Anterior Segment Diseases (conjunctiva, cornea, uvea, and lens)
1/220
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
221 Terms
What are the main categories of conjunctivitis discussed?
Viral; Bacterial; Gonococcal; Chlamydial; Allergic.
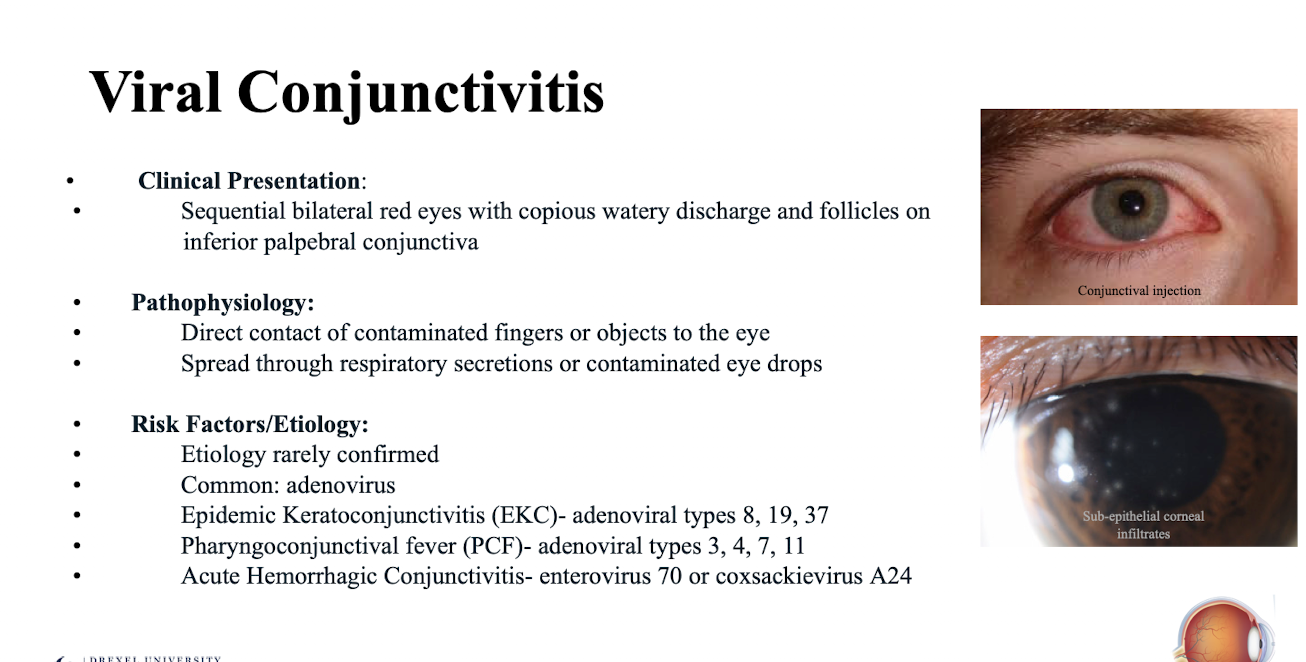
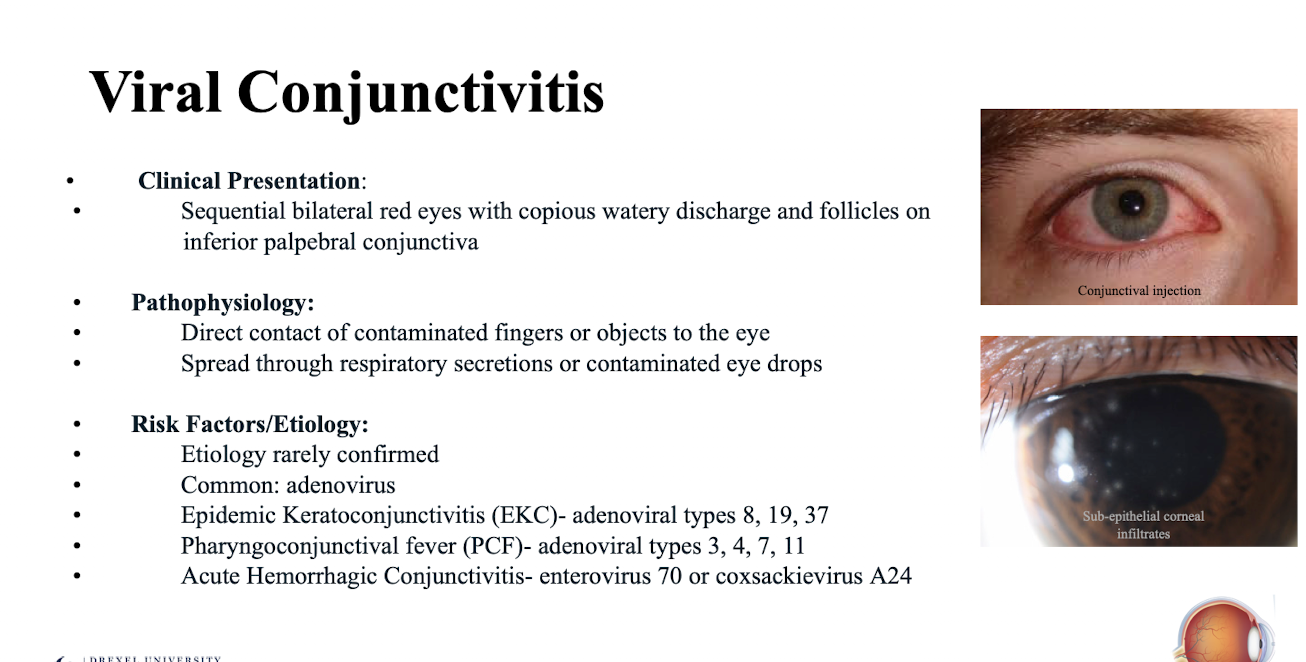
What is the typical clinical presentation of viral conjunctivitis?
Sequential bilateral red eyes with copious watery discharge and follicles on inferior palpebral conjunctiva.
Patients typically say one eye was infected then it spread to the other eye
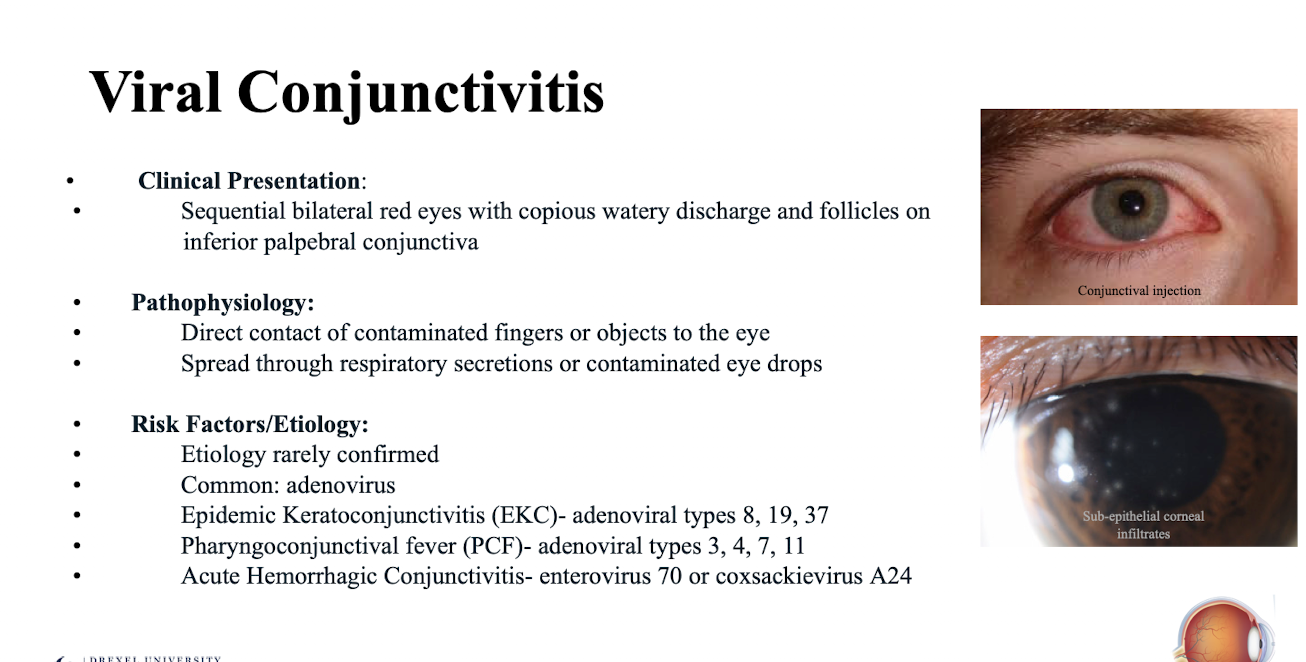
What is the pathophysiology of viral conjunctivitis?
Direct contact of contaminated fingers or objects to the eye; spread through respiratory secretions or contaminated eye drops.
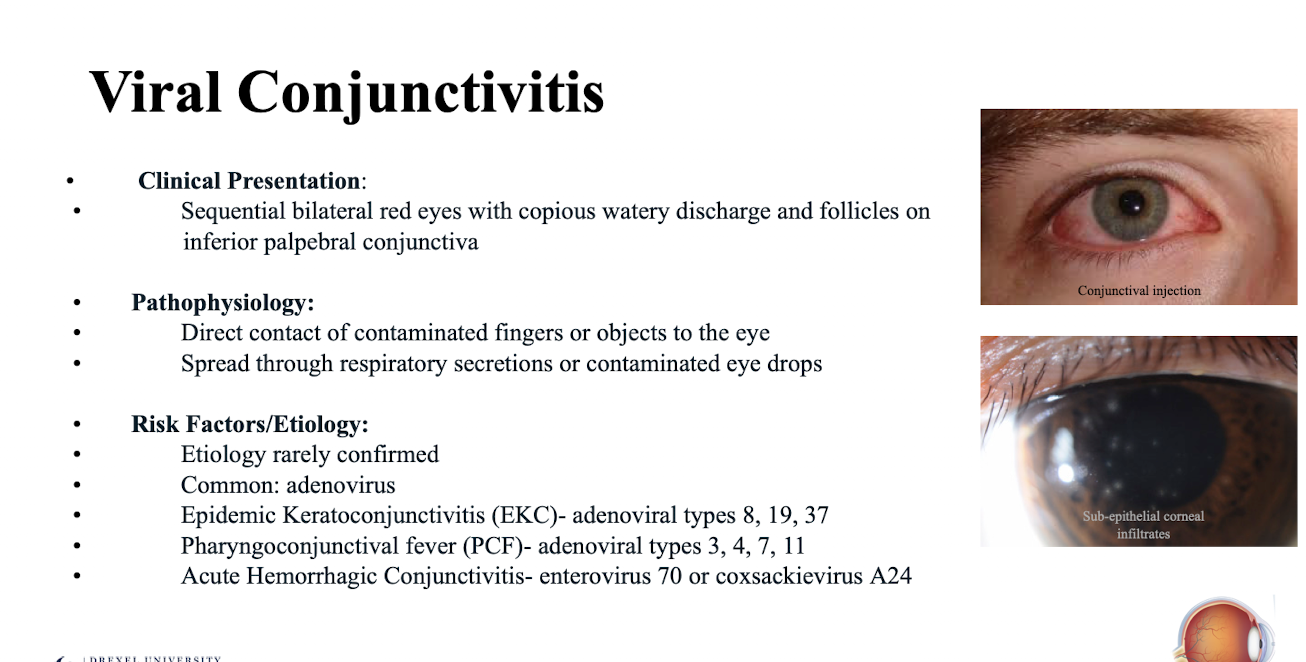
What is the most common etiology of viral conjunctivitis?
Adenovirus. Treated empirically because actual etiology is rarely confirmed
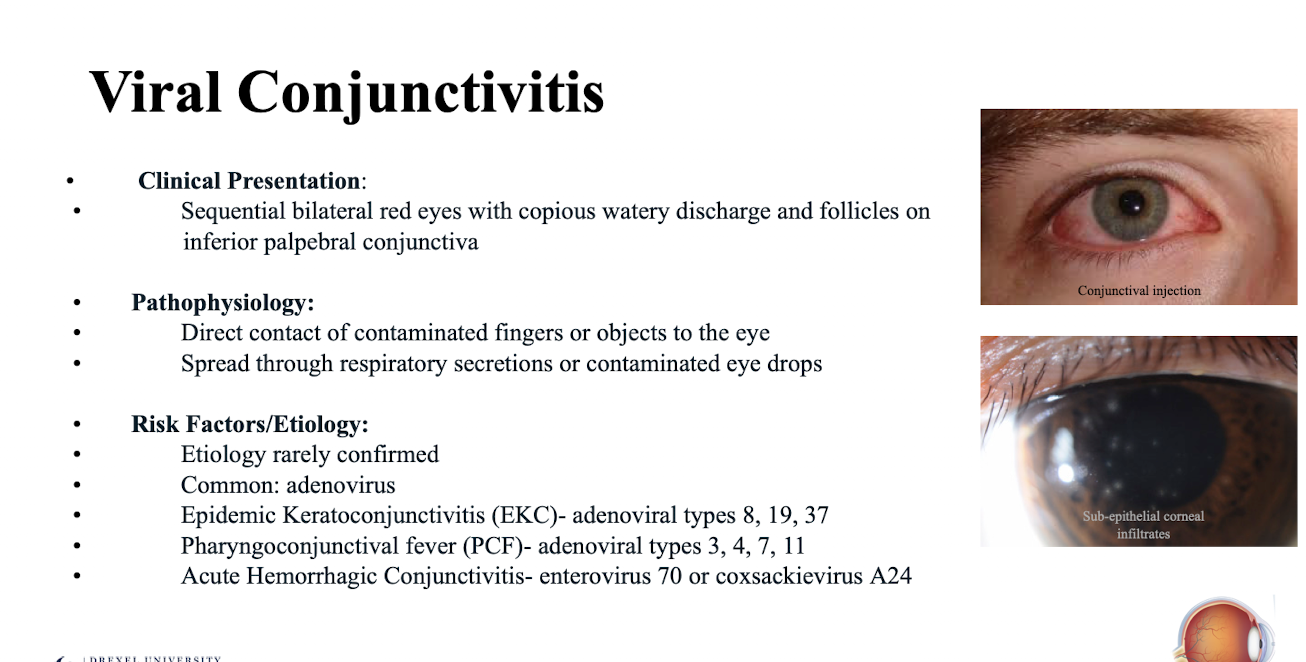
What adenoviral types are associated with Epidemic Keratoconjunctivitis (EKC)?
Adenoviral types 8; 19; 37.
What adenoviral types are associated with Pharyngoconjunctival fever (PCF)?
Adenoviral types 3; 4; 7; 11.
Which viruses cause Acute Hemorrhagic Conjunctivitis?
Enterovirus 70 or coxsackievirus A24.
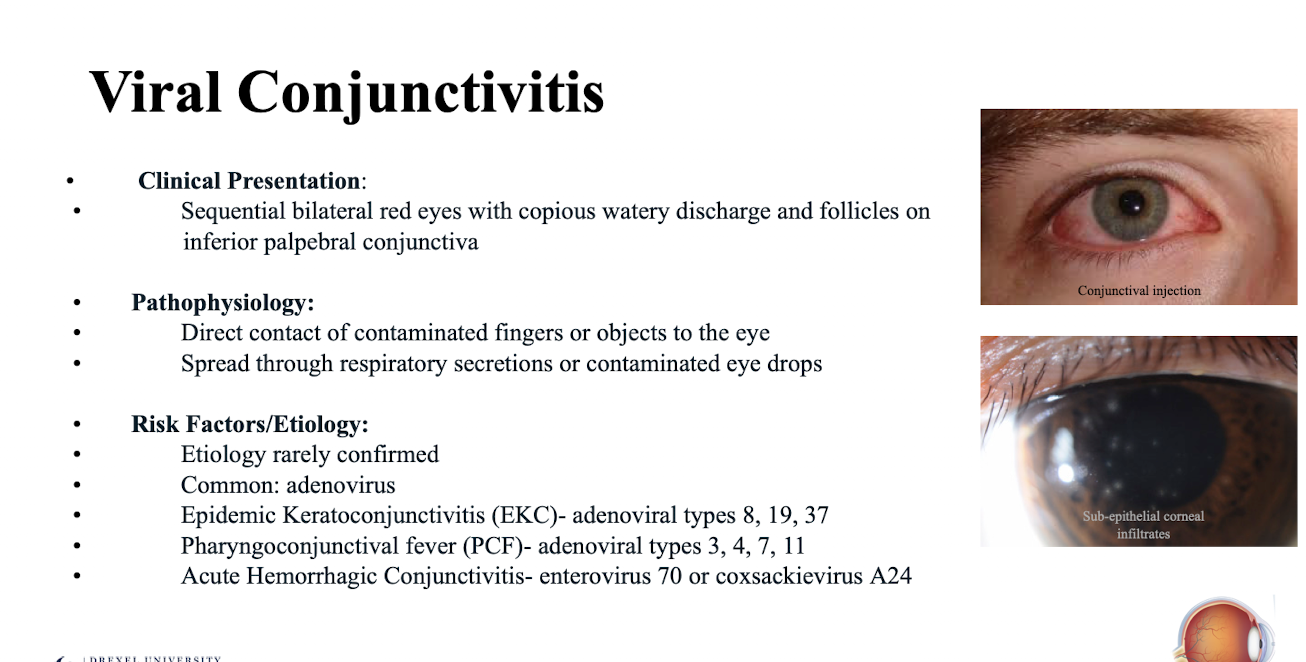
What specific findings should be assessed during diagnostic evaluation for viral conjunctivitis using a slit lamp?
Conjunctival hyperemia; follicles (pull lower lid down); pseudomembranes (pull lower lid down); and subepithelial infiltrates
What extra-ocular structures should be palpated during the diagnostic evaluation for viral conjunctivitis?
Preauricular; submandibular; and sublingual lymph nodes.
What is the general treatment/management strategy for viral conjunctivitis?
Palliative. (Self resolving virus has to run its course)
What palliative measures are recommended for viral conjunctivitis?
Cold compresses; artificial tears PRN OU.
When are topical steroids recommended in the treatment of viral conjunctivitis?
If there are subepithelial infiltrates; to prevent corneal scarring.
What are examples of topical steroids used for viral conjunctivitis with subepithelial infiltrates?
FML 0.1% TID OU x 1-2 weeks with taper;
Loteprednol 0.5% TID OU x 1-2 weeks with taper.
What hygiene education is crucial for minimizing the spread of viral conjunctivitis?
Frequent handwashing; linen hygiene encouraged.
Eduacte on contagious nature of condition
When should a patient with viral conjunctivitis be referred to an ECP for monitoring and follow up?
Within 1-2 weeks.
What is the clinical presentation of bacterial conjunctivitis?
Unilateral red eye with purulent (yellow/green) discharge; may have eyelid matting (eyelashes that are stuck together)
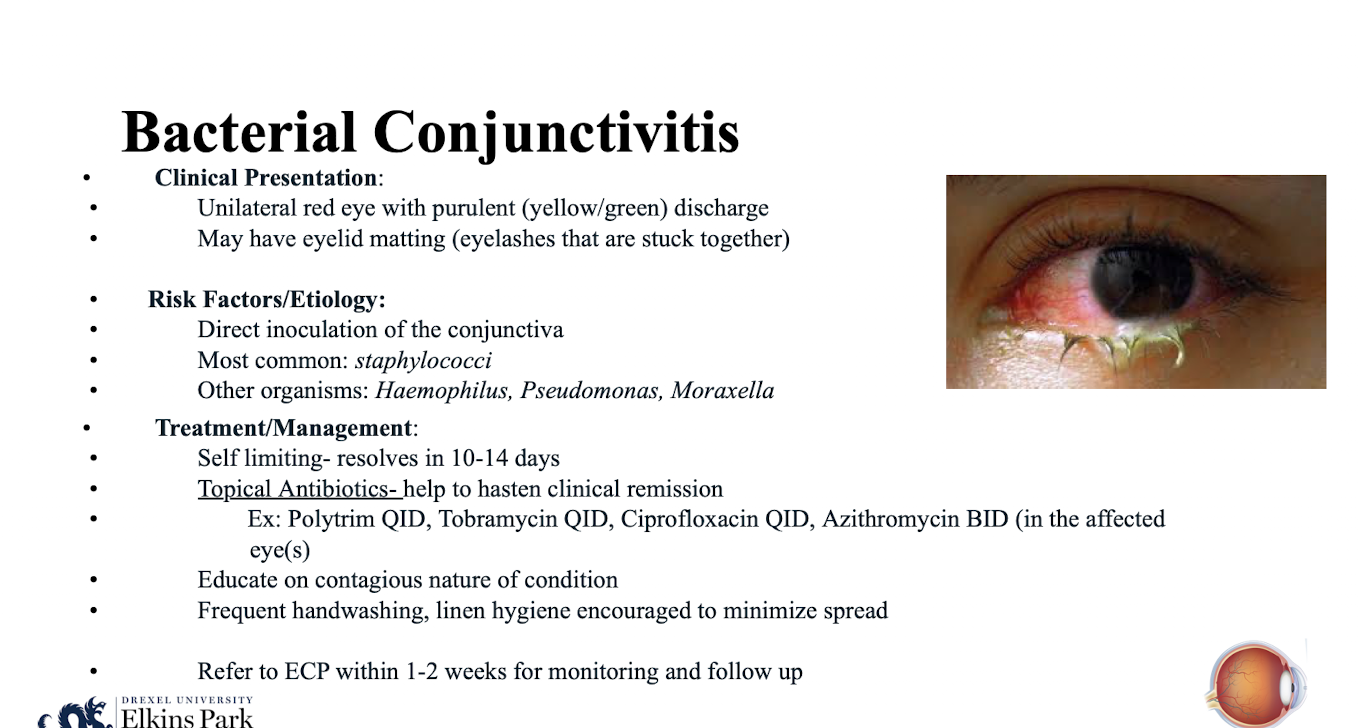
What is the most common etiology of bacterial conjunctivitis?
Staphylococci.
