Ganong Ch 25, 26; GI Physiology and Ischemia-Reperfusion MDRs
1/334
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
335 Terms
Columnar Epithelial Cells of the GI Tract
Immediately adjacent to the nutrients in the lumen
Single layer
Barrier that nutrients must traverse to enter the body
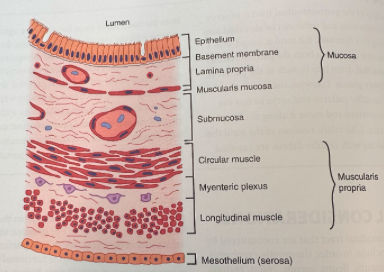
Lamina Propria of the GI Tract
Loose connective tissue below the epithelium
Contains many immune and inflammatory cells even in health
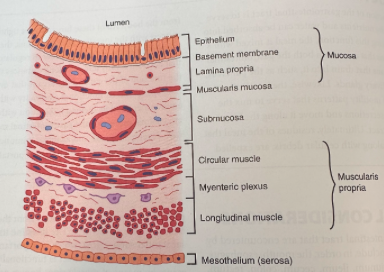
Where are the myenteric and submucosal nerve plexuses of the enteric nervous system located?
In the submucosa between the circular and longitudinal muscle layers
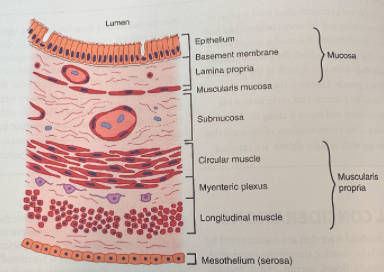
What innervates the epithelium and muscle layers of the GI tract?
Secretomotor nerves
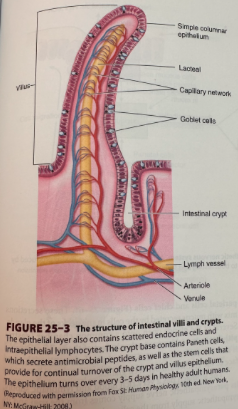
Intestinal Villi and Crypts
Villi maximize surface area throughout the small intestines
Stem cells that give rise to crypt and villus epithelial cells reside toward the base of the crypts and are responsible for completely renewing the epithelium every few days or so
Daughter cells undergo several rounds of cell division in the crypts then migrate out onto the villi where they are eventually shed
Microvilli on the apical membranes of the villus epithelial cells have a dense glycocalyx (brush border)
Protects the cells to some extent from the digestive enzymes
Brush border hydrolases also present and perform the final steps of digestion for specific nutrients
What are the paired salivary glands that produce saliva?
Parotid
Submandibular
Sublingual
Functions of Saliva
Initiates digestion, particularly of starch, mediated by amylase
Protects the oral cavity from bacteria (immunoglobulin A and lysozyme)
Lubricates food bolus (aided by mucins)
Tonicity and Acidity of Saliva
Hypotonic compared to plasma
Alkaline to neutralize any gastric secretions that reflux into the esophagus
Production and Modification of Saliva
Salivary glands consist of blind end pieces (acini) that produce the primary secretion containing the organic constituents dissolved in a fluid that is essentially identical in its composition to plasma
Composition of saliva is modified as if flows from the acini out into ducts that deliver saliva into the mouth
Na+ and Cl- are extracted and K+ and bicarbonate are added
Ducts are impermeable to water so loss of NaCl makes the saliva hypotonic
What controls salivary secretion?
Salivary secretion controlled almost entirely by neural influences
Parasympathetic branch of the autonomic nervous system plays the most prominent role
Sympathetic input increases the proteinaceous content of saliva but has little influence on volume
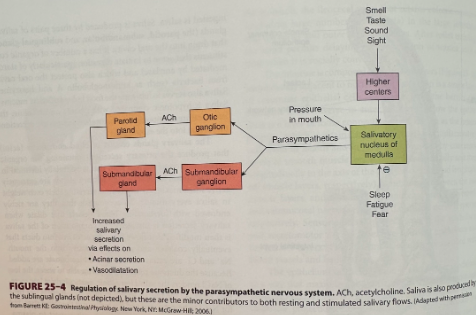
What triggers salivary secretion?
Secretion is triggered by reflexes that are stimulated by the physical act of chewing
Initiated before the meal is taken into the mouth as a result of central triggers that are prompted by thinking about, seeing, or smelling food
Salivary secretion also prompted by nausea
What inhibits salivary secretion?
