HAP II Lab Quiz (blood, lymphatic and immune systems)
1/74
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
75 Terms
What are the two general components of blood?
plasma (water and solute) and formed elements (RBCs, WBCs, platelets)
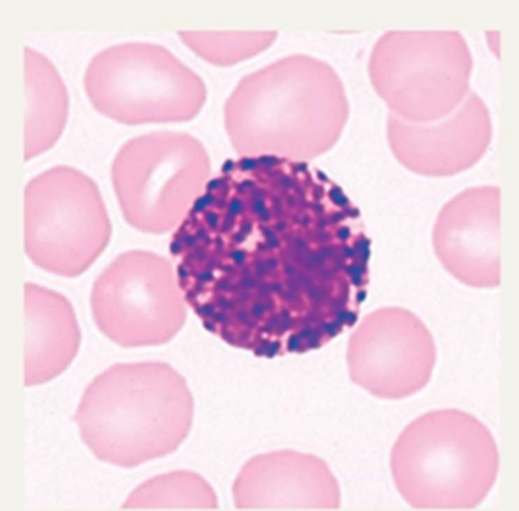
Red blood cells
erythrocytes; biconcave discs (allow for diffusion b/c flat and thin); missing most organelles; contain hemoglobin; most common formed element of blood
White blood cells
leukocytes (neutrophils, lymphocyte, monocyte, eosinophil, basophil)
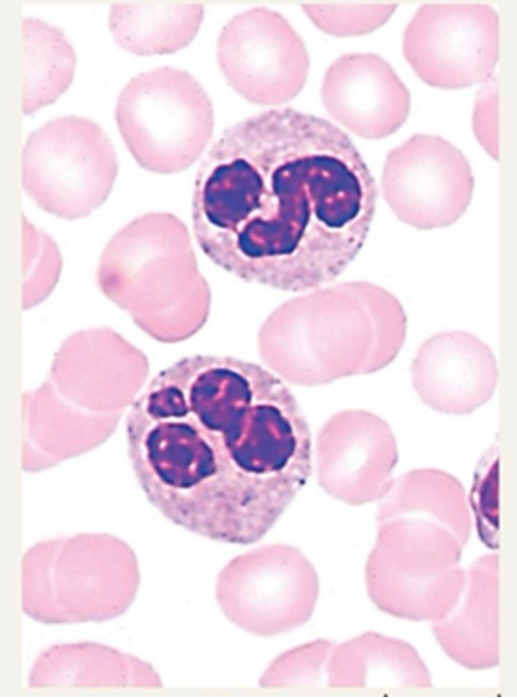
Neutrophils
most common WBC in circulation; phagocyte towards bacteria
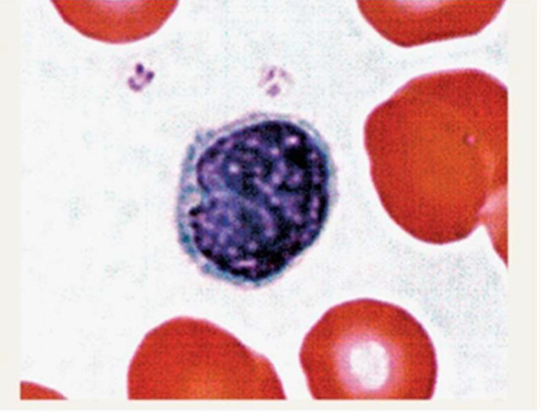
Lymphocytes
(B-cells, T-cells, NK-cells); phagocyte towards viruses
T cell
produced in the bone marrow but mature in the thymus; primarily involved in cell-mediated immunity; recognize infected cells using MHC (Major Histocompatibility Complex) molecules; helper T cells (CD4), cytotoxic T cells (CD8), regulatory T cells, memory T cells
Directly kill infected cells or activate other immune cells
Require antigen presentation via MHC molecules
B cell
produced and mature in the bone marrow; primarily involved in humoral (antibody-mediated) immunity; recognize pathogens directly using their surface antibodies and can present antigens to T cells; plasma cells and memory cells
Produce antibodies to neutralize pathogens
Can recognize free-floating antigens
Helper T cell (CD4)
Act as the "generals" of the immune response by coordinating and activating other immune cells.
Function:
Activate B cells to produce antibodies.
Stimulate cytotoxic T cells (CD8) to kill infected cells.
Recruit and regulate macrophages and other immune cells.
Activation: Recognize antigens presented by MHC class II molecules on antigen-presenting cells (APCs)
Cytotoxic T cell (CD8)
Act as the "soldiers" that directly kill infected or cancerous cells.
Function:
Recognize and destroy virus-infected, cancerous, or damaged cells.
Induce cell death via:
Perforin & Granzymes: Create holes in the target cell and trigger apoptosis
Activation: Recognize antigens presented by MHC class I molecules, which are found on all nucleated cells.
Regulatory T cell
Act as the "peacekeepers" of the immune system by preventing excessive immune responses and autoimmunity.
Function:
Suppress overactive immune responses to avoid tissue damage.
Prevent autoimmune diseases by controlling self-reactive T cells.
Help maintain immune tolerance (prevent attacking harmless substances like food or gut bacteria).
Markers: Express CD4
Mechanism of Action:
Release inhibitory cytokines
Directly suppress the activation of other immune cells.
Memory T cell
Provide long-term immunity by "remembering" past infections.
Function:
Remain in the body after an infection and quickly respond to re-exposure.
Allow for a faster and stronger immune response upon reinfection.
Types:
Central Memory T Cells (T_CM): Found in lymphoid organs, ready to proliferate if needed.
Effector Memory T Cells (T_EM): Circulate in the blood and tissues, ready for immediate action.
Resident Memory T Cells (T_RM): Stay in specificThe "antibody factories" of the immune system
Plasma cell
The "antibody factories" of the immune system.
Function:
Produce and secrete large amounts of antibodies (immunoglobulins).
Antibodies neutralize pathogens by:
Blocking their ability to infect cells (neutralization).
Marking them for destruction (opsonization).
Activating the complement system to destroy pathogens.
Short-lived (days to weeks) but produce massive amounts of antibodies while active.
Activation Process:
B cells recognize an antigen.
With the help of helper T cells (CD4 cells), they differentiate into plasma cells.
Plasma cells migrate to the bone marrow or spleen to continue antibody production.
Memory B cell
The "immune memory keepers" that provide long-term immunity.
Function:
Remain in the body for years (even a lifetime) after infection.
Rapidly respond to the same antigen if encountered again.
Differentiate into plasma cells upon reinfection, producing antibodies much faster than the first time.
Activation Process:
Form during the initial immune response.
Do not secrete antibodies immediately.
Can quickly reactivate and produce antibodies upon re-exposure to a pathogen.
Cell-mediated immunity vs. humoral (antibody-mediated) immunity
Cell-mediated immunity
T cells (especially cytotoxic T cells and helper T cells)
Target: Intracellular pathogens (viruses, some bacteria), cancer cells, and transplanted tissues.
Mechanism:
Helper T Cells (CD4): Activate cytotoxic T cells and macrophages.
Cytotoxic T Cells (CD8): Kill infected or cancerous cells directly.
Regulatory T Cells: Suppress excessive immune responses to prevent autoimmunity.
Does not involve antibodies; relies on direct cell-to-cell interactions
Humoral immunity
B cells and antibodies (immunoglobulins, IgG, IgA, etc.)
Target: Extracellular pathogens (bacteria, toxins, viruses before they enter cells).
Mechanism:
B cells recognize antigens and, with the help of helper T cells (CD4), differentiate into plasma cells.
Plasma cells produce antibodies, which:
Neutralize pathogens by blocking their ability to infect cells.
Mark pathogens for destruction by macrophages and other immune cells.
Activate the complement system, leading to pathogen destruction.
Memory B cells remain for long-term immunity.
Involves antibodies that circulate in blood and lymph.
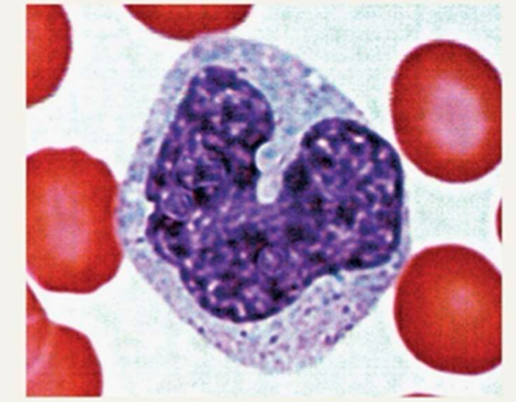
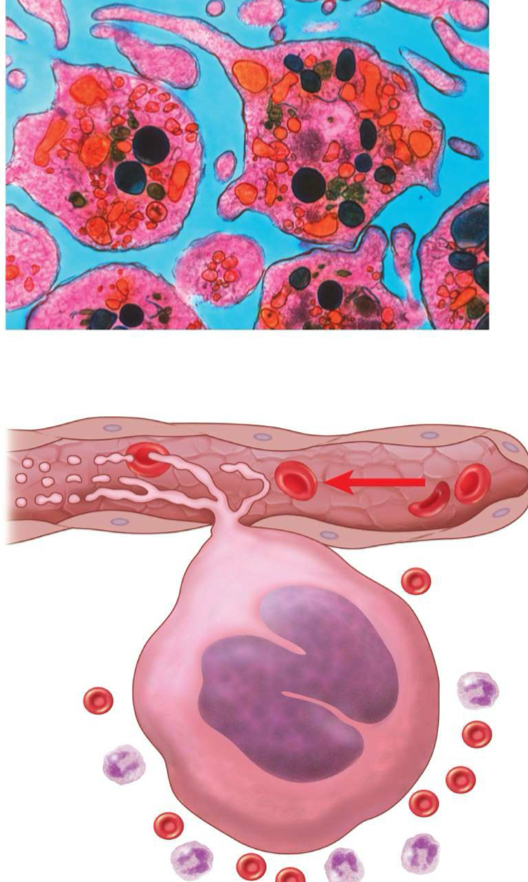
Monocyte
typically leave circulation to become macrophages; largest of the WBCs
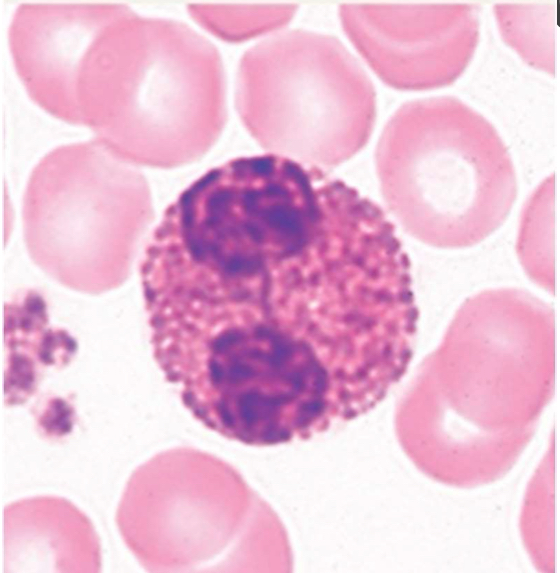
Eosinophil
phagocyte towards parasitic worms
Basophil
rarest WBC in circulation; releases histamine (inflammatory); involved in allergic reactions
Platelets
thrombocytes; aid with clotting and hemostasis; cell fragments of megakaryocytes
Antigens
markers that can trigger an immune reaction
self-antigens: found on your own cells, and should not elicit an immune response
foreign antigens: recognized as “not-self” and will elicit an immune response which can invole the production of antibodies
found on the surface of cells
Antibodies
produced by B-cells; match and bind with specific antigen; when bound they form an antibody-antigen complex which can trigger an immune reaction; found in the circulation in blood plasma
IgG antibodies
most common; late primary and early secondary responses; activates complement system; passed from carrier to unborn child via placenta (after 1st time being infected w/ same pathogen)
IgM antibodies
monomer is a surface receptor of naive B cells; secreted by plasma cells during primary response (1st time infected with pathogen)
IgA antibodies
found in body secretions: saliva, sweat, intestinal juice, milk; stops pathogens from attaching to epithelial surfaces; especially effective against digestive and respiratory pathogens; can pass immunity to an infant through breastfeeding
IgE antibodies
antibody that binds to mast cells or basophils and causes antigen-specific degranulation during an allergic response; triggers histamine release
IgD antibodies
class of antibody whose only known function is as a receptor on naive B cells; important in B cell activation
Heavy chain vs. light chain
heavy chain: larger protein chain of an antibody
light chain: small protein chain of an antibody
Antibodies in the blood
floating around in plasma; against foreign antiens naturally (A and B); antibodies for Rh-factor are present with exposure; antibodies in bloodstream will react with incompatible types and cause agglutination
How is blood type determined?
by antigens present (which in turn determines antibodies present)
How are transfusion reactions caused?
when blood type given is in conflict with antibodies in blood of recipient
Type A- blood
A antigens
anti-B antibodies
no Rh factor
can donate to A+, A-, AB+, and AB-
can receive from A- and O- donors
Type A+ blood
A antigens
anti-B antibodies
Rh factor
can donate to A+, AB+
can receive from A+, A-, O+, and O-
Type B- blood
B antigens
anti-A antibodies
no Rh factor
can donate to B+, B-, AB+, and AB-
can receive from B- and O-
Type B+ blood
B antigens
anti-A antibodies
Rh factor
can donate to B+ and AB+
can receive from B+, B-. O+, and O-
Type AB- blood
A and B antigens
no antibodies
no Rh factor
can donate to AB+ and AB-
can receive from A-, B-, AB-, and O-
Type AB+ blood
A and B antigens
no antibodies
Rh factor
can donate to AB+
can receive from A+, A-, B+, B-, AB+, AB-, O+, and O- (universal recipient)
Type O- blood
no antigens
anti-A and anti-B antibodies
no Rh factor
can donate to A+, A-, B+, B-, AB+, AB-, O+, and O- (universal donor)
can receive from O-
Type O+ blood
no antigens
anti-A and anti-B antibodies
Rh factor
can donate to A+, B+, AB+, and O+
can receive from O+ and O-
The lymphatic system functions to….
