8. peripheral arterial duplex imaging and pathology
1/125
Earn XP
Description and Tags
DMUT 4
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
126 Terms
what are the risk factors for peripheral arterial pathology/disease
smoking
diabetics >50 years
age >70 years
what are the peripheral arterial pathologies
occlusive disease, pseudoaneurysm, arteriovenous fistula (AVF), aneurysms, and atherosclerosis
occlusive disease can be found with either…
indirect testing or duplex ultrasound
indirect testing is a reliable indicator for the presence of occlusive disease but does not provide…
anatomic info
indirect testing includes…
systolic pressures, ankle/brachial index (ABI), plethysmography/photoplethysmography, exercise testing, and CW doppler analysis
why is duplex ultrasound good for investigating peripheral arterial disease
gives anatomic and physiologic info
grayscale, colour, spectral, power doppler with waveform analysis
what position should LE duplex assessment be done in for patient
supine, with leg slightly bent and externally rotated (like DVT)
what transducer is used in arterial duplex imaging
7-10 MHz linear array transducer
what techniques are used in LE duplex exams
often only one window, increase room temperature (prevent vasoconstriction), and have a doppler angle of 60 (for reproducibility, and optimize images
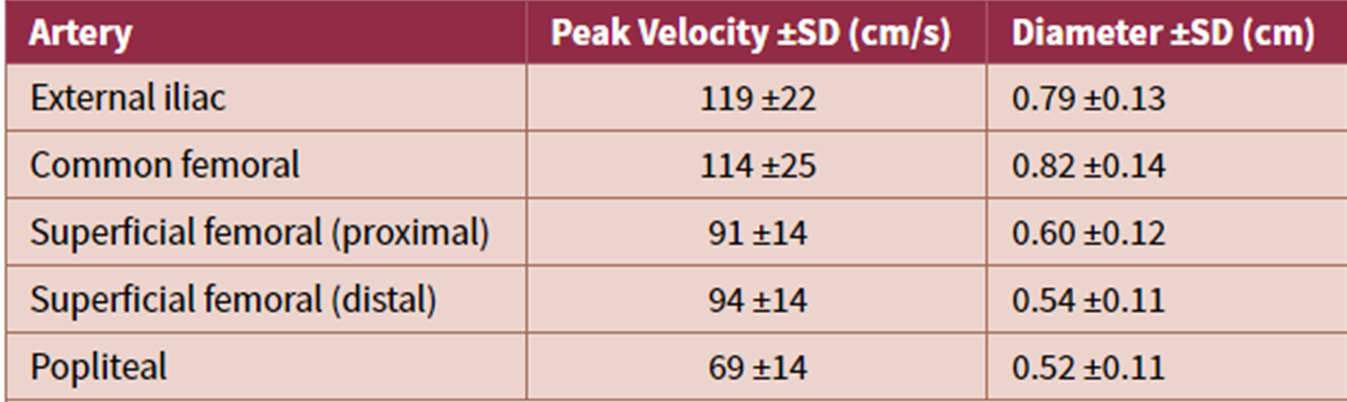
normal flow velocities table *DNTM
normal arterial flow patterns
triphasic with flow reversal in early diastole
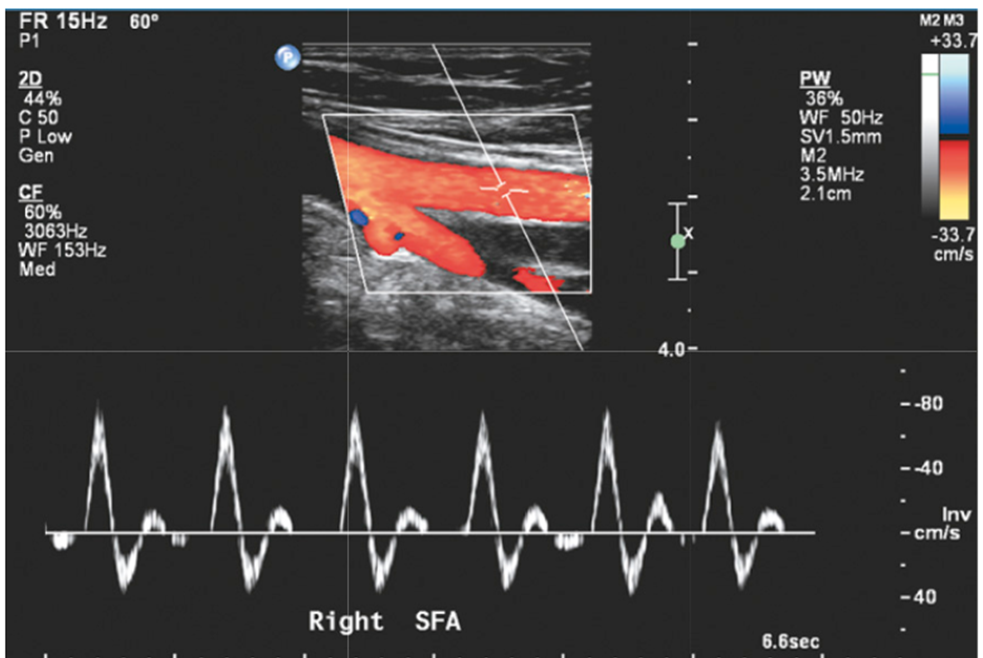
normal arterial flow waveform of SFA
when does loss of flow reversal occur in arterial waveforms
when peripheral resistance decreases, such as in exercise, reactive hyperemia, and limb warming
in laminar flow patterns where is the fastest velocities
centre of the vessel
symptoms of occlusive disease
intermittent claudication
thickened toenails/loss of toe hair
skin changes (discoloured and scaly)
forefoot pain (even at rest) and ulceration
what skin changes can occur in occlusive disease
elevation pallor (pale/white)
dependent rubor (red with foot hanging)
blueness of toes (aneurysmal emboli)
what is an indicator of severe disease and symptom of occlusive disease
forefoot pain (even at rest) and ulceration
claudication
leg discomfort/pain that worsens with activity and improves at rest
affects calf, thigh, and/or buttock
