ANHB2214 Endocrine Glands
1/45
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
46 Terms
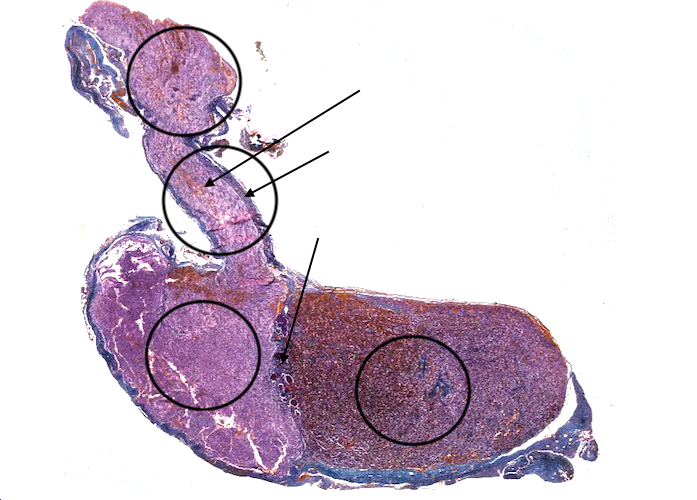
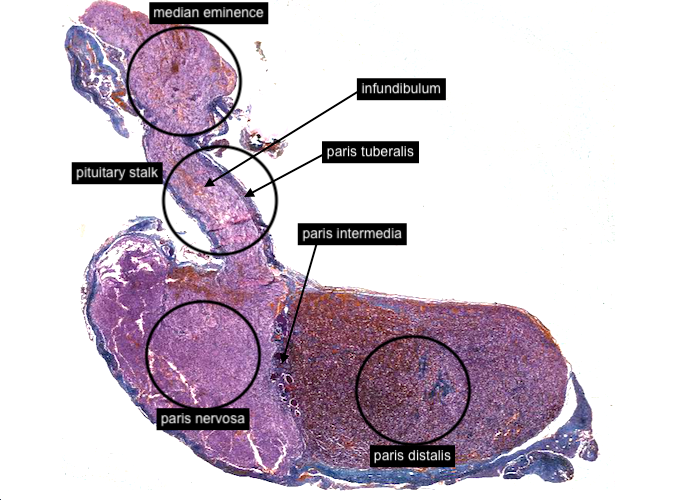
The pituitary gland (or hypophysis) has two fundamental divisions, the adenohypophysis derived from oral ectoderm and the neurohypophysis which is an extension of the brain. Each division has three parts; the pars distalis, pars intermedia, and pars tuberalis comprise the adenohypophysis and the median eminence, infundibulum and pars nervosa make up the neurohypophysis.
Unfortunately, there are some synonyms to confuse you. The anterior pituitary/anterior lobe is also called the pars distalis and the pars nervosa is named the posterior pituitary/posterior lobe. Also, the infundibulum and pars tuberalis together make up the pituitary stalk as a gross anatomical structure.
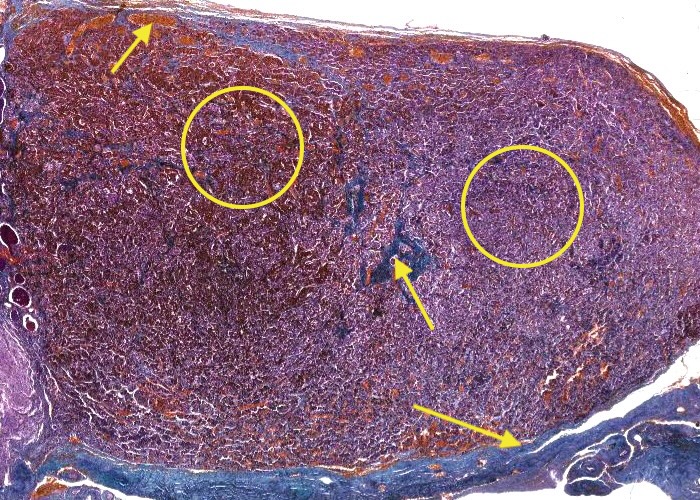
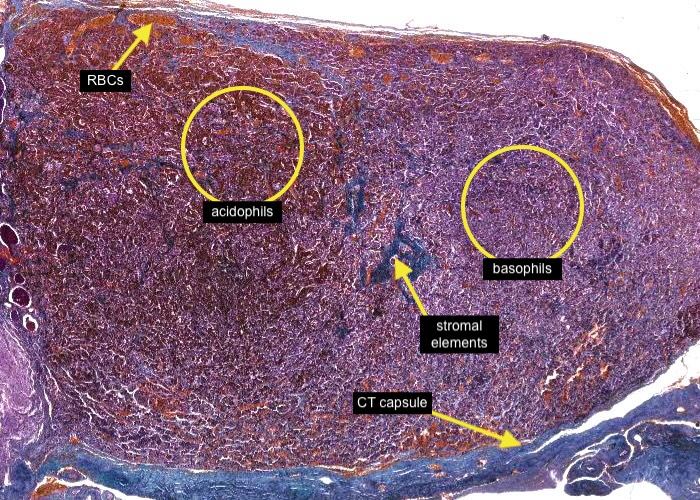
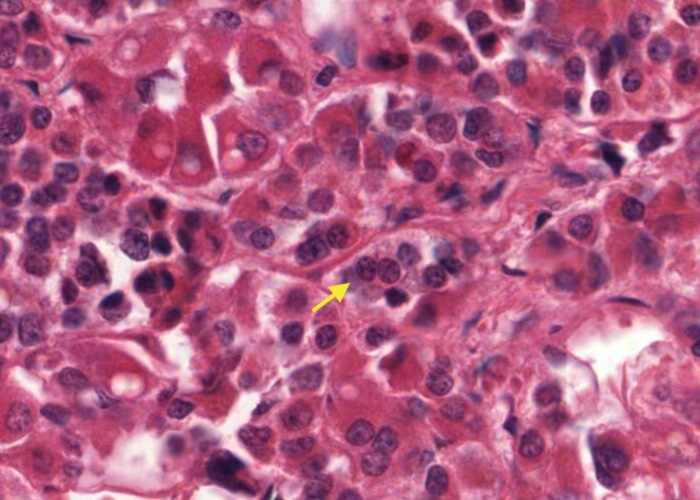
Examine the adenohypophysis (anterior pituitary) at low magnification; The stain used here clearly shows that acidophils and basophils are distributed non-uniformly. In some regions, acidophils seem to dominate, but in other regions, basophils dominate.
Like any endocrine gland the tissue is highly vascularized. At this low magnification, the small orange-stained areas are red blood cells in blood capillaries. A blue-stained, connective tissue capsule, surrounds the gland with delicate stromal elements penetrating the gland and supporting the blood vessels and parenchymal (functional) cells.
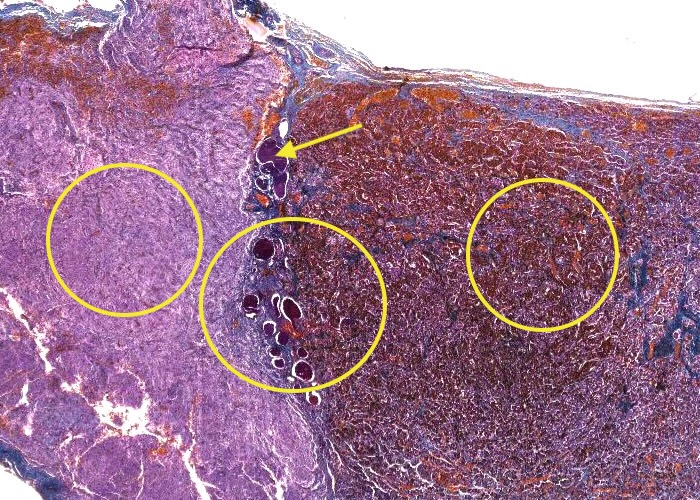
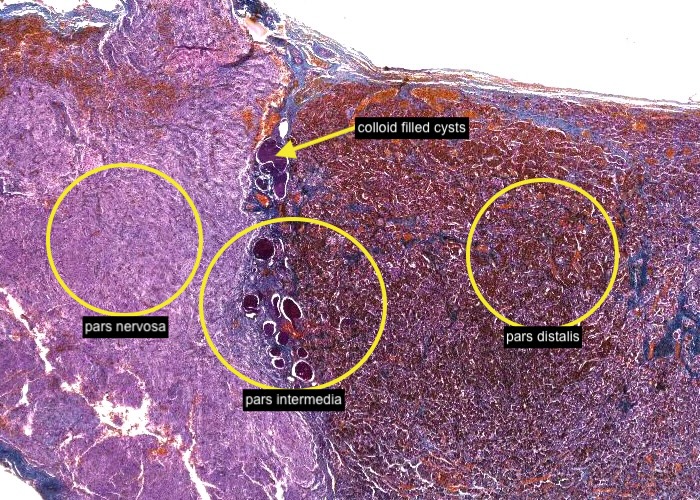
The pars intermedia is poorly represented, and in humans thought to be rudimentary. It is the thin remains of the posterior portion of Rathke's pouch and lies adjacent to the pars distalis anteriorly and the pars nervosa posteriorly. The parenchymal cells surround colloid-filled cysts. Their function, if any, is unclear.

Cuboidal parenchymal cells surround each colloid-filled cyst. Their function, if any, is unclear. When you examine the histological section you may see a few basophils that have migrated a short way from the pars intermedia into the pars nervosa.
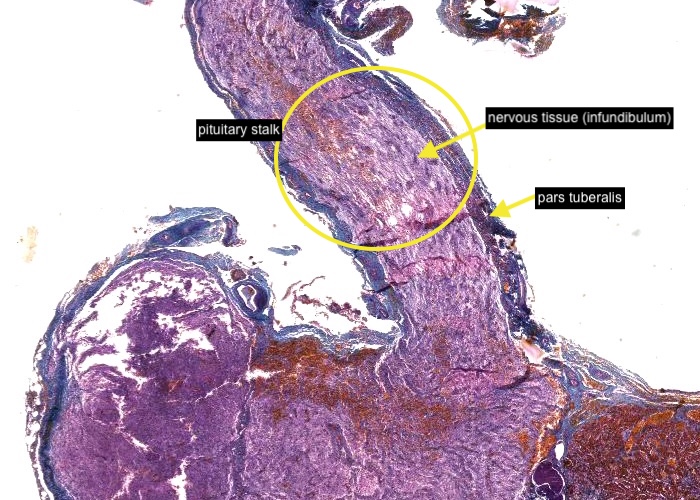
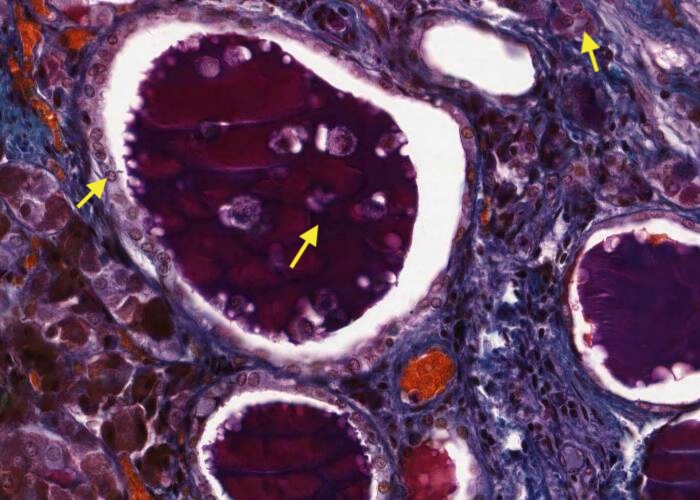
Turning to the pituitary stalk the pars tuberalis is a thin layer of adenohypophysis surrounding a core of nervous tissue (infundibulum).
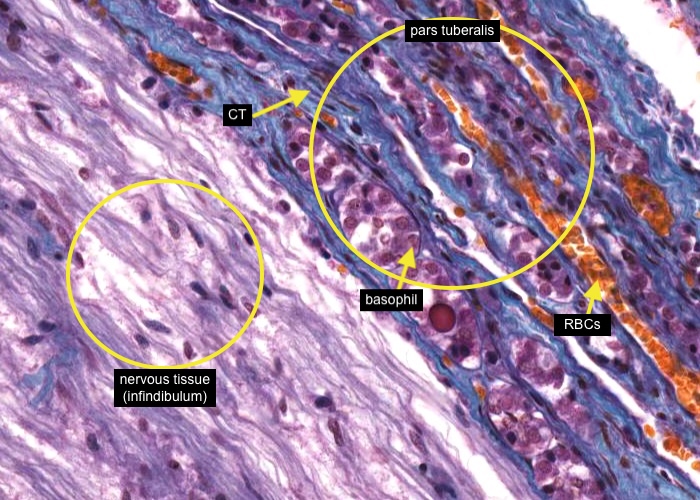
The pars tuberalis is a thin layer of adenohypophysis surrounding nervous tissue. It contains a few basophils arranged in small clusters or cords surrounded by connective tissue but its main significance is in its hypophyseal portal veins (identify each one containing orange-stained red blood cells) that carry hormone releasing factors from the median eminence to the pars distalis.
