Lecture 8 - dissecting pain: from measurement to management
1/63
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
64 Terms
why should we focus on pain anyways?
pain is the symptoms of greatest concern to patients → most likely lead to use health services
pain is heavily influenced by psychosocial processes
what is the primary purpose of pain
warns self or others of tissue damage/injury/disease; evokes care
what are some negative consequences of pain
poor health behaviours
loss of employment / income
depression, fear, anxiety
social isolation
sleep disorders
martial and family dysfunction
what is the specificity theory of pain
pain is directly proportional to the amount of tissue damage
describe how the specificity theory of pain works
upon injury, pain messages originate in nerves associated with damaged tissue and travel to the spinal cord
a signal is then sent to
a motor nerve, and
the brain, where pain is perceived
describe the problems of the specificity theory of pain
assumption of one-to-one correspondence to injury/disease
unfortunate practices
focus on pharmacological, surgical, or other medical interventions to control pain
what are unfortunate practices as specified in the purely biomedical approach to pain
blaming the patient
assuming psychiatric disorders
intentional faking of symptoms
what is the gate-control theory of pain
pain is not directly proportional to tissue damage
describe how the gate-control theory of pain works
a neural neural pain gate in the spinal cord opens or closes to modulate pain signals in the brain
involves inhibitor and projector neurons that respond to sensory input and send certain signals to the brain
what is phantom limb pain
phantom limb pain is pain experienced in an amputated limb; classified as neuropathic pain
what is the neuromatrix theory
an extension of the gate control theory of pain
a widespread network of neurons (distributed throughout the brain and spinal cord) generates a pattern that is felt as a whole body possessing a sense of self
for physical pain, what opens the gate
extent of injury
inappropriate activity level; inactivity
for physical pain, what closes the gate
medication
counter stimulation (massage, heat)
for emotional pain, what opens the gate
anxiety or worry
tension
depression
relationship problems
for emotional pain, what closes the gate
positive emotions
relaxation
social support
for cognitive pain, what opens the gate
focusing on pain
boredom
for cognitive pain, what closes the gate
distraction
concentration
involvement and interest in activities
describe the evidence that support the gate-control theory
in studies with multiple pain conditions, objective findings have no clinically significant correlation to pain levels
AMA: in up to 85% of individuals who report back pain, no pain-producing pathology can be identified
describe how the neuromatrix theory works
a network is responsible for generating bodily sensations including pain (pain is produced in the CNS)
pain can occur in the absence of signals from sensory nerves
various parts of the NS work together to respond to stimuli from the body and/or environment to create the experience of pain
each sensation is marked by a unique neurosignature or patterns of activation of the neuromatrix