the site of claudication symptoms gives general idea to the
site of disease
in a duplex assessment, the findings of stenosis or occlusion in carotid vessels can be seen such as…
visualization of plaque/narrowing
colour flow disturbance,
waveform changes (proximal, at stenosis, and distal stenosis & velocity changes)
normal flow pattern characteristics
triphasic waveform with no spectral broadening
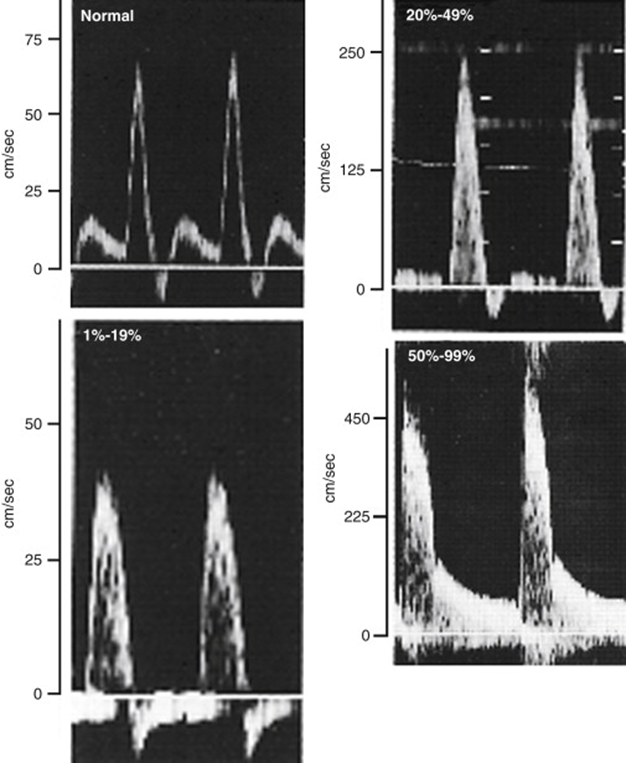
1-49% diameter reduction flow pattern characteristics
triphasic (reversed flow may be diminished)
minimal-moderate spectral broadening
peak systolic velocities increased <100% relative to adjacent prox segment
proximal and distal waveforms remain normal
50%-99% diameter reduction waveform characteristics
monophasic waveform with LOSS of reversed flow, forward flow throughout cardiac cycle
extensive spectral broadening
peak systolic velocity increased >100% relative to adjacent proximal segment
distal waveform is monophasic with reduced systolic velocity & prolonged acceleration (tardus parvus waveform)
occlusion in vessel flow patterns
no flow detected within imaged arterial segment
preocclusive “thump” may be heard proximal to site of occlusion
distal (collateral) waveforms are monophasic with reduced systolic velocities
what is the most reliable indicator for the presence of a 50% or greater stenosis?
a 2:1 systolic velocity ratio with focal velocity acceleration and post stenotic turbulence
spectral broadening and increased focal velocities on varying stenotic waveforms compared to normal waveform
post stenotic segment US (tardus parvus)
A normal study rules out significant Aorto-iliac disease but not…
minor stenosis
what should be considered if the aorto-iliac segment needs to be scanned for occlusive disease?
thigh PVR waveform
Thigh pressure
CFA doppler waveform
femoral pulse
if there is an abnormal ABI without any detectable disease in the fem-pop or tibial arteries, or abnormal thigh PVRs or waveforms, then what should be scanned?
the aorto-iliac segment, though it is difficult to image these findings indicate need for scanning the A-I segment
what vessel waveform can appear normal distal to a mild iliac stenosis but does not rule out iliac disease?
the CFA waveform
SFA segment on colour
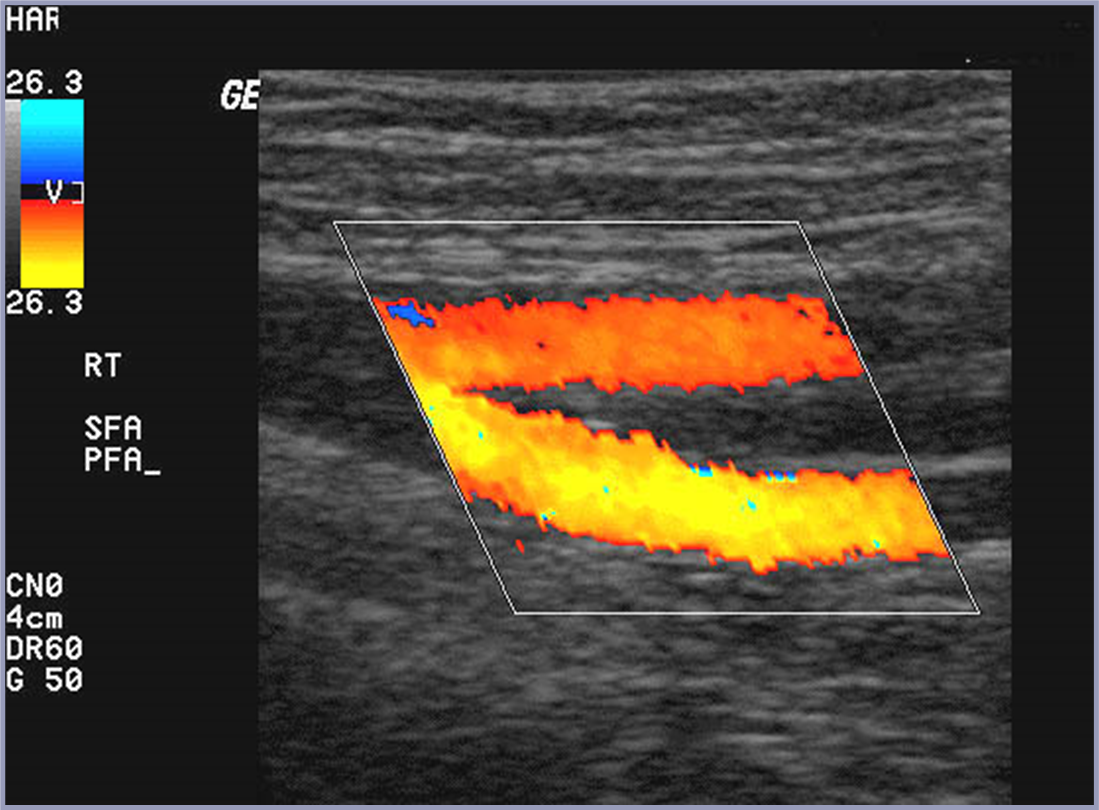
for the SFA segment, what should be evaluated with colour doppler?