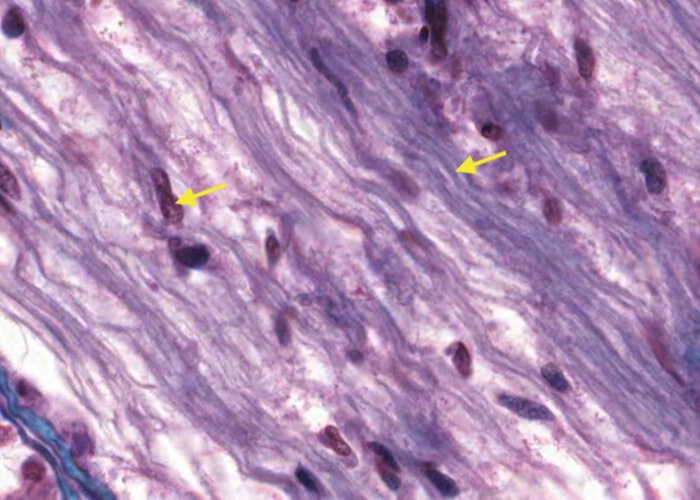
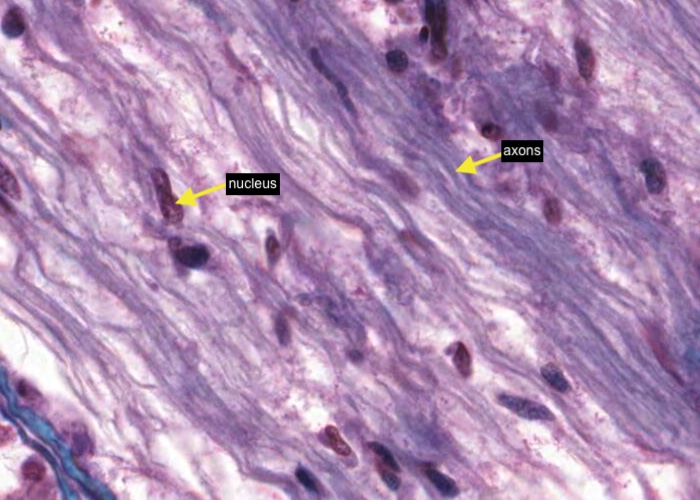
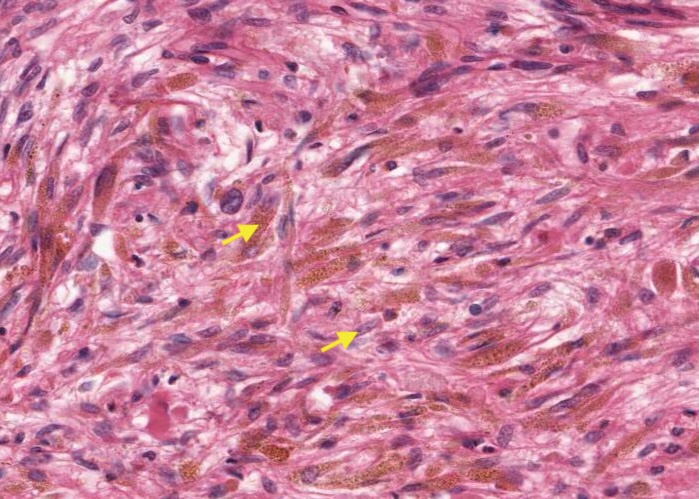
As you would have noticed when you viewed the pars tuberalis, the infundibulum differs markedly from the adenohypophysis in cellular composition. The bulk of the infundibulum is made up of non-myelinated, neurosecretory axons running in parallel down the stalk forming what is called the hypothalamohypophyseal tracts. There are no neuron cell bodies in the pituitary gland as they are located in the median eminence. Each nucleus that you see is of a glial cell which, in this gland, is called a pituicyte.
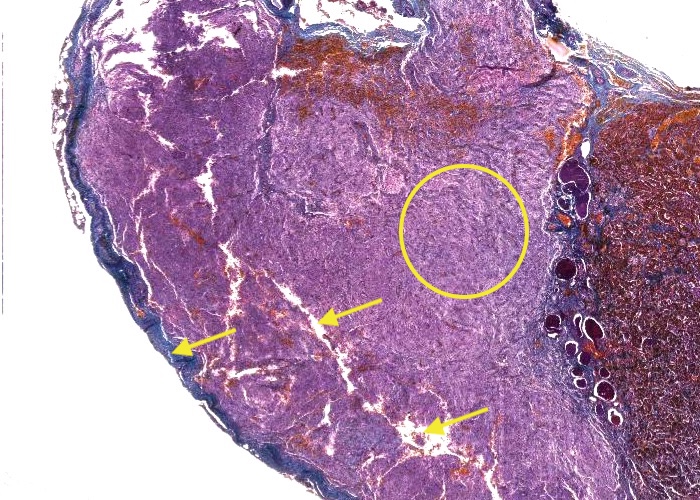
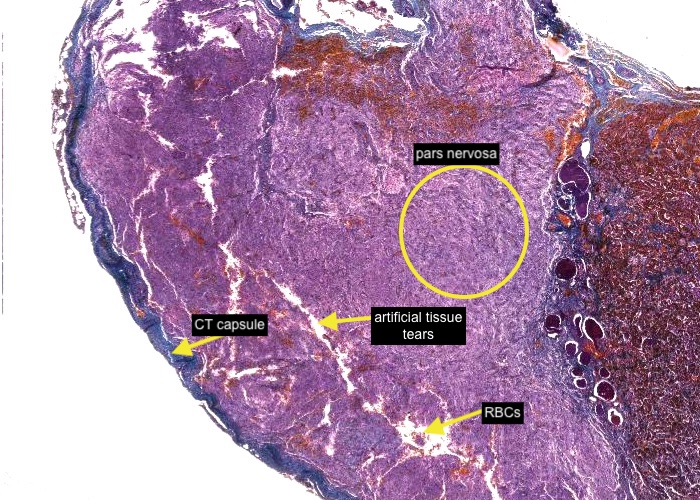
The pars nervosa is the neural part of the pituitary gland and has a similar appearance and composition to the infundibulum except that the axons do not run so straight. There are some artifactual tissue tearing and loose red blood cells in this part of the section. Note the connective tissue capsule.
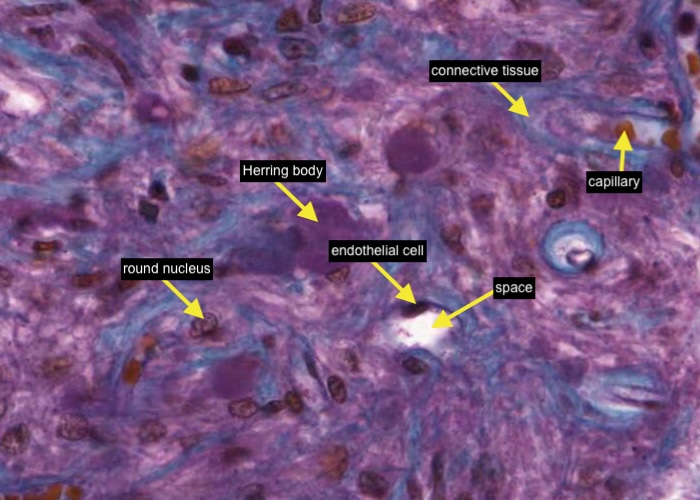
The Herring bodies are poorly preserved in this section. Their granules have lysed and each Herring body looks like an amorphous bluish blob. This is how they frequently look on slides (and in pictures in text books) but do not worry, they are preserved the way they should be in the next section - i.e. Pituitary (H&E). The light, blue-stained, connective tissue septa encase the axons and remember each roundish nucleus you see is that of a glial cell called? Of course an elongated nucleus adjacent to a space could belong to an endothelial cell lining a capillary.
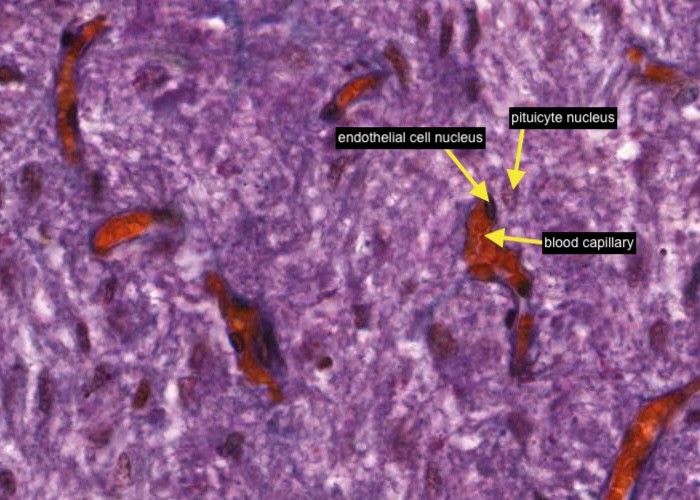
Whilst there are also fibroblasts and apparently mast cells in the posterior lobe of the pituitary (pars nervosa) most cells present are the pituicyte with a round or oval nucleus. Each pituicyte is associated with a fenestrated blood capillary and resembles an astrocyte in having a supporting role. Make sure you can distinguish the nucleus of a pituicyte from a more elongated and darker stained endothelial cell nucleus that will be closely associated with the capillary wall.

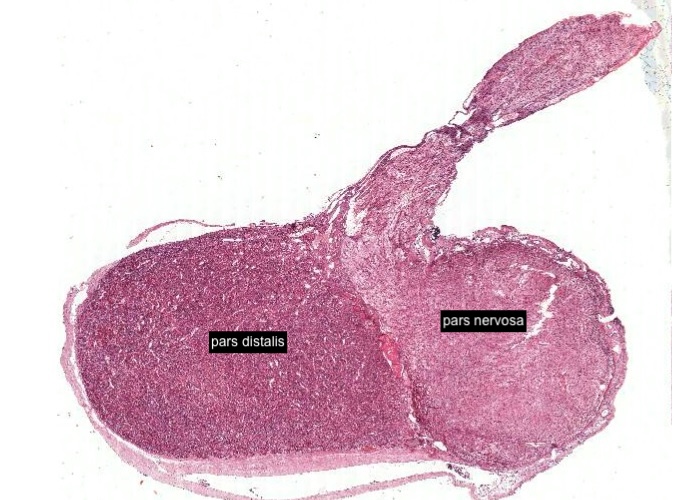
This image is facing the opposite to the previous one you have been viewing. It is useful to look at this H&E stained section and view the characteristics of the anterior pituitary/anterior lobe (pars distalis) and the posterior pituitary/posterior lobe (pars nervosa).
where are the acidophils?
H&E does not clearly distinguish acidophils from basophils. The stain that differentiates them is PAS (a component of the polychrome stain) you saw in the prevous histological section. It stains the hormones that are glycosylated and not those that are simple peptides without sugar moieties. Since this leads to some cells ending up purplish while others are orangish, the conventional appellations of basophil and acidophil have been inappropriately extended to them. Collectively, the two together are called "chromophils". The chromophobes are easily distinguished from the chromophils. They continue to stain palely.
Well, there are still some regions where cells with a very acidophilic stain are noticable which will be acidophils.
icdentify acidophillic stain
Acidophils are readily identified by the strong acidophilic staining of their cytoplasm.
identify basophil
Basophils can be identified by their cytoplasm clearly basophilic.
A
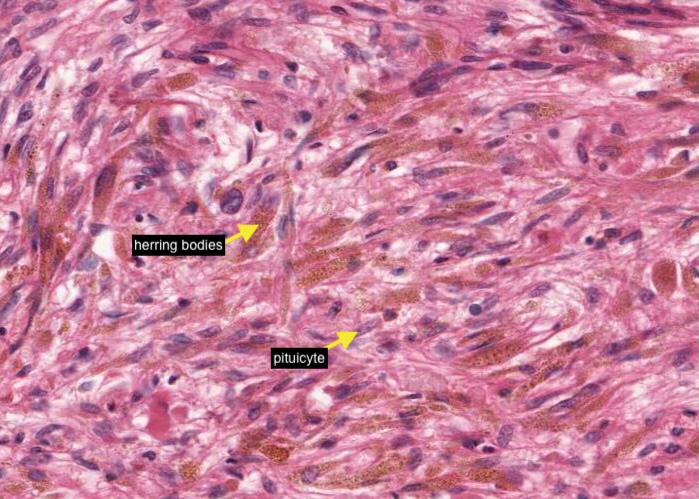
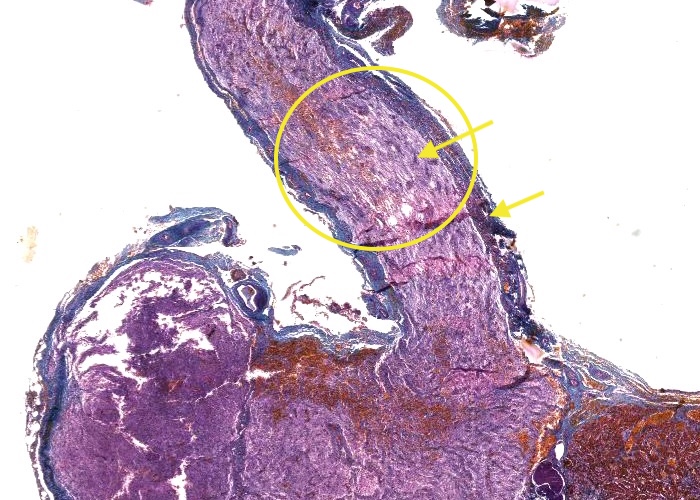
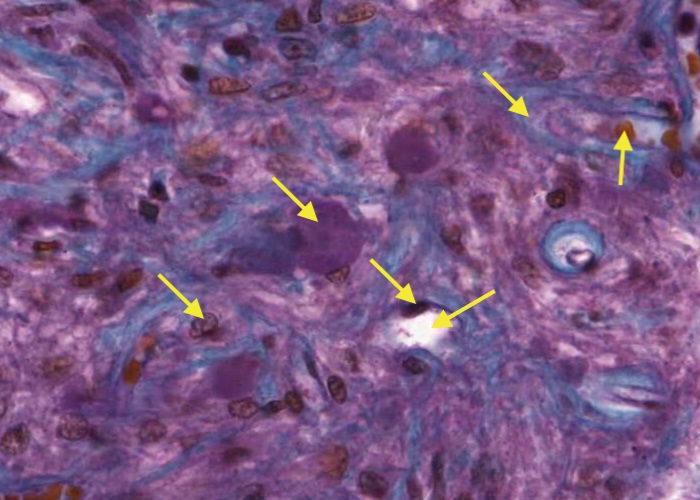
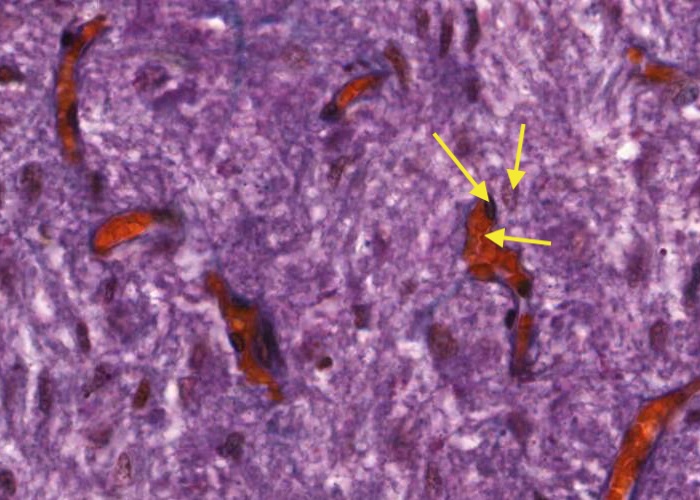
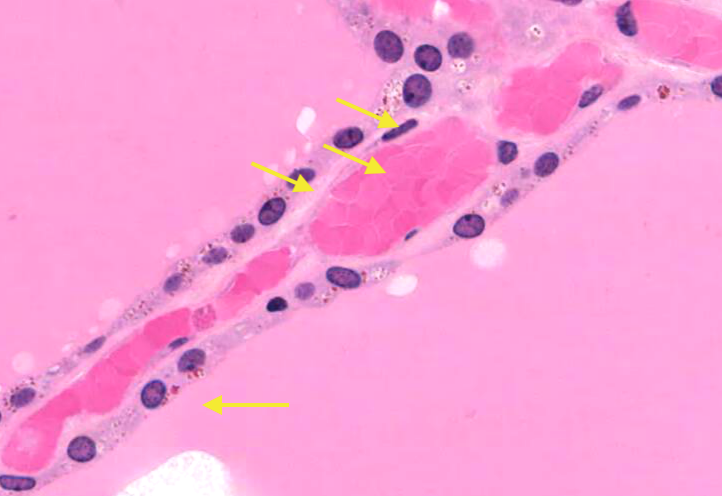
s you would have understood from viewing the pars nervosa stained with a polychrome stain most cells present are the pituicyte. But, what is striking in this image are the swollen ends of the axons (Herring bodies) containing brown-stained vesicles.
