hypersensitivity and anaphylaxis
1/26
Earn XP
Description and Tags
block 2 week 2 ctb
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
27 Terms
hypersensitivity
one of 3 ways in which immune responses can be harmful to the body overall
includes:
allergy: relatively localised, mild-moderate reactions
anaphylaxis: systemic, life-threatening reactions
epidemiology/risk factors
7% of children in UK develop allergies during childhood
many do not persist into adulthood
common food allergies:
milk
eggs
bananas
nuts
sesame seeds
fish
shellfish
possible reasons
improved hygiene and less parasitic infections
vit D deficiency
dietary changes (later introduction of food items)
hypersensitivity
inappropriate and excessive immunological reaction to an external antigen due to dysfunctional control of the immune system
allergy = local reaction (mucous membranes, skin, lungs)
anaphylaxis = systemic reaction (shock and death)
allergen = antigen that induces hypersensitivity reaction
autoimmunity
inappropriate immune response to self‑antigens (autoantigens).
most relevant cells in hypersensitivity
mast cells
eosinophils
basophils
innate and adaptive immunity diagram
hypersensitivity involves both innate and adaptive immune responses
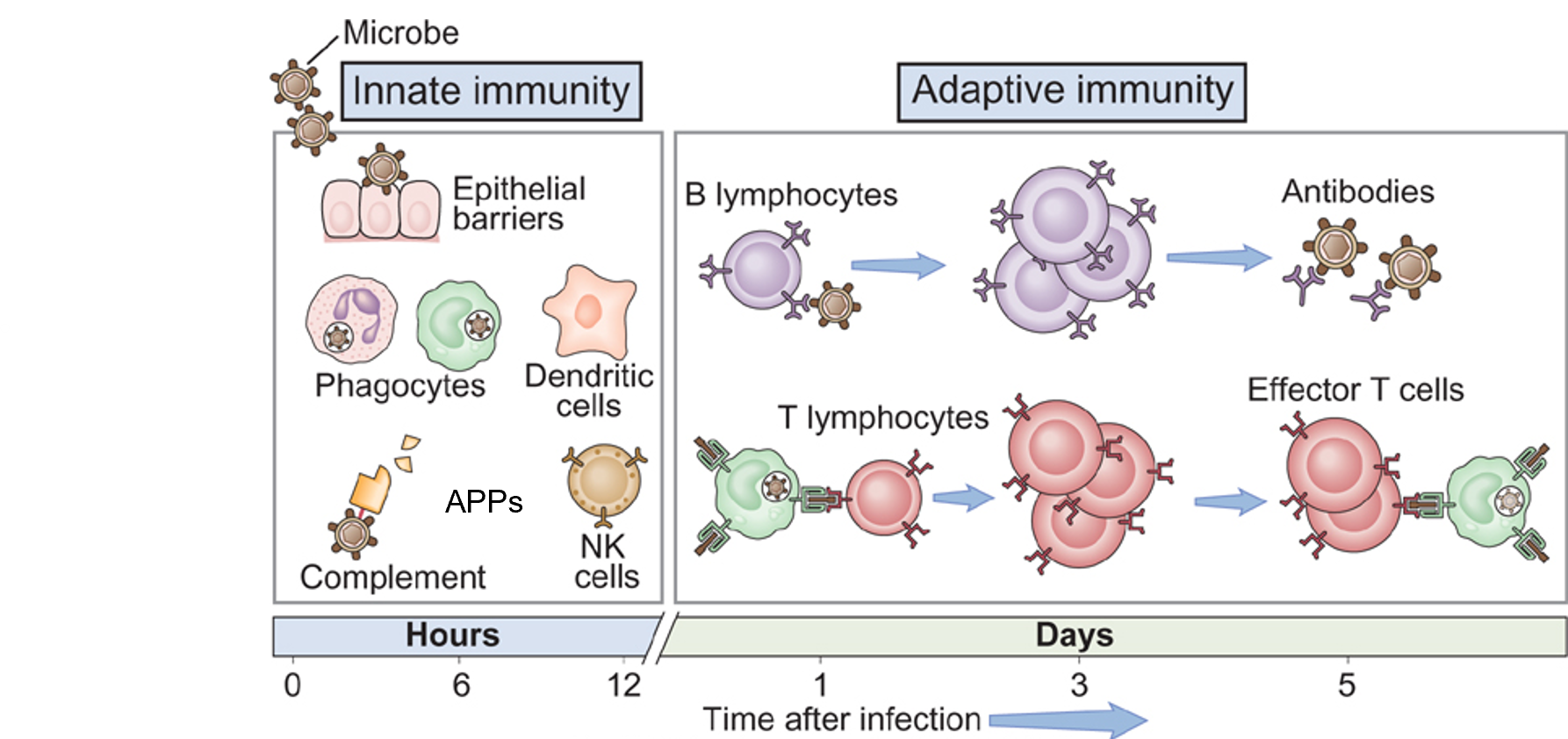
innate immune system
Rapid, non‑specific, no memory.
