METABOLISM + EXERCISE
1/46
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
47 Terms
What are the immediate effects of exercise on the body
increased heart rate - increased secretion of adrenaline that stimulates the sympathetic nervous system
vasodilation of arterioles - greater blood flow to skeletal muscles + signalled by nitrous oxide from endothelium
increased stroke volume - more blood leaves left ventricle per beat
increased breathing rate - increased ventilation —> increased conc. gradient so more O2 diffuses in and CO2 diffuses out
increased breathing depth - electrical impulses sent to intercostal muscles + diaphragm —> contract more forcibly
reduced blood flow to digestive system
What are the long term effects of exercise on the circulatory system
increased VO2 max
increased stroke volume
increased heart size - hypertrophy ( increased cardiac muscle size) —> stronger contractions
increased no. of RBCs - athlete’s have thicker (more viscous) blood as more dense
decreased resting heart rate
what are the long term effects of exercise on the respiratory system
increased breathing rate
increased tidal volume (vol of air inhaled/exhaled at rest)
increased vital capacity (max. volume of air exhaled after a deep breath in) - due to developed intercostal muscles + diaphragm
increased density of capillaries in lungs - increased SA for gas exchange
what are the long term effects of exercise on the skeletal system
increased efficiency in lipid metabolism in muscle fibres - conserves CBH stores in muscle cells
increased capillary network surrounding muscle fibres
increased vascularisation of muscles (inc. size/no. blood vessels that deliver to the skeletal muscles)
increased myoglobin glycogen stores
increased size/no. mitochondria
what is aerobic fitness
the ability of your heart and lungs to respond to the demands of aerobic exercise
how to achieve aerobic fitness
20 mins of aerobic exercise every day over a sustained period at 70% max. heart rate
factors that affect aerobic fitness
age
gender
smoking
diet
alcohol consumption
mindset/amount of exercise you do
drug use
benefits of having good aerobic fitness
stronger skeletal muscles
decreases risk of type 2 diabetes
lowers blood pressure
improves mental health
greater cardiovascular health - lowers risk of stroke/heart attack
What does F.I.T.T stand for
frequency
intensity
time
type of training
3 ways to measure the success of a training program?
larger VO2 max
lower resting heart rate
shorter recovery time
What does VO2 max mean?
the maximum rate that oxygen can be taken in and used
what’s the units of VO2 max
dm³ kg^-1 m^-1 / dm³ min^-1
EQ: Describe how VO2 max is measured (INDIRECT)
graded exercise test e.g multilevel treadmill
at 3 min intervals increase speed + incline of treadmill
measure the O2 and CO2 concentration of inhaled and exhaled air
VO2 max is when oxygen consumption remains steady whilst intensity of exercise increases
continue until person is fatigued
What to do BEFORE assessing someone’s VO2 max
person must consent
carry out risk assessment to check for pre-existing medical conditions
ensure all participants have had training on how to use equipment
what’s a DIRECT measure of VO2 max
use a gas analyser
measure ventilation rate and conc. of O2 and CO2 in the inhaled and exhaled air
PROS/CONS of direct measure
more accurate data obtained
BUT specific equipment needed
What are the methods of enhancing athletic performance
erythropoietin
blood doping
steroids
carbohydrate loading
How does erythropoietin enhance performance
Erythropoietin (EPO) is a hormone that stimulates RBC production
inject body with recombinant erythropoietin
more RBCs produced —> more haemoglobin —.> more O2 transported to muscles —> inc. rate of aerobic respiration
PROS / CONS of erythropoietin
PROS:
more RBCs = more oxygen to muscles = more aerobic respiration
good for endurance sports
CONS:
too many RBCs can make blood more viscous = inc. risk of blood clots, heart attack + stroke
How does blood doping enhance performance
Artifically increasing no. of RBCs by injecting either your own blood (removed months before competition) or a donor’s
extra blood = more RBCs = more haemoglobin = more O2 transported to muscles = more aerobic respiration
PROS:
increases VO2 max
delays muscle fatigue - longer aerobic respiration
CONS:
illegal
more RBCs = thicker blood = inc. risk of blood clots/stroke
greater heart strain - contract harder to pump thicker blood
what’s the structure of haemoglobin
quaternary structure - 4 ppc
haem group attached to centre of each ppc
each haem group can carry 1 OXYGEN MOLECULE
What does association and dissociation mean?
association/loading = binding of an O molecule to 1 haem group to form oxyhaemoglobin
dissociation/unloading = release of an O molecule from a haem group
Describe and explain the shape of an oxygen dissociation curve
SIGMOIDAL SHAPE:
initially, there’s a small increase in partial pressure of O2, so a small increase in % saturation of Hb
there’s a larger increase in PO2 so a larger increase in % sat of Hb
there’s a smaller increase in PO2 so a smaller increase in & sat Hb
at 0, all the Hb is bound to an O molecule
What is cooperative binding
it’s hard for the 1st haem group to bind to oxygen as it’s hidden
but after the 1st haem group binds with O, Hb undergoes a conformational change, so it’s easier for the 2nd and 3rd haem group to bind (haem groups become more exposed)
hard for 4th haem group to bind as there’s a lower chance of O binding to that specific haem group (less likely to collide)
Difference between adult Hb and fetal Hb
fetal Hb has HIGHER AFFINITY FOR OXYGEN —> binds more readily to O2 and less willing to release it
increases exchange of O2 from mum to fetus
exchange of blood occurs in placenta by a counter current system that ensures they never mix
difference between adult Hb curve and fetal Hb curve
fetal Hb curve is shifted more LEFT (not far left as O would only be released at really low PO2)
What does it mean if an O dissociation curve was shifted more RIGHT
decreased affinity of Hb for oxygen
more oxygen is released at low PO2
so more oxygen is available for aerobic respiration
so higher rate of aerobic respiration
structure of MYOGLOBIN
only found in muscles
made up of 1 ppc attached to 1 haem group
so only binds to 1 oxygen molecule
function of myoglobin
stores O2 in skeletal muscles
HIGHER affinity for oxygen than Hb —> only releases O2 at really low PO2
What factors affect oxygen dissociation from respiratory pigments?
