45) reabsoprtion and secretion
1/23
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
24 Terms
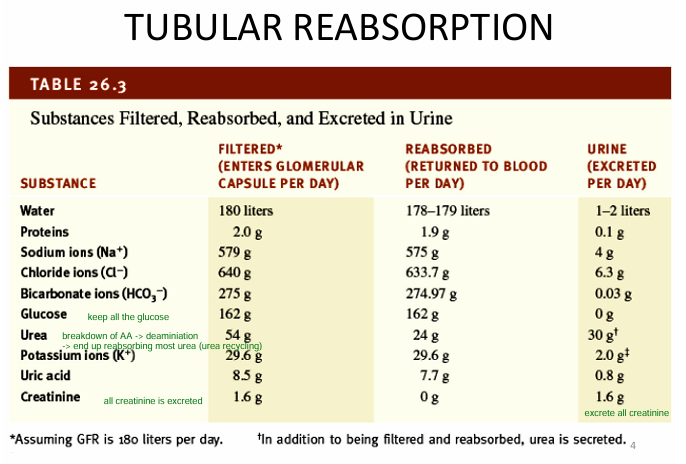
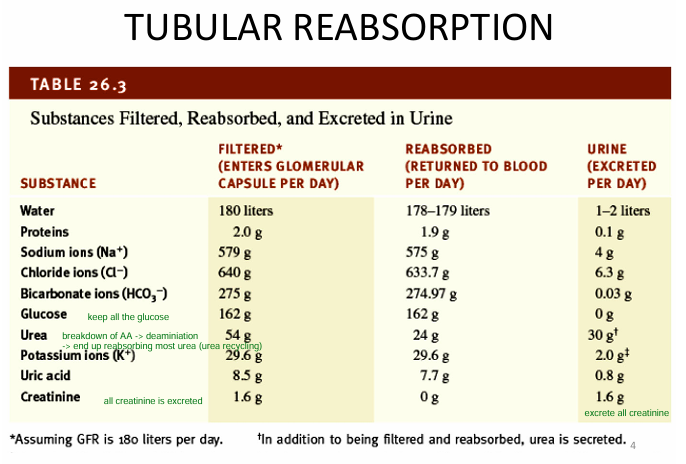
General note: Tubular reabsoprtion of specific ions
-secrete ALL creatinine
-reabosrb half UREA (for urea recycling)
-keep ALL GLUCOSE
What are the REABSOPRTION ROUTES?
1) Paracellular = b/w cells; mainly water
2) Transcellular = across cells; use of pumps/channels
(basolateral surface)
How does PRIMARY active transport and 2NDARY active transport work?
Whats the function of TUBULAR SECRETION?
1) regulate blood pH
2) eliminate substances from the body (mainly H+, K+, ammonium)
- creatinine
What are the general points about transport (doubt you need to rmbr)
1) renal tubule contain MANY TRANSPORT MECHANISMS
2) solutes transported in ONE DIRECTION
- determined via (conc gradient, location of transportion)
3) NaK+ pump located in BASOLATERAL MEMBRANE
- keeps intracellular Na+ LOW (allows for 2ndary active transport)
→ ensures reabsoprtion of Na on APICAL SURFACE
4) Solute reabsoprtion drive MOST WATER ABSOPRTION