what is the current state of the research on the possible etiology of phantom limb pain
may be triggered by other types input, lack of normal sensory input, or incongruence between types of input due to lack of limb
what are the theories of pain that are more supported by evidence
gate-control theory of pain
neuromatrix theory of pain
what is the definition of pain
an unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage
what is the main problem with trying to define pain or trying to detect pain
it is impossible to definitively know whether another creature’s subjective experience is like our own
what are the ways we can measure pain
self-report measures of pain
nonverbal measures of pain
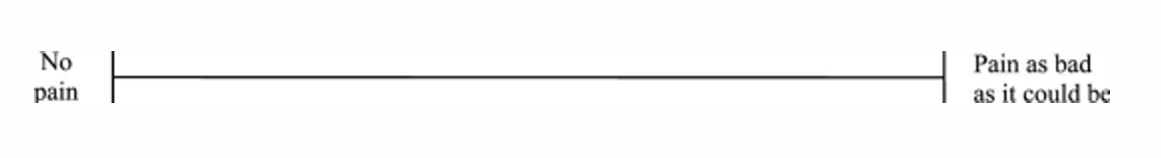
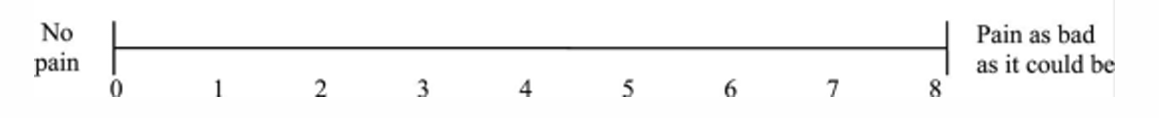
what are the types of pain rating scales
graphic rating scales
verbal rating scales (adjectives)
numerical rating scales
what are graphic ratings scales like
what are verbal ratings scales like

what are numerical rating scales like
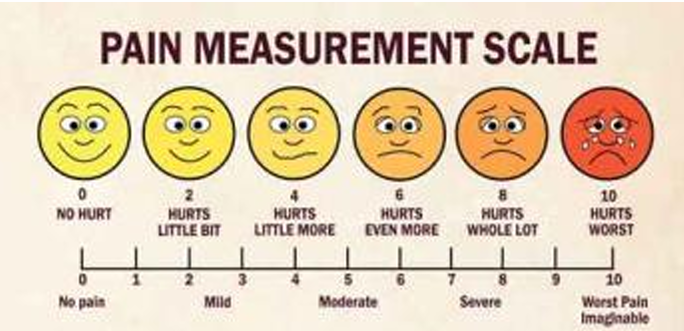
what is a valid tool for assessing pain specifically in young people
wong-baker faces pain rating scale
what is the significance about the phantom limb pain
pain cannot originate from the tissue that is supposedly causing the pain
what are the nonverbal measures of pain
look at pain behavioursw
what are pain behaviours
observable behaviours that occur in response to pain
what are some examples of pain behaviours
facial and audible expression of distress
distortions in posture or gait
negative affect (mood, anxiety, depression)
avoidance of activity
how do emotions affect pain
positive emotions appear to reduce pain
negative emotions tend to worsen (and result from) pain
people with chronic pain tend to also experience… what types of emotions
high levels of depression, anxiety, and/or anger; high levels of these emotions are associated with high levels of subsequent pain/disability
how are pain and stress linked
pain is stressful
stress and produce pain and worsen the pain experience
what are some ways to cope with pain
maladaptive coping
catastrophizing
adaptive coping
acceptance
what are the good ways to cope with pain
adaptive coping
acceptance
what are the bad ways to cope with pain
maladaptive coping
catastrophizing
what is maladaptive coping
destructive thinking; helplessness
what is catastrophizing
frequent, magnified negative thoughts about pain
magnification, rumination, and helplessness
what are the consequences of using catastrophizing to cope
catastrophizing increases as pain intensity increases
plays a major role in transitioning from acute to chronic pain
what is adaptive coping
relaxation
distraction
redefinition of pain (reappraisal)
readiness to change, taking an active role
what is acceptance
being inclined to engage in activities despite the pain and disinclined to control or avoid the pain
what are the benefits of having high levels of pain acceptance
pay less attention to their pain
have greater self-efficacy for performing daily tasks
function better
use less pain medication than those with low pain acceptance
how does social support affect pain
social support attenuates feelings of pain
describe the importance of social networks in pain coping