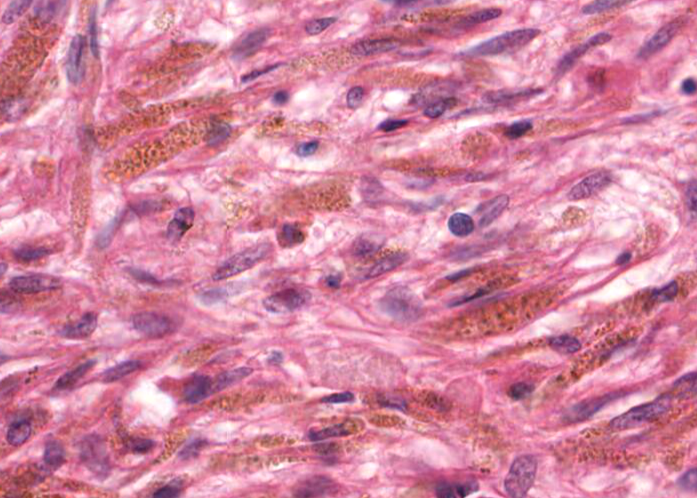
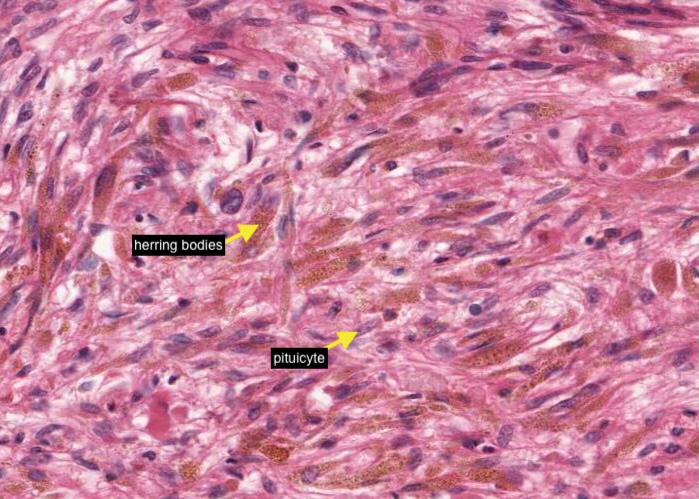
The Herring bodies are excellently preserved in this H&E stained section of the pituitary gland. You should scan the pars nervosa carefully at high magnification to find them as oval shaped packets of brownish granules.
Each packet represents the granule-filled end of an axon next to a capillary (which may not be caught in the section). Herring bodies tend to be clustered so scan around.
Herring bodies contain oxytocin or ADH (vasopressin) secreted by different neurons in the hypothalamic nuclei.
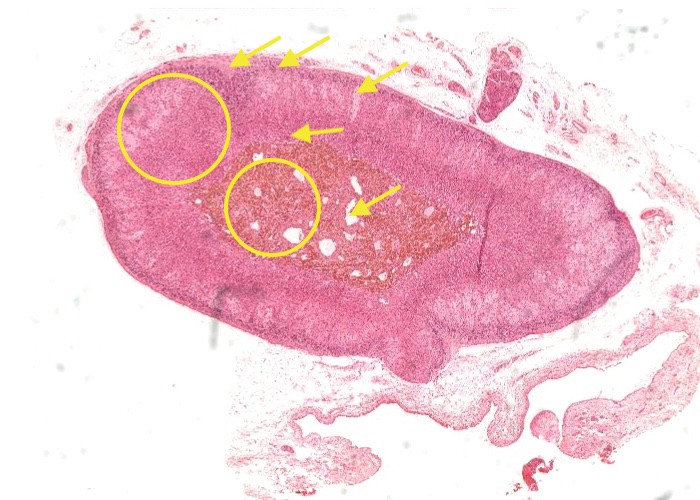
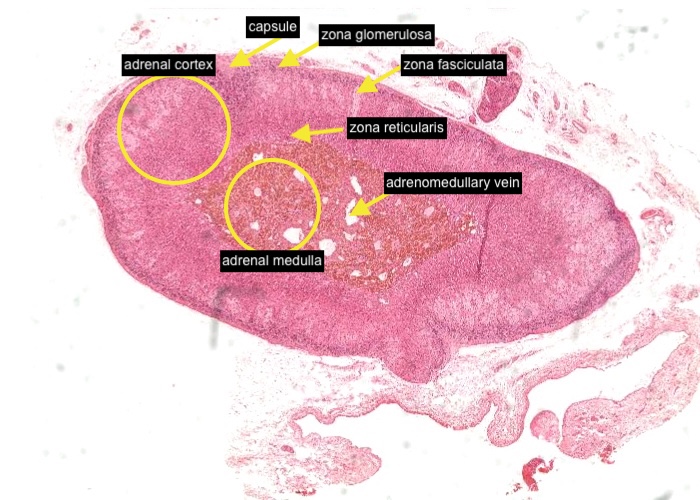
This is a good section to review small blood vessels in the surrounding tissues of the adrenal gland - and a large vein.
It's easy to distinguish the adrenal cortex from the adrenal medulla because chromaffin cells (in the medulla) are stained yellowish brown by the “chromaffin reaction” in clear contrast with the cortical cells. Each of the very large, clear profiles you can see is most likely an adrenomedullary vein. The chromaffin cells secrete adrenalin (epinephrine) and noradrenaline (norepinephrine).
The adrenal cortex has three distinct zones that stain differently (progressing from exterior i.e. near the capsule to interior, near the medulla) :
zona glomerulosa - cells secrete mineralcorticoids (e.g. aldosterone).
zona fasciculata - cells secrete glucocorticoids (e.g. corticosterone and cortisol).
zona reticularis - cells secrete gonadocorticoids (e.g. dehydroepiandrosterone or DHEA).
The zones are variable in thickness, depending on the plane of section.
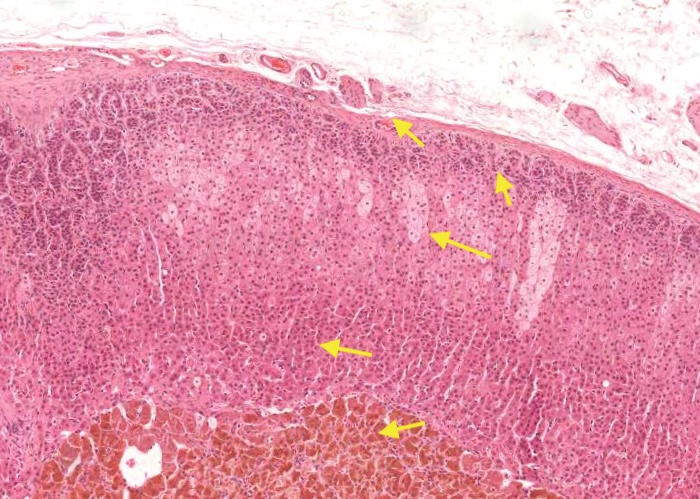
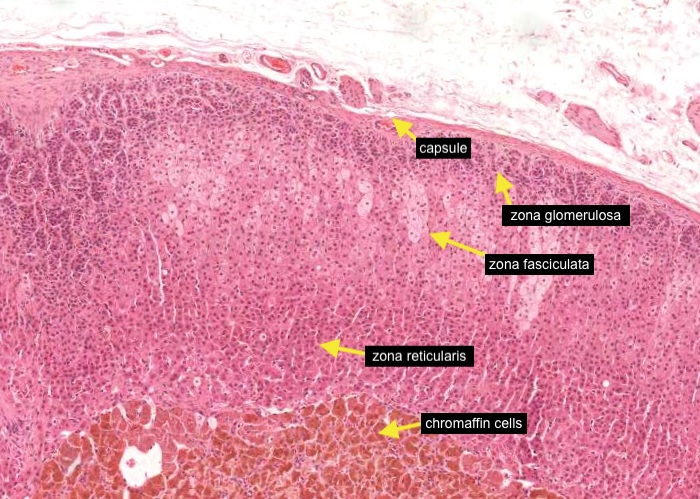
At this higher magnification, again note the chromaffin cells (in the medulla) and the three distinct zones of the adrenal cortex:
zona glomerulosa (just under the capsule)
zona fasciculata
zona reticularis
You can now view more characteristics of these "zones" in the next few items.

Note the small blood vessel in the capsule.
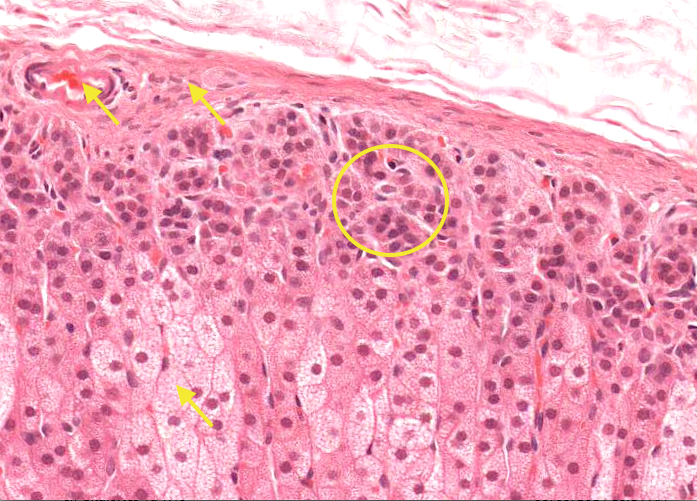
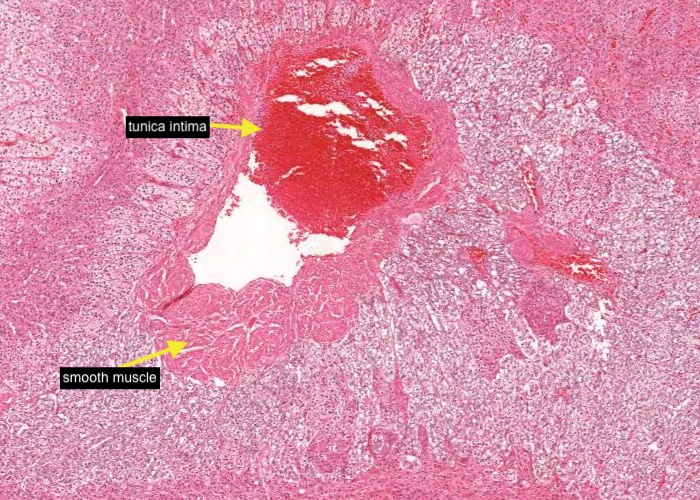
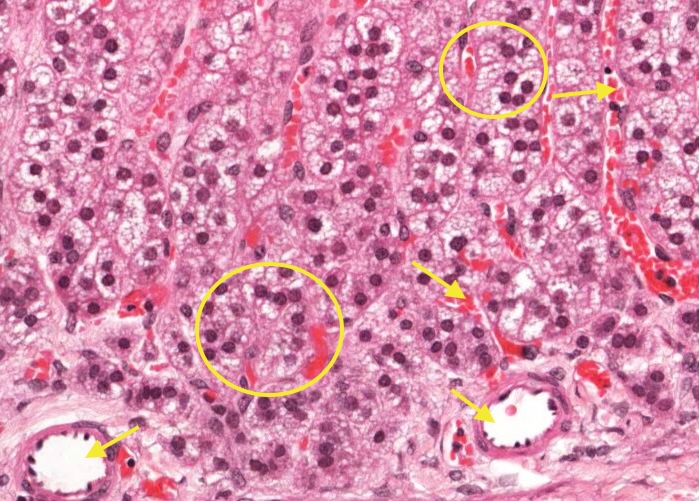
The layers of the cortex can be visually distinguished in two ways. One is by the orientation of the columns of cells (and hence of the capillaries between them). In the outer zona glomerulosa the cells are arranged in closely packed clusters. The cells are also quite small. The clusters straighten out into an almost perfectly radial alignment in the adjacent zona fasciculata.