Cellular and humoral components.
adaptive immune responses
Slower onset, highly specific.
Generates immunological memory.
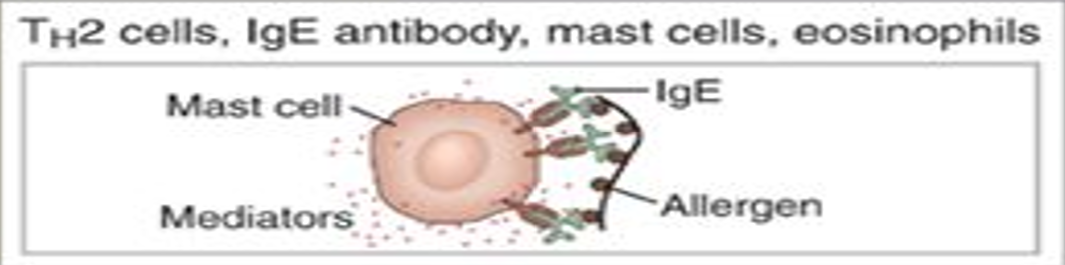
type I hypersensitivity: immediate/IgE mediated
mediators:
IgE
mast cells
basophils
eosinophils
examples:
allergies
anaphylaxis
asthma
atopy
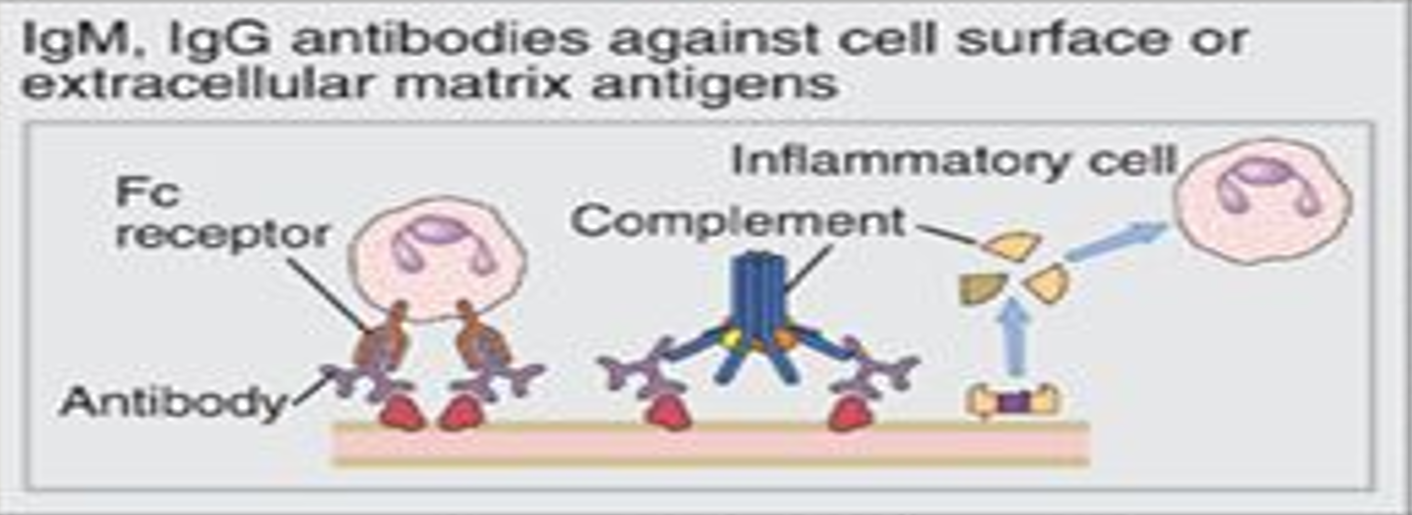
type II hypersensitivity: AB-dependent
mediators:
IgM
IgG
examples:
autoimmune haemolytic anaemia
Goodpasture’s Syndrome
myasthenia gravis
Graves
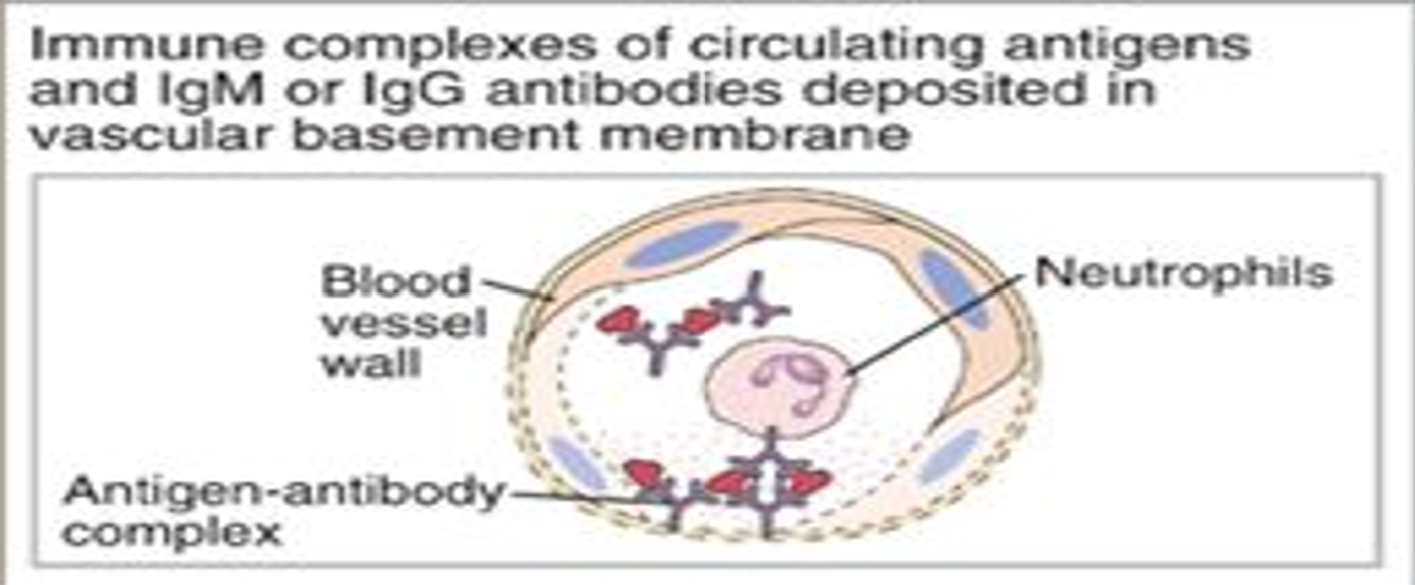
type III hypersensitivity: immune complex mediated
mediators:
immune complex
examples:
serum sickness
extrinsic allergic alveolitis (EAA)
rheumatoid arthritis
systemic lupus erythematosus
type IV hypersensitivity: delayed/cell-mediated
mediators:
T lymphocytes
macrophages
examples:
allergic contact dermatitis
chronic transplant rejection
multiple sclerosis
tuberculin skin test
type I hypersensitivity
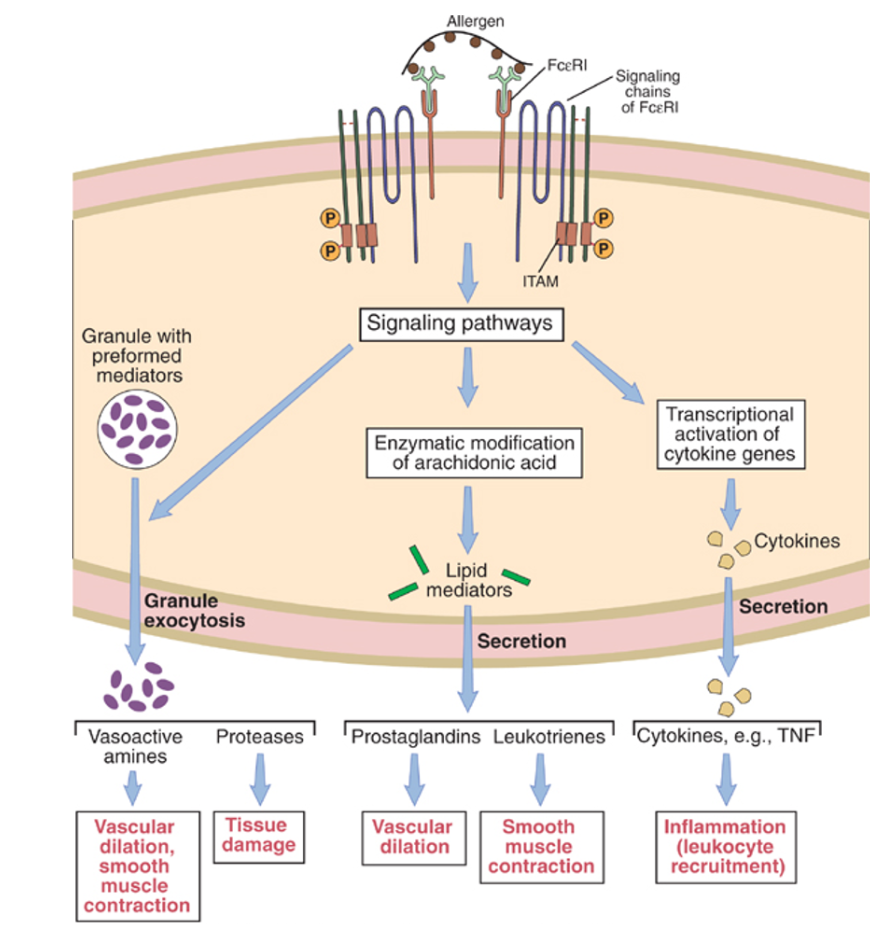
mast derived mediators (vasoactive amines, lipid mediators, cytokines)
cytokine mediated inflammation (eosinophils, neutrophils)
type II hypersensitivity
complement and Fc receptor mediated recruitment and activation of leukocytes (neutrophils and macrophages)
opsonisation and phagocytosis of cells
abnormalities in cellular function (eg hormone receptor signalling)
type III hypersensitivity