the distal CFA and bi of the CFA into the SFA and profunda femoris (PFA)
proximal right SFA
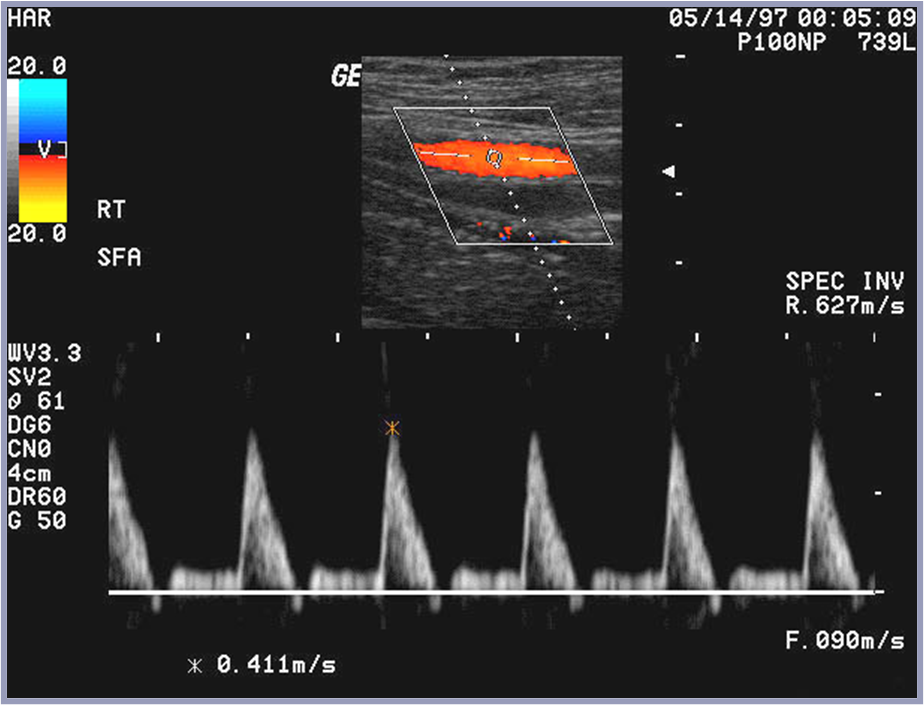
left SFA on US
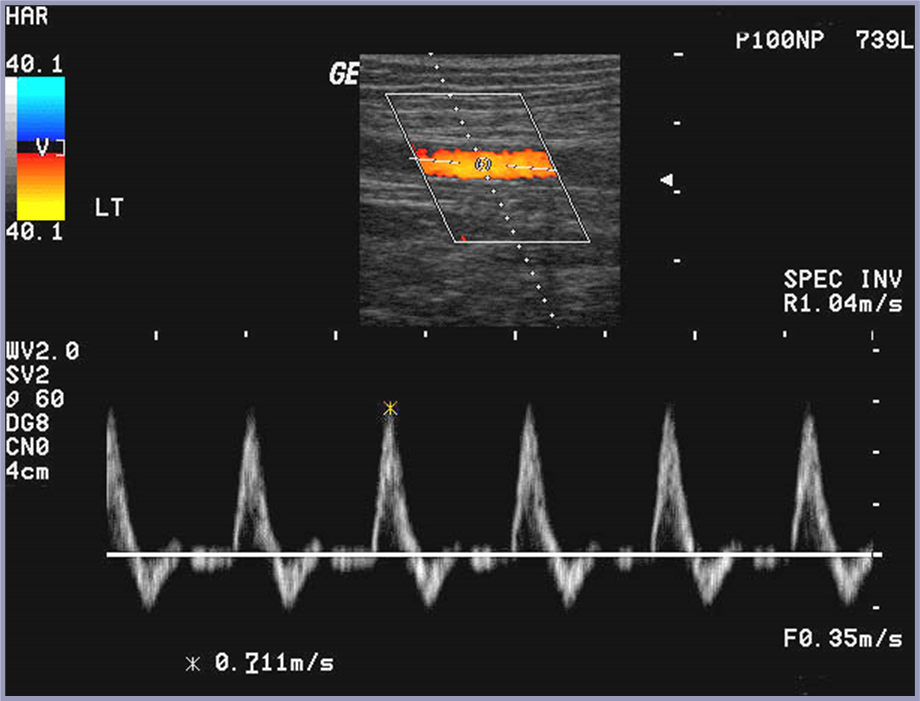
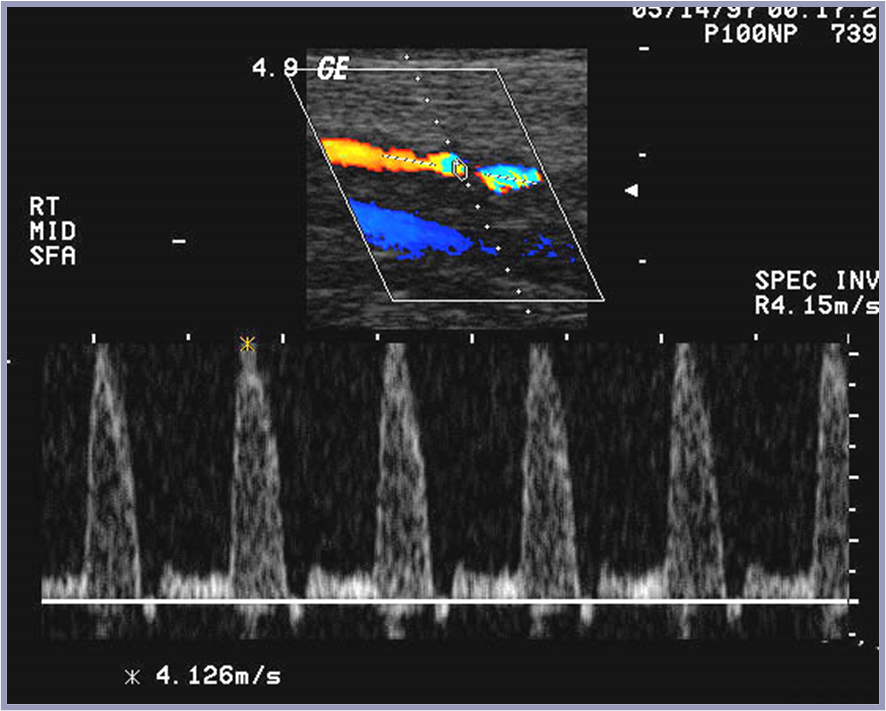
SFA stenosis on US
spectral tracing of SFA stenosis US
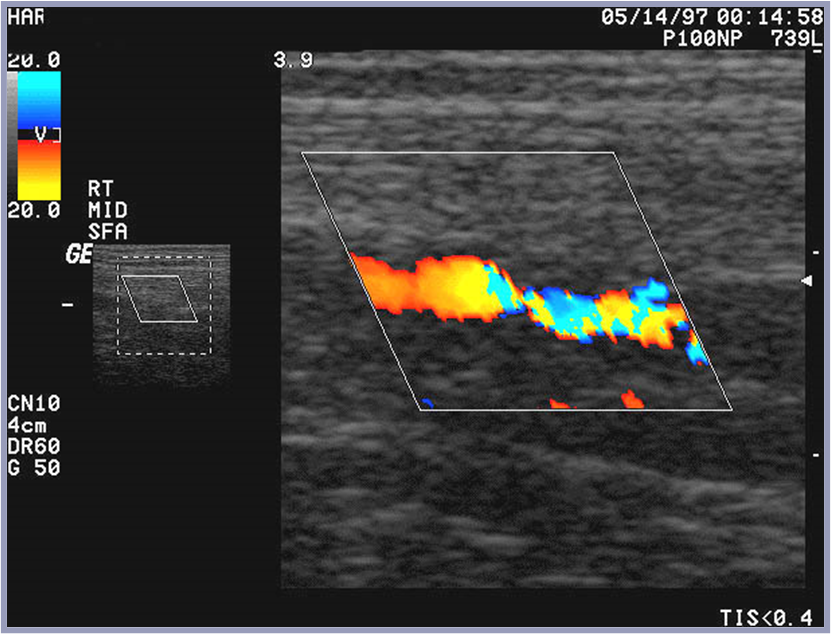
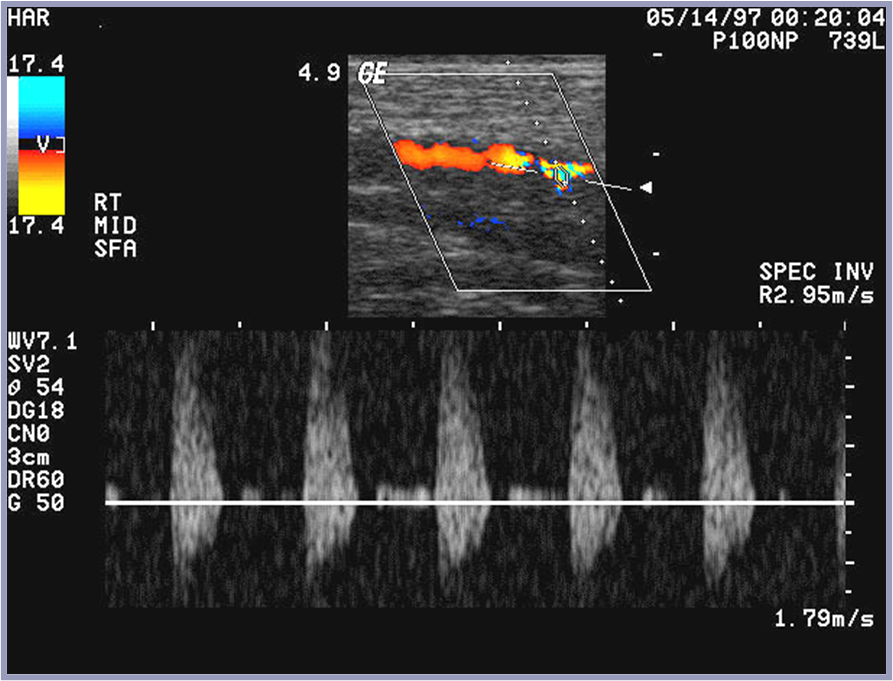
