Week 2: UE peripheral nerves
1/33
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
34 Terms
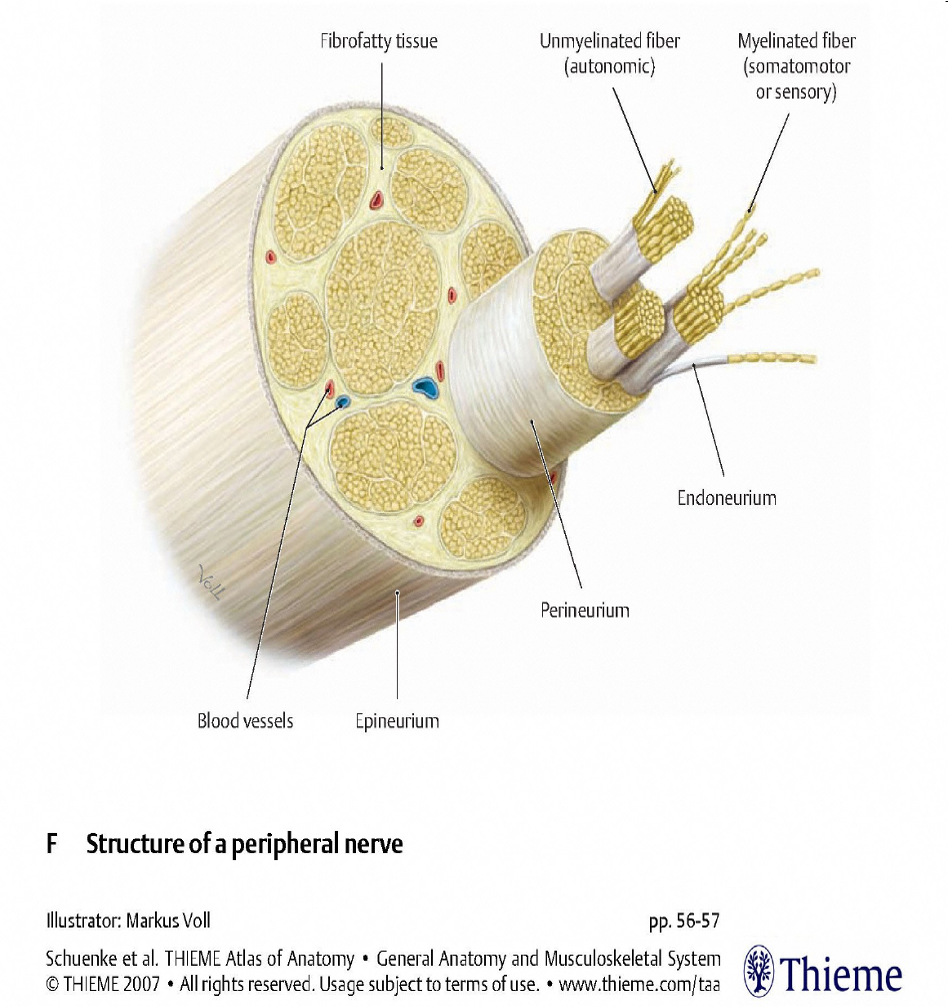
epineurium
outermost protective layer
perineurium
surrounds each fascicle
endoneurium
wraps each axon (nerve fiber)
Neuropraxia
sunderland type: 1 | Axon is intact, expect complete recovery in 4-12 wks |
when ur foot is asleep and ur scared ur gonna fall over when you stand up
Axonotmesis
sunderland type 2 | Axon is damaged, endonuerial tubes are intact Typically complete recovery but time depends on distance from injury to the innervated end organ Prognosis is fair. |
takes a few months for the axon to grow back to original spot
the more proximal the injury, the longer it will take longer to grow back
Neurotmesis
sunderland types 3, 4, 5 | Axon, myelin and connective tissue are damaged. Requires surgery. Prognosis is poor. |
Nerve Injuries
•Compression
•Clean cut
•Crush, stretch – damage over a greater area
•(Root) avulsion – most damaging
•Axonal regeneration occurs at approx 1mm/day
•After initial latent period of 3-4 weeks
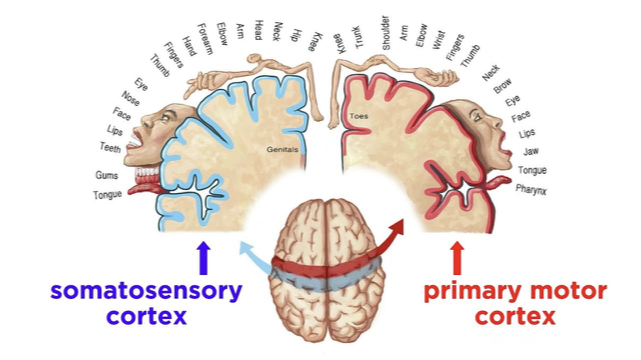
Changes occur in the central nervous system (CNS) with peripheral nerve injuries
•Movement and sensibility go together
•Neural reorganization occurs when there is diminished input to the sensory cortex and integration with the motor cortex
when one area is not getting messages, the surrounding areas creep in and eventually take over. the non-receiving area stops working
Hand therapy assessment of nerve function
•History and occupational profile
•ADL’s and IADL’s
•Observation: Resting posture, Sudomotor, pilomotor
