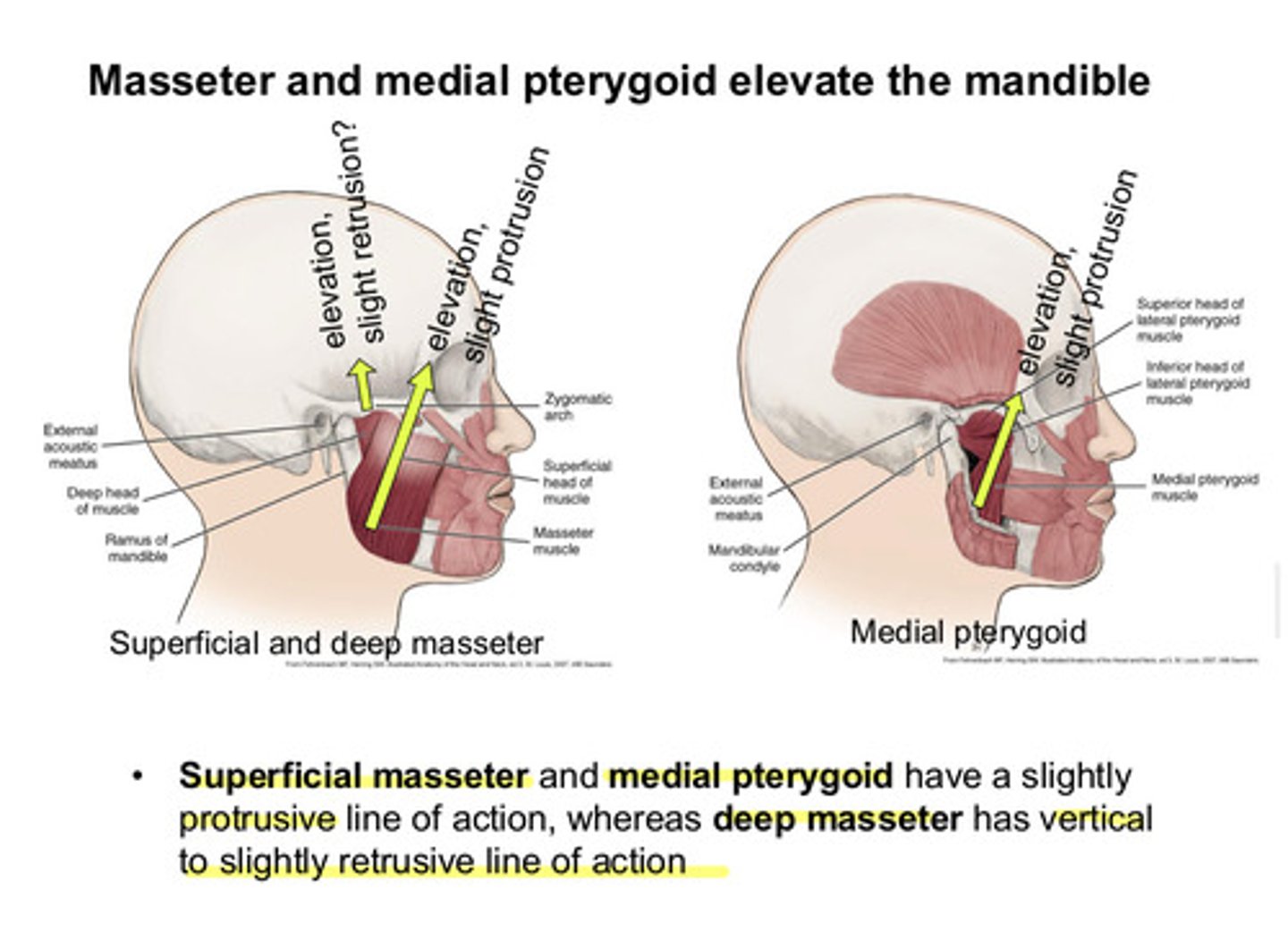
what is the action of the medial pterygoid
elevation and slight protrusion
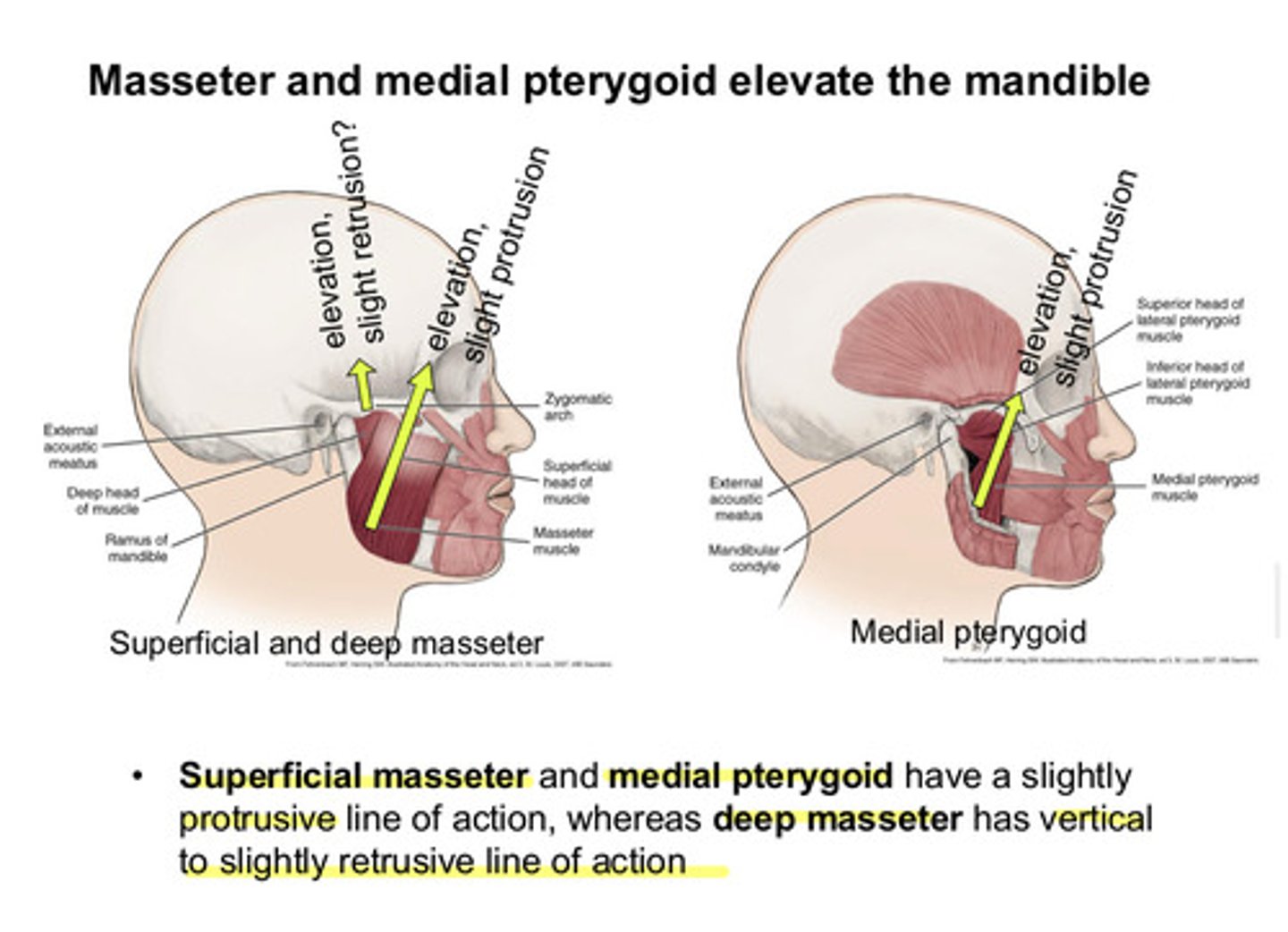
so which 2 muscles that act on the TMJ elevate the mandible