return fluid and proteins leaked out of capillaries back to general circulation; absorbs fat from the digestive system; helps trigger the immune system response
Parts of the lymphatic system
lymphoid tissue and lymph
lymphatic vessels
lymphatic capillaries
collecting vessels
trunks
ducts
thoracic duct (cisterna chyli)
right lymphatic duct
lymph nodes
other lymphatic organs
tonsils
peyer’s patches
spleen
thymus
Lymph flow
one way path; capillaries to subclavian veins; no pump (skeletal muscle contractions, arteries and veins (systemic pressure and hydrostatic pressure), and smooth muscle); very low pressure
Lymph nodes
afferent (towards) and efferent (away) vesels; capsule; outer cortex (follicles; B & T cells); inner medulla (sinus channels; reticular endothelial cells and macrophages)
Catecholamines
epinephrine & norepinephrine (flight or fight response)
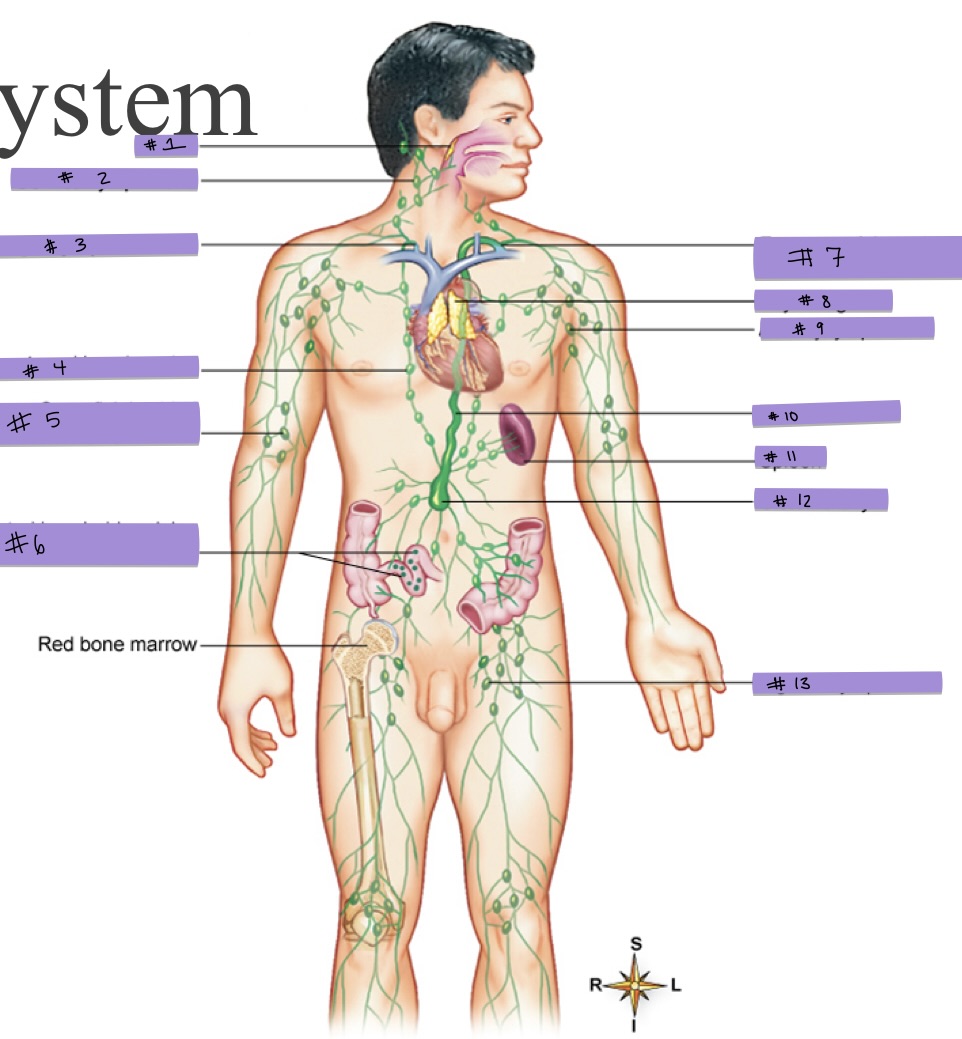
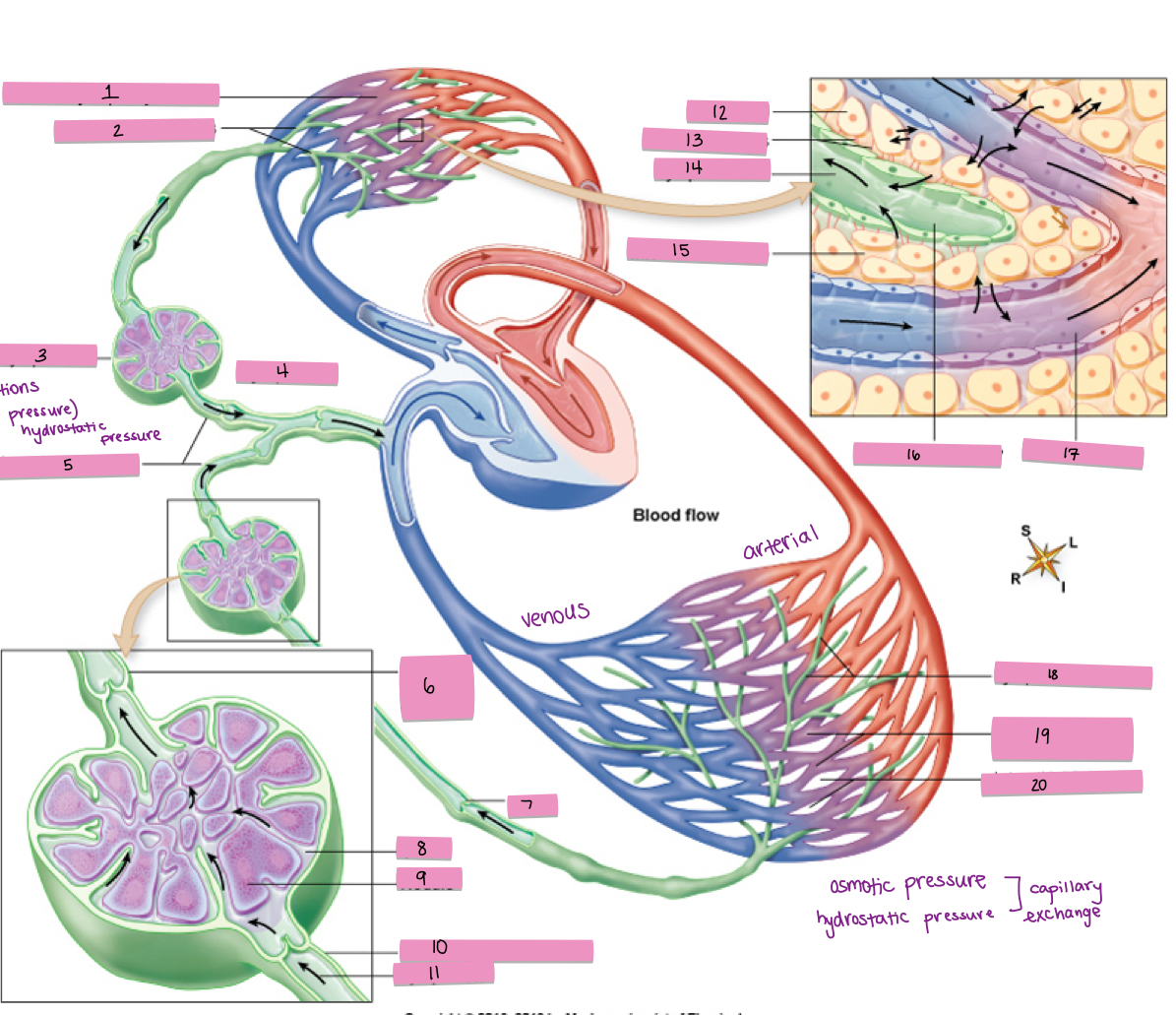
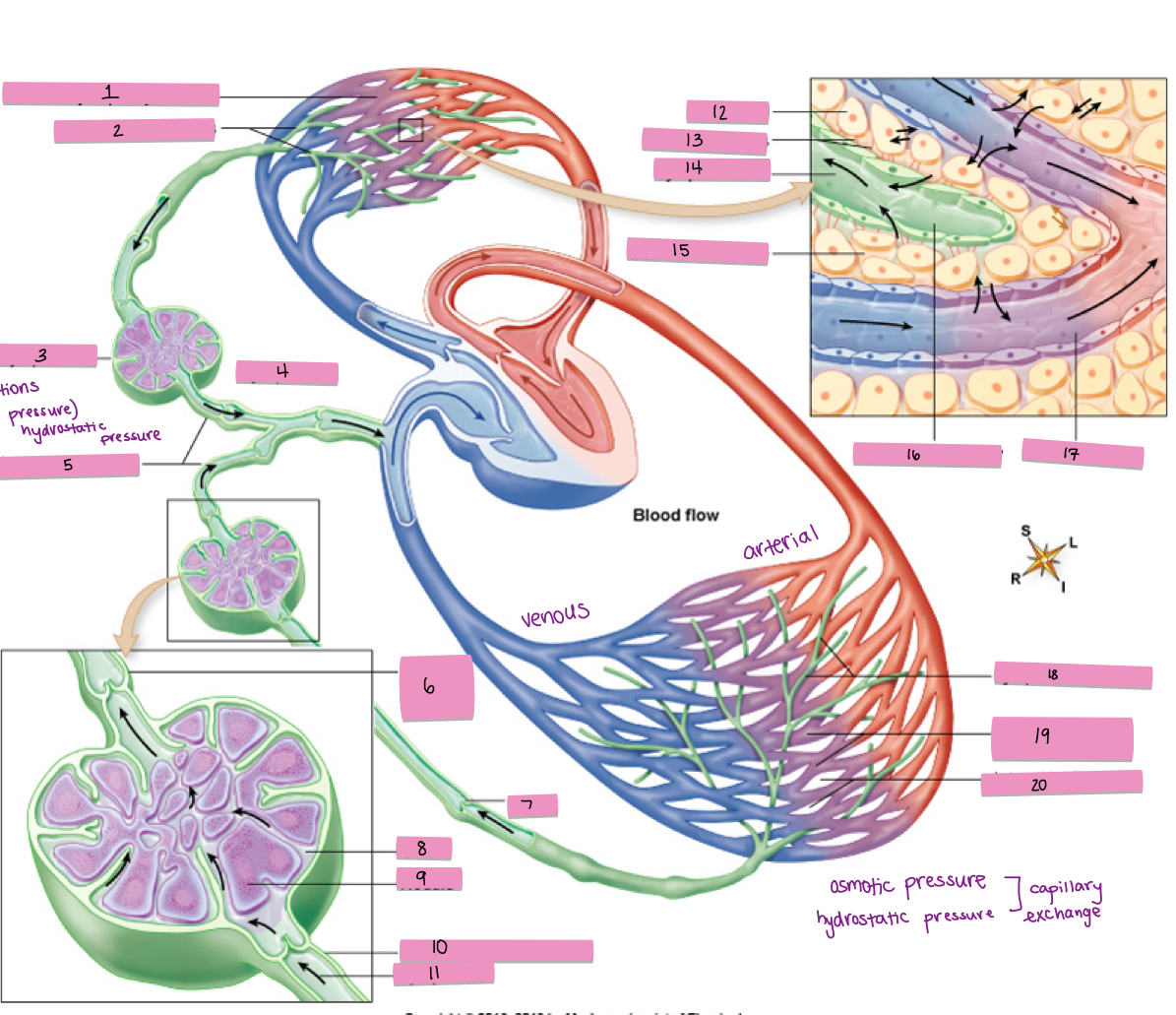
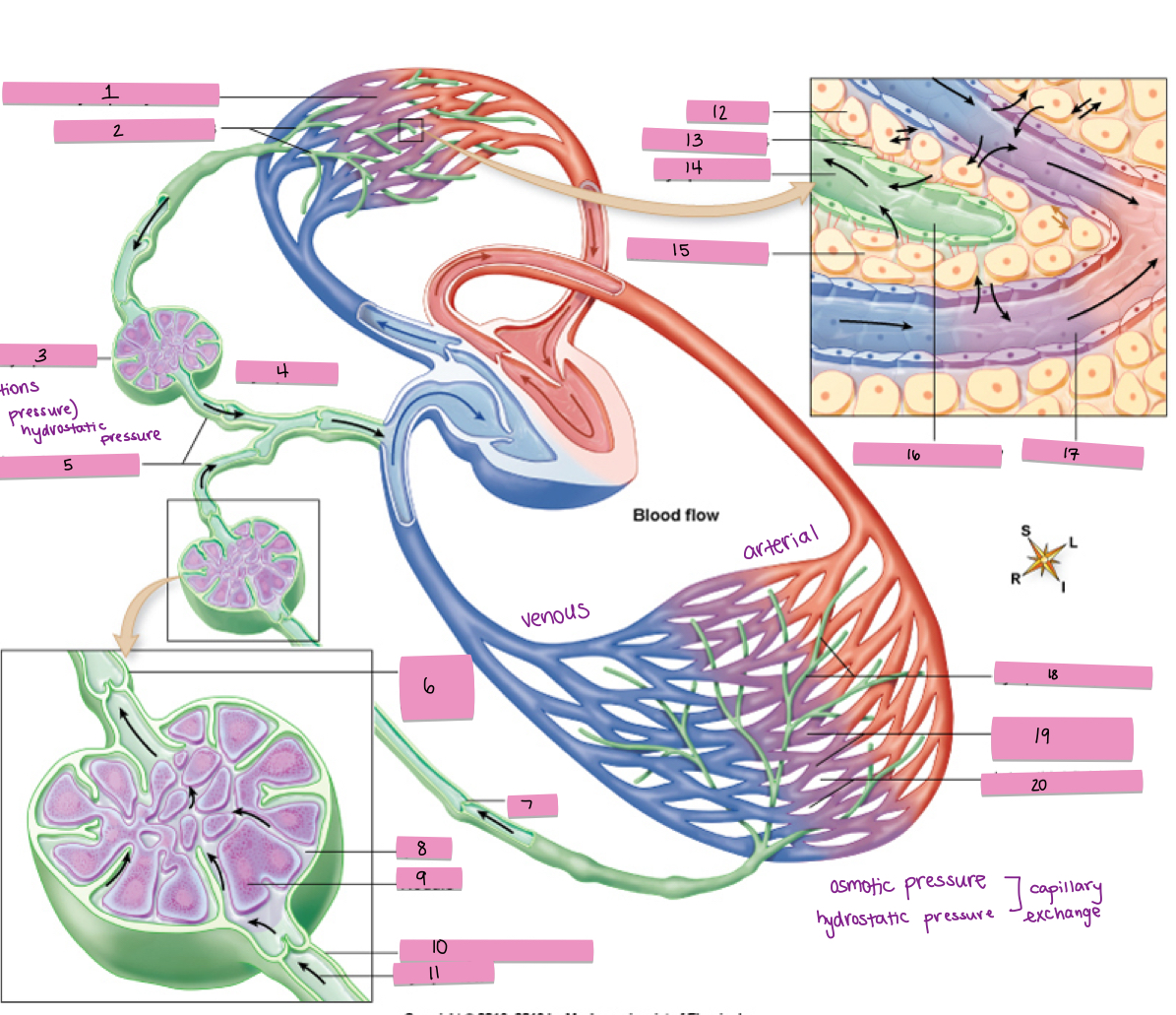
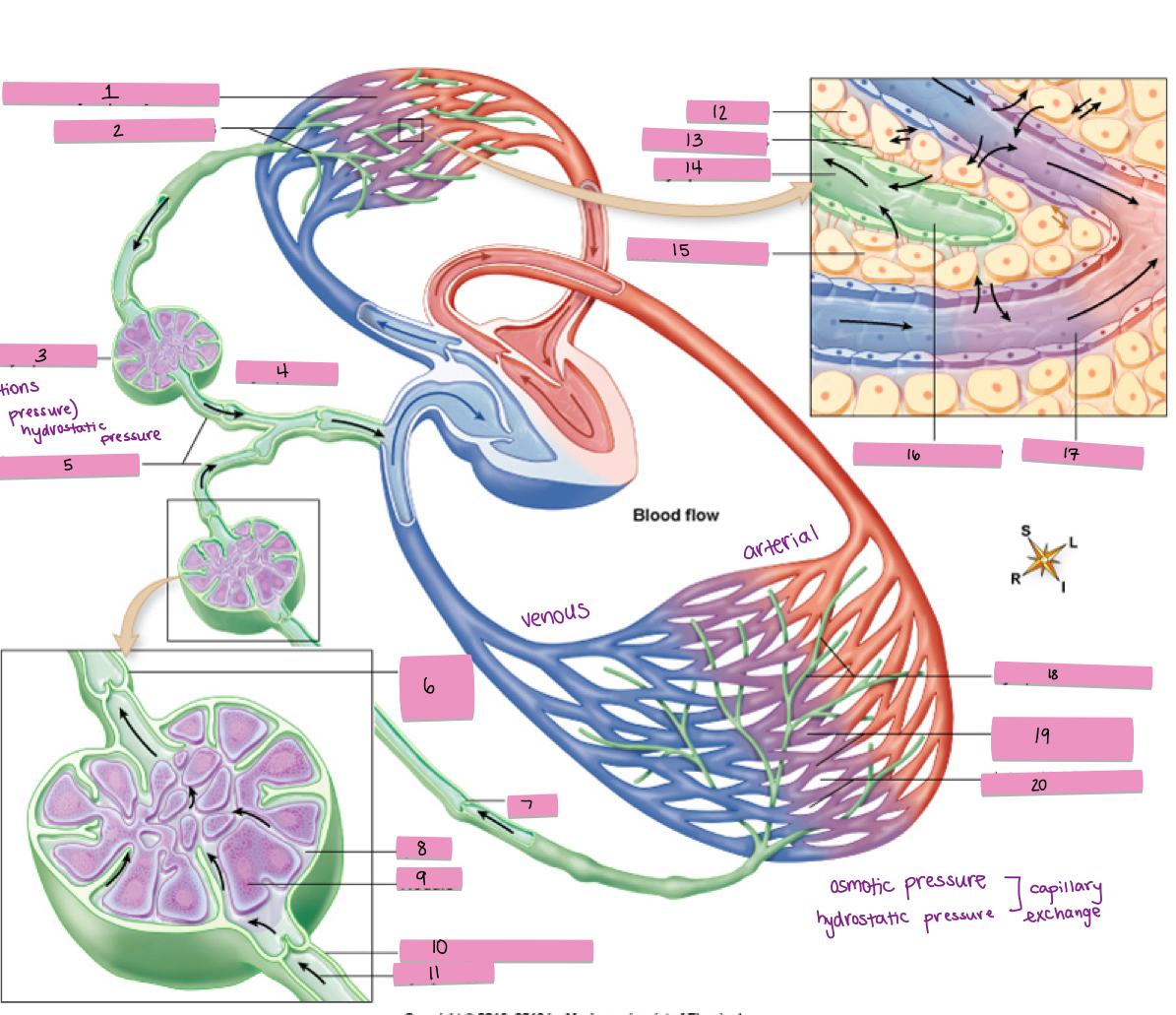
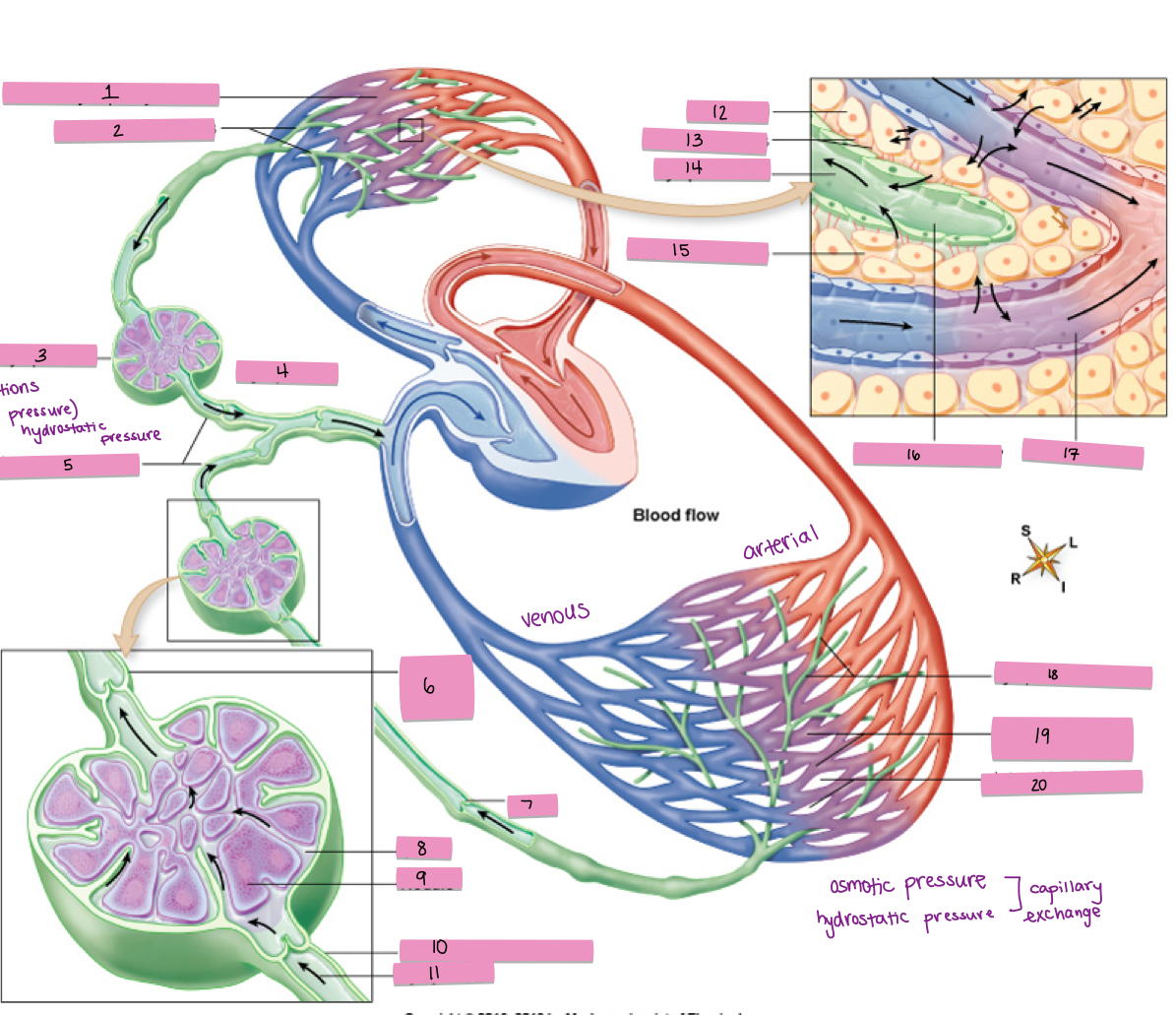
What is #1 pointing to?