post stenotic turbulence of SFA (mid) US
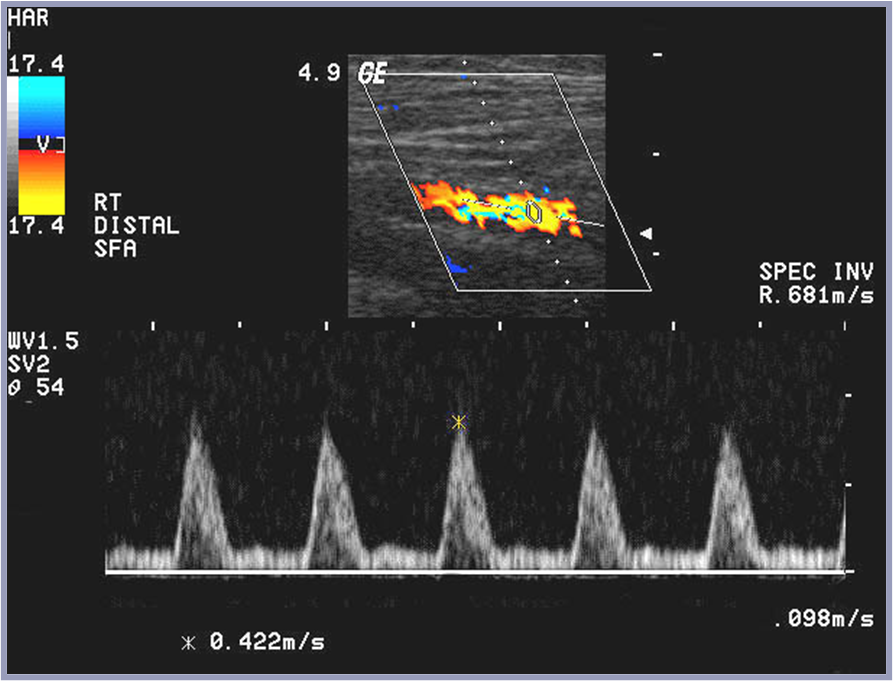
distal right SFA US
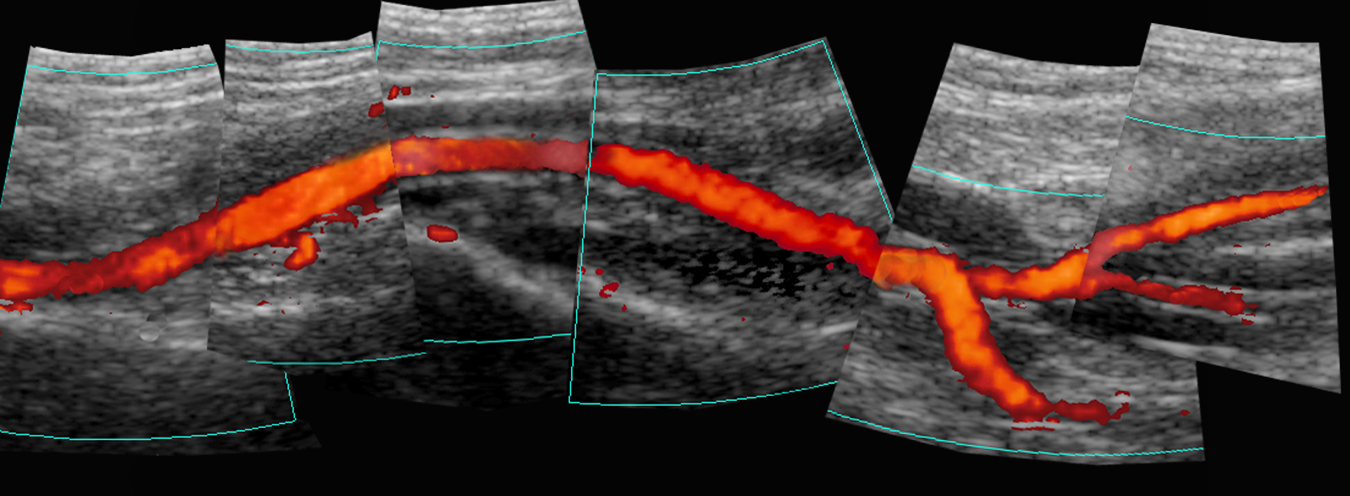
composite SFA occlusion on US
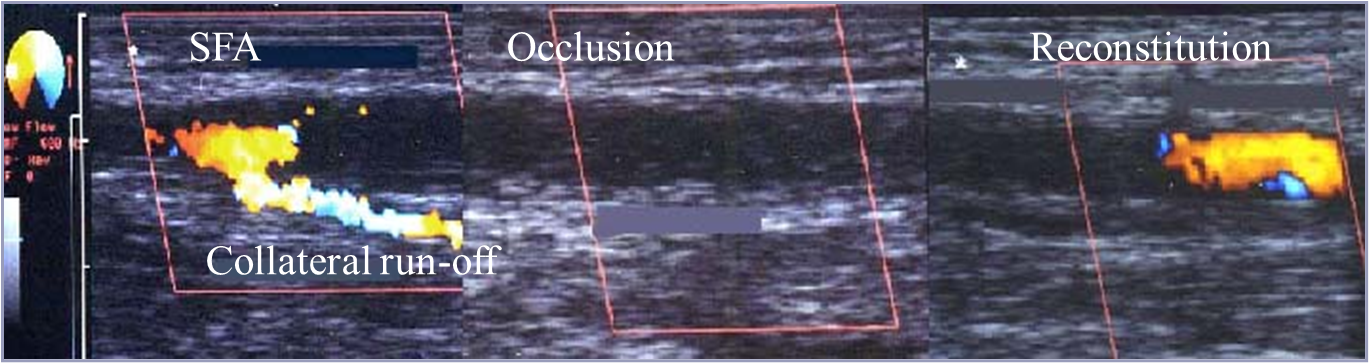
collateral inflow of SFA in TR US
flow entering an artery is usually reconstituted flow and indicates…
more proximal disease
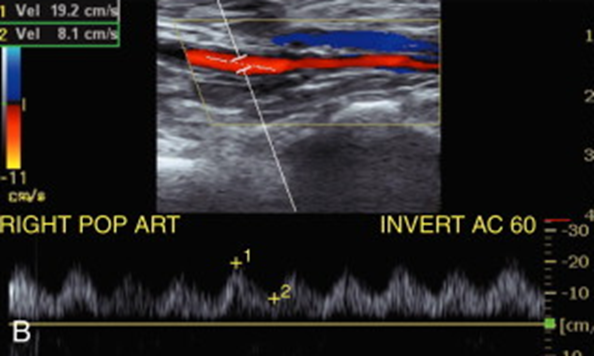