masseter and medial pterygoid both have a slightly protrusive line of action, whereas deep masseter has vertical to slightly retrusive line of action
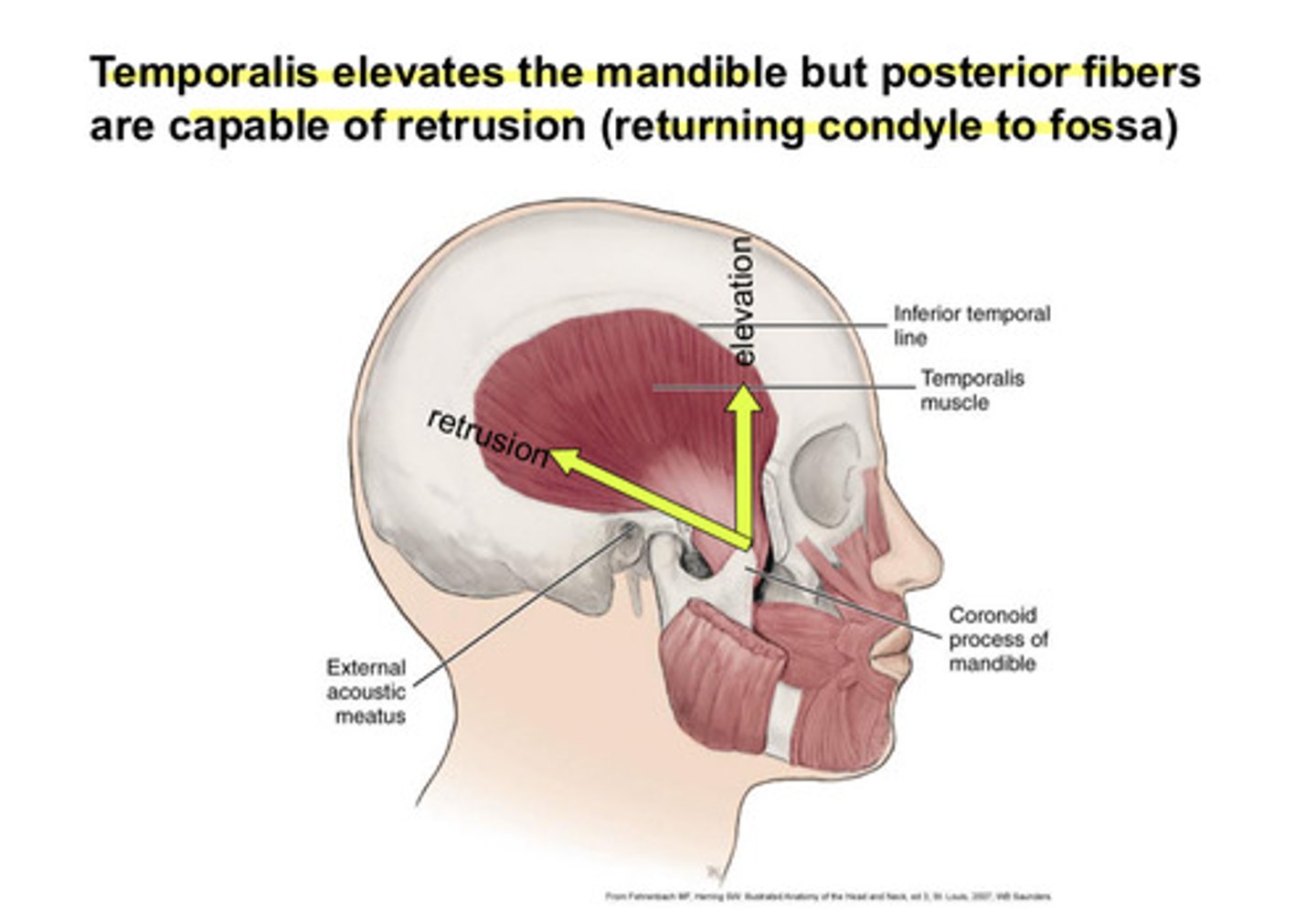
the temporalis muscle does what to the