Allograft Rejection of Organ Transplants
1/22
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
23 Terms
What is tissue typing?
Testing for matches between donor and recipient HLA to reduce risk of rejection.
Perfect matches are rare.
What does allograft rejection involve?
Adaptive immune response (memory response) to alloantigens on donor allograft
Alloreactive T cells recognise donor HLA molecules (via direct and indirect presentation
High numbers of alloreactive T cells (haven’t been negatively selected because we don’t have HLA from host so wouldn’t have been exposed during T cell development/selection)
What is the role of memory cells in allogeneic graft rejection?
Memory cells from previous infections cross-react with allogenic MHC molecules (so strong and rapid response can happen without prior exposure to donor tissue)
A T cell that once fought a virus
Sees the donor’s MHC
And thinks: “This looks foreign and dangerous”
→ Activates immediately
What is the role of dendritic cells in T cell recognition of alloantigens?
Donor DCs (“passenger” leukocytes) express high levels of MHC I and MHC II molecules which are recognised by T cells and activate CD4+/CD8+ T cells
DCs also exhibit “cross-presentation” where endogenous Ag peptides can be expressed on HLA Class I molecules
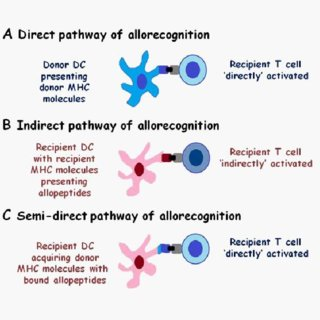
What are the three methods of alloantigen presentation in T cell recognition?
Direct presentation
Indirect presentation
Semi-direct presentation
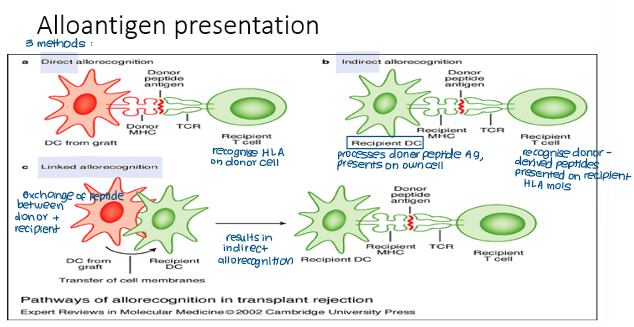
What is direct allorecognition?