•Tests of sensibility: Semmes-Weinstein, static and moving 2-point discrimination, Ten-test, Moberg, neural tension
•Muscle testing
•Range of motion
•Edema, wounds, scars
Upper Quarter Proximal Screening
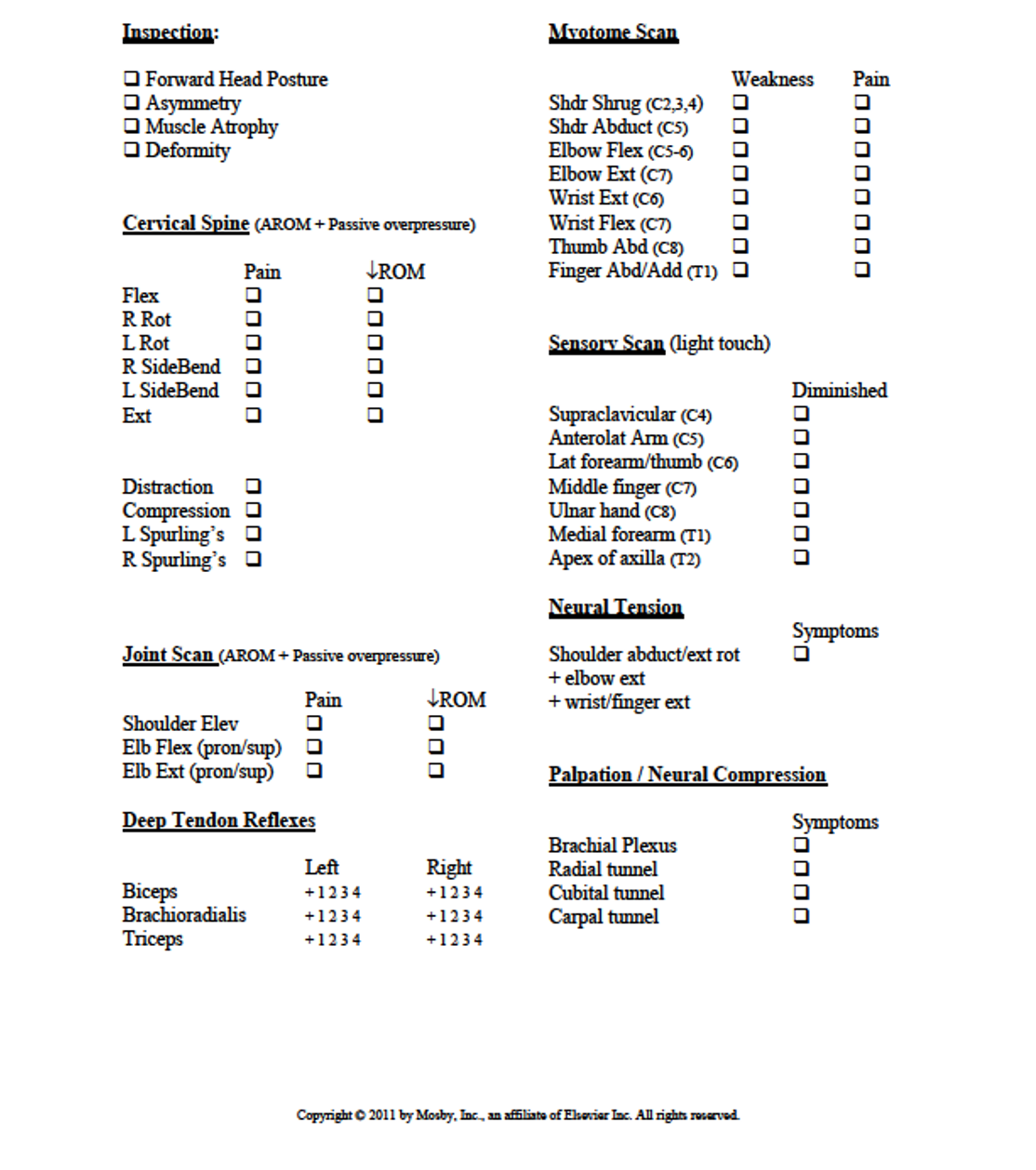
ask how they are feeling in the shoulder or neck. do they have a history of pain or tightness?
does it feel more painful or tight in certain movements? (ex: raising ur hand above to reach for something)
Multiple & Double Crush Syndromes
“_ may cumulatively cause alteration in the neural transmission & produce patient symptoms, although each site in isolation may not be sufficient to cause patient symptoms”. (Novak & Mackinnon, 2003)
basically having compression in two spots of an upper extremity
For example: a proximal nerve compression can cause a distal entrapment site to be more vulnerable to compression or vice versa.
Upper Limb Neural Tension Testing (ULNTT) definition and reasoning
•Nervous system is a continuum
•A healthy system has the ability to elongate, glide & attenuate a limited amount of tension (putting on a sleeve of a shirt, u want ur whole arm/nerve to slide and glide)
•When adverse neural tension is present there can be a reduction in intra & extraneural mobility, impaired intraneural blood & fluid flow
•Remote movement can affect nerve gliding & circulation at another site. (Walsh, 2005)
depression of shoulder
one of the first causes of pressure on nerves causing pain
Upper Limb Neural Tension Testing
•Elongating or stretching nerves (strain) is replaced with mobilization, sliding, gliding or flossing.
•We add tension to the length of the nerve at one joint while shortening it (removing tension) at another joint.