popliteal artery power doppler composite US (proximal to PTA)
the anterior tibial artery is seen to dive what direction on US?
goes off posteriorly
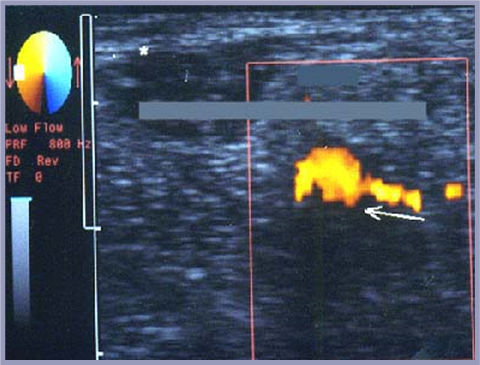
tibio-peroneal trunk US with colour
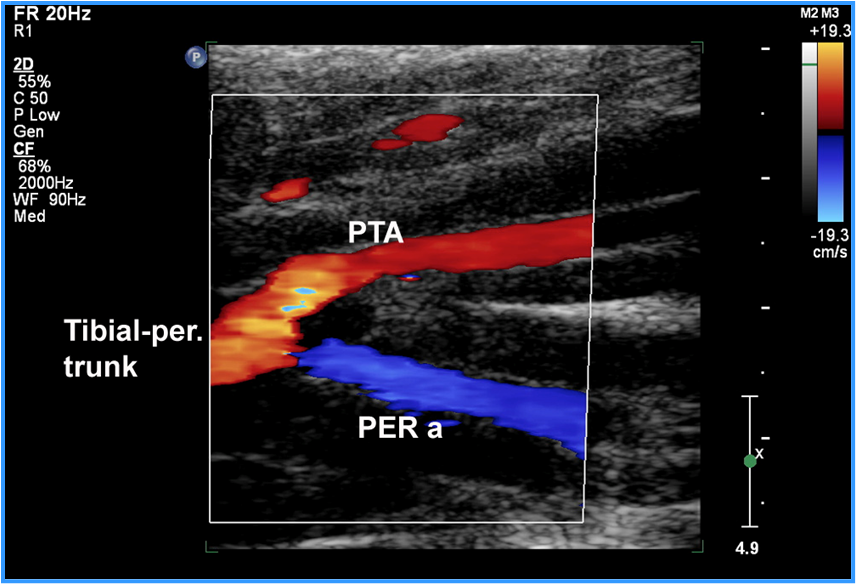
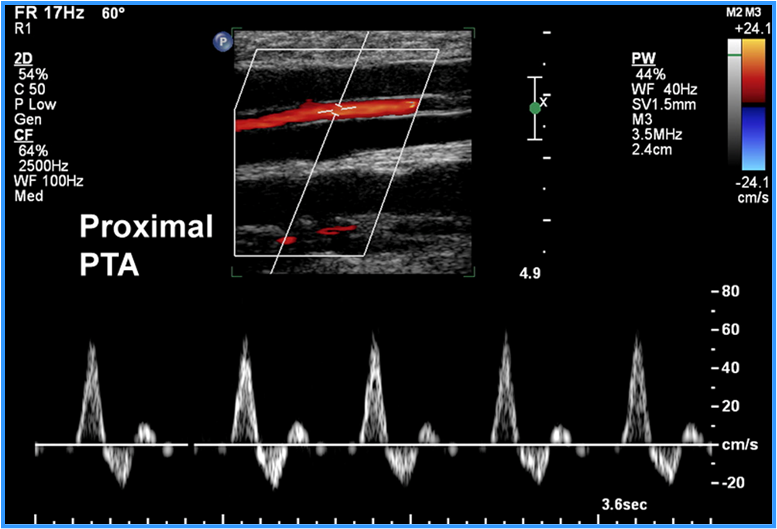
proximal PTA spectral US
radial & ulnar arteries can be used in what procedure?