mandible (and what about its posterior fibers)
temporalis (anterior vertical fibers) elevates the mandible, but posterior horiztonal fibers are capable of retrusion (returning condyle to fossa)
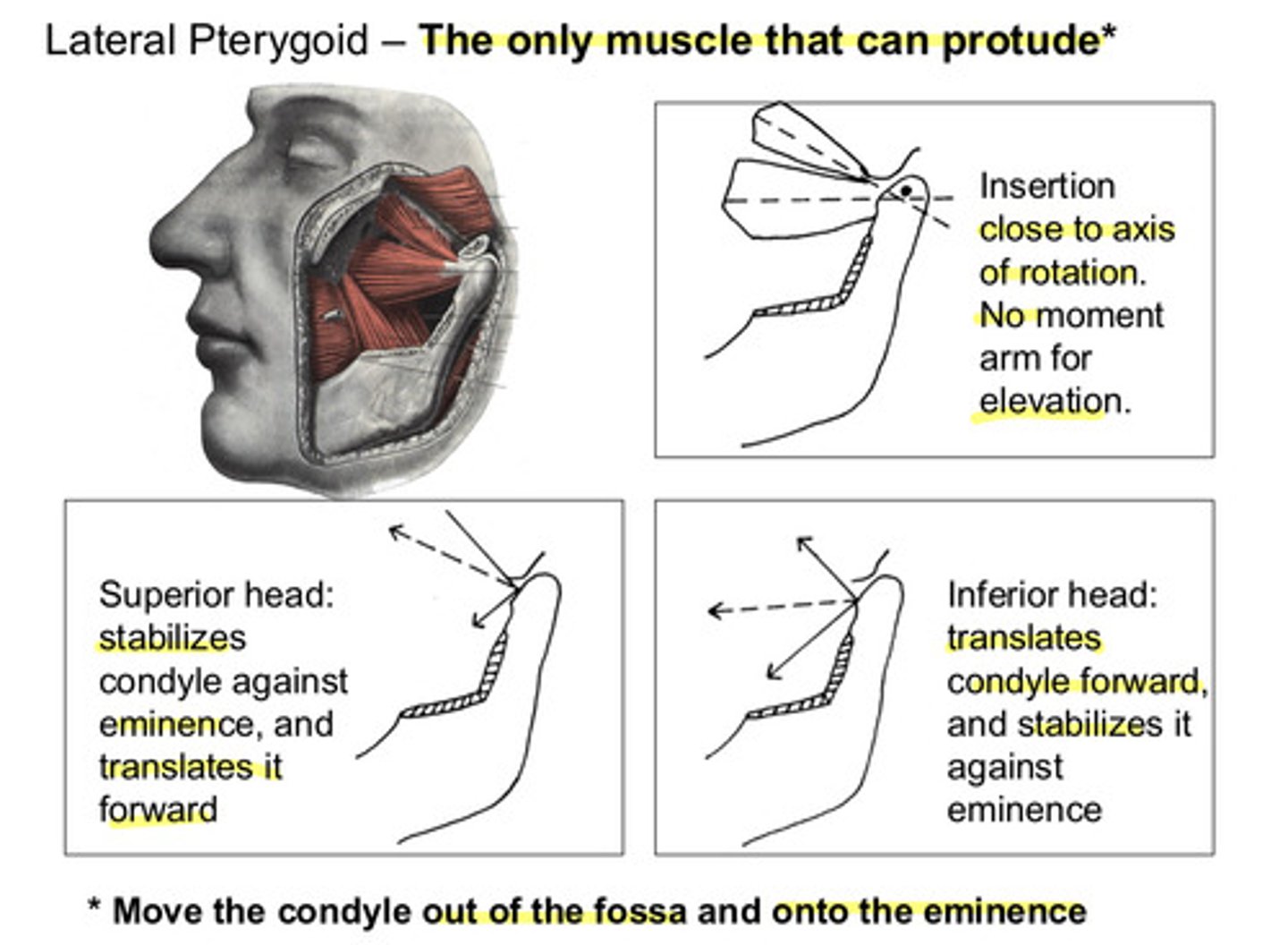
