OCR A Level Biology Module 4
1/176
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
177 Terms
Define disease
A condition that impairs the normal functioning of an organism
Define pathogen
organism that causes disease. e.g. bacteria, viruses, fungi and protoctists (type of single-celled eukaryotic organism).
What is a communicable disease?
A disease that can spread between organisms
Examples of diseases caused by bacteria (and what it affects)
Tuberculosis ---> animals, typically humans+cattle.
Bacterial meningitis ---> humans
Ring rot ---> potatoes, tomatoes.
Examples of diseases caused by viruses (and what it affects)
HIV/AIDS ---> humans
Influenza ---> animals+humans
Tobacco mosaic virus (TMV) ---> plants
Examples of diseases caused by fungi (and what it affects)
Black sigatoka ---> banana plants
Ringworm ---> cattle
Athlete's foot ---> humans
Examples of diseases caused by protoctists (and what it affects)
Potato/tomato late blight--->potatoes/tomatoes
Malaria ---> animals+humans
How can communicable diseases be spread?
direct and indirect transmission.
direct transmission
- disease transmitted directly from one organism to another.
- droplet infection (coughing/sneezing droplets of mucus/saliva directly onto someone), sexual intercourse, touching an infected organism.
Examples of direct transmission diseases
- HIV transmitted between humans via sexual intercourse and from a mother to unborn child through placenta.
- Athlete's foot spread via touch.
indirect transmission
When a disease is transmitted from one organism to another via an intermediate ---> incl. air, water, food, vector (another organism).
Examples of indirect transmission diseases
- Potato/tomato late blight spreads when spores are carried between plants - first in the air, then in water.
- Malaria spreads between humans + animals via mosquitoes (insects that feed on blood). Acts as vectors - spread the protoctists that cause the disease.
pathogen transmission routes
direct contact
vectors
water
wind
indirect contact
How do living conditions affect disease transmission?
overcrowded living conditions increase the transmission of many communicable diseases.
How do social factors affect disease transmission?
social factors (e.g. income, occupation, area where person lives) can increase transmission of communicable diseases.
Example of how living conditions can increase disease transmission
Tuberculosis (TB) is spread directly via droplet infection and indirectly because the bacteria can remain in air for long periods of time and infect new people.
- risk of TB increased in crowded living conditions.
Example of how social factors can increase disease transmission
Risk of HIV infection high in places where there's ltd. access to good healthcare and health education.
Example of how climate can increase disease transmission
- potato/tomato late blight common during wet summers because the spores need water to spread.
- malaria most common in tropical countries which are humid and hot - ideal conditions for mosquitoes (malaria vectors) to breed.
What are the animal defences that act as barriers to infection?
- skin
- mucous membranes
- blood clotting
- inflammation
- wound repair
- expulsive reflexes
What occurs if pathogens make it past the animal defences?
Immune system responds.
Animal defences - the skin
- physical barrier, blocks pathogens.
- chemical barrier, produces antimicrobial chemicals.
Animal defences - mucous membranes
- protect body openings exposed to environment.
- some membranes secrete mucus (traps pathogens + contains antimicrobial enzymes).
Platelets
fragments of cells in blood that form series of chemical reactions that take place when exposed to damaged blood vessels, forming blood clots.
Animal defences - blood clotting
- blod clot = mesh of protein fibres.
- plug wounds, preventing pathogen entry + blood loss.
- formed by series of chemical reactions that take place when platelets are exposed to damaged blood vessels.
Animal defences - inflammation
triggered by tissue damage - damaged tissue release molecules which: increase permeability of blood vessels, (leak fluid into surrounding area) and vasodilation.
- swelling caused, helps isolate pathogens that may have entered.
- molecules cause vasodilation, increasing blood flow to area - makes it hot + brings WBCs to area.
Animal defences - wound repair
- surface repaired by outer layer of skin cells dividing and migrating to edges of wound.
- tissue below wound contracts to bring edges of the wound close together.
- repaired with using collagen fibres - too many = scar forms.
Animal defences - expulsive reflexes
- incl. coughing + sneezing - to expel foreign objects, including pathogens, automatic.
- sneeze happens when mucous membranes in nostrils ate irritated by dust/dirt.
- cough stems from irritation in respiratory tract.
What are the plant defences that act as barriers to infection?
- physical plant defences (e.g. waxy cuticle, cell walls, callose).
- chemical plant defences (e.g. antimicrobial chemicals)
Describe the physical plant defences
- waxy cuticle, barrier against pathogen entry + stop water collecting on leaf, which could cause infection.
- cell walls, physical barrier against pathogens that make it past waxy cuticle.
- polysaccharide callose deposited between cell walls and plasma membranes during times of stress (e.g. pathogen invasion).
- callose deposition makes it harder for pathogens to enter cells, deposition at plasmodesmata limit spread of viruses between cells.
Describe the chemical plant defences
- antimicrobial chemicals kill pathogens/inhibit growth.
- other chemicals secreted are toxic to insects - reduces insect-feeding on plants + reduces risk of infection by viruses carried by insect vectors.
Examples of chemical plant defences
- Saponins produced, destroy cell membranes of pathogens.
- phytoalexins inhibit the growth of pathogens.
Examples of the skin acting as a barrier to infection
- skin cells secrete fatty acids, such as oleic acid, that can kill some bacteria. Can also lower pH of skin, create acidic environment that's difficult for pathogens to colonise.
- skin cells secrete lysozyme, enzyme which catalyses breakdown of carbohydrates in cell walls of some bacteria.
Examples of mucous membranes acting as a barrier to infection
- gas-exchange system, goblet cells produce mucus, cilia beat + move mucus up trachea to throat to be swallowed.
What is the immune response?
The body's defensive reaction to a foreign antigen. Antigens on pathogen's cell surface identified as foreign + immune system cells activated.
What are the different immune responses?
- non-specific response
- specific response (antigen specific, involves T + B lymphocytes).
Antigen
molecules (usually proteins/polysaccharides) found on surface of cells.
