Lecture 11 Solid Organ Transplant
1/25
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
26 Terms
Autografts def
transplant from one part of the body to another in the same individual
What is an isograft (also called what)
(also called syngeneic graft) transplant between genetically identical individuals
What is a xenograft?
A transplant between different species, such as from animal to human.
What is an allograft?
A transplant between genetically different individuals of the same species.
What are alloantigens?
specific antigens on the donor organ that the recipient's immune system identifies as "foreign," triggering rejection
antibodies and T cell that react against the alloantigens are called
alloreactive
The principal alloantigens are
proteins of the MHC/HLA class
LMN blood typing system
When a graft is transplanted for the first time, it is referred to as a and may be rejected within
primary graft
rejected within 14 days
When another graft from the same donor is transplanted the second time or more times, then the graft is said to be a what and rejected when?
secondary graft
rejected within 5-6 days
Hyperacute rejection timing
within minutes to hours following the transplant
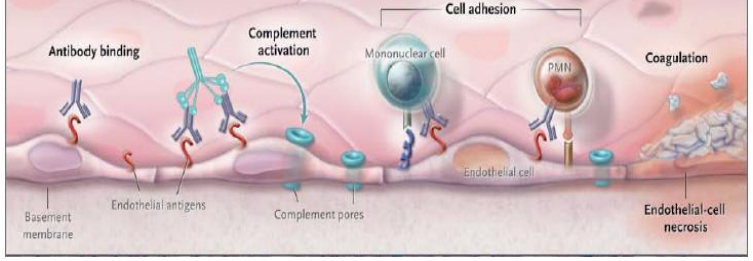
Hyperacute rejection involves antibodies such as ___ and bind to where
IgM antibodies
bind to the graft vascular endothelium immediately after transplant
For hyperacute rejection, the antibodies bind to antigen on the graft and activate what system resulting in what? (think of blood)
Results in what? (overall what happens to transplant?)
complement system and clotting system
leading to necrosis and failure
Accelerated organ rejection involves what other cells?
A rejection caused by both antibodies and T cells that is difficult to treat .
Acute Rejection: timing and is mediated through what cells?
Occurs days to weeks post-transplant and is mediated through T cells and antibodies specific to alloantigens in the graft
Chronic Rejection: timing
occurs months to years post-transplant
Chronic Rejection is clinically seen as
narrowing of the graft blood vessels
inflammation + fibrosis of the transplant
Narrowing of the graft blood vessels happens during what rejection and is also called
graft arteriosclerosis
Which rejection is usually the target of immunosuppressive therapy that we covered?
chronic rejection
Rejection is caused by the immune system recognizing the graft as foreign. The specific antigens targeted are called
alloantigens
The principal alloantigens are proteins of the
major histocompatibility complex (MHC)
HLA
What is Tissue Typing?
Matching HLA antigens on leukocytes between the donor and recipient is a strategy used to prevent incompatibility-based rejection
Why use Tissue Typing?
MHC/HLA are the principal alloantigens that must be matched between donor and recipient to minimize the risk of transplant rejection.
acute rejection example
CD8+ CTLs directly destroying graft cells or CD4+ T cells secreting cytokines to induce inflammation.
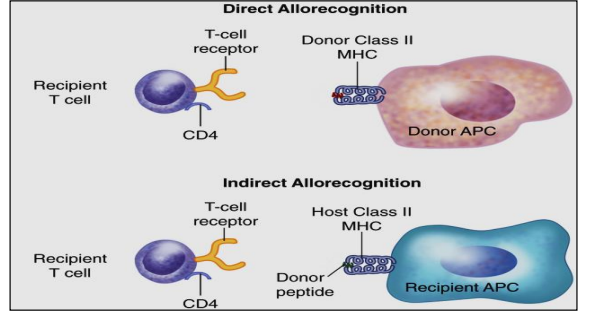
What is the Direct Pathway of Allorecognition
DONOR antigen presenting cells (APCs) migrate out of allograft tissue and present DONOR antigen through donor APC surface MHC-II molecules to the recipient’s CD4+ T cells (donor-recipient).
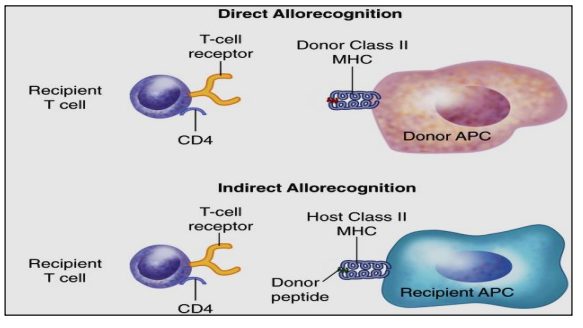
What is the indirect pathway of Allorecognition?
RECIPIENT’s APCs migrate into allograft (transplanted) tissue and phagocytize donor antigen.
These recipient APCs display DONOR antigen to recipient T cells (recipient-recipient). This is a more important long-term mechanism that may cause rejection to occur over months to years.
Three phase of immunosuppressive therapy
Induction, Maintenance, and anti-rejection phase