Evolution- The Natural History of the HIV Epidemic chp 1 pg1-30
1/13
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
14 Terms
How does it spread? How can it be slowed?
A new HIV infection occurs when bodily fluids carrying the virus from an infected person come into contact with a mucous membrane or the bloodstream of an uninfected person. HIV can be transmitted through semen, vaginal and rectal secretions, blood, and breast milk. Common modes of transmission include heterosexual and homosexual sex, oral sex, sharing needles, transfusion with contaminated blood, other unsafe medical procedures, childbirth, and breastfeeding.
The epidemic has spread differently in various regions. In sub-Saharan Africa and parts of south and southeast Asia, heterosexual sex has been the most common route of transmission. In Europe and North America, male-to-male sex and needle sharing among injection drug users have been the primary modes.
Medical interventions can help slow the spread of HIV. For example, the use of antiviral drugs can reduce the risk of transmission from an infected mother to her infant by about 40%. Circumcision can reduce the risk of men contracting HIV by about half, and antiviral vaginal gels offer similar benefits for women.
Drug Cocktail vs. one drug only
The initial treatment for HIV involved a single drug, such as azidothymidine (AZT), which interferes with the virus's reverse transcriptase enzyme, preventing it from completing its life cycle. While these single-drug therapies initially showed promise by halting the decline of T-cells, patients eventually stopped responding to the treatment.
The failure of a single drug is due to evolutionary principles. A population of HIV virions living inside a patient can evolve to become resistant to a single drug. HIV's reverse transcriptase is prone to mutation, and some mutations can alter the enzyme's structure, making it less susceptible to the drug's effects. As the drug kills off the susceptible virions, the drug-resistant mutants survive and reproduce, leading to a population of HIV that is no longer affected by the therapy. This process, which is a form of natural selection, can lead to a patient developing full-blown AIDS even while on the medication.
To combat this resistance, drug cocktail therapy, or highly active antiretroviral therapy (HAART), was introduced. This involves using multiple drugs that target different stages of the HIV life cycle, such as reverse transcriptase and protease inhibitors. This makes it extremely difficult for the virus to evolve resistance, because it would need to acquire multiple, simultaneous mutations that confer resistance to all the drugs in the cocktail. This is far less likely to occur than a single mutation that confers resistance to one drug.
Therapy and evolutionary principles
HIV therapy is a prime example of evolution in action. The virus's high mutation rate and rapid replication cycle create a vast amount of genetic variation. When a drug is introduced, it acts as a selection pressure. Virions with mutations that allow them to resist the drug's effects have a survival advantage, allowing them to replicate more successfully than their susceptible counterparts. Over time, this leads to the evolution of a drug-resistant viral population. The success of multidrug therapy is a direct application of evolutionary principles—by using multiple selection pressures (multiple drugs), the probability of the virus evolving resistance is dramatically reduced.
Are humans evolving due to HIV selection pressure?
The AIDS pandemic could, in principle, lead to the evolution of human populations. The CCR5-Δ32 allele is a specific genetic mutation that confers a degree of resistance to HIV. Individuals who are homozygous for this allele are highly resistant to HIV infection, while heterozygotes show some resistance. This allele is an example of an existing genetic variation that could be favored by natural selection in the presence of HIV.
Because HIV acts as a strong selective pressure, the frequency of the CCR5-Δ32 allele would be expected to increase in populations where HIV is prevalent. The textbook states that while this is a plausible scenario in theory, it is unlikely to lead to rapid evolution in any real human population at present. This is because the overall mortality rate from HIV, while devastating, is not high enough globally to cause a rapid, population-wide shift in allele frequency.
Why study evolution
Understand/insights into life and death
What is HIV, how does it spread, and how does it cause AIDS?