Main stages of the immune response
- phagocytosis
- T lymphocyte activation
- B lymphocyte activation + plasma cell production
- antibody production
Opsonin receptors
located on phagocytic cells, constant region on antibody binds to them to cause phagocyte to engulf pathogen/s)
Describe phagocytosis in the immune response
- pathogen's antigens recognised.
- cytoplasm of phagocyte moves round pathogen, engulfing it - made easier by opsonins.
- pathogen now contained in phagosome.
- lysosome fuses with phagosome. Enzymes breakdown pathogen.
- phagocyte sticks the pathogen's antigens on its surface to activate other immune system cells - phagocyte now acts as an antigen-presenting cell (APC).
- neutrophils move towards a wound in response to cytokines (released by cells at site of wound).
Neutrophils
type of phagocyte, first WBC to respond to a pathogen inside the body.
Cytokines
proteins that act as messenger molecules.
Phagosome
vesicle containing the pathogen in cytoplasm of phagocyte.
Describe T lymphocyte activation in the immune response
- type of WBC.
- surface covered with receptors that bind to antigens presented by APCs.
- each T lymphocyte has a different receptor, when meeting a complementary antigen, it binds + activates T lymphocyte (clonal selection).
- activated T lymphocyte divide to produce clones which differetiate into different types of T lymphocytes (clonal expansion).
What are the different types of activated T lymphocytes?
- T helper cells = release substances to activate B lymphocytes.
- T killer cells = attach to antigens on pathogen, kill cell.
- T regulatory cells = suppress immune response from other WBCs - helps stop immune system cells attacking host's body cells.
- Memory cells.
Describe B lymphocyte activation and plasma cell production in the immune response
- B lymphocytes are a type of WBC, covered with antibodies (proteins that bind antigens to form an antigen-antibody complex).