Direct inoculation of the conjunctiva
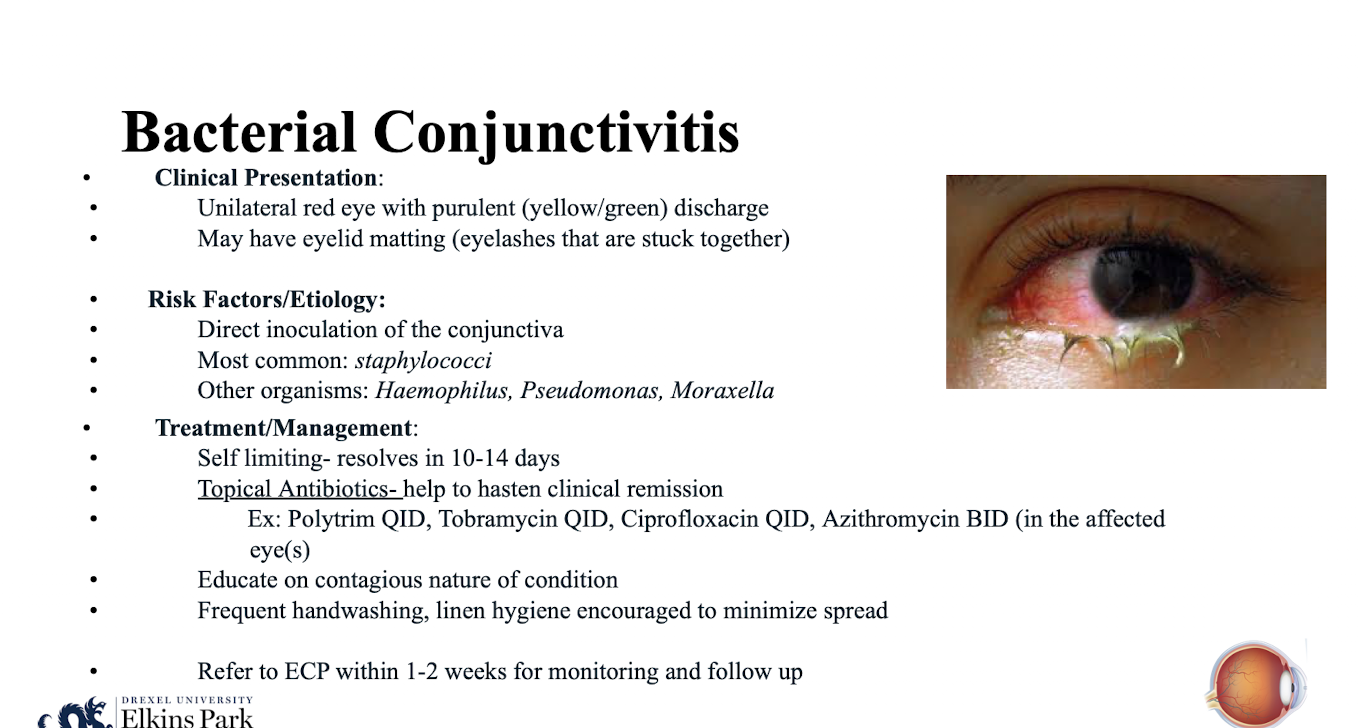
What other organisms commonly cause bacterial conjunctivitis?
Haemophilus; Pseudomonas; Moraxella.
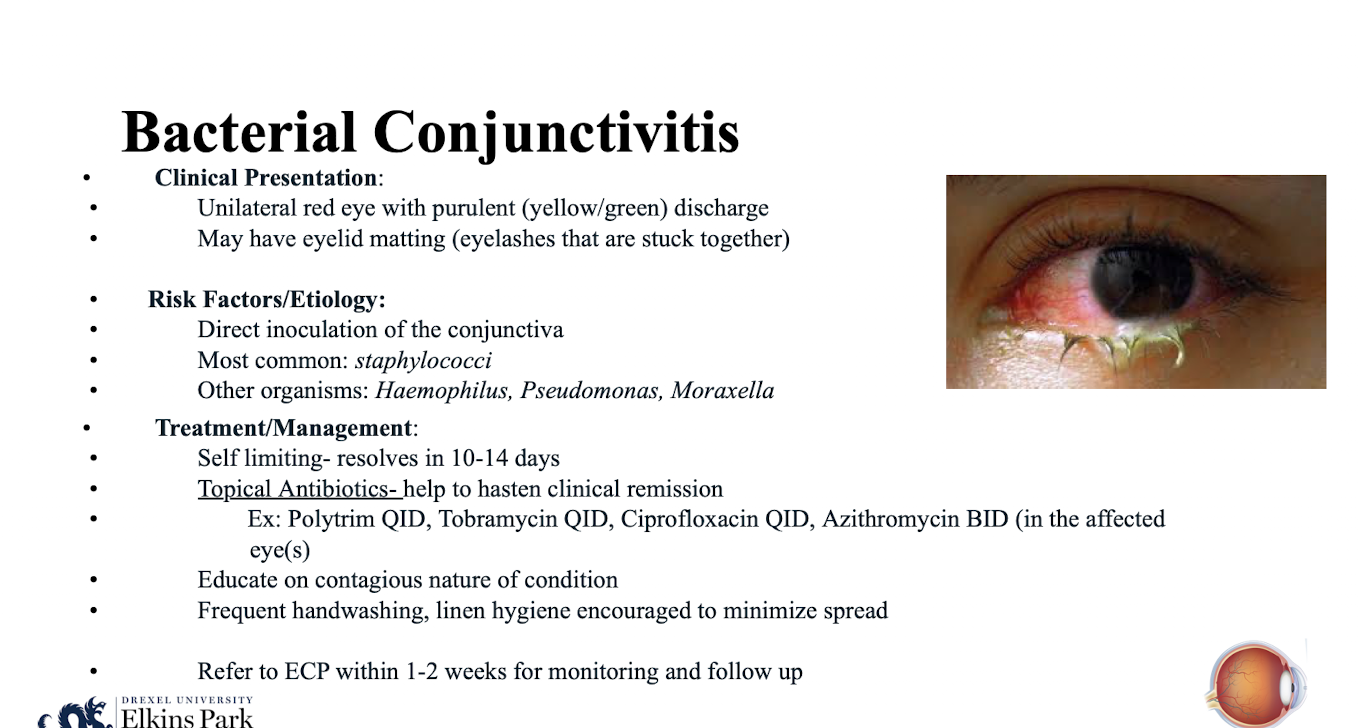
What is the typical natural course of bacterial conjunctivitis if left untreated?
Self limiting- resolves in 10-14 days.
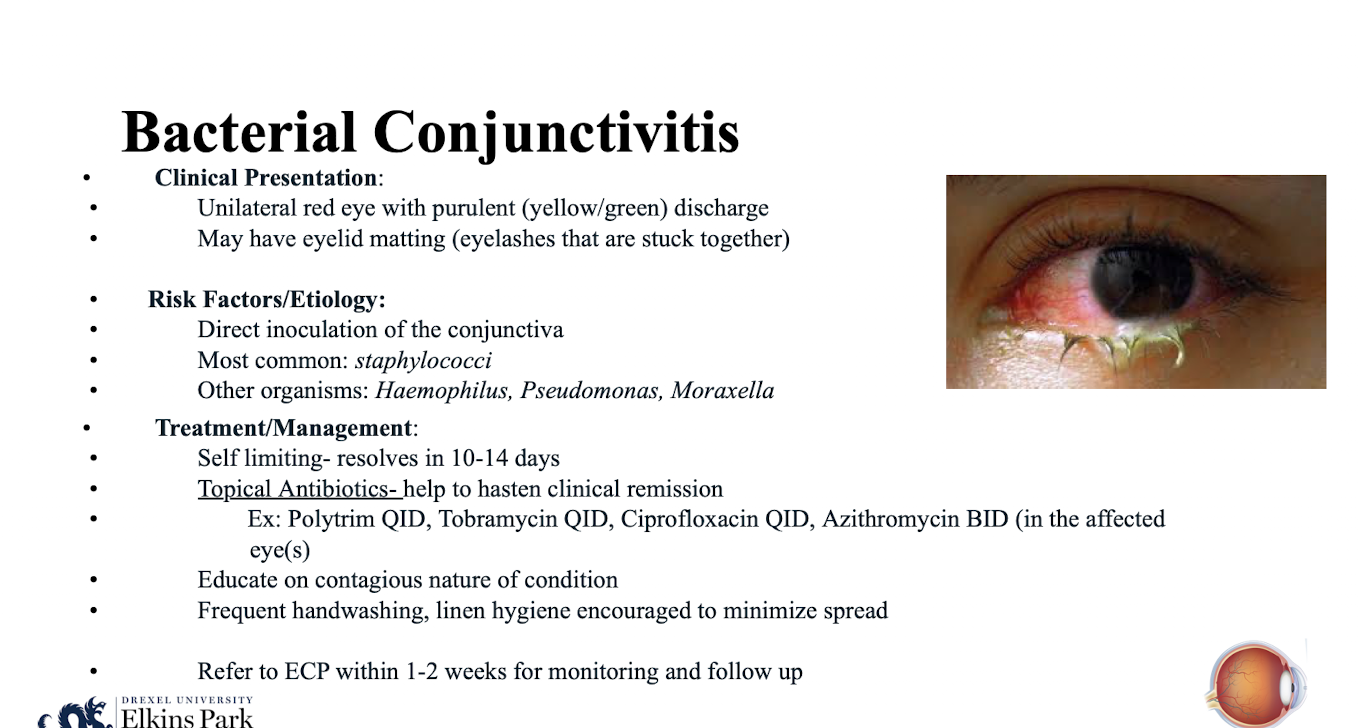
How do topical antibiotics aid in the management of bacterial conjunctivitis?
They help to hasten clinical remission.
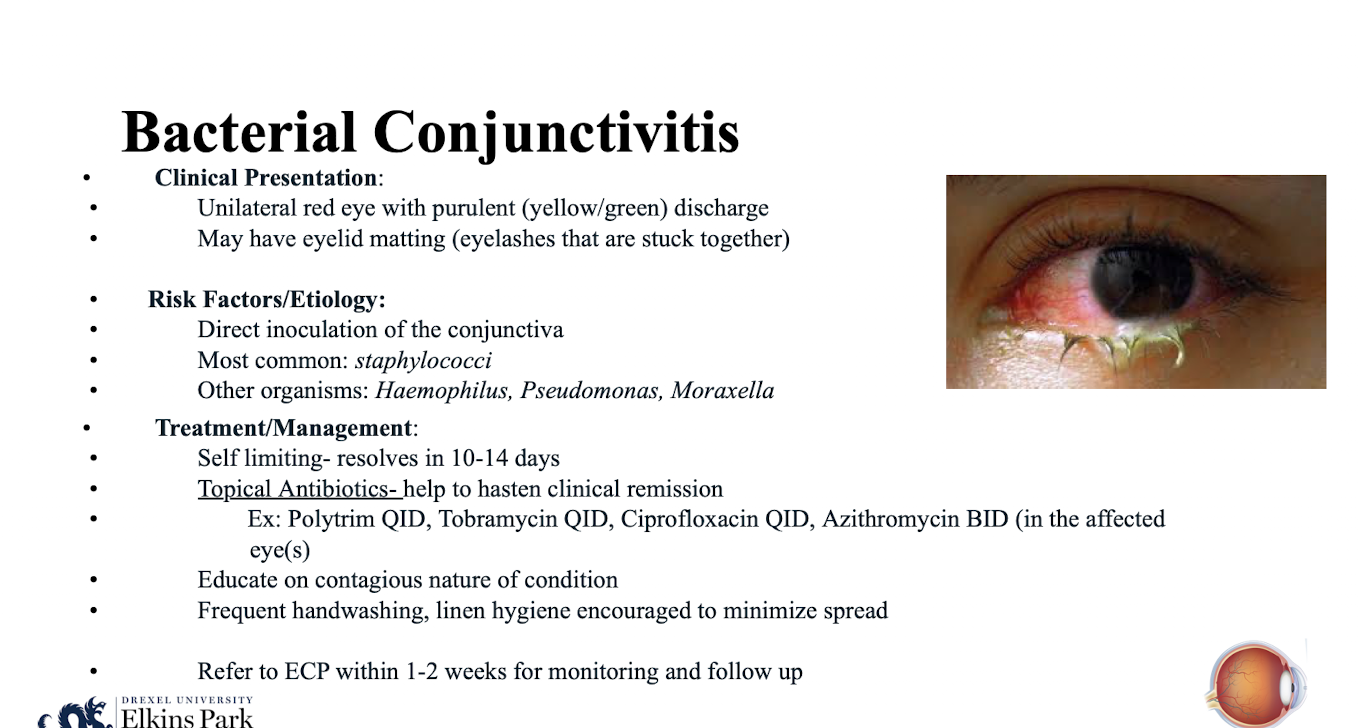
What are examples of topical antibiotics used for bacterial conjunctivitis?
Polytrim QID; Tobramycin QID; Ciprofloxacin QID; Azithromycin BID (in the affected eye(s)).
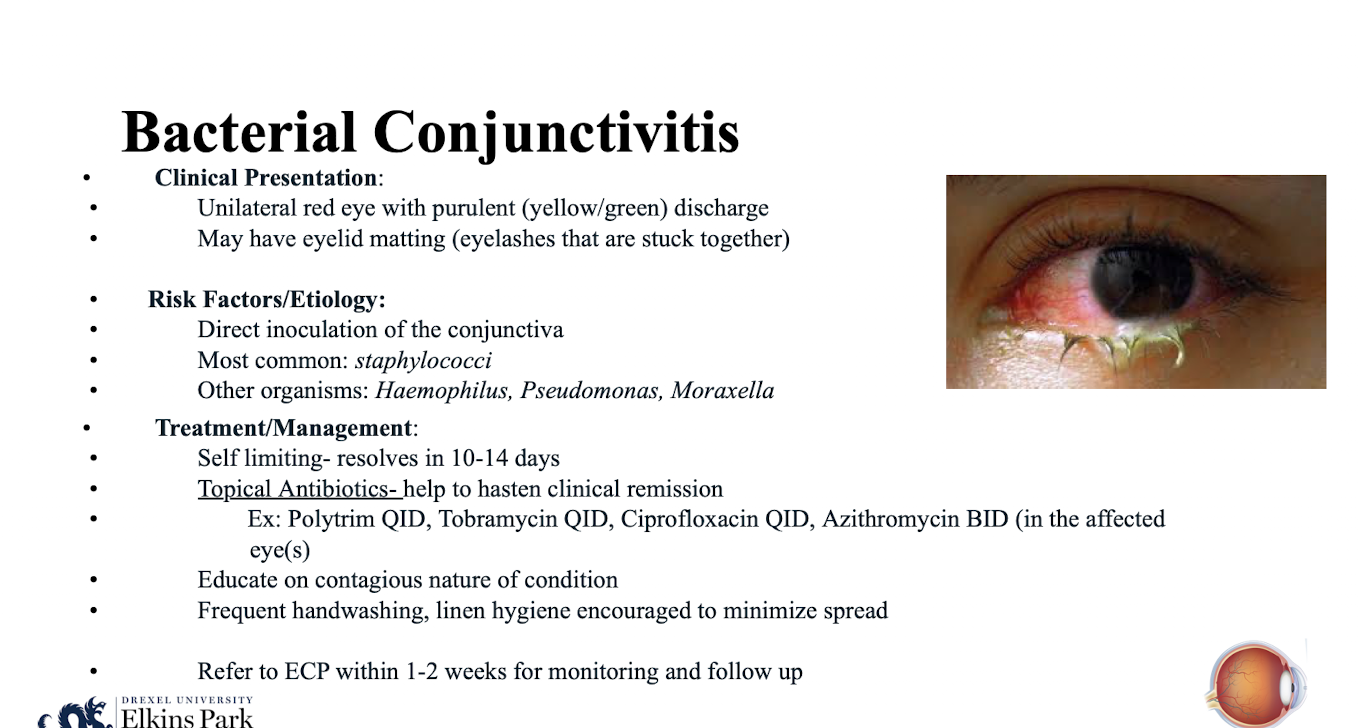
When should a patient with bacterial conjunctivitis be referred to an ECP?
Within 1-2 weeks for monitoring and follow up.
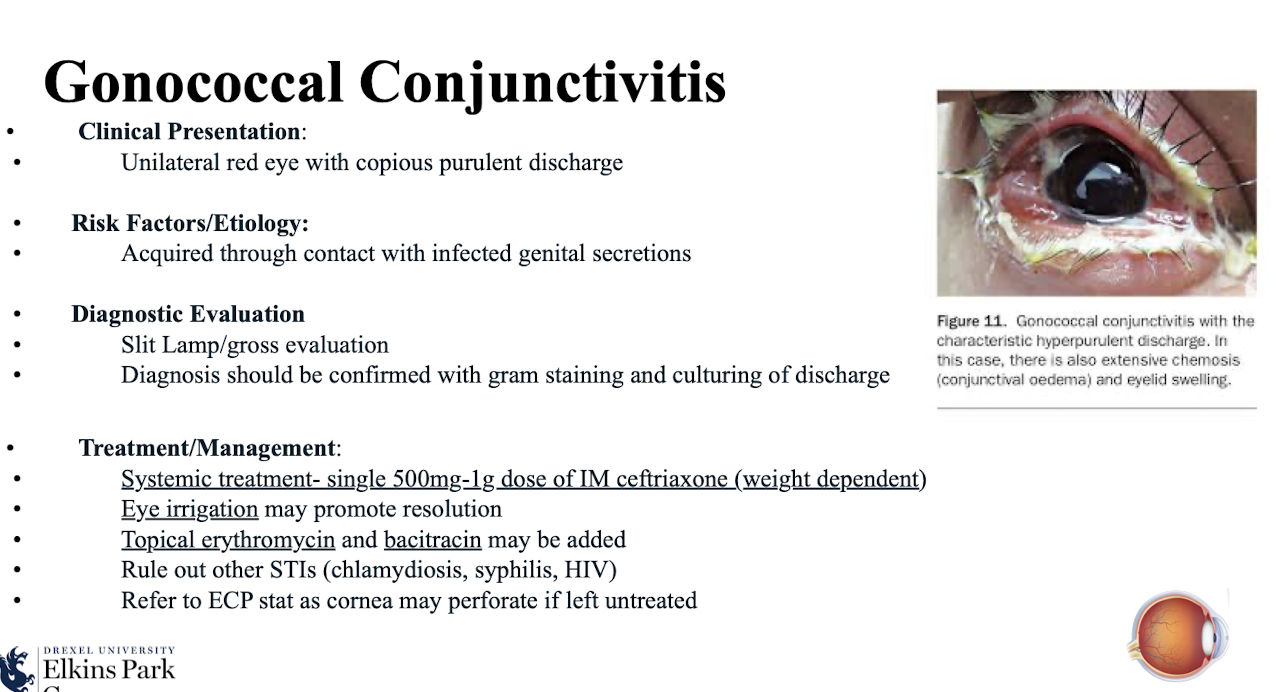
What is the clinical presentation of gonococcal conjunctivitis?
Unilateral red eye with copious purulent discharge
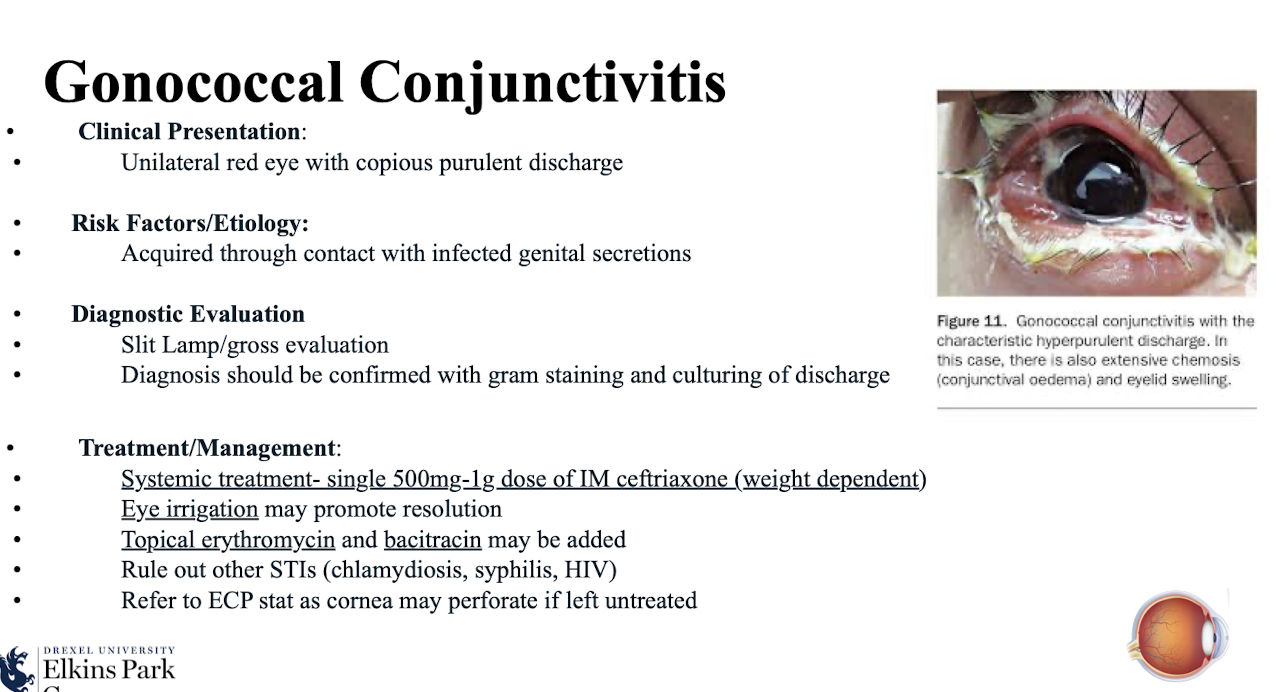
How is gonococcal conjunctivitis typically acquired?
Through contact with infected genital secretions.
How should the diagnosis of gonococcal conjunctivitis be confirmed?
With gram staining and culturing of discharge.