CABG - Allan’s test
veins can be harvested for what bypasses?
fem-pop and fem-tibial bypass
duplex is used for
interval F/U post intervention
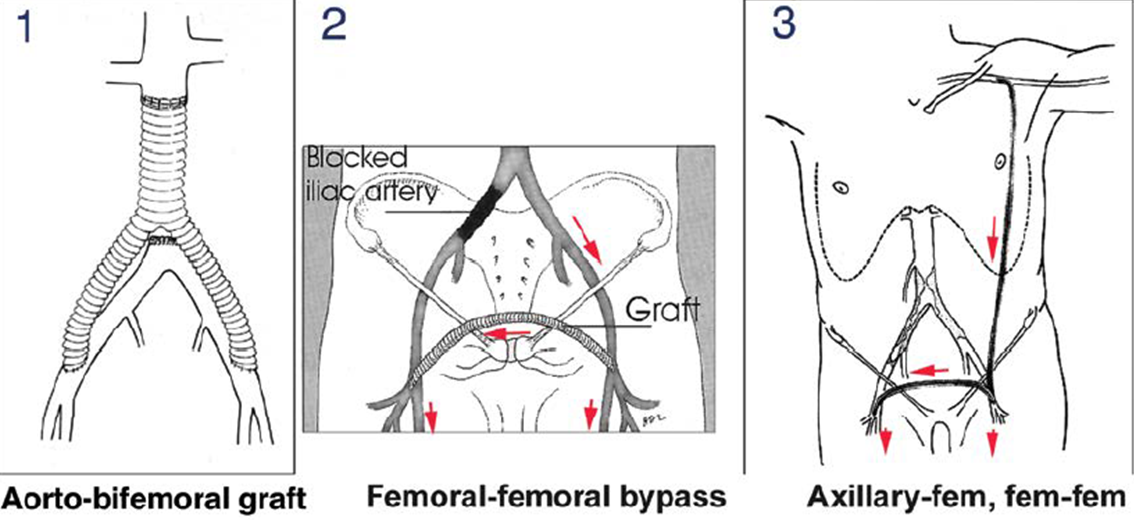
what are the 3 types of grafts for supra-inguinal bypass
bypass diseased distal AO/iliacs (EVAR)
bypass single iliac artery
bypass entire abdominal aorta
diagram of the 3 types of grafts for supra-inguinal bypass
3 categories for graft failure
technical failure (0-30 days post-op)
fibrointimal hyperplasia (1month-2years post-op)
progression of atherosclerosis
bypass grafts are preformed to avoid…
amputation, AKA “limb salvage”
Method for examining bypass grafts and stents
obtain ABIs and PVRs
do not perform segmental pressures over bypass
evaluate using grayscale, colour, doppler
assess for stenosis, wall irregularity, aneurysms, pseudoaneurysms, AVF
assess anastomosis for stenosis/defects
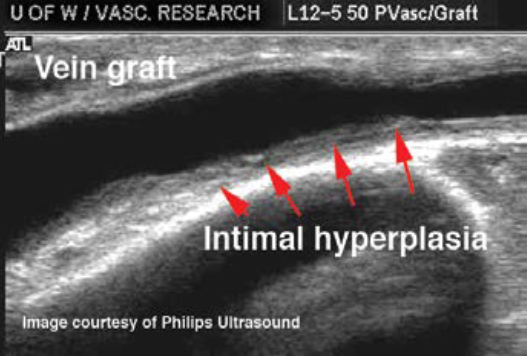
neo-intimal hyperplasia
check for hematoma/seroma post-op
obtain PSVs along graft & prox feeding & distal runoff. stenotic regions prox, at and distal
neo-intimal hyperplasia
overgrowth of plaque like material in vessels
in-situ vein graft on US showing intimal hyperplasia
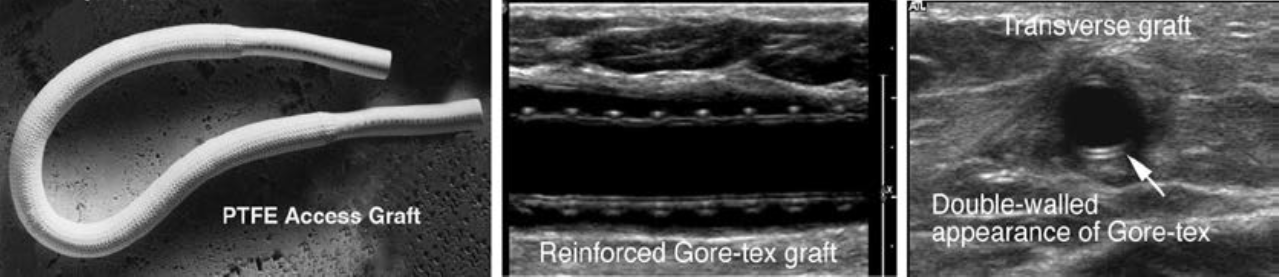
reinforced access graft on US
in situ vein graft stenosis US
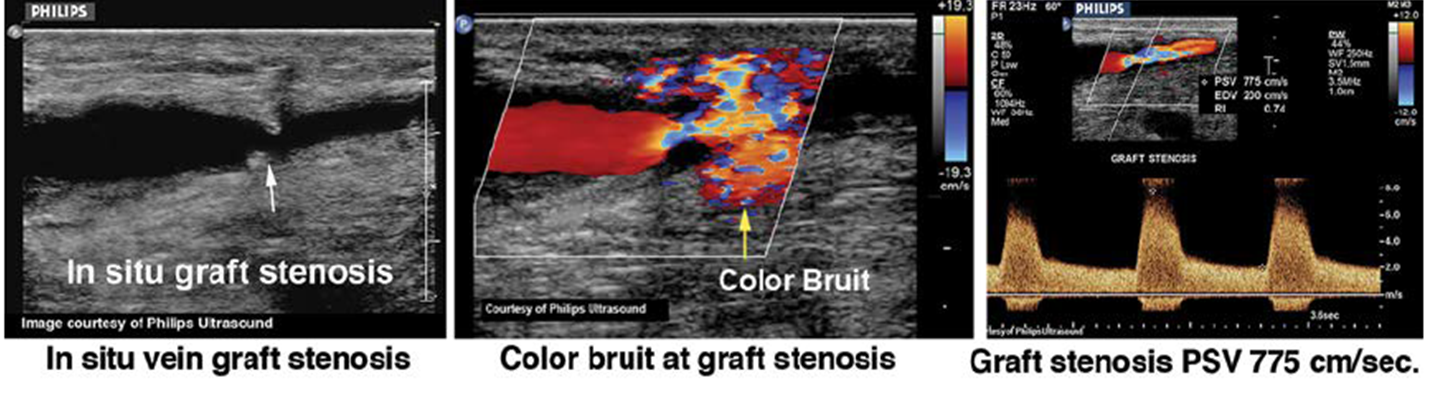
in bypass grafts and stents when evaluating for stenosis follow the general rule of these when comparing to pre-stenotic segment
velocity doubling (2:1 ratio)
post-stenotic turbulence
distal tardus parvus
if velocities are less than 40-45cm/s in the graft the patient is at risk for what?