The layers also differ in the appearance of the cells. The cells of the middle zona fasciculata are largest and palest.
Unfortunately, all the extensive sinusoidal capillaries surrounding each cluster is not visible.
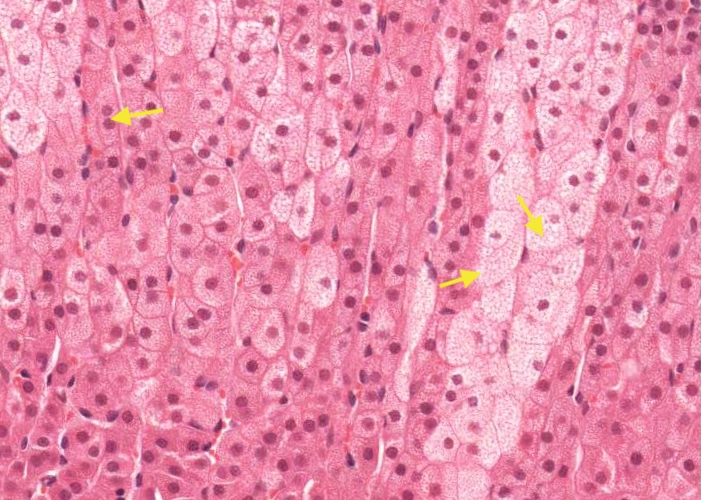
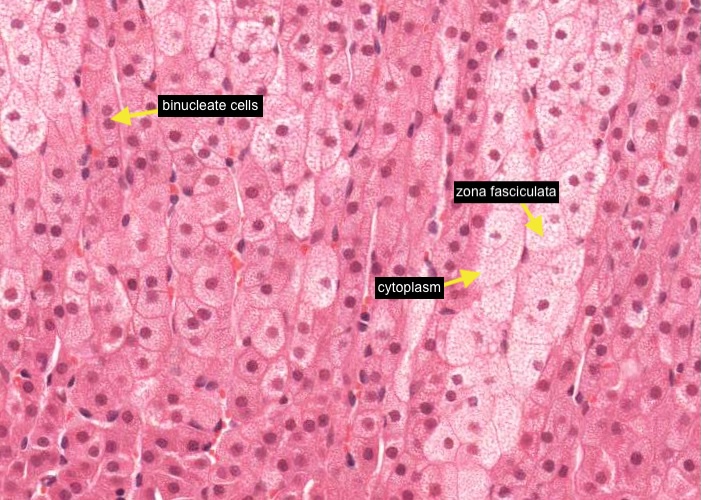
The cells of the middle zona fasciculata are largest and palest and arranged in long, straight cords only a few cells thick. It is quite common to see binucleate cells. This zone occupies about 80% of the cortex volume.
A sharp eye viewing the histological section at maximum magnification can see that the cytoplasm of these cells looks foamy. This is due to the numerous lipid droplets (containing precursors for synthesizing steroid hormones) which filled their cytoplasm until they were leached out during slide preparation. The cells of the two adjacent zones look darker because they synthesize hormones less actively and store substantially less lipid droplets in their cytoplasm.
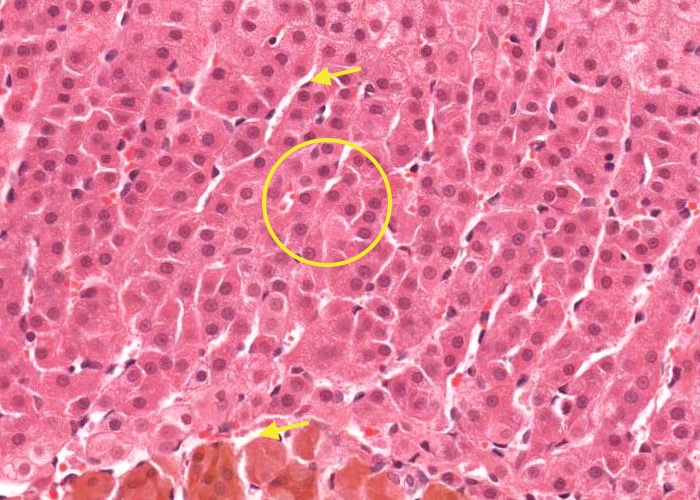
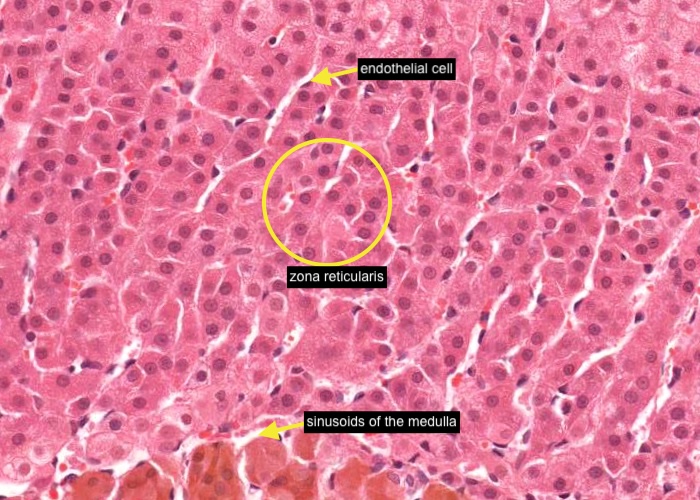
Notice that the cells of the zona reticularis are much smaller than the cells in the adjacent zona fasciculata. They are arranged in anastomosing cords and some of the blood capillaries are visible adjacent to these cords of cells - look for a flattened (squamous) endothelial cell nucleus. As the blood leaves the zona reticularis it enters the sinusoids of the medulla and bathes these cells.
Developmentally, as well as physiologically, the cortex and the medulla are distinct glands. The cortex is derived from mesodermal mesenchyme, the medulla from neural crest cells. The neural crest is also the origin of the peripheral nervous system and in several ways the adrenal medulla resembles an organ that starts out developing as a sympathetic ganglion and then switches to an endocrine developmental pathway half way along.
The cells that would become postganglionic sympathetic neurons neglect to send out axons or dendrites. They do develop the enzymes for making catecholamines but just release their secretions locally (as neuroendocrine cells) into an adrenomedullary vein.
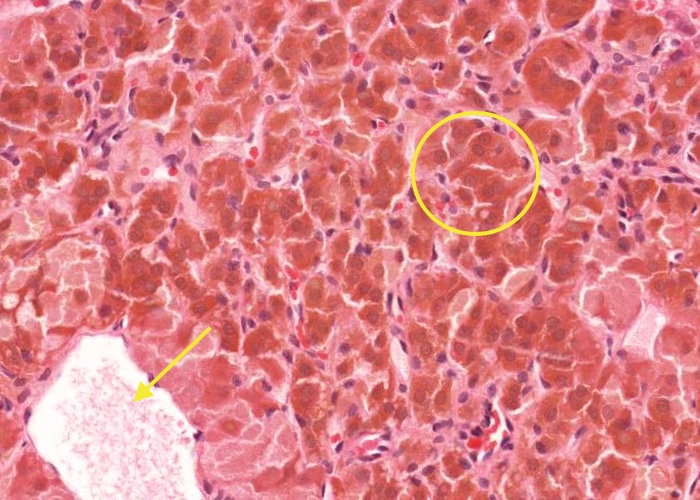
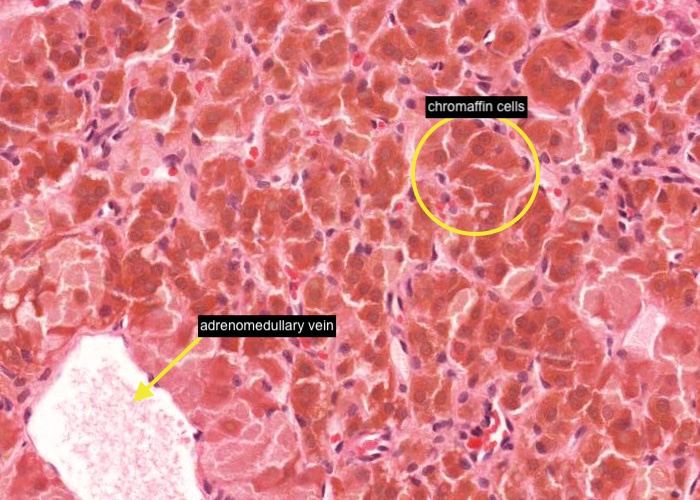
Postganglionic sympathetic neurons release norepinephrine (noradrenaline) but the adrenal medulla has two populations of secretory cells - one releases norepinephrine and the other epinephrine (adrenaline). These two types of cells look very similar. Both are stained by the so-called chromaffin reaction specific for the adrenal medulla (it stains catecholamines). Therefore, both types are given the same name of chromaffin cells. They are innervated by preganglionic sympathetic axons.
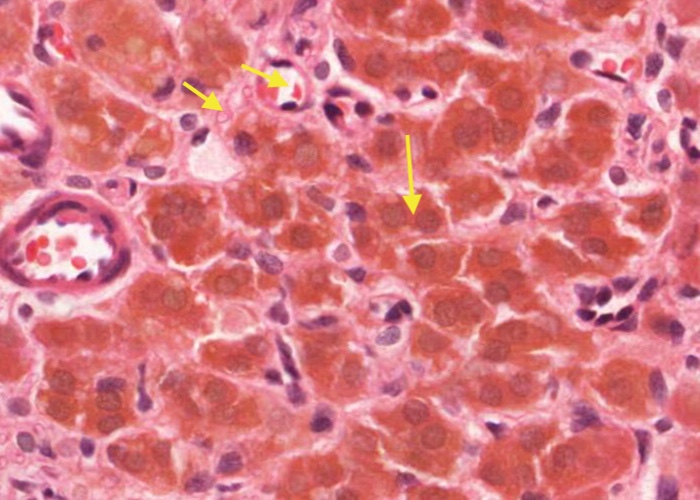
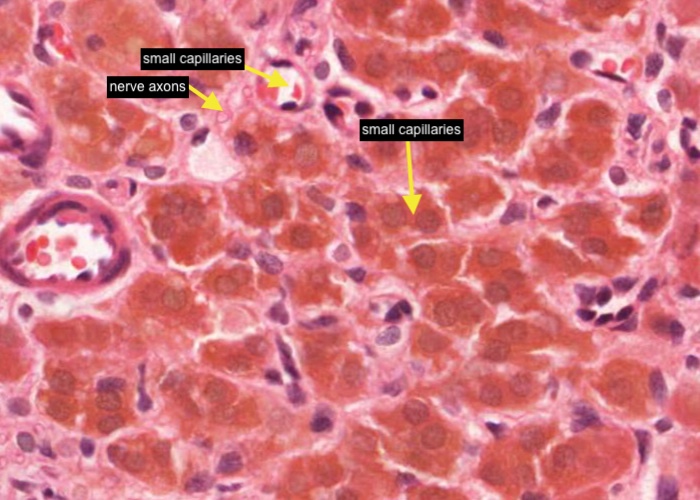
The parenchymal cells of the adrenal medulla are the chromaffin cells (often called medullary cells). They are modified neurons. They reside in small clusters amongst connective tissue elements, nerve axons and small capillaries.
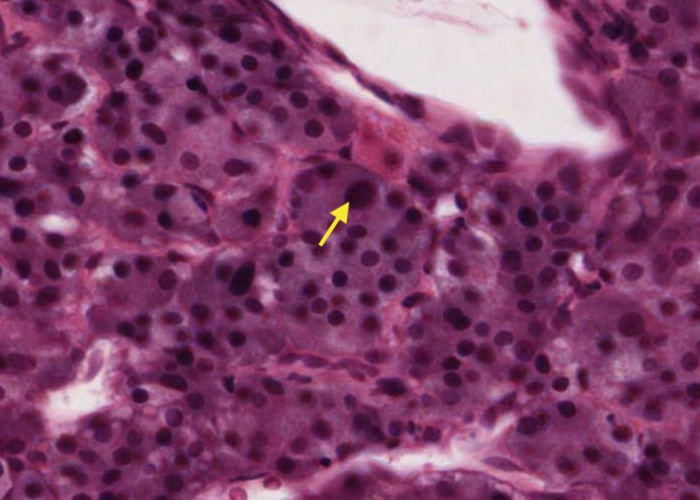
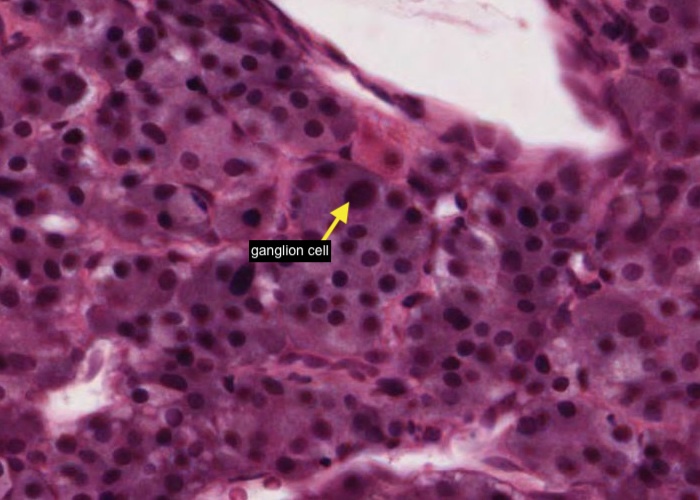
This developmental story (how the adrenal medulla got its sympathetic ganglion-like characteristics) offers an explanation for another curious detail of the gland. The medulla has the odd ganglion cell scattered about (i.e. postganglionic sympathetic neuron). It is a large cell with a large circular nucleus. It is as though some of the developing neurocrest cells did not get the message to switch over to endocrine-type cells. You have to look very hard to find one.