Recipient T cells recognise intact HLA molecules alone and/or peptide:MHC complexes on donor DCs
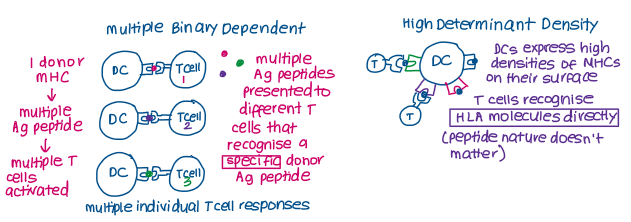
What are the two models of direct allorecognition that explain the high frequency of T-cell responses in direct allorecognition?
Multiple binary determinant model
High determinant density model
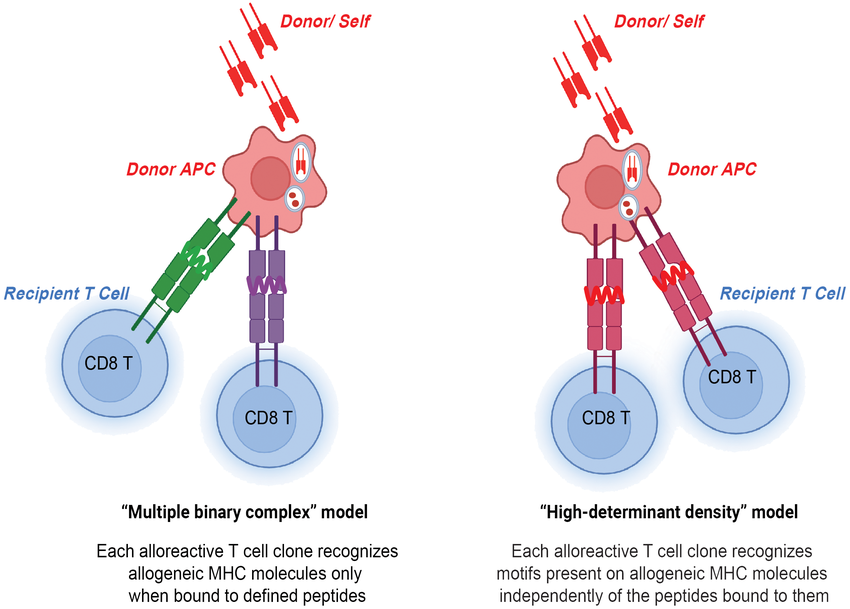
Multiple binary determinant model
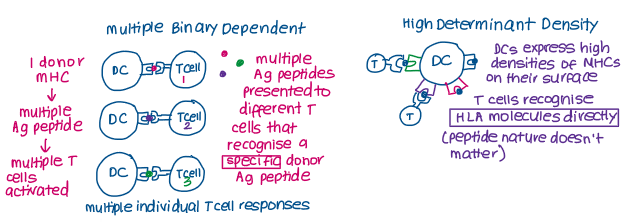
High determinant density model
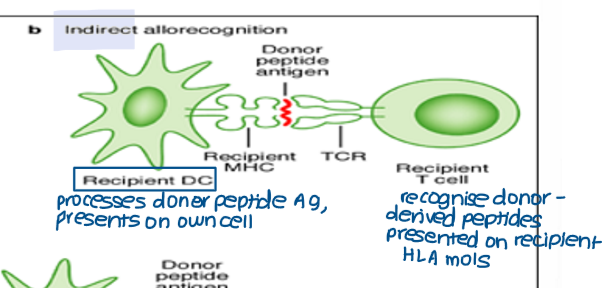
What is indirect allorecognition and how does it happen?
Recipient T cells recognise donor-derived peptides presented on recipient HLA molecules.
Recipient DCs migrate into graft and acquire donor peptides (HLA)
Recipient DCs process donor HLA molecules
Alloreactive T cells recognise processed donor HLA molecules presented on recipient DCs
What is semi-direct (linked) allorecognition and how does it happen?
Involves direct transfer of HLA molecules between donor and recipient DCs
Recipient APCs (DCs) capture intact donor MHC-peptide complexes, often via extracellular vesicles (like DC exosomes)
Recipient DCs present intact donor MHC molecules on their own surface.
Alloreactive T cells recognize these donor MHC molecules (along with their bound peptides) presented by the recipient's APCs, leading to activation and graft rejection.

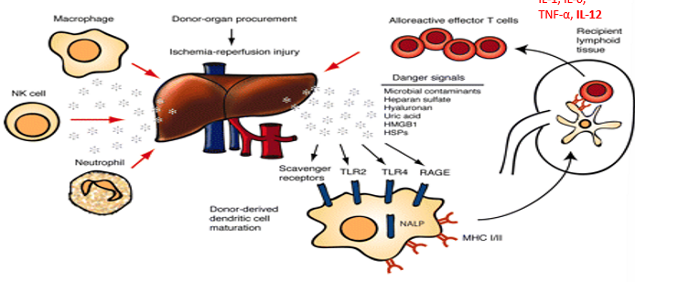
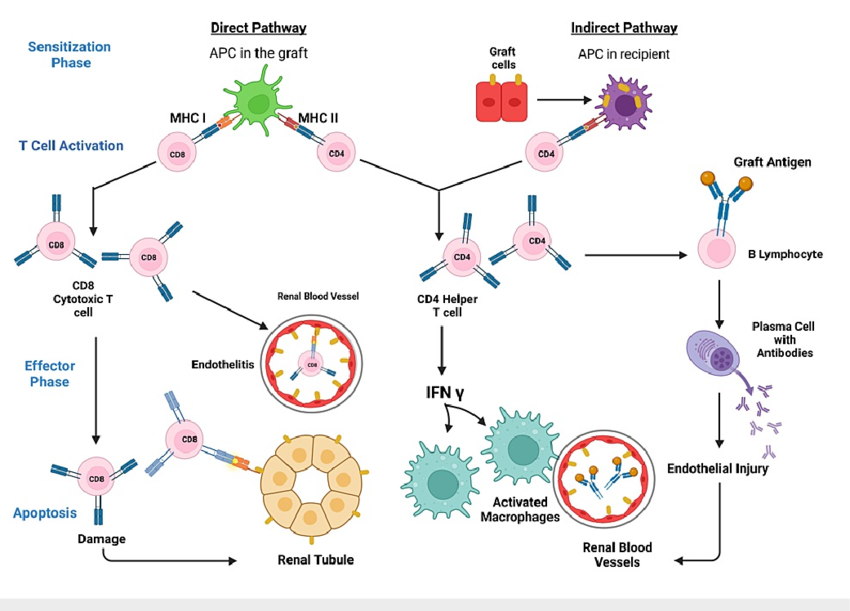
The immune response (rejection) to alloantigens occurs in two main phases:
Sensitisation phase
Effector phase
What happens in the sensitisation phase?
