midterm 1
5.0(2)
5.0(2)
Card Sorting
1/26
Earn XP
Description and Tags
Last updated 12:21 AM on 12/14/22
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
27 Terms
1
New cards
Which of the following represent threats to our way of life?
a. Misinformation and willful ignorance
b. High uptake of vaccination
c. MMR vaccines and thimerosal
d. Smallpox vaccines
e. None of the above – I choose this option
a. Misinformation and willful ignorance
b. High uptake of vaccination
c. MMR vaccines and thimerosal
d. Smallpox vaccines
e. None of the above – I choose this option
a. Misinformation and willful ignorance
2
New cards
Which statement about vaccination is false:
a. Before vaccines, infectious diseases were rampant, damaging, and often deadly
b. Vaccines expose individuals to highly active and infectious microbes to elicit adaptive immunity
c. Vaccines expose individuals to non-dangerous and/or subdued microbes to elicit adaptive immunity
d. After widespread vaccination campaigns around the globe, common diseases like smallpox, polio, and measles dropped dramatically, if not eradicated.
e. Misinformation has led to unnecessary outbreaks due to a drop in vaccination rates
a. Before vaccines, infectious diseases were rampant, damaging, and often deadly
b. Vaccines expose individuals to highly active and infectious microbes to elicit adaptive immunity
c. Vaccines expose individuals to non-dangerous and/or subdued microbes to elicit adaptive immunity
d. After widespread vaccination campaigns around the globe, common diseases like smallpox, polio, and measles dropped dramatically, if not eradicated.
e. Misinformation has led to unnecessary outbreaks due to a drop in vaccination rates
b. Vaccines expose individuals to highly active and infectious microbes to elicit adaptive immunity
3
New cards
What is humoral immunity referring to?
a. The immunity driven by T lymphocytes, particularly cytotoxic T cells.
b. The immunity driven by soluble bacterial antigens
c. The immunity driven by phagocytes such as macrophages
d. The immunity driven by soluble immune molecules like antibodies
e. The immunity driven by a great sense of humour
a. The immunity driven by T lymphocytes, particularly cytotoxic T cells.
b. The immunity driven by soluble bacterial antigens
c. The immunity driven by phagocytes such as macrophages
d. The immunity driven by soluble immune molecules like antibodies
e. The immunity driven by a great sense of humour
d. The immunity driven by soluble immune molecules like antibodies
4
New cards
Which statement about adaptive vs. innate immunity is false?
a. Adaptive immunity is not germ-line encoded, but innate immunity is.
b. Adaptive immunity takes about a week to develop and build, while innate immunity is available for immediate action
c. Sequential infections (or booster shots) lead to adaptive immunity with similar first and second responses, but very strong secondary response of innate immunity
d. Antibodies are part of the adaptive immune response, while pattern recognition receptors are part of the innate response
e. Adaptive immunity depends on genetic recombination in differentiating B and T cells to generate antigen receptors, while innate immunity depends on germ-line inherited receptors
a. Adaptive immunity is not germ-line encoded, but innate immunity is.
