Week 10 - Protozoan part 2
1/78
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
79 Terms
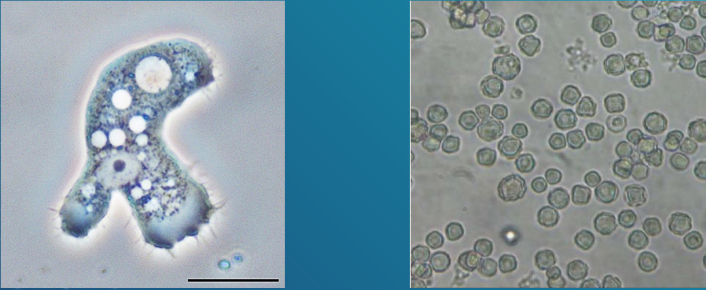
Acanthamoeba
It usually causes infection in immunocompromised patients.
It is a free-living amoeba that causes inflammation of the brain substance and its meningeal coverings (meningoencephalitis)
Found widely in soil, contaminated freshwater lakes, and other water environment
It is able to survive in cold water
Infective stage is the cyst; wjile pathogenic stage is the trophozoite
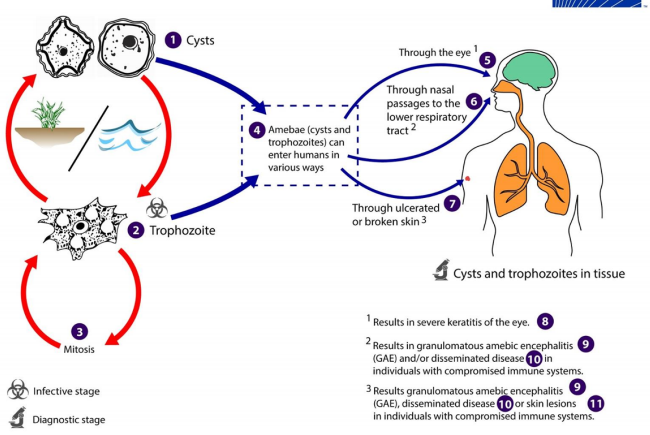
Aspiration or nasal inhalation
Direct invasion in the eye
Swimming in contaminated water
Contact lenses
Contaminated tap water
Inhalation from dust with cyst
acanthamoeba can be acquired through:
life cycle of Acanthamoeba
Granulomatous amoebic encephalitis
Infections among immunocompromised individuals
Parasite produces ___ and brain abscesses
Symptoms develop slowly and may include: headache, seizures, stiff neck, nausea and vomiting
The brain lesions may contain both the trophozoites and the cysts
In rare instances. it may spread in the kidneys, pancreas, prostate, and uterus
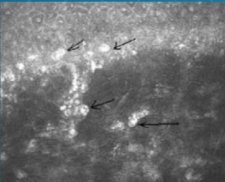
Keratitis (acanthamoeba)
Infection of the cornea of the eye
Symptoms include severe eye pain, and vision problems. Loss of vision may occure due to perforation of the cornea.
cerebrospinal fluid
finding both acanthamoeba trophozoites and cysts in the ___ as well as brain tissue and corneal scrapings.
Calcofluor white
a stain usually used to demonstrate fungi, may be used to demonstrate the acanthamoeba in corneal scraping specimens
Fluorescent microscopy of corneal scrapings
Pentamidine
Ketoconazole
Flucytosine
medicines for infections by acanthamoeba
Topical miconazole
Chlrhexidine
Itraconazole
Rifampicin
Propamidine
medicine for eye and skin involvement against acanthamoeba
Propamidine
medine with a best success record for acanthamoeba
Prevented through adequate boiling of water
Regular disinfection of contact lenses is also advised
Contact lens wearers are also advised to avoid using homemade non-sterile saline solutions
prevention and control for acanthamoeba
Naegleria
Classified as a free-living protozoan
Found worldwide in soil and contaminated water environment
Can survive in thermal spring water
Known pathogen worldwide is Naegleria fowleri, which is the only amoeba with 3 identified morphologic forms - trophozoites, flagellate, and cyst forms
The trophozoite: exhibits amoeboid motility, “slug-like'.
Flagellate Form: pear-shaped; equipped with 2 flagella that is responsible for the parasite’s jerky or spinning movement.