complement and Fc receptor mediated recruitment and activation of leukocytes
type IV hypersensitivity
macrophage activation, cytokine-mediated inflammation
direct target cell lysis, cytokine mediated inflammation

epidemiology of type I hypersensitivity
~20% of people in developed countries experience allergy at some point.
Atopy:
Genetic/familial predisposition to allergy (e.g. eczema, asthma).
Environmental factors also important.
common allergens/presentations of type I hyoersensitivity
Environmental:
Pollens → hay fever
House dust mites
Animal dander
Insect venoms:
Bee stings, wasps (risk of anaphylaxis)
Food and drugs:
Higher risk of systemic exposure and anaphylaxis.
pathology of type I hypersensitivity
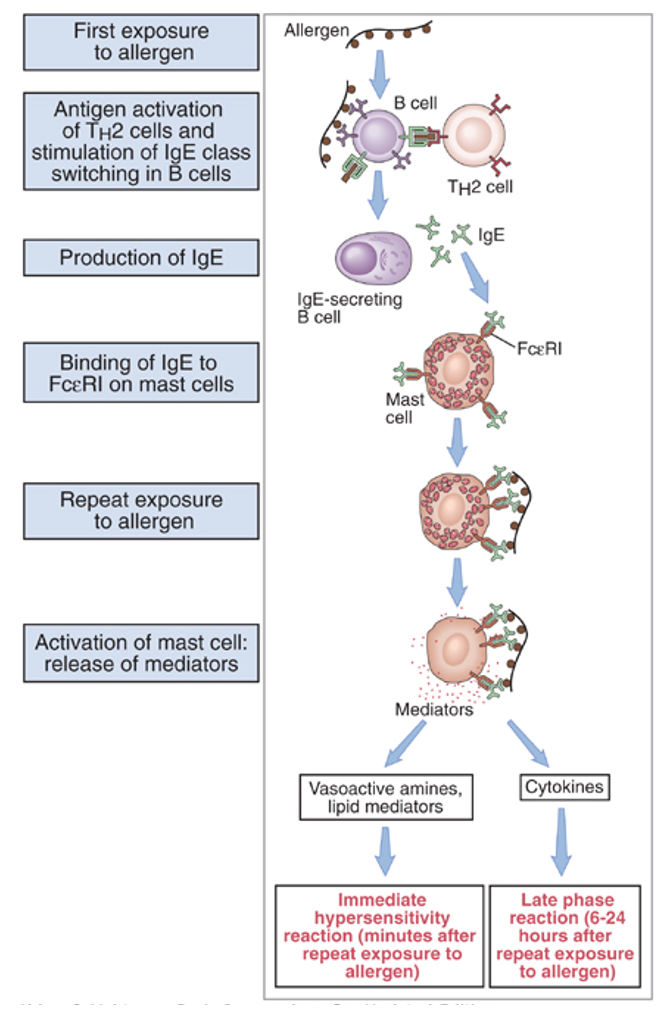
mast cell degranulation of hype I hypersensitivity
clinical features of type I hypersensitivity
Sensitisation occurs first (IgE production & binding to mast cells)
Thereafter exposure generates immediate response (degranulation)
Airway & eye mucous membranes → pruritus & sneezing
rhinorrhoea & lacrimation
Skin → pruritus & urticaria (also seen in Type IV reactions)
Oral & intestinal mucous membranes → pruritus & angioedema
Systemic exposure → anaphylaxis = local swelling, flushed, faint, dyspnoea, peri-oral paraesthesia, throat/chest tightness, wheeze, pale, sweaty, hypotensive
pathophysiology of type I hypersensitivity in depth
