Block 1B - H+N Cancers (HPC, Salivary Gland, Oral Cavity)
1/174
Earn XP
Description and Tags
ONCOL 310 - Clinical Oncology II. University of Alberta
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
175 Terms
What vertebral levels is the hypopharynx located
between C3-C6 (oropharynx → esophageal inlet)
what is the superior, inferior, anterior, posterior, and lateral borders of the hypopharynx
superior = hyoid bone
inferior = upper esophageal sphincter or inf. cricoid cartilage
anterior = larynx
posterior = retropharyngeal space (prevertebral fascia)
lateral = piriform sinus
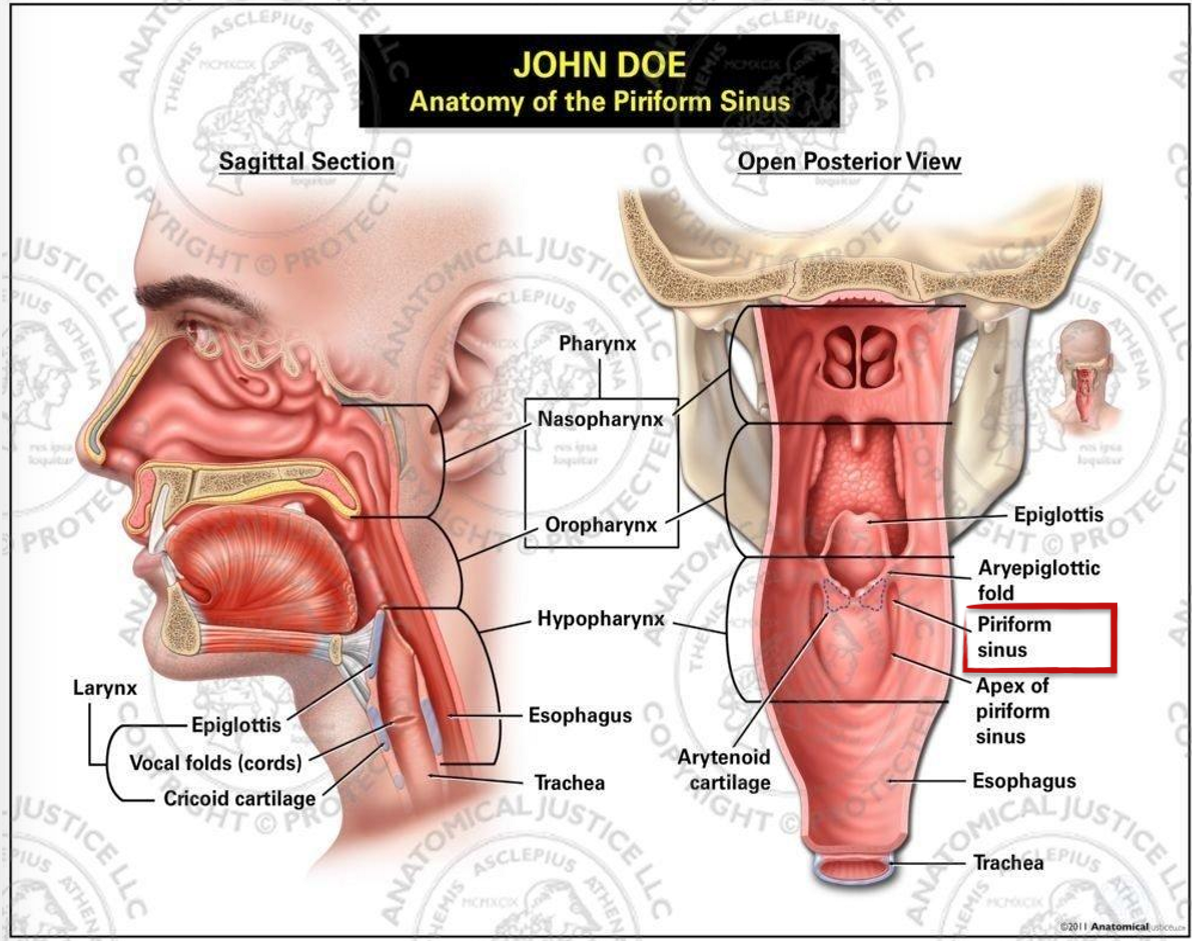
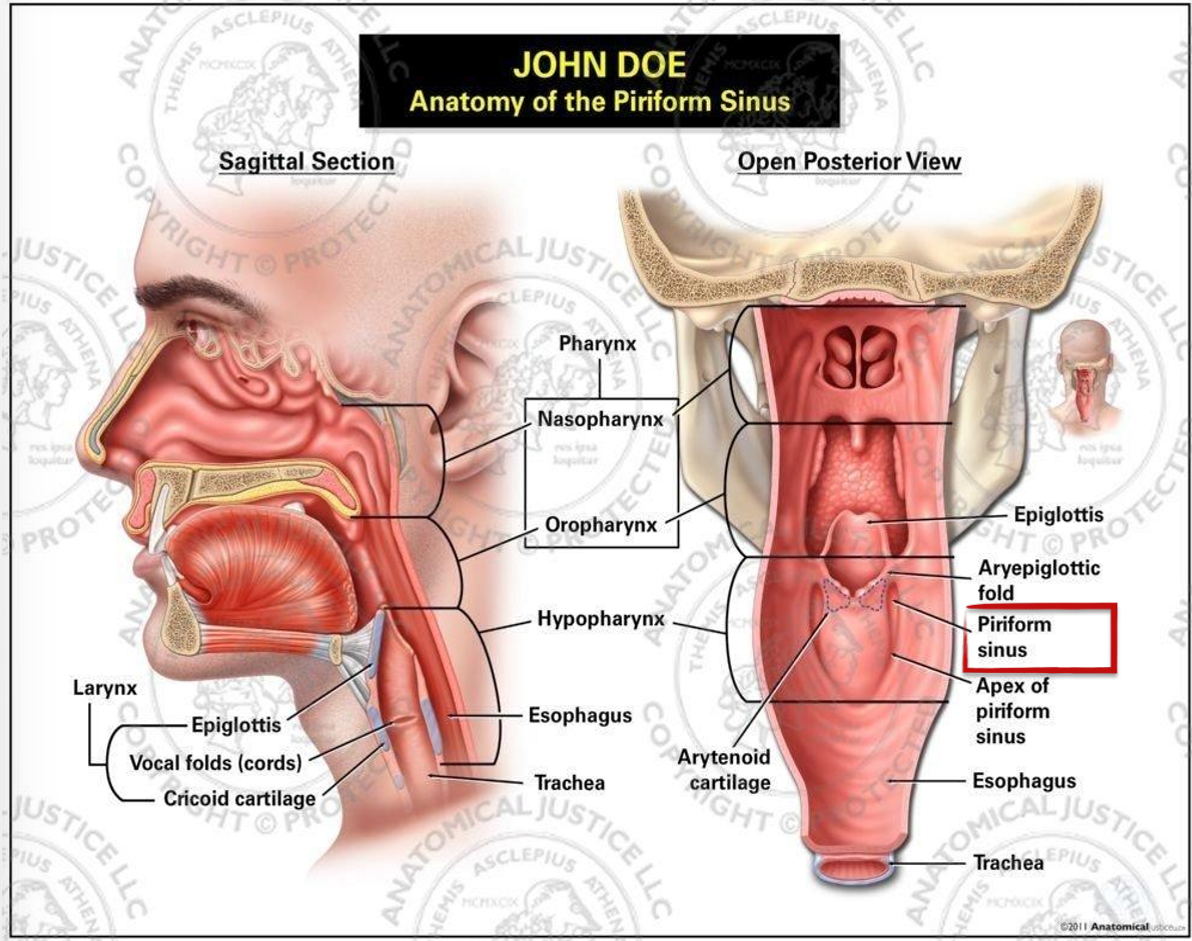
what are the three anatomical regions of the hypopharynx?
posterior pharyngeal wall
pirifrom sinus
postcricoid
what two cranial nerves are located in the hypopharynx
CN IX (glossopharyngeal)
CN X (vagus)
Hypopharynx Carcinoma (HPC) epidemiology
how many cases in canada
M:F
age range
165 cases in canada (only make up 7% of all H+N cancers)
M:F = 3:1
Age range: 55-70 years
5 etiological factors of HPC
excessive alcohol consumption + smoking
upper HPC
iron + Vit C deficiencies
lower (post cricoid) HPC
previous RT
Plummer-Vinson syndrome
long-term iron def.
HPV (unclear)
describe the natural history of HPC
HPC arises from the epithelial layer of the mucous membrane. they are aggressive and often have early metastasis (most pts have cervical LN presentation and 50% have a neck mass)
what percent of patients with HPC present with distant mets? and what percent of patients with HPC have synchronous second primary tumors
33%
distant mets more common on HPC than any other H+N cancer
4-15% present with second primary tumors
why is HPC often asymptomatic
because there are many recesses and spaces in the larynx
clinical presentation of HPC
dysphagia, odynophagia, globus sensation, otalgia, neck mass, weight loss
how can large HPC tumors present
airway obstruction, hoarseness, or aspiration
describe the physical exam to assist in diagnosing HPC