b. Adaptive immunity takes about a week to develop and build, while innate immunity is available for immediate action
c. Sequential infections (or booster shots) lead to adaptive immunity with similar first and second responses, but very strong secondary response of innate immunity
d. Antibodies are part of the adaptive immune response, while pattern recognition receptors are part of the innate response
e. Adaptive immunity depends on genetic recombination in differentiating B and T cells to generate antigen receptors, while innate immunity depends on germ-line inherited receptors
c. Sequential infections (or booster shots) lead to adaptive immunity with similar first and second responses, but very strong secondary response of innate immunity
5
New cards
Which statement on granulocytes is incorrect:
a. Neutrophils are a type of granulocytes
b. Neutrophil granules contain antimicrobials that are secreted onto bacteria
c. Neutrophils belong to the myeloid lineage
d. Neutrophils can generate reactive oxygen species and “bleach” to kill microbes
e. All statements are correct. I have to pick e
a. Neutrophils are a type of granulocytes
b. Neutrophil granules contain antimicrobials that are secreted onto bacteria
c. Neutrophils belong to the myeloid lineage
d. Neutrophils can generate reactive oxygen species and “bleach” to kill microbes
e. All statements are correct. I have to pick e
e. All statements are correct. I have to pick e
6
New cards
Natural killer cells target host cells for death if:
a. A host cell expresses MHC-I on its surface
b. A host cell fails to express MHC-I with an antigen on its surface
c. A host cell fails to express MHC-I on its surface
d. A host cell expresses MHC-II on its surface
e. A host cell expresses phosphatidylserine on its surface
a. A host cell expresses MHC-I on its surface
b. A host cell fails to express MHC-I with an antigen on its surface
c. A host cell fails to express MHC-I on its surface
d. A host cell expresses MHC-II on its surface
e. A host cell expresses phosphatidylserine on its surface
c. A host cell fails to express MHC-I on its surface
7
New cards
What can you say about the follicles in lymph nodes?
a. Follicles are not found in lymph nodes. They are found in the thymus and provide a niche to differentiate CD4+ and CD8+ T cells
b. They form a niche with fibroblastic reticular cell conduit to help T cells collide with antigen-presenting cells via MHC-II::peptide-TCR interactions
c. Follicles form niches for differentiation and maturation of myeloid cells
d. They form a niche with follicular dendritic cells with extensive cell protrusions to help B cells screen for BCR-cognate antigen interactions.
e. Follicles are found in bone marrow, not lymph nodes
a. Follicles are not found in lymph nodes. They are found in the thymus and provide a niche to differentiate CD4+ and CD8+ T cells
b. They form a niche with fibroblastic reticular cell conduit to help T cells collide with antigen-presenting cells via MHC-II::peptide-TCR interactions
c. Follicles form niches for differentiation and maturation of myeloid cells
d. They form a niche with follicular dendritic cells with extensive cell protrusions to help B cells screen for BCR-cognate antigen interactions.
e. Follicles are found in bone marrow, not lymph nodes
d. They form a niche with follicular dendritic cells with extensive cell protrusions to help B cells screen for BCR-cognate antigen interactions.
8
New cards
Which cell type helps license B cells expressing a BCR that recognizes a foreign antigen to become a plasma cell, i.e., an antibody-producing cell.
a. CD4+ T cell
b. CD8+ T cell
c. T regulatory cell (Treg)
d. Antigen-presenting cell
e. Mast cells
a. CD4+ T cell
b. CD8+ T cell
c. T regulatory cell (Treg)
d. Antigen-presenting cell
e. Mast cells
a. CD4+ T cell
9
New cards
You want to do an experiment to measure the total number of T cells per mL of blood of patients infected with COVID-19 versus individuals with no known infection. Using flow cytometry (as in Spangrude et al,), which antibodies against “Cluster of Differentiation” would you use?
a. Anti-CD3 antibodies
b. Anti-CD4 antibodies
c. Anti-CD8 antibodies
d. Anti-CD16 (a phagocytic receptor)
e. Anti-CD21, a BCR co-recepto
a. Anti-CD3 antibodies
b. Anti-CD4 antibodies
c. Anti-CD8 antibodies
d. Anti-CD16 (a phagocytic receptor)
e. Anti-CD21, a BCR co-recepto
a. Anti-CD3 antibodies
10
New cards
An antibody engineered to express a single Fab fragment and no Fc fragment will:
a. have reduced affinity for its cognate epitope
b. have reduced avidity for its cognate antigen
c. still be able to bind to Fc receptors
d. have bivalency towards its cognate antigen
e. be able to cluster Fc receptors
a. have reduced affinity for its cognate epitope
b. have reduced avidity for its cognate antigen
c. still be able to bind to Fc receptors
d. have bivalency towards its cognate antigen
e. be able to cluster Fc receptors
b. have reduced avidity for its cognate antigen
11
New cards
Receptor clustering upon ligand binding is important for many immune receptors primarily because it:
a. helps concentrate ligands to initiate extracellular signalling
b. helps with conformation changes on the receptor
c. helps concentrate weakly active Src-family kinases to turn them on and drive signal transduction
d. helps increase affinity of receptor-ligand binding
e. None of the above. I select this option
a. helps concentrate ligands to initiate extracellular signalling
b. helps with conformation changes on the receptor
c. helps concentrate weakly active Src-family kinases to turn them on and drive signal transduction
d. helps increase affinity of receptor-ligand binding
e. None of the above. I select this option
c. helps concentrate weakly active Src-family kinases to turn them on and drive signal transduction
12
New cards
The combined effect of IL-1 and IL-6 on macrophages is 10-times stronger than the effect of
IL-1 or IL-6 alone. Thus, the outcome of IL-1 and IL-6 can be said to be context-dependent.