tonsils
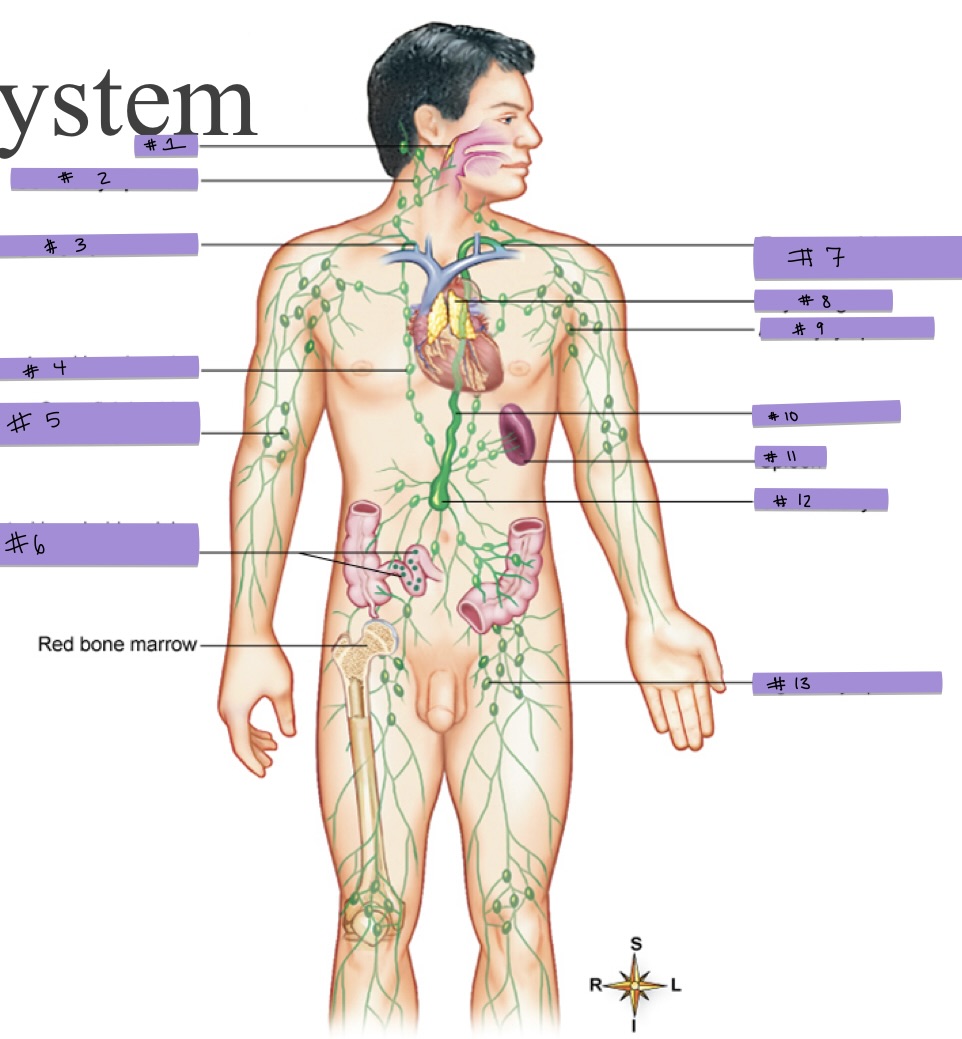
What is #2 pointing to?
cervical lymph node
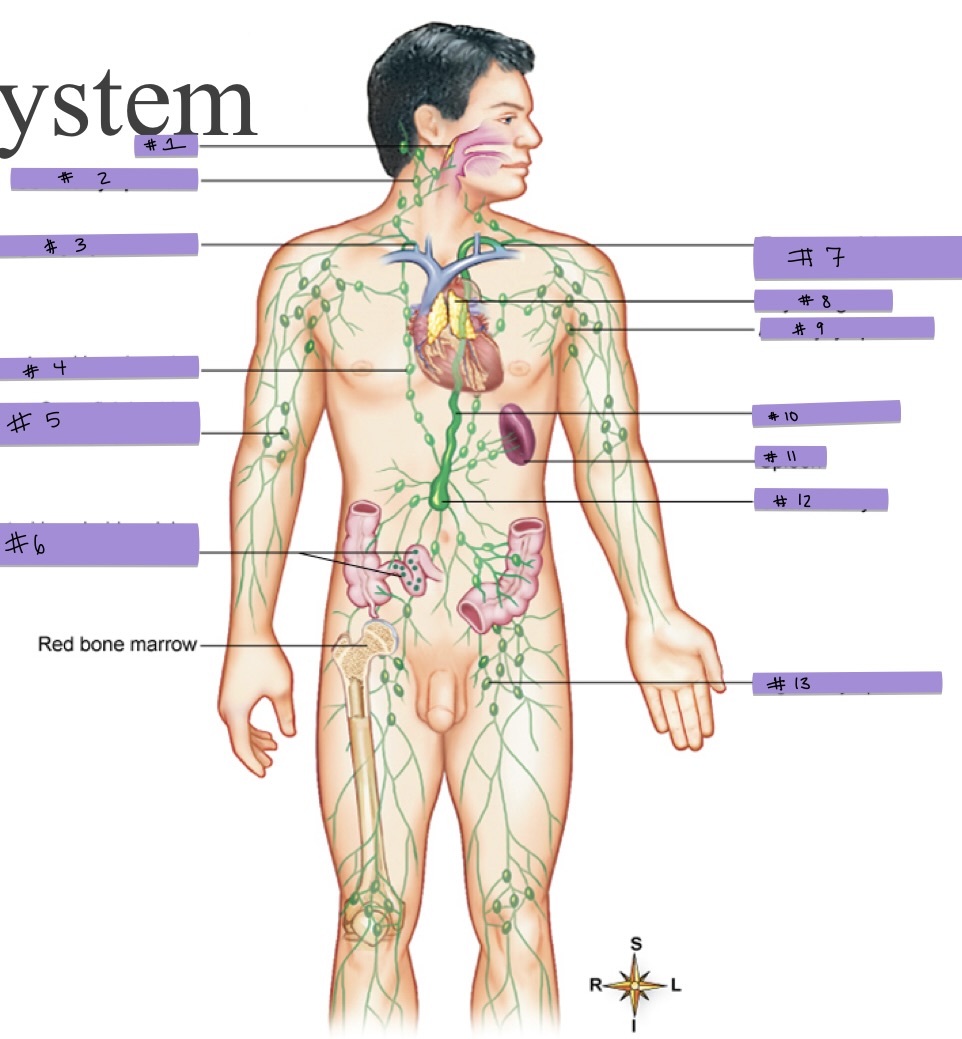
What is #3 pointing to?
right lymphatic duct
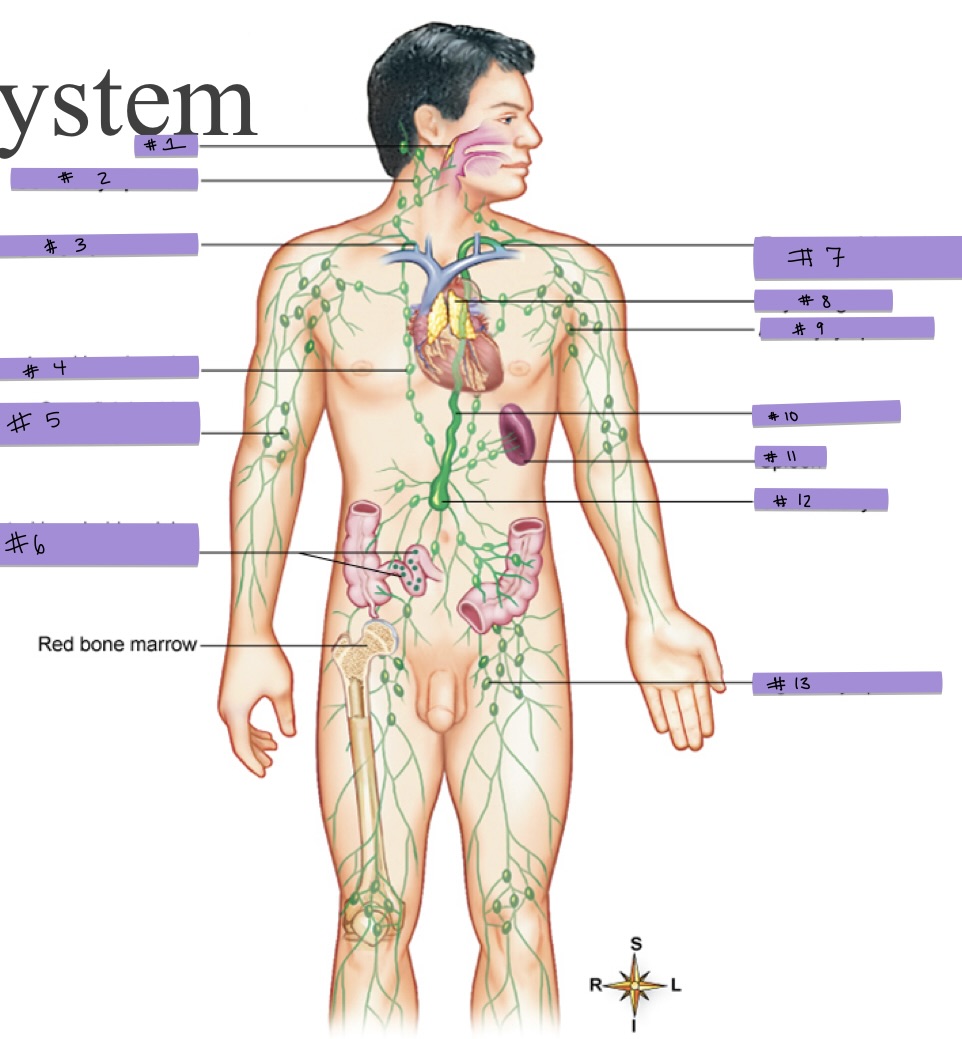
What is #4 pointing to?
parasternal lymph nodes
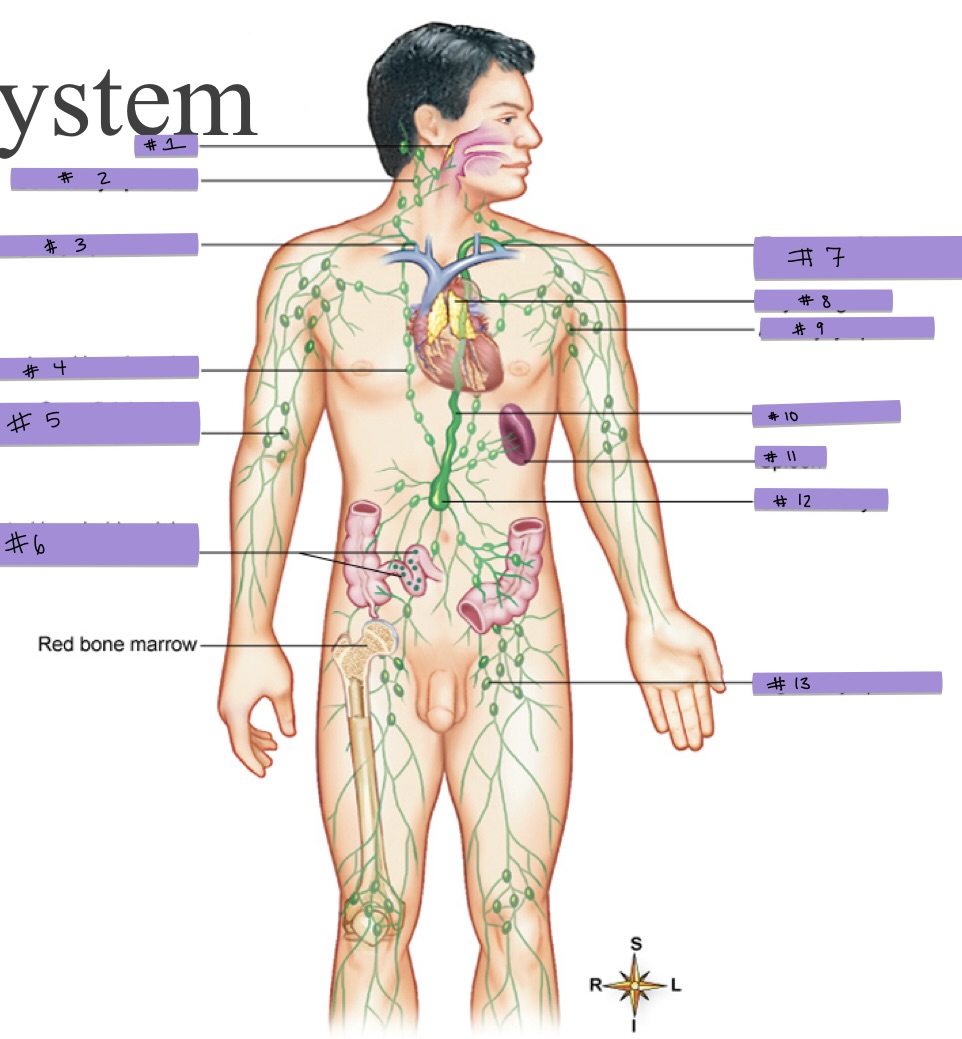
What is #5 pointing to?