Slit Lamp/gross evaluation done first
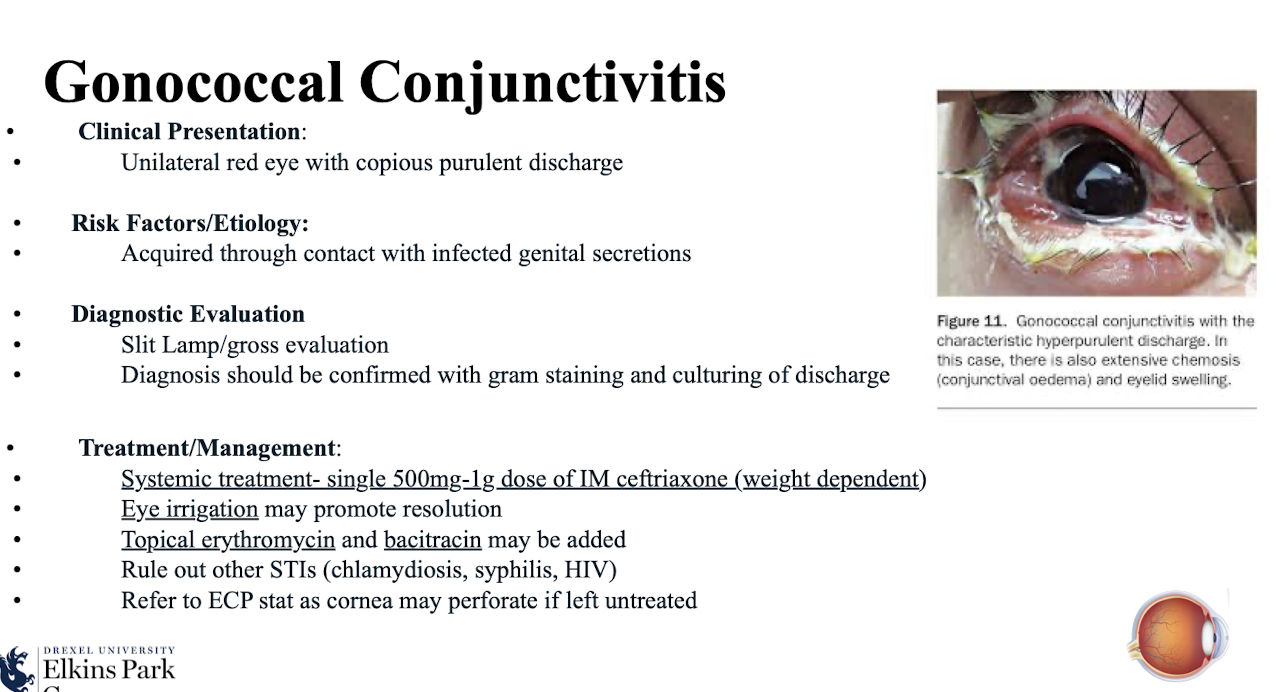
What is the systemic treatment for gonococcal conjunctivitis?
Single 500mg-1g dose of IM ceftriaxone (weight dependent).
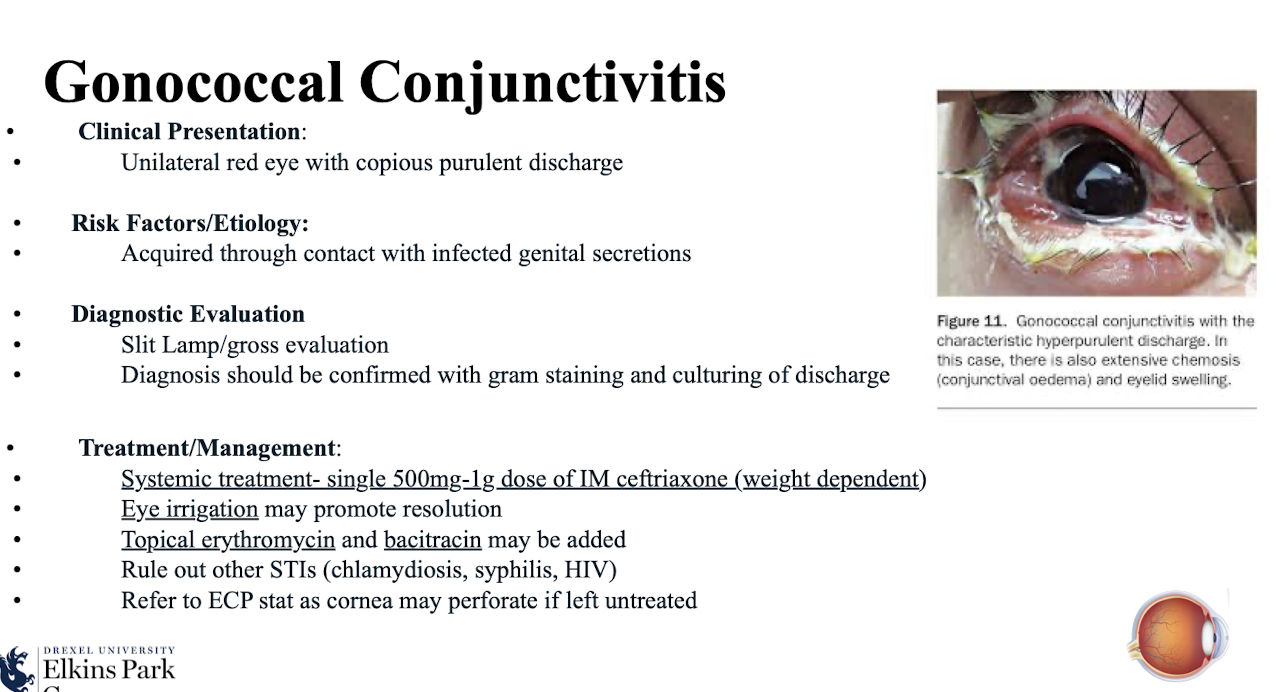
What adjunctive treatments may be added for gonococcal conjunctivitis?
Eye irrigation; topical erythromycin and bacitracin.
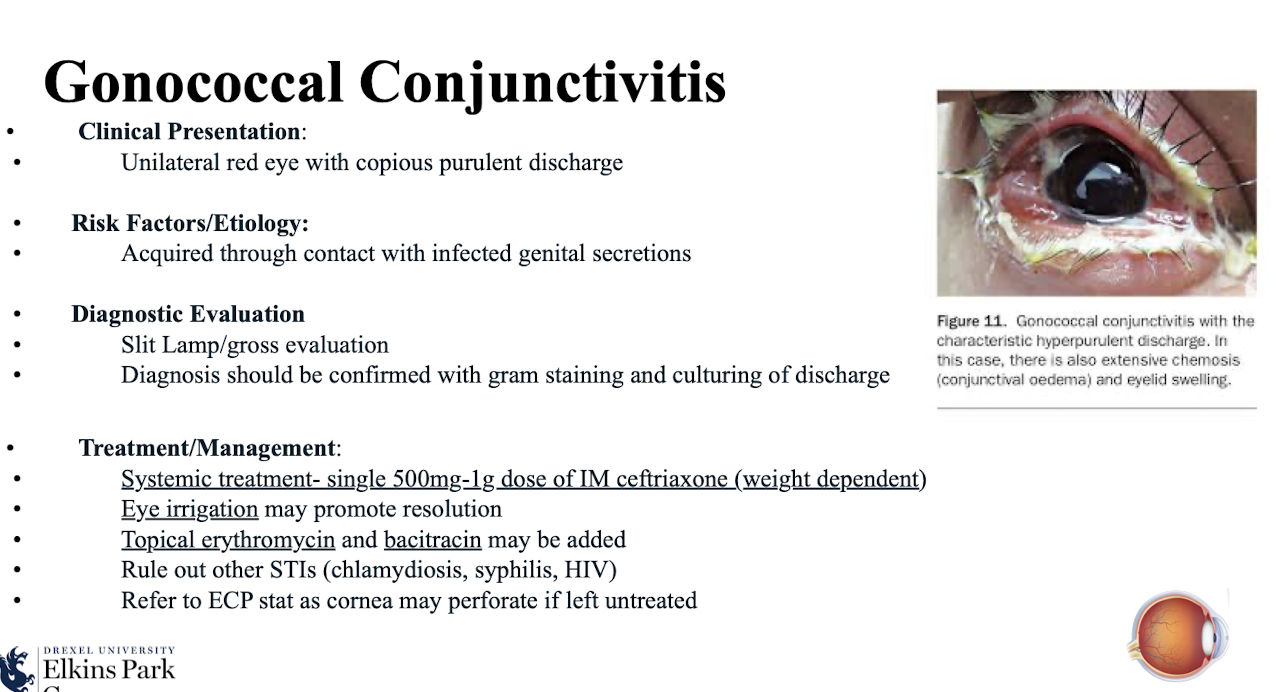
What crucial step must be taken when managing gonococcal conjunctivitis regarding STIs?
Rule out other STIs (chlamydiosis; syphilis; HIV).
Why is emergent referral to an ECP necessary for gonococcal conjunctivitis?
Cornea may perforate if left untreated.
What type of Chlamydial Conjunctivitis is the most common infectious cause of blindness worldwide?
Trachoma
Approxmately 40 million people affected and 1.2 million people blind
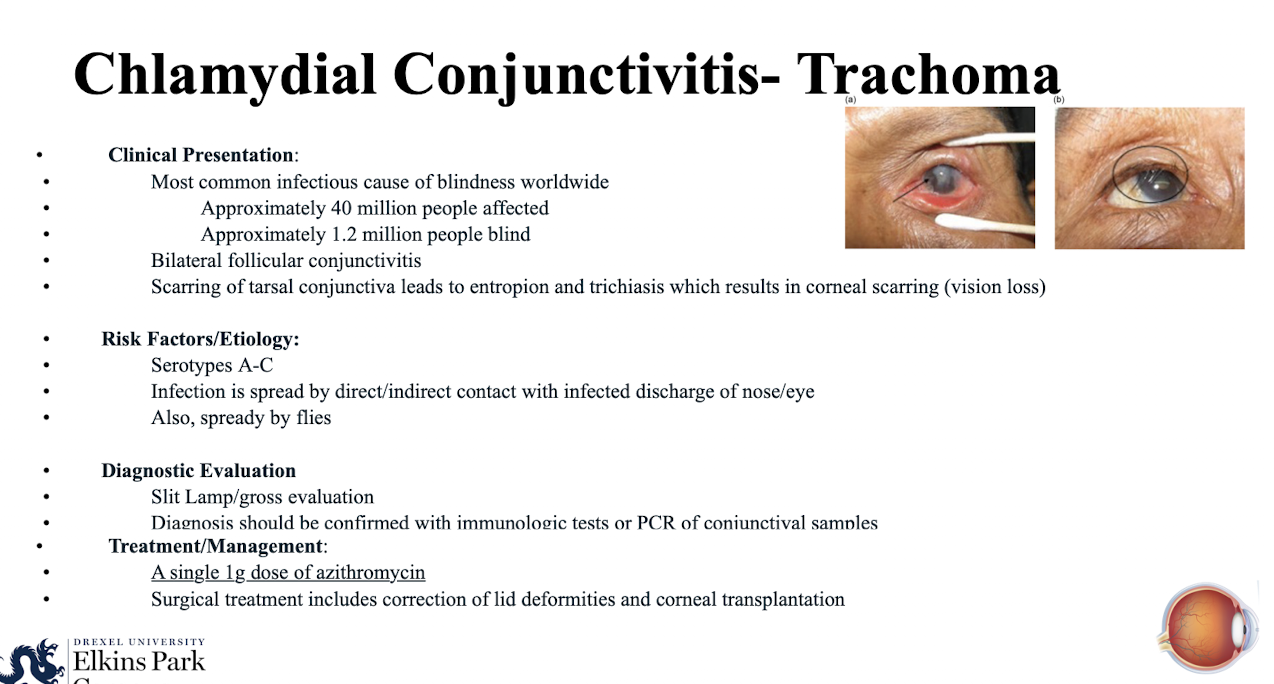
What is the clinical presentation of Chlamydial Conjunctivitis- Trachoma that leads to vision loss?
Bilateral follicular conjunctivitis; scarring of tarsal conjunctiva leads to entropion and trichiasis which results in corneal scarring (vision loss).
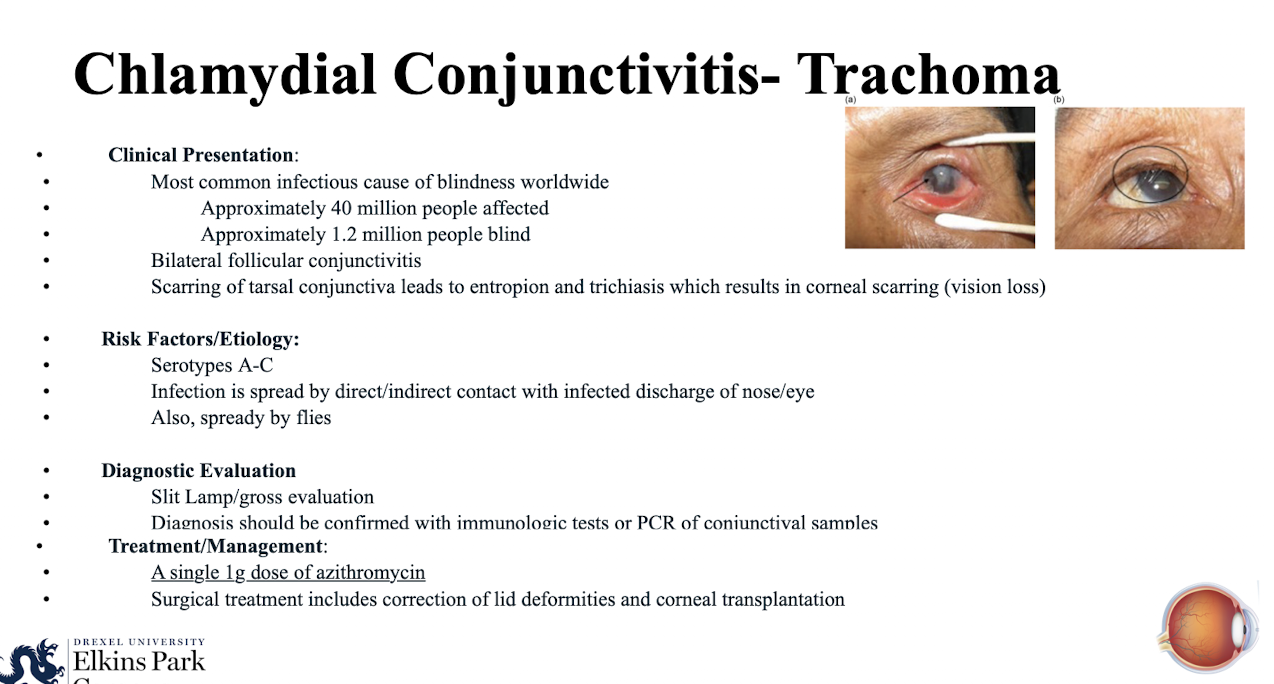
What serotypes are responsible for Chlamydial Conjunctivitis- Trachoma?
Serotypes A-C.
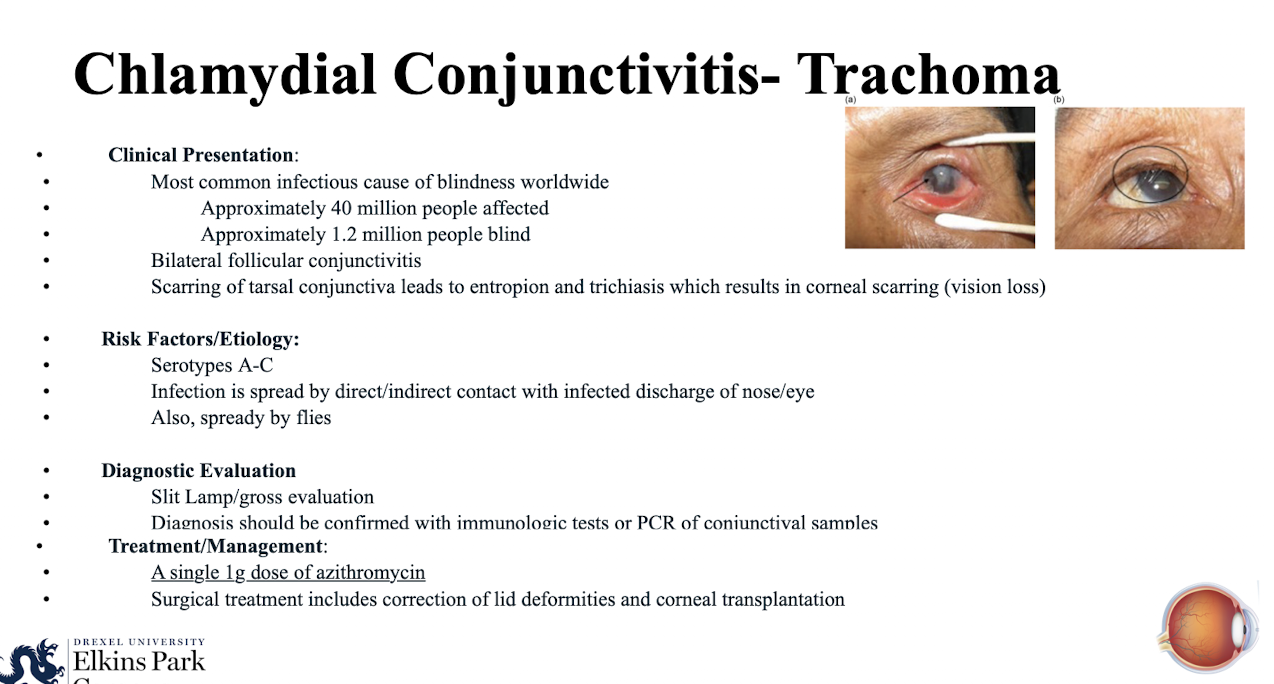
How is Trachoma spread?
By direct/indirect contact with infected discharge of nose/eye; also; spready by flies.
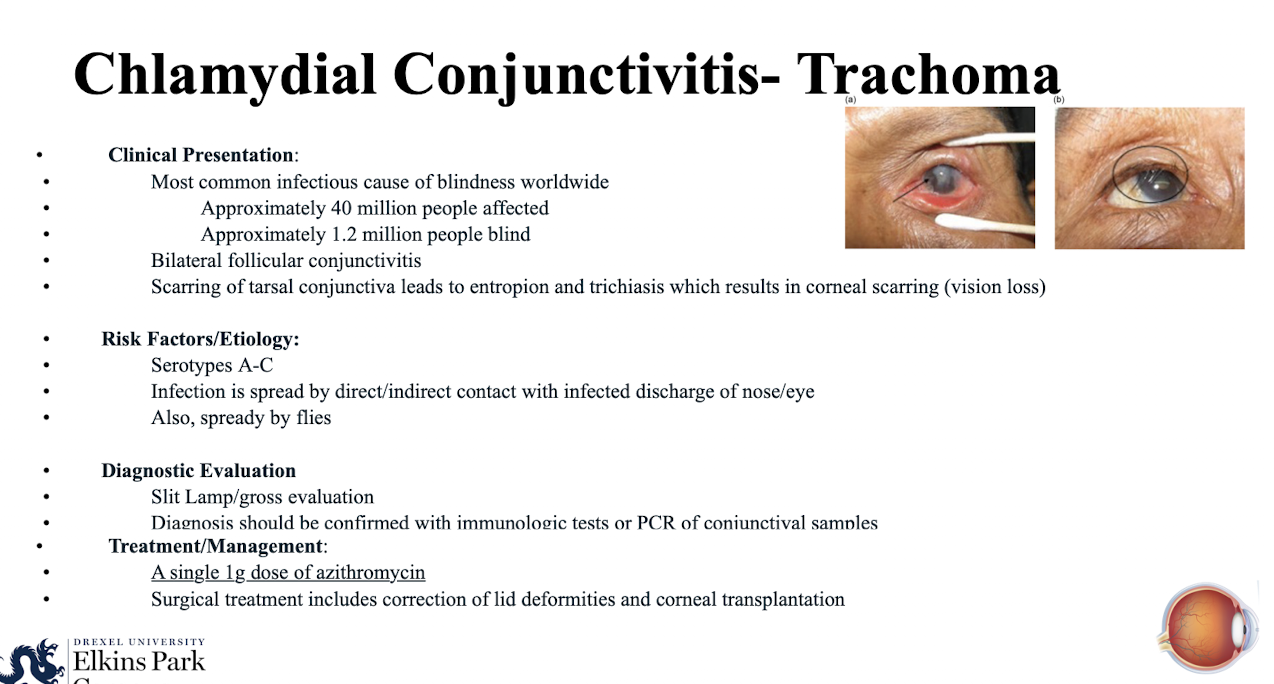
How is the diagnosis of Trachoma confirmed?
Slit Lamp/gross evaluation then
With immunologic tests or PCR of conjunctival samples.
