haematology
1/74
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
75 Terms
what are the main functions of blood ?
transport, regulation, protection
what is the avg. volume of blood in an adult ?
4.5 - 5.5L
what is the pH of blood
alkaline - pH 7.4
what causes blood to appear bright red or darker ?
oxygen
bright red = oxygenates
darker = deoxygenated
what are the 2 main components of blood ?
plasma and cellular components
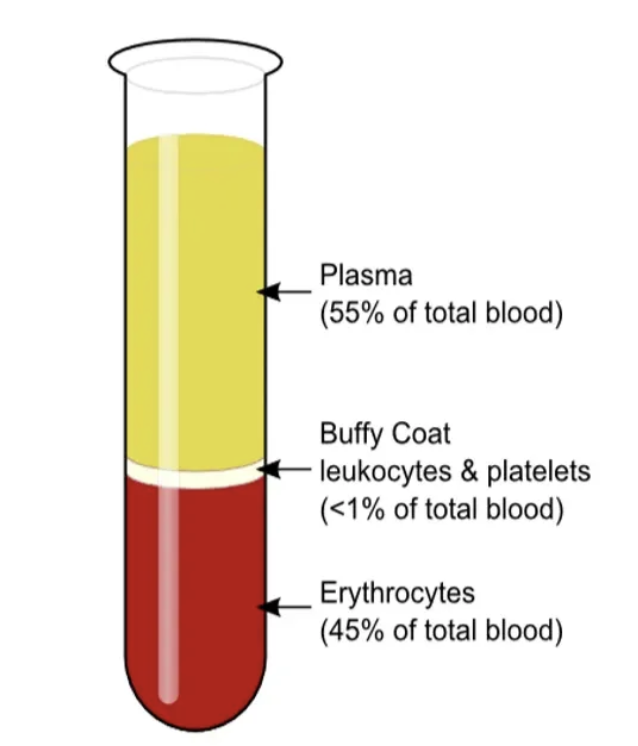
what are the 3 main cellular components of blood ?
platelets, leukocytes, erythrocytes
composition of plasma
90% water 10% solutes (eg. albumin, fibrinogen, globulins)
what % of blood do erythrocytes make up ?
45
what is unique about mature erythrocytes
anucleated, no organelles
what is the avg. lifespan of erythrocytes ?
120 days - high turnover rate
what protein do erythrocytes contain and what is its function ?
Hb - binds and transports oxygen
how many oxygen molecules can one Hb reversibly bind ?
4
why don’t erythrocytes use the oxygen they carry ?
generate ATP anaerobically
how many g of Hb per 100ml of blood ?
13 - 18
how and where are erythrocytes produced ?
haematopoiesis in red bone marrow - axial skeleton, girdles, proximal femur/humerus
what stimulates erythrocyte production ?
demand for oxygen - regulated by erythropoietin
what differentiates leukocytes (WBCs) from other blood cells ?
only “true cells” with nuclei and organelles
diapedesis
process by which leukocytes leave blood vessels to reach tissues
leukocytes account for what % of blood volume ?
1
mnemonic for leukocytes abundance
never let monkeys eat bananas
Neutrophils > Lymphocytes > Monocytes > Eosinophils > Basophils
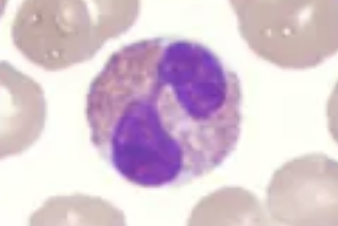
which leukocytes are granulocytes ?
neutrophils, eosinophils, basophils
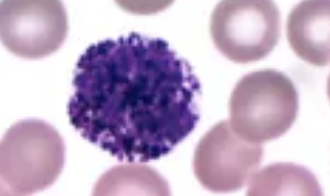
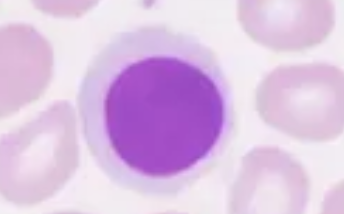
which leukocytes are agranulocytes ?
lymphocytes and monocytes
how and where are leukocytes produced ?
leukopoiesis in bone marrow
where do lymphocytes mature ?