- each B lymphocyte has a different shaped antibody on its membrane, so different ones bind to different shaped antigens.
- B lymphocyte activated by binding to complementary antigen and helped by substances from T helper cells (clonal selection).
- activated B lymphocyte divides into plasma cells + memory cells. (clonal expansion).
Define antibody
made in response to an antigen (made by an activated B-lymphocyte), attaches antigens so they can be phagocytised.
What ISN'T a role of antibodies
- destroy antigens directly
- BUT to help immune cells destroy pathogens effectively.
define plasma cells
a fully differentiated B cell that produces a single type of antibody.
another name for antibodies
immunoglobulins
Describe antibody production in the immune response
- plasma cells secrete loads of the antibody (specific to the antigen).
- these bind to pathogen's antigens, forming lots of antigen-antibody complexes (signal for immune system to attack/destroy pathogen.
Cell signalling and the immune response
- cell releases/presents a substance that binds to receptors on another cell (causes response in the other cell).
- cell signalling helps activate the different types of WBCs that are needed.
Example of cell signalling in the immune response
- T helper cells release interleukins (type of cytokine) that bind to receptors on B lymphocytes.
- B lymphocytes are activated as the T helper cells are signalling to the B lymphocytes there's a pathogen in the body.
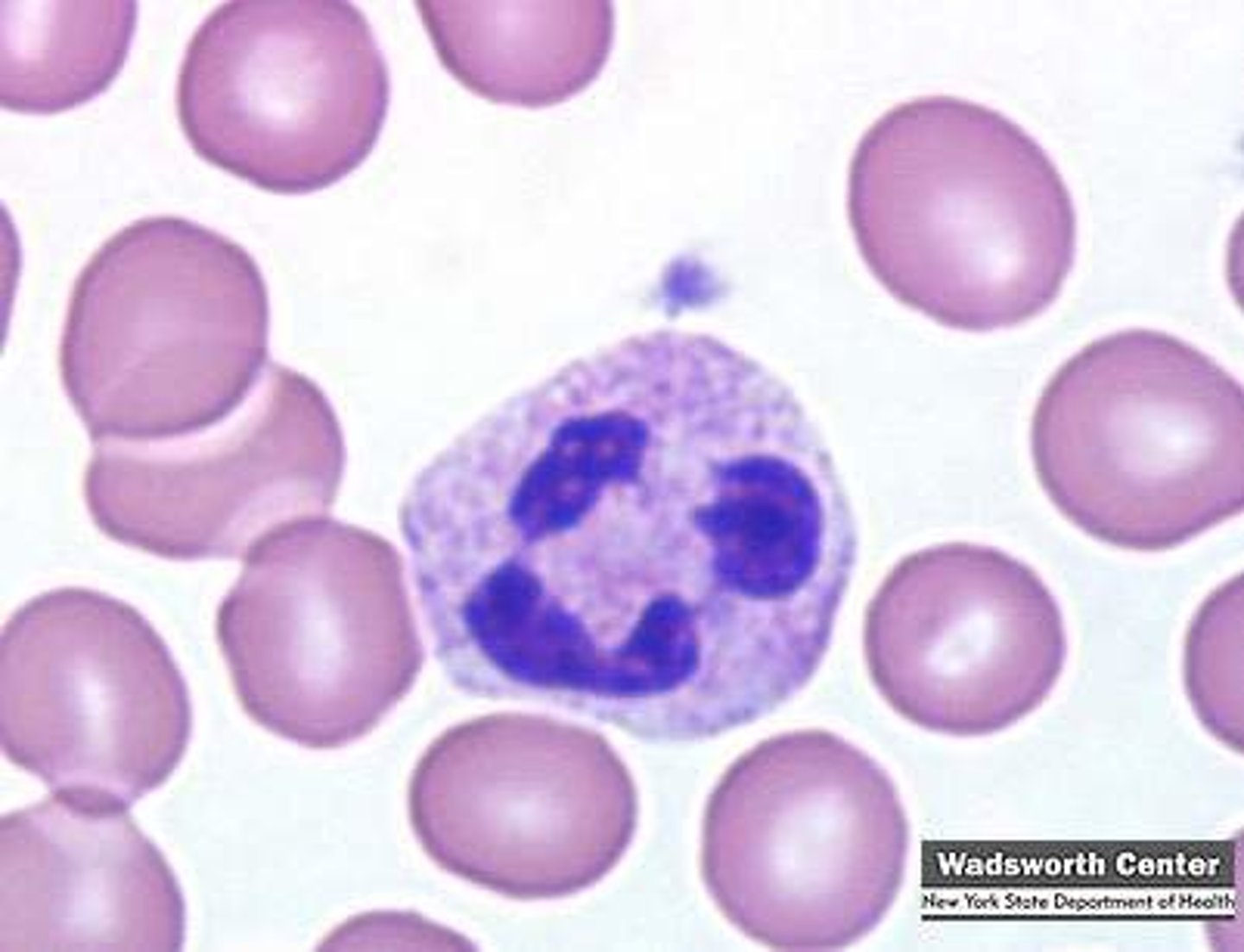
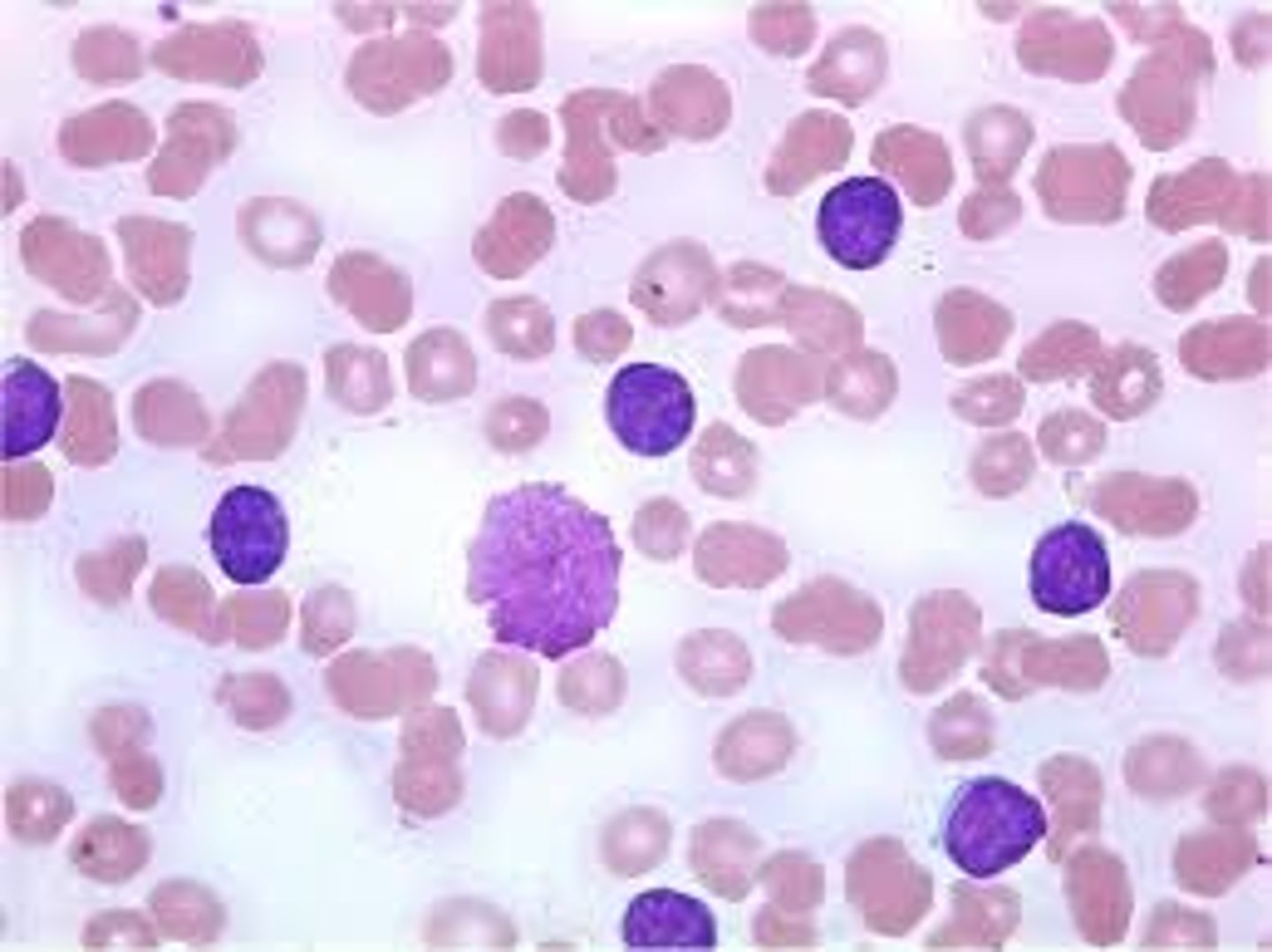
Blood smears
- RBCs = easy to spot, no nucleus.
- neutrophil = nucleus is multi-lobed, grainy cytoplasm.
- monocyte = biggest WBC, type of phagocyte. Kidney-bean shaped nucleus, non-grainy cytoplasm.
- lymphocyte = nucleus takes u most of cell, little (non-grainy) cytoplasm to be seen.