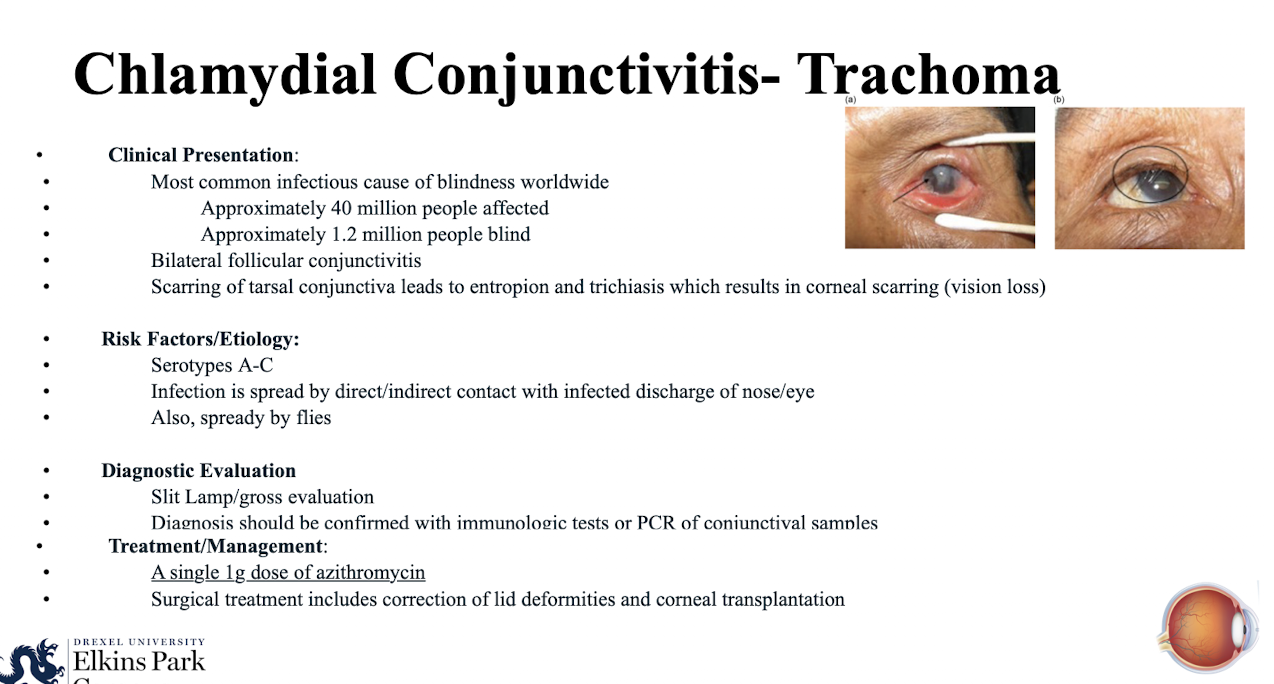
What is the primary medical treatment for Trachoma?
A single 1g dose of azithromycin.
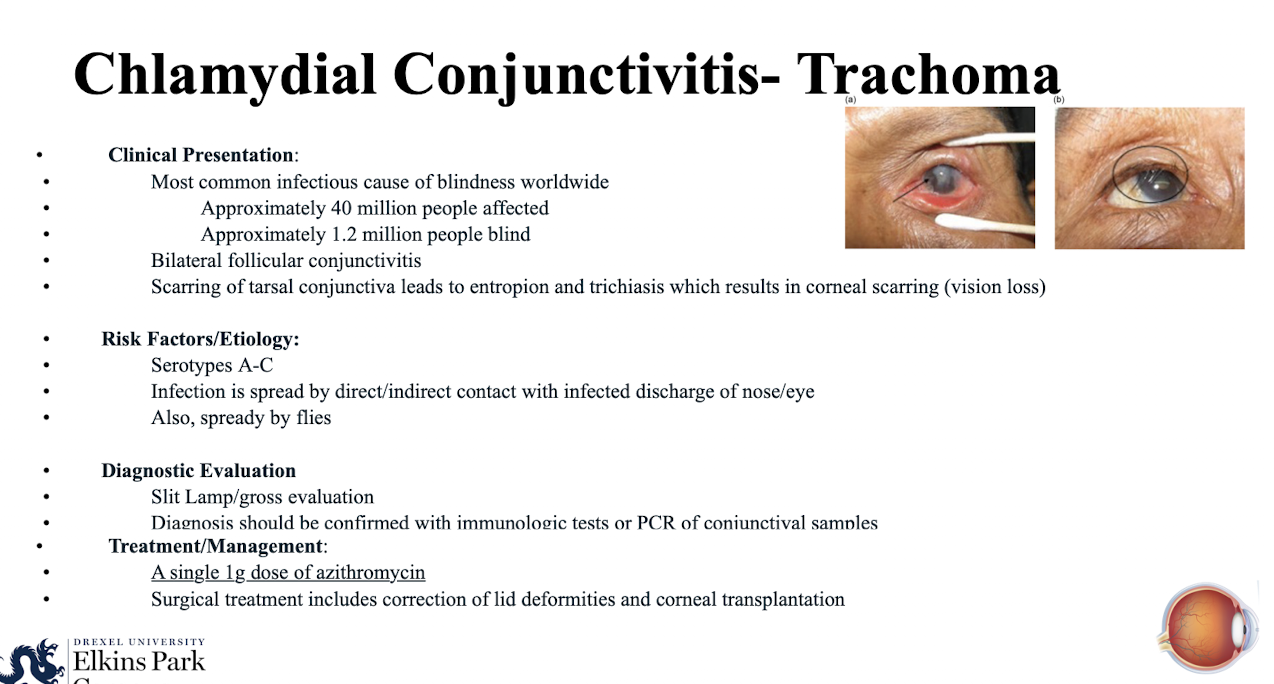
What surgical treatments may be indicated for Trachoma?
Correction of lid deformities and corneal transplantation.
What is the clinical presentation of Inclusion Conjunctivitis?
Starts with acute redness; discharge and irritation; leads to chronic follicular conjunctivitis that does not improve with topical antibiotic and/or steroid therapy
What serotypes are responsible for Inclusion Conjunctivitis?
Serotypes D-K.
How is Chlamydial Inclusion Conjunctivitis diagnosed and confirmed?
Slit Lamp/gross evaluation then
With immunologic tests or PCR of conjunctival samples.
What is the treatment regimen for Inclusion Conjunctivitis?
Doxycycline 100mg PO BID for 7 days.
What assessment is required for all cases of Inclusion Conjunctivitis?
All cases should be assessed for genital tract infections and other STIs.
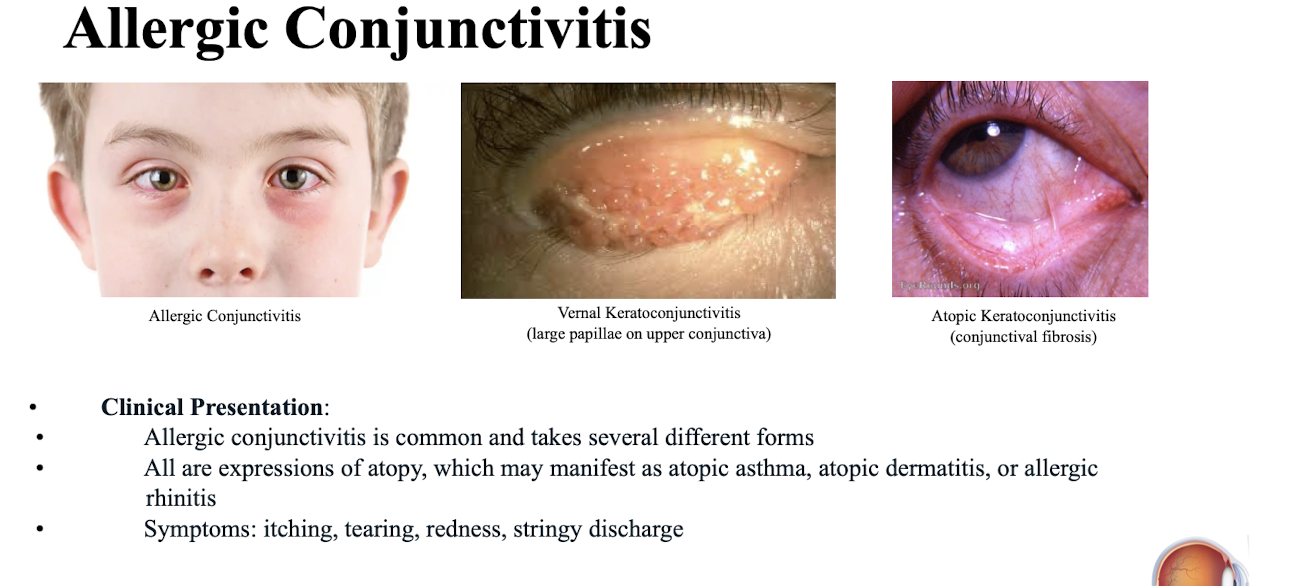
What three forms of allergic eye disease are mentioned?
Allergic Conjunctivitis; Vernal Keratoconjunctivitis (large papillae on upper conjunctiva); Atopic Keratoconjunctivitis (conjunctival fibrosis)
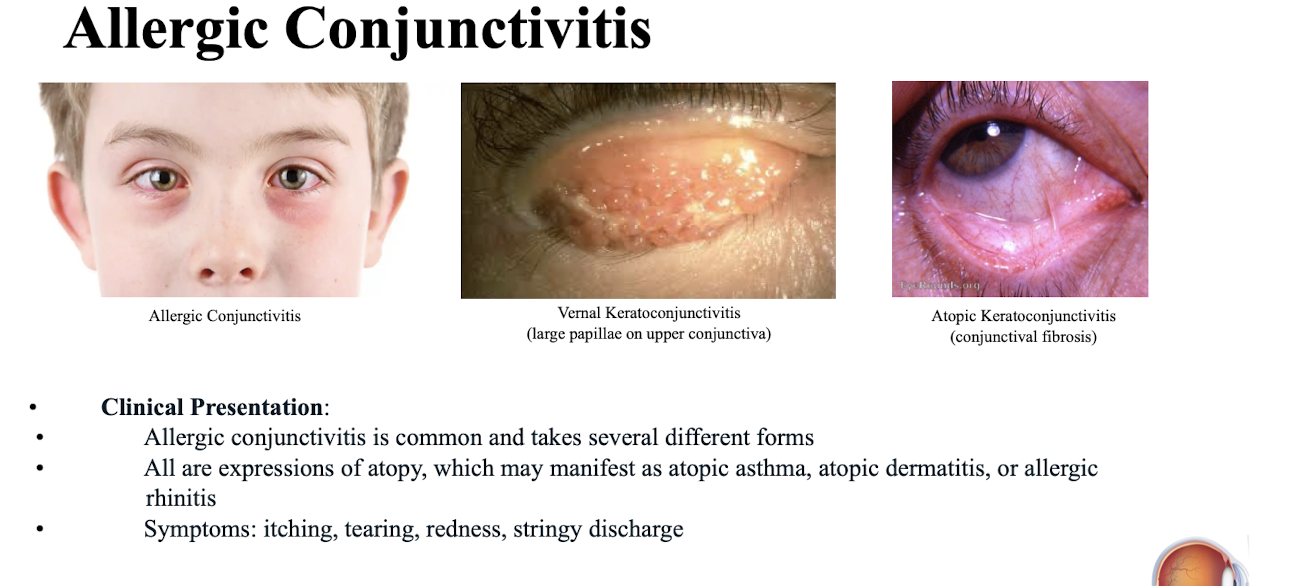
Allergic conjunctivitis is an expression of what underlying condition?
Atopy.
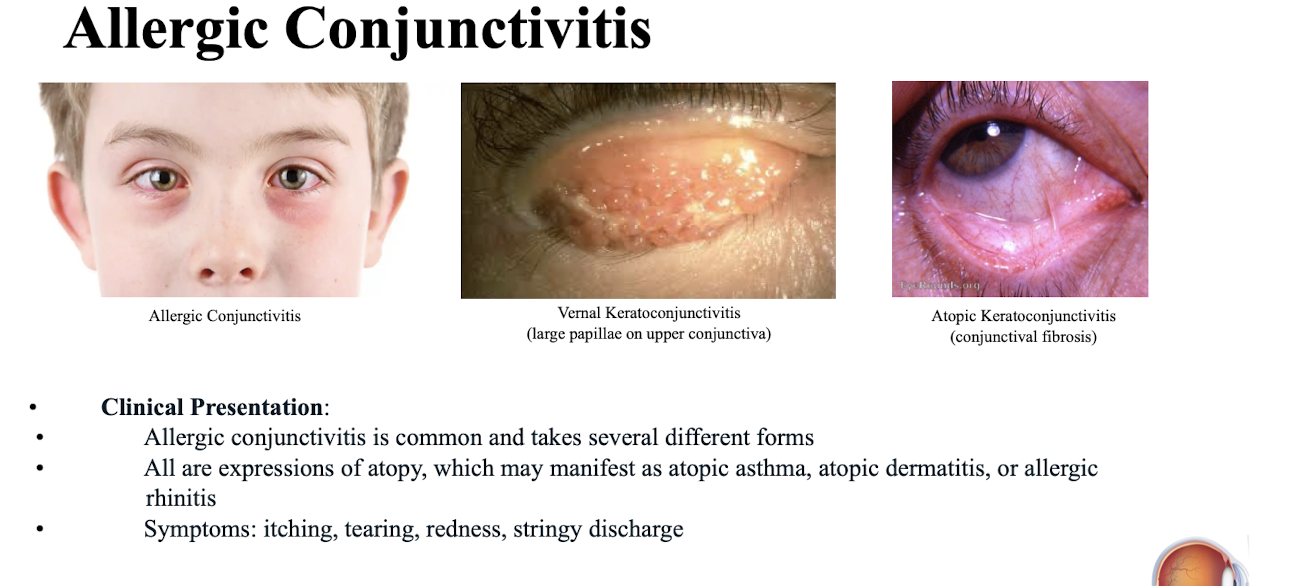
What are common systemic manifestations of atopy?
Atopic asthma; atopic dermatitis; or allergic rhinitis.
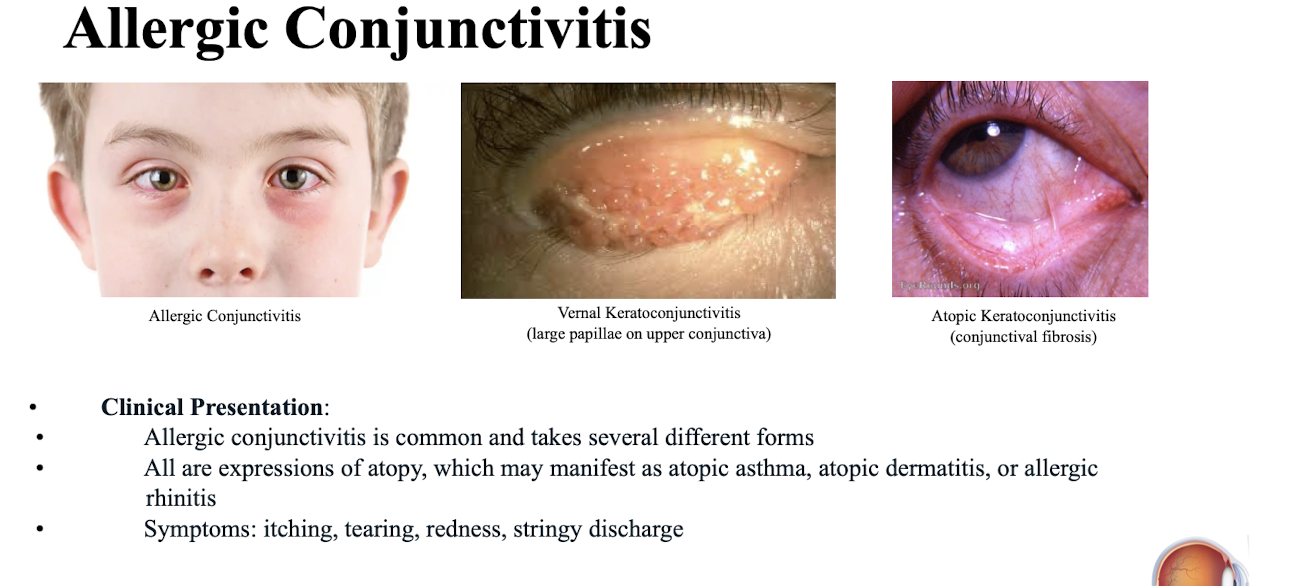
What are the common ocular symptoms of Allergic Conjunctivitis?
Itching; tearing; redness; stringy discharge.
What is the most common form of allergic eye disease?
Allergic Conjunctivitis
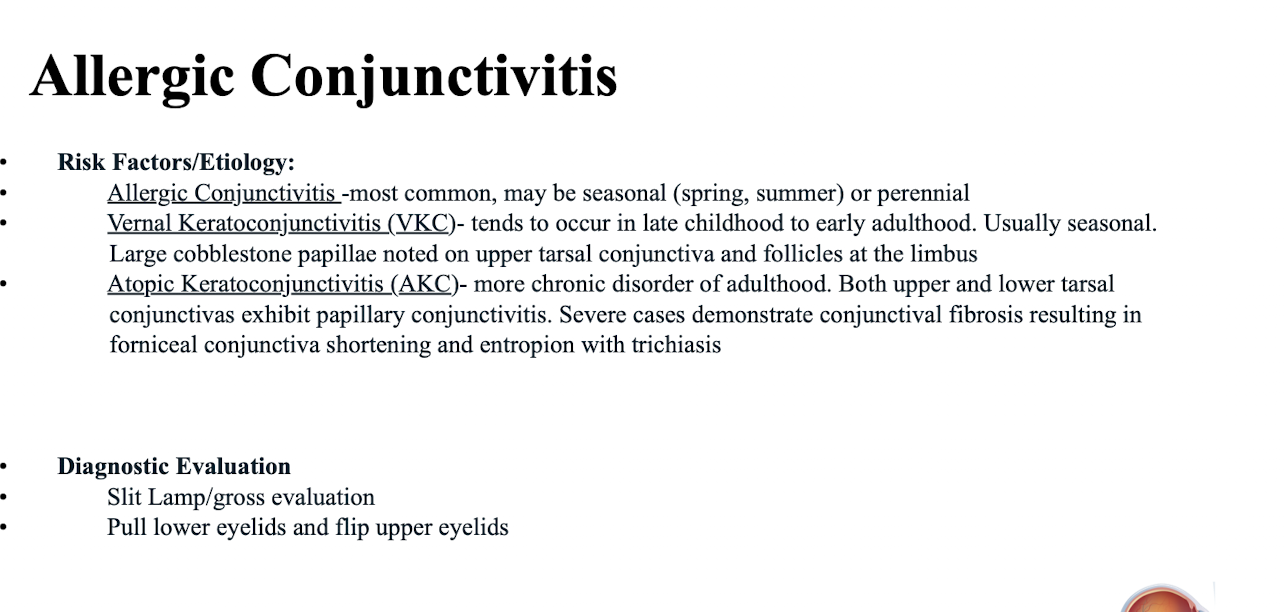
What are the characteristics of Allergic Conjunctivitis based on timing?
May be seasonal (spring; summer) or perennial.
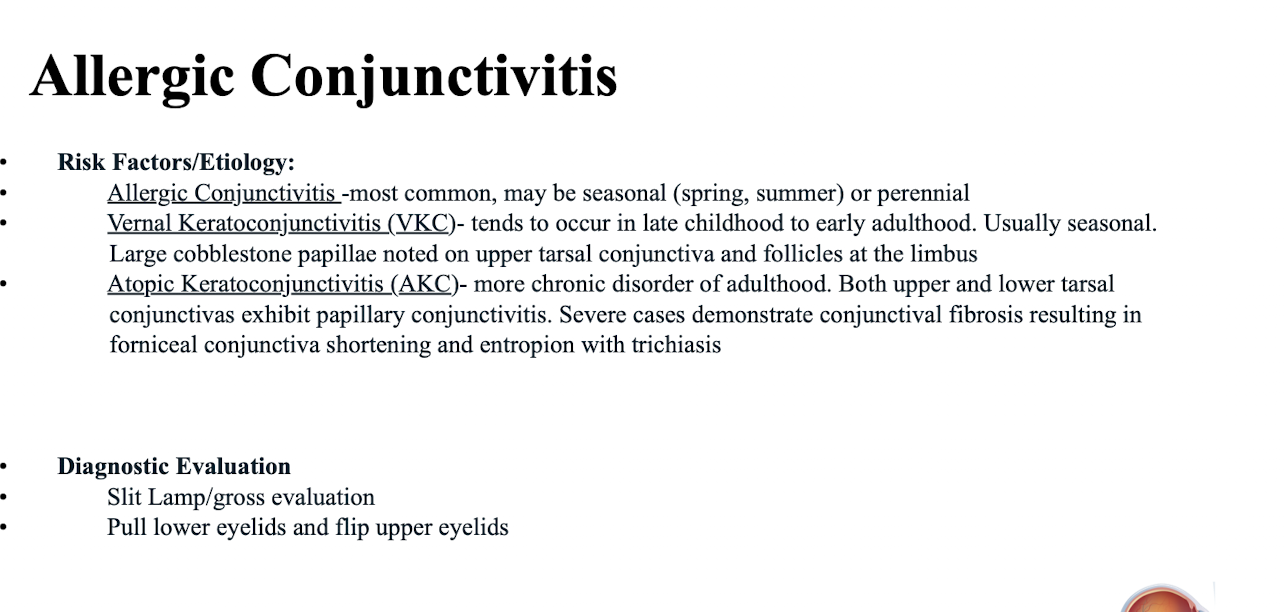
What are the key findings associated with Vernal Keratoconjunctivitis (VKC)?
Large cobblestone papillae noted on upper tarsal conjunctiva and follicles at the limbus.
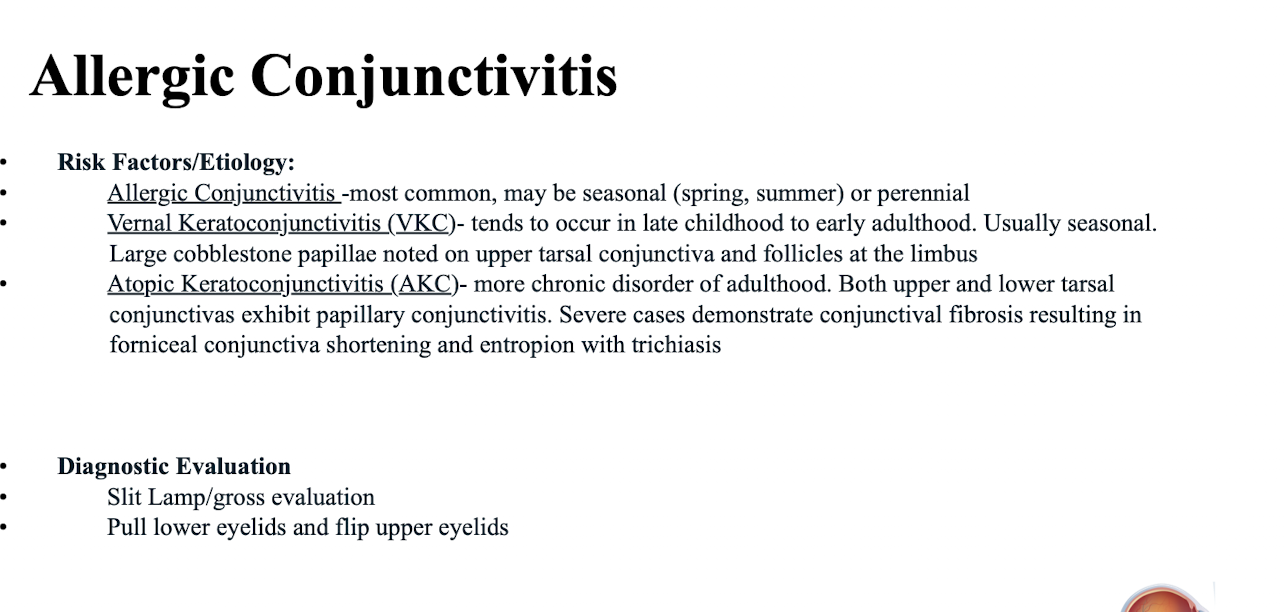
What are the characteristics of Atopic Keratoconjunctivitis (AKC)?
