MOD 8 -T and L Spine Fractures Lecture
1/49
Earn XP
Description and Tags
50 question-and-answer flashcards covering mechanisms, presentations, treatments, and complications of traumatic, osteoporotic, pathological, disc, sacrum, and coccyx fractures.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
50 Terms
What are the most common sites for traumatic spine fractures?
T12, L1, and L2 (thoracolumbar region).

What are common causes of pathological spine fractures?
Osteoporosis and metastases.

What spinal structure can herniate and lead to pain?
Intervertebral discs.
What function is retained with a fracture at T1–T4?
Full head, neck, shoulders, and arm movement.
What limitations occur with a T1–T4 fracture?
No lower body/leg movement and sensory loss below the nipples.
What function is retained with a T5–T9 fracture?
Same as above, plus some upper body strength.
What function is retained with a T10–L1 fracture?
Full upper body movement and possible partial lower body/leg movement.
What is a Chance fracture?
A horizontal fracture through the spine, commonly from Seatbelt Syndrome.

What other injuries often accompany traumatic spine fractures?
Fractures of the calcaneus and sternum.

What is the typical mechanism for a Chance fracture (Traumatic Fracture of Spine/ Seatbelt syndrome)?
Seatbelt restrains pelvis while torso is thrown forward (flexion/distraction).

What are general mechanisms for traumatic spinal fractures?
Flexion/distraction, compression (burst fractures), and dislocation.
How are traumatic fractures treated?
Bracing after healing begins; surgery if unstable or healing is delayed.
Name possible complications of traumatic spinal fractures.
Abdominal wall rupture, injury to bowel, spleen, aorta, uterus, sigmoid colon, or spinal cord injury.

What happens to the vertebrae in osteoporosis-related fractures?
The vertebra collapses, often anteriorly, causing kyphosis.
What is the cause of osteoporosis-related fractures?
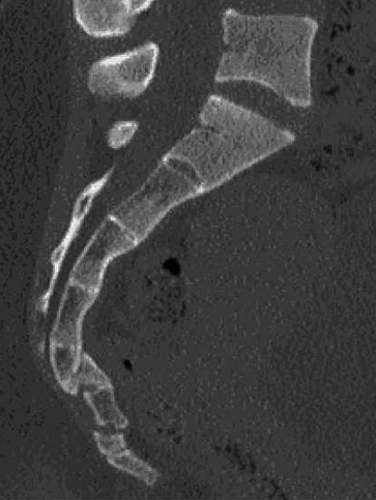
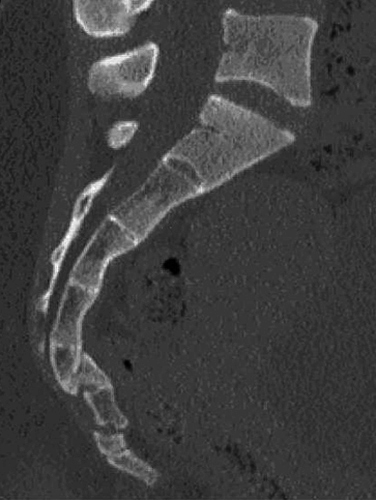
Bone matrix loss exceeds new bone formation (image shows T12 compressed).

How are osteoporosis-related fractures treated?
Kyphoplasty/vertebroplasty (cement injection), or surgery for stability and mobility.

What are complications of osteoporosis-related spine fractures?
Persistent pain and loss of height.
What causes pathological fractures of the spine?
Disease processes like cancer, osteomyelitis, or bone cysts.

What is the etiology of pathological fractures?
Weakened bone structure fractures with minimal or no trauma.

How are pathological fractures treated?
With bracing or surgery depending on severity.
What are complications of pathological fractures?
Inability to bear weight and nerve root compression.

What are symptoms of intervertebral disc herniation?
Pain, numbness, tingling, and bladder issues.
What causes disc herniation?
Compression or distraction forces, often from heavy lifting with poor technique.

What is the first line of treatment for disc injuries?
Rest, anti-inflammatories, and possibly steroids.
When is surgery considered for disc injuries?
When conservative treatments fail.

What complications can result from disc herniation?
Worsening pain, nerve compression, bowel or bladder dysfunction.
What causes sacrum and coccyx fractures?
Direct falls or impacts.
What is the typical appearance of sacrum and coccyx fractures?
Linear traumatic fractures; coccyx may displace anteriorly.
How is a coccyx fracture typically treated?
Rest and natural healing.
How is a sacral fracture treated?
Surgical stabilization may be required.
What are potential complications of sacral or coccyx fractures?
Ongoing pain and deformity.
Why is the thoracolumbar region (T12–L2) especially vulnerable to fractures?
It’s a transition zone between the relatively rigid thoracic spine and the more mobile lumbar spine.
What is Seatbelt Syndrome and how is it related to spinal fractures?
Injury pattern where a seatbelt restrains the pelvis but torso moves forward, causing a Chance fracture.
What type of spinal fracture is commonly associated with flexion-distraction injuries?
Chance fracture.
What are burst fractures and what mechanism causes them?
Vertebral body is crushed in all directions, typically caused by axial compression.
Which abdominal organs can be affected by spinal trauma?
Small bowel, spleen, aorta, uterus, sigmoid colon, abdominal wall/muscles.
What neurological complication is associated with vertebral fractures?
Spinal cord injury or nerve root compression.
What is the risk if a pathological fracture compromises the vertebral body?
Structural collapse, loss of mobility, and potential spinal instability.
What is the purpose of kyphoplasty or vertebroplasty?
To inject bone cement into a fractured vertebra to restore strength and reduce pain.
When is surgery indicated for vertebral fractures?
When the fracture is unstable or does not heal with conservative treatment.
Why might a brace be used in spinal fracture recovery?
To immobilize the spine and allow healing.
What symptoms suggest nerve involvement from a disc injury?
Numbness, tingling, pain radiating down the legs (sciatica), bladder or bowel changes.
What is the typical cause of disc herniation in younger individuals?
Lifting heavy objects improperly or sudden twisting motions.
What is the long-term risk of untreated disc herniation with nerve compression?
Chronic pain, loss of function, and in severe cases, permanent neurological damage.
What common activity might aggravate a coccyx fracture during healing?
Sitting, especially on hard surfaces.
Why might a sacral fracture require surgery, but a coccyx fracture usually does not?
Sacral fractures can affect pelvic stability and nerves; coccyx injuries are usually stable.
What kind of deformity might result from sacral or coccygeal injury?
Abnormal angulation or protrusion of the tailbone.
How can you distinguish between an osteoporotic and a pathological fracture on imaging?
Osteoporotic fractures usually involve vertebral compression; pathological fractures may show lytic lesions or abnormal bone structure.
What underlying disease processes are commonly associated with pathological fractures?
Metastatic cancer, bone infections (osteomyelitis), and bone cysts.
What’s a key difference in trauma requirement between osteoporotic and pathological fractures?
Osteoporotic fractures may occur with minor trauma; pathological fractures can happen with little to no trauma.