palpation, direct or indirect laryngoscopy, fiberoptic endoscopy, CN function
what blood work can be done to diagnose HPC
CBC, liver function tests, blood chemistry
what is the main imaging modality to diagnose HPC
contrast enhanced CT and MRI to determine the extent of the primary tumor
CXR may also be used to evaluate lung involvement
what would be the purpose of using an FDG-PET or PET-CT to diagnose HPC
FDG-PET is used to diagnose occult, residual, and recurrent tumors
PET-CT is used for high specificity post treatment
what are the three main prognostic indicators of HPC
size of primary tumor
extent of local spread of primary
extent of involvement of regional LNs (mets)
what hypopharynx region has the highest incidence of HPC, what area has the lowest?
highest: piriform sinus
lowest: post-cricoid
what are three reasons why HPC has the lowest survival rate of H+N cancers
poorly differentiated and asymptomatic presentation = advanced disease
emergence of secondary primary
development of distant mets
what are the three routes of spread of HPC
local spread
to subsites of hypopharynx, larynx, and cartilage
lymphatic spread
hematogenous spread
what is the most common hematogenous metastatic site of HPC
lung
what is HPC’s mechanism of skip metastasis
the tumor can spread within mucosa beneath the epithelium and it will resurface at various locations
describe the 2 paths of lymphatic spread of HPC from the piriform sinus to the supraclav nodes
jugulodigastric → middle deep cervical chain or jugulo-omohyoid or paratracheal → lower deep cervical → supraclavicular
retropharyngeal → superior deep cervical →jugulodiagastric → middle deep cervical —> posterior cervical chain —> supra clav
describe the path of lymphatic spread of HPC from the posterior pharyngeal wall to the supraclav nodes
retropharyngeal → superior deep cervical →jugulodiagastric → middle deep cervical —> posterior cervical chain —> supra clav
what percent of HPC tumors are squamous cell carcinoma
95% of tumors
what percent of HPC are keratinizing? non-keratinizing?