More chronic disorder of adulthood; both upper and lower tarsal conjunctivas exhibit papillary conjunctivitis; severe cases demonstrate conjunctival fibrosis resulting in forniceal conjunctiva shortening and entropion with trichiasis.
What diagnostic steps are emphasized for Allergic Conjunctivitis?
Slit Lamp/gross evaluation; pull lower eyelids and flip upper eyelids.
What is the first-line management for mild and moderately severe allergic disease?
Avoid allergen
What topical medications are used for mild/moderate allergic disease?
Topical mast cell stabilizer/antihistamine combo eyedrops;
Pataday QD-BID OU.
Systemic Antihistamine - Loratadine 10mg QD PO
Cool compresses
What topical medications are used for acute exacerbations and severe allergic eye disease (VKC and AKC)?
Topical corticosteroids (Loteprednol 0.5% BID OU);
Topical cyclosporine or tacrolimus (Cyclosporine 0.05%/Restasis BID OU;
Tacrolimus 0.1% ung applied to the LL BID OU).
When should a patient with Allergic Conjunctivitis follow up with an ECP?
In 1-2 weeks.
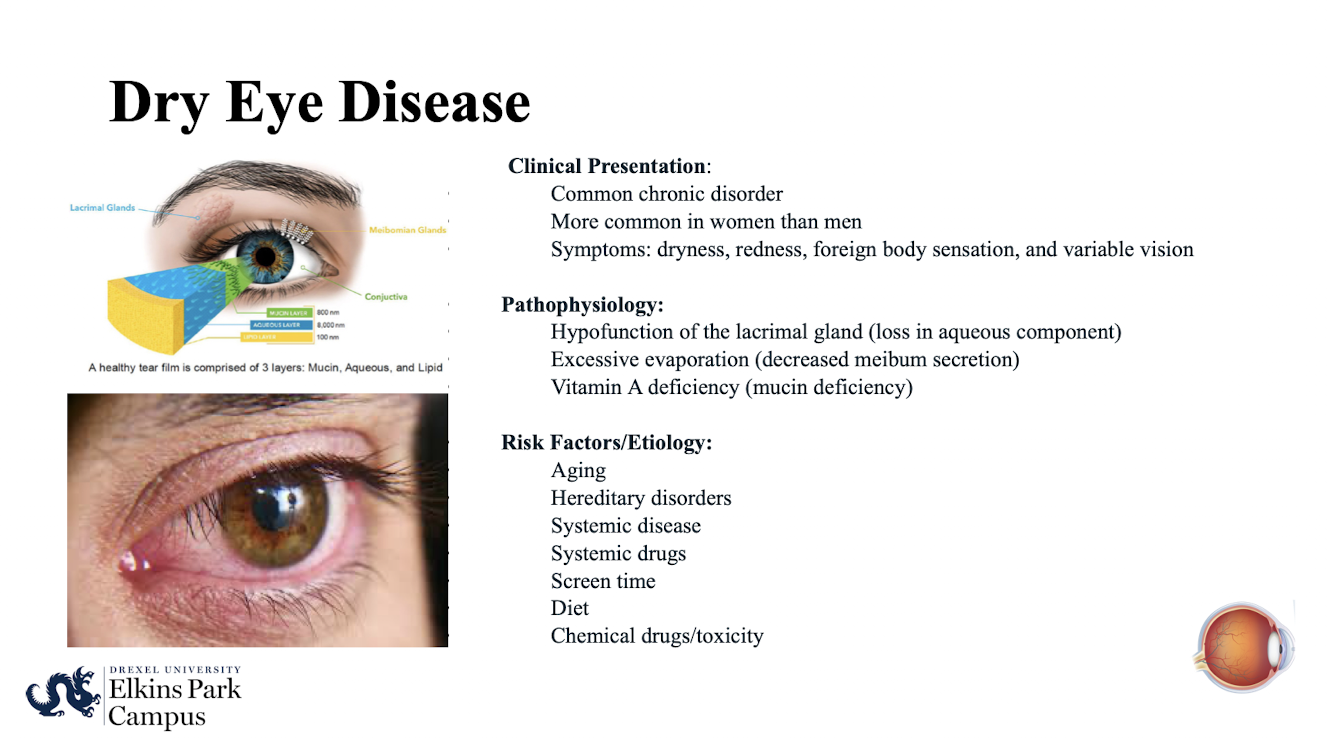
What are the clinical characteristics and common symptoms of Dry Eye Disease (DED)?
Common chronic disorder; more common in women than men; symptoms include dryness; redness; foreign body sensation; and variable vision
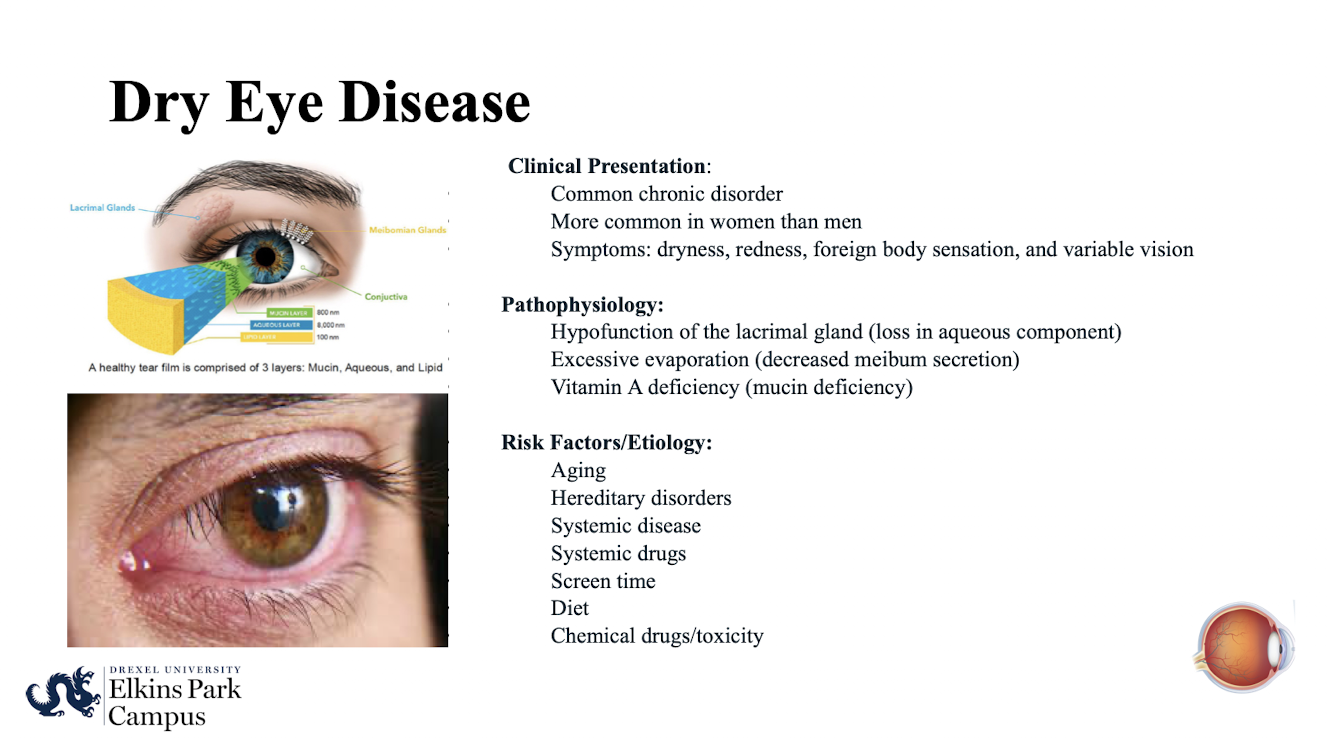
What three main pathophysiological mechanisms contribute to Dry Eye Disease?
Hypofunction of the lacrimal gland (loss in aqueous component); excessive evaporation (decreased meibum secretion);
Vitamin A deficiency (mucin deficiency).
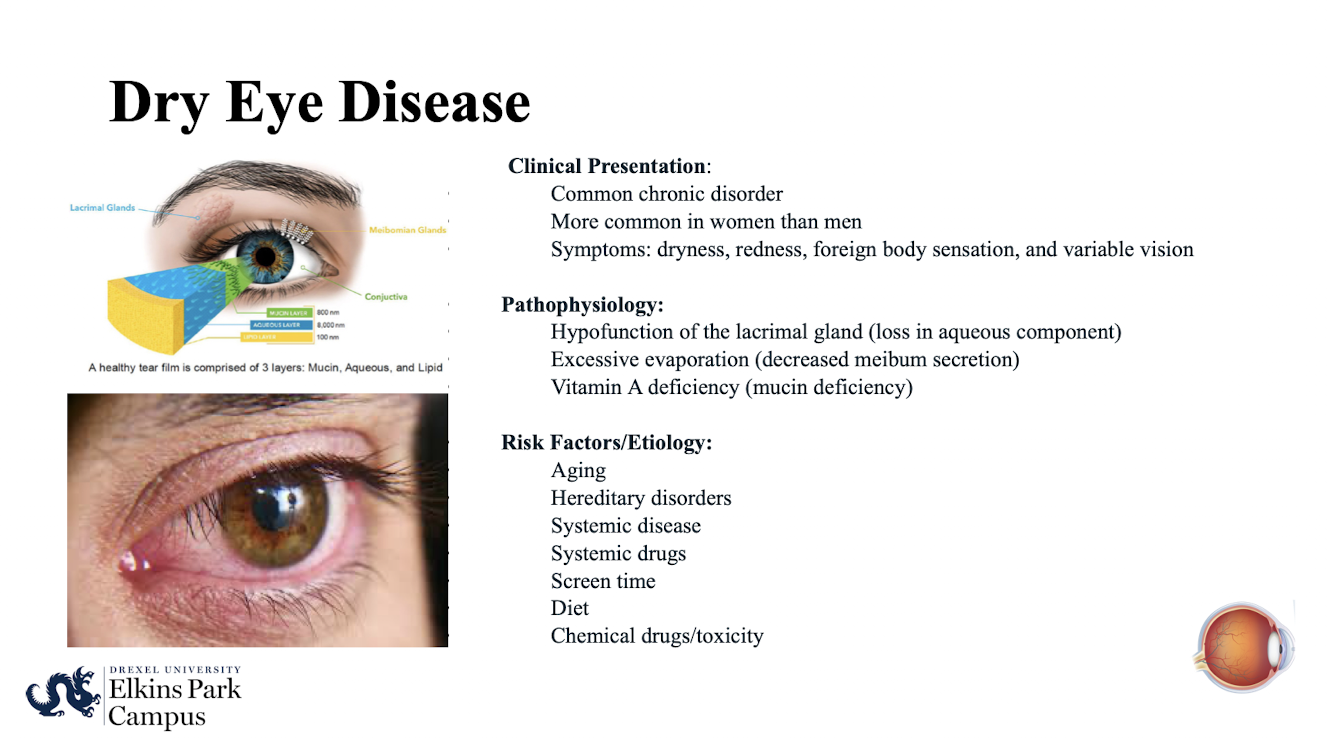
What are major risk factors/etiologies for Dry Eye Disease?
Aging; hereditary disorders; systemic disease; systemic drugs; screen time (you blink less); diet; chemical drugs/toxicity.
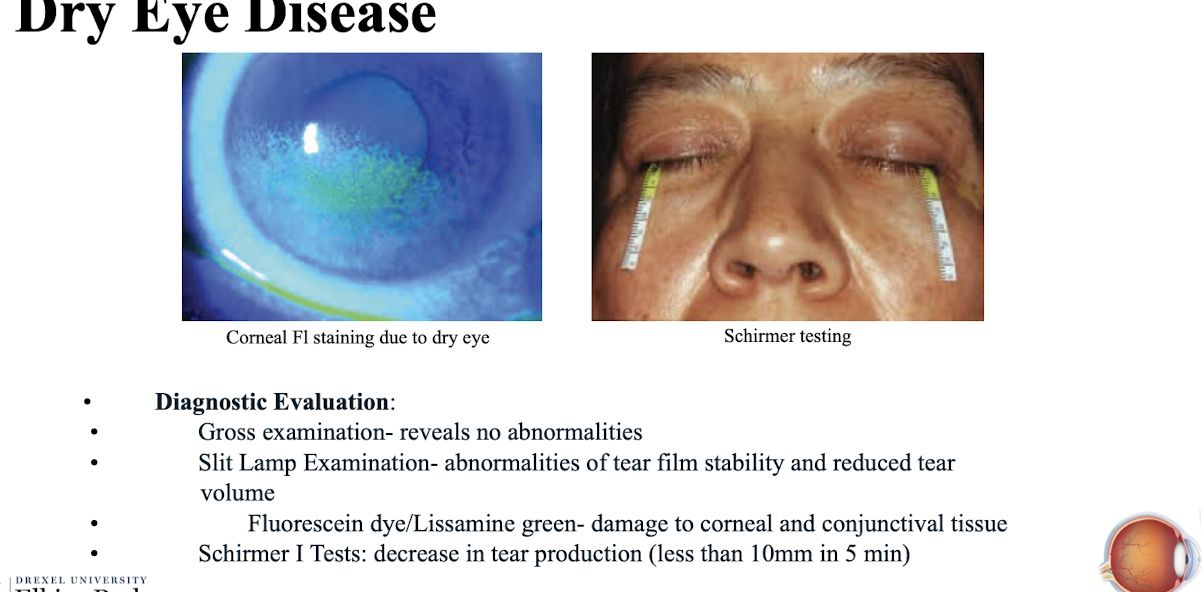
What is revealed by a gross examination in Dry Eye Disease?
No abnormalities
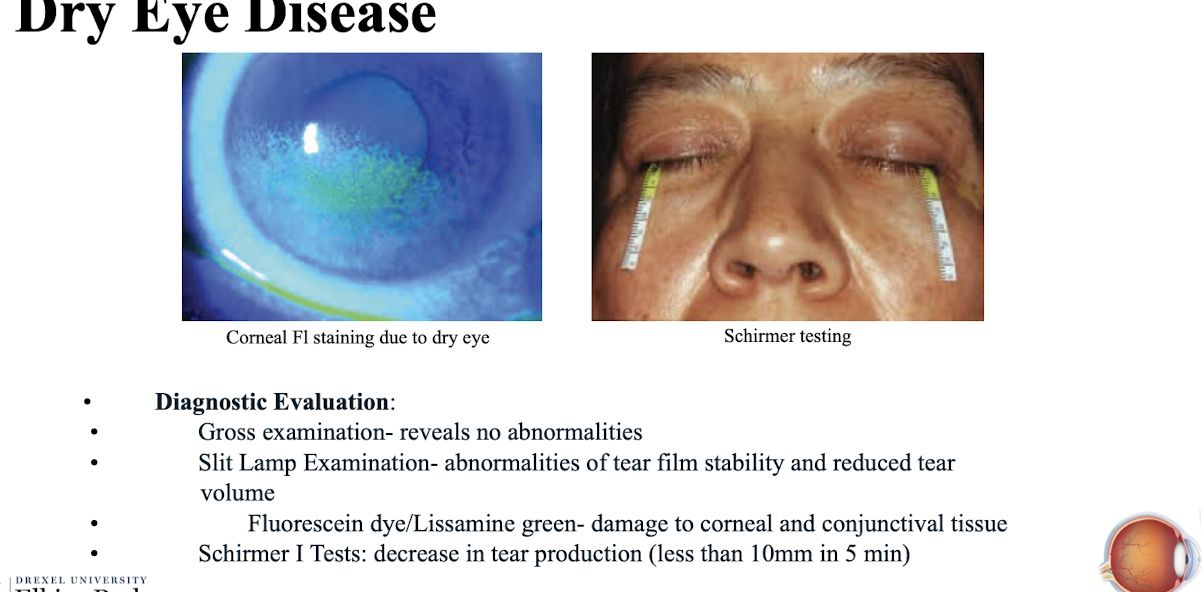
What does a Slit Lamp Examination reveal in Dry Eye Disease?
Abnormalities of tear film stability and reduced tear volume.
Dry spots look like dirzzle on a ca windshield
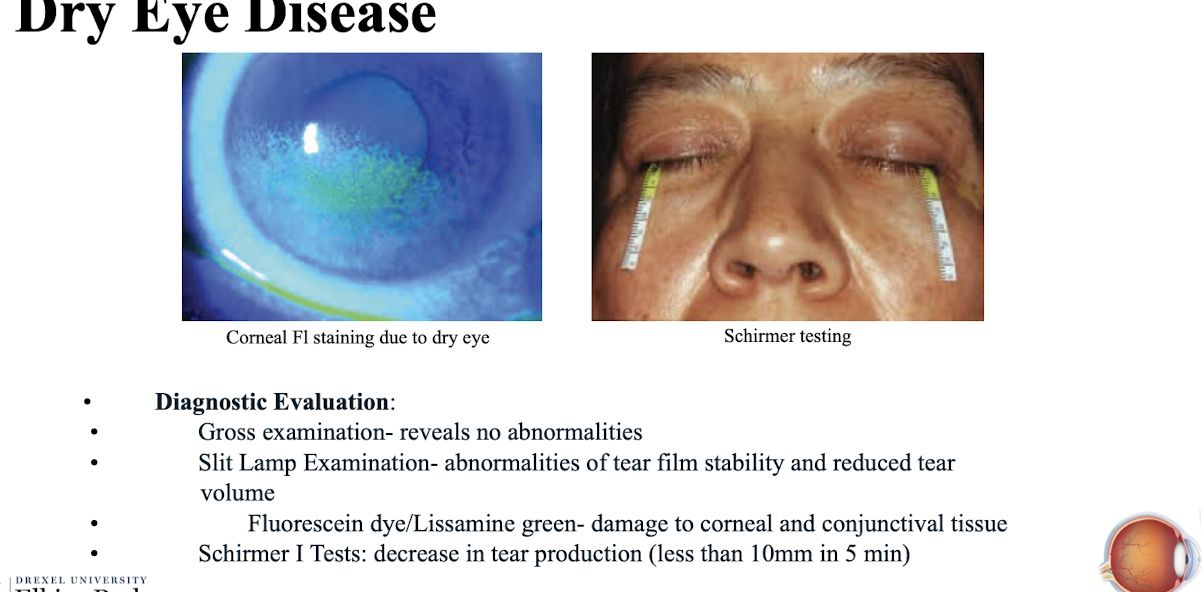
What dyes are used to assess damage to corneal and conjunctival tissue in DED?
Fluorescein dye/Lissamine green.
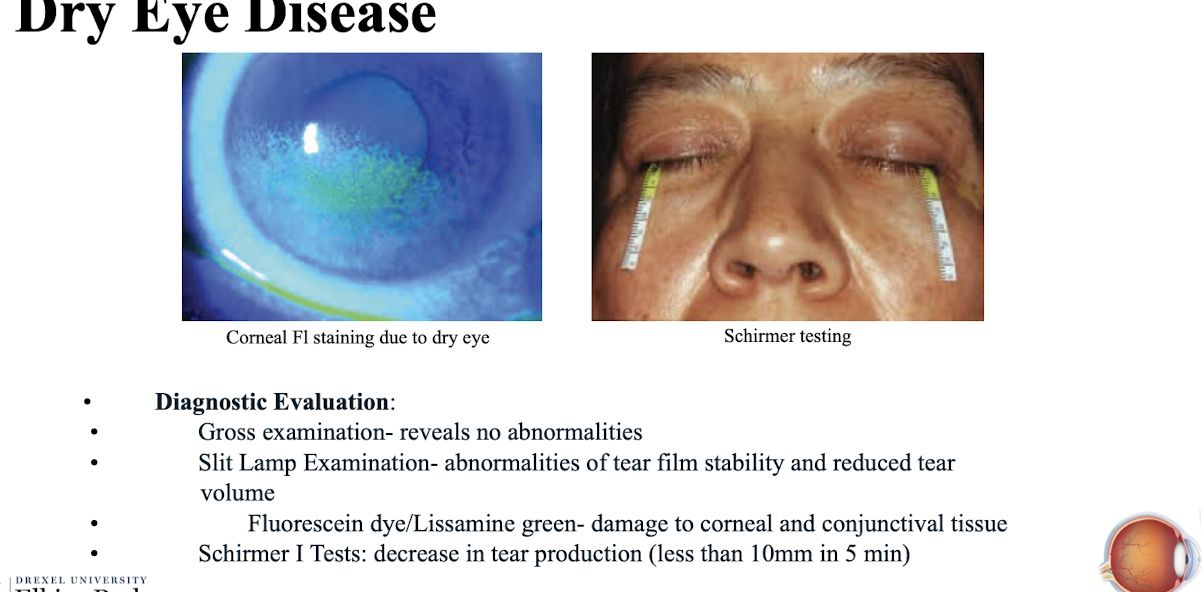
What result on the Schirmer I Test indicates decreased tear production?
Less than 10mm in 5 min.
What is the management for Aqueous Deficiency DED?
