CA2: Voice disorders
1/73
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
74 Terms
Voice disorder (dysphonia)
voice characterised by an abnormality of pitch, volume, resonance and/ or quality that is inappropriate for the age, gender, or culture of the speaker.
Whats dysphonia?
A change in voice quality
Whats aphonia?
total loss or absence of voice
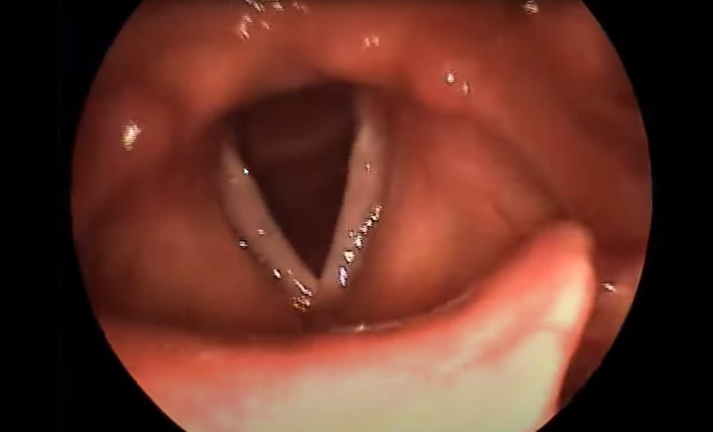
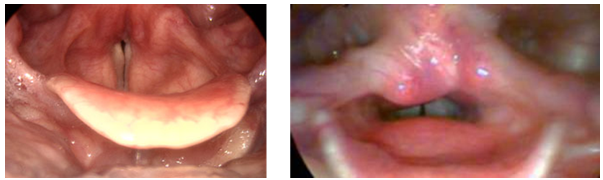
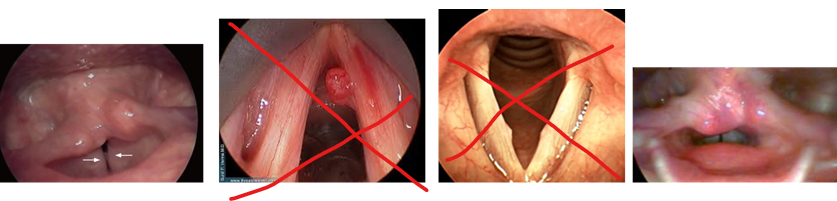
Anything wrong with this?
Normal larynx (not voicing)
pearly white moist vocal folds

What is this?
Muscle tension dysphonia – Too much muscle tension when voicing, you wont see a good view of vocal folds. Tissues are a bit pink or red so patient could report some soreness in throat. Arytenoids may look puffy. Not to be confused with supra glottic squeeze (compensatory muscle tension)
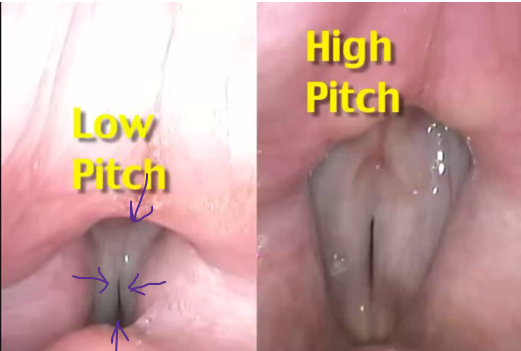
Whats this?
Supraglottic squeeze - muscles coming in from top, bottom and sides
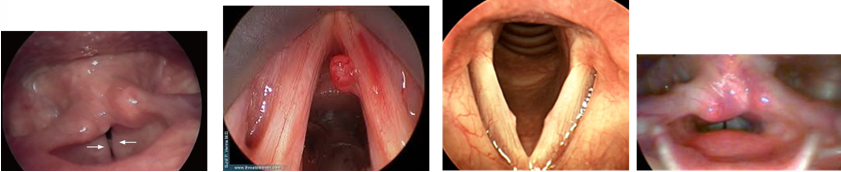
What up with this?