where does the lateral pterygoid muscle attach to on the TMJ
attaches to the pterygoid fovea & into disc/capsule
the lateral pterygoid is the only muscle that can ________?
protrude (move the condyle out of the fossa and onto the eminence)
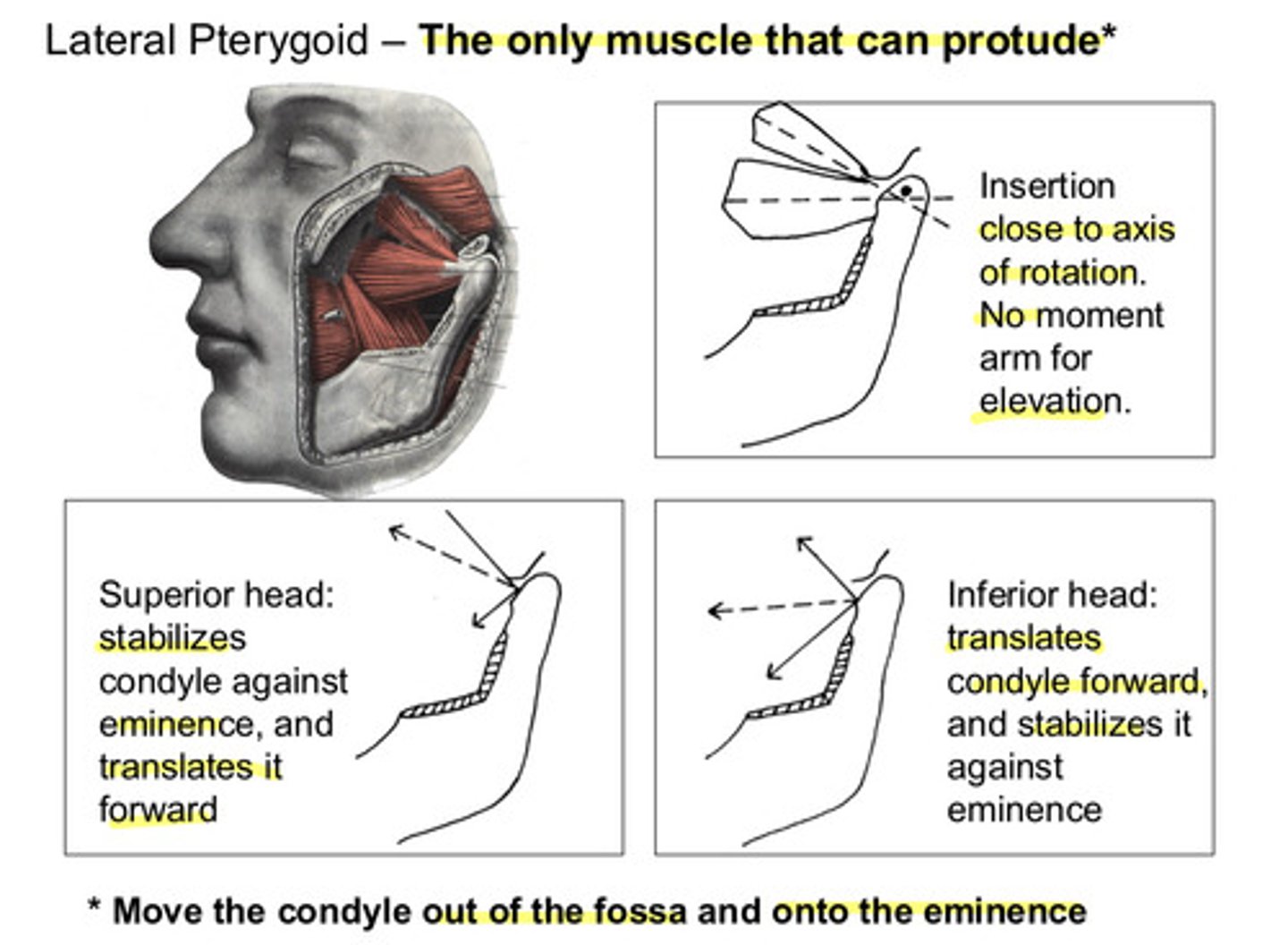
the lateral pterygoid inserts close to the axis of rotation, therefore there is not a moment arm for ?
for elevation
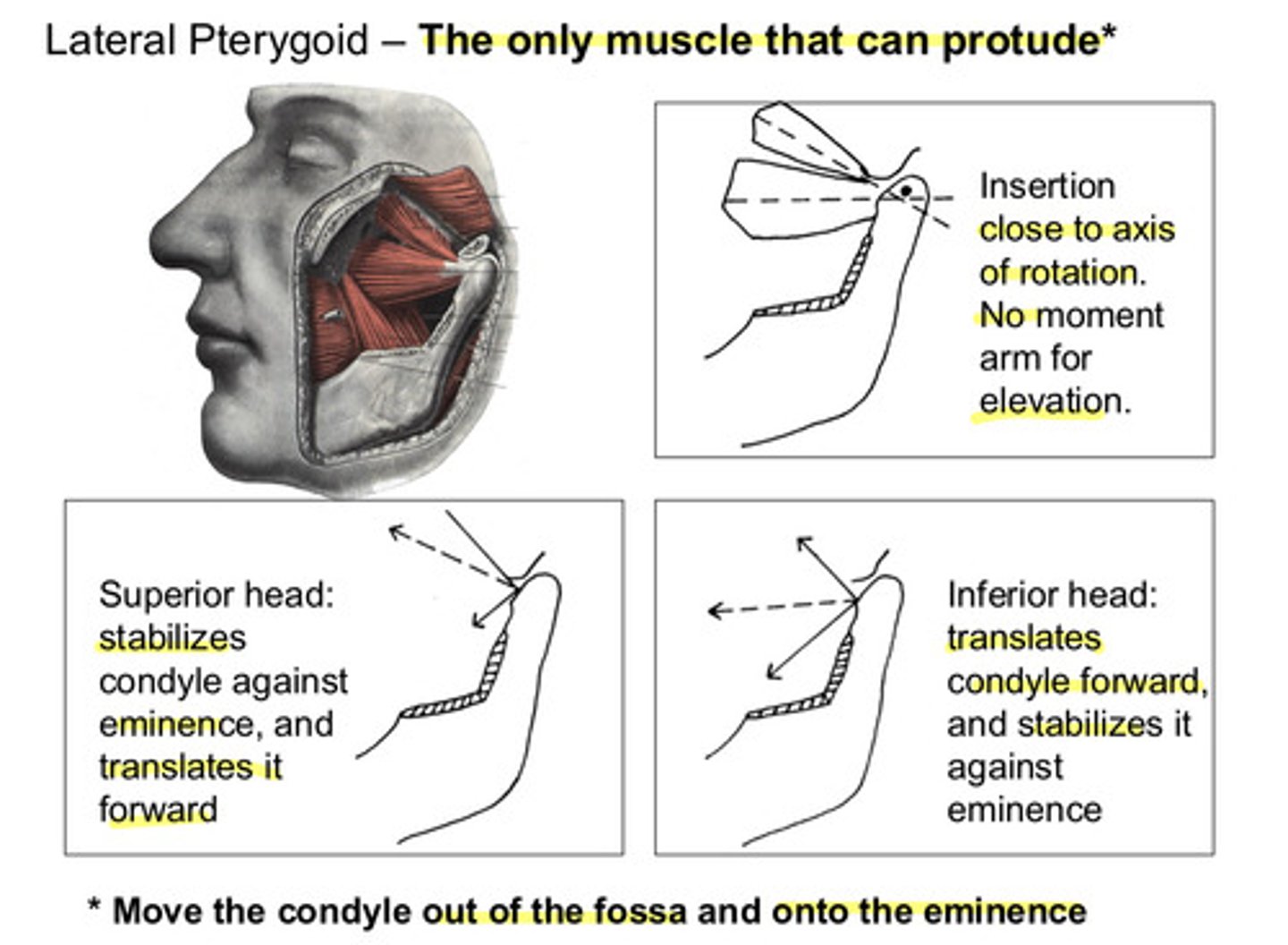