Fear
Fatigue
Sleep
What do glands in the cardia and pyloric region of the stomach secrete?
Mucus
What is the parasympathetic nerve supply of the stomach?
Vagus
What is the sympathetic nerve supply of the stomach?
Celiac plexus
What are the phases of gastric secretion?
Cephalic phase - stomach readies itself to receive a meal before its taken in
Gastric phase
Intestinal phase - once the meal has left the stomach
Contents of Normal Gastric Juice (Fasting State)
Cations: Na+, K+, Mg2+, H+ (pH approximately 3.0)
Anions: Cl-, HPO2-, SO42-
Pepsins
Lipase
Mucus
Intrinsic factor
What do surface mucous cells secrete?
Mucus
Trefoil peptide
Bicarbonate
What do parietal cells secrete?
HCl
Intrinsic factor
What do enterochromaffin like cells secrete?
Histamine
What do chief cells secrete?
Pepsinogen
Gastric lipase
Trefoil Peptides
Stabilize the mucus-bicarbonate layer
Intrinsic Factor
Important for later absorption of Vitamin B12 or cobalamin
Pepsinogen
Precursor of pepsin which initiates protein digestion
Lipase
Digests dietary fats
What are the 3 primary stimuli of gastric secretion?
Gastrin
Histamine
Acetylcholine
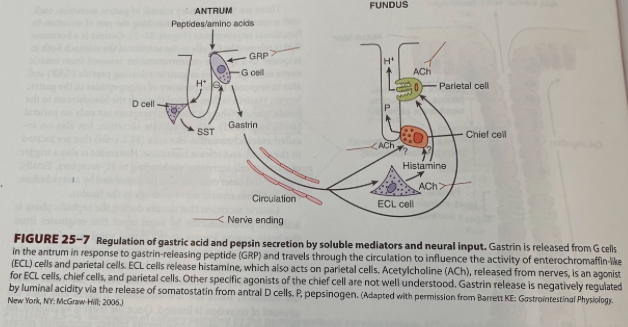
Stimulus of Gastric Secretion - Gastrin
Released by G cells in the antrum of the stomach
Released in response to gastrin-releasing peptide (GRP) and the presence of oligopeptides in the gastric lumen
Binds to receptors on parietal (and likely chief) cells to activate secretion
Binds to enterochromaffin-like cells (ECL cells) to release histamine
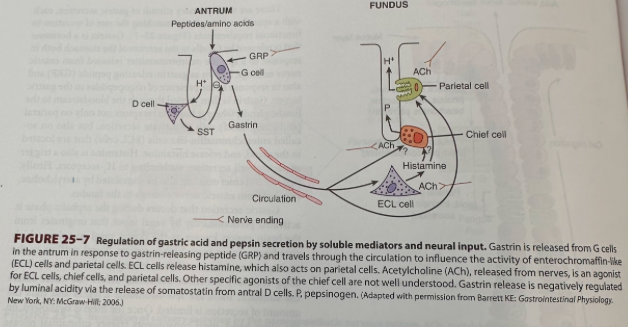
Stimulus of Gastric Secretion - Histamine
Trigger for parietal cell secretion via binding to H2 receptors
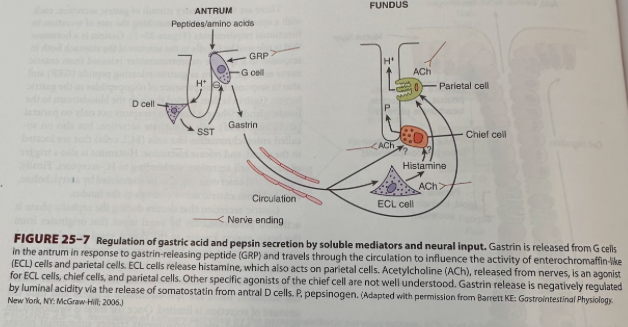
Stimulus for Gastric Secretion - Acetylcholine
Stimulates parietal and chief cells
Released from enteric nerve endings in the fundus
Gastric Secretion During the Cephalic Phase
Activated predominantly by vagal input
Originates from the dorsal vagal complex
Vagal outflow to the stomach releases GRP and acetylcholine, initiating secretory function
Gastric Secretion During the Gastric Phase
The meal triggers substantial release of gastric secretion
Physical presence of the meal distends the stomach and activates stretch receptors, which provoke a "vago-vagal" as well as local reflexes that further amplify secretion