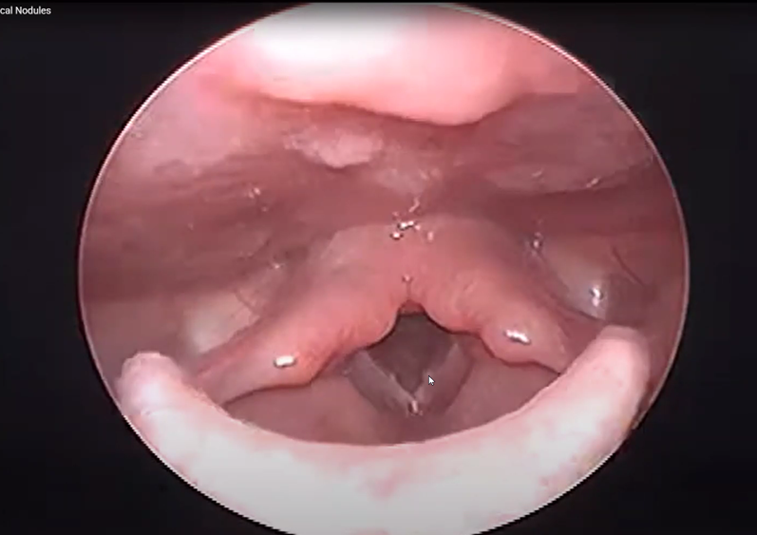
vocal nodules
Sounds very hoarse. Always bilateral – on both folds.
If you stop vocal abuse, the nodules can settle. If you carry on it gets harder and harder, nodules can start off soft like a starter blister.
Always same area - 1/3 up vocal chord
Whats up with this?
vocal fold palsy
Paralysis of vocal chord, vocal chord may be in fixed position unable to move. Will see asymmetry of vocal folds and arytenoids. Arytenoid may lose tone and flop over, obstructing larynx and causing problem with airway/ breathing. Little vocal fold vibration.
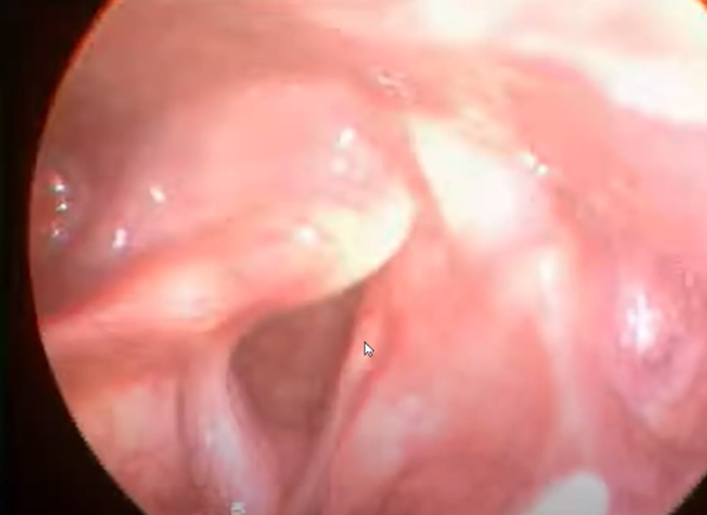
Whats up with this?

Reinkes edema
Social smokers get it more than heavy smokers, floppy sacs of fluid on vocal folds, need to get removed in surgery.
What does stroboscopy involve?
• Vocal folds vibrate too quickly for the naked eye to see the vibrations
• Flashes of light from the stroboscope are synchronised to the frequency of vocal fold vibration, but occur with a slight time delay.
• The viewer’s brain interprets the series of images of the vocal folds at different points in the vibratory cycle as movement.
• The result is that the vocal folds appear to be moving in ‘slow motion’ and we can see the detail of the vibratory wave.

What are PROMs?
Patient reported outcome measures
• Voice handicap index (VHI)
• VHI-10
• Voice symptoms scale (VoiSS)
• Voice related quality of life measure (V-RQOL)
• Voice activity and participation profile (VAPP)
• Vocal tract discomfort scale (VTD)
How to sample someones voice?
• Conversation
• Reading (standard passage – e.g. Rainbow Passage/ Arthur the Rat – available on Moodle)
• Monologue (eg. What did you do yesterday? Tell me about your last holiday. Tell me about your journey here today.)