what does the superior head of the lateral pterygoid do?
stabilizes the condyle against the eminence, and translates it forward
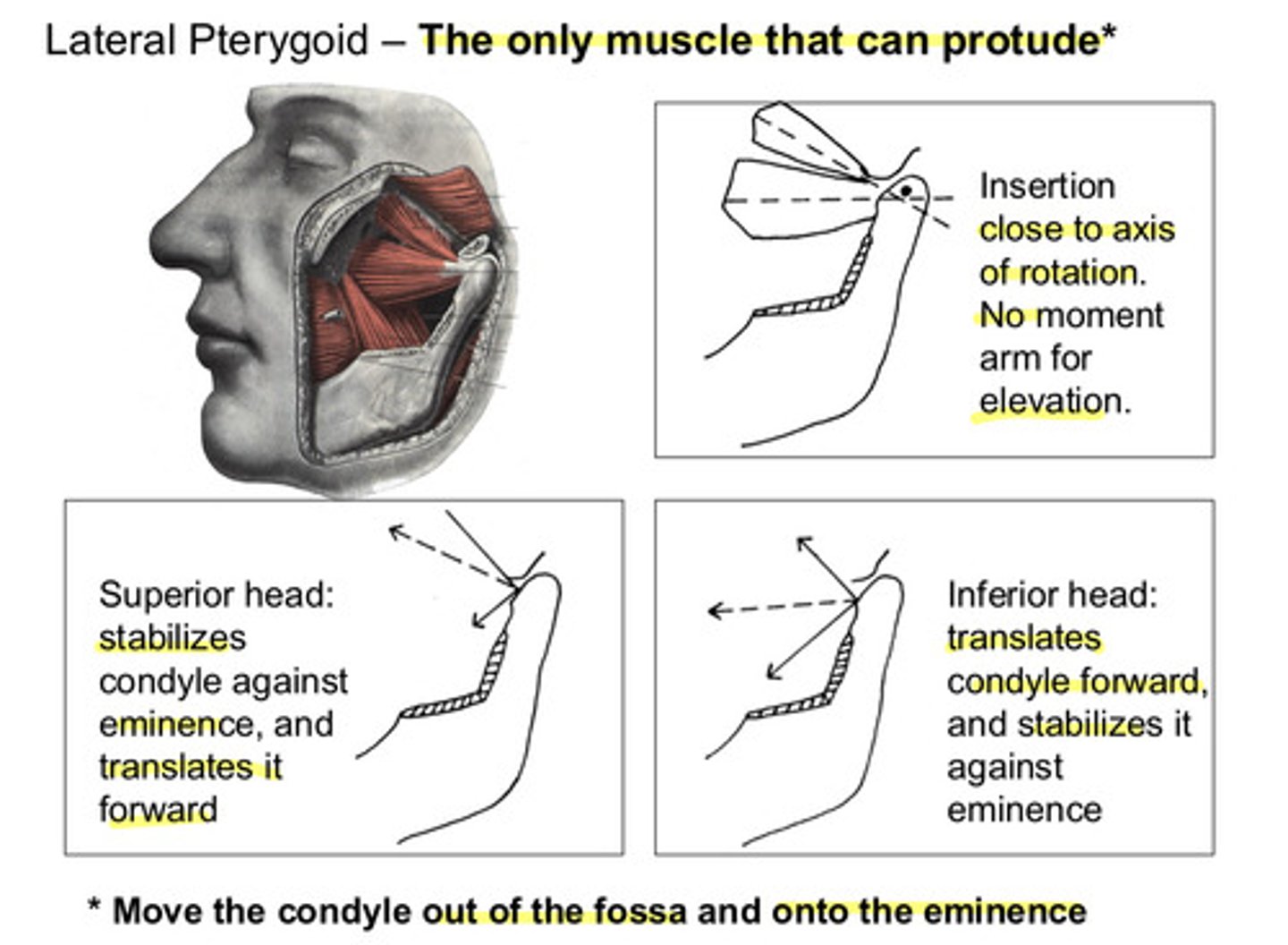
what does the inferior head of the lateral pterygoid do?