60% keratinizing
33% non-keratinizing
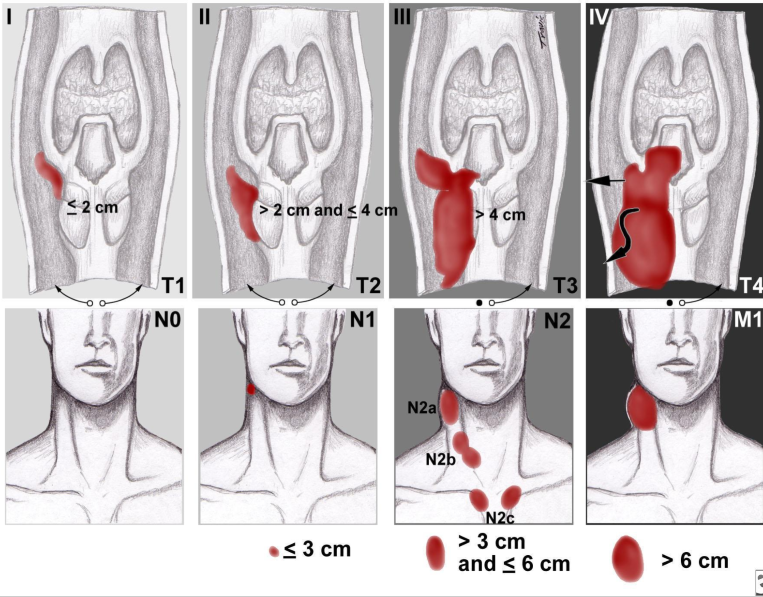
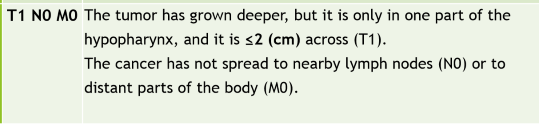
Stage I HPC
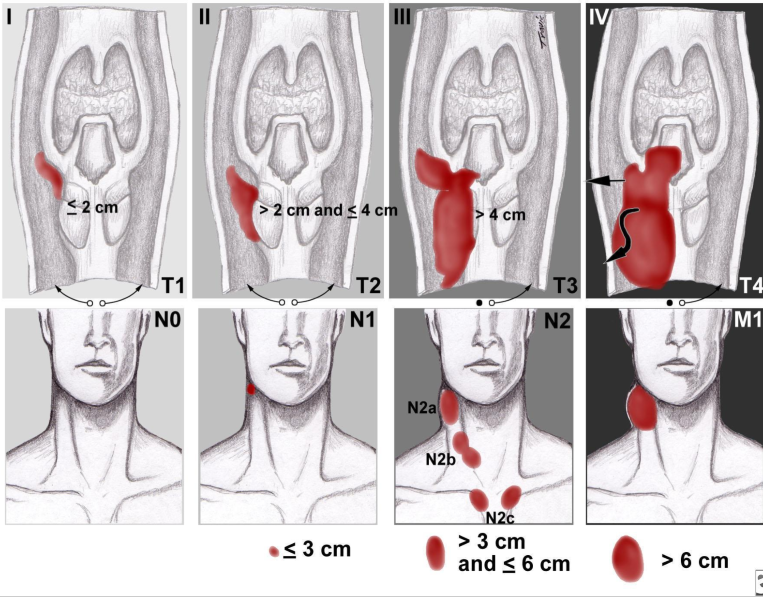
Stage II HPC
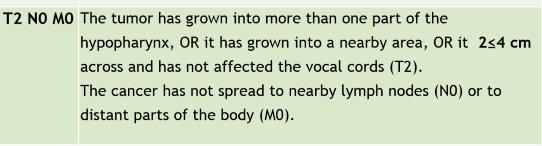
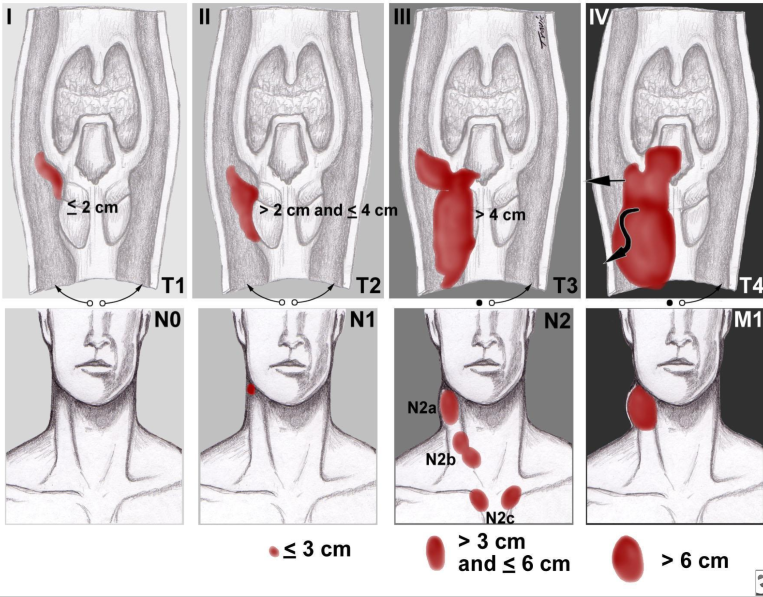
Stage III HPC
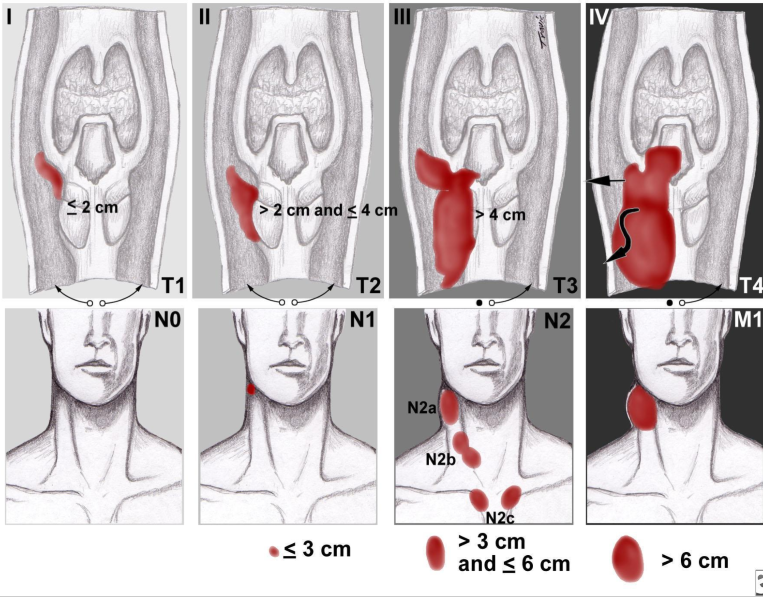
Stage IV HPC

What three surgeries can be used stage I HPC
partialy laryngectomy or pharyngectomy
total laryngectomy
laryngopharyngectomy
includes larynx, vocal cord and pharynx
typically used for T3 or T4 disease
what is the primary treatment for stage I and II HPC
ChemoRT with cisplatin
to spare larynx and maintain speech
may also irradiate cervical lymph nodes
when would RT be used alone in early stage HPC
if patient has comorbidities or early piriform sinus lesions
when would PORT be used for early stage HPC
if there is a high risk of recurrence
What are are two primary treatments for Stage I LN involved HPC
primary: RT bilateralal neck to include lateral cervical and retropharyngeal LN
also can do laryngopharyngectomy + neck dissection (loss of speech occurs)
what are the two primary treatments for Stage II HPC
surgery + PORT
RT bilateral neck (like stage I) with neoadjuvent chemotherapy
what are the two mainstay treatments of early stage HPC
surgery + RT are mainstays
chemotherapy used more so for advanced disease
each treatment plan is individualized
what is the main treatment of stage III HPC
Surgery + PORT (3-4 weeks after resection)