• S:Z ratio (Eckel and Boone, 1981) measures the comparative duration of sustained s and z phonemes. Should hols and z sound for 15 – 20 seconds (s is voiceless, z is voice sound). Can tell us about breath support
• Maximum phonation time – vowels (/a/, /i/, /u/) (should be ~15-20 seconds)
• Pitch glides (top to bottom, bottom to top, high to low pitch, how is their range? Can they control their pitch)
• Counting 1-5 increasing in loudness
• Vegetative sounds (eg. cough, throat clear, laugh, hmm, uh huh)
• NB confidentiality guidelines for audio recording
What is perceptual analysis?
Subjective judgment about the sound of the voice, what words might you use to describe a voice? Clients may not be familiar with SLT terminology
Perceptual assessments of voice on Moodle: Oates & Russell (1998) and CAPE-V (2006)
What are the categories in GRBAS perceptual rating scale?
• Grade – overall severity of voice change /disorder
• Roughness – irregularity in vocal fold vibration
• Breathiness – air escape between vocal folds
• Asthenia – weakness, lack of power
• Strain – related to excessive muscle tension / effort
Apart from GRBAS, what are other aspects of voice quality? PVDVVTNR
• Pitch – too high/too low
• Volume – too loud/too quiet
• Diplophonia - double pitch phonation
• Vocal Fry / Glottal Fry
• Vocal stability
• Tremor
• Nasality – hypo/hypernasality
• Resonance – chest/head/nasal
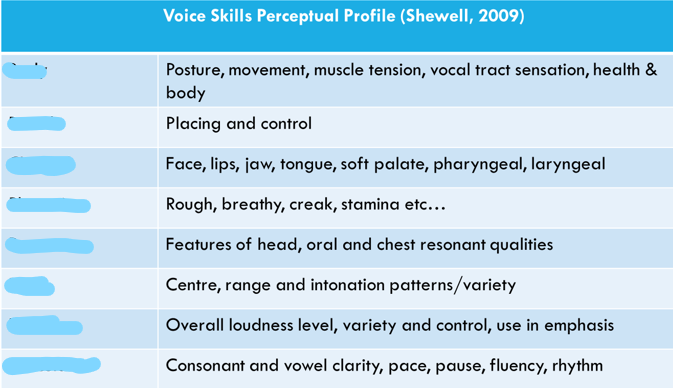
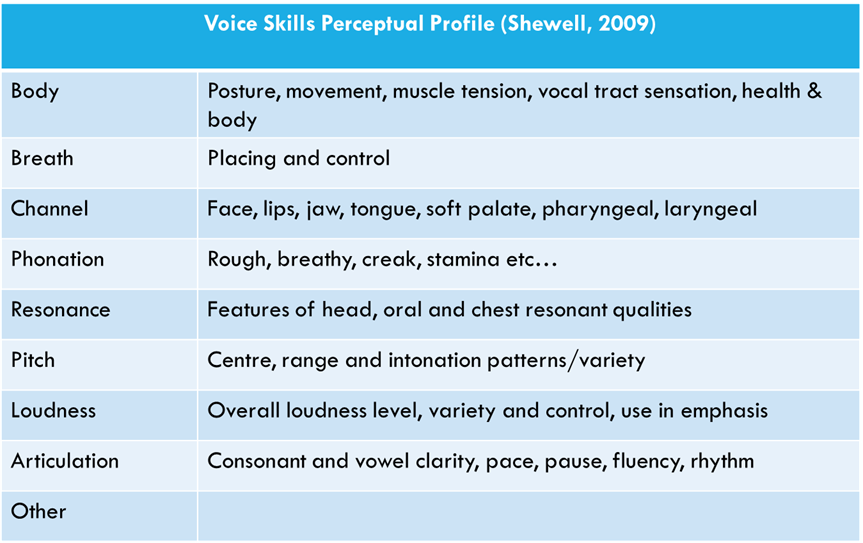
Regarding observational assessments, what aspects of voice quality do these descriptions describe?
What does acoustic analysis look at? FAJSH
• Fundamental frequency (pitch)
• Amplitude (loudness)
• Jitter (variation in fundamental frequency)
• Shimmer (variation in amplitude)
• Harmonics-to-noise ratio
These are all objective measurements
What are the resonating chambers?