thymus, bone marrow
what is the lifespan of leukocytes
granulocytes < 9 days
lymphocytes - hours to decades
monocytes - several months

neutrophil
eosinophil
basophil
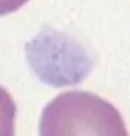
lymphocyte
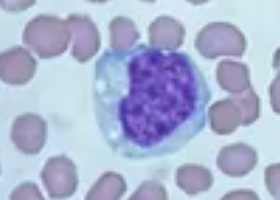
monocyte
T lymphocyte
directly responds to tumour and virus infected cells
B lymphocyte
produce specific antibodies against antigens
once leaving the bloodstream monocytes become…
macrophages
all leukocytes originate from…
early myeloid or lymphoid progenitors
what are platelets derived from ?
budding off megakaryocytes
lifespan of platelets
10 days
what do platelet granules contain ?
calcium - important for clotting
what is the primary function of platelets ?
initiate clotting at sites of vessel injury
platelet
haemostasis
localised multistep process to stop bleeding
what are the key steps in haemostasis ?
starts with platelet plug
ends with fibrin blood clot
what triggers the coagulation cascade ?
intrinsic (contact) or extrinsic (tissue factor) pathways
the intrinsic and extrinsic pathways converge to form
common coagulation pathway
outline the common coagulation pathway
factor X converted to Xa (active form)
prothrombin (factor II) converted to thrombin (IIa)
converts fibrinogen (factor I) to fibrin monomers
factor XIIIa cross links to form soft fibrin clot
what guides neutrophils to site of infection ?
chemotaxis
what is extravasation ?
adhesive interaction between neutrophils and capillary walls
what leukocytes originate from myeloid progenitors ?
neutrophils, monocytes, eosinophils, basophils
what leukocyte originates from lymphoid progenitors ?
lymphocytes
what is erythrocytosis
persistently elevated Hb and RBC count
Hb thresholds for erythrocytosis
> 185g/L in males
165 in females
4 types of erythrocytosis
relative - plasma conc.
apparent - raised haematocrit
idiopathic - no clear mechanism
absolute - congenital or acquired
what is anaemia ?
low RBCs / Hb
reduced oxygen carrying capacity
what Hb levels indicate anaemia ?
< 130 g/L in males
120 in non pregnant females
what is haemorrhagic anaemia ?
significant loss of RBCs leading to decreased haemoglobin
but normal erythropoiesis
acute haemorrhagic anaemia
sudden and often traumatic eg. stab wound
chronic haemorrhagic anaemia
slow / over long period of time eg. internal bleed
causes of decreased erythrocyte production
iron/B12 deficiency
renal failure
bone marrow failure
drugs
haemolytic anaemia
premature RBC destruction
causes of haemolytic anaemia
allo and auto immune responses
haemolytic uraemic syndrome
prolonged mechanical trauma
jaundice is caused by
buildup of bilirubin in blood
what causes WBC disorders ?
oncogenic mutations
cause disregulation of WBC production and function
examples of WBC disorders
leukaemia, lymphoma, multiple myeloma, MDS
leukaemia
accumulation of abnormal WBCs in blood or bone marrow
lymphoid or myeloid lineage
lymphoma
malignancy of lymphoid origin
restricted to lymphoid organs
acute vs chronic leukaemia
acute - rapid progression, accumulation of ‘blast cells’, children
chronic - slower, mature but dysfunctional
blast cells
immature blood cells that are precursors to mature blood cells
general symptoms of leukaemia
fatigue, weight loss, infections, bruising, enlarged lymph nodes
leukaemia treatments
chemotherapy, radiotherapy, bone marrow/stem cell transplant
what happens in hypercoagulable states ?
increased clotting risk (e.g. DVT, thrombosis)
what happens in hypocoagulable states ?
increased bleeding tendency
clot breakdown by fibrinolysis
haemophilia
inherited bleeding disorder due to missing clotting factors
haemophilia A is a deficiency of
factor VIII
haemophilia B is a deficiency of
factor XI
who is more commonly affected by haemophilia ?
males - X linked recessive
treatment for haemophilia A and B
Octacog alfa (A)
Nonacog alfa (B)
desmopressin
recombinant proteins