Donor DCs (“passenger” leukocytes) migrate into recipient lymph nodes
Alloantigen presentation to T cells via direct, indirect and semi-direct/linked allorecognition
Alloreactive T cells are primed and activated
Clonal expansion of T cells (CD4+/CD8+/alloreactive memory cells)
Donor DCs initiate inflammatory response (secrete pro-inflammatory cytokines like IL1, IL-6, IL-12, TNF-a which recruit other immune cells and cause inflammation)
The effector phase is driven by which cells?
CD4+ T helper cells
What happens in the effector phase?
CD4+ T helper cells release cytokines (IL-2, IFN-γ, TNF) to increase immune activity and HLA expression
CD8⁺ cytotoxic T cells destroy donor cells presenting the alloantigen (HLA Class I molecules).
Alloreactive B cells produce alloantibodies to bind donor antigens in response to IFN-γ(humoral response: complement-mediated lysis or opsonisation)
What are the three mechanisms of organ rejection and how long after transplantation do they occur?
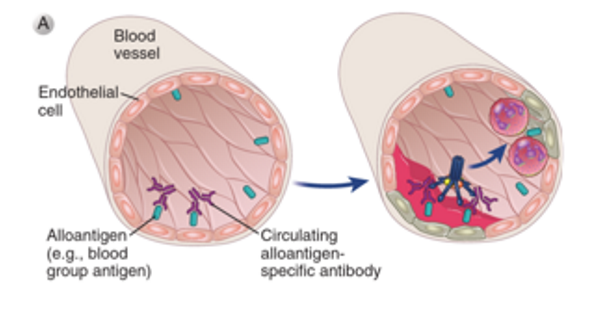
Hyperacute rejection (within hours)
Acute rejection (first few weeks)
Chronic rejection (years)
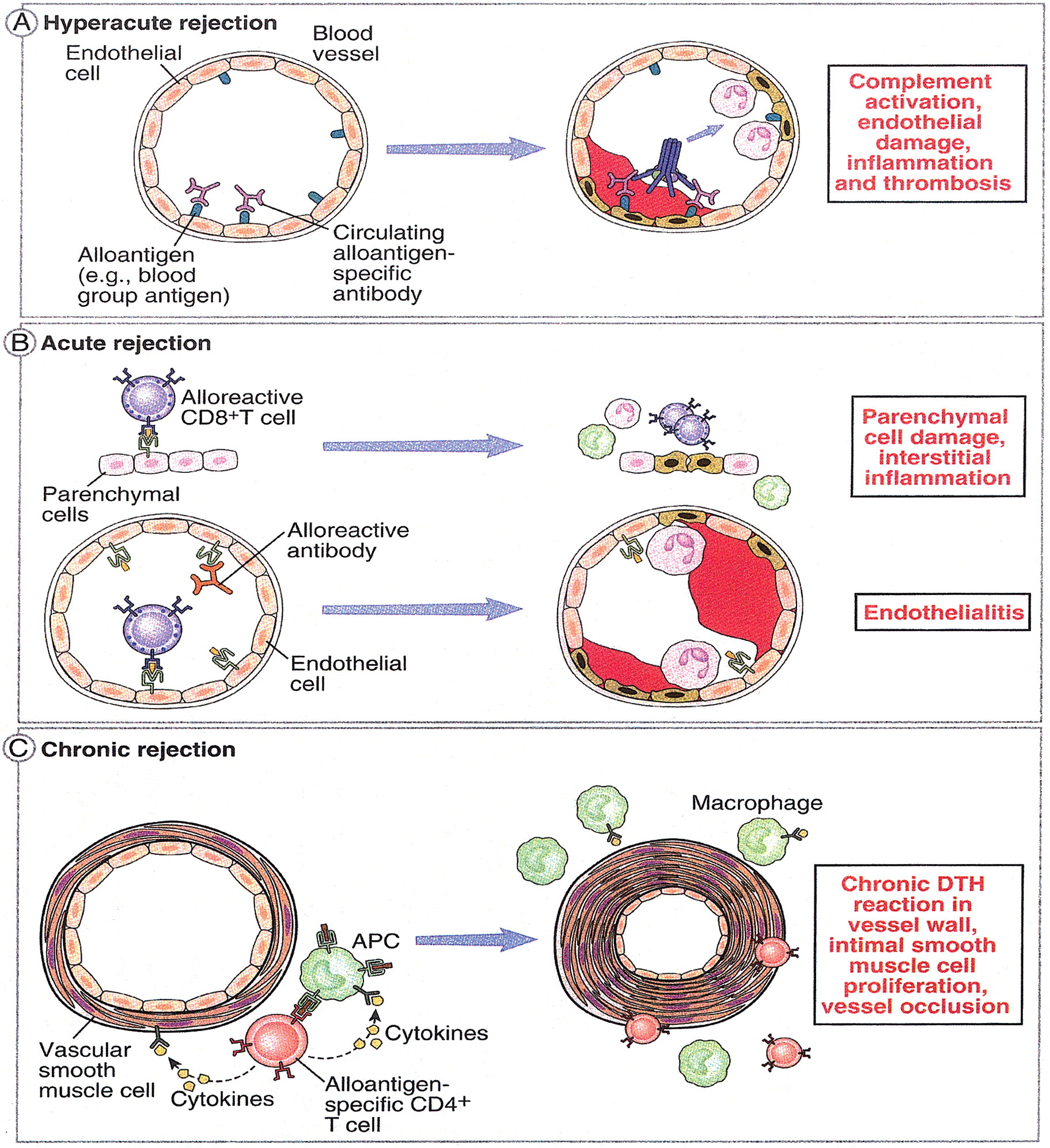
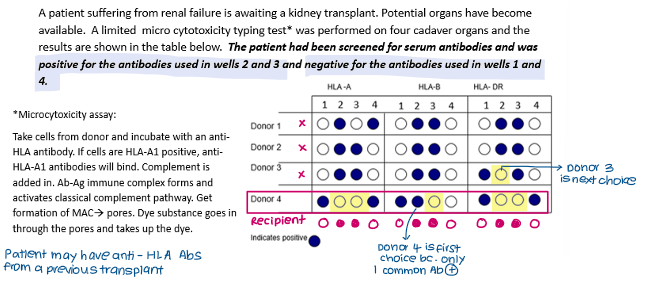
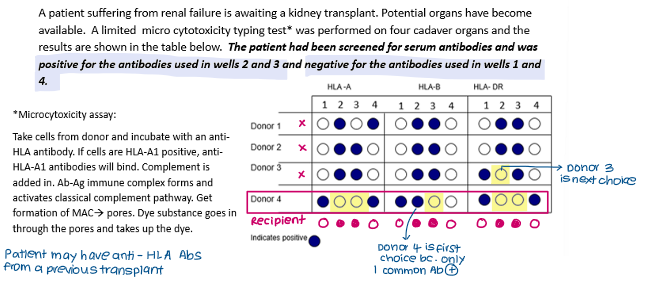
How does hyperacute rejection occur?