•Goal is to maximize excursion of nerve while minimizing strain.

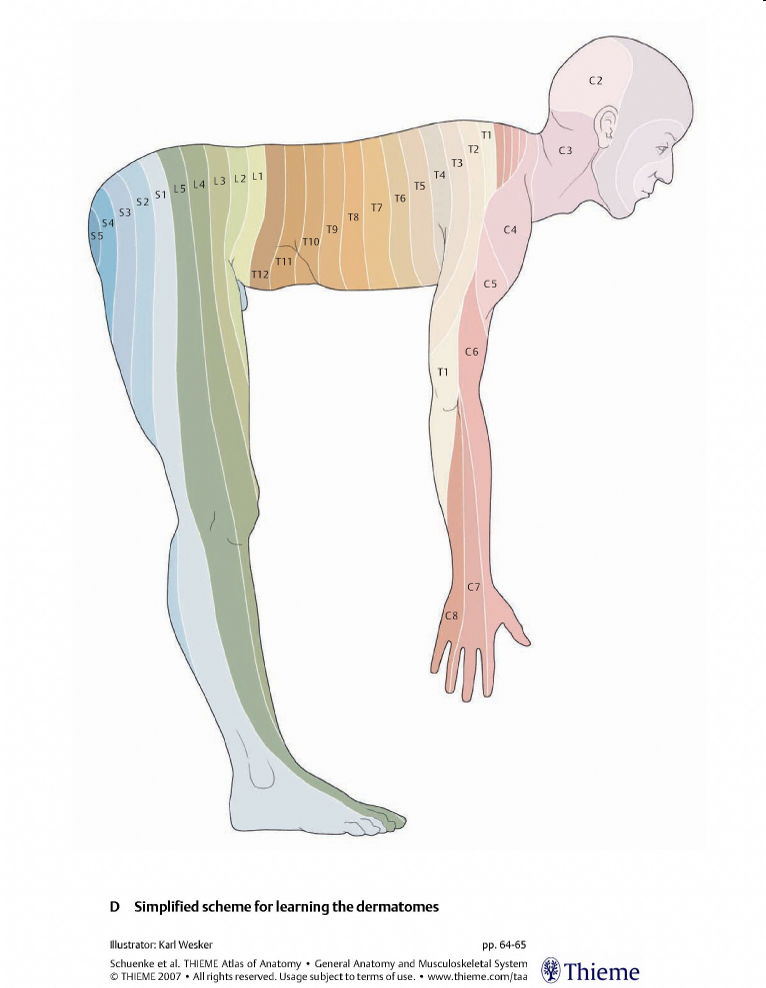
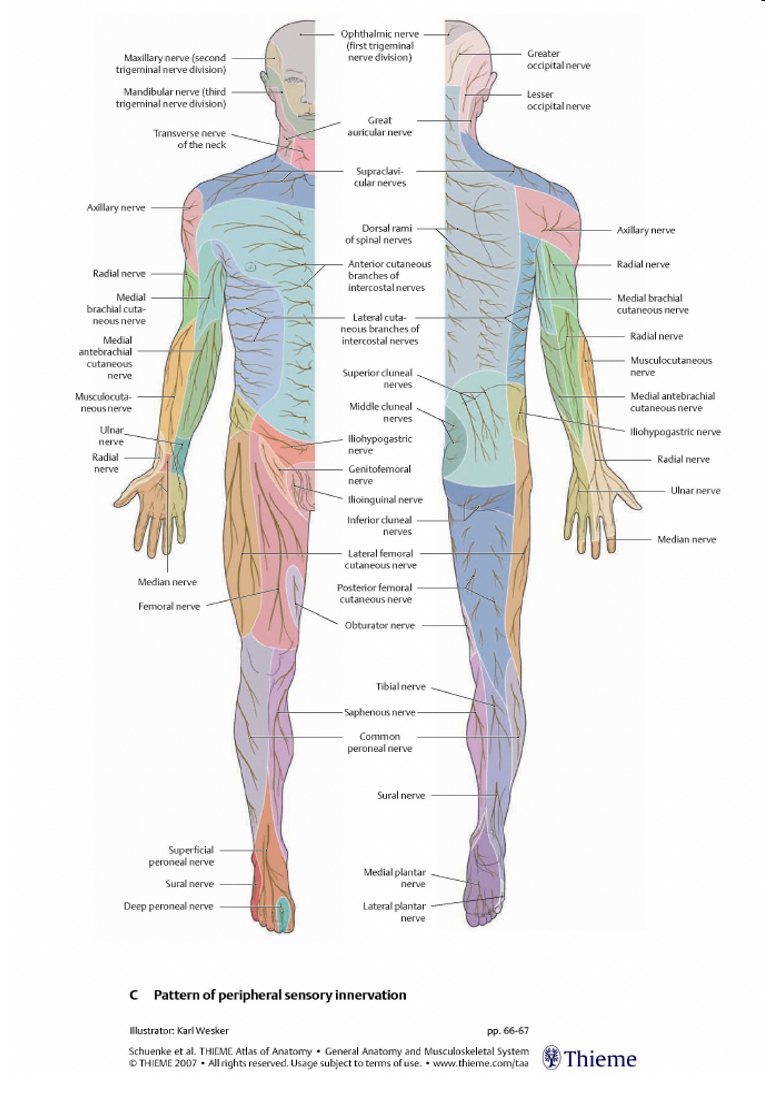
Dermatomes vs. Peripheral nerves
Surgical repair
•Decompression
•Direct repair
•Nerve graft
•Graft comes from self, cadaveric tissue
•Bioartificial conduit
•Nerve Transfer
•
•Tendon transfers when nerve is not successfully repaired.