What term best describes this concept here?
a. Antagonistic signalling
b. Redundant signalling
c. Pleiotropic signalling
d. Paracrine signalling
e. Synergistic signalling
IL-1 or IL-6 alone. Thus, the outcome of IL-1 and IL-6 can be said to be context-dependent.
What term best describes this concept here?
a. Antagonistic signalling
b. Redundant signalling
c. Pleiotropic signalling
d. Paracrine signalling
e. Synergistic signalling
e. Synergistic signalling
13
New cards
Which event below is not part of BCR signalling?
a. Phosphorylation of CD3 co-receptor subunits on their ITAM motif
b. Phosphorylation of Iga, Igb coreceptors on their ITAM motif
c. BCR clustering and recruitment to lipid rafts
d. Activation of Src-family tyrosine kinases
e. Recruitment of adaptor proteins to form a signalling complex
a. Phosphorylation of CD3 co-receptor subunits on their ITAM motif
b. Phosphorylation of Iga, Igb coreceptors on their ITAM motif
c. BCR clustering and recruitment to lipid rafts
d. Activation of Src-family tyrosine kinases
e. Recruitment of adaptor proteins to form a signalling complex
a. Phosphorylation of CD3 co-receptor subunits on their ITAM motif
14
New cards
Which of the following is NOT an event for B-cells after successfully generating a BCR-antigen signal and after being licensed by CD4+ T cells to expand into a clonal population.
a. The mRNA encoding the BCR subunits undergoes a different mRNA splicing event to produce soluble antibodies like IgG
b. Certain B cell clones will undergo antibody class switching by mRNA splicing or even genetic recombination
c. Specific clonal cells from the original activated B cell undergoes more genetic recombination to find new BCR sequences that bind to new epitopes
d. Certain B cells from this clonal population will differentiate into memory cells
e. All events above happen during B cell activation due to BCR-antigen signalling. I have to select this option as the only available option that makes sense.
a. The mRNA encoding the BCR subunits undergoes a different mRNA splicing event to produce soluble antibodies like IgG
b. Certain B cell clones will undergo antibody class switching by mRNA splicing or even genetic recombination
c. Specific clonal cells from the original activated B cell undergoes more genetic recombination to find new BCR sequences that bind to new epitopes
d. Certain B cells from this clonal population will differentiate into memory cells
e. All events above happen during B cell activation due to BCR-antigen signalling. I have to select this option as the only available option that makes sense.
c. Specific clonal cells from the original activated B cell undergoes more genetic recombination to find new BCR sequences that bind to new epitopes
15
New cards
If you wanted to develop new medicines to fight hyper-inflammatory diseases driven by the
AP-1 transcription factor, which proteins would you target?
a. Calcineurin phosphatase
b. Protein kinase C family
c. Phopholipase C family
d. The MAPK module
e. Ubiquitylation machinery
AP-1 transcription factor, which proteins would you target?