superficial cubital (supratrochlear) lymph nodes
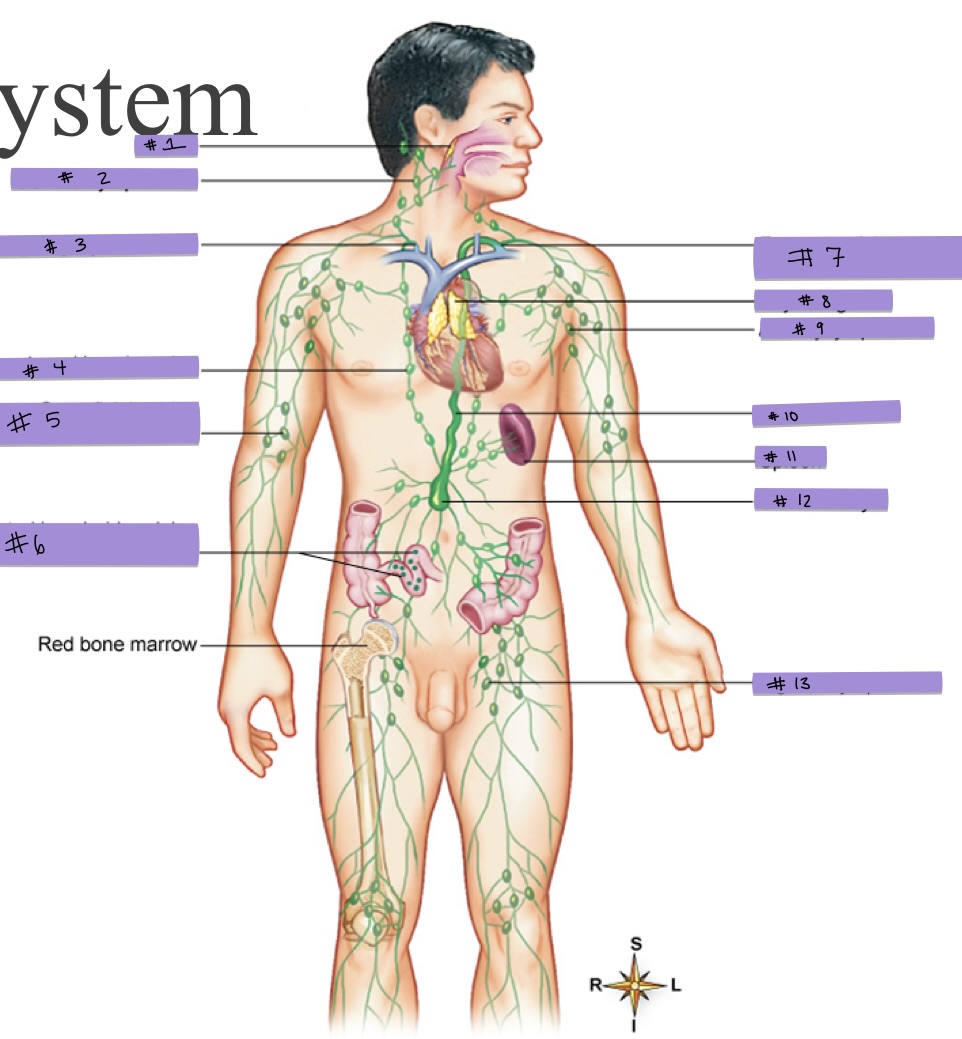
What is #6 pointing to?
aggregated lymphoid nodules (Peyer patches) in intestinal wall
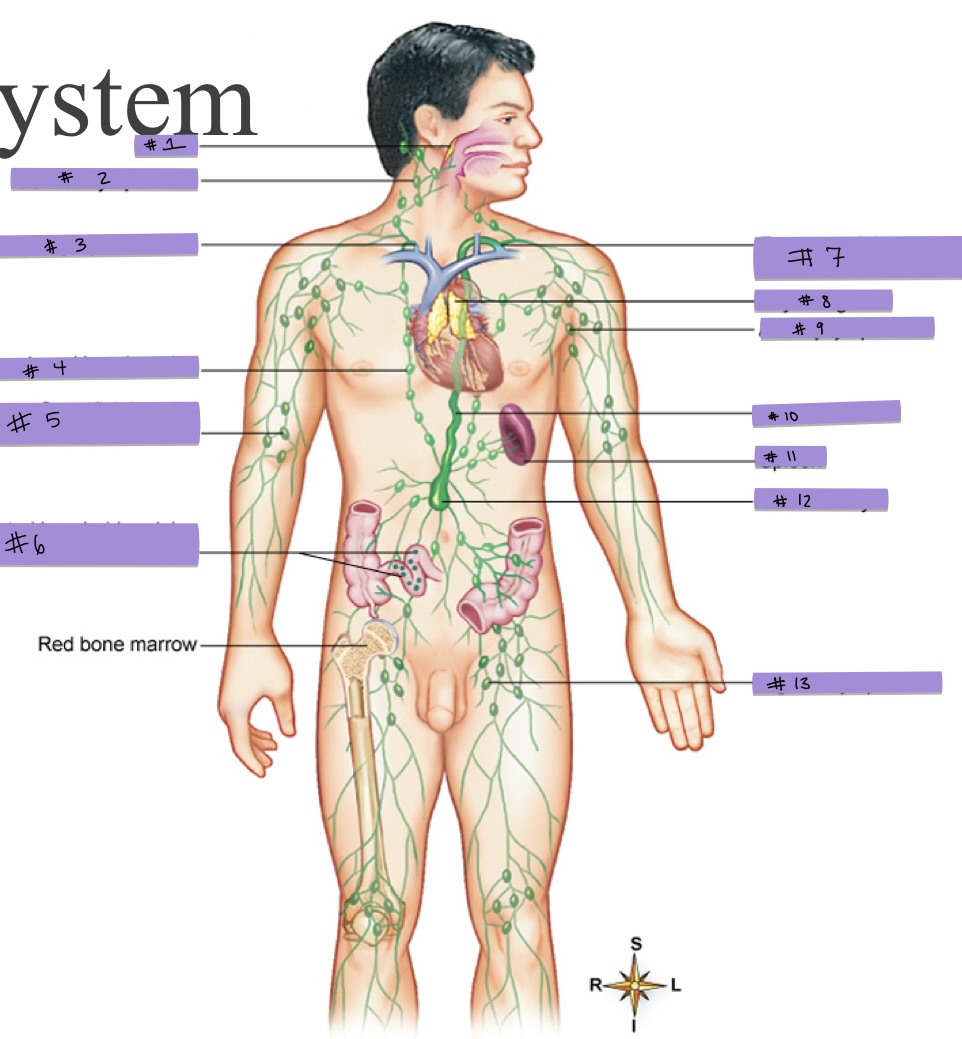
What is #7 pointing to?
entrance of thoracic duct into subclavian vein
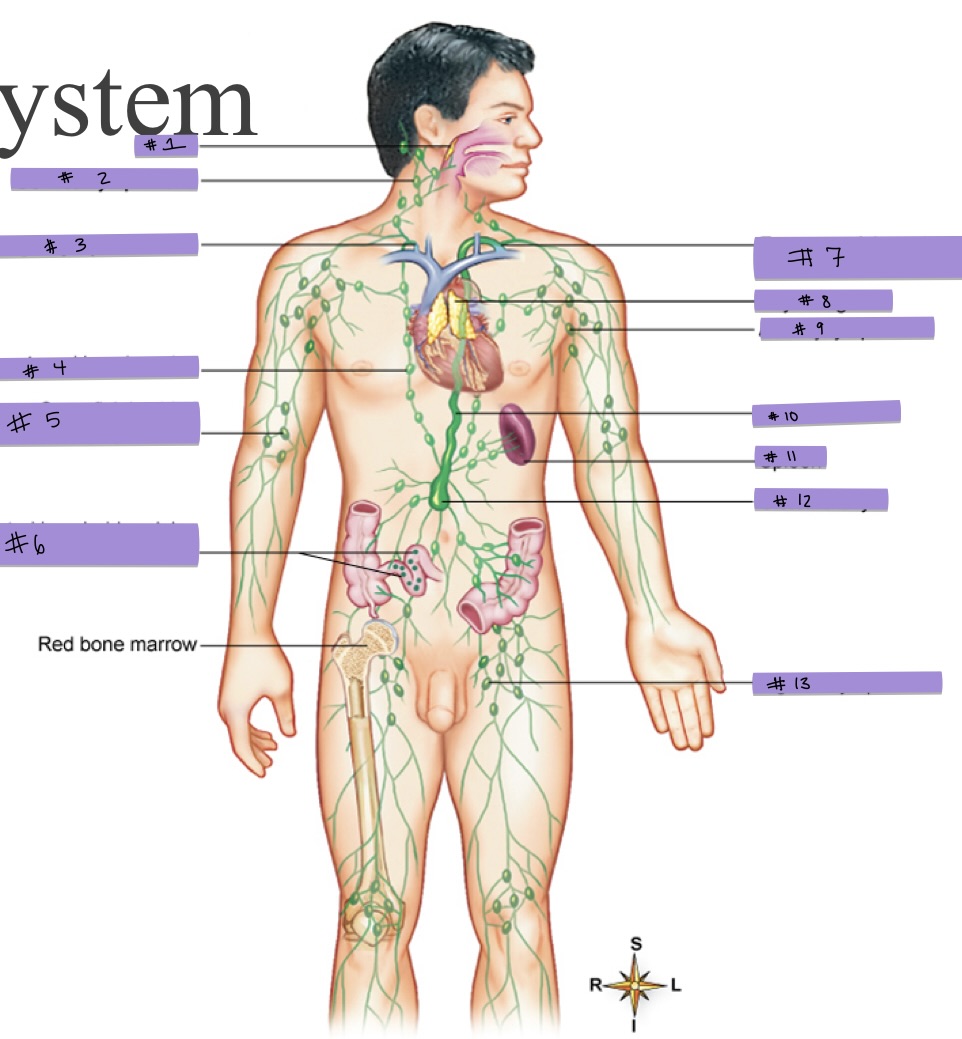
What is #8 pointing to?
thymus gland
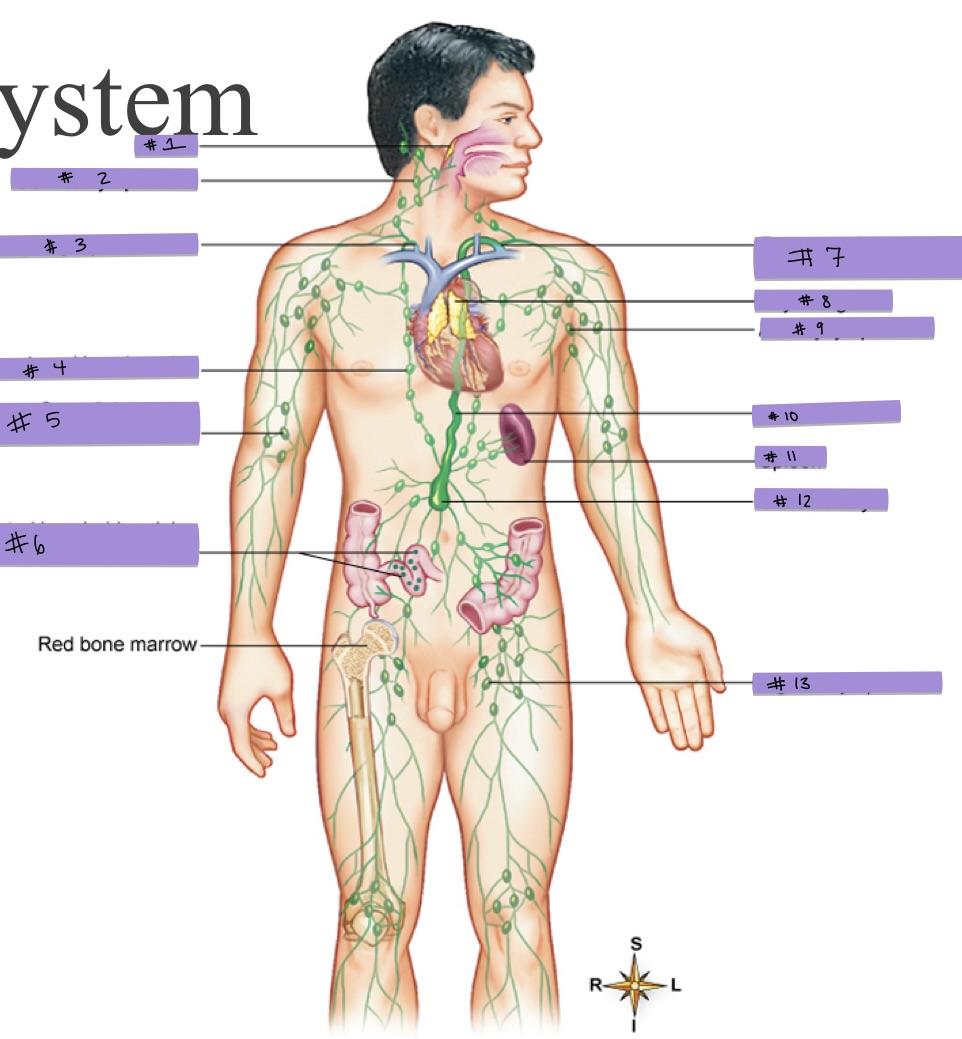
What is #9 pointing to?
axillary lymph node
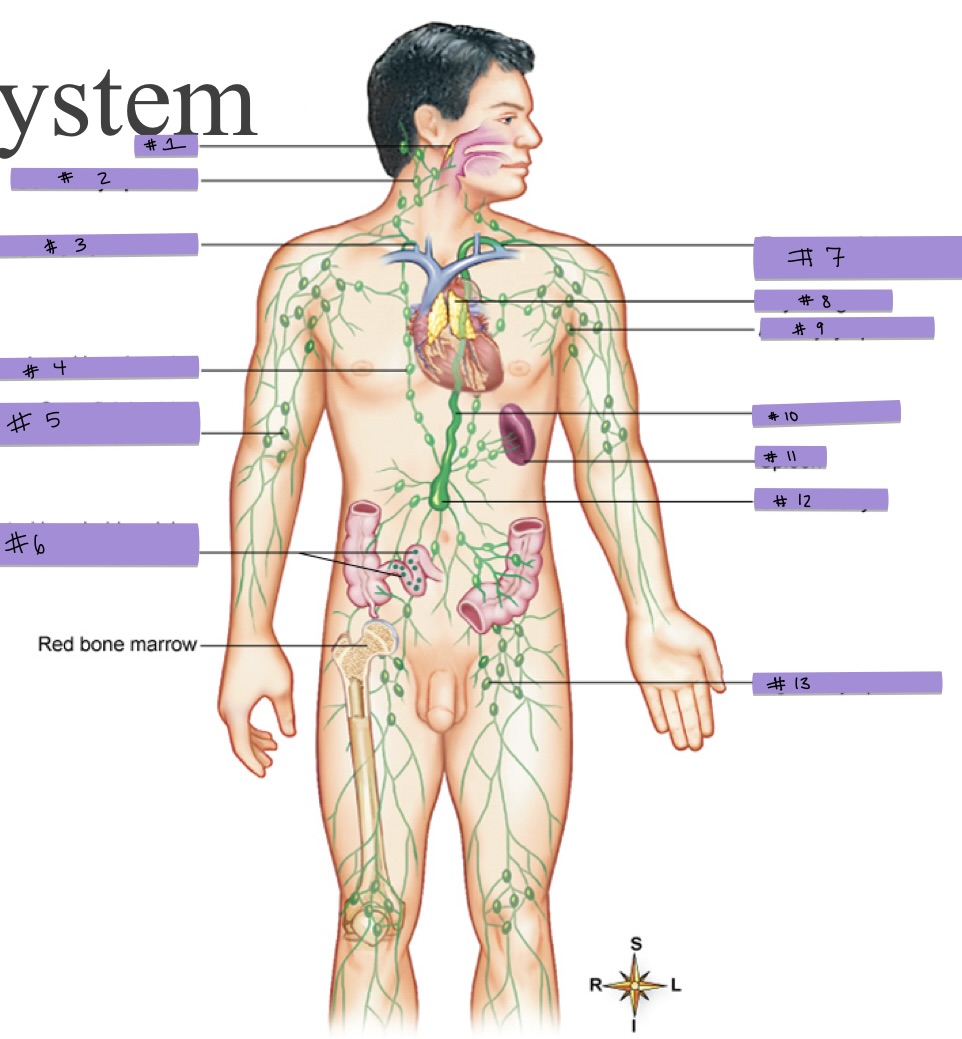
What is #10 pointing to?