Presence of the meal buffers gastric acidity
Otherwise acidity would serve as a feedback inhibitory signal to shut off secretion secondary to the release of somatostatin
Somatostatin
Inhibits G and ECL cells and secretion by parietal cells themselves
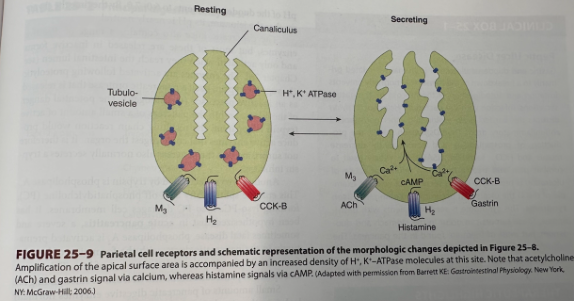
Secretion by the Parietal Cells
Have many mitochondria that supply energy to drive the apical H+,K+ ATPase, or proton pump, that moves H+ ions out of the parietal cell against a large concentration gradient
At rest, the proton pumps are sequestered in the parietal cell in tubulovesicles
When the parietal cells begin to secrete, these vesicles fuse with invaginations of the apical membrane area (canaliculi), amplifying the apical membrane area and positioning the proton pumps to begin acid secretion
Apical membrane also contains K+ channels which supply the K+ ions to be exchanged for H+ and Cl- channels that supply the counterion for HCl secretion
Secretion of protons is accompanied by the release of equivalent numbers of bicarbonate ions into the bloodstream
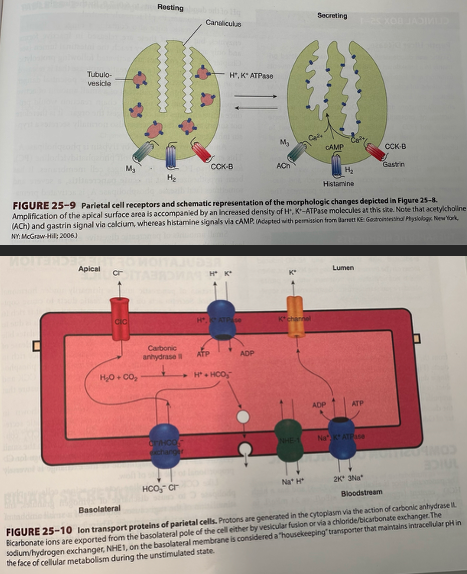
How do gastrin and acetylcholine promote secretion from the parietal cell?
By elevating cytosolic free calcium concentrations
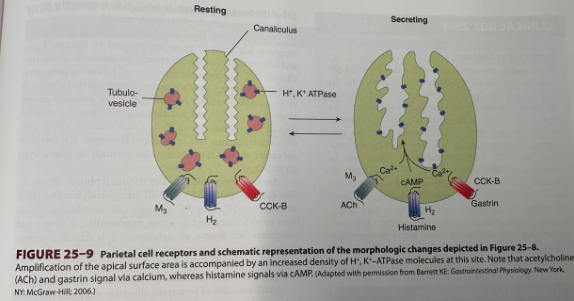
How does histamine stimulate increased secretion from the parietal cell?
By increasing intracellular cAMP
Synergistic Effect of Activation of the Parietal Cell
Pathways for activation are synergistic with a greater additive effect when histamine plus gastrin or acetylcholine are present, or all three
High rates of secretion can be stimulated with relatively small changes in availability of each of the stimuli
Therapeutically significant because secretion can be markedly inhibited by blocking the action of only one of the triggers (commonly histamine via H2-antagonists)
What enzyme does the salivary glands produce?
Salivary a-amylase
What activates salivary a-amylase?
Cl-
What is the substrate for salivary a-amylase?
Starch
Catalytic Function or Products of Salivary a-Amylase
Hydrolyzes 1:4a linkages, producing a-limit dextrins, maltotriose, and maltose
What are the enzymes produced by the stomach?
Pepsins (pepsinogens)
Gastric lipase
What activates pepsinogens?
HCl
What is the substrate for pepsin?