graft thrombosis,
lower extremity aneurysms characteristics
more common in pop a. or SFA
may be bilateral
often asymptomatic with mural thrombus
what can be mistaken for venous thrombus?
mural thrombuswhat
what should be done to distinguish between a mural thrombus and a venous thrombus
ensure visualization of both vessel and use spectral doppler to differentiate between artery and vein
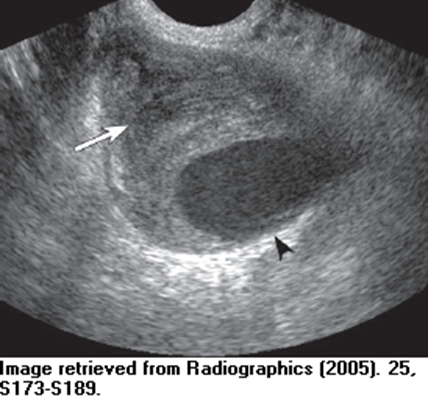
POP A aneurysm mimicking DVT US
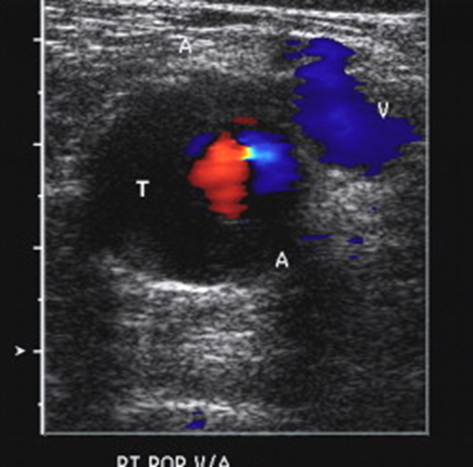
spectral doppler confirming arterial waveform for POP A aneurysm
what has a jhigh association with AAA
popliteal artery aneurysms
symptoms of pop a aneurysm
claudication
rest pain
limb ischemia
blue toe
nerve compression
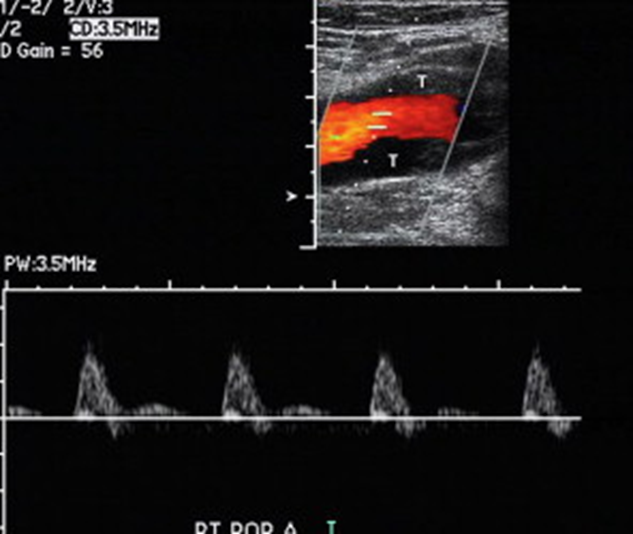
popliteal aneurysm in TR and LONG US
the normal popliteal artery should measure…
5-6mm
popliteal artery aneurysms have a high association with…
AAA
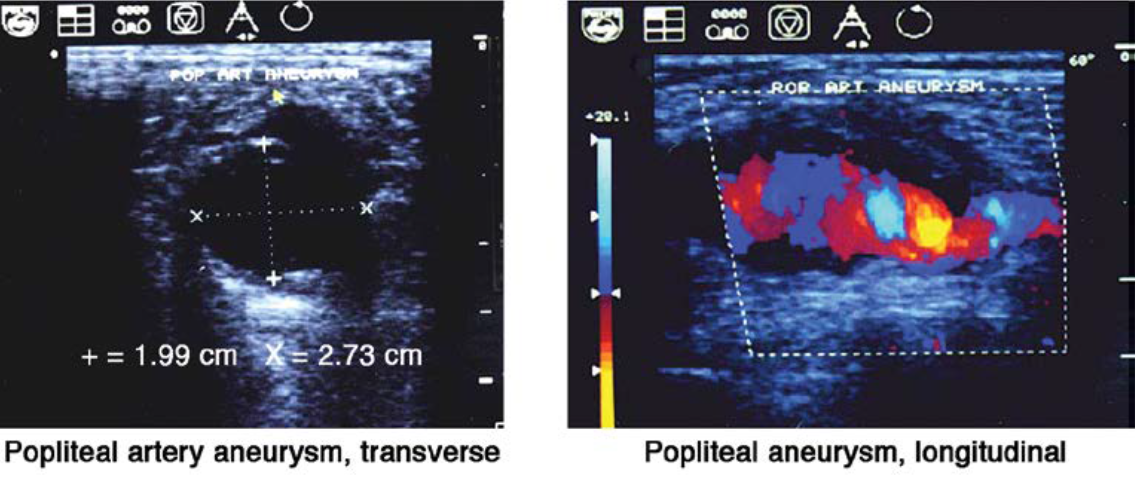
pseudoaneurysm
puncture of arterial wall from procedure that balloons adventitia wall outward
diagram for types of aneurysms compared to normal vessel
what is the most common site for interventional arterial access route (via cardiac catheterization)
femoral artery
a false aneurysm is not confined by
all 3 walls.