• Resonating chambers are: larynx, pharynx, oral cavity, nasal cavity.
• You are able to divert more or less air into these, and manipulate the shape or intensity of some of these vibratory chambers
• The chest also vibrates when phonating (more in men than women)
Factors impacting voice care/hygiene?
Hydration, reflux, breathing
Why is hydration important for vocal care/hygiene?
• Uppermost layer of the vocal folds is a mucosal epithelium
• Vocal folds require lubrication to produce a smooth mucosal wave
• Keeps mucous and secretions thinner and easier to clear; reducing risk of throat clearing
• Biochemical and physical protection against pathogens and particles
What is indirect or systemic hydration in voice care/ hygiene?
Based on systemic hydration, as liquids do not pass over the vocal folds when swallowed
Avoidance/reduction of caffeine (inc coffee, tea, cola)
Recommendations are 2L water per day for females, and 2.5L for males
More if any additional dehydrating factors (e.g. medication)
What is direct hydration in voice care/ hygiene?
Steam inhalation – clean steam (no astringents!) as moist gases pass over the vfs during inhalation
May help to soothe and relax tense musculature
May help with focus on breathing
May provide an opportunity for voice rest during a busy day (especially for professional voice users such as teachers)
Visual strategy that may help in a busy environment to signal voice rest to others
‘old school’ bowl, hot water and towel method;
‘new-fangled’ portable steamers;

What can increase atmospheric hydration?
Humidifiers, bowls of water by radiator, open windows…
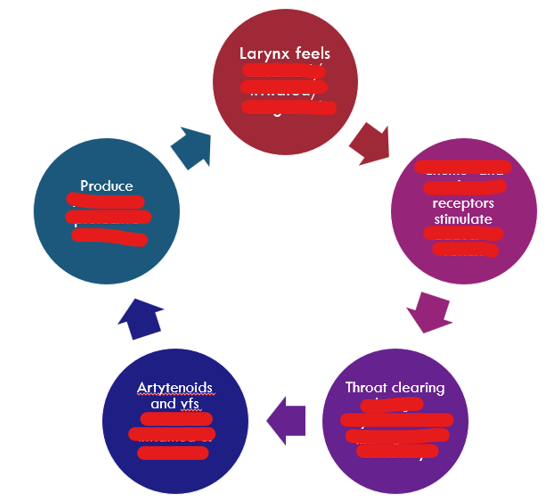
Why is throat clearing bad? Follow the cycle
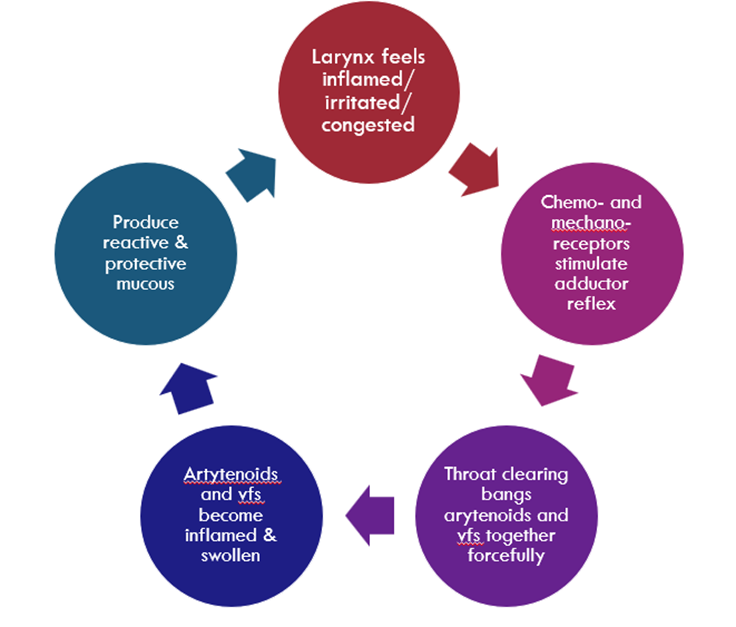
How to avoid throat clearing cycle?