Cyst: non-motile form
>The amoeboid trophozoite form is however the only form that is known to exist in humans

Life Cycle of Naeglaria fowleri
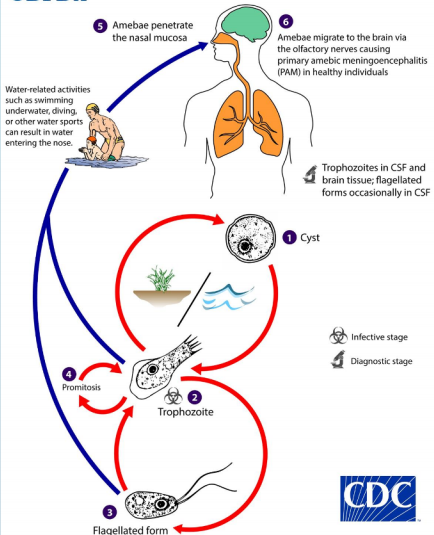
Epidemiology and Pathogenesis of Naeglaria
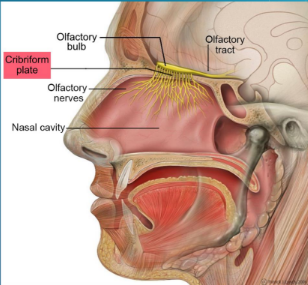
Usually acquired transnasally when swimming in contaminated
Parasite penetrates the nasal mucosa and cribriform plate, enters the central nervous system, and produces a rapidly fatal meningitis and encephalitis (primary amoebic meningoencephalitis)
Unlike Acanthamoeba, the parsite produces infection in otherwise healthy individuals, usually children.'
In some instances, the parasite may be acquired trhough inhalation of dust containing the parasite
The entire life cycle of the parasite (amoeboid trophozoites > Flagellate trophozoite > amoeboid trophozoites > cyst form) occures entirely in the external environment.
Asymptomatic infection (Naegleria)
The most common clinical preentation in patients with colonization of the nasal passages.
Primary Amoebic Meningoencephalitis (PAM)
The result of colonization of the brain by the amoeboid trophozoites leading to rapid tissue destruction
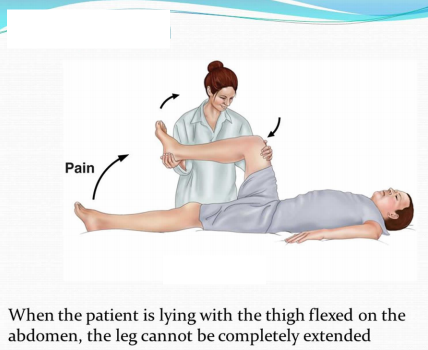
Symptoms: sore throat, nausea, vomiting, fever and headache. May eventually develop meningeal irritation (e,g, Kernig’s sign), as well as alterations in their senses of smell and taste.
If untreated, patients may die within one week after onset of symptoms.
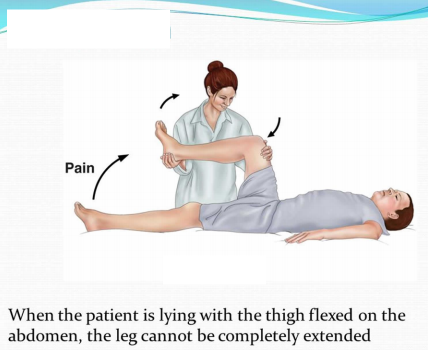
Kernig’s sign
Cerebrospinal fluid
finding of the amoeboid trophozoites (Naeglaria) in the __
Amphotericin B
Treatment of choice of Naeglaria is ___ in combination with miconazole and rifampicin
But treatment is ineefective because of its rapidly fatal course. However, some patients have been shown to recover from infection due to early detection and initiation of treatment.
Prevention of contamination of water sources
Adequate chlorination of swimming pools and hot tubs
Prevention and Control (Naeglaria)
Hemoflagellates Leishmania spp.