includes 1 or 2 of the arterial walls
what artery is most commonly affected with pseudoaneurysms
CFA (iliac and SFA are possible as well)
clinical symptoms of pseudoaneurysms
audible bruit
palpable, pulsating mass
ecchymosis (red & bruised)
complications that can occur from pseudoaneurysms
rupture
thrombosis of adjacent veins (compression can cause venous stasis)
sonogrpahic appearance of a pseudoaneurysm
assess puncture site
contained fluid collection adjacent to normal vessels
variable appearances (echogenic thrombus or swirling low-level echoes)
demonstrate “neck” of pseudoaneurysm (diameter & length)
CD = yin-yang sign
spectral = to-and-fro waveform
what is a differential for pseudoaneurysm
hematomawh
at is the most important thing to measure and assess during a pseudoaneurysm
the neck of the pseudoaneurysm (want to know for treatment)
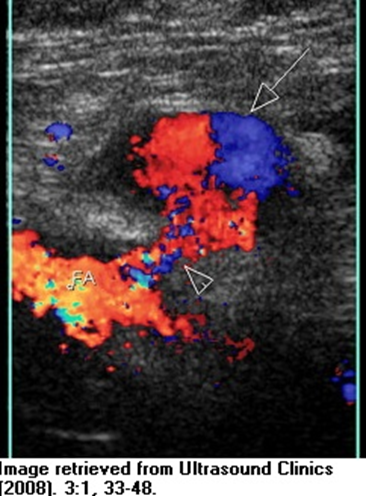
pseudoaneurysm Yin-yang sign US
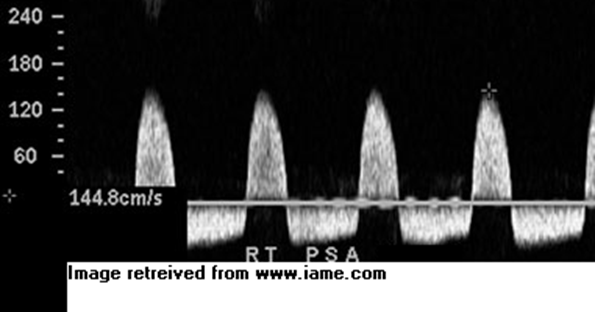
to-and-fro on spectral doppler from pseduoaneurysm
thrombus formation in pseudoaneurysm US
a short and wide neck on the pseudoaneurysm is important to document because…
if thrombin is used then it can travel to native artery and occlude it. So documenting it as short and wide means they look for alternative treatment (surgery)
what characteristics are best to have in the pseudoaneurysm neck
long and skinny to treat with thrombin
Treatment for pseudoaneurysm
ultrasound guided/sandbag compression
ultrasound guided thrombin injection
surgical repair (when neck is short and wide)
Ultrasound guided thrombin injection has the potential to thrombose to …
femoral artery (if short and wide neck)
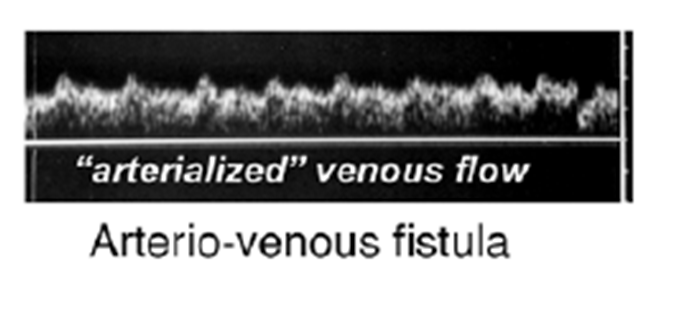
arteriovenous fistulas (AVF)
abnormal connection between adjacent arteries and veins
can be congenital or iatrogenic
iatrogenic causes of AVF
arterial or venous catheterization or intervention
penetrating trauma
AVF sonographic appearance
visualized color jet (shows connection)
high velocity waveform (turbulence, ambiguous arterial/venous patterns)
color bruit (color speckle over tissue)
arterialized venous flow on spectral
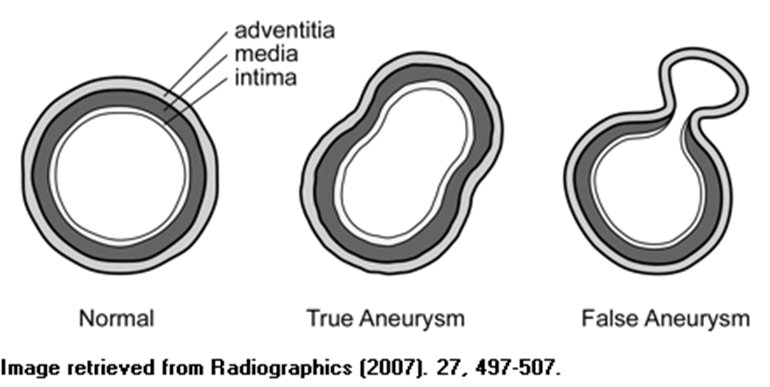
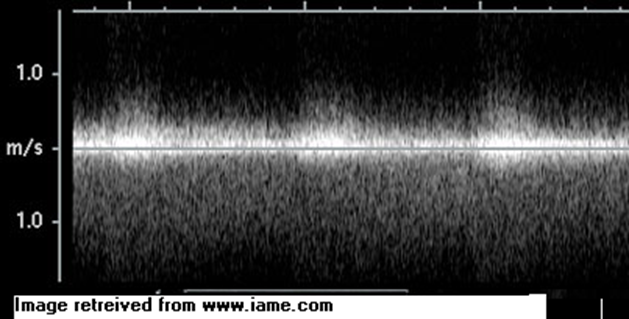
color on AVF between CFV & PFA
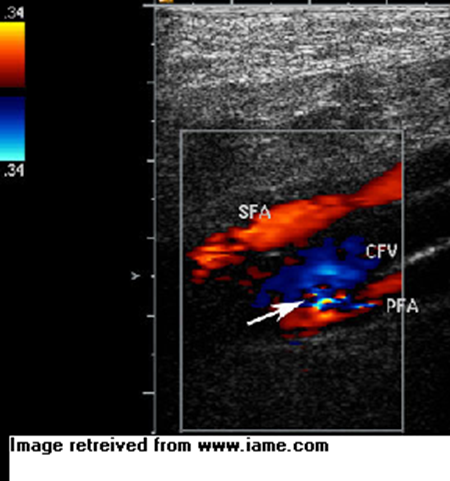
spectral tracing of CFV & PFA
blue toe syndrome
acute ischemic event
painful cyanotic regions to toes or foot
what causes blue toe syndrome
thrombo-emboli leading to occlusion
buerger’s disease is also called
thromboangitis obliterans
what is bueger’s disease
a fixed occlusive inflammatory process that causes thrombosis of digital arteries (fingers and toes)
bueger’s disease diagram

buerger’s disease is most commonly related to
male population and smokers,
can also occur in occupational trauma
primary Raynaud’s phenomenon
vasospastic disorder without underlying disease. the digital and palmar arteries without obstruction and perfusion to the digits at rest is normal