surgical reconstructions need to be completed
what three types of surgical reconstructions can be done
free flap transfer
free jejunal autograft
pec major myocutaenous flap
what neoadjuvent/adjuvent combined chemo can be used for stage III HPC
cisplatin + 5FU
what is the main treatment for stage IV resectable HPC
Laryngopharyngectomy + adjuvent chemoRT
or surgery ± adjuvent RT
what is the main treatment for Stage IV unresectable HPC
chemoRT with cisplatin or cetuximab (targeted therapy)
what potential treatment options can be used for recurrent HPC
surgery (if RT fails), chemotherapy (for mets), immunotherapy, salvage surgery
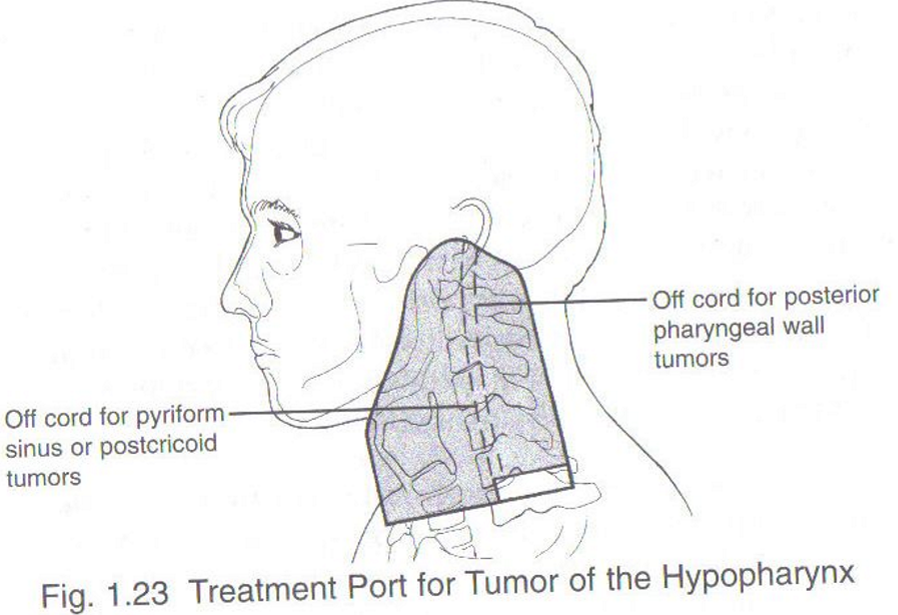
what is the superior, inferior, anterior, and posterior borders for HPC radiation
sup: inf border of mandible and mastoid process to base of skull
inf: inf of cricoid cartilage to encompass extent of tumor + 1.5-2.0 cm
ant: anterior to thyroid cartilage with a margin around tumor extension
post: post to the spinous processes with a margin around all nodal disease
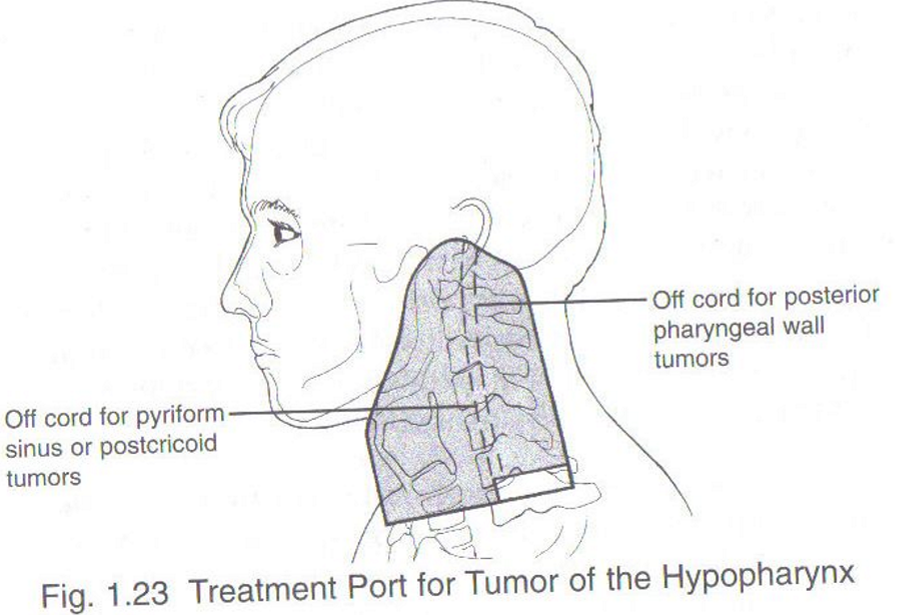
how many phases did conventional RT treatment to HPC have
2 or three phases
this is required to irradiatie the tumor and nodes to a radical dose while keeping spinal cord dose within tolerance
what should the fields cover in conventional HPC RT
should cover from the skull base to the cricoid cartilage with an anterior split neck field to treat LN below cricoid
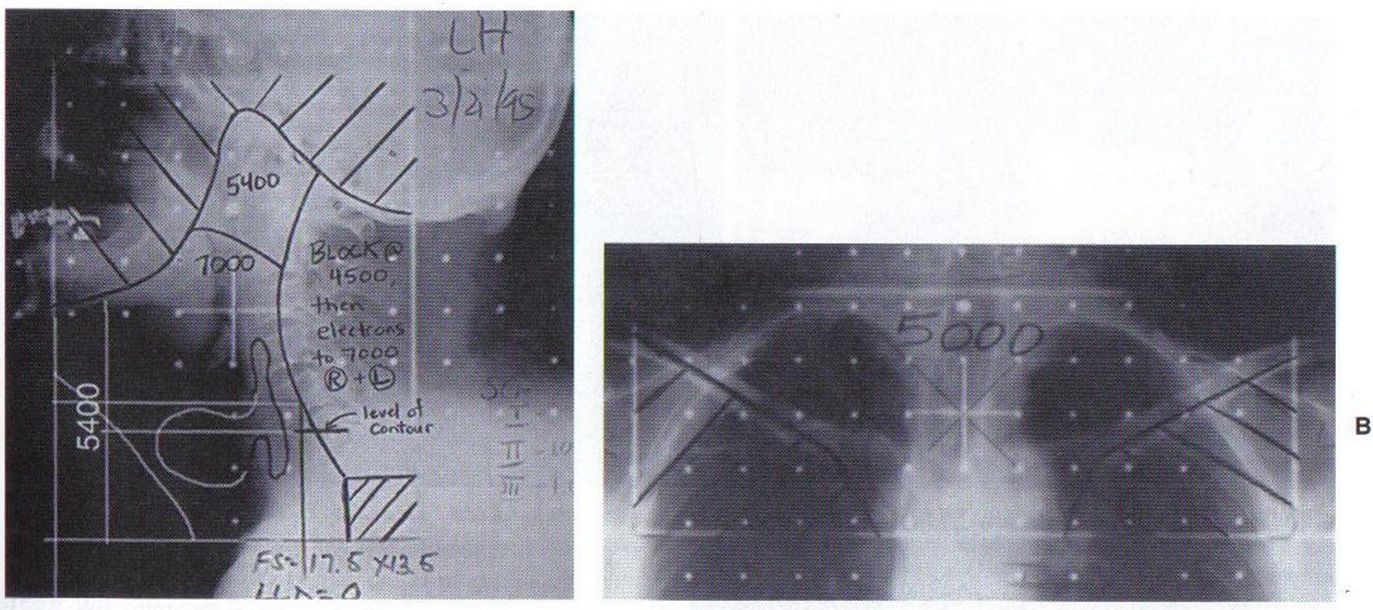