They do actually have a role. They innervate cells of the cortex and effect their secretory activity and also innervate blood vessels and some of the abdominal organs via splanchnic nerves.
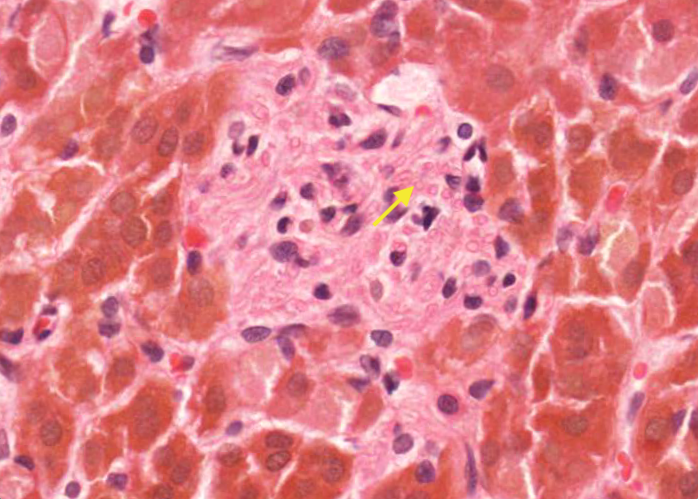
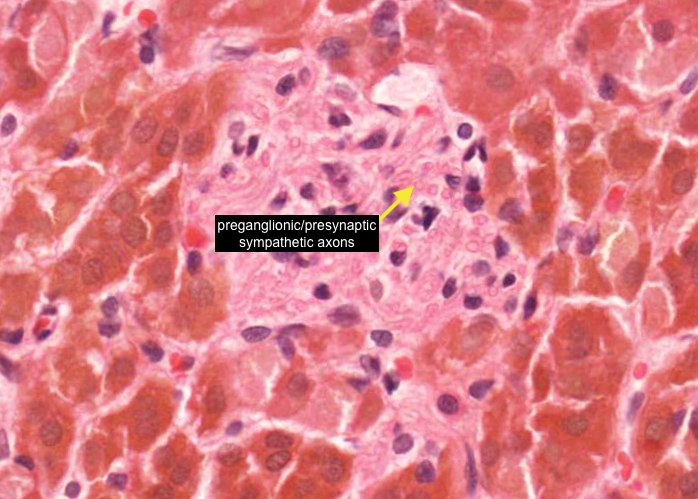
The chromaffin cells are innervated by preganglionic/presynaptic sympathetic axons which appear as tiny pink dots scattered through the medulla.
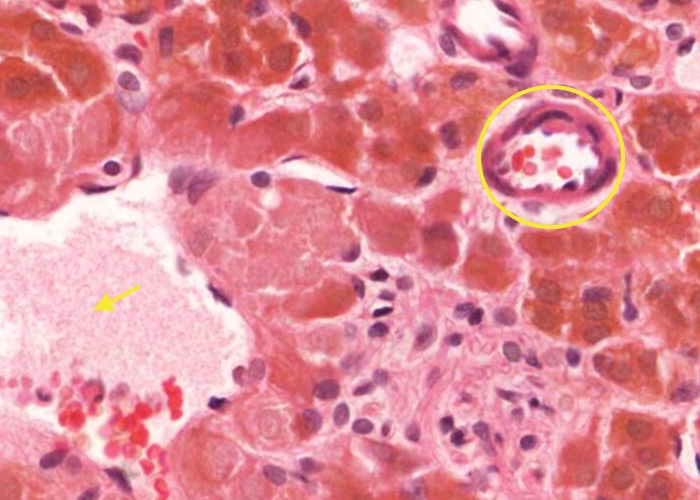
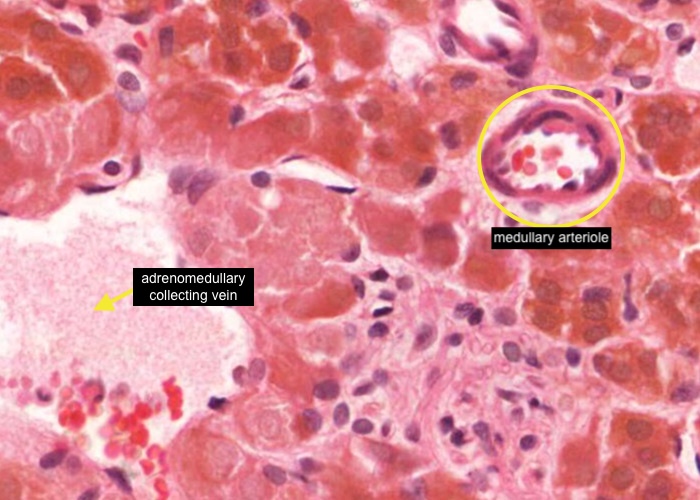
One other feature of the vasculature that you will have to hunt for on this section, and still may not see satisfactorily, is a medullary arteriole.
These small arterioles run down the thickness of the cortex from the capsule to the medulla but gain their name from the fact that they deliver fresh blood to the medulla. Thus, the cells of the medulla have a dual blood supply - a direct arterial supply as well as venous blood that the cortical cells have first access to. All the blood in cortical blood and medullary blood sinusoids will then flow into a small branch of the adrenomedullary collecting vein.
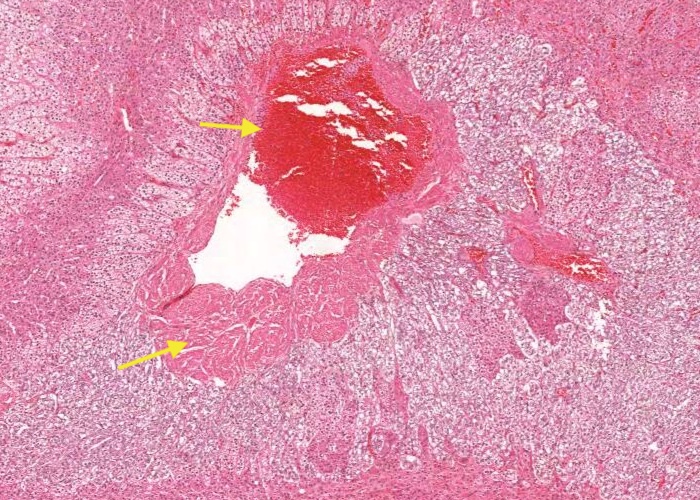
The central adrenomedullary vein and its tributaries have longitudinally oriented smooth muscle cells (muscle cushions). In some places, the smooth muscle bundles may be absent and the cells of the adrenal medulla are close to the tunica intima.
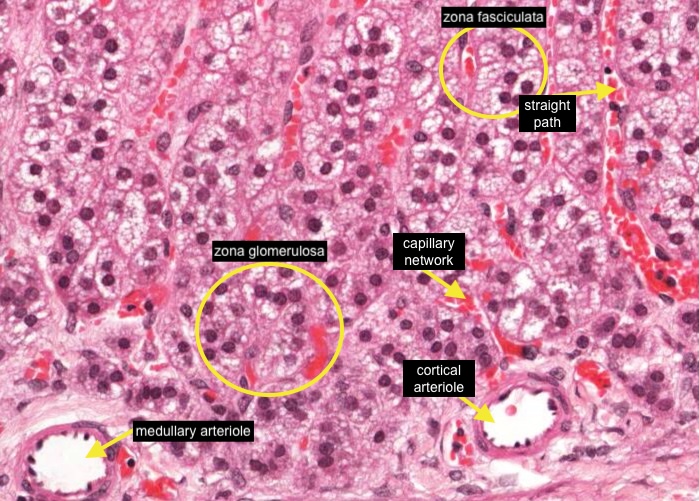
If you scan along the capsule you will see small arterioles. One may be a cortical arteriole that will form an extensive capillary network around the zona glomerulosa and then an almost straight path alongside cells of the zona fasciculata to then supply cells in the zona reticularis and adrenal medulla.
Another arteriole within the capsule may be a medullary arteriole which will travel straight through the adrenal cortex then form a sinusoidal network within the adrenal medulla. Blood will then drain into the adrenomedullary collecting veins and exit the adrenal via the central adrenomedullary vein.
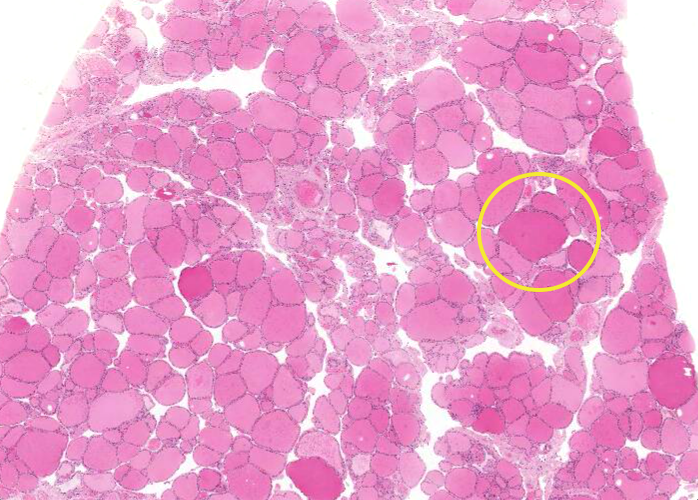
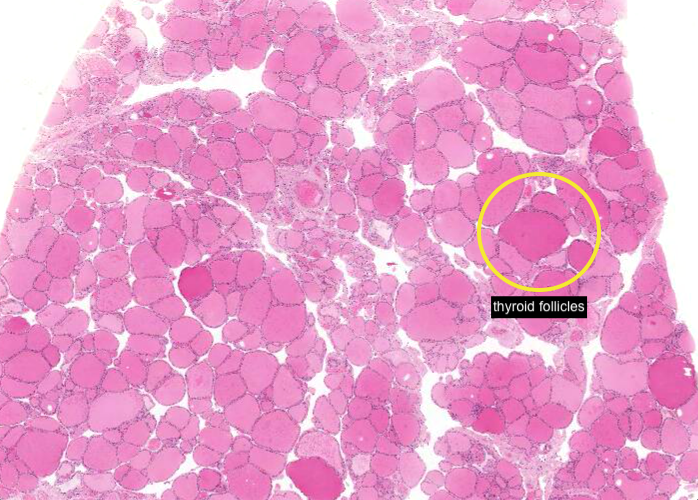
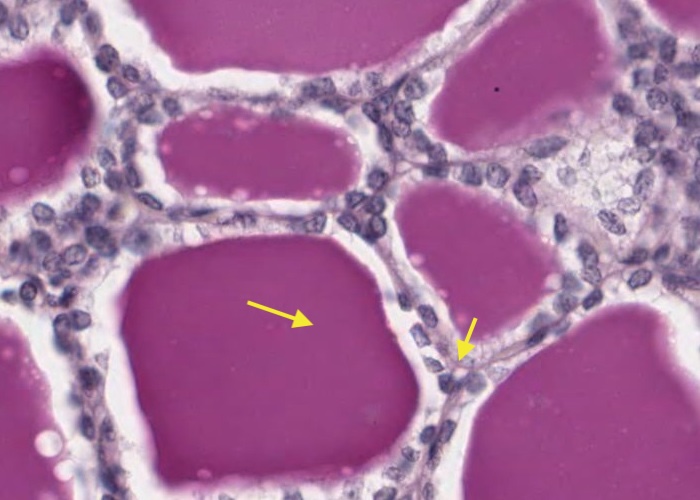
Under low magnification note that the thyroid gland is filled with round, blank, pink structures. These are thyroid follicles, the main structural and functional unit of the gland. They vary in diameter so you see profiles here of different sizes.
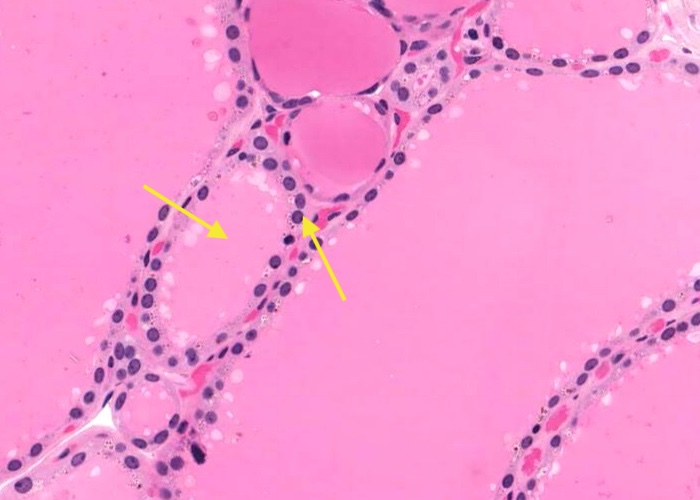
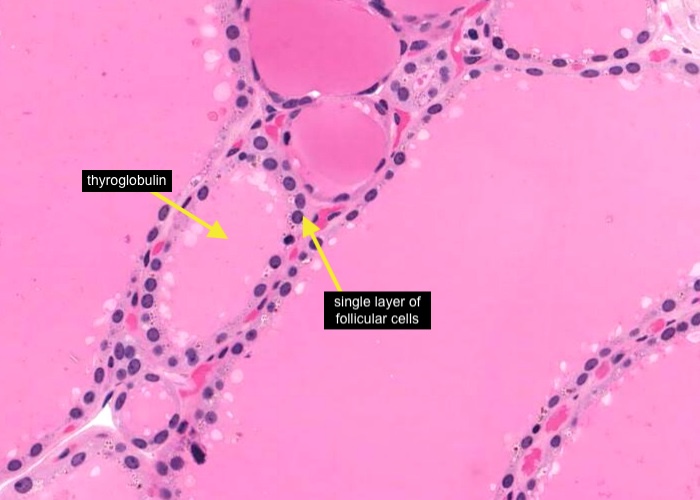
Under higher magnification observe that a single layer of follicular cells form a simple epithelium around each follicle. The basement membrane is on the outer side of the epithelium. The material inside the follicle is mostly the iodinated glycoprotein called thyroglobulin but histologists call it “colloid” the same name that they use for the unrelated goo in the cysts of the pars intermedia of the pituitary gland!