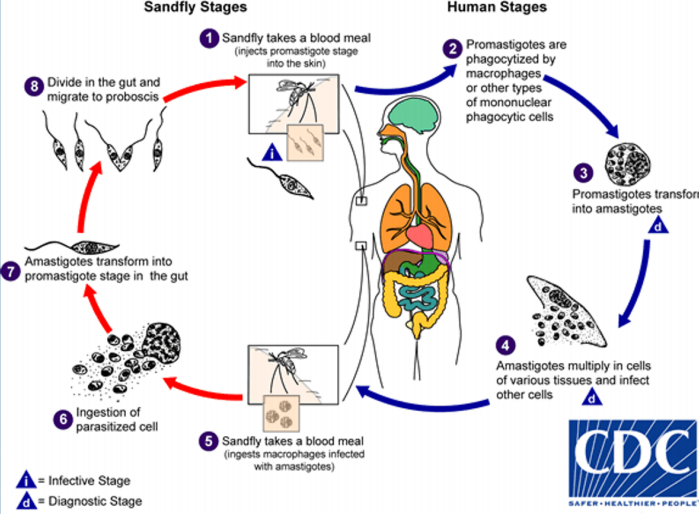
Life cycle of the parasite involves a vector, the female sandly of the Phlebotomus and Lutzomyia genera
They are the obligate intracellular parasites. It has 3 morphologic forms: amastigote, promastigote, and epimastigote.
The infective stage is promastigote
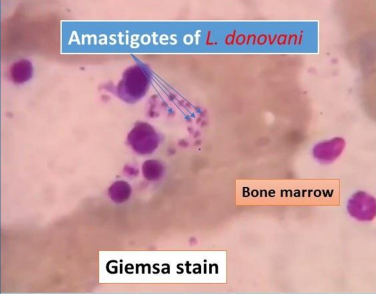
The pathogenic stage and diagnostic form is amastigote.

Life Cycle of
Hemoflagellates Leishmania spp.
Epidemiology and Pathogenesis
Has a worldwide distribution. Natural reservoirs include rodents, ant eaters, dogs, and cats.
In endemic areas, the parasite may be transmitted in human-vector-human cycle.
3 major strains of Leishmania:
Leishmania dinivani (visceral leishmaniasis)
Leishmania tropica (cutaneous leishmaniasis); and
Leishmania braziliensis (mucocutaneous leishmaniasis).
Leishmania dinivani
Leishmania tropica
Leishmania braziliensis
3 major strains of Leishmania
Leishmania donovani Complex
Is the causative agent visceral leishmaniasis (also known as kala-azar or dumdum fever)
The complex consists of:
L. donovani chagasi
L. donovani donovani
L. donovani infantum
The promastigote is injected into the human host through bite of the sandfly. After entry into the host, it loses its flagella, is engulfed by macrophages, and transforms into amastigotes
The organs of the reticuloendothelial system (liver, spleen and bone marrow) are the most severly affected
L. donovani chagasi
L. donovani donovani
L. donovani infantum
Leishmania donovani Complex consist of
L. donovani chagasi
is mainly seen in Central America (mainly Mexico, West Indies, and South America) and is transmitted by the Lutzomiya sandfly
L. donovani donovani
found in parts of Africa and Asia (Thailand, India, China, Burma, and East Pakistan) and is transmitted by the Phlebotomus sandfly
L. donovani infantum
also transmitted by Phlebotomus sandfly and is found mainly in Mediterranean Europe, Near East and Africa.
2 weeks to 18 months
After incubation period of ____ , the disease beings with intermittent fever, weakness and weight loss
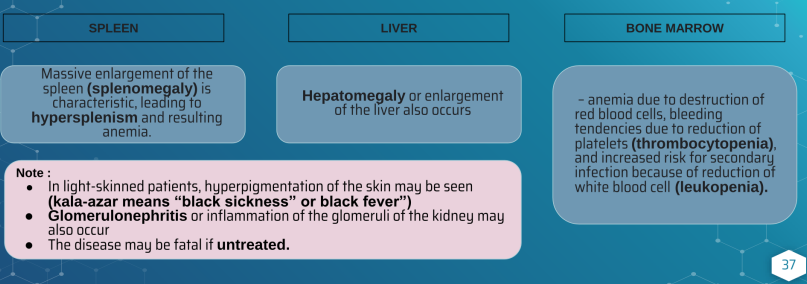
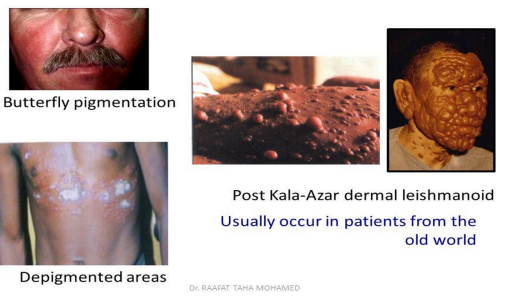
Skin changes in visceral leishmaniasis
Montenegaro skin test
Screening test for Hemoflagellates Leishmania spp. is called ___. This test is similar to the tuberculin skin test for the diagnosis of tuberculosis
It is used as screening for large population at risk but not used for diagnosis
Definitive diagnosis is done by demonstration of the amstigote from Giemsa stained slides of specimen from blood, bone marrow, lymph nodes, and biopsies of infected areas.