Sensitisation Phase (First Exposure)
Allergen recognised by:
B cells
T helper 2 (Th2) cells
B cells differentiate into plasma cells producing IgE.
IgE binds via Fc region to receptors on:
Mast cells
Eosinophils
Basophils
No clinical symptoms at this stage.
Activation Phase (Second Exposure)
Allergen binds to IgE on mast cell surface.
Triggers mast cell activation and degranulation.
Mast Cell Degranulation
Release of:
Preformed granules:
Vasoactive amines (e.g. histamine)
Proteases
Lipid mediators:
Prostaglandins
Leukotrienes
Cytokines:
Recruit additional immune and inflammatory cells
type IV hypersensitivity
Pathology = usual T cytotoxic cell response (slow & specific), but still inappropriate & excessive (as per definition)
So unlike Type 1 (immediate/IgE-mediated) hypersensitivity,
Type IV (delayed/cell-mediated) = slower & more specific/localised
Various allergens causing few diseases :
eg. nickel, other metals, latex
→ allergic contact dermatitis (slowly developing, pruritic, localised)
Other examples not truly “inappropriate & excessive” (eg. chronic organ rejection) or else autoimmune (eg. MS) or diagnostic (eg. TST)
Clinical features = slowly developing, localised immune reactions
investigations for hypersensitivity
Laboratory Markers
Tryptase:
Released from mast cells
Elevated in Type I reactions
IgE: often raised