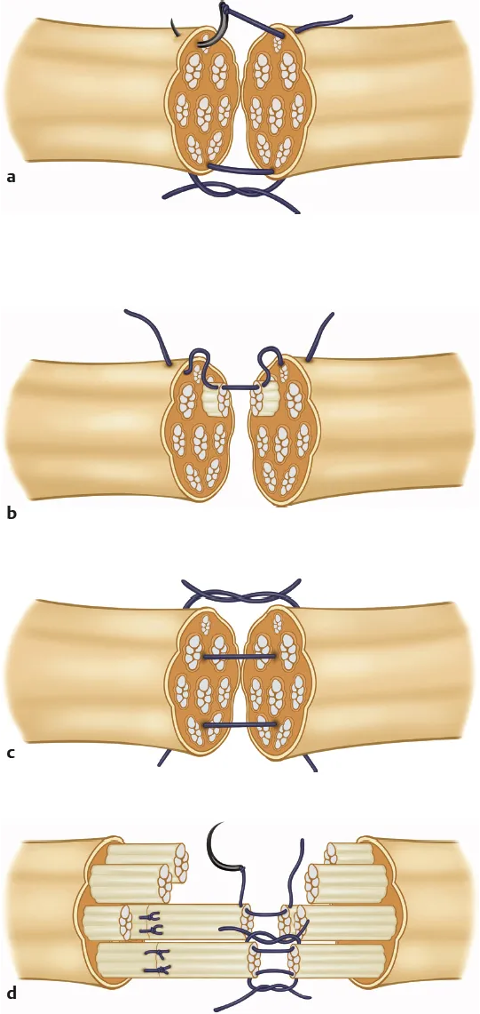
Post-op care of nerve injuries
•Initial immobilization in a range that protects the repair
Avoid tension on repair
•Mobilization to promote excursion of nerve
•Motor and sensory re-education
the more proximal the injury the more harder the healing process
be careful about infections
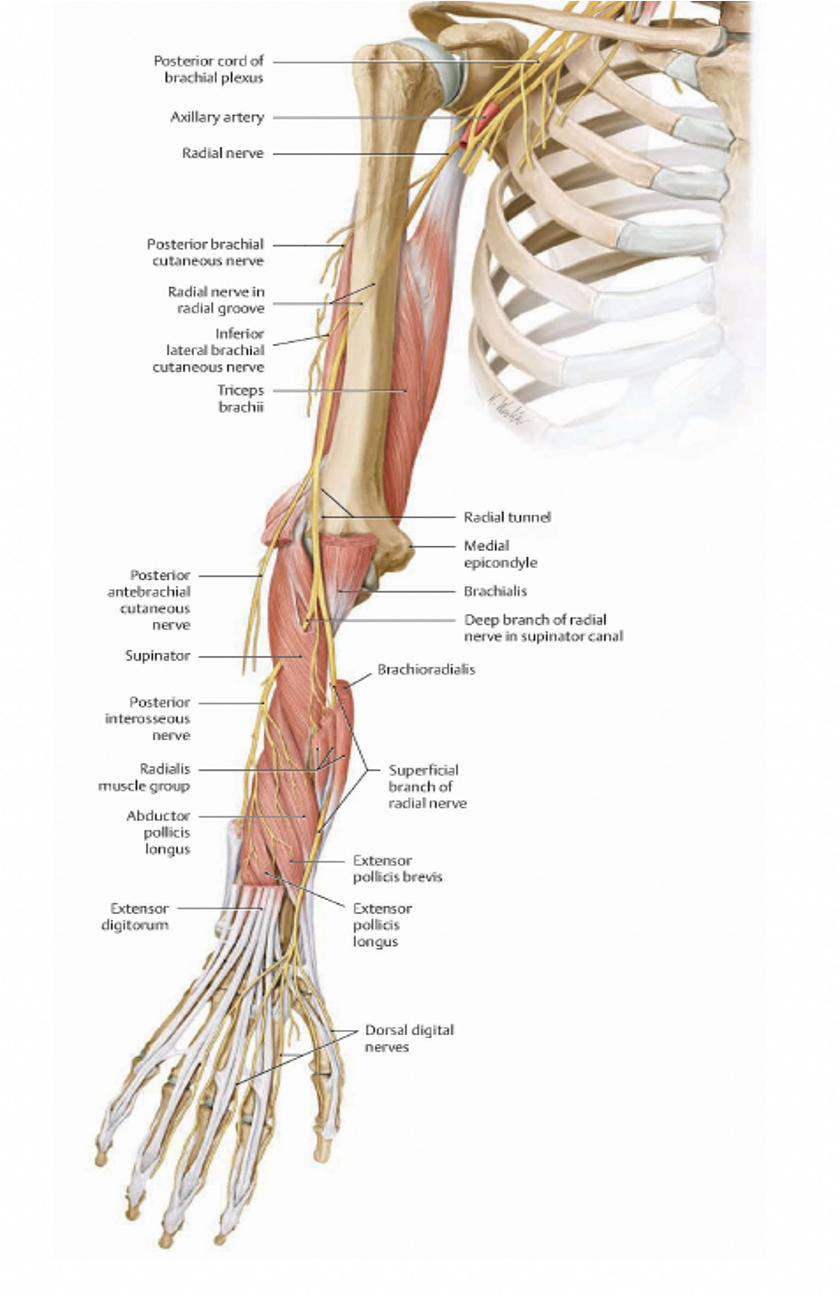
Radial Nerve
Triceps,
Anconeus,
Brachioradialis
ECRL, ECRB
Supinator
Extensor Digitorum
Extensor Digiti Minimi
Extensor Carpi Ulnaris
EPL, EPB
Extensor Indicis
Abductor Pollicis longus
what happens when a nerve is taken from a spot to do a nerve graft
it becomes numb
usually the sural nerve in leg bc its ok if its a little numb
what usually helps depression on nerves
allowing more space for the nerves
ex: carpal tunnel surgery, they cut up the ligament and offer more space for the nerves