temperature
pH
CO2
How does temperature affect O2 dissociation
INCREASE temp = shifts RIGHT
higher temp weakens association between O2 molecules and haem groups + disrupts H bonds in tertiary/quaternary structure
affinity decreases
e.g during exercise, muscle temp inc
How does pH affect O2 dissociation
DECREASE pH = shifts RIGHT
decreased pH = increased H+ ion conc. = more binding to Hb to form more haemoglobinic acid that reduced affinity
How is CO2 transported in the blood
dissolved in the blood plasma
as hydrogen carbonate ions dissolved in plasma
combines with NH2 groups on Hb to form carbaminohaemoglobin
Explain how haemoglobin acts as a buffer
CO2 reacts with water to form carbonic acid (H2CO3)
this reaction is catalysed by carbonic anhydrase
H2CO3 dissociates to form H+ and HCO3- (hydrogen carbonate/bicarbonate)
Due to an imbalance of charges, Cl- ions diffuse into RBC via CHLORIDE SHIFT
H+ ions combines with Hb to form haemoglobinic acid
H+ ions also reduces the affinity of oxyhaemoglobin, HbO8, (that’s already present in the RBC) for oxygen, so O2 diffuses out of the RBC
What happens when the partial pressure of CO2 is low
Hydrogen carbonate (HCO3-) ions diffuses back into the RBCS, whilst Cl- ions diffuses out
HCO3- ions reacts with H+ ions to reform carbonic acid (H2CO3)
H2CO3 is hydrolysed by carbonic anhydrase to form CO2 which diffuses out of the RBCs into the plasma
CO2 is exhaled
types of muscle
cardiac - myogenic so contracts without external stimulation needed
smooth muscle - contains actin/myosin but not striated
skeletal - striated muscle
describe the ultrastructure of skeletal muscle
muscle fibre - long, cylindrical multinucleated cell
myofibril - rod-like structures running through the fibres, made up of sarcomeres
myofilaments - THICK = myosin, THIN = actin
sarcoplasmic reticulum = stores and releases Ca2+ ions needed for muscle contraction + contains T TUBULES that conduct the action potential into the muscle fibre
Sarcolemma = encloses the muscle fibre and separates it
what is a sarcomere
1 contractile unit of a myofibril
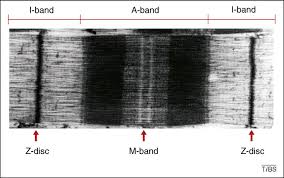
describe a sarcomere
A band = DARK BAND that shows where the myosin is
I band = LIGHT BAND = only ACTIN
actin = THIN
myosin = THICK
H ZONE = area of just myosin
M line = centre of H zone
Z Disc = marks start and end of sarcomere
what are the proteins found in muscle fibres
troponin - has a Ca2+ binding site
tropomyosin - blocks the actin-myosin binding site
actin
myosin - tail and head (complementary to A/M binding site)
What is the sliding filament theory
sarcolemma depolarises
T tubules depolarises
this causes Ca"2+ ion channels to open and Ca2+ ions diffuse out
Ca2+ ions binds to the troponin which causes the tropomyosin to move
this exposes the actin-myosin binding site on the actin molecules
myosin heads binds complementary to the actin to form a cross bridge
myosin head tilts backwards and ADP + Pi is released —> POWER STROKE
ratchet mechanism as cross bridges break and reform as actin filaments slides forwards
ATPase in myosin hydrolyses ATP to ADP + Pi to release the myosin head from the actin
sarcomere shortens
What happens at a cholinergic synapse
ACTION POTENTIAL arrives at the presynaptic membrane causing the depolarisation of the motor neurone membrane
Ca2+ ion channels open and Ca2+ ions diffuses down the electrochemical gradient and into the synaptic knob
this stimulates acetyl choline containing vesicles to fuse with the presynaptic membrane
acetyl choline (ACH) molecules are released into the synaptic cleft by exocytosis
ACH diffuses across the synaptic cleft and binds to acetyl choline receptors on the post synaptic membrane
this causes Na+ ion channels to open and Na+ ions to diffuse down the electrochemical gradient and into the sarcolemma
sarcolemma gets depolarised
acetyl choline is broken down by acetylcholineesterase to acetase and choline to prevent permanent depolarisation
choline reabsorbed back into presynaptic membrane and reacts with acetyle coA to form ACH again
what happens at neuromuscular junction
What does EPOC mean
the increased volume of oxygen consumed after vigorous exercise