after what dose should the fields be reduced posteriorly to avoid the spinal cord? what can be used to treat the level V nodes instead?
after 44-45 Gy
use electrons to treat these nodes instead
Modern HPC RT treatment
energy
technique
D/F for high risk
D/F for intermediate risk
D/F for low risk
6 MV IMRT or VMAT
70 Gy / 33 f to high risk CTV
59.4 Gy / 33 f to intermediate risk
50-54 Gy / 33 for elective risk
describe the set-up for modern HPC RT treatment
AIO board with a 5 point shell, neutral head rest, arms by sides, knee and ankle rest
what D/F is used for Piriform Sinus HPC definitive RT ? what about for surgery + PORT
Definitive: 66-70 F / 30-33 fractions
PORT: 60/30 fractions
what D/F is used for pharyngeal wall definitive HPC RT? what about for surgery + PORT?
Definitive: 66-70 F / 30-33 fractions
PORT: 60/30 fractions
same as for piriform sinus
acute side effects of HPC RT
erythema, dry and moist desquamation, xerostomai, mucositis, dysphagia, infection, cavities
chronic side effects of HPC RT
telangietasia, hypo/hyperpigmentation, fibrosis xerostomia, trismus, osteonecrosis, hypothyroidism
what is the new standard care for recurrent or metastatic H&N SCC?
immunotherapy
first line therapies for H+N cancers should now include immunotherapy with pembrolizumab
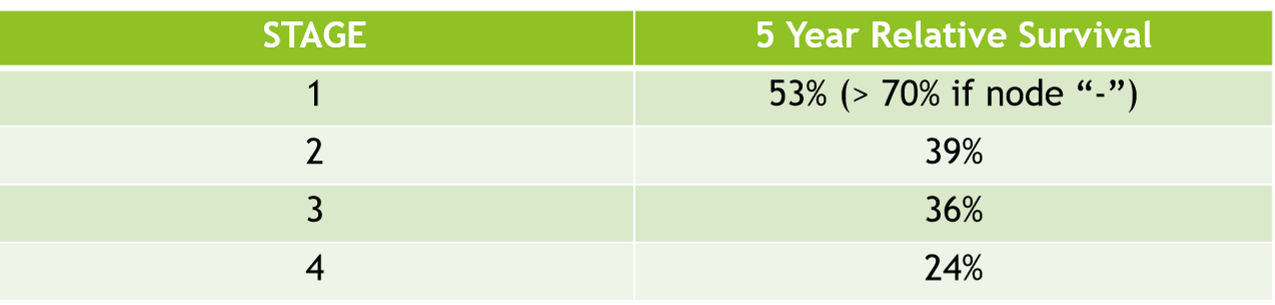
what is the 5 year overal survival of HPC
25-40%
poorest survival rate of all H+N cancers
what are the three major salivary glands?