a. Calcineurin phosphatase
b. Protein kinase C family
c. Phopholipase C family
d. The MAPK module
e. Ubiquitylation machinery
d. The MAPK module
16
New cards
Cyclosporines and tacrolimus are common immunosuppressants prescribed to organ transplant recipients to cut the chances of organ rejection. Both these drugs inhibit calcineurin. Based on this, which molecular pathway is being suppressed to avoid organ rejection?
a. NFAT transcription factor
b. AP-1 transcription factor
c. NF-kB transcription factor
d. MAPK kinase module
e. The 401 Highway pathway
a. NFAT transcription factor
b. AP-1 transcription factor
c. NF-kB transcription factor
d. MAPK kinase module
e. The 401 Highway pathway
a. NFAT transcription factor
17
New cards
The immune system exists to protect your body from threats such as bacteria and viruses that can infect. However, in Chapter 1, as part of the overview of the immune system, we learned that the immune system could fail or “go wrong”. Name two ways the immune system might
fail or be dangerous to you and briefly explain their consequences to your health. Indicate if this is due to over or under activity of the immune system. EXCEPTION: Don’t talk about transplants and cancer here. /4
fail or be dangerous to you and briefly explain their consequences to your health. Indicate if this is due to over or under activity of the immune system. EXCEPTION: Don’t talk about transplants and cancer here. /4
Autoimmunity: this is a condition where the immune system turns on self-tissues and self-antigens causing tissue damage.
OR Allergies and asthma; this is an example of immune over-activity caused by hypersensitity of the immune function to a trigger like an allergen. Accept: this causes respiratory problems and/or can
cause uncontrolled immune reaction.
Or Dysbiosis, results from an imbalance in how the body handles microbiota causing more inflammation then there should exist – affects various organs like the intestinal tract, and can lead to diabetes, neurological conditions, heart problems, weight gain.
OR immunodeficiency caused by loss-of-function mutations in immune-related genes; increases probability to infection/more susceptible to infection.
OR immunodeficiency due to acquired/environmental factors. Example, HIV infection destroys immune function increasing odds for other infections.
OR Allergies and asthma; this is an example of immune over-activity caused by hypersensitity of the immune function to a trigger like an allergen. Accept: this causes respiratory problems and/or can
cause uncontrolled immune reaction.
Or Dysbiosis, results from an imbalance in how the body handles microbiota causing more inflammation then there should exist – affects various organs like the intestinal tract, and can lead to diabetes, neurological conditions, heart problems, weight gain.
OR immunodeficiency caused by loss-of-function mutations in immune-related genes; increases probability to infection/more susceptible to infection.
OR immunodeficiency due to acquired/environmental factors. Example, HIV infection destroys immune function increasing odds for other infections.
18
New cards
Are hematopoietic stem cells totipotent? Explain – HINT: Don’t forget to explain what totipotent is in your answer
No. /1
Totipotent means that stem cell can differentiate into any and all cell types. /1
However, HSCs can only differentiate into blood cell types. They are tissue-specific stem cells.
NOTE: Okay if they say HSCs are pluripotent as long as they acknowledge HSCs can only become blood cell types. /2
Totipotent means that stem cell can differentiate into any and all cell types. /1
However, HSCs can only differentiate into blood cell types. They are tissue-specific stem cells.