thoracic duct
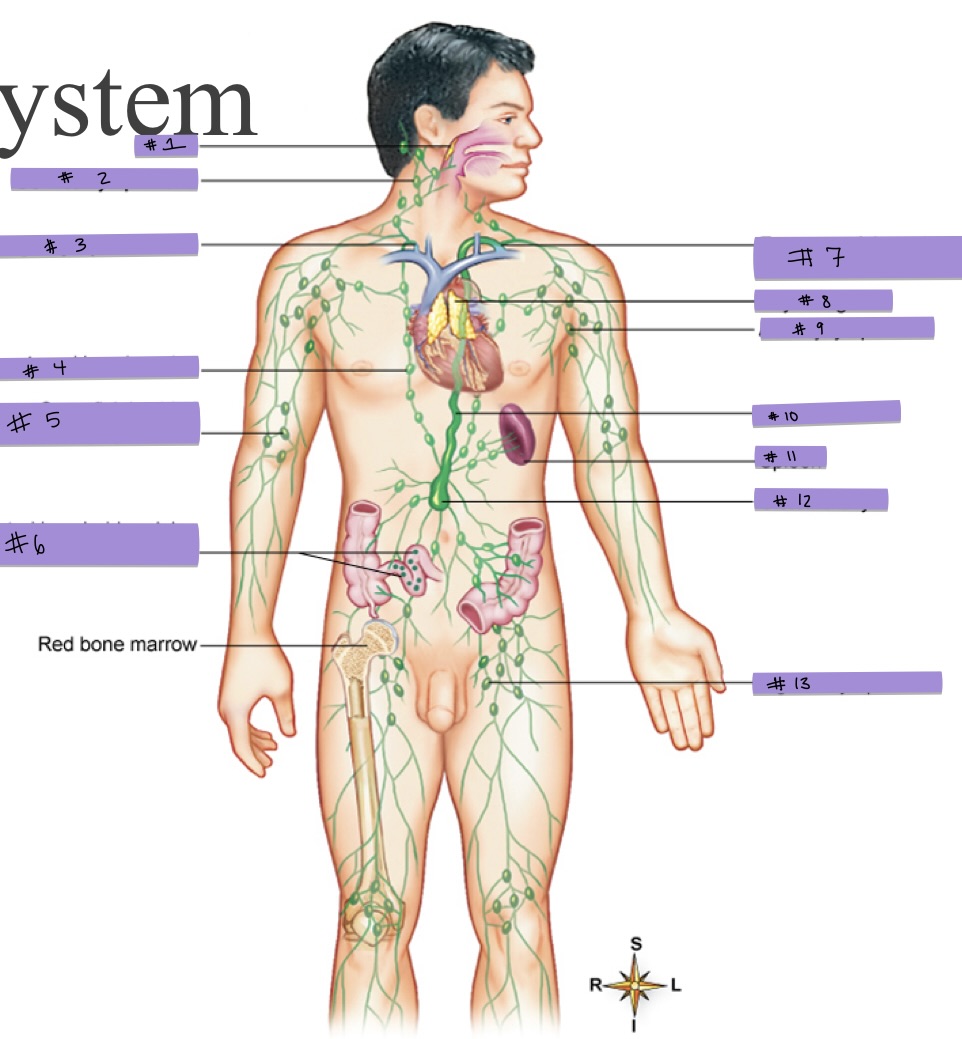
What is #11 pointing to?
spleen
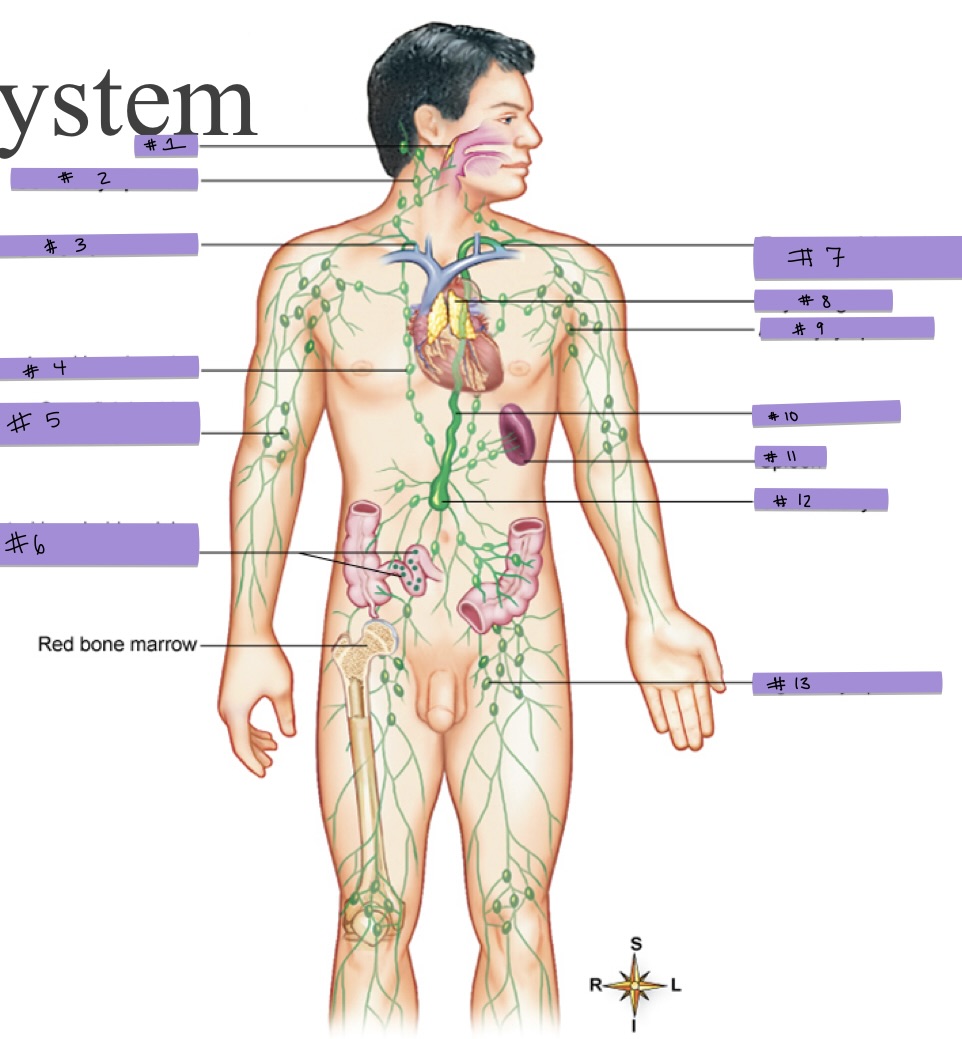
What is #12 pointing to?
cisterna chyli
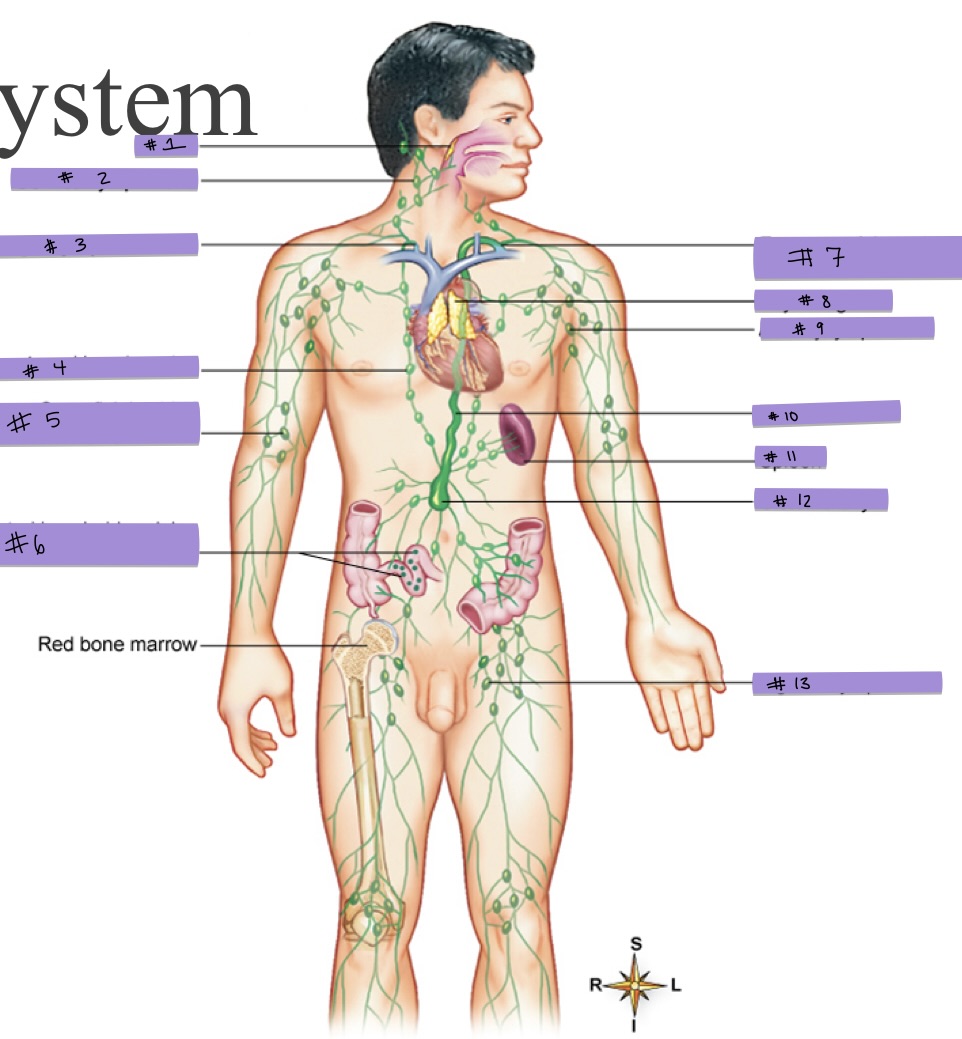
What is #13 pointing to?
inguinal lymph node
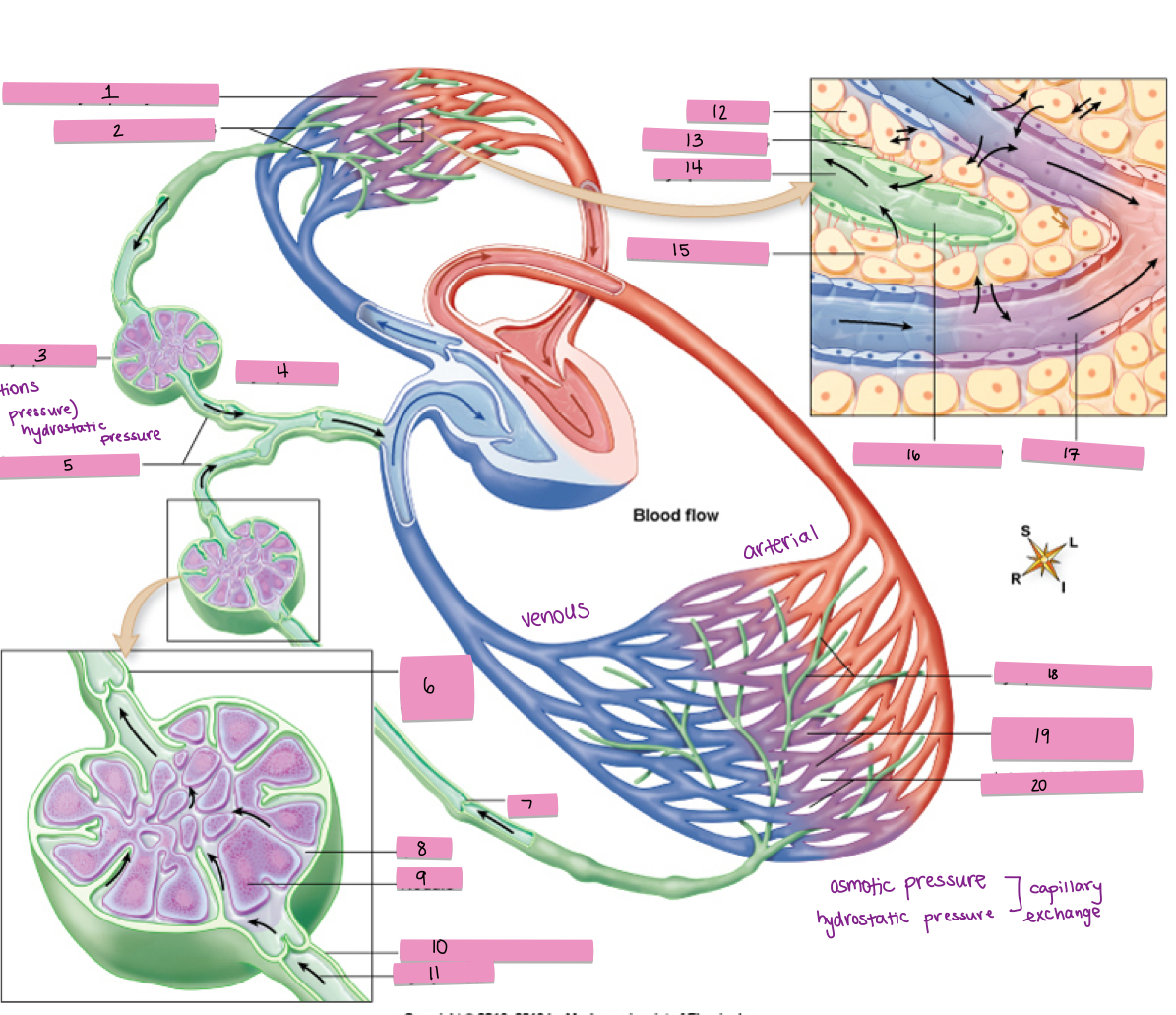
What is #1 pointing to?
pulmonary capillary network
What is #2 pointing to?
lymphatic capillaries
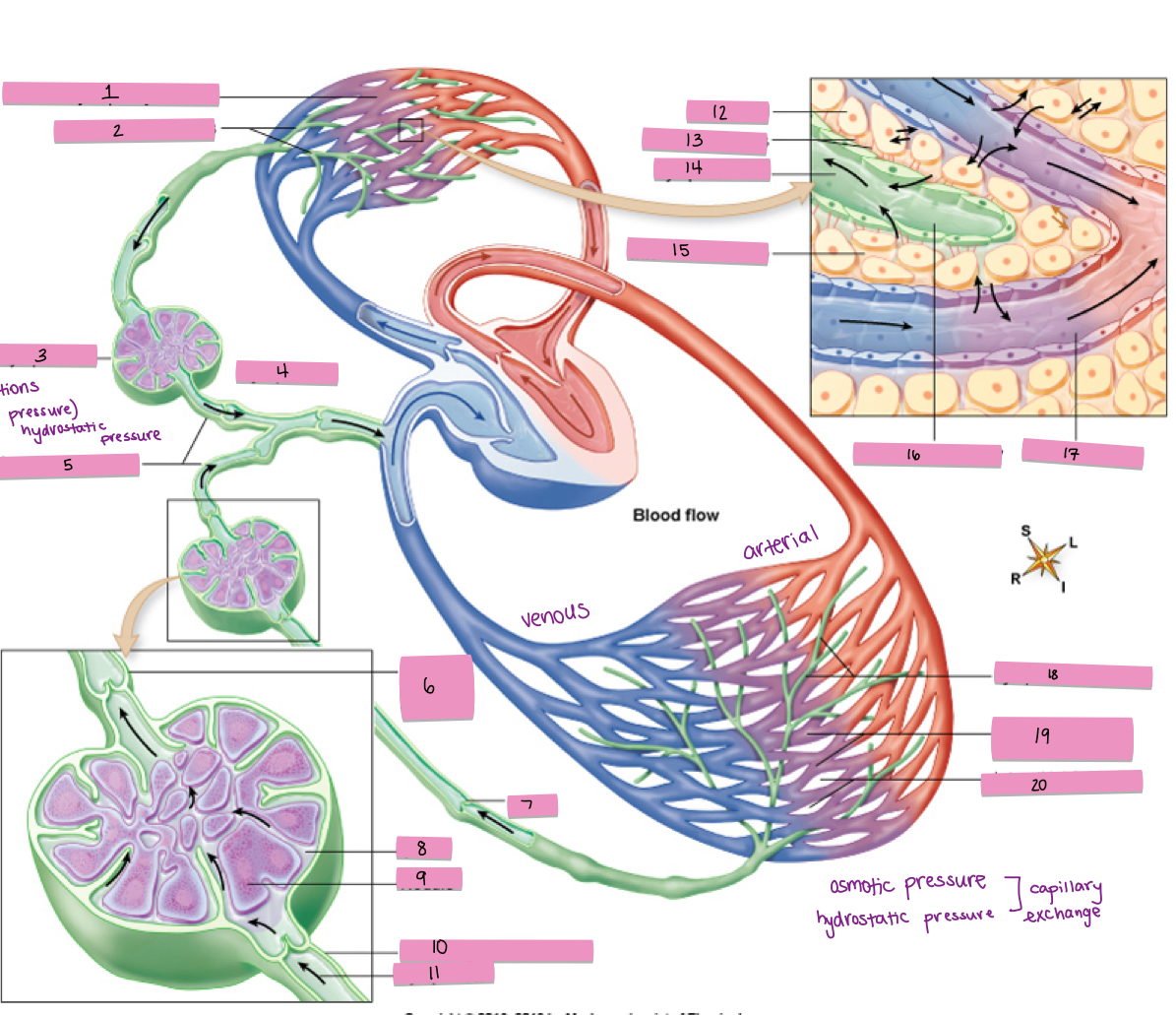
What is #3 pointing to?