Culture of blood, bone marrow, and other tisues may also be done, which will show the promastigote forms.
Serologic tests are now available such as indirect fluorescent antibody (IFA), enzyme-linked immunosorbent assay (ELISA), or direct agglutination test (DAT).
Liposomal amphotericin B (Ambisome)
drug of choice for Hemoflagellates Leishmania spp is _____
Sodium stibogluconate
the medicine for Hemoflagellates Leishmania spp is ____ jas also been found to be effective but the development of resistance may occur.
gamma interferon in combination with pentavalent antimony
other patients with leishmaniasis have shown favourable response to__
Control of the vector population is important in the prevention of infection
The use of repellents, protective clothing, and installation of screens may be helpful
Prompt treatment of infected humans is essential to help halt the spread of the disease
Prevention and Control of Hemoflagellates Leishmania spp
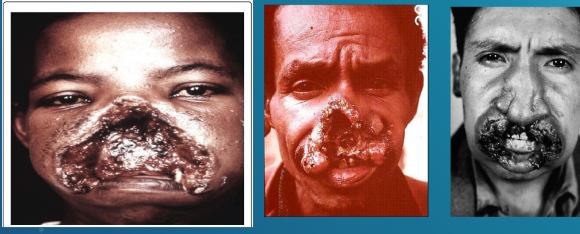
Leishmania braziliensis Complex
Is the causative agent of mucocutaneous leishmaniasis which involves skin, cartilage, and mucous membranes
Infection with it occurs most commonly in Brazil and Central America, primarily in construction and forestry workers
The complex consist of:
L. panamensis (Panama and Colombia)
L. peruviana (Peruvian Andes
L. guyanensis (The Guianas, parts of Brazil and Venezuela
Infection is transmitted by sandflys (Lutzomyia and Psychodopigus) through skin bite.
The promastigotes invade the reticuloendothelial cells where they transform into amastigotes (diagnostic stage)
Reproduction of the amastigotes result in tissue destruction. The amastigotes are taken up by the vector during a blood meal and are transformed into promastigotes.
Mucocutaneous Leishmaniasis
also called espundia, begins with a papule at the site of insect bite, then forms metastatic lesions, usually at the mucocutaneous junction of the nose and mouth
Disfiguring granulomatous, ulcerating lesions destroy the nasal cartilage (tapur nose) but not the adjacent bone.
Death can occur from secondary infections.
Laboratory Diagnosis of mucocutaneous leishmaniasis
Sodium stibogluconate
most widely used treatment for mucocutaneous leishmaniasis is ____, although resistnace has been shown to develop
Liposmal Amphotericin B
Oral antifugal drugs (Fluconazole, ketoconazole, and itraconazole)
Alternative drugs for mucocutaneous leishmaniasis are:
The most important preventive measure is the control of the insect vector
Measures should be undertaken to protect individuals from sandfly bites using netting, window screens, protective clothing, and insect repellents
Prompt treatment can also help prevent spread of the disease
Prevention and Control for Leishmania braziliensis Complex
Leishmania tropic complex
The complex consists of:
L. tropica
L. aethiopica
L. major
These are the causative agents of what is referred to as Old World cutaneous leishmaniasis
The life cycle of it is similar to what of L. braziliensis. All three members of the complez are transmitted by the Phlebotomus sandfly and primarily attacks the human lymphoid tissue of the skin
Old World Cutaneous Leishmaniasis
Is also known as Oriental sore, and Baghdad or Delhi boil.
It is characterized by one or several pus-containing ulcers that may heal spontaneously
Initial lesion: small, pruritic red papule at the bite site.