Due to pre-existing antibodies to donor antigens (e.g. HLA, blood group antigens)→ second-set rejection
Pre-existing recipient antibodies bind to donor endothelial cells → complement activation and ADCC → vascular damage, thrombosis.
How does acute rejection occur?
Primary response following sensitisation phase
Cell-mediated immunity (CD8⁺ cytotoxic T cells) and/or humoral immunity (newly formed alloantibodies).
Alloreactive CD8+ cells destroy donor APCs displaying Class I molecules
Antibody-mediated rejection of donor cells-endothelial cells major target
Amplified by alloreactive CD4+ T helper cells
Interstitial infiltration by lymphocytes
Endothelial swelling
How does chronic rejection occur?
Slow, ongoing immune response; both cell- and antibody-mediated mechanisms contribute.
Recipient DCs mediate slow rejection process.
Vascular changes: Intimal thickening → ischemia
Fibrosis in graft tissue
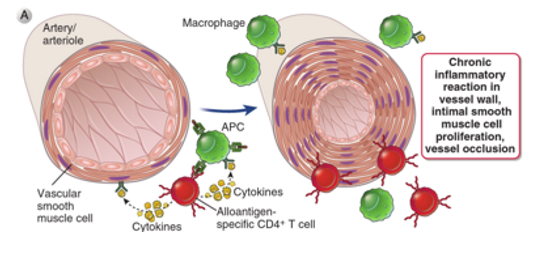
Which type of rejection typically involves indirect allorecognition?
chronic
Which type of rejection typically involves direct allorecognition?
acute
Which type of allograft is always tolerated?
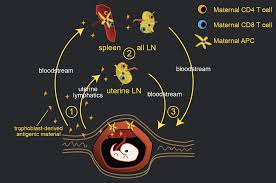
Fetus- carries paternal MHC and MnAgs different to the mother but is not rejected.
“fetomaternal tolerance”