OTC Artificial Tears/Ointments BID-QID OU;
Preservative free formulations can be dosed more often (anytime you dose something QID)
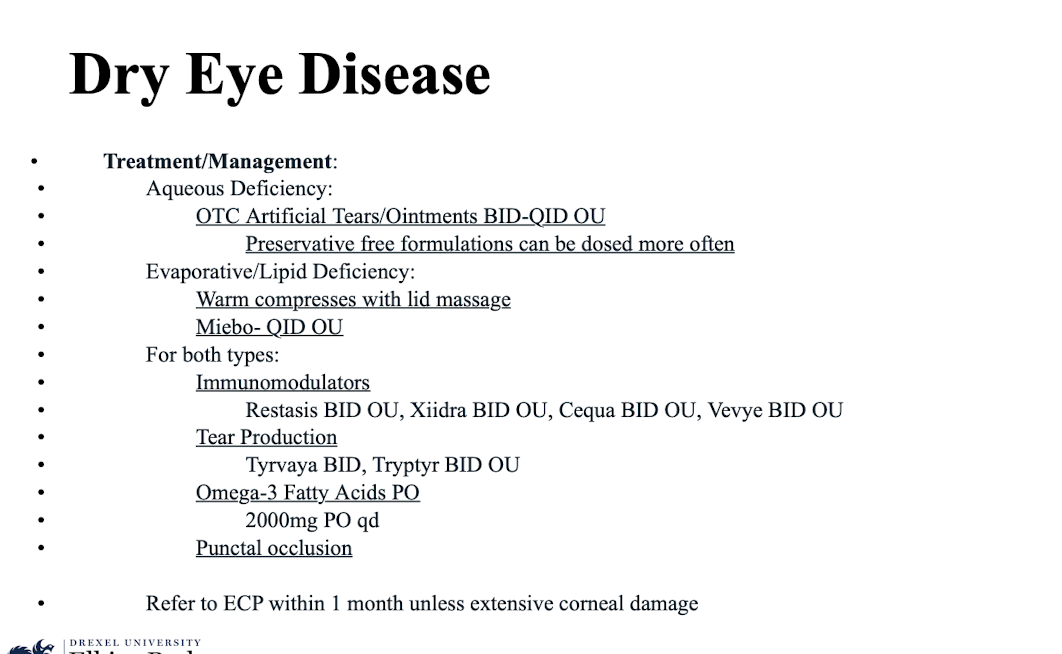
What is the management for Evaporative/Lipid Deficiency DED?
Warm compresses with lid massage; Miebo- QID OU.
What immunomodulators are used for both types of DED?
Restasis BID OU; Xiidra BID OU; Cequa BID OU; Vevye BID OU.
What treatments are used to promote tear production in DED?
Tyrvaya (parasympathomimetic) BID; Tryptyr BID OU.
Omega-3 Fatty Acids PO - 2000mg PO qd
Punctal occlusion (plugs trap tears so they dont go through the drainage system)
When should a patient with Dry Eye Disease be referred to an ECP?
Within 1 month unless extensive corneal damage.
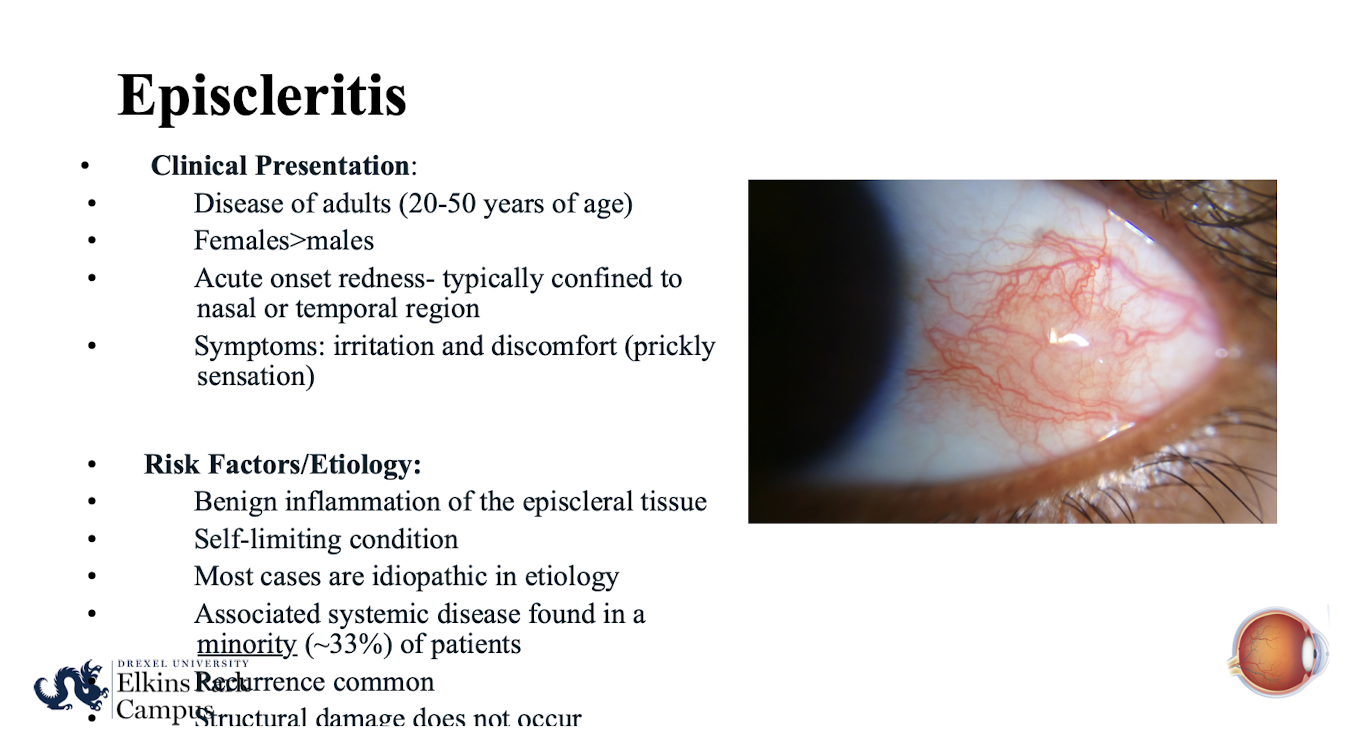
What is Episcleritis?
Benign inflammation of the episcleral tissue
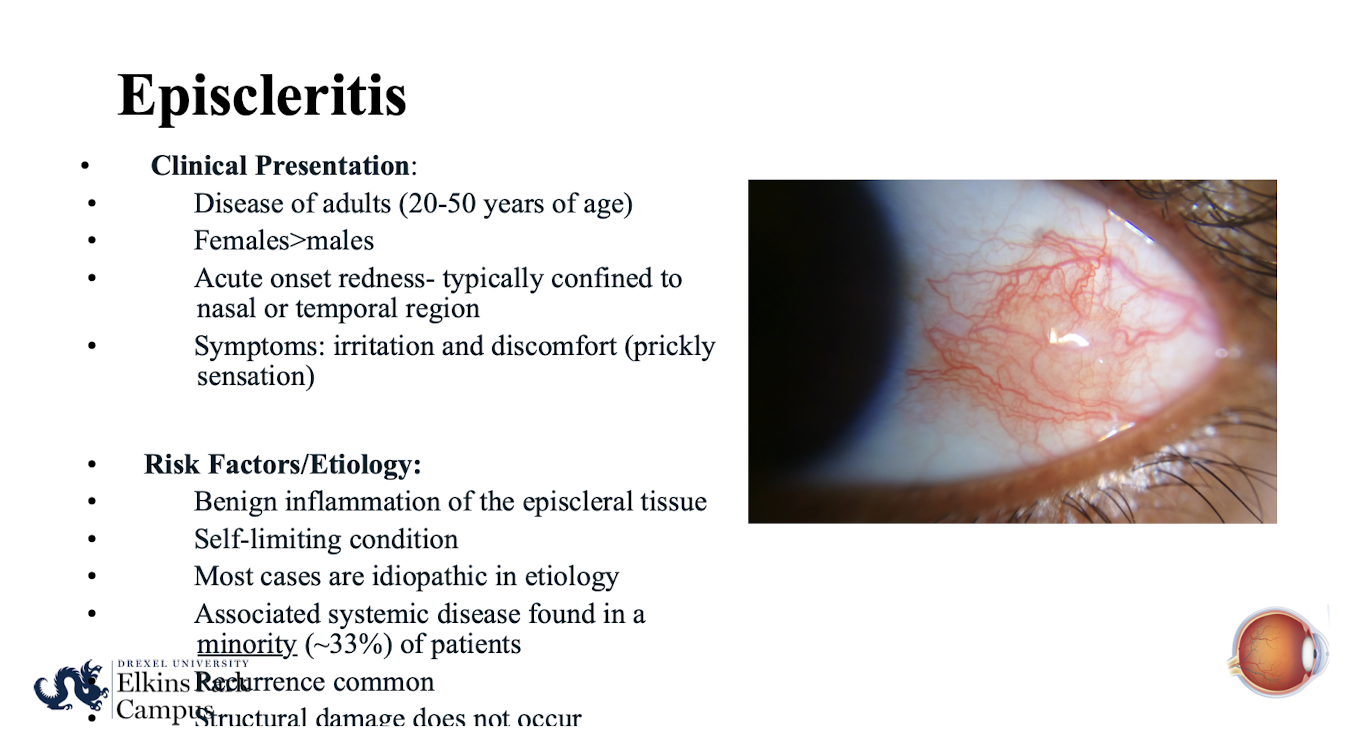
Who is typically affected by Episcleritis?
Adults (20-50 years of age); Females>males.
What is the clinical presentation of Episcleritis?
Acute onset redness- typically confined to nasal or temporal region; symptoms include irritation and discomfort (prickly sensation).
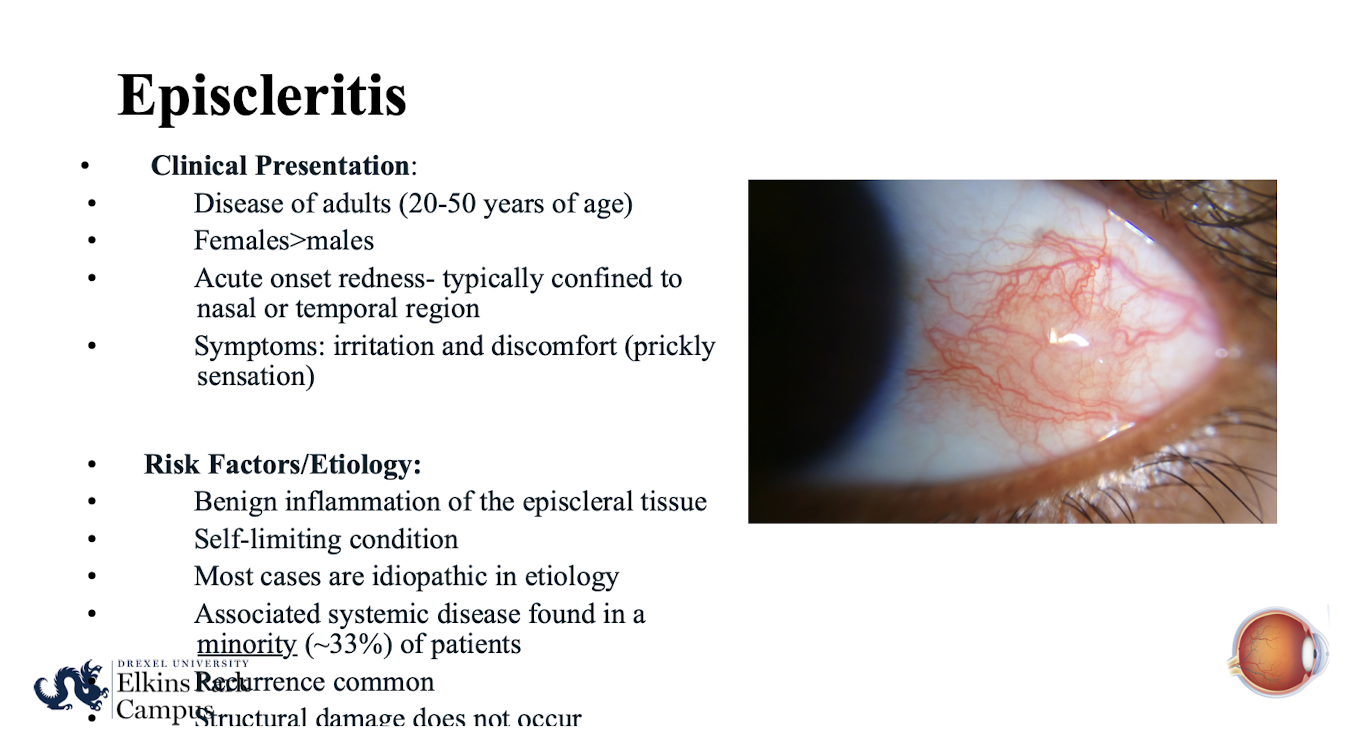
What is the typical etiology and course of Episcleritis?
Most cases are idiopathic in etiology; self-limiting condition.
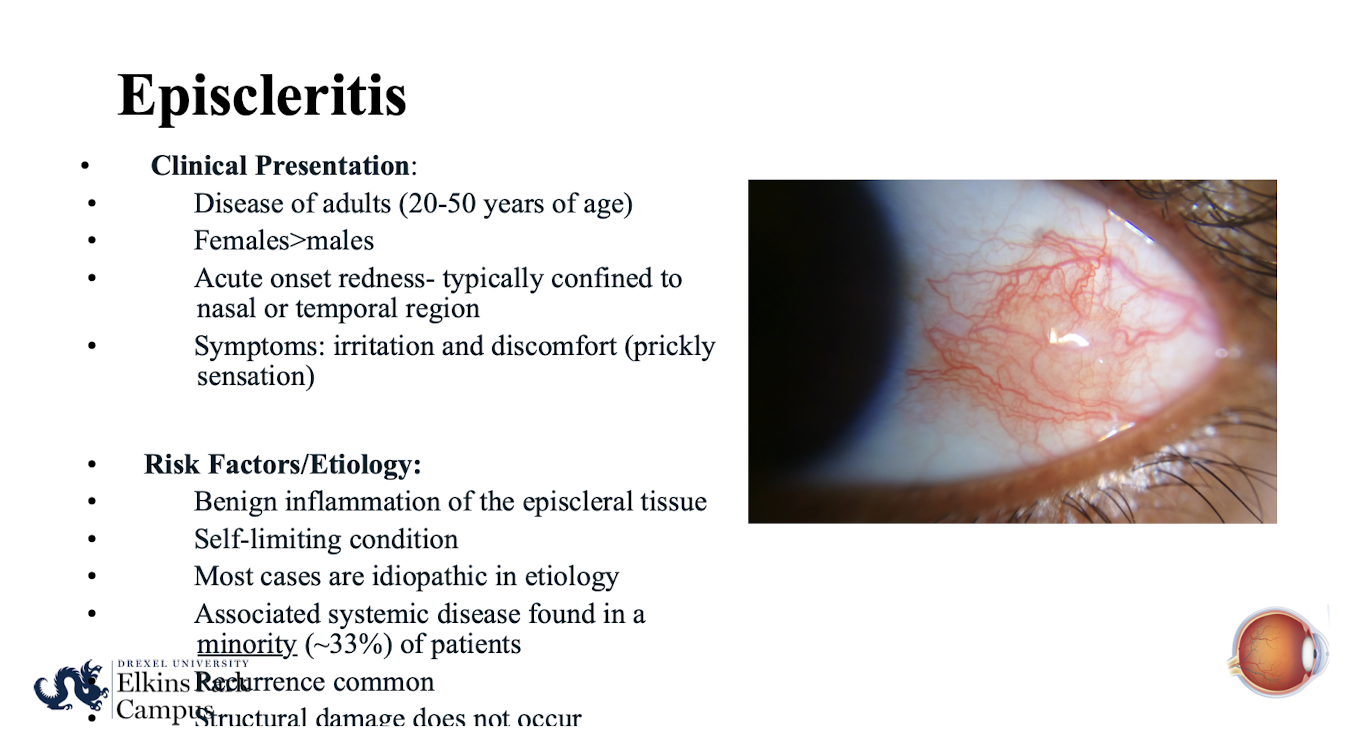
What percentage of Episcleritis cases are associated with systemic disease?
A minority (~33%) of patients.
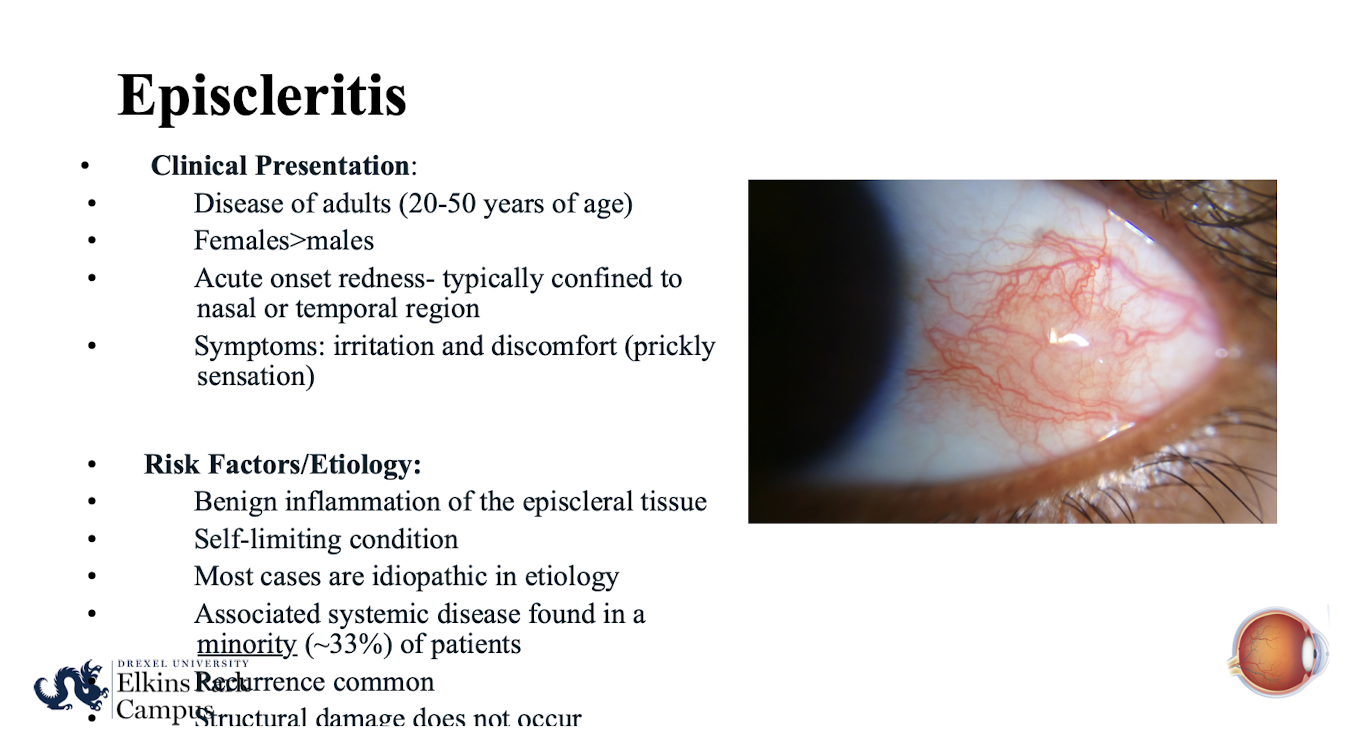
Does structural damage occur in Episcleritis?
No; structural damage does not occur. But recurrence is common
How is episcleritis diagnosed? What is the treatment for mild-moderate symptoms of Episcleritis?
Dx: Slip lamp/ gross evaluation
Chilled artificial tears PRN in the affected eye
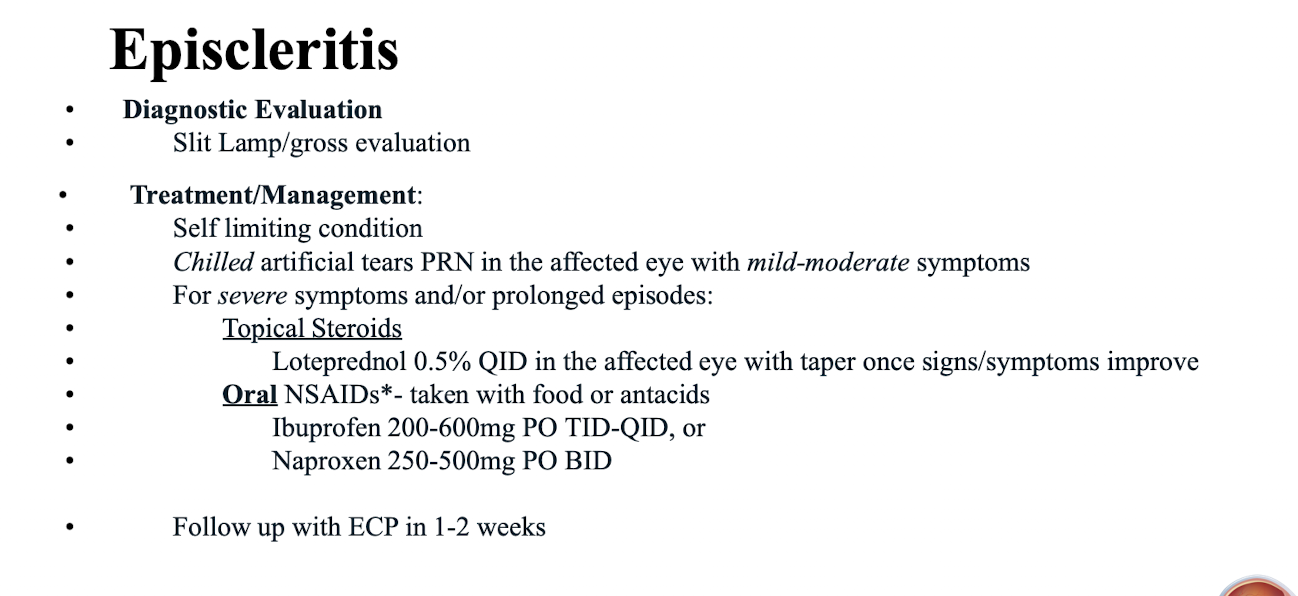
What is the treatment for severe symptoms and/or prolonged episodes of Episcleritis?