In patients with allergy and hypersensitivity responses, spontaneous healing does not occure.
>Thick skin plaques with multiple nodules may develop especially on the limbs and face.

Laboratory Diagnosis for Leishmania tropic complex
Microscopic examination of Giemsa-stained slides of fluid aspirated from beneath the ulcer bed is the usual diagnostic procedure of choice. Reveals the typical amastigotes.
Culture of specimen will show the promastigote form
Serologic tests are also available
Treatment for Leishmania tropic complex
The drug of choice is sodium stibogluconate
Steroids with application of heat to the infected lesions may be used.
Other alternative drugs are meglumine antimonite, pentamidine, and oral ketoconazole
Paromomycin ointment may be helpful in the healing of the ulcers
Prevention and Control for L. tropica
Preventive measures same with forms of leishmaniasis
However, unlike the other leishmania, a vaccine has been developed against it which is currently undergoing clinical trials.
Trypanosoma spp.
Are also hemoflaggellates like Leishmania. The major difference between the two lies in their diagnostic stages, which is the amastigote for Leishmania and the trypomastigotigot for the trypanosome
The trypomastigotes are curved, assuming the shape of letters C, S, or U.
The trypomastigotes are visible in the peripheral blood

Trypanosoma cruzi
Primarily found in South and Central America
Transmitted by the bite of the reduviid or triatomid bud (Triatoma or “cone-nose” bug).
It is transferred to a human host when feces of the bug containing the infective trypomastigotes is deposited near the bite site.
The feces are then introduced into the bite site when the host scratches the bite area.
Other routes of transmission include blood transfusion, sexuak intercourse, transplacental transmission, and through the mucous membranes, when the bite is near the eye or mouth.
Humans and animals (domestic cats and dogs, and wild species such as armadillo, raccoon, and rat) serve as resevoir hosts.

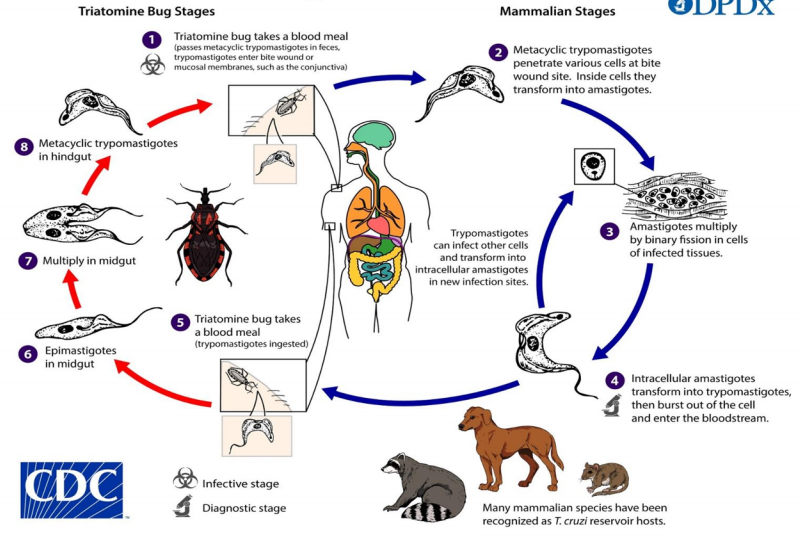
Life cycle of Trypanosoma cruzi
Chagas Disease (American Trypanosomiasis)
The acute phase begins with a nodule (chagoma) near the bite size; also with unilateral swelling of the eyelid with conjuctivitis (Romana’s sign)
The eyelid swelling may be due to the bug feces being accidentally rubbed into the eye
This is accompanied by fever, chills, malaise, myalgia, and fatigue.
Patients may recover or may enter the chronic phase.
Chronic Phase: Hepatosplenomegaly, enlargement of lymph nodes (lymphadenopathy), and myocarditis with cardia arrhythmia characterize the chronic phase of Chagas disease.