translates the condyle forward, and stabilizes it against eminence
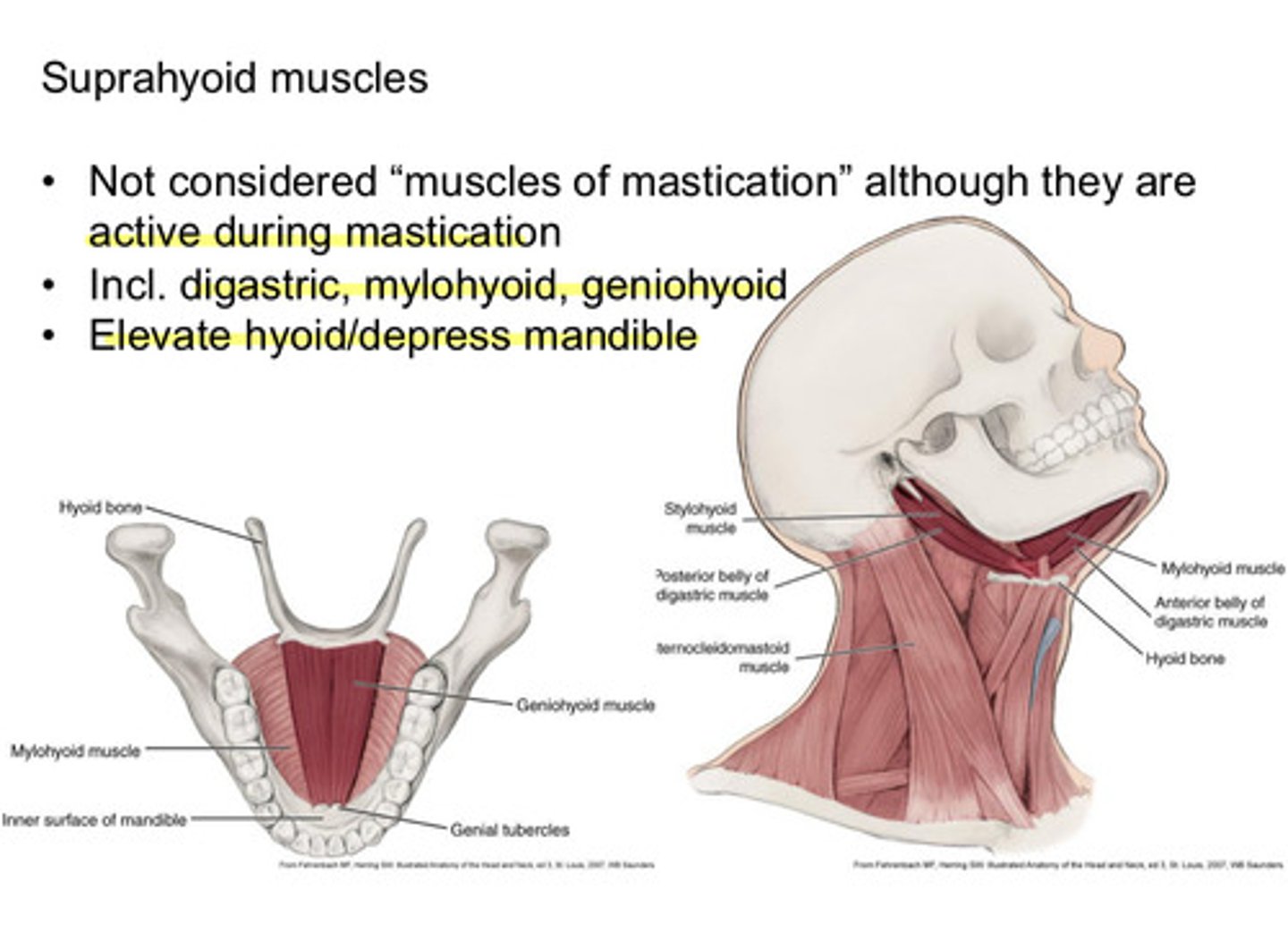
what do the suprahyoid muscles do and are they considered "muscles of mastication"
they are not considered "muscles of