Eosinophil count: may be raised
Skin Testing
Skin Prick Testing
Small drops of allergens applied to skin.
Skin pricked with stylet.
Read at ~15 minutes.
Positive if lesion is ≥3 mm larger than negative control.
Controls:
Negative: saline
Positive: histamine
Patch Testing
Used for multiple allergens.
No skin pricking.
Patches left in place for 2–3 days.
Useful for Type IV reactions.
hypersensitivity treatments
Avoidance
Avoid known allergens where possible.
Pharmacological Treatment
Mast cell stabilisers:
Prevent degranulation
Often t
opical (eye drops, nasal sprays)
Antihistamines:
Block histamine receptors
Topical or systemic
Steroids:
Reduce inflammation and immune response
Topical or systemic
Leukotriene receptor antagonists:
Block inflammatory mediators
Systemic tablets
De-sensitisation : also called “allergen immunotherapy”
relies on creating tolerance to allergens
by exposure to gradually increasing doses
delivered sublingually or subcutaneously
small risk of anaphylaxis during therapy
requires weekly/monthly treatment for ~3 years
ABC treatment of hypersensitivity
Airway – Breathing – Circulation
Lie patient down
High-flow oxygen
IV fluids
Adrenaline (epinephrine) 500 mcg IM (0.5 ml of 1mg/ml)
IV chlorphenamine (anti-histamine)
IV hydrocortisone (steroid)
Nebulised salbutamol (bronchodilator)
Repeat adrenaline IM if no improvement after 5 minutes