- 90% of water reabsorbed via OSMOSIS due to Na+, Cl-, glucose reabosrption in proximal convoluted tubule
-10% regulated by ADH in collecting duct
5) transporters have an UPPERLIMIT on how fast they can work
- if they’re all occupied, you may get glucose in urine (premise of diabetes)
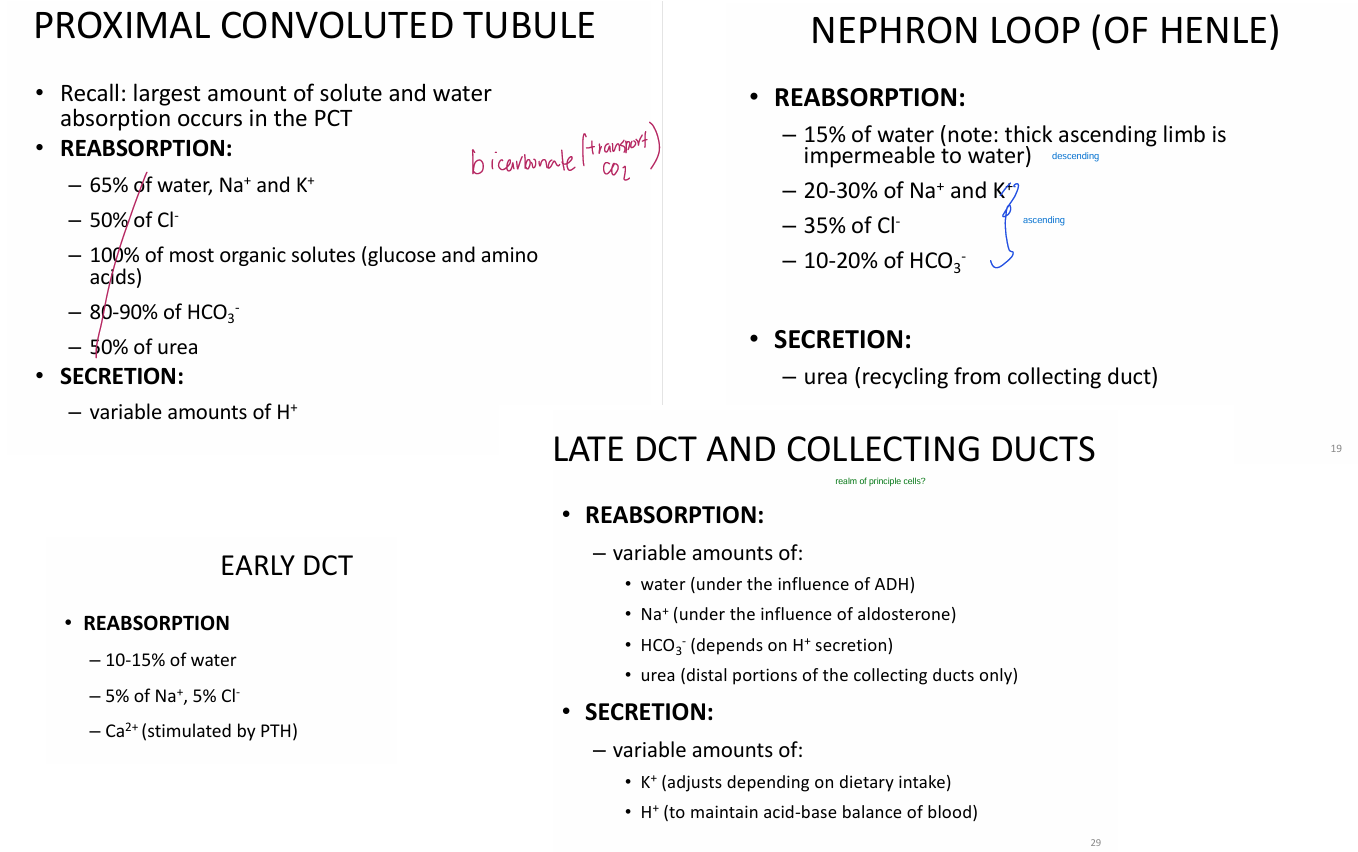
What is the function of the PROXIMAL convoluted tubule?
1) most resabsoprtion of water + solute
2) secrete SOME H+
When is there urea reabsoprtion?
45-50% of filtered urea reabsorbed by PROXIMAL CONVULUTED TUBE via passive diffusion
- additional urea reasborbed by ADH @ collecting duct (discussed later)
(urea reabsorbed via following the water; after osmotic gradient created)
bowmans capsule
- capsular epithelium = simple squamous
- visceral epithelium (hose) = modified simple squamous
Proximal tubule = simple cuboidal
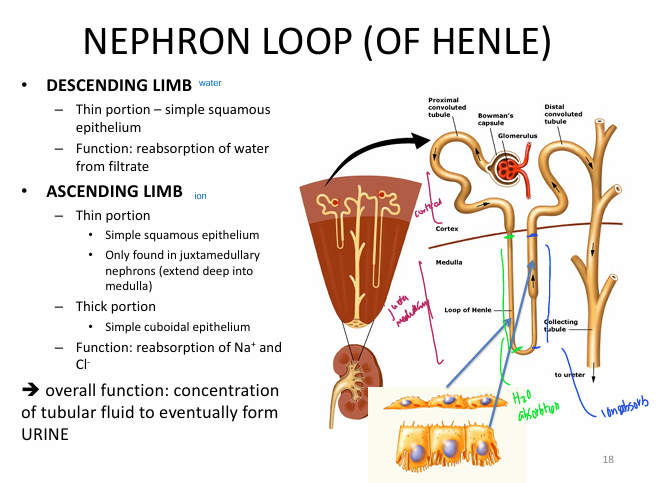
Nephron loop
Descending limb = simple squamous epithelium
Ascending limb =
simple squamous epithelium (thin portion)
simple cuboidal epithelium (thick portin)
Distal tubule = simple cuboidal epithelium
Describe the fxn of the LOOP OF HENLE.