• Sip water
• Hard swallow
• Huff/ hull
• Quick, short inhalations through nose
• Inhale through nose and exhale through pursed lips
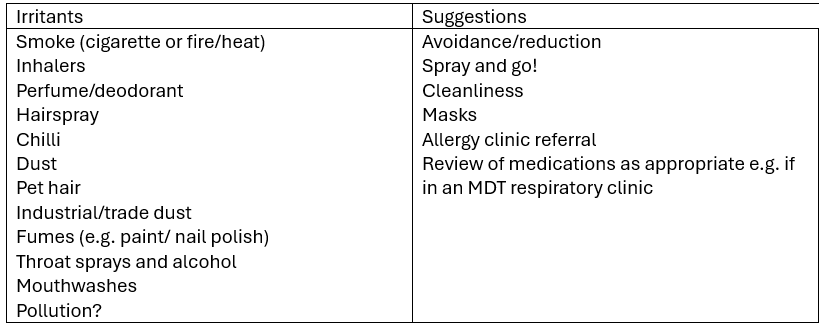
Irritants and suggestions for throat clearing?
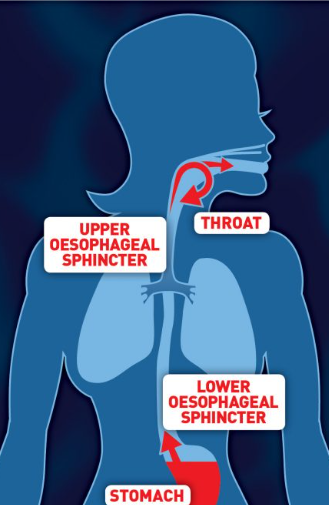
What is reflux in regards to voice care/ hygiene? 2 types of reflux
• Gastro-oesophageal reflux (GORD)
• Laryngo-pharyngeal reflux (LPR)
• Stomach contents: acid, bile and pepsin
• GORD can irritate oesophageal lining and can lead to Barrett’s oesophagus. Dysfunction of lower oesophageal sphincter.
• LPR can irritate pharyngeal/laryngeal structures. Dysfunction in upper oesophageal sphincter.
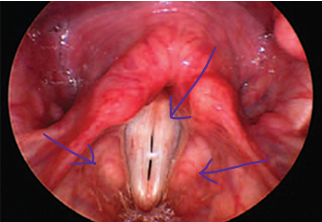
Observable characteristics of reflux on vocal folds?
• Red (erythema) swollen arytenoids (oedema)
• May be a characteristic blueish appearance to the tissues in the interarytenoid space
• Thickening of laryngeal tissues (hypertrophy - increase in muscle size)
• Swollen ventricular folds (+/- ventricular obliteration - loss of normal ventricular structure)
• Granuloma / granulation - small area of chronic inflammation in the body, characterized by a cluster of white blood cells
• Thick, sticky mucous (or perception of)
• Globus pharyngeus - the sensation of having a lump in your throat without any physical obstruction
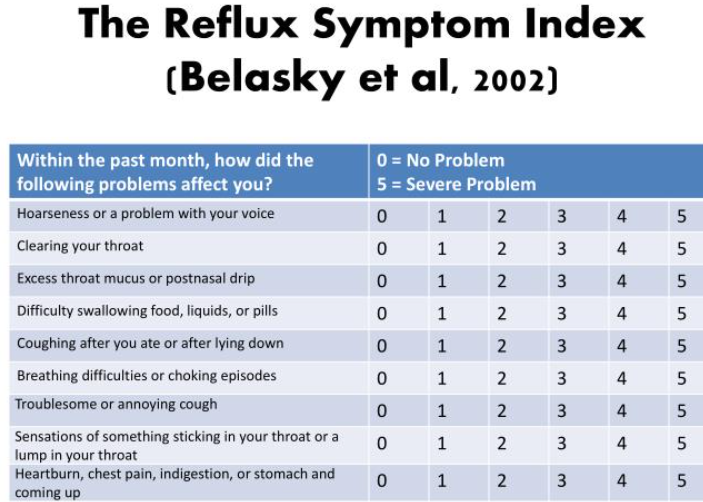
• See Reflux Symptom Index (RSI)
Patient symptoms of reflux?