NOTE: Okay if they say HSCs are pluripotent as long as they acknowledge HSCs can only become blood cell types. /2
19
New cards
What does it mean for an HSC to self-renew? Why is this important? What would happen to your blood cell number if HSCs lost this property? /5
When an HSC divides during mitosis, one of the daughter cells does not differentiate into another cell type – instead that daughter cell maintains the HSC state - this is self-renewal. /2
HSC self-renewal ensures that we maintain a pool of HSCs during hematopoiesis by preventing all HSCs from terminally differentiating. /2
If HSCs could not self-renew, we would deplete HSC population and eventually our ability to make blood cells would disappear. /1
HSC self-renewal ensures that we maintain a pool of HSCs during hematopoiesis by preventing all HSCs from terminally differentiating. /2
If HSCs could not self-renew, we would deplete HSC population and eventually our ability to make blood cells would disappear. /1
20
New cards
HSCs differentiate into two major lineages. What are these lineages? HINT: Just the names. /2
Myeloid /1 and Lymphoid /1
21
New cards
Macrophages and neutrophils belong to which lineage in Question 2C? What is a common function of these two cell types? /2
Myeloid lineage. /1
A common function is phagocytosis (okay if they also say chemotaxis, secretion of cytokines, coordinate immune response). /1
A common function is phagocytosis (okay if they also say chemotaxis, secretion of cytokines, coordinate immune response). /1
22
New cards
B cells belong to what lineage in Question 2C? What do B cells do in general? /2
Lymphoid lineage /1
They generate antibodies /1
They generate antibodies /1
23
New cards
A family has four kids that are all immunocompromised and very susceptible to viral, but not bacterial infections. After several studies to try to understand the reason, scientists discovered that the children i) have normal levels of antibodies in their serum, ii) normal B cell count, but iii) reduced T cell count. Moreover, high-resolution MRI shows that their thymus did not develop properly. /5
What is kind of organ is the thymus? Generally, what is the thymus responsible for? HINT: Simple statements is enough here. /3
What is kind of organ is the thymus? Generally, what is the thymus responsible for? HINT: Simple statements is enough here. /3
Primary lymphoid organ /1
Selecting and differentiating CD4+ and CD8+ T lymphocytes (naïve T cells). /2
Selecting and differentiating CD4+ and CD8+ T lymphocytes (naïve T cells). /2
24
New cards
A family has four kids that are all immunocompromised and very susceptible to viral, but not bacterial infections. After several studies to try to understand the reason, scientists discovered that the children i) have normal levels of antibodies in their serum, ii) normal B cell count, but iii) reduced T cell count. Moreover, high-resolution MRI shows that their thymus did not develop properly. /5
Given that the children have normal antibody levels, but reduced T cell count, what do you think is failing at the thymus and how might this explain their susceptibility to viral infections. /2
Given that the children have normal antibody levels, but reduced T cell count, what do you think is failing at the thymus and how might this explain their susceptibility to viral infections. /2
Generation of CD8+ cytotoxic T cells must be defective (It can’t be CD4+ T cells because antibody levels is normal). /1
These cells are important to kill virus-infected host cells, reducing the ability of viruses to replicate and spread. /1
These cells are important to kill virus-infected host cells, reducing the ability of viruses to replicate and spread. /1
25
New cards
Answer each (total /7)
A. Are interferons cytokines? Yes or no. /1
B. What microbes induce interferon expression? HINT: Just the name. /1
C. Give two specific changes to cellular function that interferons elicit to fight these specific microbes? /2
D. What receptor might drive interferon transcription: the Toll-like receptor 3, which binds to dsRNA, or a TCR against a peptide of said microbe expressed on a CD4+ T cell. Explain your reasoning. HINT: including the reason for one and reasoning for why not the other. /3
A. Are interferons cytokines? Yes or no. /1
B. What microbes induce interferon expression? HINT: Just the name. /1
C. Give two specific changes to cellular function that interferons elicit to fight these specific microbes? /2
D. What receptor might drive interferon transcription: the Toll-like receptor 3, which binds to dsRNA, or a TCR against a peptide of said microbe expressed on a CD4+ T cell. Explain your reasoning. HINT: including the reason for one and reasoning for why not the other. /3
A. Yes
B. Viruses
C.TWO (Mark first two): One point each.
Reduce protein synthesis;
Produce ribonucleases,;
Express genes that fight viral replication;
Reduce host cell replication;
Drive adaptive immunity.
Overall, fight viruses.
D.TLRs are PRRs that bind specific types of MAMPs and can differentiate between microbe classes. TLR3 is a PRR that binds to dsRNA, which is often found on viruses. Thus, TLR3 is likely responsible for inducing interferons. /2
TCR on CD4+ cannot tell if peptide is viral or not. /1
B. Viruses
C.TWO (Mark first two): One point each.