Follicular cells have a double secretory function.
They synthesize and secrete thyroglobulin into the follicle in the manner of an exocrine process. Enzymes at the cell surface iodinate the tyrosine residues of the protein as it is secreted. The follicle thus becomes a reservoir for the iodinated substrate of thyroxin. The colloid is the iodinated glycoprotein (thyroglobulin).
Follicular cells also phagocytize droplets of thyroglobulin from inside the follicle and break it down to form thyroxin which the cells secrete basally into capillaries in a typical endocrine manner. You can see evidence of this process. The follicular cells have orangish inclusions in their cytoplasm which are digestion vacuoles of thyroglobulin. The amount of stroma between follicles is minimal.
The aggregations of red blood cells indicates the very extensive system of capillaries. Every follicular cell is close to one. The flattened nucleus you can find probably belong to an endothelial cell, along with a few fibroblasts.
parafollicular cells/C cells?
The thyroid also contains a second type of secretory cell. Parafollicular cells (C cells) secrete the hormone calcitonin. These clusters of cells are located in the stroma between the follicles (as their name suggests) and look pale in comparison to follicular cells (as their alternative name, clear cell = C cell, suggests). Their cytoplasm give the impression of containing tiny vesicles. Look around for them but do not be disappointed to find only doubtful candidates. There are specific stains for these cells but they have not been used in any of the set of tissues in this online interactive atlas.
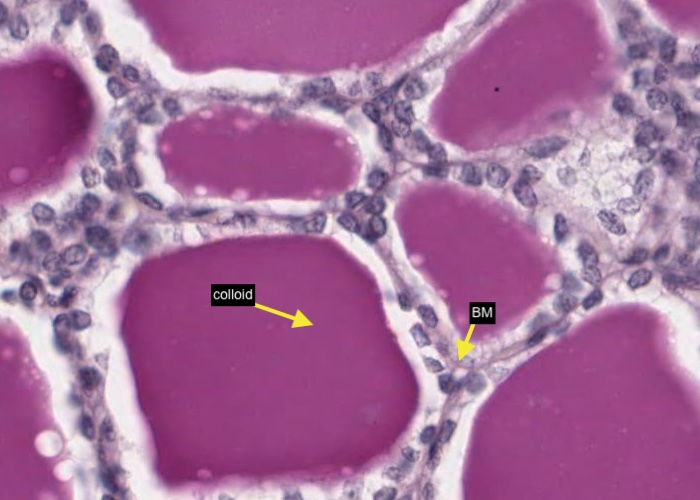
Note the intense staining of the colloid with PAS. The stain also allows you to visualize the basement membrane around each follicle. Their cells do form a true epithelium. PAS is a poor stain for examining the follicular cells themselves.
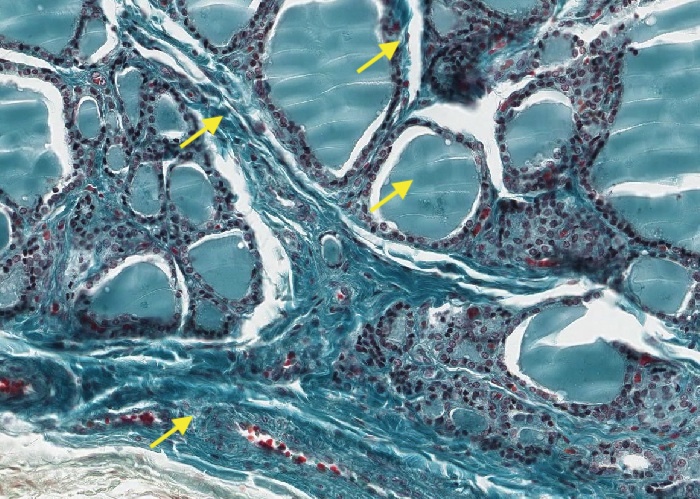
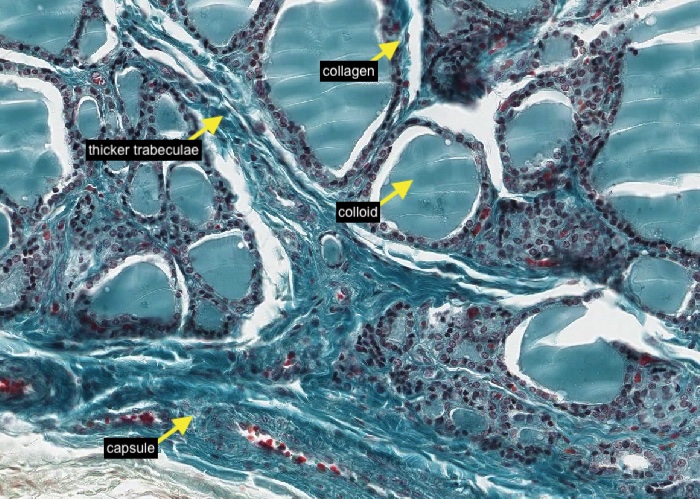
Masson stain emphasizes stroma while still giving good views of cells. It shows that there is a small amount of collagen between adjacent follicles, but not much.
Somewhat thicker trabeculae penetrate the gland to provide a pathway for blood vessels and outline lobes and lobules. Also, the nondescript capsule around the tissue shows up well.
The stain here does not provide any new insights about the follicular cells but it is a bit better than H&E for picking out possible parafollicular cells.
Ignore the gouges in the colloid as artifacts.

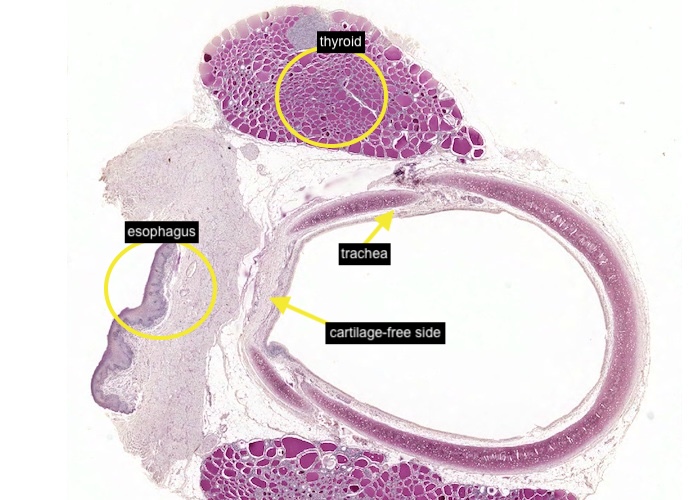
This section demonstrates the location of the thyroid in the body. The section transverses the trachea at the level of the thyroid. The trachea is the large circle in the centre flanked by the two, darkly-stained, purple lobes of the thyroid.
You might as well pause a moment and notice the orientation of the trachea and the esophagus. When your professor of gross anatomy tells you that the cartilage-free side of the trachea lies next to the esophagus you can say "Of course we know that, we have already taken histology". Think a minute so you can also say "and we also understand the physiological rational for this".
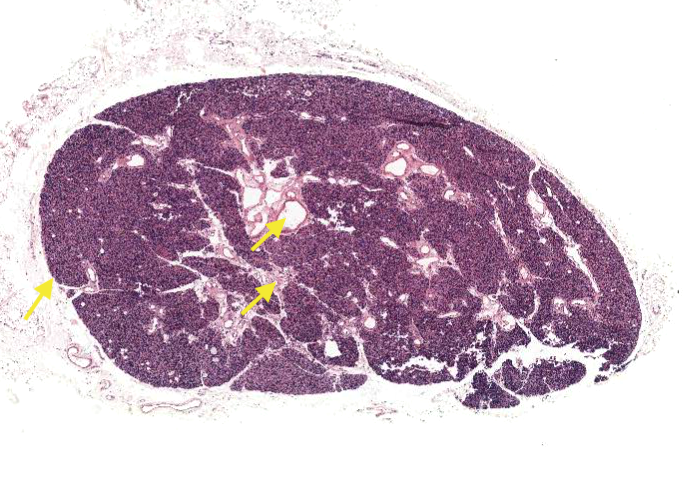
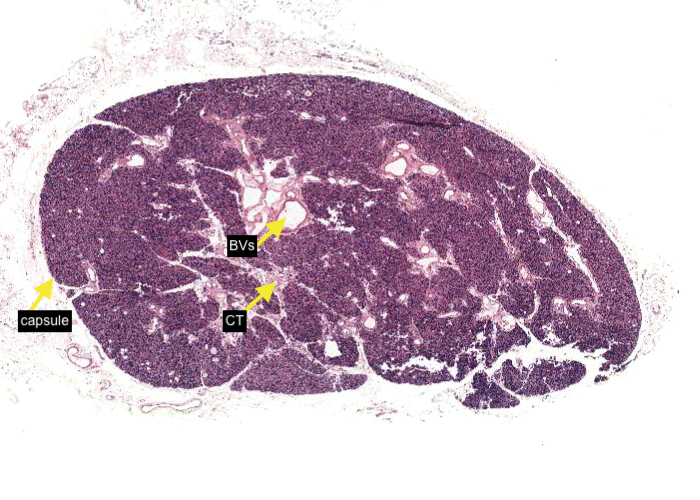
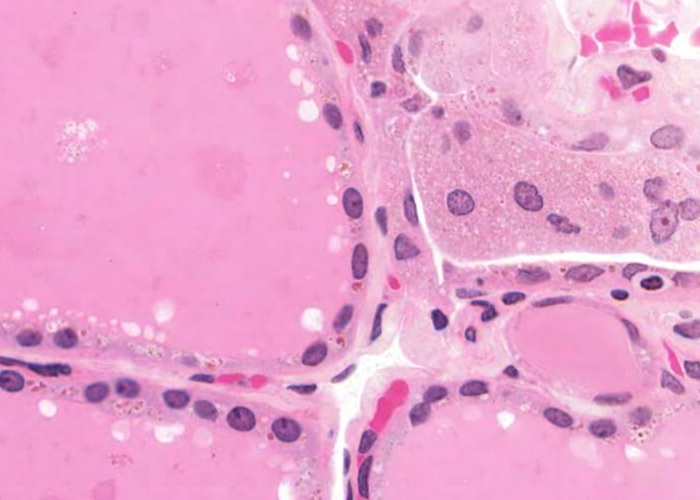
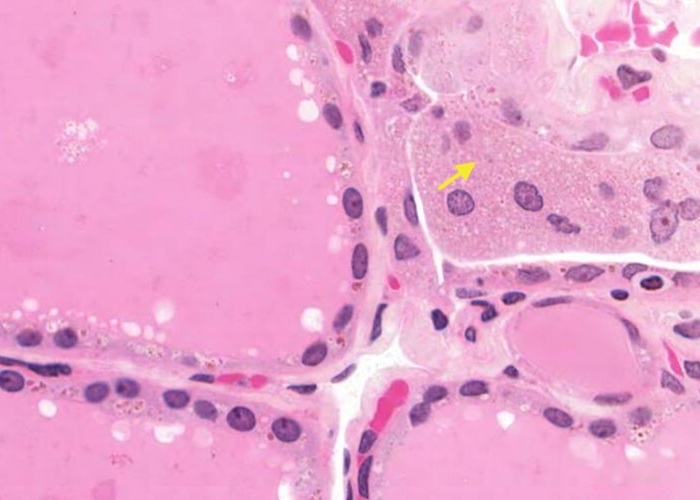
A very thin capsule separates the parathyroid from the thyroid. Connective tissue septa divide the gland into indistinct lobules containing densely packed cells. Numerous large blood vessels travel within these connective tissue elements.
Under medium magnification, examine the parathyroid section.
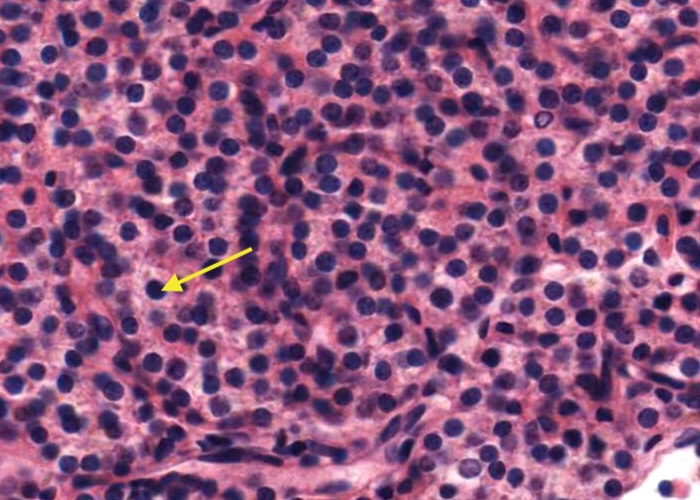
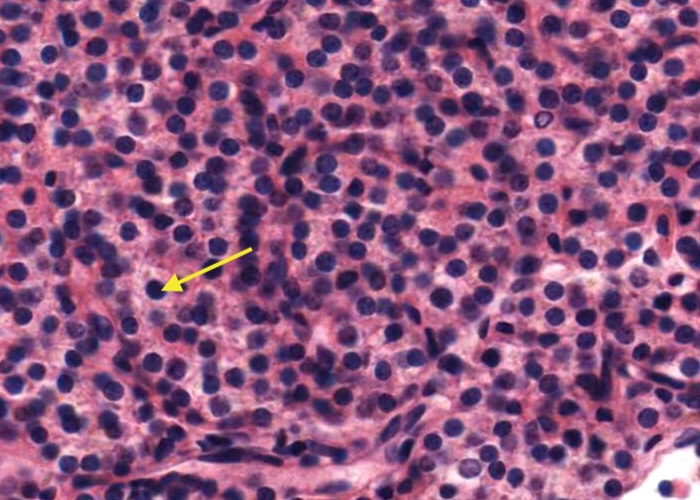
Most of the parenchymal cells are pale-staining chief cells = principal cells. They are small cells with central, round nucleus.