Topical Steroids (Loteprednol 0.5% QID in the affected eye with taper once signs/symptoms improve); Oral NSAIDs*- taken with food or antacids (Ibuprofen 200-600mg PO TID-QID; or Naproxen 250-500mg PO BID).
When should a patient with Episcleritis follow up with an ECP?
In 1-2 weeks.
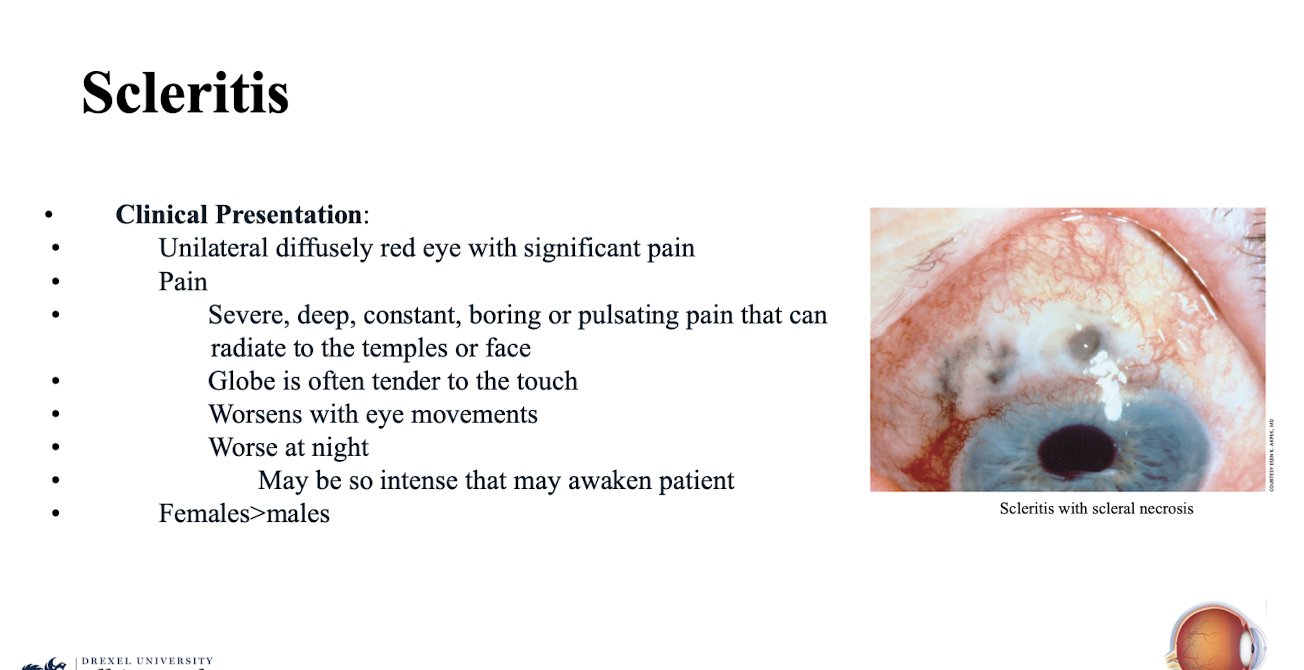
What is the clinical presentation of Scleritis regarding redness and pain?
Unilateral diffusely red eye with significant pain
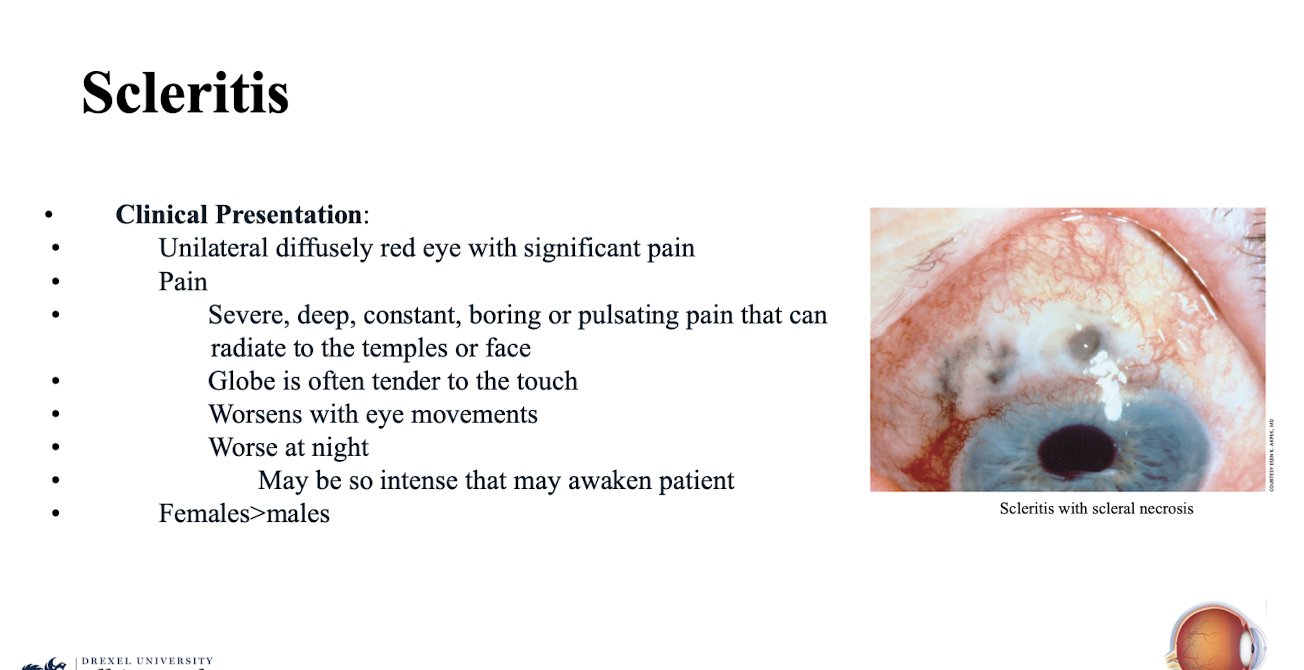
Describe the pain associated with Scleritis?
Severe; deep; constant; boring or pulsating pain that can radiate to the temples or face; worse at night; may be so intense that may awaken patient.
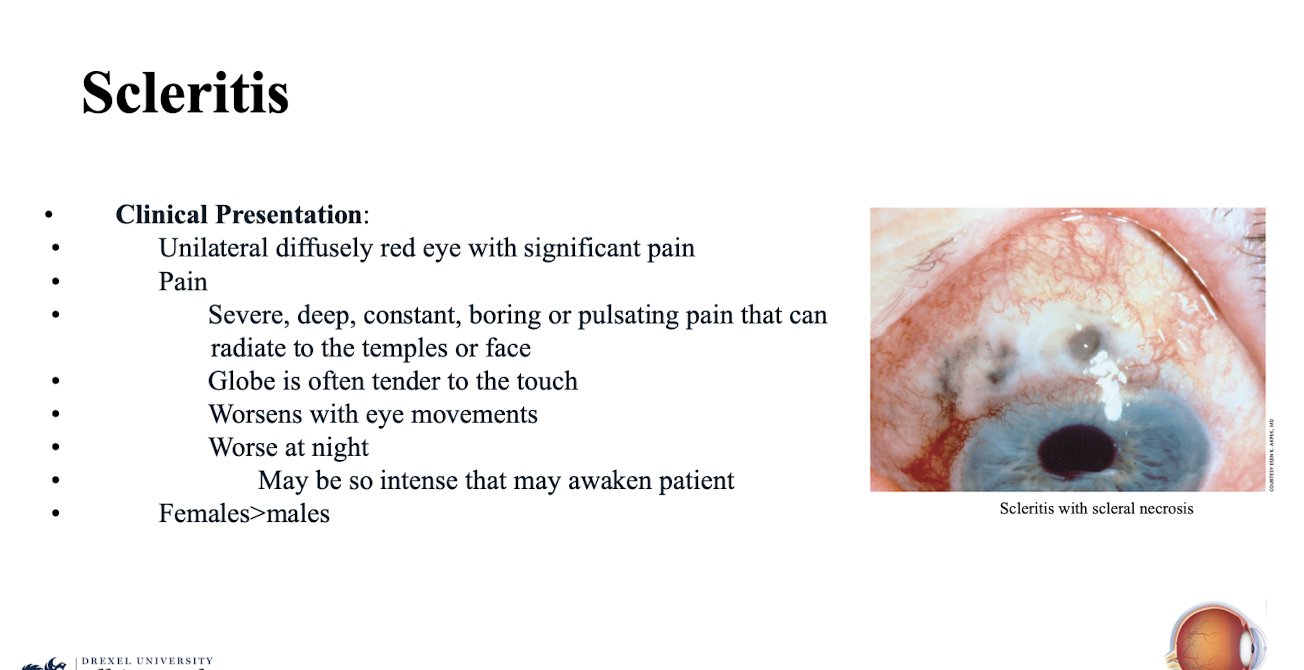
What physical finding is often noted in Scleritis related to pain?
Globe is often tender to the touch; worsens with eye movements.
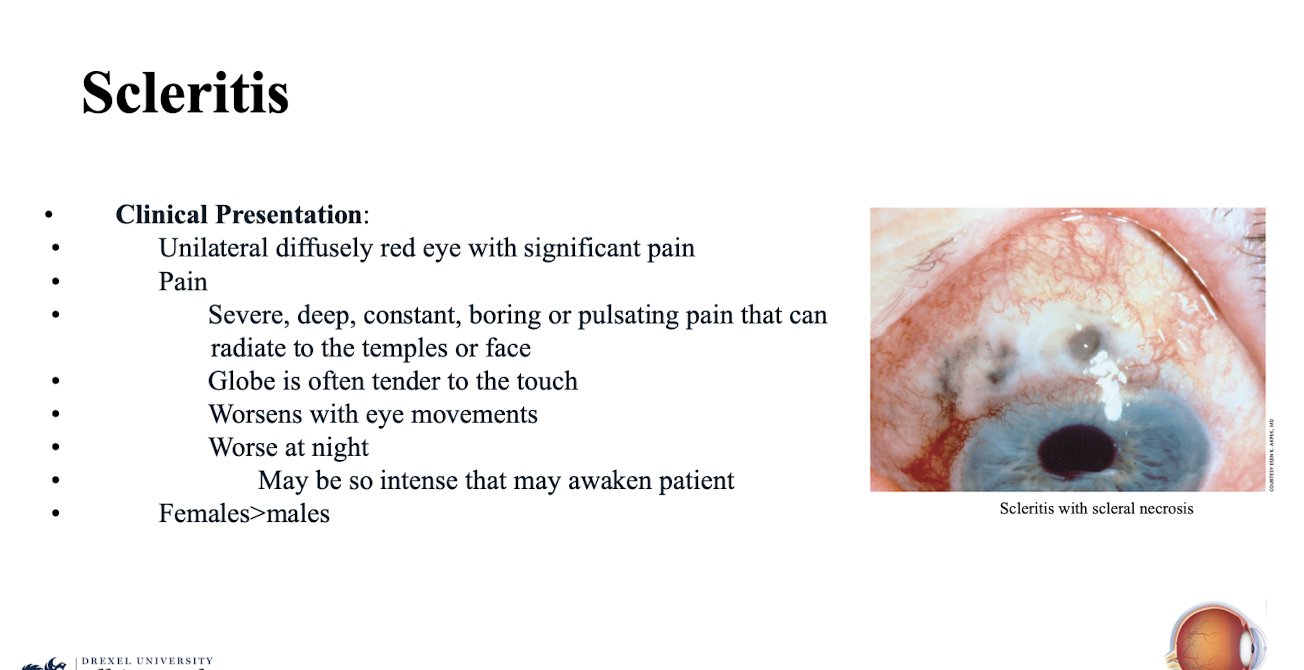
What demographic is more commonly affected by Scleritis?
Females>males.
What is Scleritis characterized by?
An uncommon condition characterized by cellular infiltration and edema of the entire thickness of the sclera resulting in significant pain
What serious complication can inflammation of the sclera lead to?
Ischemia and necrosis; eventually leading to scleral thinning and perforation of the globe.
What underlying condition is Scleritis frequently associated with?
Underlying systemic immunologic disease.
What type of infections can cause Scleritis?
Bacterial; fungal or protzoan infections. However most scleritis presentations are non-infectiousand it often occurs in the 4-6th decade of life
What diagnostic step is required to assess the full sclera in Scleritis?
Pull eyelids up to assess superior and inferior sclera.
What is the urgent treatment/management requirement for Scleritis?
Stat referral to ECP for evaluation and initiation of oral steroids.
What is the clinical presentation of a Subconjunctival Hemorrhage?
Unilateral; pain-less red eye; usually sectoral; blood beneath conjunctiva; may have chemotic appearance
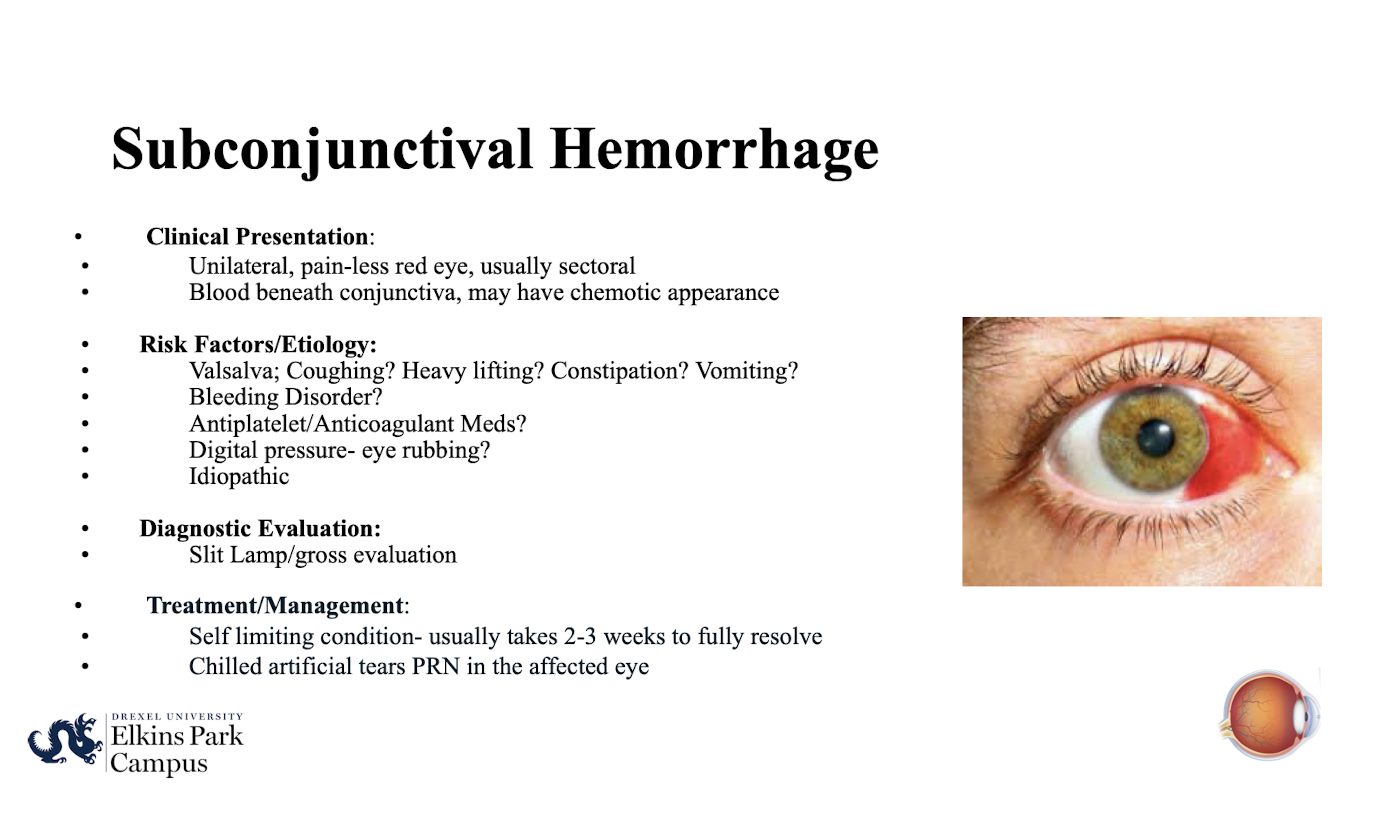
What are common risk factors or etiologies for Subconjunctival Hemorrhage (related to Valsalva maneuvers)?
Valsalva; Coughing; Heavy lifting; Constipation; Vomiting.
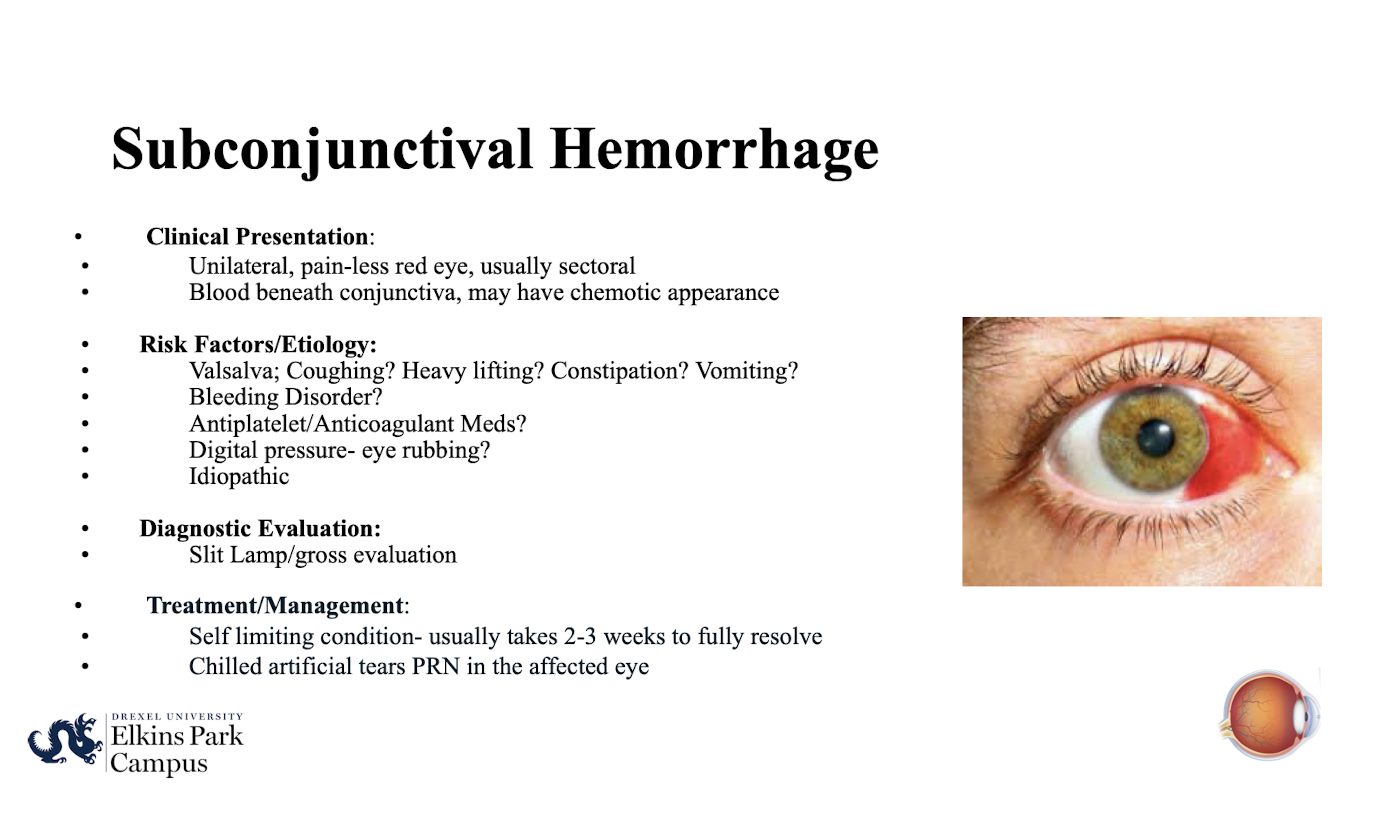
What medical conditions/factors should be ruled out in Subconjunctival Hemorrhage?
Bleeding Disorder; Antiplatelet/Anticoagulant Meds; Digital pressure- eye rubbing; Idiopathic.