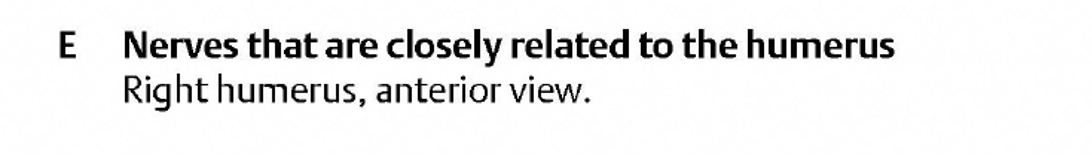
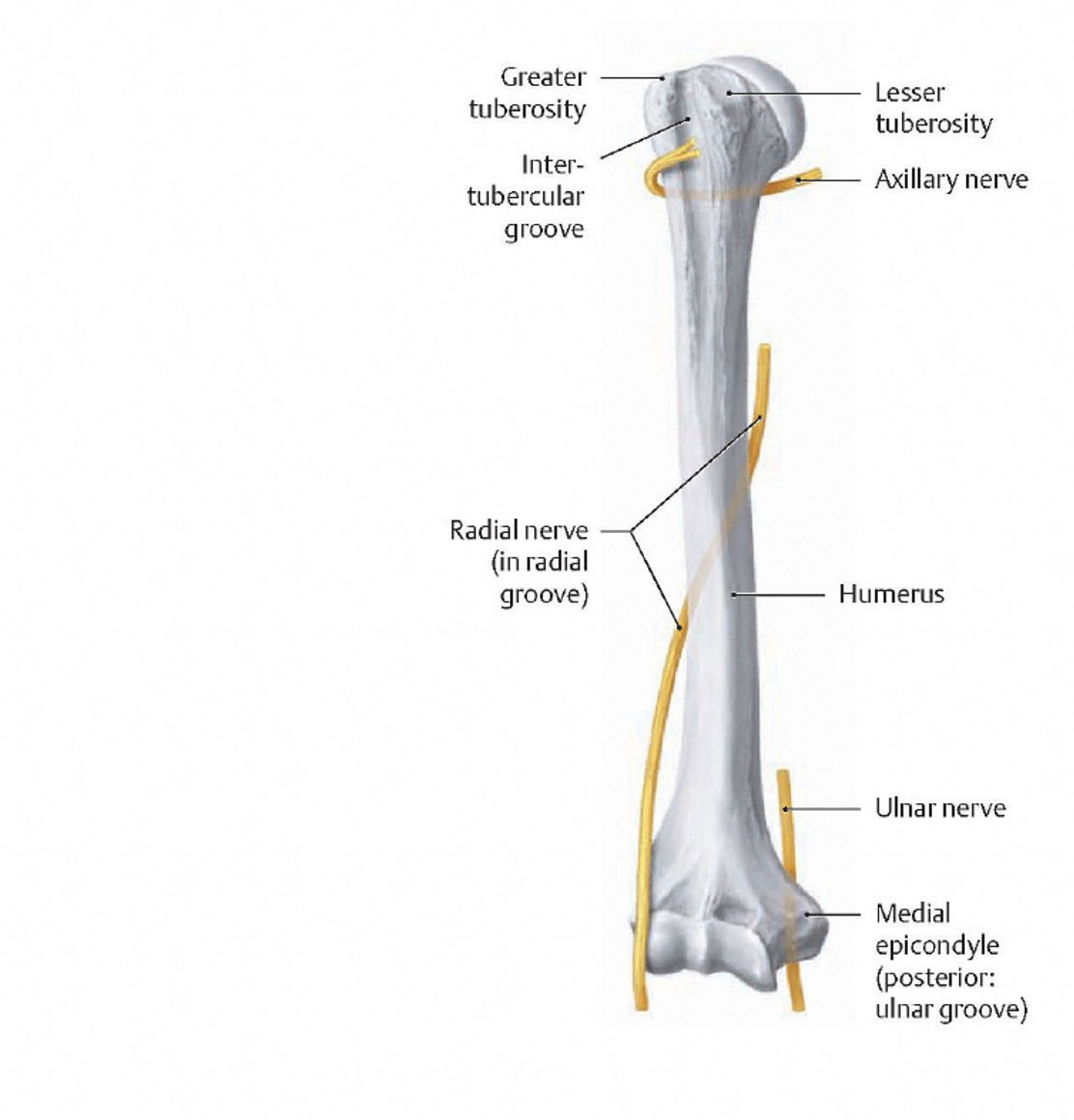
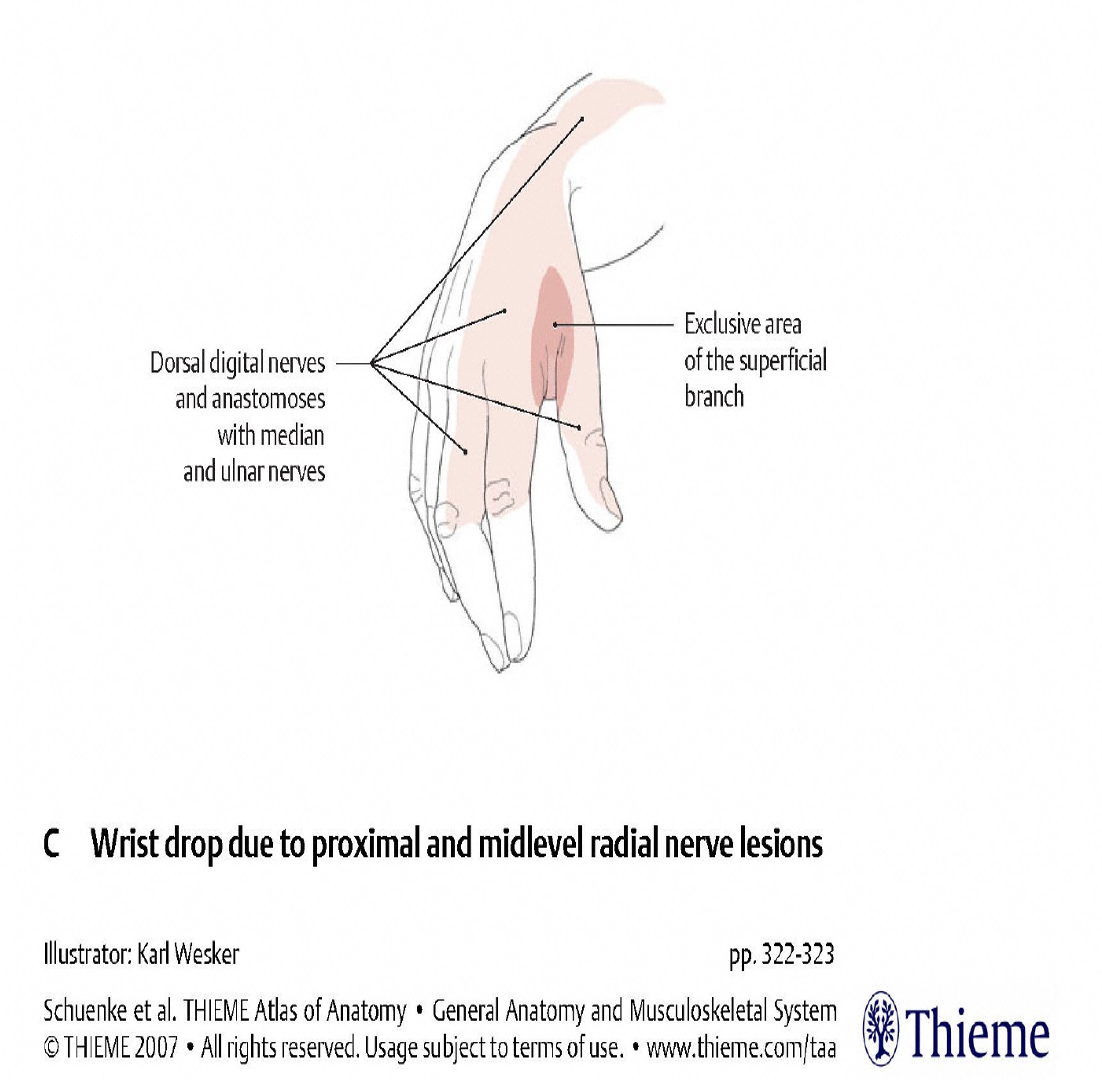
Sensory distribution of the radial nerve and radial nerve palsy
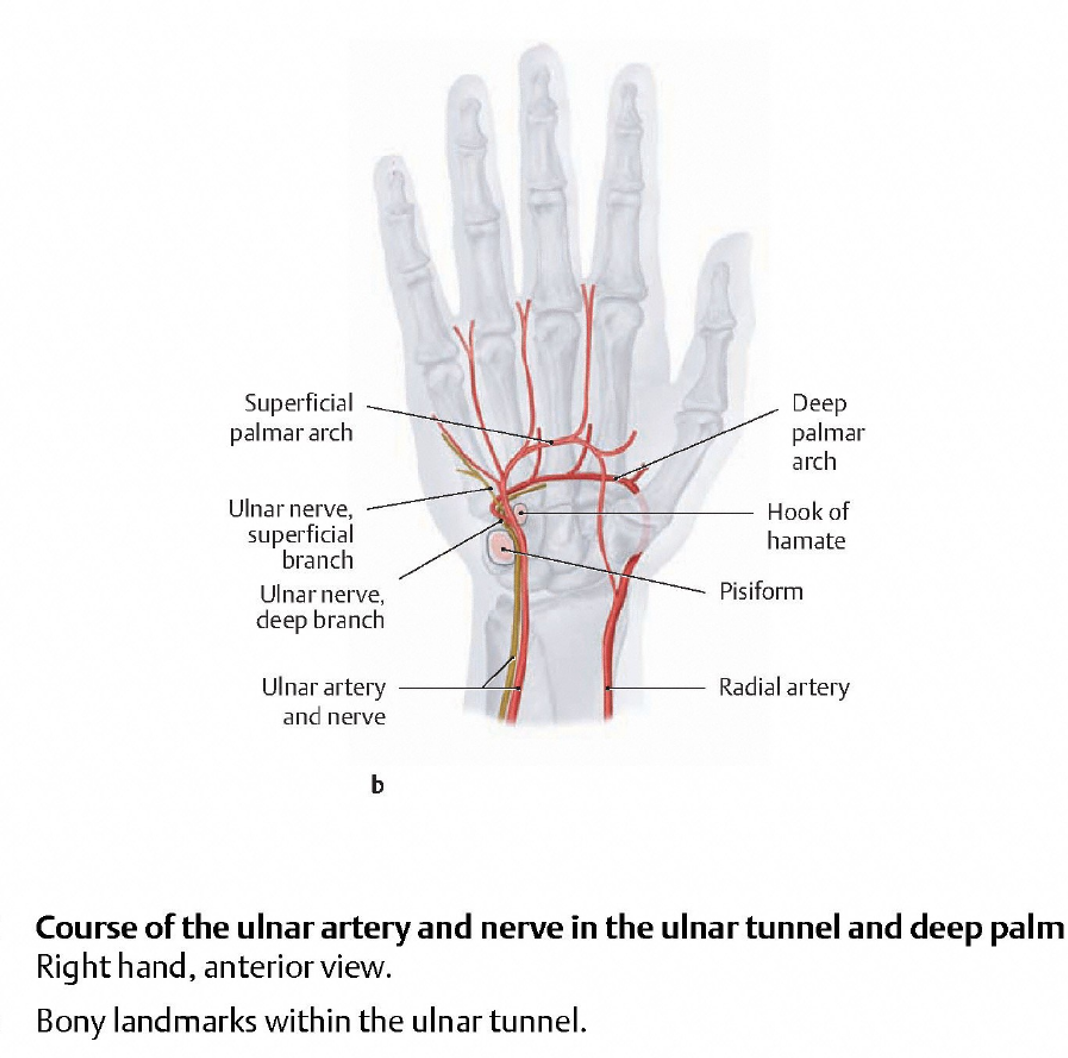
Ulnar Nerve
Innervates
Flexor Carpi ulnaris
Flexor Digitorum profundus (ring & small)
FDM, ADM, ODM
Palmaris brevis
Palmar & dorsal interossei
Adductor pollicis
Flexor pollicis brevis (deep head),
Lumbricals to ring & small fingers
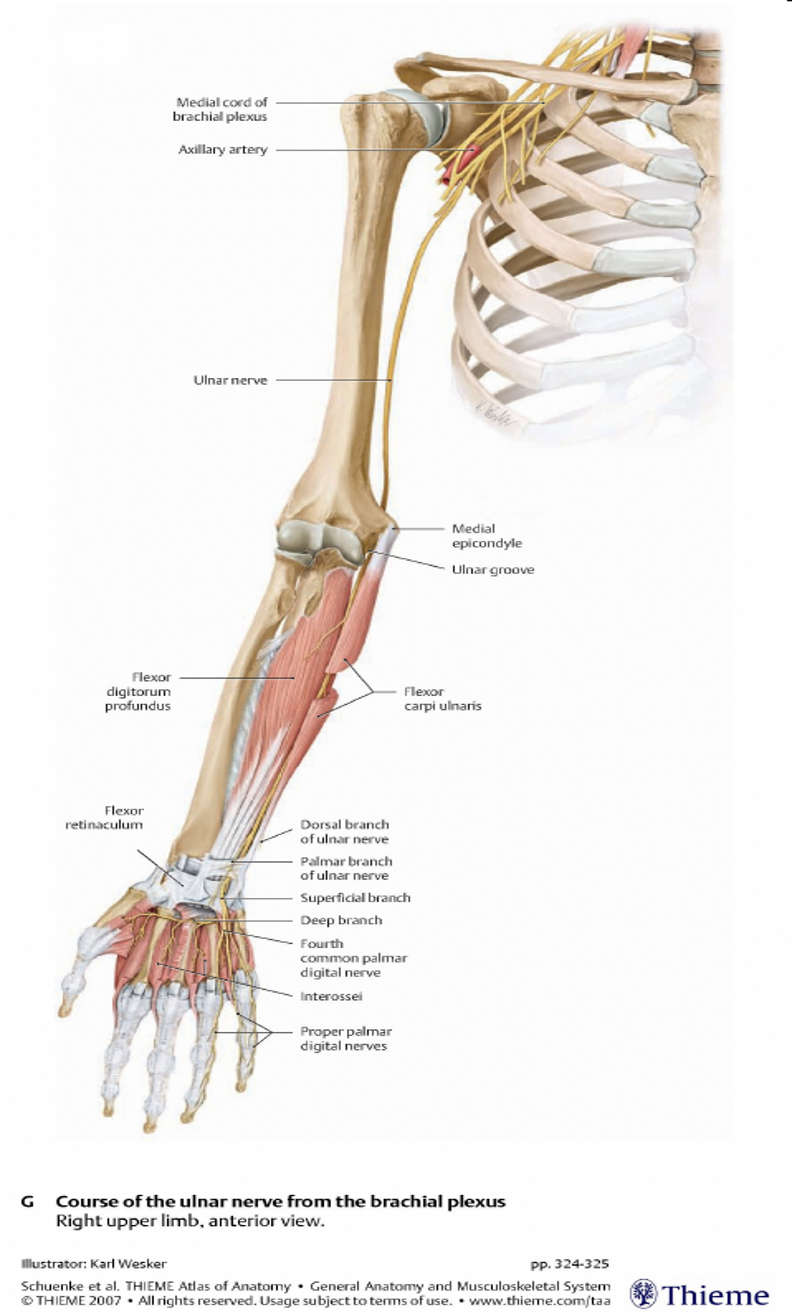
Ulnar Nerve compression:
Guyon’s Canal
•Pain in ulnar hand
•Weak hypothenar muscles
•Sensory loss at small and ½ ring finger
Ulnar nerve palsy
•Claw hand posture
•Froment’s sign
•Wartenberg’s sign
•Atrophy intrinsics and hypothenar
•Loss of power grip and key pinch

Median Nerve
Innervates:
Pronator teres,
FCR, PL
FDS