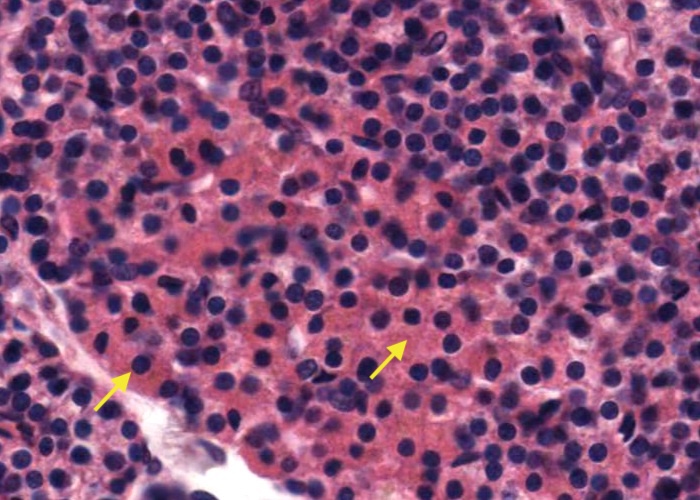
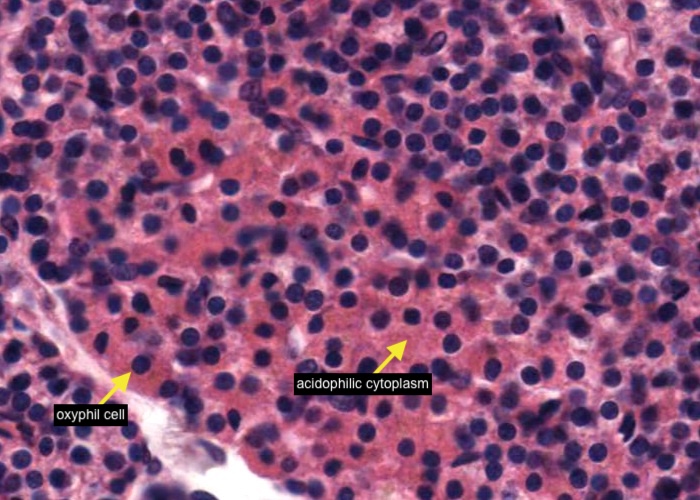
A much less numerous parenchymal cell of the parathyroid gland is the oxyphil cell. They are located in small clusters and have a distinctive acidophilic cytoplasm. They are large cells relative to their neighboring principal (chief) cells so there is a bit of extra space between them and the surrounding nuclei.
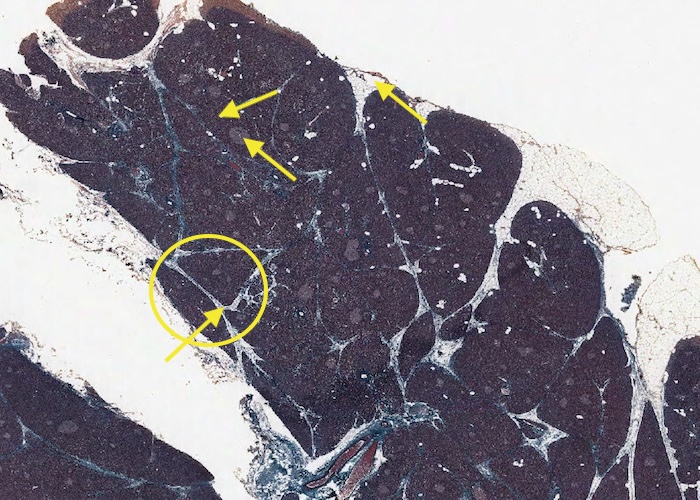
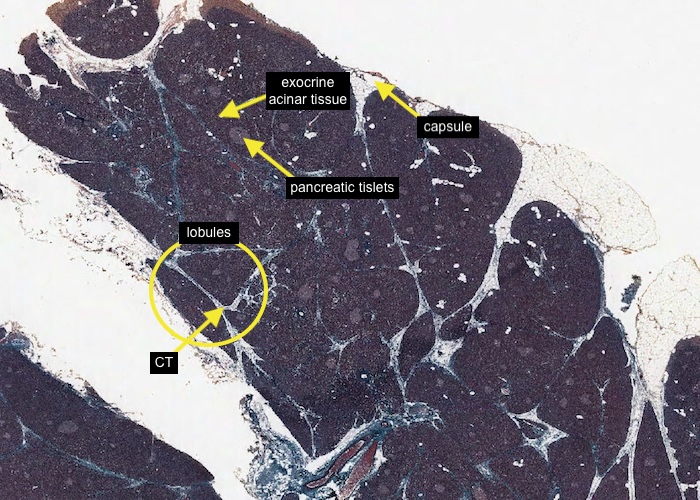
As is the case with most glands, the pancreas is divided into small lobules by septa of connective tissue penetrating the parenchymal cells from the capsule which has associated areas of adipose tissue.
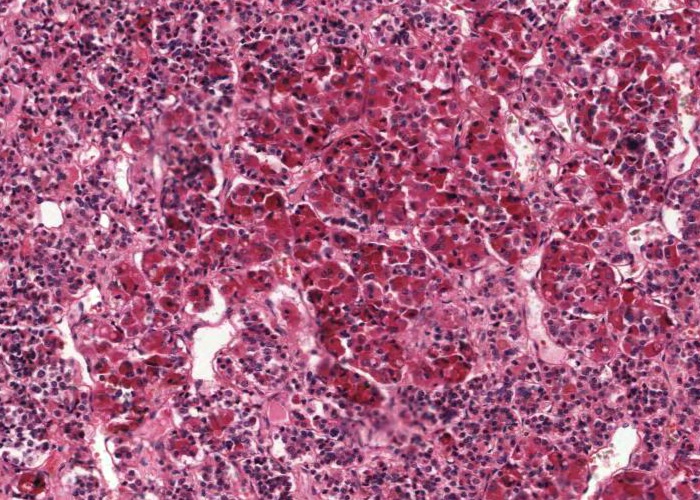
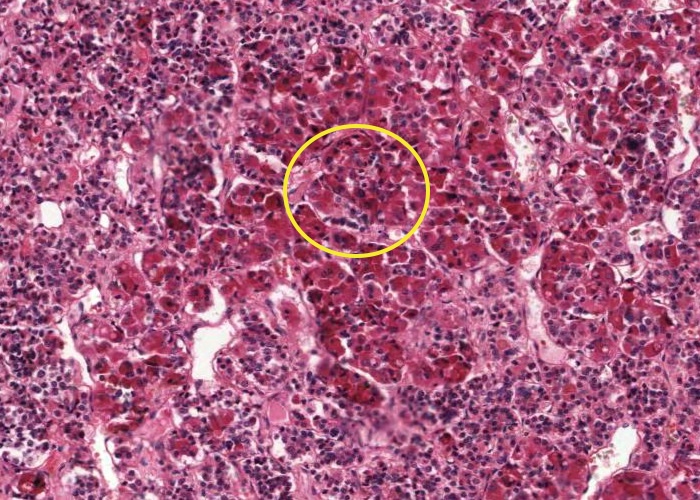
At this low magnification you can recognise pale-stained, pancreatic islets of endocrine cells (islets of Langerhan) within darker-stained, exocrine acinar tissue.
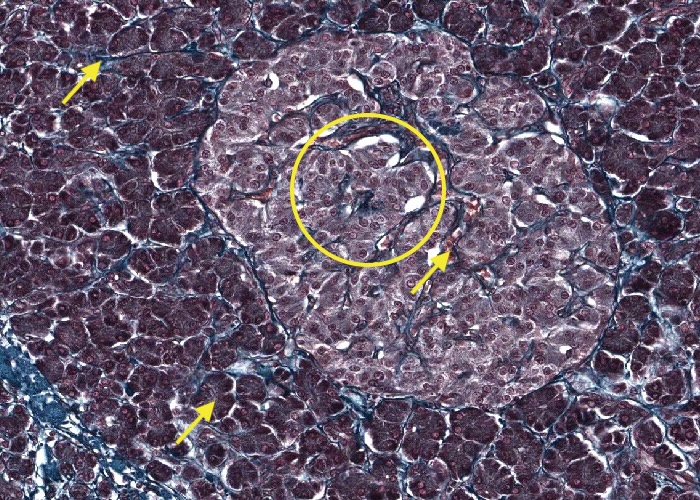
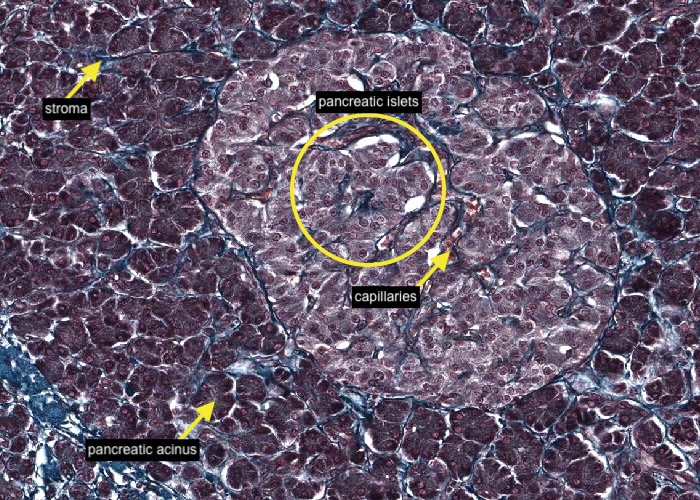
Connective tissue is stained blue or green. Note that the stroma encircles every pancreatic acinus (a cluster of exocrine cells) as well as each lobule. Note also, how well the pale-staining islet of Langerhan (pancreatic islet) stands out.
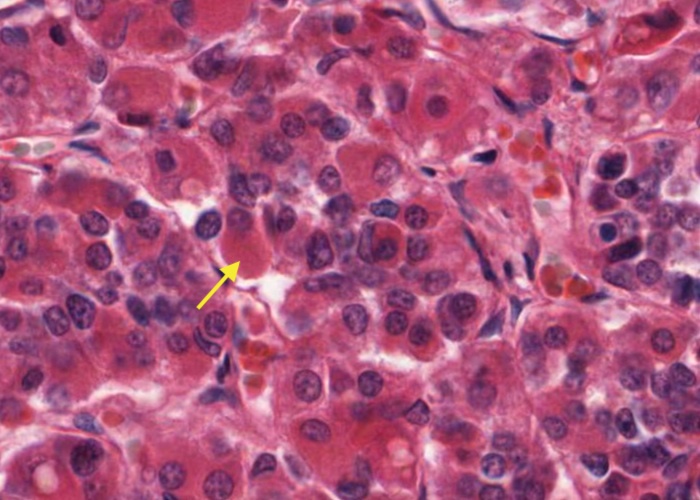
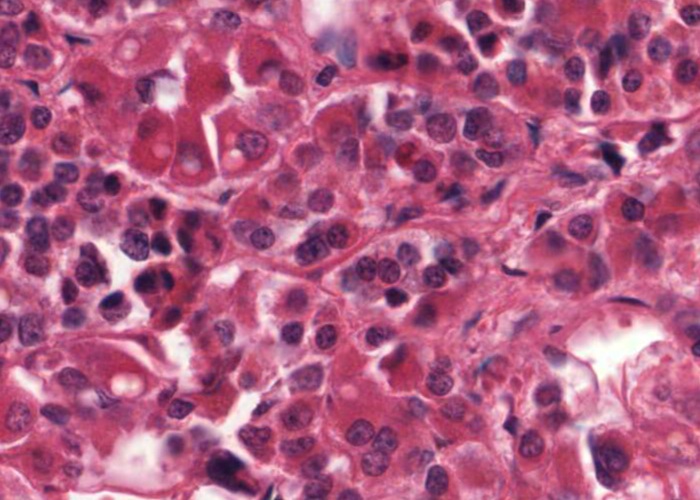
The islet is quite vascular with numerous capillaries as expected for endocrine tissue. Islets have four distinct types of secretory cells. By using appropriate stains it would be possible to distinguish them on the basis of size, nuclear appearance and position within the islet, but they all look the same here. The best way to distinguish them is immunohistochemically with antibodies to the individual hormones that they secrete i.e. insulin, glucagon, somatostatin and pancreatic polypeptide.