sublingual, submandibular, and parotid gland
there are also minor salivary glands beneath the mucosa of the buccal cavity
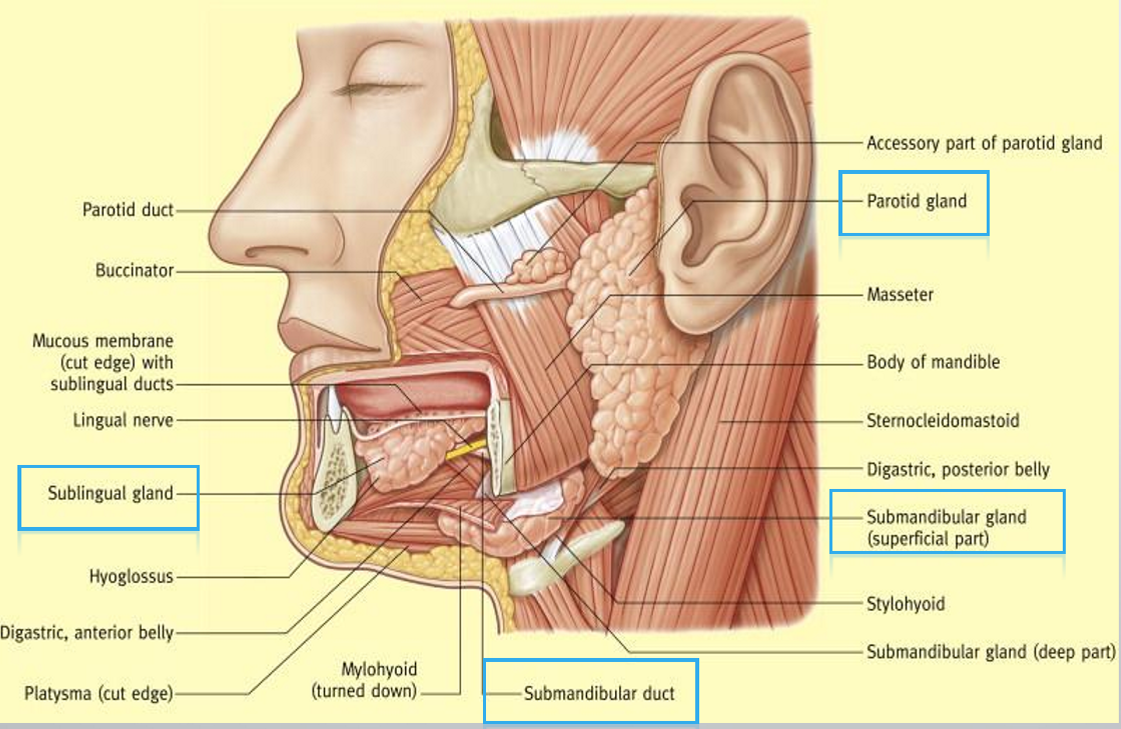
what are the 4 main ducts connected to the salivary glands
Stensen’s duct, wharton’s duct, Bartholin’s Duct, and Duct of Rivinus
what three cranial nerves are relevant for treating the salivary glands
CN III: oculomotor
CN V: trigeminal
CN VII: facial nerve
what arteries supply blood to the major salivary glands
maxillary, transverse facial, lingual, and facial arteries
branches of the external carotid artery
Salivary gland cancer epidemiology
what percent are benign
where do 80% of tumors originate
how rare are these cancers?
M:F
typical age range
65% benign
originate in the parotid gland
very rare: only make up 0.5% of all malignancies
M:F = 1.1:1.6!!!
> 50 years
what percent of _____ are malignant
parotid gland
submandibular gland
sublingual gland
Parotid = 20-25%
submandibular = 35-40%
sublingual gland = > 90%
Although the etiology of salivary gland cancers is mostly unknown, what are three potential etiological factors?
Radiation to the head and neck
HIV infection —> lymphoma
skin cancer spreading to salivary gland lymph nodes
describe the natural history of salivary gland cancers
the tumor starts as an asymptomatic malignant mass lasting on average 3-6 months before it begins to spread via local invasion to skin or cranial nerves
high grade tumors can have up to 44% cervical LN involvement
what are the most common sites of mets for salivary gland tumors and what is is the route of spread?
lungs and bone are most common, and sometimes liver
travels hematogenously
what is the typical clinical presentation of salivary gland cancers?
typically is a painless non-ulcerative mass in front of ear or in neck
facial nerve paralysis, pain, ulceration, dysphagia, and difficulty articulating speech may occur as well
what is the most cost effective and readily available imaging modality for diagnosis of salivary gland tumors?
ultrasound
can also due an aspiration along side the U/S
what 3 other imaging modalities can be used to diagnose salivary gland tumors
CT with contrast
Contrast enhanced MRI for soft tissue and neural involvement
PET-CT for high grade tumors, locoregional recurrence and metastatic disease
what type of biopsy is typically used to diagnose salivary gland tumors