lymph node
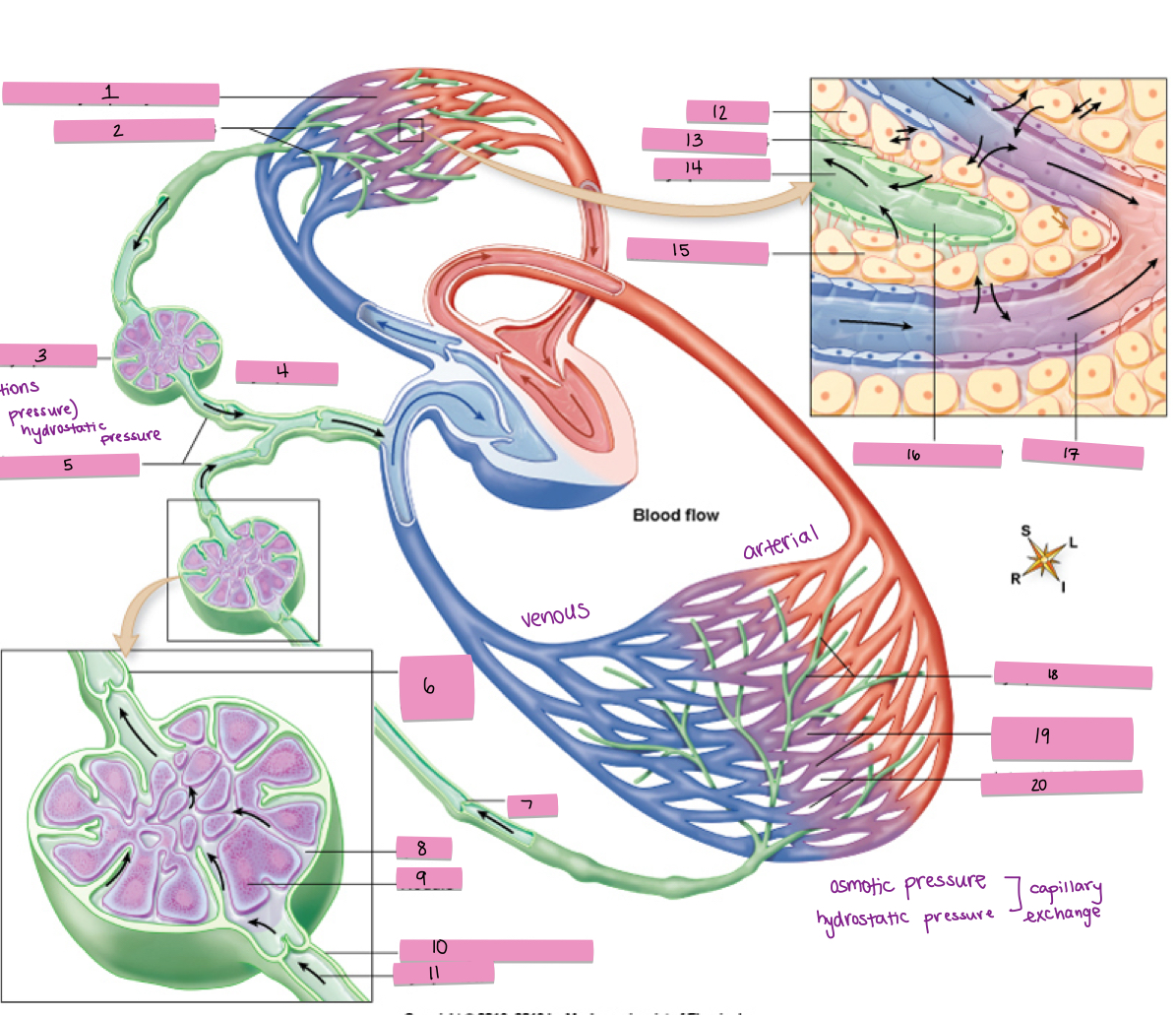
What is #4 pointing to?
lymph flow
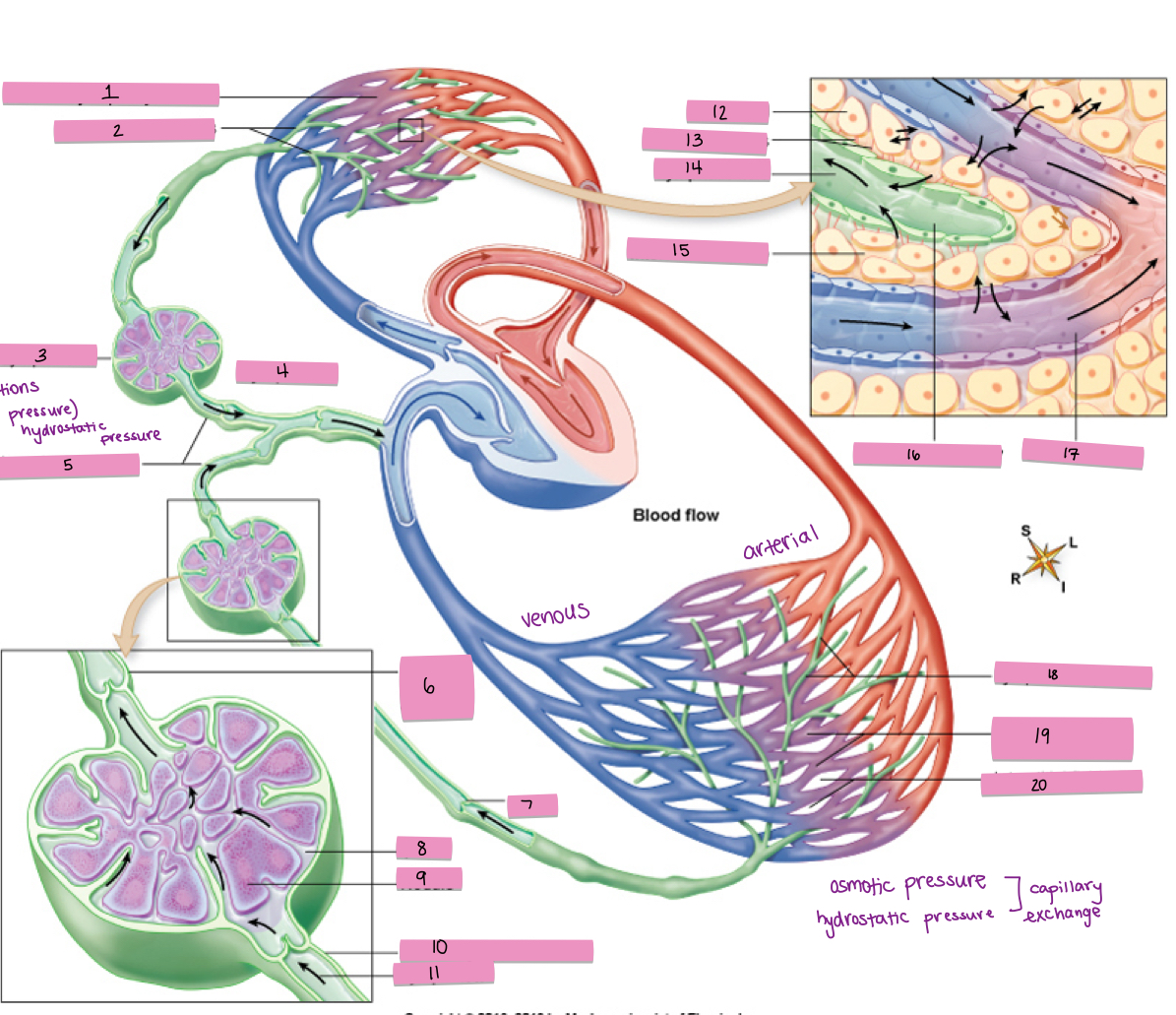
What is #5 pointing to?
lymphatic vessels
What is #6 pointing to?
efferent lymphatic vessel
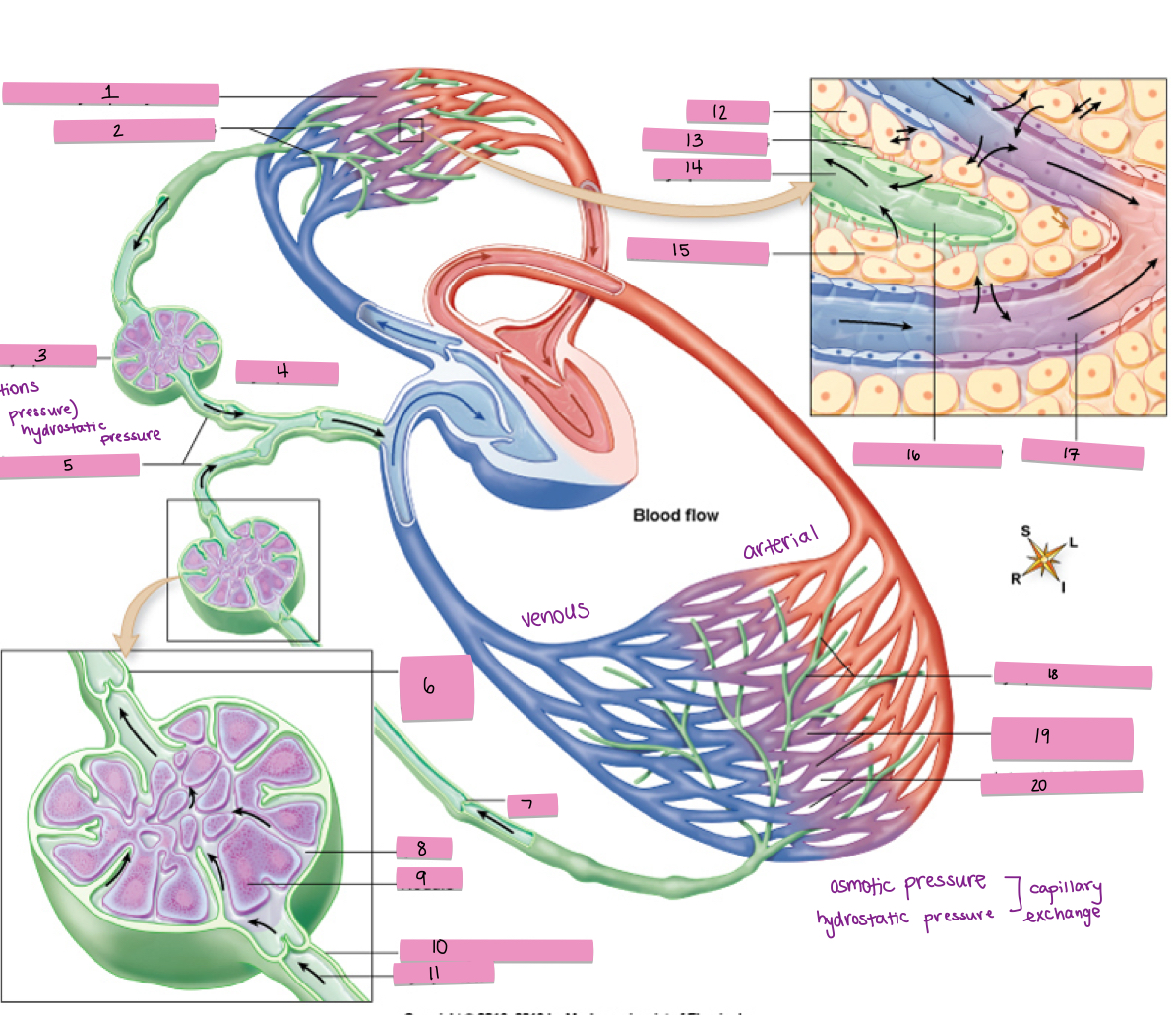
What is #7 pointing to?
valve
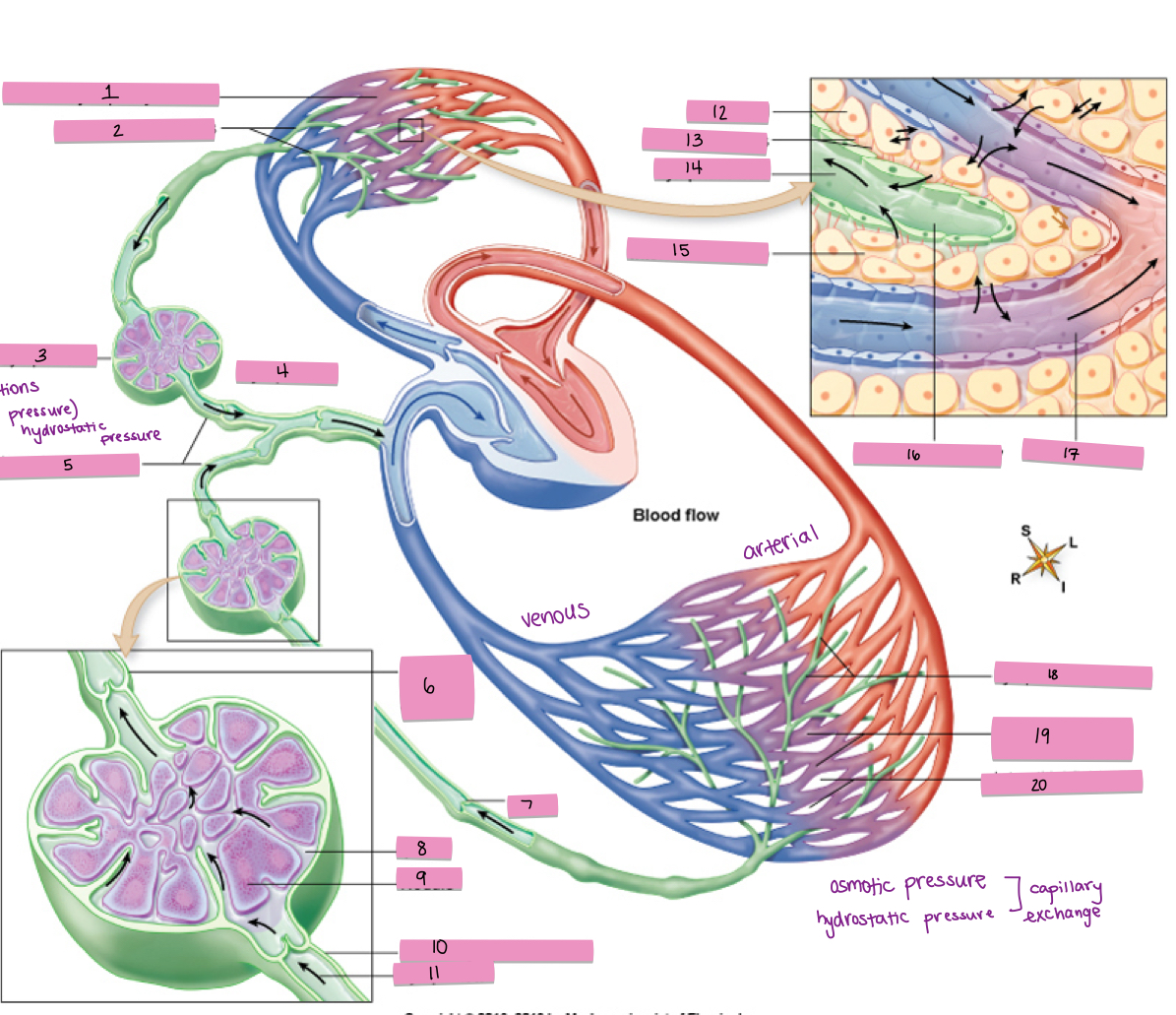
What is #8 pointing to?