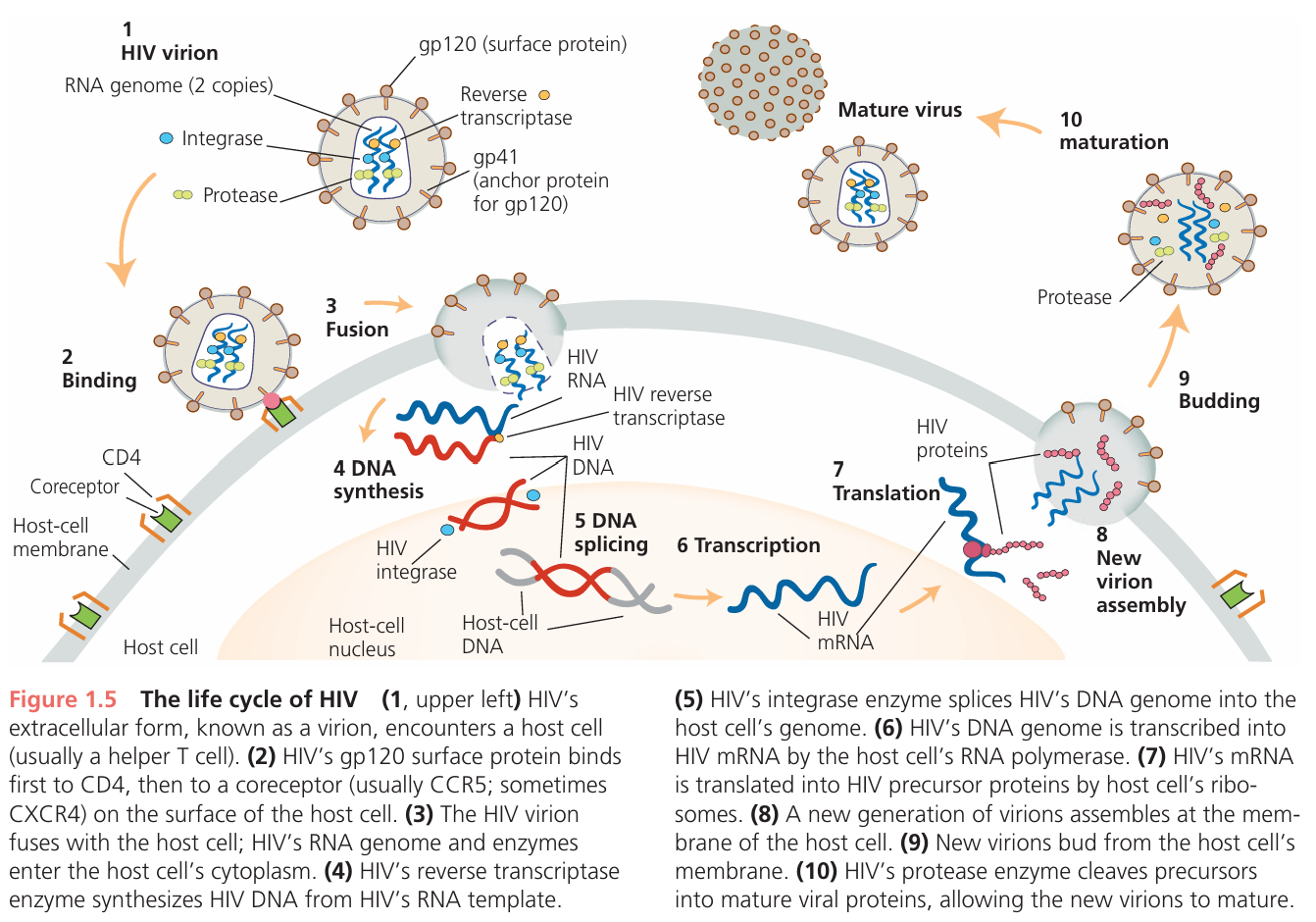
HIV is an intracellular parasite incapable of reproducing on its own. HIV invades specific types of cells in the human immune system. The virus hijacks the enzymatic machinery, chemical materials, and energy of the host cells to make copies of itself, killing the host cells in the process.
A new HIV infection starts when a bodily fluid carries the virus from an infected person directly onto a mucous membrane or into the bloodstream of an unin fected person. HIV travels via semen, vaginal and rectal secretions, blood, and breast milk (Hladik and McElrath 2008). It can move during heterosexual or homosexual sex, oral sex, needle sharing, transfusion with contaminated blood products, other unsafe medical procedures, childbirth, and breastfeeding.
HIV causes AIDS by specifically attacking immune cells called CD4 T cells (including helper T cells and memory T cells), which are essential for coordinating the entire immune response. The infection progresses through three phases in an untreated person:
Acute Phase: HIV replicates explosively, causing a high level of virus in the blood and a sharp drop in CD4 T cells, especially in the gut.
Chronic Phase: Virus levels may stabilize but continue to rise over time. The patient has few symptoms, but CD4 T cell counts gradually fall.
AIDS Phase: This begins when CD4 T cell counts drop below a critical level (200 cells/mm³). The immune system collapses, leaving the patient vulnerable to deadly opportunistic infections.
The process is complex and not solely due to the virus directly killing cells. A key mechanism is a vicious cycle:
HIV's initial attack on the gut damages the intestinal barrier, allowing bacteria to leak into the bloodstream.
This bacterial leakage, along with the HIV infection itself, causes chronic and widespread activation of the immune system.
While this immune response tries to fight the infection, it ironically helps HIV, which replicates best in activated immune cells. This intense, constant battle ultimately exhausts the immune system and permanently damages lymph nodes, where new T cells are made.
Over time, the body cannot replace lost CD4 T cells, leading to immunodeficiency (AIDS).
The text concludes that the logical way to stop HIV from causing AIDS is to prevent it from replicating, using antiviral drugs like AZT. However, it notes that using just one drug only offers temporary benefits.
Why do therapies using just one drug, and sometimes therapies using multiple drugs, work well at first but ultimately fail?
Are human populations evolving as a result of the HIV pandemic?
Where did HIV come from?
Why are untreated HIV infections usually fatal?