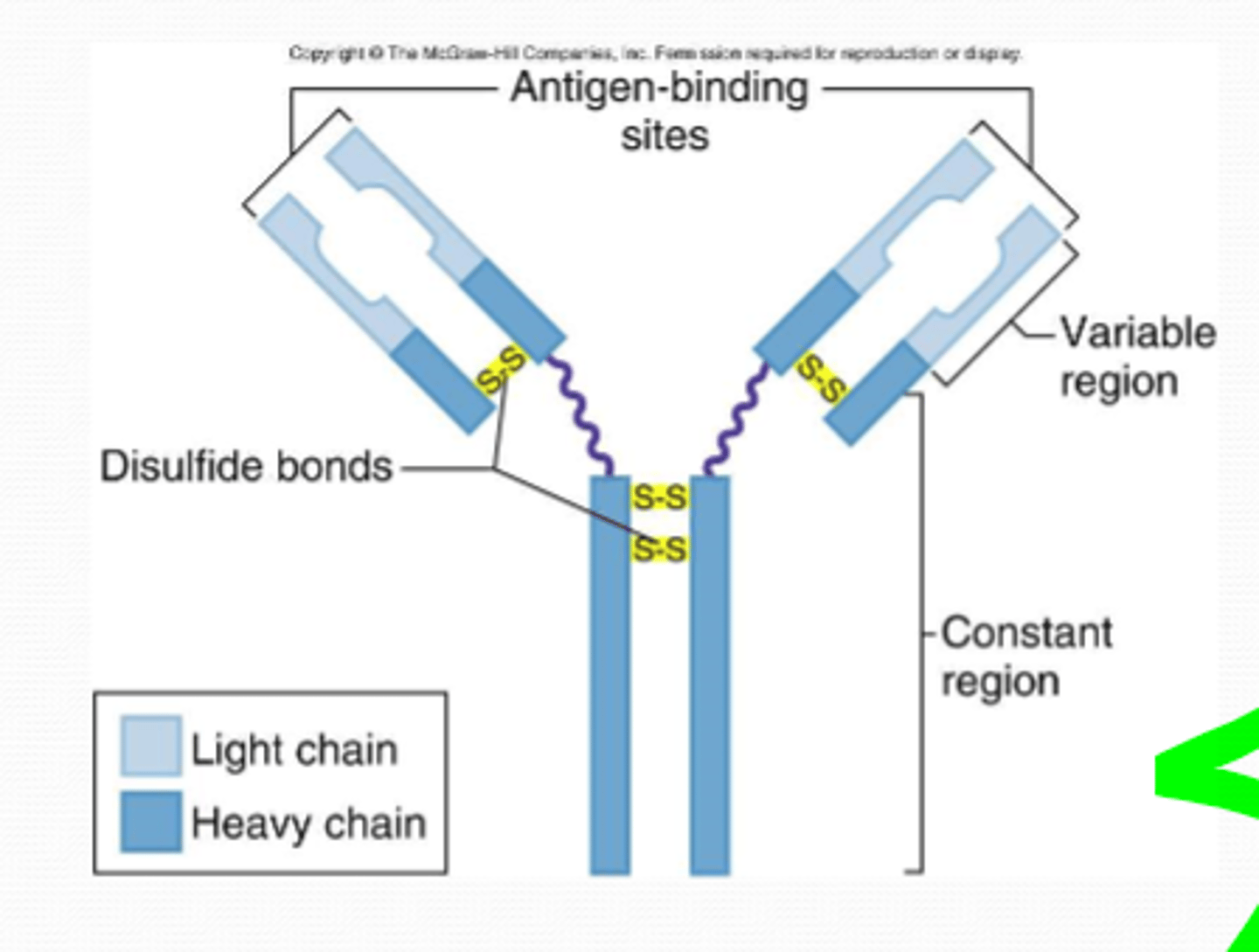
Antibody stucture
- Y-shaped proteins
- 4 polypeptide chains, held by disulfide bridges
- constant region = same in ALL antibodies (bind to receptors on immune system cells)
- variable regions = site where antibody binds to specific antigen (forming antigen-binding sites)
- 'heavy' chains = 2x longest chains
- 'light' chains = 2x shortest chains
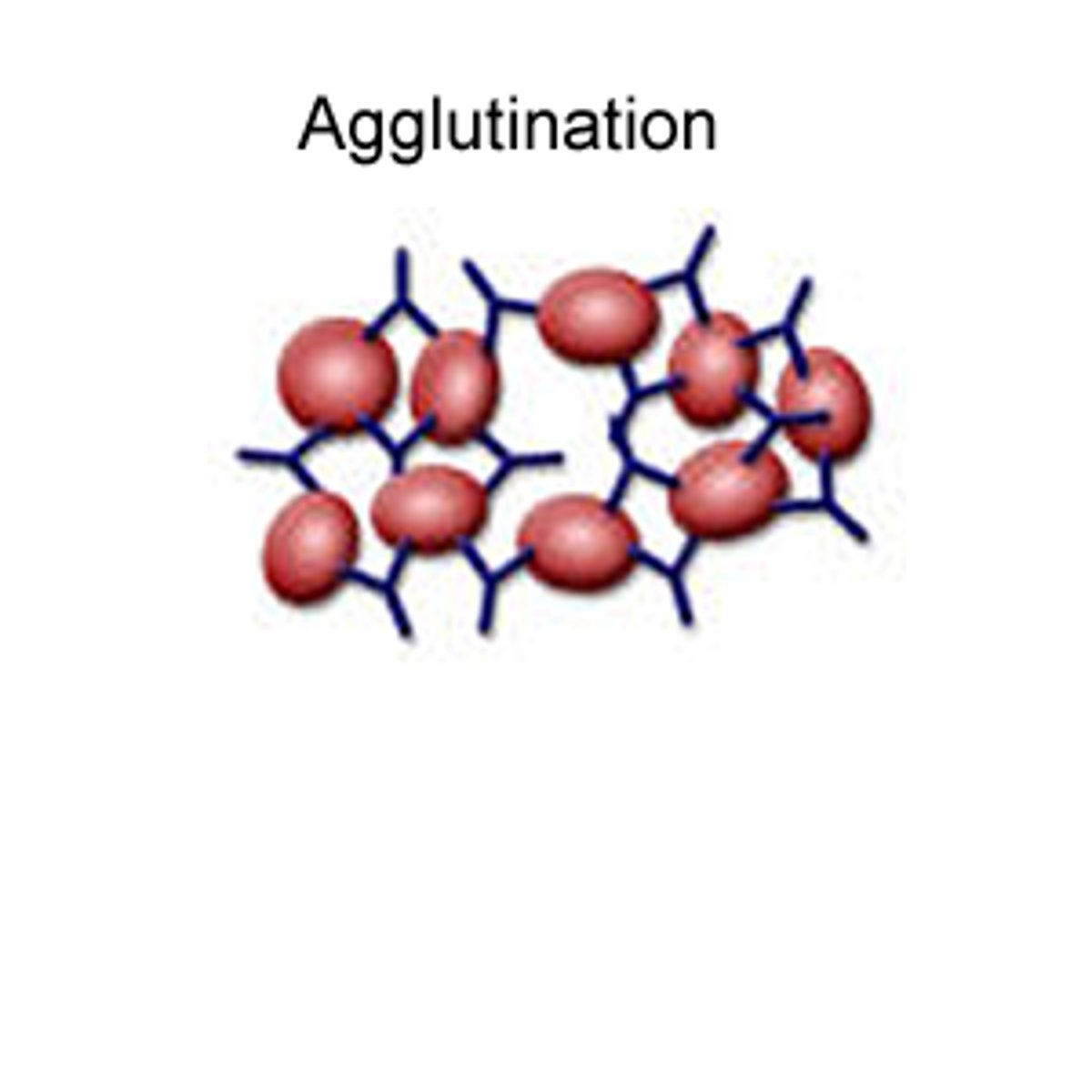
What are the 3 roles of antibodies in clearing infections?