sinus
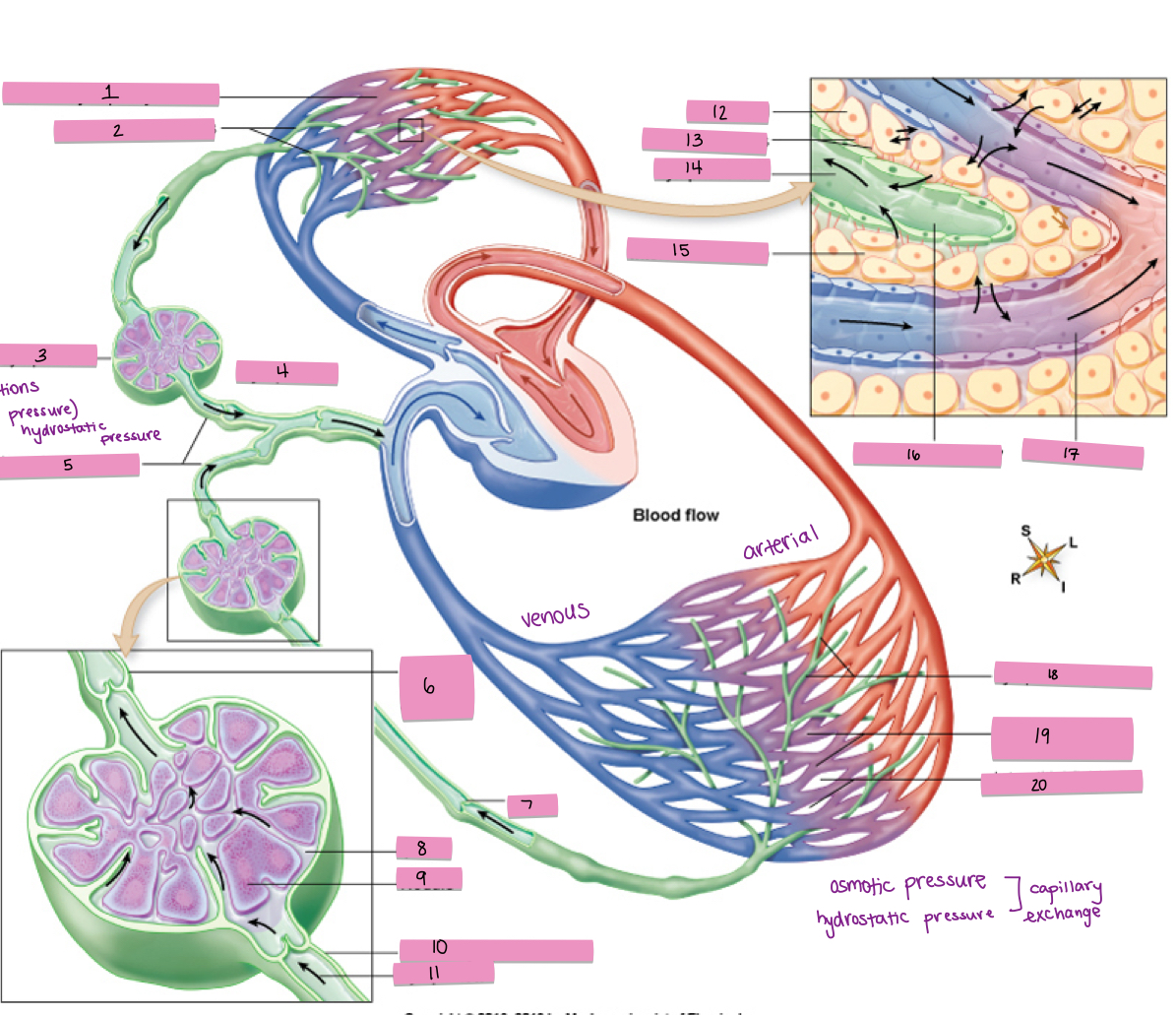
What is #9 pointing to?
nodule
What is #10 pointing to?
afferent lymphatic vessel
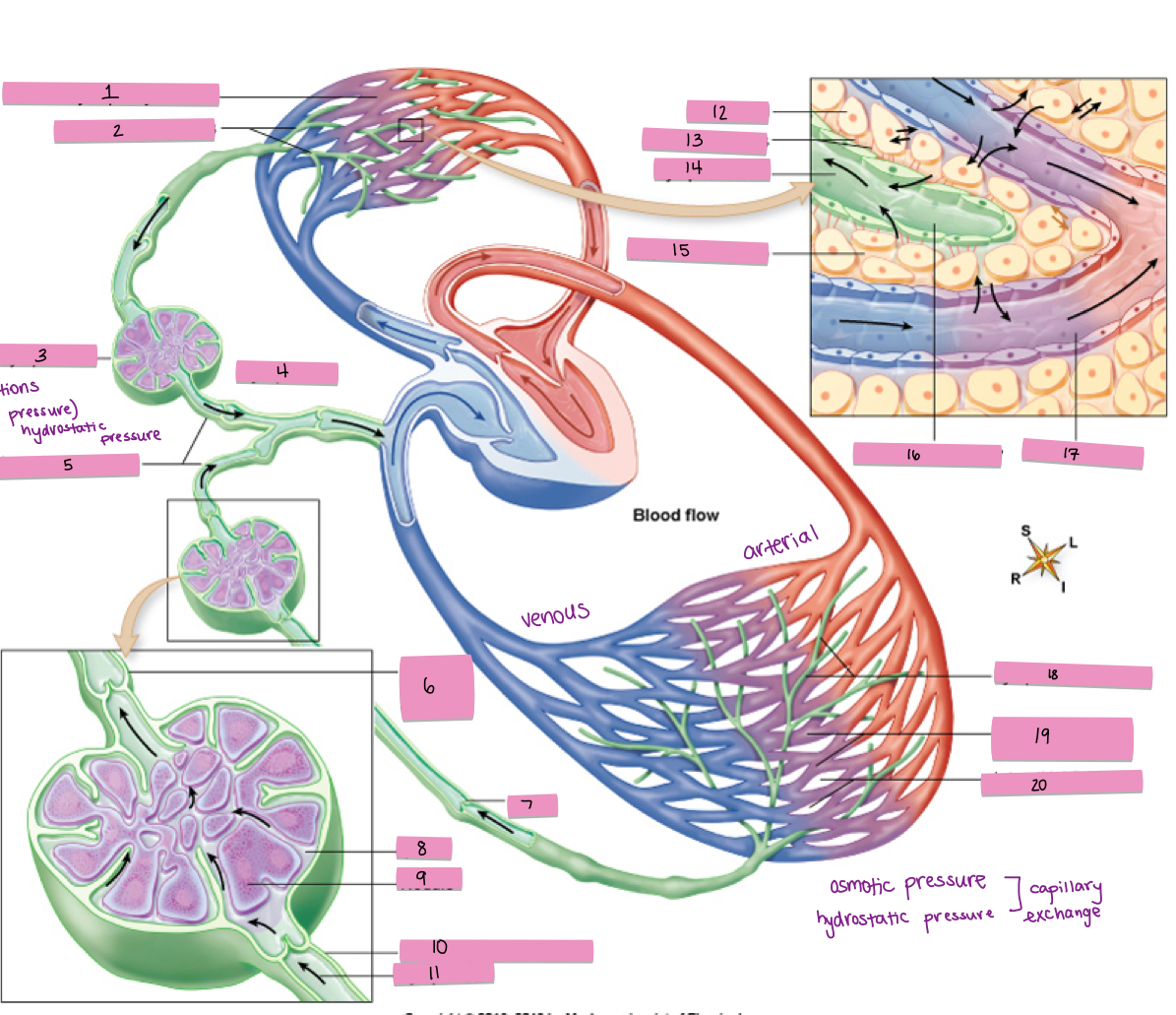
What is #11 pointing to?
lymph flow
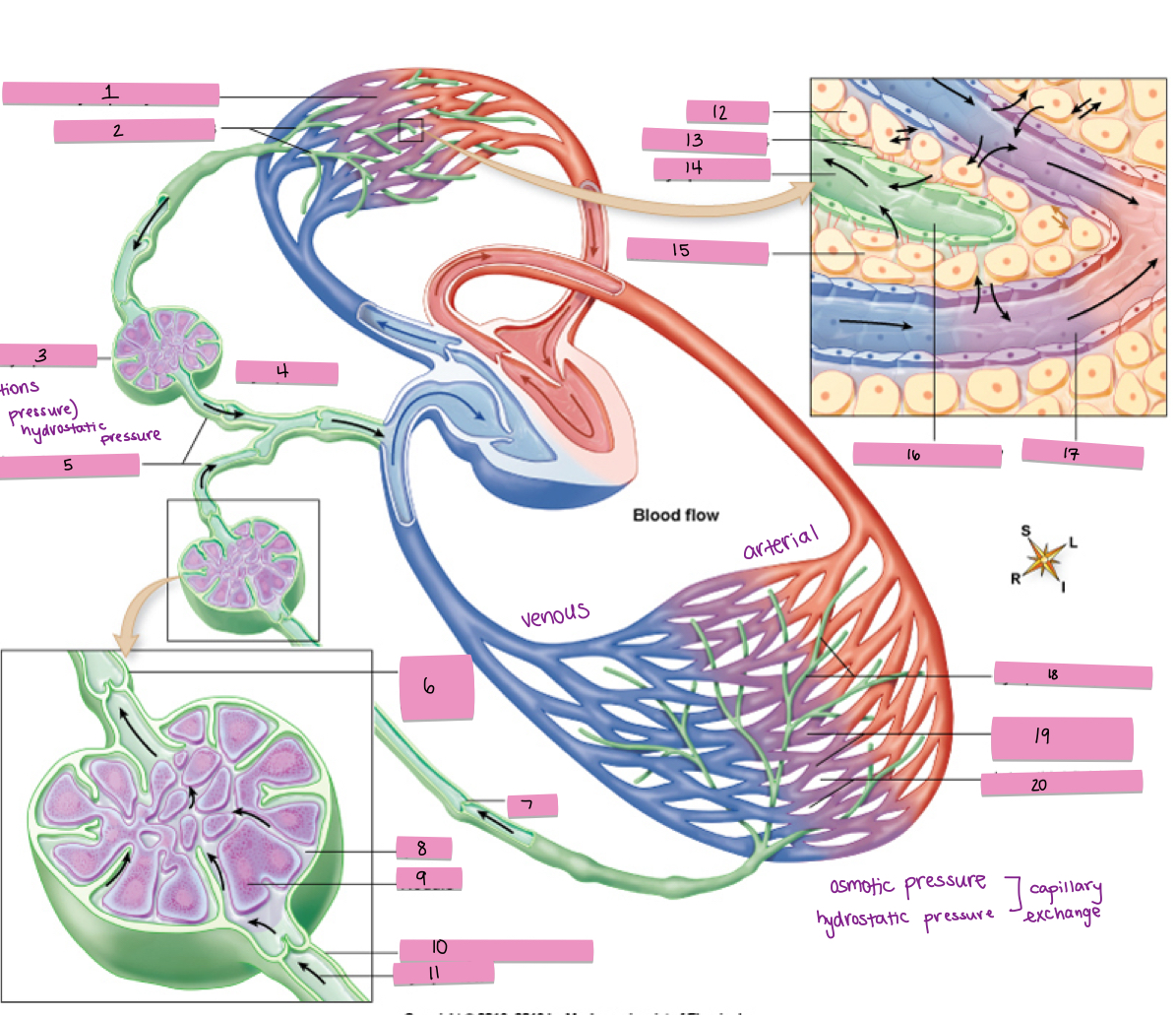
What is #12 pointing to?
tissue cell
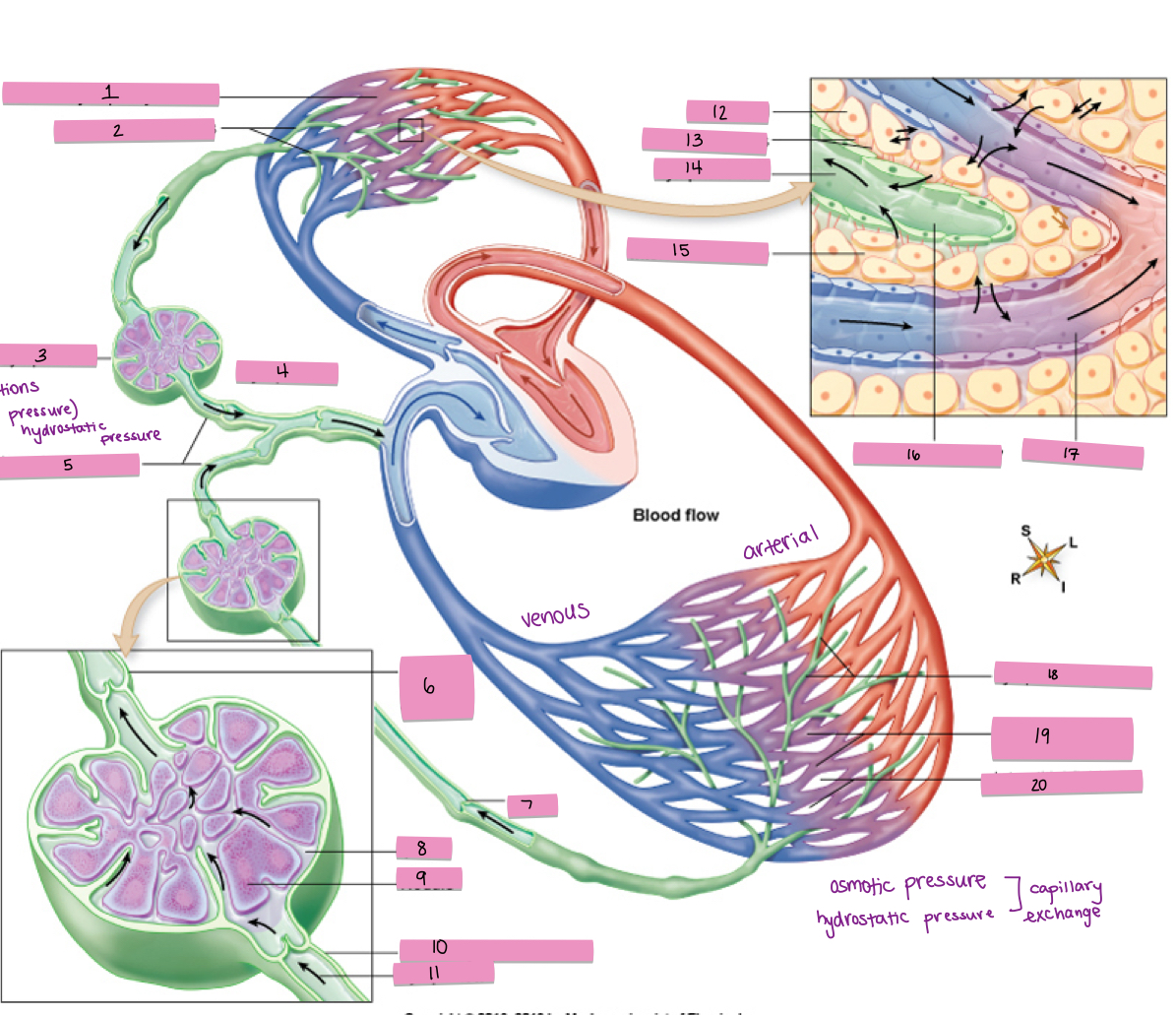
What is #13 pointing to?
anchoring fibers
What is #14 pointing to?
lymphatic fluid
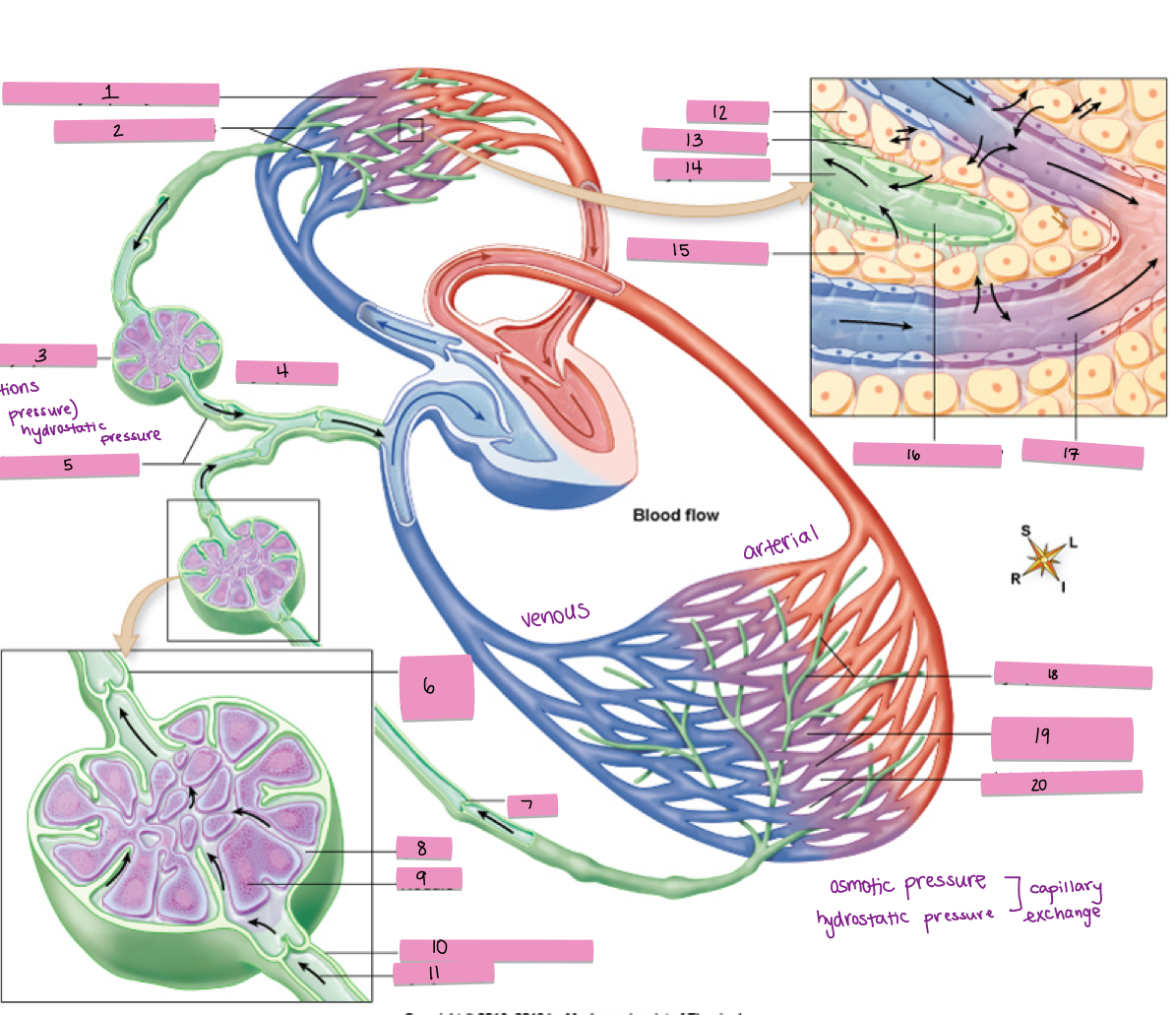
What is #15 pointing to?