FNAB
what are some favourable prognostic indicators of salivary gland cancers
tumor is in major salivary gland (parotid or submandibular)
small size, low grade, negative margins, node negative
most early stage low grade tumors are curably be adequate surgical resection alone
what makes salivary gland cancers interesting pathologically
they are the most heterogenous group of tumors in any tissue of the body
what is the most common histology for salivary gland tumors
mucoepidermoid carcinoma
most in parotid gland, 35% of malignant salivary gland tumors

what is the most common histology for salivary gland tumors in minor salivary glands
adenoid cystic cancer
what are some other examples of histological subtypes of salivary gland cancer
adenocarcinomas, hemangiomas, lipoma, sarcomas, lymphomas
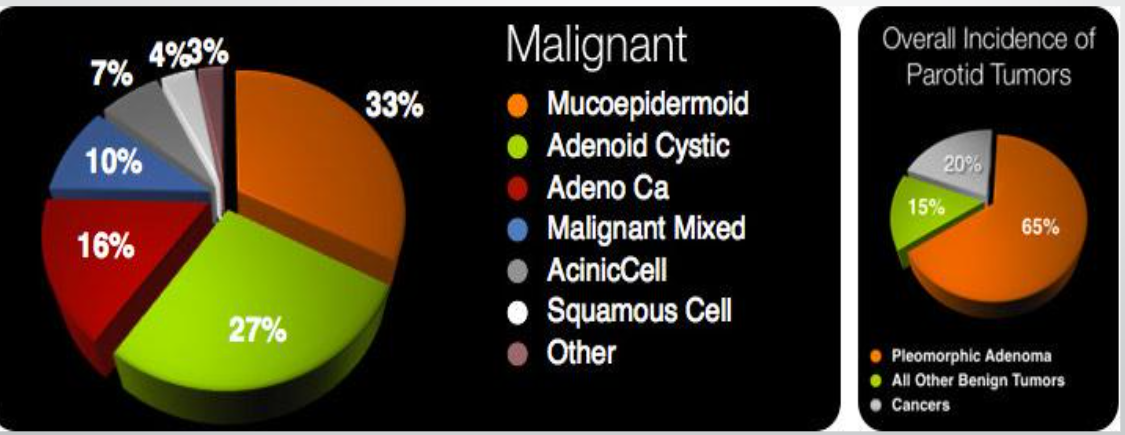
what is the most common benign tumor subtype of parotid gland cancers
pleomorphic adenoma
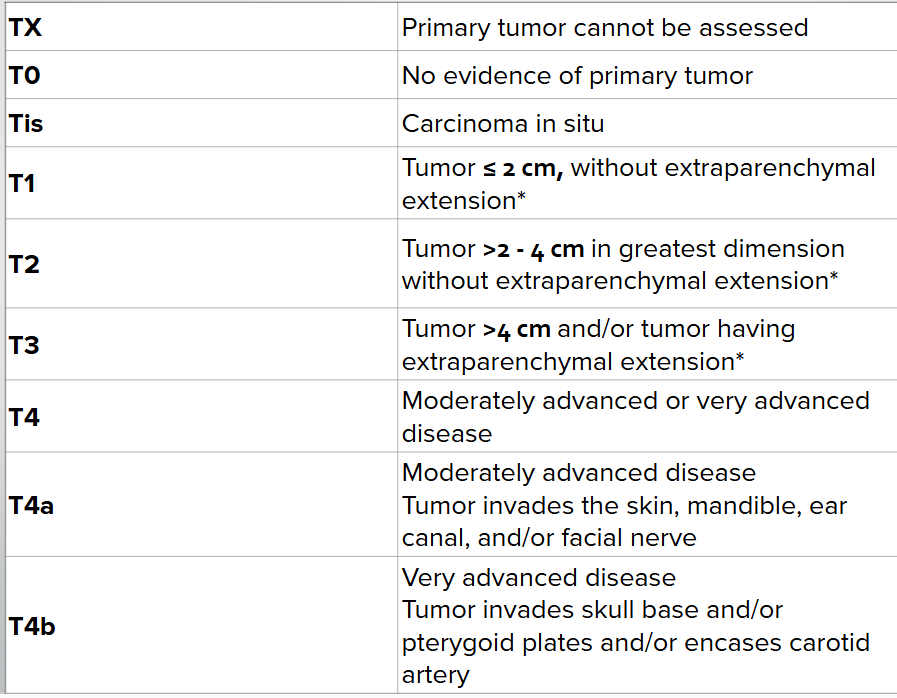
Salivary Gland TNM Staging - T
as T increases, so does the size of tumor and the extent of invasion
extraparenchymal extension = evidence of invasion of soft tissues or nerve
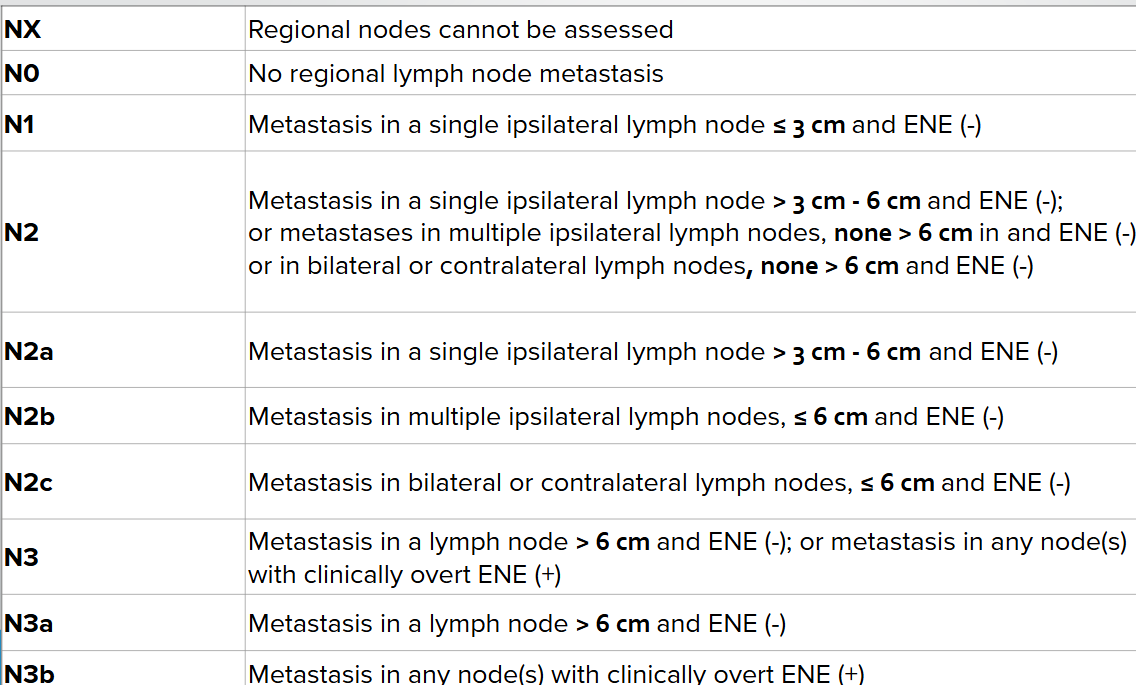
Salivary Gland TNM Staging - N
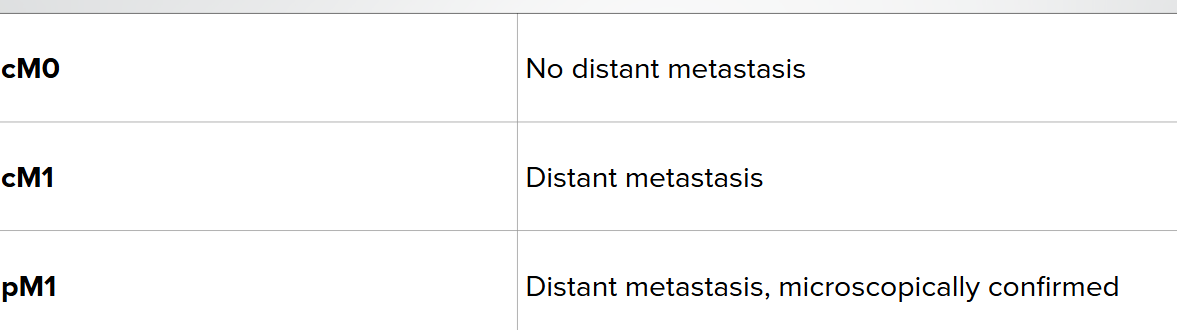
Salivary Gland TNM Staging - M
what are the three grades of salivary gland cancer
grade 1 = low grade: resembles normal SG cells. good prognosis
grade 2 = intermediate grade : moderately differentiated
grade 3 = high grade: does not resembel SG cells, grows ± spread quickly, poor prognosis
What is the cornerstone treatment of salivary gland tumors
surgery
complete excision with preservation of neural structures is the goal
when is adjuvent RT used for treatment of salivary gland tumors
for high grade tumors at risk of locoregional failure
Describe the treatment of T1-2, N0 low grade parotid cancer
parotidectomy w/o nerve resection and neck node dissection
describe the treatment of T1-2 N0, high grade parotid cancer
parotidectomy ± nerve resection ± neck node dissection + adjuvent RT
describe the treatment of T3, N0 parotid cancer
extensive parotidectomy ± nerve resection ± neck node dissection + adjuvent RT
describe the treatment of T4 parotid cancer
extensive parotidectomy + nerve resection + neck node dissection + radiation therapy
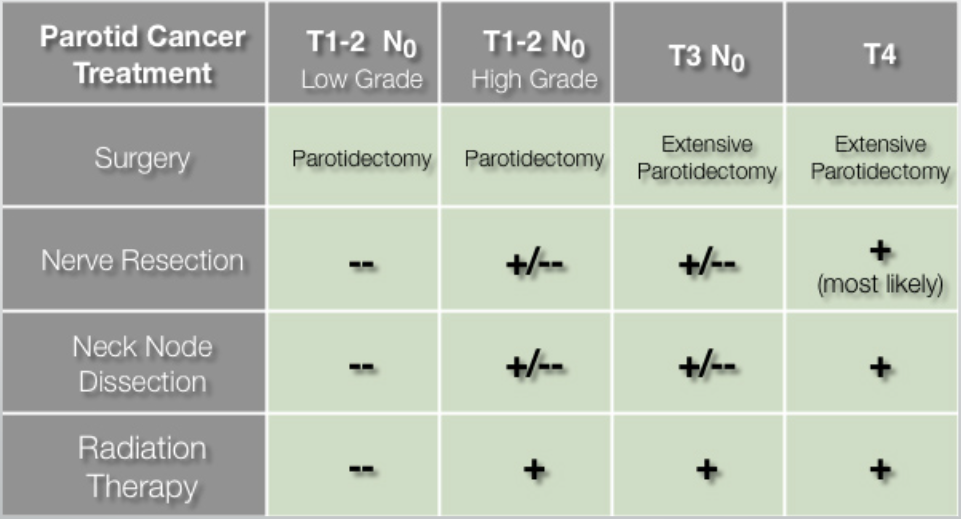