1) Agglutinating pathogens
2) Neutralising toxins.
3) Preventing pathogen binding to human cells.
Agglutination of pathogens
- antibody can bind to two pathogens at same time, pathogens become clumped together.
- easier for multiple pathogens to be engulfed at once
- harder for pathogens to enter host cells
Antibodies in neutralising toxins
- antibodies bind to toxins released by phagocytes and neutralise them, prevents damage by toxins.
Antibodies in preventing the pathogen binding to human cells
- antibodies bind to pathogen's antigens = block cell-surface receptors the pathogens need to bind to host cells.
---> pathogen can't attach to host cells.
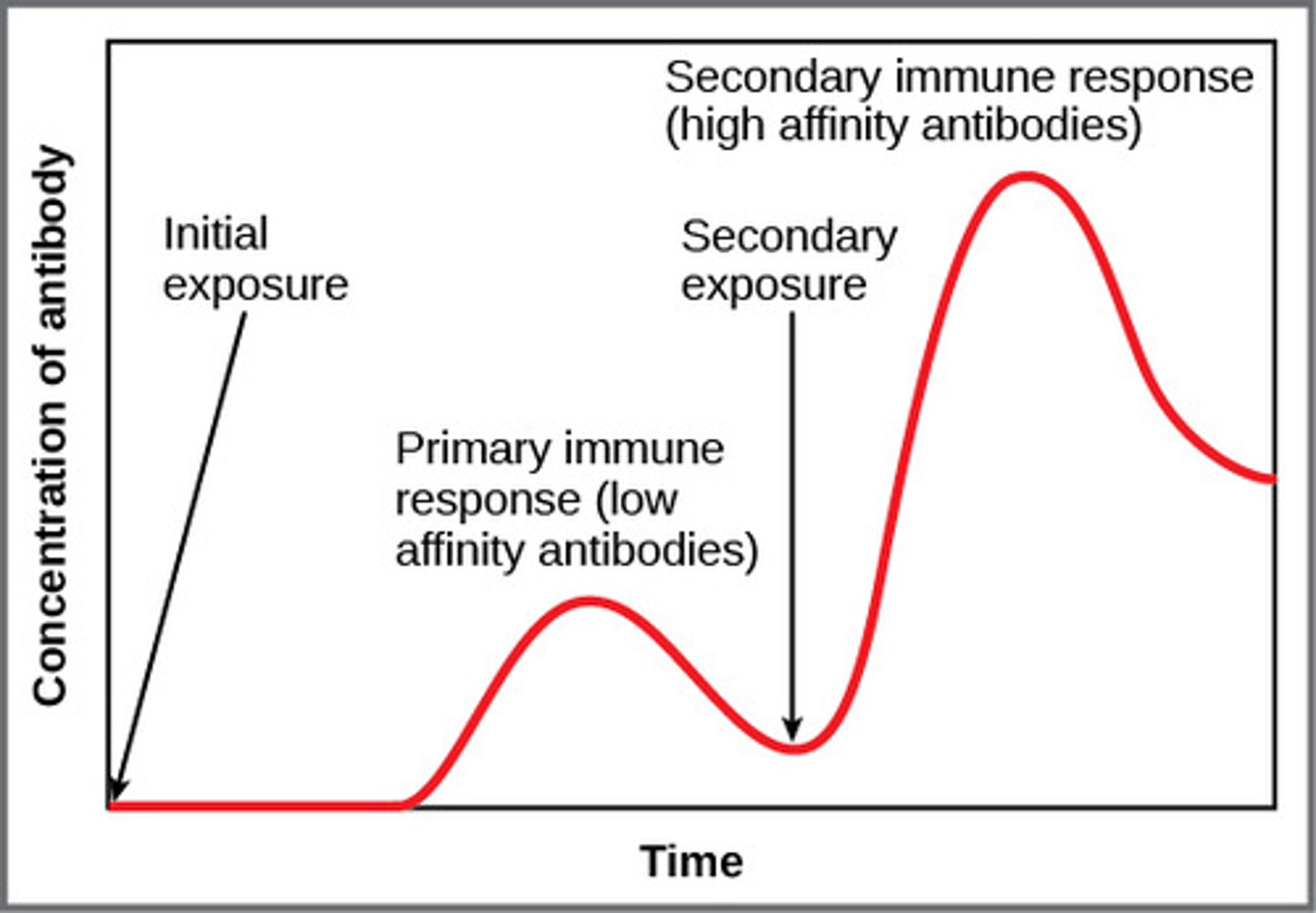
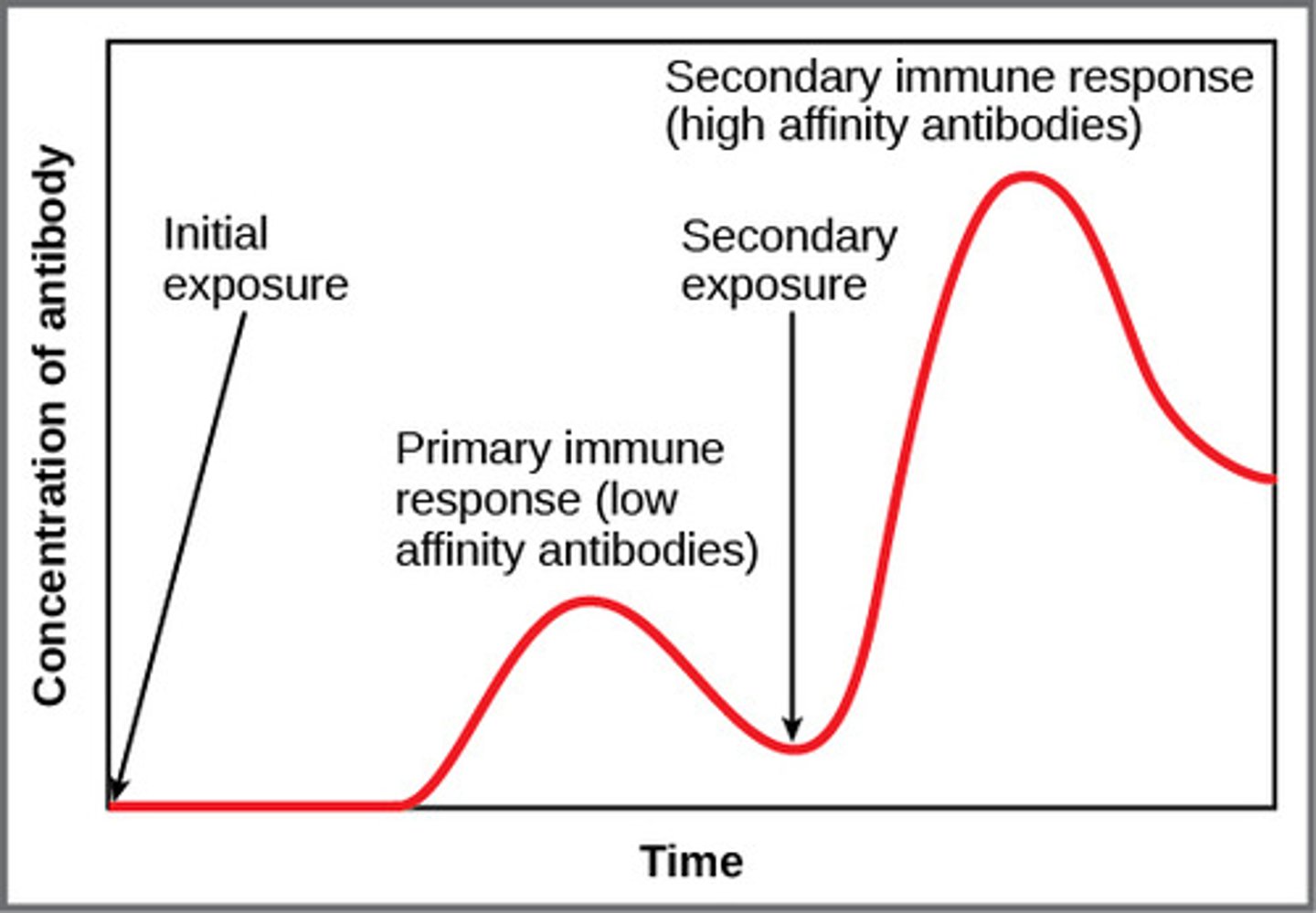
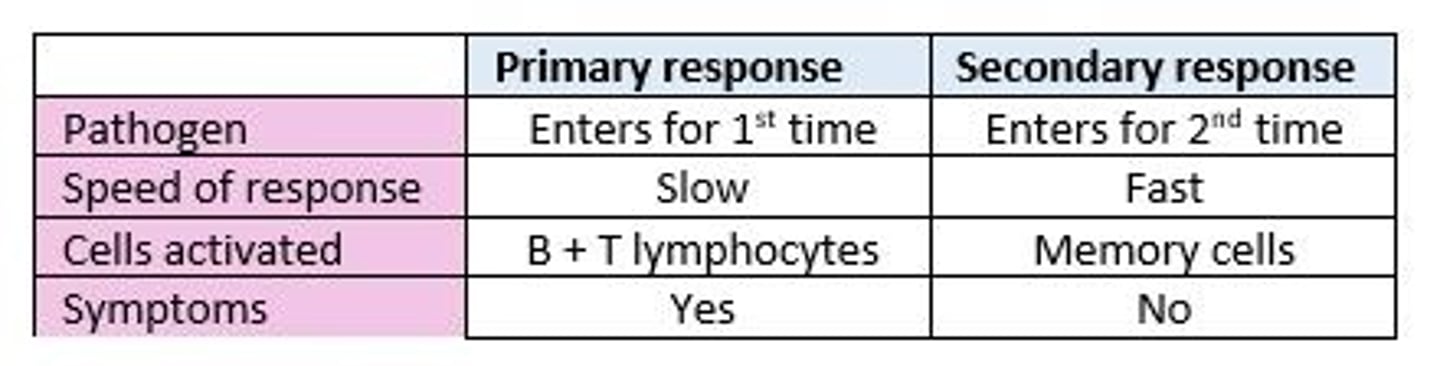
primary immune response
- pathogen enters body for first time, immune system activated.
- slow (aren't many B lymphocytes that can make the antibody needed to bind to pathogen), eventually enough produced to overcome infection.
- symptoms of disease will be shown.
- after exposure to antigen, T + B lymphocytes produce memory cells. (these memory cells remain in body for a long time).
- memory T lymphocytes remember specific antigen second time around.
- memory B lymphocytes record specific antibodies needed to bind to antigen.
- person is now immune.
Memory T lymphocytes
- remember specific antigen + recognise it a second time around.
Memory B lymphocytes
record specific antibodies needed to bind to the antigen.
secondary immune response
- immune system will produce a stronger, immune response.
- clonal selection happens faster, memory B lymphocytes divide into plasma cells that produce the right antibody to the antigen.