Reduce protein synthesis;
Produce ribonucleases,;
Express genes that fight viral replication;
Reduce host cell replication;
Drive adaptive immunity.
Overall, fight viruses.
D.TLRs are PRRs that bind specific types of MAMPs and can differentiate between microbe classes. TLR3 is a PRR that binds to dsRNA, which is often found on viruses. Thus, TLR3 is likely responsible for inducing interferons. /2
TCR on CD4+ cannot tell if peptide is viral or not. /1
26
New cards
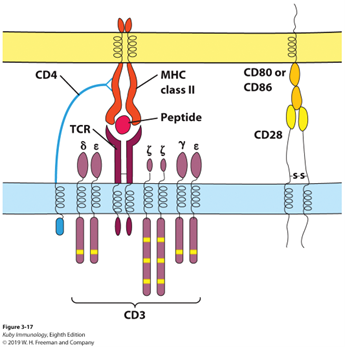
Using the diagram below, explain the main biochemical and/or cellular function of each component shown. In your answer, indicate which cell type is expressing that component. Do not bother describing structure. Focus on function. /10
In T cells:
TCR – t cell receptor. Undergoes genetic recombination to form unique TCRs that recognize specific antigenic peptides presented on MHC. /2
CD3 co-receptor – made of several subunits, containing the ITAM motif. Once TCR-binds to antigens, ITAMs are phosphorylated to activate signalling /2
CD4: increases specificity and avidity for MHC-II::peptide complexes over MHC-I. /2
CD28: co-receptor that helps secure T cells to antigen presenting cells expressing CD80/86 /1
On APCs:
MHC-II complex is responsible for holding antigenic peptide and presenting to the T cell
Peptide: antigenic peptide derived from a microbe. /2
CD80/86 expressed co-receptors in APCs. Only expressed in activated APCs, helping to reduce autoimmunity because this is not expressed by APCs displaying self-peptides /1
TCR – t cell receptor. Undergoes genetic recombination to form unique TCRs that recognize specific antigenic peptides presented on MHC. /2
CD3 co-receptor – made of several subunits, containing the ITAM motif. Once TCR-binds to antigens, ITAMs are phosphorylated to activate signalling /2
CD4: increases specificity and avidity for MHC-II::peptide complexes over MHC-I. /2
CD28: co-receptor that helps secure T cells to antigen presenting cells expressing CD80/86 /1
On APCs:
MHC-II complex is responsible for holding antigenic peptide and presenting to the T cell
Peptide: antigenic peptide derived from a microbe. /2
CD80/86 expressed co-receptors in APCs. Only expressed in activated APCs, helping to reduce autoimmunity because this is not expressed by APCs displaying self-peptides /1
27
New cards
In relation to innate immune defense, answer the following: /9
A. Explain how lung mucus and cilia are part of the innate immune system. /4
B. Lysozyme is an antimicrobial protein. What does it do and name one tissue/fluid where lysozyme is expressed in? /3
C. LL-37 is an antimicrobial peptide. How do they kill bacteria? /2
A. Explain how lung mucus and cilia are part of the innate immune system. /4
B. Lysozyme is an antimicrobial protein. What does it do and name one tissue/fluid where lysozyme is expressed in? /3
C. LL-37 is an antimicrobial peptide. How do they kill bacteria? /2
A. Mucus coats the epithelial layer of respiratory track. It is sticky and traps microbes. /2
Cilia on the lung epithelia beat to move mucus and microbes to help clear lungs. /2
B. Enzyme that cleaves glycosidic bonds in bacterial cell wall /2. Tears/saliva /1
C. Bind to membranes and form pores, causing permeability and damage. /2
Cilia on the lung epithelia beat to move mucus and microbes to help clear lungs. /2
B. Enzyme that cleaves glycosidic bonds in bacterial cell wall /2. Tears/saliva /1
C. Bind to membranes and form pores, causing permeability and damage. /2