Who mostly had HIV
men who have sex with men
What reduces the rate of HIV transmission
-antiviral drugs (lowers risk that mothers will pass it to new borns, also effective between men to men)
-Circumcision reduces risk that men will get it, antiviral vaginal gels for women
-condoms
HIV life cycle
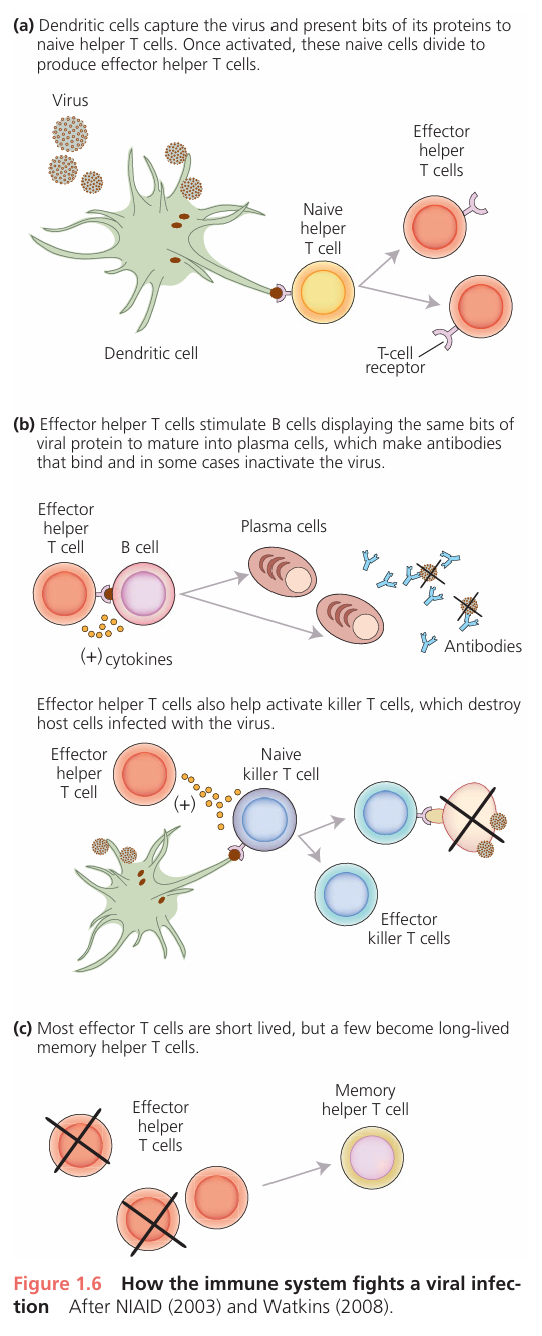
The life cycle includes an extracellular phase and an intra cellular phase. During the extracellular, or infectious phase, the virus moves from one host cell to another and can be transmitted from host to host. The extracel lular form of a virus is called a virion or virus particle. During the intracellular, or replication phase, the virus replicates. HIV initiates its replication phase by latching onto two proteins on the surface of a host cell. After adhering first to CD4, HIV attaches to a second protein, called a coreceptor. This leads to fusion of the virion’s envelope with the host’s cell membrane and spills the contents of the virion into the cell. The contents include the virus’s genome (two copies of a single-stranded RNA molecule) and two viral enzymes: reverse transcriptase, which transcribes the virus’s RNA genome into DNA; and integrase, which splices this DNA genome into the host cell’s genome. Once HIV’s genome has infiltrated the host cell’s DNA, the host cell’s RNA polymerase transcribes the viral genome into viral mRNA. The host cell’s ribo somes synthesize viral proteins. New virions assemble at the host cell’s membrane, then bud off into the bloodstream or other bodily fluid. Inside the new virions, HIV’s protease enzyme cleaves precursors of various viral proteins into functional forms, allowing the virions to mature. The new virions are now ready to invade new cells in the same host or to move to a new host. A notable feature of HIV’s life cycle is that the virus uses the host cell’s own enzymatic machinery—its polymerases, ribosomes, and tRNAs, and so on—in almost every step. This is why HIV, and viral disease in general, is so difficult to treat. It is a challenge to find drugs that interrupt the viral life cycle without also disrupting the host cell’s enzymatic functions and thus causing debilitating side effects. Effective antiviral ther apies usually target enzymes specific to the virus, such as reverse transcriptase and integrase.
Immune system and HIV
Your body tries to fight HIV the same way it fights any virus.
The Alarm: Special immune cells (dendritic cells) find the HIV virus and act like scouts. They grab a piece of the virus and take it to the "command center" (a lymph node).
Calling for Backup: In the command center, they show the virus piece to the "generals" of the immune system, called helper T cells. This activates the helper T cells.
Launching the Attack: The activated helper T cells start giving orders. They tell other parts of the immune system to fight:
They tell B cells to make antibodies, which are like sticky tags that attach to the virus to mark it for destruction.
They activate killer T cells, which hunt down and destroy your own body's cells that are already infected with the virus.
Creating Memory: After the fight, most of these helper T cells die off. But a few turn into "memory cells" that stay in your body, ready to react quickly if HIV shows up again.
The Big Problem with HIV:
The tricky part is that HIV specifically attacks and destroys the very same helper T cells that are trying to coordinate the fight. Over time, the virus slowly wins this battle, weakening the immune system and making it hard for the body to defend itself.