- memory T lymphocytes are activated + divide into correct type of T lymphocytes to kill cell carrying the antigen.
- usually gets rid of pathogen before you show symptoms.
Maintaining Immunity
- Memory B and T cells only have a limited lifespan
- Once all memory cells have died the person is no longer immune.
- Immunity is maintained by continually being exposed to the pathogen so we are continually making memory cells.
- e.g. in the same environment/booster vaccines.
Comparison on the primary and secondary immune response
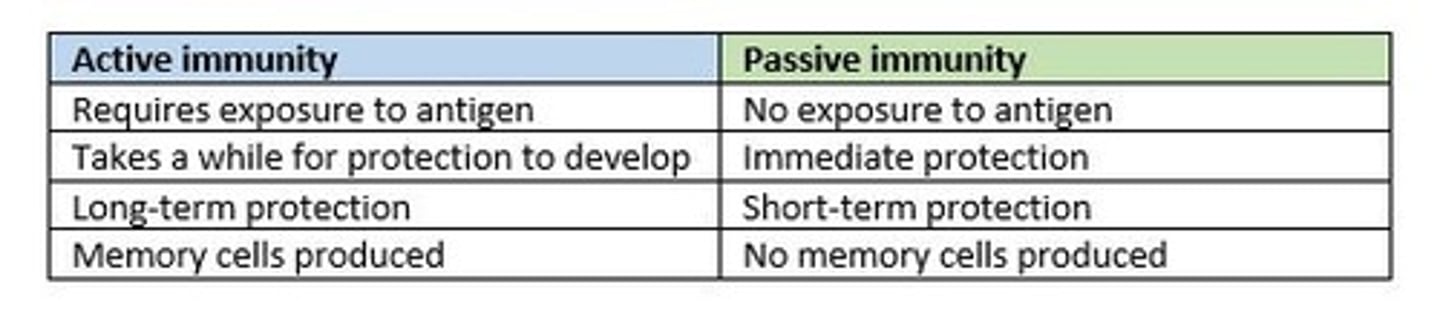
Two types of immunity
active and passive
active immunity
Immune system makes its own antibodies after being stimulated by an antigen...
Natural = immune after catching a disease.
Artificial = immune after you're given a vaccination containing a harmless dose of antigen.
passive immunity
Immunity you get from being given antibodies by a different organism (immune system doesn't produce antibodies of its own)...
Natural = baby becomes immune due to antibodies received from mother, through placenta + breast milk.
Artificial = injected with antibodies from someone else. e.g. if you contract tetanus you're injected with antibodies collected from blood donations.
comparison of the two types of immunity
autoimmune diseases
- immune system treats self-antigens as foreign antigens and launches an immune response against the organism's own tissues.
- usually chronic, can often be treated, not cured.
Examples of autoimmune diseases
- Lupus, immune system attacks cells in connective tissues. Causes + pain + inflammation. Can affect skin, joints, and organs like the heart + lungs.
- Rheumatoid arthritis, immune system attacks cells in the joints, causing pain + inflammation.
Purpose of vaccinations
- contain antigens, cause body to produce memory cells against particular pathogen without it causing disease (become immune w/o getting symptoms).
- these may be free or attached to a dead or attenuated (weakened) pathogen.
- injected or taken orally- disadvantage of oral = could be broken down by enzymes/too large to be absorbed into blood.
herd immunity
- if most people in population are vaccinated, disease becomes rare - people who haven't even been vaccinated unlikely to get disease (no one to catch it from).
- prevents epidemics.
Routine Vaccinations
- Offered to everybody
--> MMR = measles, mumps, rubella. Contains attenuated versions.
--> meningitis C vaccine = protects against bacteria that cause meningitis C.
Changing vaccines and vaccination programmes
- some pathogens can change their surface antigens ---> memory cells produced following a vaccination won't recognise the different antigens.
- primary immune response must be carried out.
- ...vaccine and vaccination programme may have to change regularly.
Example of changing vaccines and vaccination programmes
- influenza virus, changes every year, new strains of virus form regularly due to changing of antigens on surface of influenza virus.
- governments + health authorities create a vaccination programme using the most suitable vaccine for the next strain of virus.
antibiotics
- chemicals that kill/inhibit growth of bacteria.
- treat antibacterial infections.
- target bacterial cells without damaging human body cells.
- created by Alexander Fleming, 1928.
- death rate from infectious bacterial diseases decreased.
- risks: side effects, allergic reactions and antibiotic resistance.
Antiobiotic Resistance
- genetic mutations make some bacteria resistant to an antibiotic.
- bacteria is better able to survive + reproduce in host.
- leads to an allele for antibiotic resistance passed on to lots of offspring.
- example of natural selection.
Problems with antibiotic resistance
- superbugs more common (resistant to most common antibiotics).
- less able to treat potentially life-threatening bacterial infections.
Examples of antibiotic-resistant bacteria
- MRSA, causes serious wound infections.
- C. difficile, infects digestive system, antibiotics kill other bacteria in digestive system --> allowing it to flourish. Produces a toxin causing diarrhea, fever, cramps.
Preventing antibiotic resistance
- Reducing the use of antibiotics for minor infections or to prevent infection.
- Patients taking the full course of antibiotics to ensure all bacteria are dead to prevent the creation of a population of antibiotic resistant bacteria.
Sources of medicines
- many manufactured using natural compounds found in plants, animals or microorganisms.
- e.g. penicillin-fungus, cancer drugs-soil bacteria, Alzheimer's disease drug-daffodils.
- only a small amount have been investigated so far. Possible sources need to be protected by maintaining biodiversity on Earth.
future of medicine
- personalised medicine = genes determine how your body responds to certain drugs (certain drugs more effective for some people than others).
- synthetic biology = using technology to design and make artificial proteins, cells + even microorganisms. (e.g. bacteria engineered to destroy cancer cells, leaving healthy cells intact).
Define biodiversity
The variety of living organisms in an area
What are the 3 levels of biodiversity?
habitat diversity, species diversity and genetic diversity
Define habitat diversity
The number of different habitats in an area
Define habitat
- habitat = area inhabited by a species.