1) Descending limb = reabsorption of WATER from filtrate
2) Ascending limb = thin + thick = reabsorption of Na+ & Cl-
Overall fxn = concentration of tubular fluid to form URINE
What is concurrent flow?
tubular fluid in ascending and descending limb is moving in OPPOSITE DIRECTIONS
What is concurrent multipler?
concurrent flow through descending and ascending limbs of loop of henle
→ establishes progressively INCREASING osmotic gradient in renal medulla (higher NaCl concentration the deeper you are)
→ kidney able to create concentrated urine
where to we maximize Na and Cl transport?
thick ascneding limb due to concurrent multuipler
What is the function of the distal convoluted tubule?
1) reabsoprtion of:
- Na, Ca, water via PRINCIPAL CELLS (receptors for ADH and aldosterone)
2) secretion of H+ via INTERCALATED CELLS
(from here onwards is good)
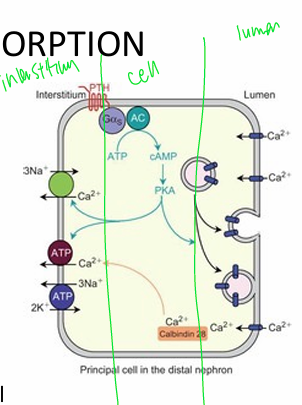
What is the significance of Parathyroid hormone in kidneys?
Low blood calcium → activate PTH
→ PTH binds to PTH receptors @ EARLY DCT
→ places Ca2+ channels onto apical surface
→ Calcium reabsorbed from lumen → cell
→ more Ca2+ reabsorbed into interstitium via Na-Ca antiporter on basolateral surface
(Ca to interstitium; Na to cell)
Whats special about principal cells in terms of K+?
Principal cells have K+ leakage on BOTH apical and basolateral surface. Therefore can either:
- diffuse into tubular fluid (apical)
- return to interstitium/blood (basolateral)
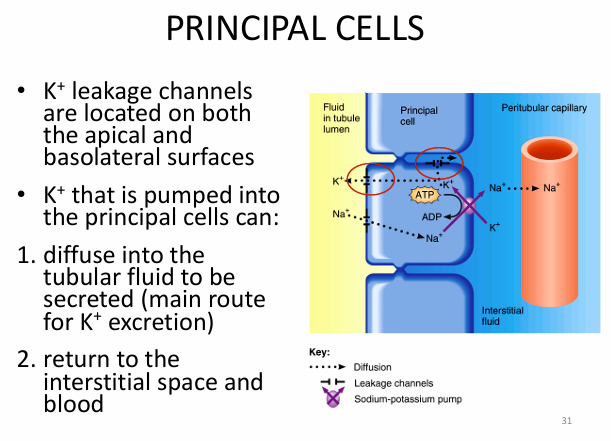
Discuss the PRINCIPAL CELLS.
Located in LATE distal convoluted tubule
1) K+ leakage cells on both apical and basolateral surface
2) Na K+ pump on basolateral
3) Na leak channels on apical
(constant pumping of Na into interstitium via NaK+ pump allows passive reabsorption through Na leak channels on apical surface | lumen → cell)

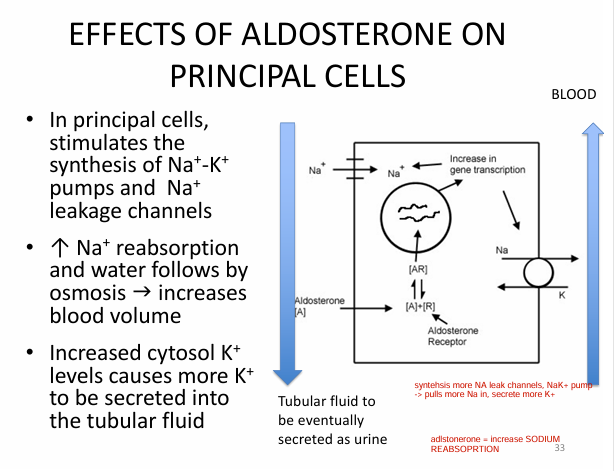
Discuss the significance of ALDOSTERONE on the kidneys makes sense at time of notes)
0) Increased BLOOD K+ levels
0) Decreased BV or BP
1) Activate RAAS
2) Activates aldosterone secretion
3) Aldosterone binds to principal cells in DCT
→ increase Na K+ pumps on basolateral surface + Na leakage on apical surface
→ increased Na+ reabsoprtion (b/c NaK+ pumping more Na into interstitium → more Na passive reabsoprtion from Na leak channels)
→ water follows by osmosis (due to increased Na in interstitium; so high osmolarity)
→ increased BLOOD VOLUME
4) Increased K+ in cytosol (cell) (from K+ from NaK+ pump) → more K+ secreted into tubular fluid
Discuss the significance of ADH for kidneys (makes sense at time of notes)
0) Increased blood osmolarity (hella salty; bunch of solutes)
0) Decreased BV or BP
1) Release ADH from posterior pituitary
2) ADH binds to principal cells in DCT
3) Vesicles containing aquaporin fuse to apical surface
4) INCREASED WATER REABSOPRTION (H2O from lumen → cell → interstitium)
5) Increased blood volume

What’s the significance of ADH on urea recycling?