when would adjuvent RT potentially be added to low grade parotid gland cancers
if there are positive margins or spillage or perineural invasion
how does the T3/T4 surgical treatment change for parotid gland vs salivary gland
parotid = total parotidectomy ± LN dissection
salivary = surgical resection ± LN dissection
if there is complete resection of the salivary gland tumor, what is then done?
typically only surveillance or chemoRT if the histology is adenocystic or there are adverse features (ECE, neural invasion, LN mets, etc)
if there is incomplete resection of the salivary gland tumor, what is then done
another surgical resection if possible or chemoRT
what treatment is done for unresectable T4a and T4b salivary gland tumors?
definitive RT or chemoRT
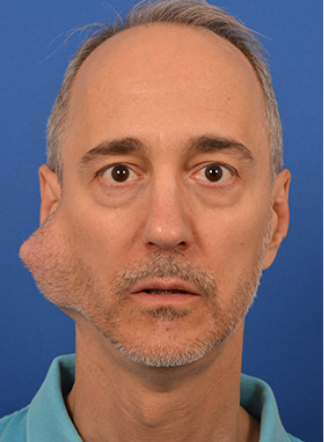
what are the major complication of total parotidectomy? what are some other complications
facial nerve paresis
scarring, facial nerve damage, morbidity
what are two major complications of neck node dissections for salivary gland tumors
cervical lymphadenopathy nd facial nerve paralysis
what combination chemo can be used for treating salivary gland tumors
cisplatin/carbo + 5FU
70-80% of salivary gland tumors arise in what gland?
the parotid gland
what is the typical spread of parotid gland tumors
painless local spread infiltrating the whole gland
what cranial nerve has the biggest risk of invasion via a parotid gland tumor?
the facial nerve (CN VII)
motor, sensory, and parasympathetic functions of CN VII (facial nerve)
motor = facial expression
sensory = taste to anterior 2/3 of tongue
parasympathetic = innervates lacrimal, submandibular, and sublingual glands
clinical presentation of a parotid gland tumor invading the facial nerve
xerostomia, lagophtalmos (loss of ability to close eye completely), ageusia (loss of taste)
what are local symptoms of parotid gland tumors
swelling in parotid area, facial palsy, local pain, tenderness, rapid growth
what do the majority of parotid gland cancer patients present with
asymptomatic parotid mass
what are late/advanced stage symptoms of parotid gland tumors
trismus, severe pain, growth into parapharyngeal space encroaching on other cranial nerves
this is very rare
what is the best predictor of nodal metastasis of parotid gland tumors
facial nerve involvement
in addition to tumor grade