- habitat includes: physical factors such as soil, temp. range and living factors, like availability of food, presence of predators.
Define species diversity
- number of different species (species richness) and the abundance of each species (species evenness) in an area.
- species = group of similar organisms able to reproduce to give fertile offspring.
Define genetic diversity
- the variation of alleles within a species/population of species.
- e.g. human blood type determined by alleles.
How is data on biodiversity collected?
- number of different species in a habitat found out/number of individuals in each species.
- sample of population taken (reduces time consumption) + estimates about whole habitat taken from sample.
Describe random sampling
- makes sure sample isn't biased.
- random number generator to pick coordinates along a tape.
- each sample site has same probability of being chosen.
What are the 3 types of non-random sampling?
- systematic
- opportunistic
- stratified.
When would non-random sampling be used?
- when there's a lot of variety in the distribution of species in the habitat and you want to make sure all areas are sampled / all different species are sampled.
Describe systematic sampling
- samples are taken at fixed intervals, often along a line.
Describe opportunistic sampling
- samples are chosen by the investigator.
- simple to carry out
- data will be biased.
Describe stratified sampling
- different areas in a habitat are identified and sampled separately in proportion to their part f the habitat as a whole.
Species richness and how it's measured
- number of different species in an area.
- high the number = greater the species richness.
- measured by taking random samples of a habitat and counting the number of different species.
Species evenness and how it's measured
- measure of the relative abundance of each species in an area.
- more similar the pop. size of each species = greater the species evenness.
- measured by taking random samples of a habitat and counting no. of individuals of each different species.
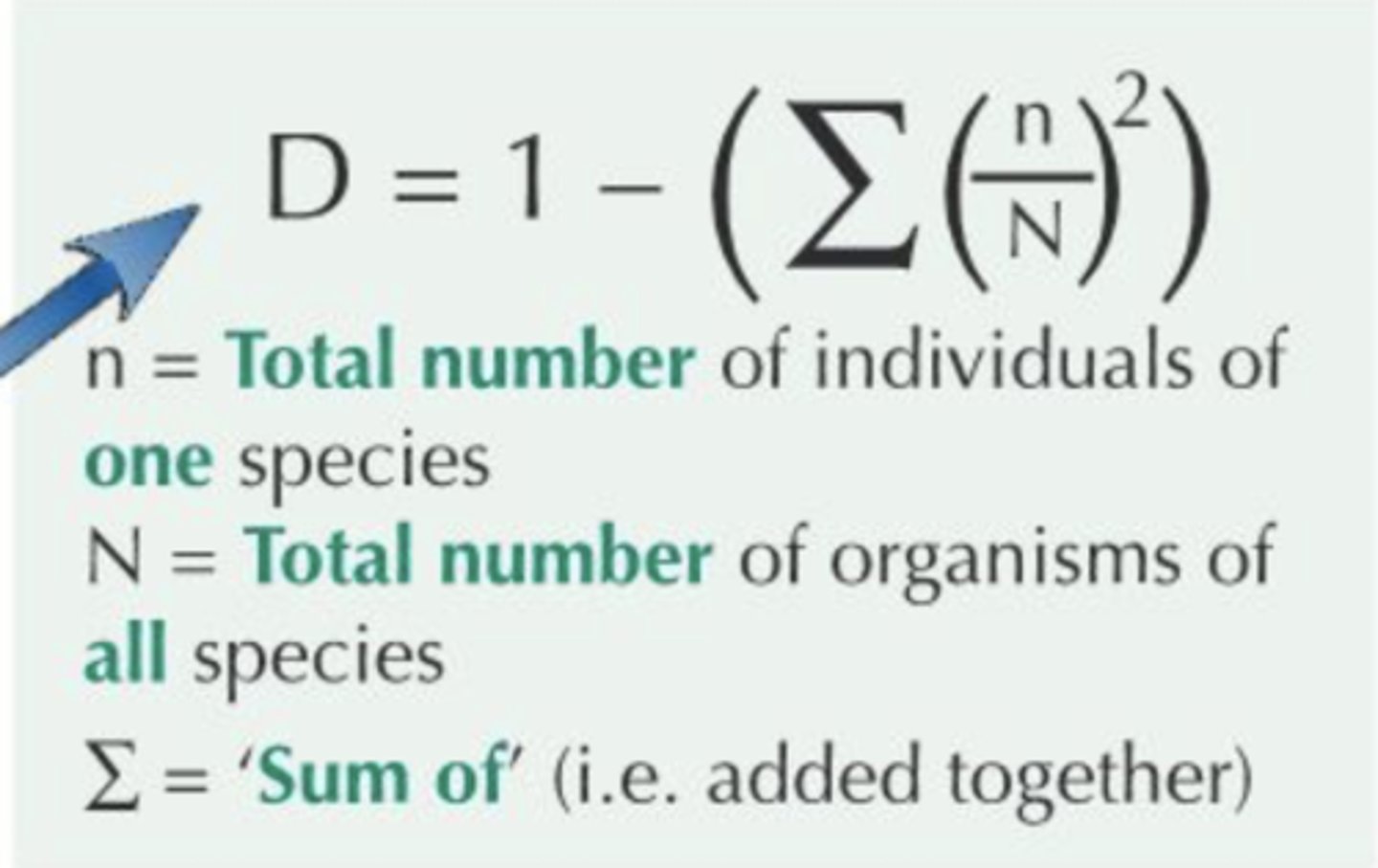
Simpson's Index of Diversity
- measures species diversity.
- always a value between 0 and 1.
- closer index is to 1, more diverse the habitat and greater its ability to adapt to change.
- greater the species richness/evenness = higher the value of Simpson's Index.
Importance of genetic diversity
- Diverse gene pool gives a population more flexibility to survive in a changing environment
- The more genetically diverse a population, the more ways it has to adapt
What is polymorphism?
- describes a locus that has two or more alleles.
--> alleles of the same gene are found at the same point (locus) on a chromosome.