FDP (1 & 2)
FPL
Pronator quadratus
Thenars: APB, FPB, OP
Lumbricals 1 & 2
Median Nerve (proximal to wrist)
palmar cutaneous branch (sensory to mid palm)
Passes through the carpal tunnel & sends off:
Recurrent branch
(motor to 3 thenar muscles)
Digital nerves
(Sensory to radial 3 ½ digits)
Motor branch to Lumbricals
(of the index & middle fingers)
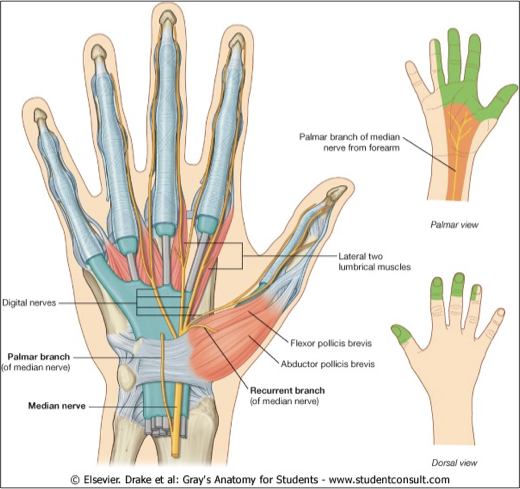
Median nerve palsy
•Loss of median intrinsics (lumbricals 1 & 2)
•Loss of thumb palmar abduction (APB, FPB, OP)
•Sensory loss to tip of thumb, index finger and middle finger
•Fine motor skills, precision pinch, manipulation of objects and writing
Intervention following nerve injury
Patient education
Protecting muscles and tendons from shortening or lengthening while the nerve heals (prevent imbalances)
•Orthoses (splints)
•Passive Range of Motion (PROM)