Cardiac muscle is the most frequently and most severly affected tissue
Loss of tone of the colon and esophagus due to destruction of the Auerbach’s plexus may lead to abnormal dilatation of these organs, called megacolon and megaesophagus; respectively
CNS involvement may also be seen in the form of meningoencephalitis and cysts
Death may occur due to cardia failure and arrhythmias
Laboratory Diagnosis of Trypanosoma cruzi
benznidazole
nifurtimox
Drug of choice for Trypanosoma cruzi are ___ but these are less effective during the chronic phase of the disease
Allopurinol
Ketoconazole
Alternative agents for Trypamosoma cruzi are ___
Protection from the bite of the reduviid bug, improvement of housing conditions, and insect control
Education regarding the disease and its transmission is also helpful
prevention and control for trypamosoma cruzi
trypanosoma brucei gambiens and Trypanosoma brucei rhode
Two species are similar in morphology and life cycle
Involce the tsetse fly (Glossina) as the vector
Resevoir
Humans: for T. brucei gambiense;
Domestic animals (especially cattle) and wild animals serve as the resevoir for T. brucie rhodesiense
The infective and pathogenic stage is the trypomastigote
T. gambiense infection: (West African or Gambian Sleeping Sickness) is chronic while;
T. rhodesiense infection: (East African or Rhodesian Sleeping Sickness) is more rapidly;
The disease is endemic in sub-Saharan African is the natural habitat of the tsetse fly. T. gambiense causes disease along the water courses in West Africa while T. rhodesiense causes disease mostly in the arid regions of East Africa.
Life Cycle of trypanosoma brucei gambiens and Trypanosoma brucei rhode

African Sleeping Sickness
The initial lesion is an indurated ulcer called thancre at the site of the insect bite
Intermitten weekly fever and lymphadenopathy then develop.
Enlargement of the posterior cervical lymph nodes (Winterbottom’s sign) is commonly seen
Other manifestations: red rash accompanied by pruritus, localized edema, and a delayed pain sensation (Kerandel sign)
The encephalitis is characterized by headache, insomia, and mood changes
muscle tremors, slurred speech, and apathy follow, progressing to somnolence (sleeping sickness) and coma
Untreated disease is fatal
Laboratory Diagnosis of trypanosoma brucei gambiens and Trypanosoma brucei rhode
melarsoprol
suramin
pentamidine
eflornithine
medicines for trypanosoma brucei gambiens and Trypanosoma brucei rhode are ___
The choice of drug will depend on whether the patient is pregnant or not, the age of the patient, and the stage of the disease.
Involve protection against bite of the fly
Use netting and protective clothing are recommended
Use of fly traps and insecticides may be helpful
Clearing forest around the villages are also helpful measures
Prevention and Control of trypanosoma brucei gambiens and Trypanosoma brucei rhode
Plasmodium spp.
Malaria is the caused by five plasmodia species: Plasmodium vivax, Plasmodium malrie, PLasmodium ovale, Plasmodium knowlesi, and Plasmodium falciparum
The vector and definitive host is the female Anopheles mosquito.
The sexual cycle (sporogony) occurs primarily in mosquitos; and the asexual cycle (schizogony) occurs in humans (intermediate hosts)
Occurs worldwide, primarily in tropical and subtropical areas, especially in Asia, Africa, and Central and South America
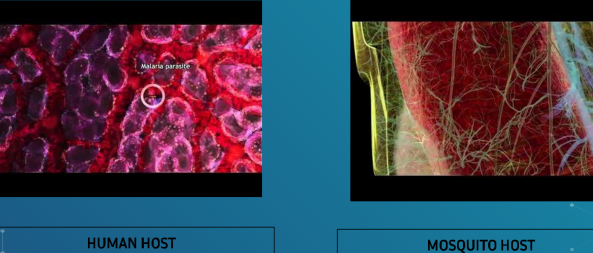
Malaria Life Cycle
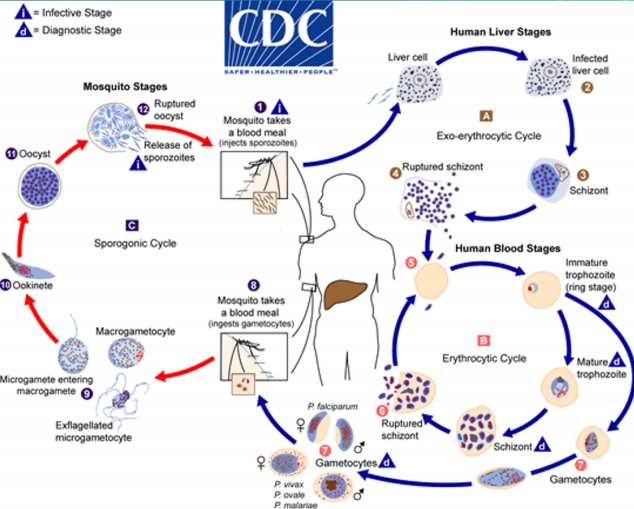
Exoerythrocytic phase
The infective stage is the sporozoite from the saliva of the biting mosquito, which is taken up by the live cells
Multiplication of sporozoites into merozoites occur during this stage
P. vivax and P. ovale produce a latent form (called hypnozoite or sleeping form) in the liver which is the cause of the relapse or recrudescence seen in vivax and ovale malaria
Erythrocytic phase
Merozoites (pathogenic stage) are re relesed from liver cells and infect the red blood cells
The parasites life cycle now enters this phase. These merozoites multiply and are eventually released to infect other red blood cells
The periodic release of merozoites causes the typical recurrent symptoms seen in malaria patients
Some merozoites then develop into microgametacytes (male gametocytes) and macrogametocytes (female gametocytes)
The gametocyte-containing red blood cells are ingested by the mosquito during feeding.