mastication" although they are active during mastication; they elevate the hyoid/depress the mandible
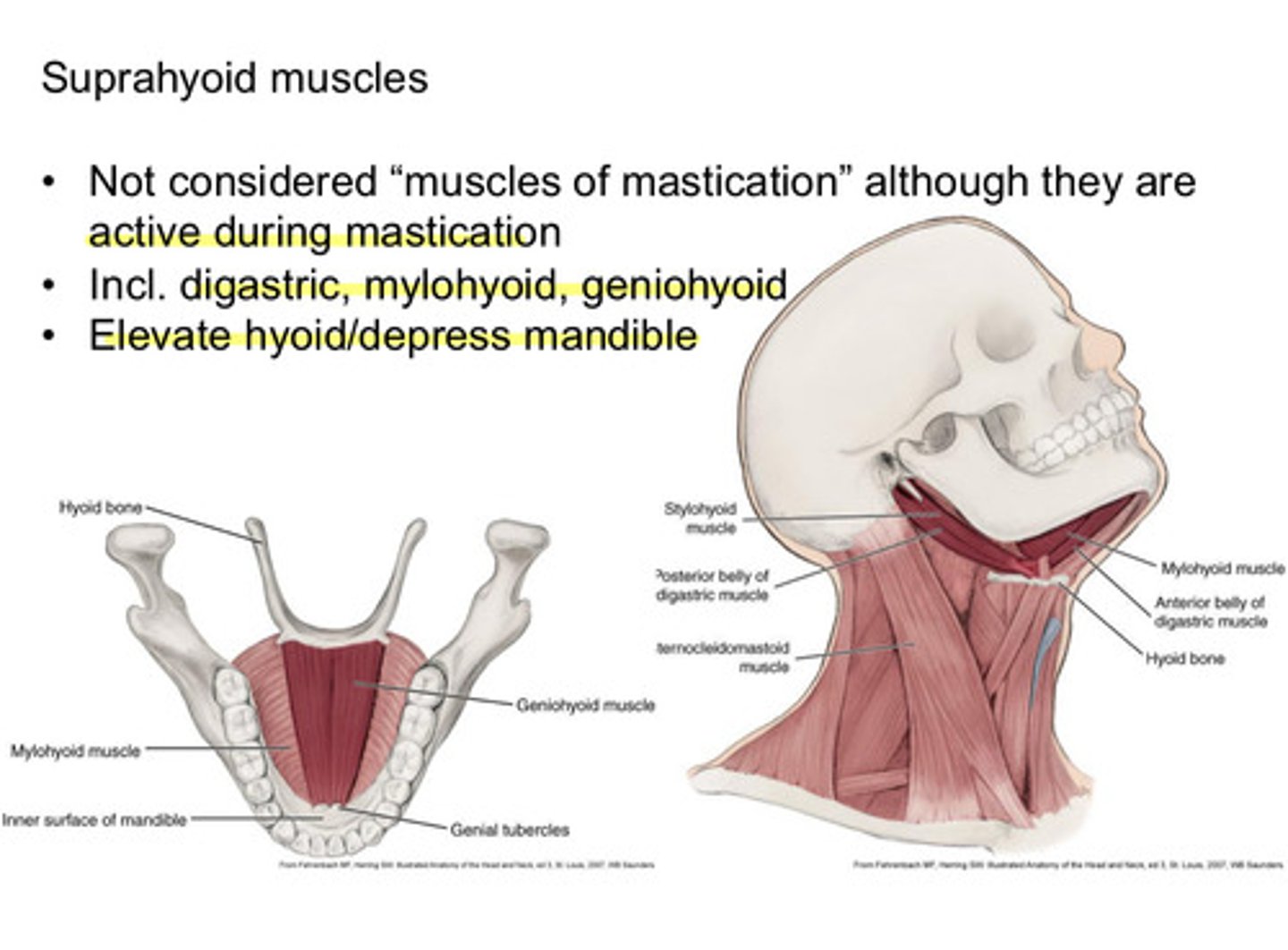
which muscles are included in the suprahyoid muscles
digastric, mylohyoid, and geniohyoid