•Active assist exercises
Increasing patient’s ability to perform functional tasks/occupations
•Splinting
•Modified methods
•Adaptive equipment
Teach safety awareness especially with sensory deficits
Neural mobilization
•Goal; promote sliding of nerves or tissue surrounding nerves,
•Can be used for conservative management or post-op
•Neural tension testing uses same positions as exercises
•Perform maneuvers slowly. 5-10 reps several times per day. It is best to under-do vs. overdo
•Approach a position of slight tension then back off and “floss” or oscillate
•Avoid strain (elongation or tension) on nerve.
Neural glides for CTS (post-op)
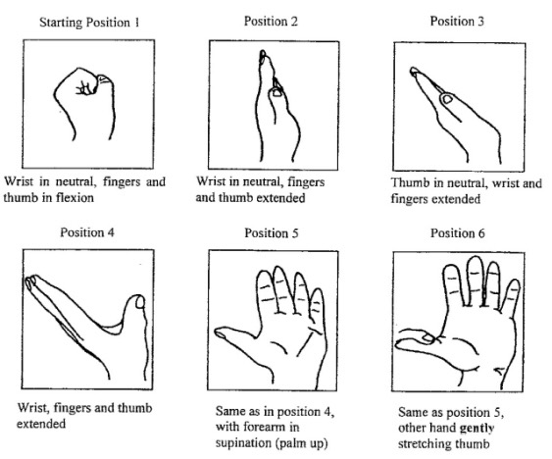
add finger abduction to last pose
Sensory Reeducation phase 1
•Begin “immediately after nerve repair to maintain cortical representation” (Rosen, 2020)
•Mental images of sensory qualities or motor actions
•Mirror visual feedback
•Auditory input
•Education to protect and compensate for insensate areas (Moscony, 2020)
Sensory Reeducation phase 2
•Begin when there is some measurable touch sensation in the palm
•Discriminate and localize shapes, textures and objects
•Use hand for functional & familiar tasks to facilitate occupational participation & decrease learned nonuse (Priya, 2012)
Desensitization
•Used for allodynia (something that is painful that normally isnt like air, sleeves, etc.) and hyperalgesia (hypersensitivity)
allodynia might lead to complex regional pain syndrome
•Gradually introduce graded non-noxious tactile stimuli to retrain the nervous system
•Patient applies stimulus to themselves frequently and looks, thinks about it, and mentally describes the sensation.