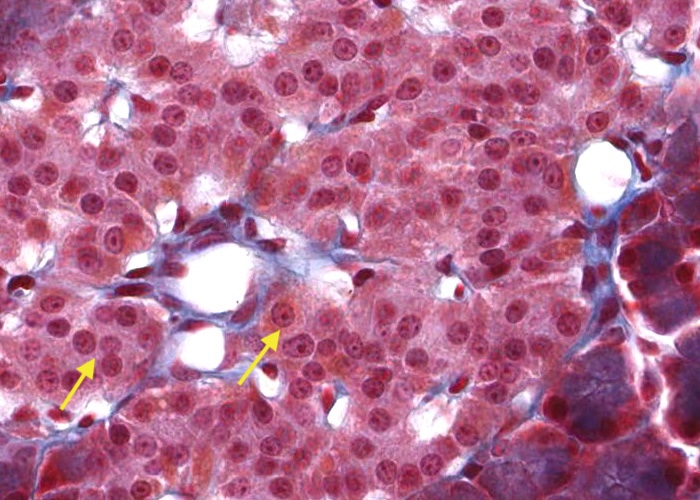
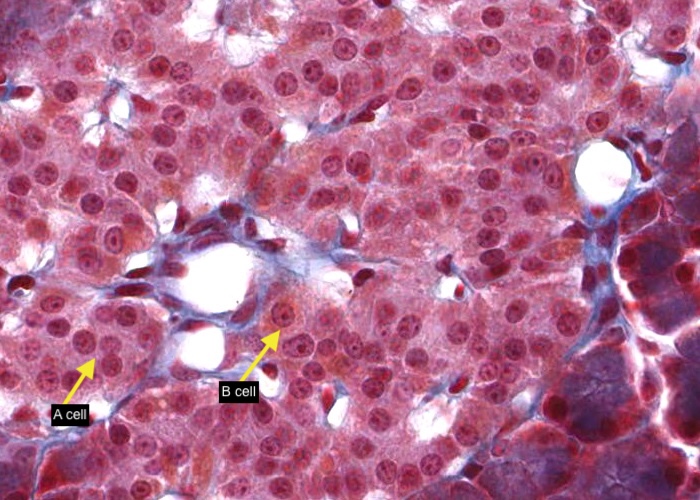
With this stain it is possible to distinguish 3 cell types - A (alpha), B (beta) and D (delta) cells:
an A cell is stained reddish/purple.
a B cell is stained orange.
a D cell stains blue.
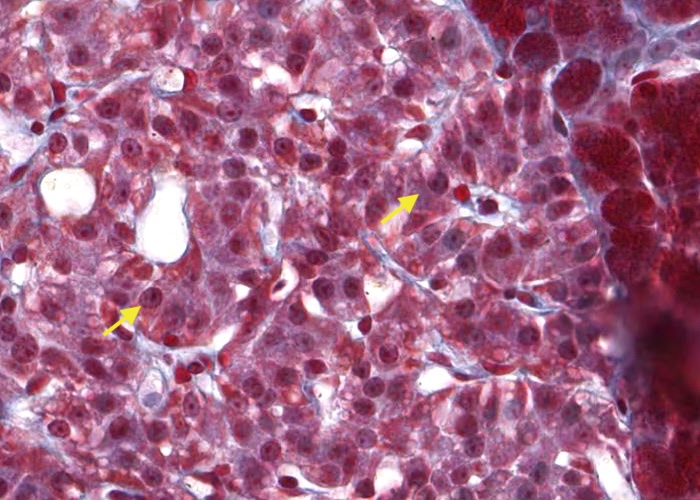
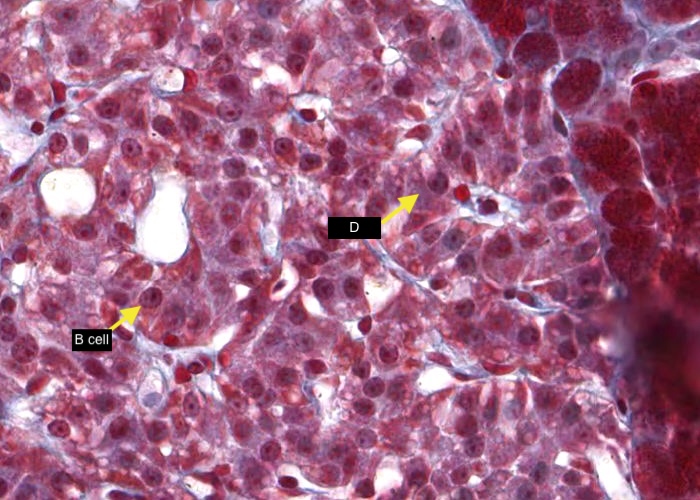
With this stain it is possible to distinguish 3 cell types - A (alpha), B (beta) and D (delta) cells:
an A cell is stained reddish/purple.
a B cell is stained orange.
a D cell stains blue.
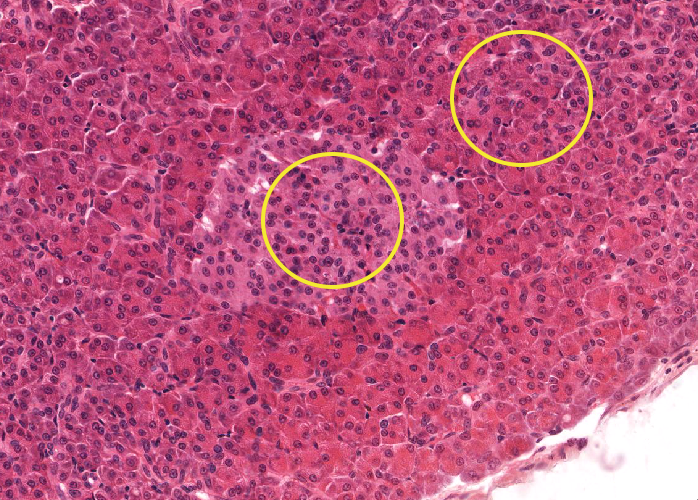
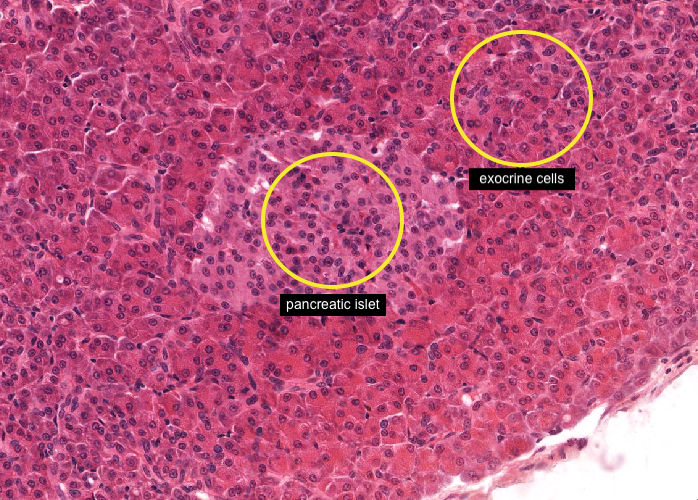
In H&E stained sections, the pancreatic islet is a cluster of smaller and lighter-stained endocrine cells embedded in darker-stained exocrine cells. It is not possible to distinguish the cells types within the pancreatic islet.
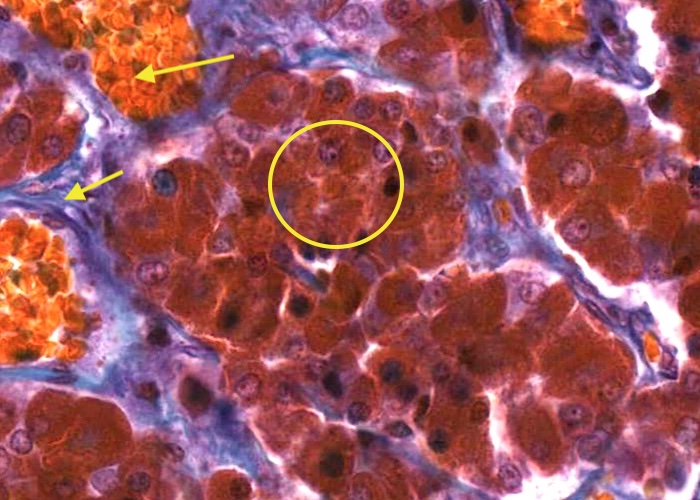
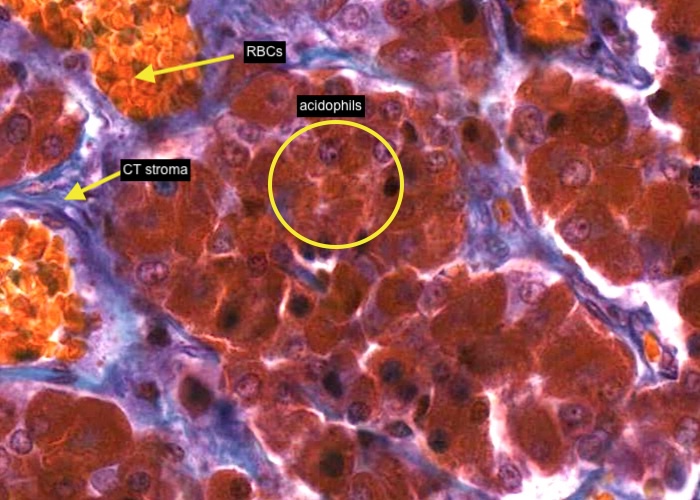
Based on the staining properties of the secretory granules within the cells, three types of parenchymal cells can be distinguished. The acidophils have an orange/brownish coloured cytoplasm. The cords of cells are supported by (bluish-stained) delicate connective tissue stroma. Sinusoidal capillaries are extensive and their red blood cells stain a bright yellow/orange.
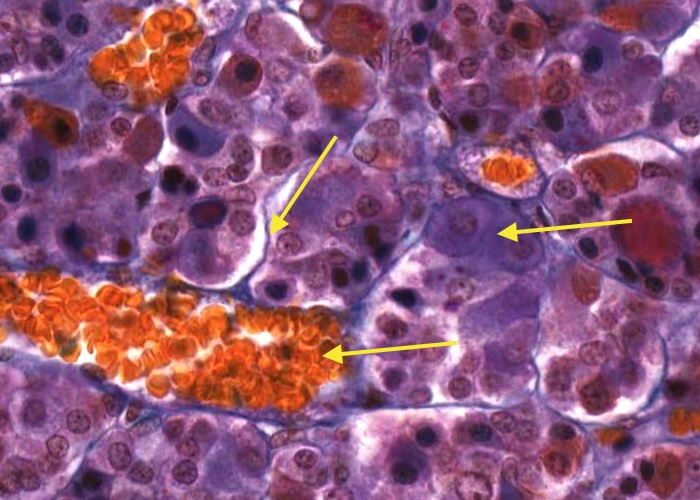
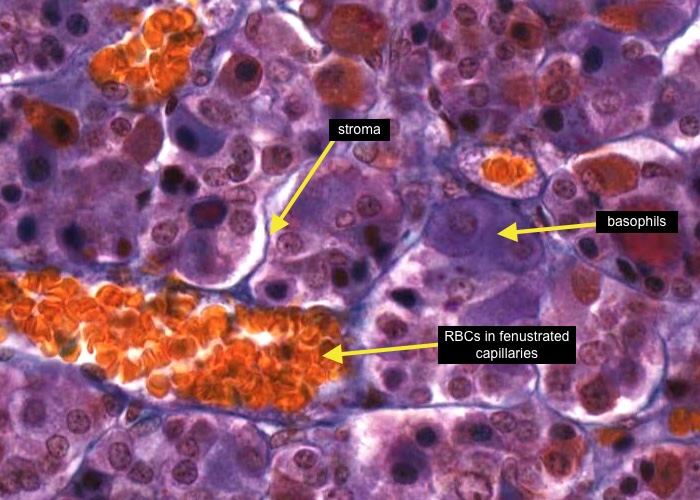
The basophils have a blue or purple stained cytoplasm. Again, notice that cords of cells are supported by delicate, thin, connective tissue stroma. Red blood cells within sinusoidal capillaries stain a bright yellow/orange.
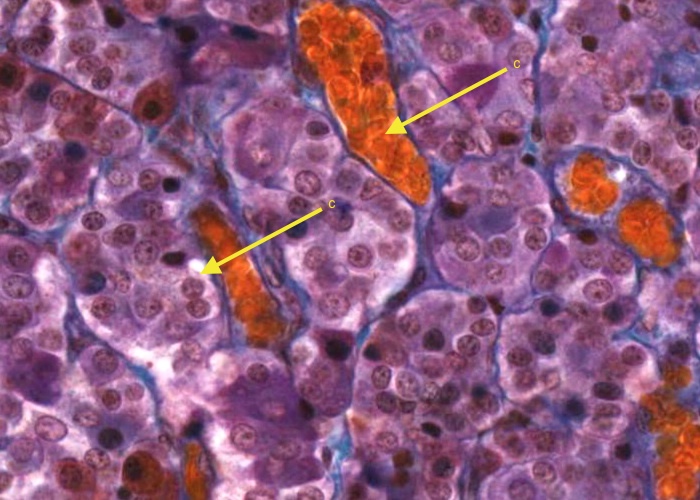
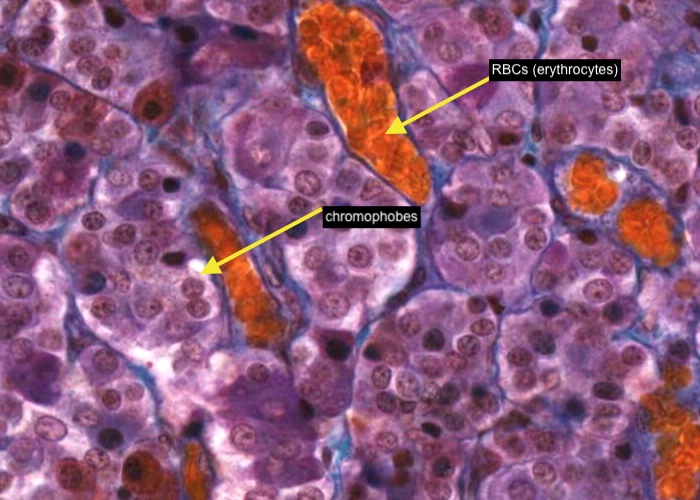
Chromophobes seem to lack a stainable cytoplasm, and the nuclei of adjacent chromophobes cluster closer together owing to the smaller size of these cells. Of course, you now know those intensely gold-coloured cells are erythrocytes (red blood cells).