the health and well-being of one’s social network affects pain outcomes
if close people have depression → increased chance to experience pain
what is a solution for the negative consequences that come with one’s social network having negative health
treat the social network of that individual
what is social pain
the experience of pain as a result of interpersonal rejection or loss
what are some examples of social pain
rejection from social group
bullying
loss of a loved one
is social pain adaptive and explain why or why not
yes
signals when social relationships are threatened
how is social pain and physical pain described linguistically
“hurt feelings”
“broken-hearted”
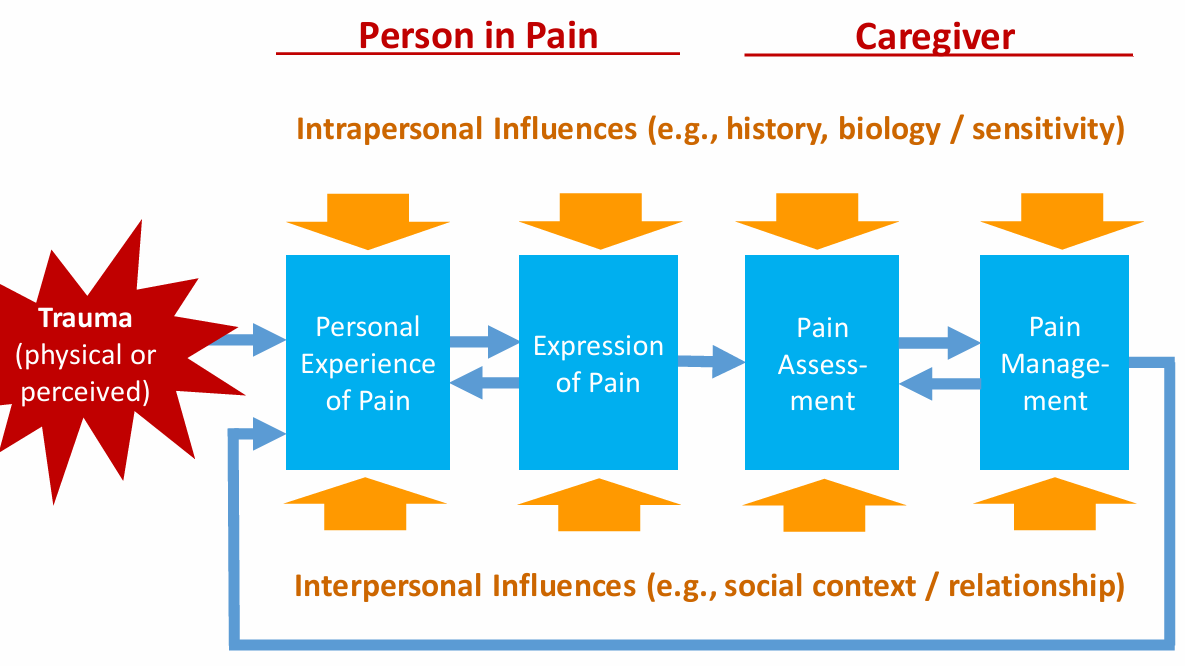
describe the social communication model of pain
when there is one or more person present how does pain unfold, caregiver is some sort of individual that brings care or comfort
person in pain: trauma → ← personal experience of pain → expression of pain →
caregiver: pain assessment → ← pain management → personal experience of pain
all factors are influenced by intrapersonal and interpersonal factors
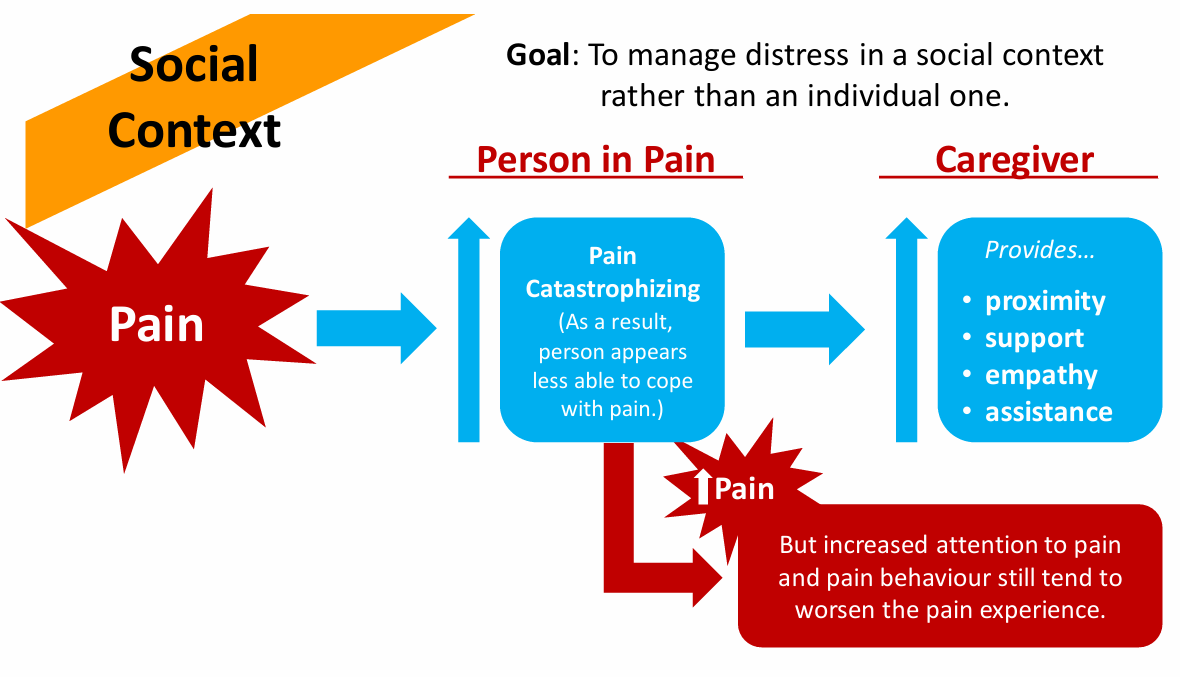
what is the goal of the communal coping model of pain catastrophizing
to manage distress in a social context rather than an individual one
describe the communal coping model of pain catastrophizing
in a social context…
pain → person in pain: pain catastrophizing → more pain
caregiver provides…
proximity
support
empathy
assistance
what is the primary treatment option for social pain
acetaminophen (tylenol)
what are the clinical interventions for pain
surgical interventions
chemical treatments (pharamacological)
stimulation therapies
physical therapy & rehabilitation
what are some examples of pharmacological interventions for pain
peripherally active analgesics (tylenol)
centrally acting analgesics / opioids (morephine)
local anaesthetics (novocaine)
what is the problem of using just medical methods for controlling pain and especially chronic pain, and why
not enough
psychosocial factors play an important role in pain experience and in the transition from acute to chronic pain, therefore treating psychological factors and challenges can be essential
is social pain the same as physical pain? describe evidence for and against
similar but not exactly the same
negative social experiences rely on the same neural system supporting the affective component of physical pain (dorsal cingulate cortex dACC and anterior insula AI)
dACC is associated with the degree of distress / pain; the AI is assoicated with emotional processing

describe the best approach to treating chronic pain
a combination of pharmacological and non-pharmacological methods
what are the purposes of psychological treatments for pain
aim to help clients…
reduce pain frequency and intensity
improve emotional adjustment to pain
increase social and physical activity
reduce use of analgesic drugs
describe the multidisiciplinary approach to pain treatment
treating chronic pain with just one method is less likely to succeed than a combined program
what is the significance of the multidisciplinary approach to pain treatment
further underscores the importance of a biopsychosocial approach