0) ADH activates urea transporters in medullary COLLECTING DUCT
1) increased urea into interstitium
2) urea = osmotically active molecule
→ urea in interstitial space = WATER FOLLOWS BY OSMOSIS
(just think; urea is hella salty)
3) as urea conc. increase in interstitium
→ diffuses back into thin portion of nephron loop
4) travels back to collecting duct
= urea recycling (just making the urine more concentrated)
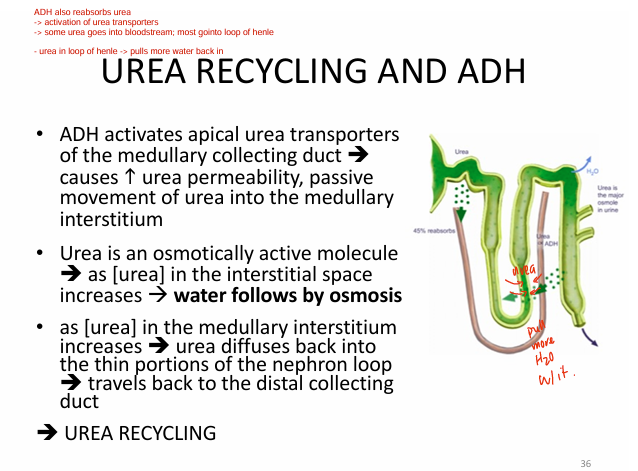
Urea is __
an osmotically active molecule
- water follows by osmosis (b/c urea is so fckin salty)
When is H+ secreted?
H+ secreted from:
- cells of PCT (makes sense)
- intercalated cells of late DCT & collecting ducts
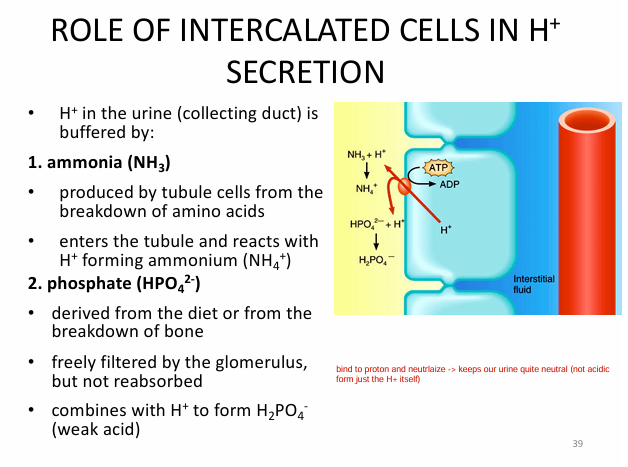
What’s the role of intercalated cells in H+ secretion?
(Inside intercalated disk)
1) CO2 converted to H+ & HCO3-
2) H+ ATPase pump uses ATP to bring H+ into lumen (excrete it) (makes urine acidic)
2) Cl- + HCO3- antiporter
- Cl- into cell
- HCO3- into interstitium (that good shit)
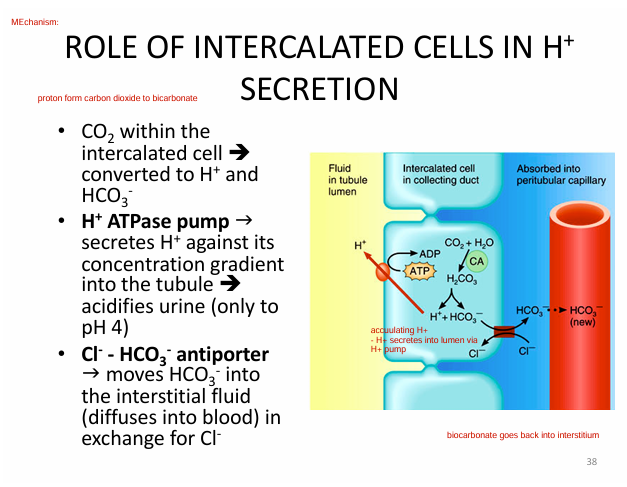
With the intercalated disk creating an acidic environment (due to pumping out H+ into lumen), how do we counteract this?
H+ in urine is buffered by:
1) ammonia (NH3)
- breakdown of A.A (deamination)
2) phosphate (HPO4²-)
- from diet/bone breakdown
filtered by glomerulus but never reabsorbed (just stays in the urine)