interstitial fluid (IF)
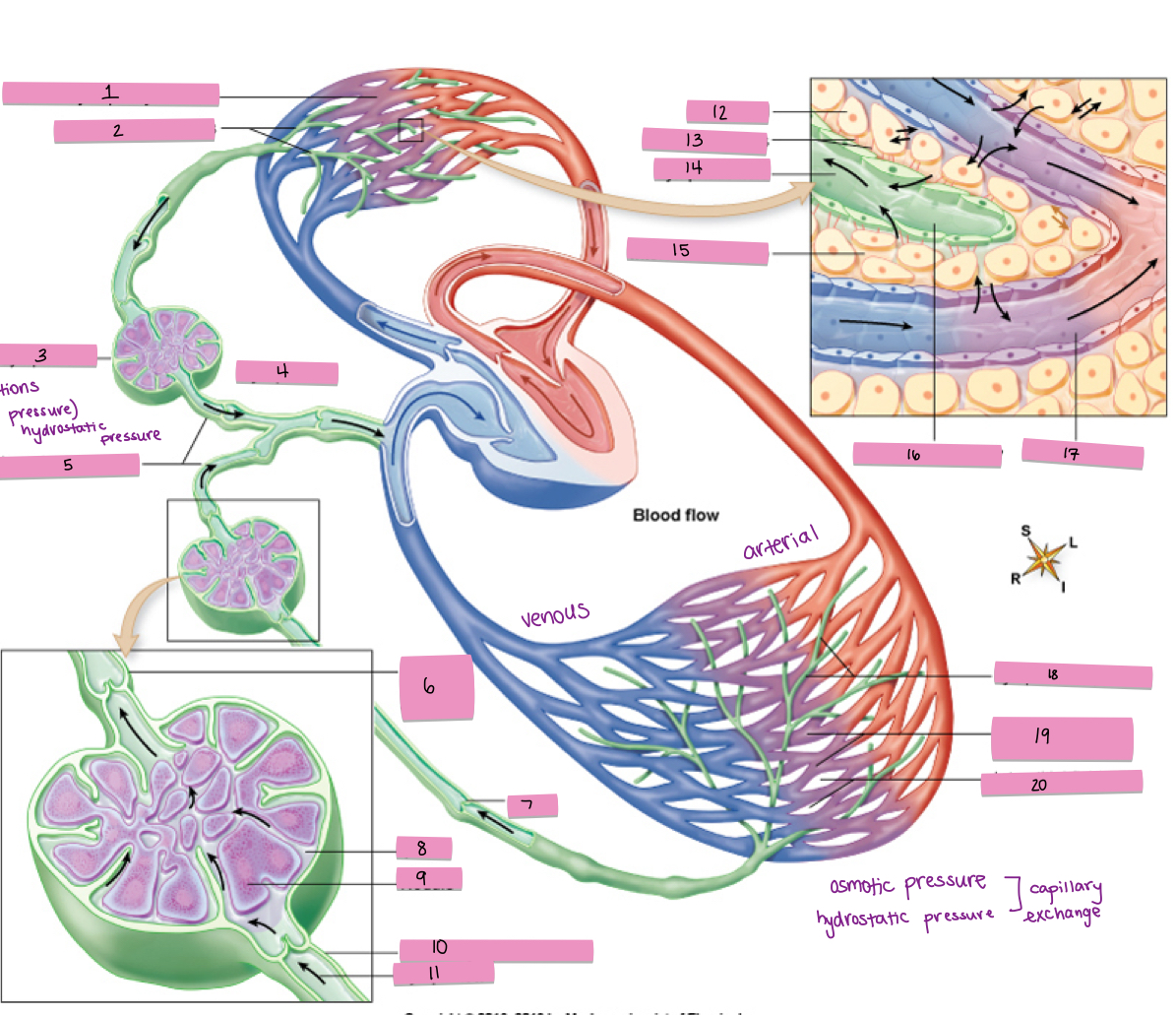
What is #16 pointing to?
lymphatic capillary
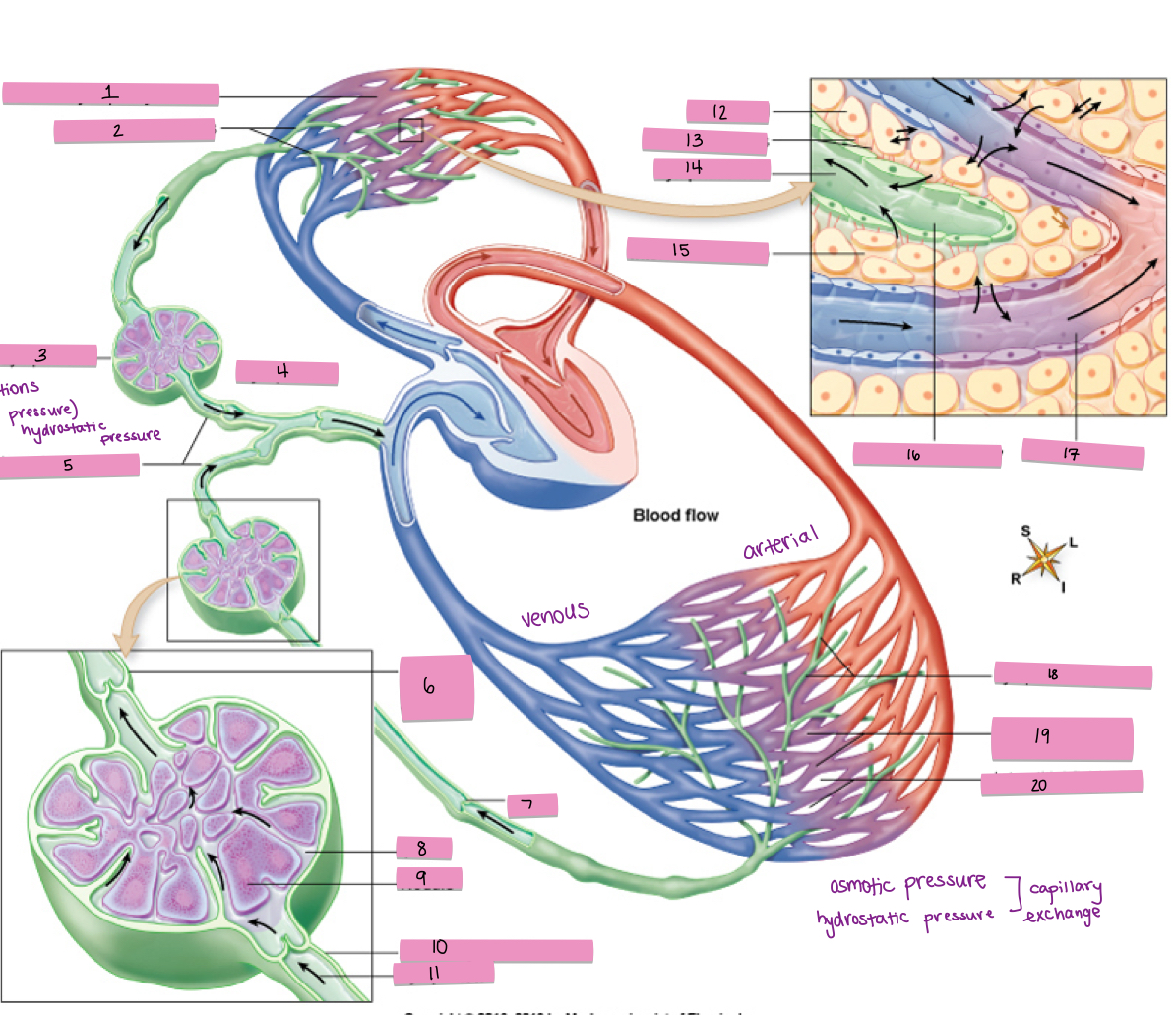
What is #17 pointing to?
blood capillary
What is #18 pointing to?
lymphatic capillaries
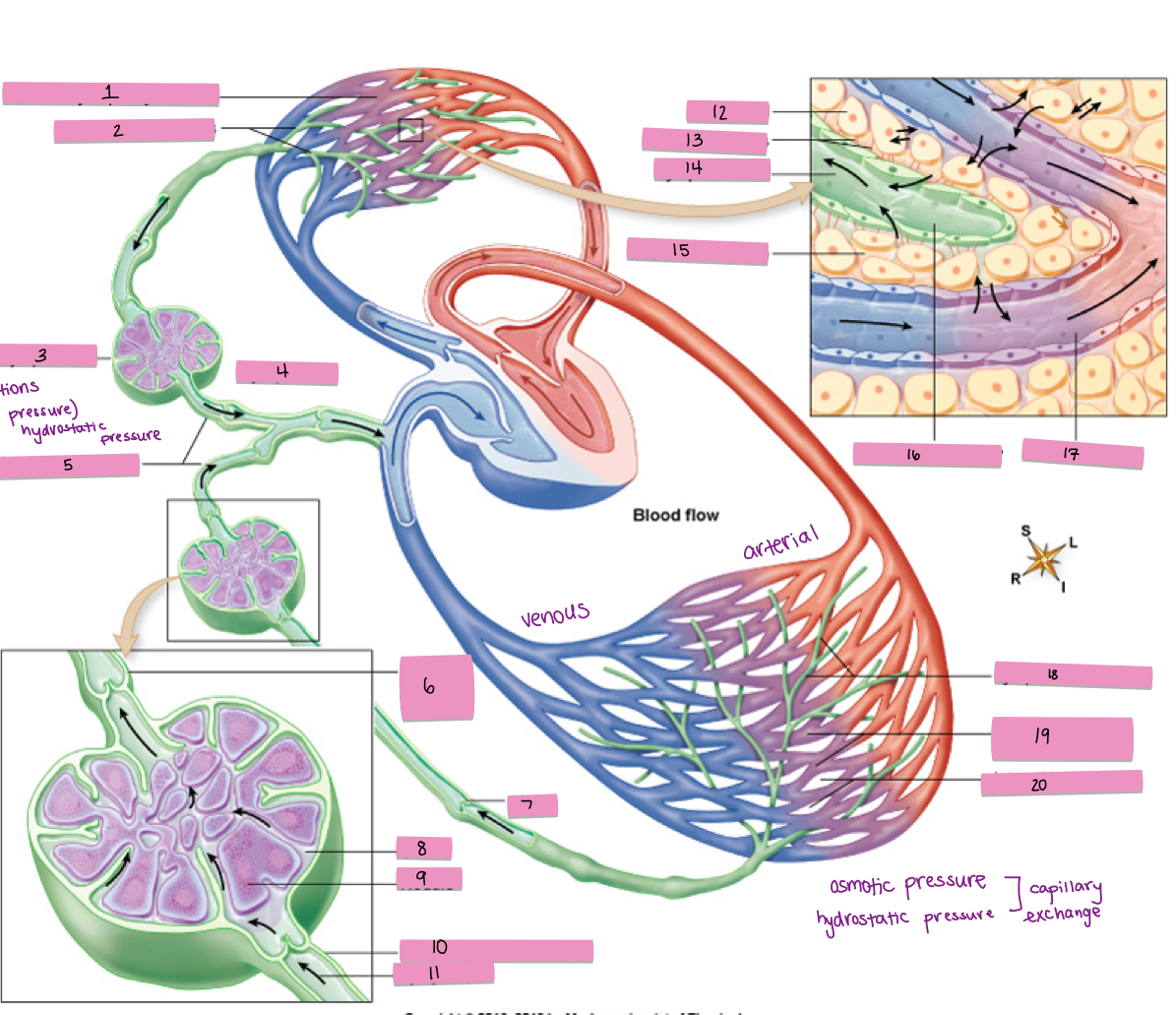
What is #19 pointing to?
systemic capillary network
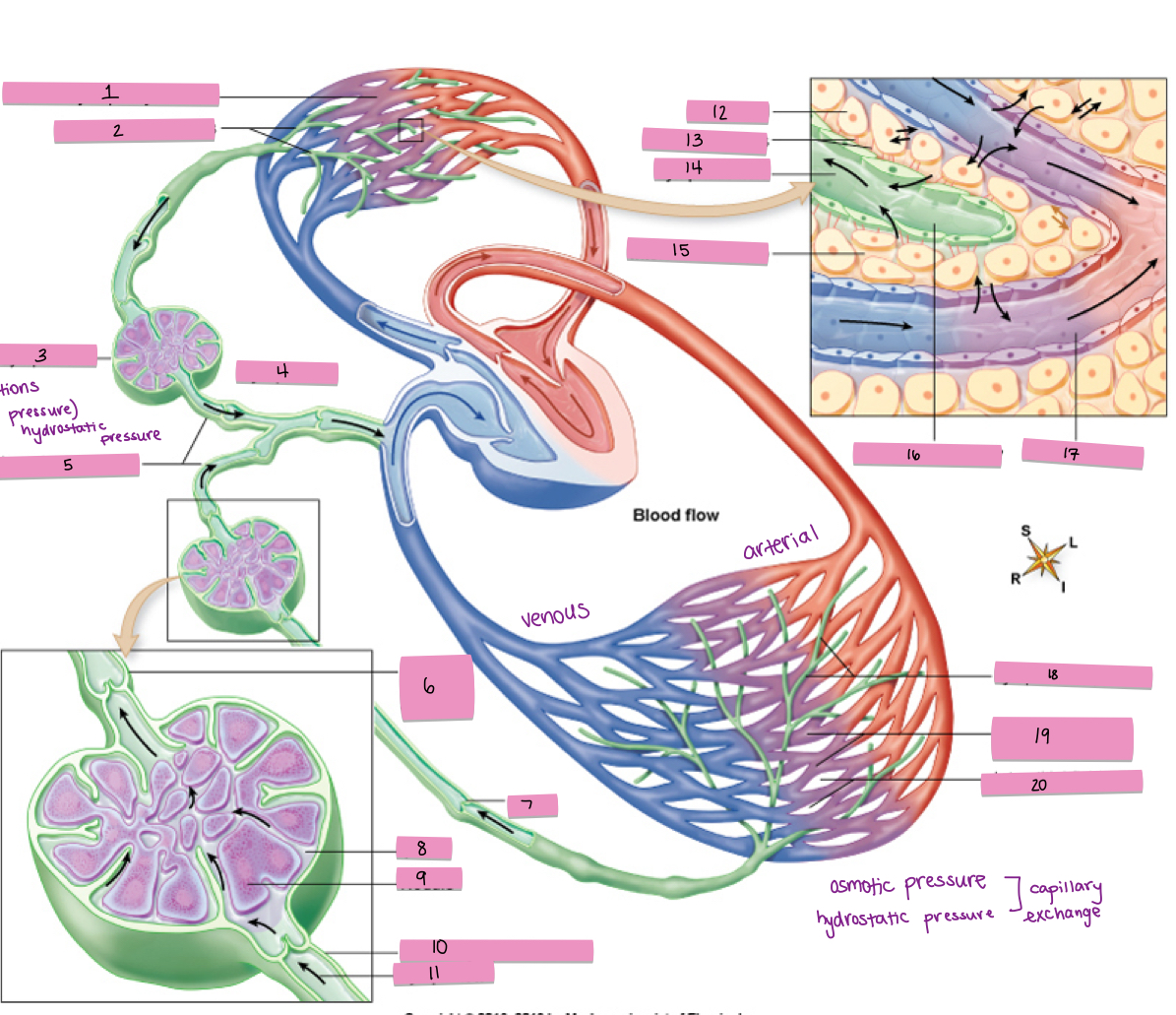
What is #20 pointing to?
interstitial fluid (IF)