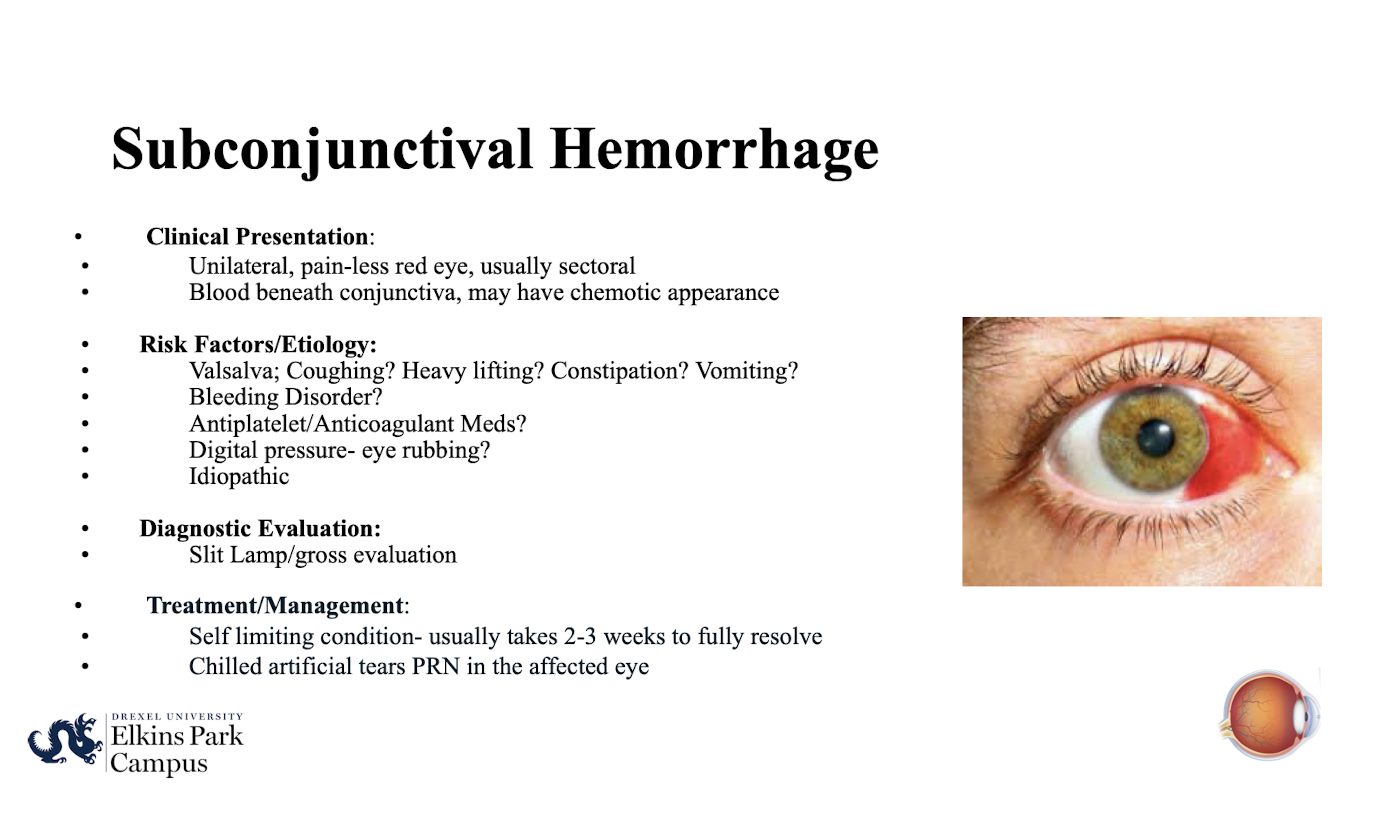
What is the typical course of a Subconjunctival Hemorrhage?
Self limiting condition- usually takes 2-3 weeks to fully resolve.
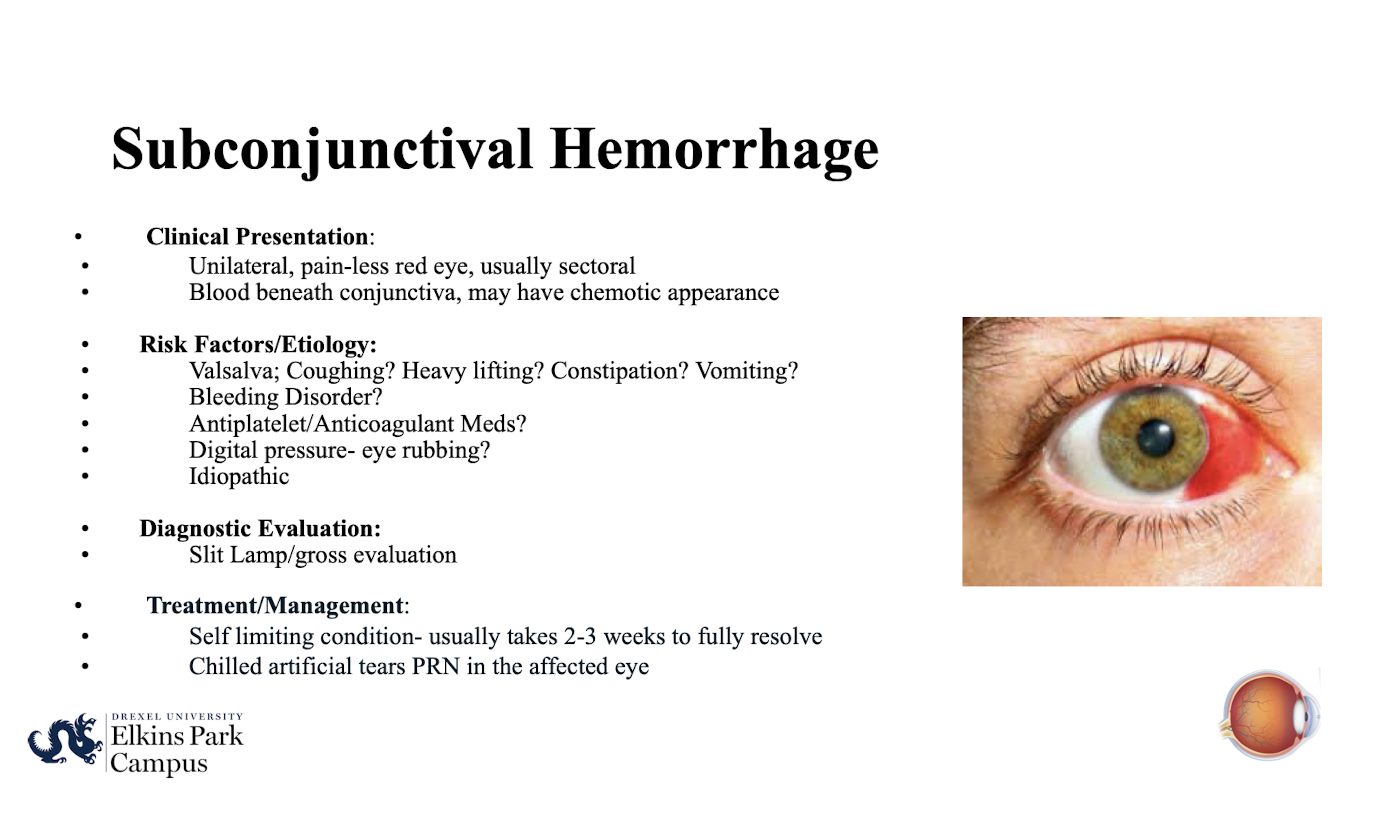
What treatment is recommended for Subconjunctival Hemorrhage?
Self limiting condition-usually takes 2-3 weeks to fully resolve. Chilled artificial tears PRN in the affected eye.
What is the clinical presentation of a Pinguecula?
Yellowish; elevated conjunctival nodule in the interpalpebral fissure. Common in persons over 35 years old
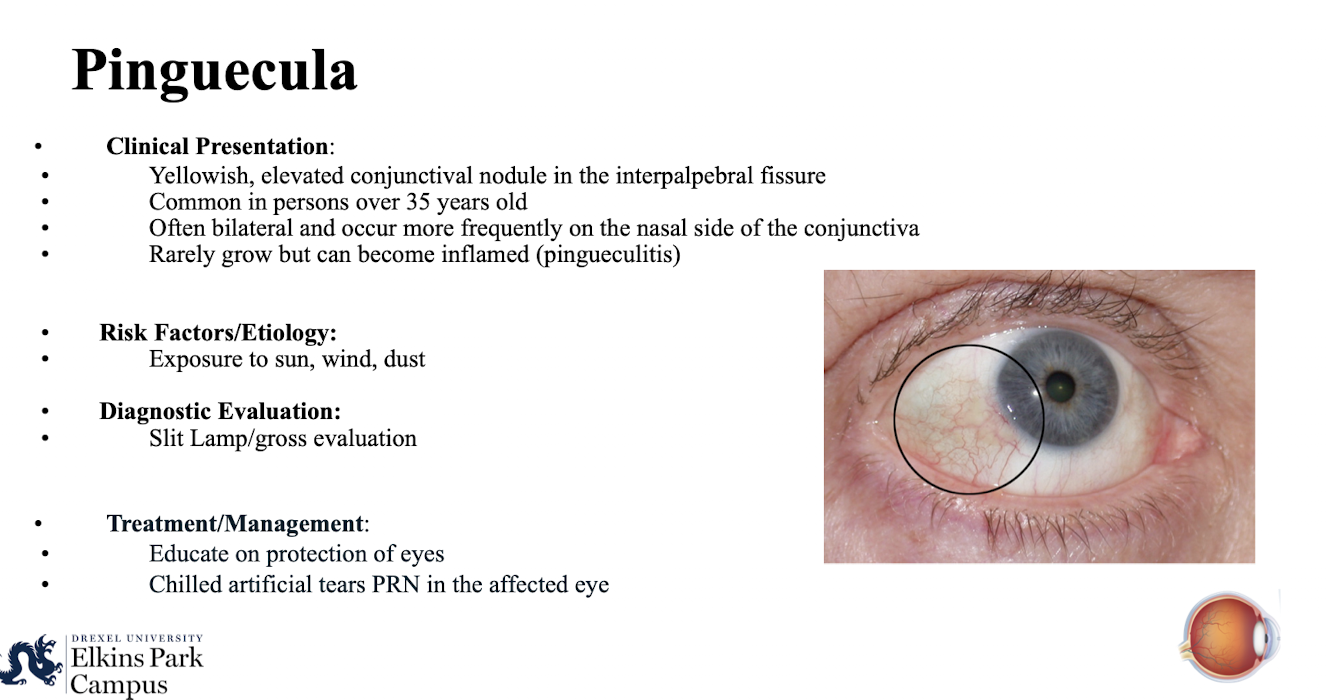
Where do Pingueculae typically occur?
Often bilateral and occur more frequently on the nasal side of the conjunctiva. rarely grow but can become inflamed (pingueculitis)
What is the term for an inflamed Pinguecula?
Pingueculitis.
What management is recommended for a Pinguecula?
Educate on protection of eyes; Chilled artificial tears PRN in the affected eye.
What are the main risk factors/etiologies for Pinguecula and Pterygium? How do you diagnose?
Exposure to sun; wind; dust.
Slit lamp/gross evaluation
What is the clinical presentation of a Pterygium?
Fleshy; triangular encroachment of the conjunctiva on the cornea
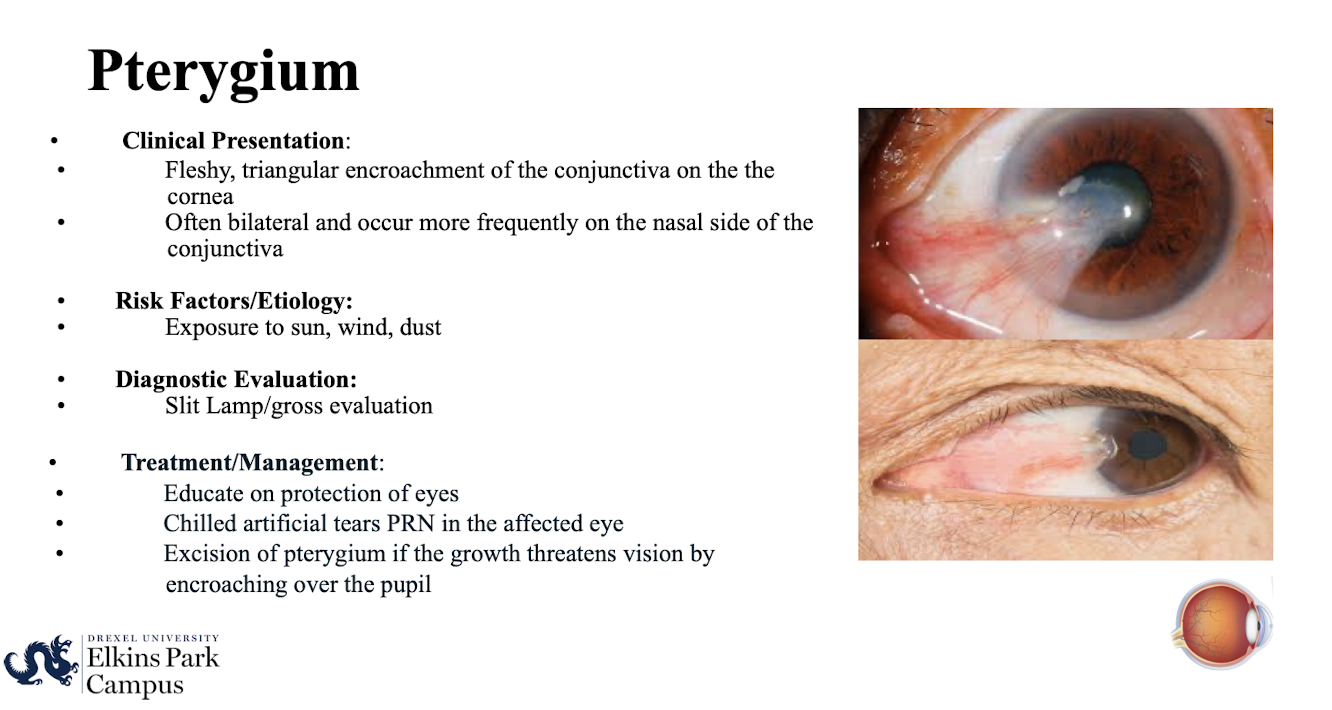
Where do Pterygia typically occur?
Often bilateral and occur more frequently on the nasal side of the conjunctiva.
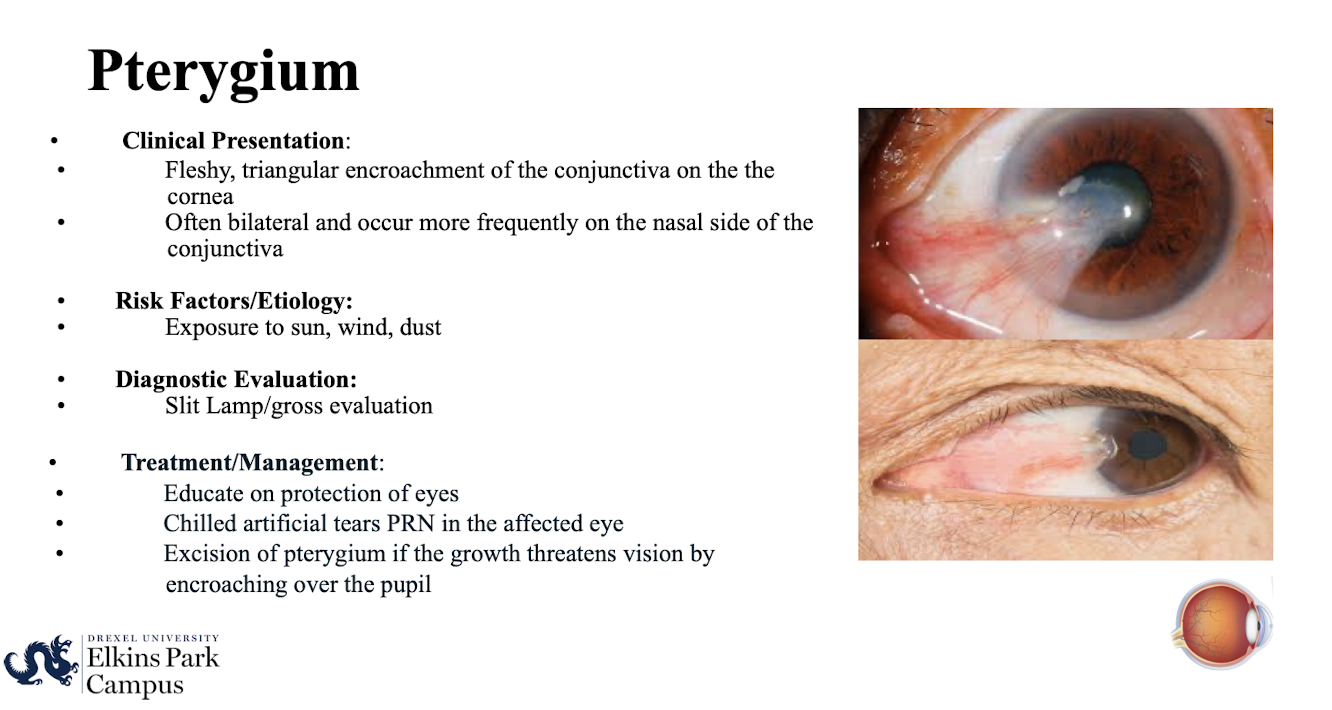
When is excision of a Pterygium indicated? What are the risk factors, diagnosis and treatment options?
If the growth threatens vision by encroaching over the pupil.
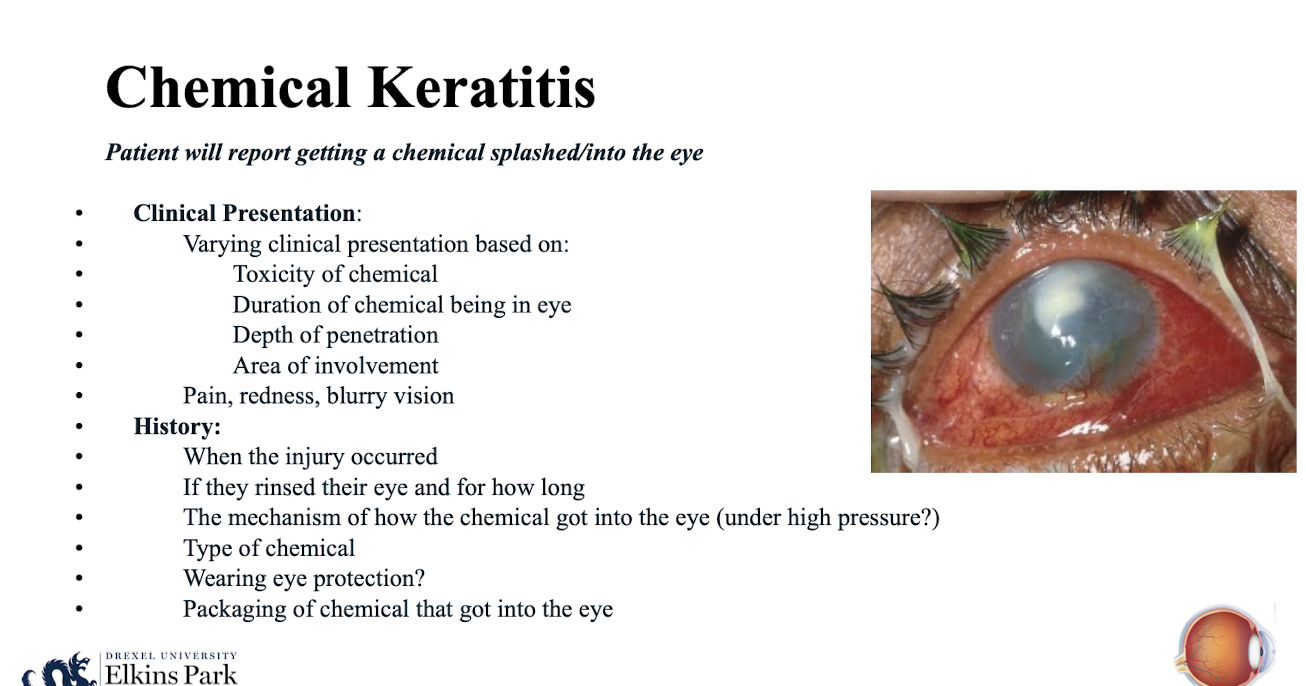
What is the defining report from a patient presenting with Chemical Keratitis?
Patient will report getting a chemical splashed/into the eye
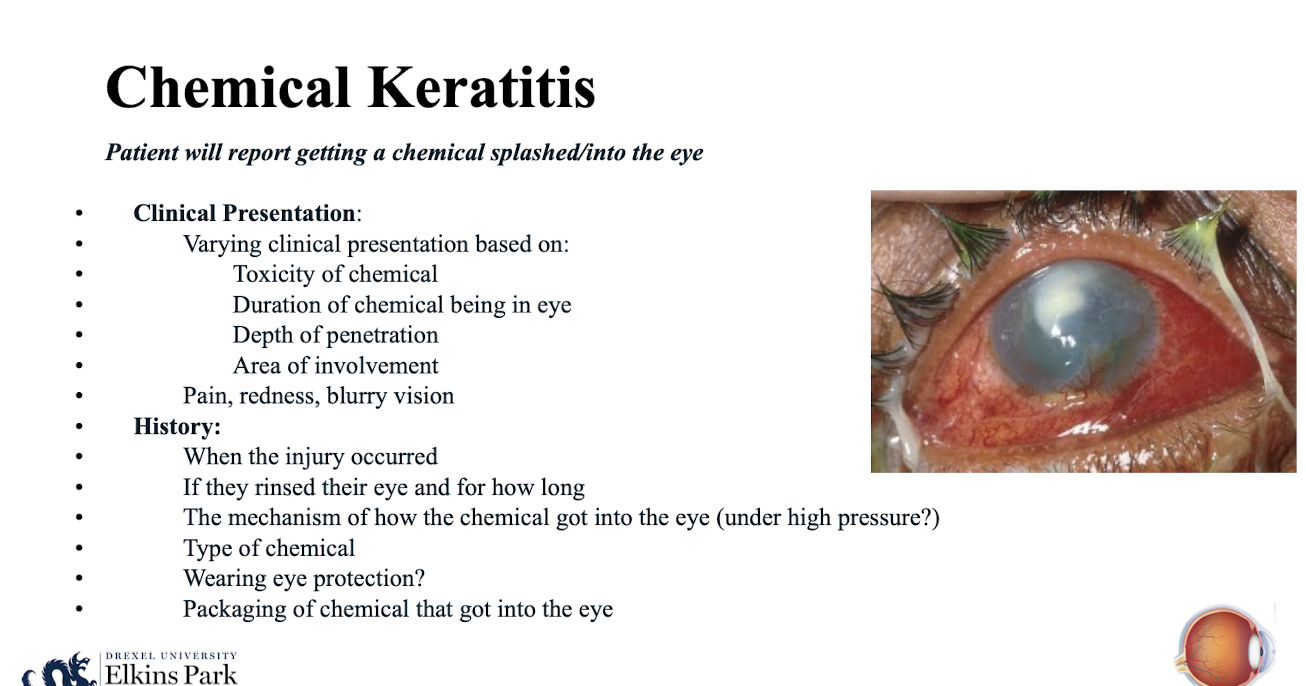
What factors determine the clinical presentation severity of Chemical Keratitis?
Toxicity of chemical; Duration of chemical being in eye; Depth of penetration; Area of involvement.