Proteins and polypeptides
Catalytic Function or Products of Pepsin
Cleave peptide bonds adjacent to aromatic amino acids
Substrate of Gastric Lipase
Triglycerides
Catalytic Function or Products of Gastric Lipase
Fatty acids and glycerol
Enzymes Produced by the Exocrine Pancreas
Trypsin (trypsinogen)
Chymotripsins (chymotripsinogens)
Elastase (proelastase)
Carboxypeptidase A (procarboxypeptidase A)
Carboxypeptidase B (procarboxypeptidase B)
Colipase (procolipase)
Pancreatic lipase
Cholesteryl ester hyrolase
Pancreatic a-amylase
Ribonuclease
Deoxyribonuclease
Phospholiapse A2 (prophospholiapse A2)
Trypsinogen Activator
Enteropeptidase
Chymotrypsinogen Activator
Trypsin
Proelastase Activator
Trypsin
Procarboxypeptidase A Activator
Trypsin
Activator of Procarboxypeptidase B
Trypsin
Activator of Pancreatic a-Amylase
Cl-
Activator of Prophospholipase A2
Trypsin
Substrate of Trypsin
Proteins and polypeptides
Substrate of Chymotrypsins
Proteins and polypeptides
Substrate of Elastase
Elastin, some other proteins
Substrate of Carboxypeptidase A
Proteins and polypeptides
Substrate of Carboxypeptidase B
Proteins and polypeptides
Substrate of Colipase
Fat droplets
Substrate of Pancreatic Lipase
Triglycerides
Substrate of Cholesteryl Ester Hydrolase
Cholesteryl esters
Substrate of Pancreatic a-Amylase
Starch
Substrate of Ribonulcease
RNA
Substrate of Deoxyribonuclease
DNA
Substrate of Phospholipase A2
Phospholipids
Catalytic Functions or Products of Trypsin
Cleave peptide bonds on carboxyl side of basic amino acids (arginine or lysine)
Catalytic Functions or Products of Chymotrypsins
Cleave peptide bonds on carboxyl side of aromatic amino acids
Catalytic Functions or Products of Elastase
Cleaves bonds on carboxyl side of aliphatic amino acids
Catalytic Functions or Products of Carboxypeptidase A
Cleave carboxyl terminal amino acids that have aromatic or branched aliphatic side chains
Catalytic Functions or Products of Carboxypeptidase B
Cleave carboxyl terminal amino acids that have basic side chains
Catalytic Functions or Products of Colipase
Binds pancreatic lipase to oil droplet in the presence of bile acids
Catalytic Functions or Products of Pancreatic Lipase
Monoglycerides and fatty acids
Catalytic Functions or Products of Cholesteryl Ester Hydrolase
Cholesterol
Catalytic Functions or Products of Pancreatic a- Amylase
Hydrolyzes 1:4a linkages, producing a-limit dextrins, maltotriose, and maltose
Catalytic Functions or Products of Ribonuclease
Nucleotides
Catalytic Functions or Products of Deoxyribonuclease
Nucleotides
Catalytic Functions or Products of Phospholipase A2
Fatty acids, lysophospholipids
Enzymes Produced by Intestinal Mucosa
Enteropeptidase
Aminopeptidases
Carboxypeptidases
Endopeptidases
Dipeptidases
Maltase
Lactase
Sucrase
Isomaltase
Nuclease and related enzymes
Substrate of Enteropeptidase
Trypsinogen
Substrate of Aminopeptidases
Polypeptides
Substrate of Carboxypeptidases
Polypeptides
Substrate of Endopeptidases
Polypeptides
Substrate of Dipeptidases
Dipeptides
Substrate of Maltase
Maltose, maltotriose
Substate of Lactase
Lactose
Substrate of Sucrase
Sucrose; also maltotriose and maltose
Substrate of Isomaltase
a-limit dextrins, maltose
Maltotriose
Substrate of Nuclease and Related Enzymes
Nucleic acids
Catalytic Functions or Products of Enteropeptidase
Trypsin
Catalytic Functions or Products of Aminopeptidases
Cleave amino terminal amino acids from peptide
Catalytic Functions or Products of Carboxypeptidases
Cleave carboxyl terminal amino acid from peptide
Catalytic Functions or Products of Endopeptidases
Cleave between residues in midportion of peptide
Catalytic Functions or Products of Dipeptidases
Two amino acids
Catalytic Functions or Products of Maltase
Glucose
Catalytic Functions or Products of Lactase
Galactose and glucose
Catalytic Functions or Products of Sucrase
Fructose and glucose
Catalytic Functions or Products of Isomaltase
Glucose
Catalytic Functions or Products of Nuclease and Related Enzymes
Pentoses and purine and pyrimidine bases
What is pancreatic secretion controlled by?
In part by a reflex mechanism
In part by the GI hormones secretin and cholecystokinin (CCK)