Sexual reproduction then ensues
female mosquito vector
Main mode of transmission of malaria
black water fever
the dark color of the patient’s urine is due to kidney damage giving rise to the term
P. falciparum
causes malignant tertian malaria since it causes severe infection which is potentially life-threatening due to extensive brain (cerebral malaria) and kidney damage
Tertian Malaria
48 hours malaria
Quartan malaria
72 hours
Toxoplasma gondii
defenitive host: domestic cat or other felines
intermediate host: humans and other mammals
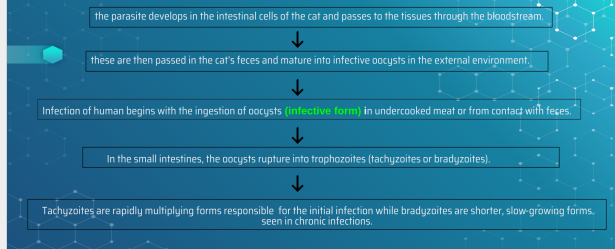
Epidemiology and Pathogenesis of
Toxoplasma gondii
Toxoplasmosis (Infection in immunocompetent individuals)
Usually asymptomatic
Acute infection may manifest non-specific symptoms such as chills, fever, headache, and fatigue'
Thia may be accompanied by inflammation of lymph nodes (lymphadenitis)
Chronic infection may manifest with lymphadenitis, hepatitis, myocarditis, and encephalomyelitis
Chlorioretinitis leading to blindness may also occure
Toxoplasmosis (Congenital Infection)
Occurs in infants born to mothers who were infected during pregnancy
Infection during the first trimester of pregnanacy may result to miscarriage, stillbirth, or severe infection (encephalitis, microcephaly, hydrocephalus, mental retardation, and pneumonia).
If the infant acquires during the last trimester, symptoms may not develop until months to years after delivery
The most common manifestation is chorioretinitis with or without blindness
Toxoplasmosis (infection in immunocompromised hosts)
Usually manifest with neurologic symptoms similar to patients with encephalopathy, meningoencephalitis, or brain tumors.
Reactivation of latent toxoplasma infection is common. Other sites of infection include the lungs, eye, and testes
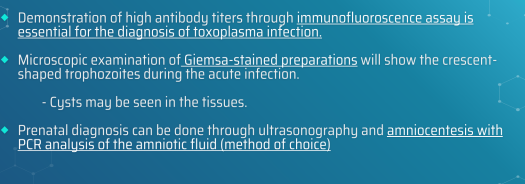
Toxoplasmosis (Laboratory Diagnosis)
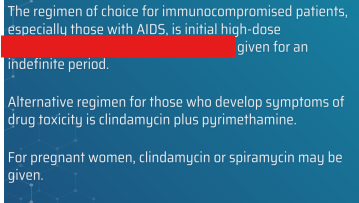
Pyrimethamine plus sulfadiazine
treatment for toxoplasmosis
THe most effective preventive measure is through adequate cooking of meat
Pregnant women should refrain from eating undercooked meat and should avoid contact with cats and refrain from handling litter boxes.
Cats should not be fed raw meat
prevention and control of Toxoplasma gondii