Management of reflux - PPI and A
• Proton Pump Inhibitors (PPIs – e.g. Omeprazole, Lansoprazole etc), increasingly less popular but reduce production of stomach acid
• Alginate (e.g. Gaviscon Advance) increasingly more popular. Natural compounds derived from seaweed that can help manage reflux symptoms by forming a gel-like barrier on top of stomach acids, preventing them from flowing back into the oesophagus.
Management for acid reflux (not medicinal)
• Diet (esp fatty, processed, spicy, acidic, chocolate) and volume/ timing of food
• Alcohol
• Caffeine
• Smoking
• Weight management and clothing
• Bed raise/left side lying/ inversion
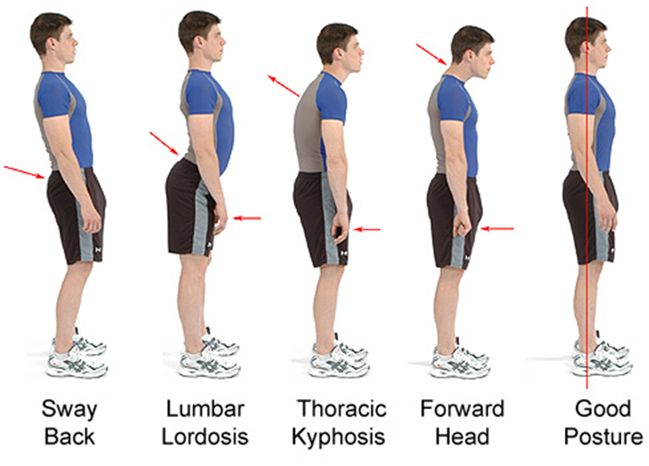
Management for reflux - posture and alignment
• Neutral head position
• Relaxed, aligned shoulders
• Neutral spine (natural curves)
• Tilted pelvis
• Soft knees
• Support through legs and abdomen
Why are cough/cold/throat medications sometimes bad?
They are typically numbing and astringent (a substance that shrinks or constricts body tissue) so you can’t feel the damage you are doing
Upper costal breathing vs diaphragmatic breathing
Upper costal - chest rises, upper lungs fill with air, little/no engagement or inflation of diaphragm and lower lungs, lower ribcage stationary
Diaphragmatic breathing - Chest and shoulders remain still and relaxed, diaphragm contracts and increasing thoracic space, air sucked into lower lungs, lower ribcage expands laterally, anteriorly (& posteriorly to some degree), diaphragm relaxes and thoracic space decreases on exhalation
problems and benefits of upper costal breathing
Problems: disrupts alignment, poor inflation, reduced capacity, limited breath for speech, shoulders tend to rise with chest (tension) and body slumps down and forward on exhalation
Benefits: normal for most people when awake, easier when sitting, maintains ‘desirable’ body shape
problems and benefits of diaphragmatic breathing
Problems: Requires some conscious effort and often training, involves abdomen expanding on inhalation – many people are uncomfortable with this! Intercostal muscles may have lost range/ease of motion with long-term disuse
Benefits: Allows maintenance of good posture, significantly larger breath capacity and therefore support for speech, allows engagement of abdominals to support exhalation
The greater the vocal demand, the more important efficient breathing is to protect the voice
Extending breath beyond introductory work (2 steps, give examples)
Diaphragmatic breathing only (no voice)
· Rest breathing
· Increasing duration
· Focus on long and smooth airflow
· Short bursts/ pulses
· Decreasing intensity
· Increasing intensity
· Waves
Coordinating breathing with phonation (with voice)
• Sigh/conscious exhalation/ stifled yawn etc.
• Voiceless trills
• *Voiced trills
• Voiceless fricatives
• *Voiced fricatives
• *Vowels (monophthongs)
• *Vowels (diphthongs)
• *VC
• *CV
• Extending to words/ phrases/ sentences etc………
NB: this hierarchy may need to be adjusted if the client has phonation issues such as muscle tension and requires work on this
How are voice disorders classified (McGlashans’ categories)? 4
Inflammation, neoplastic/ structural, muscle tension imbalance, neuromuscular
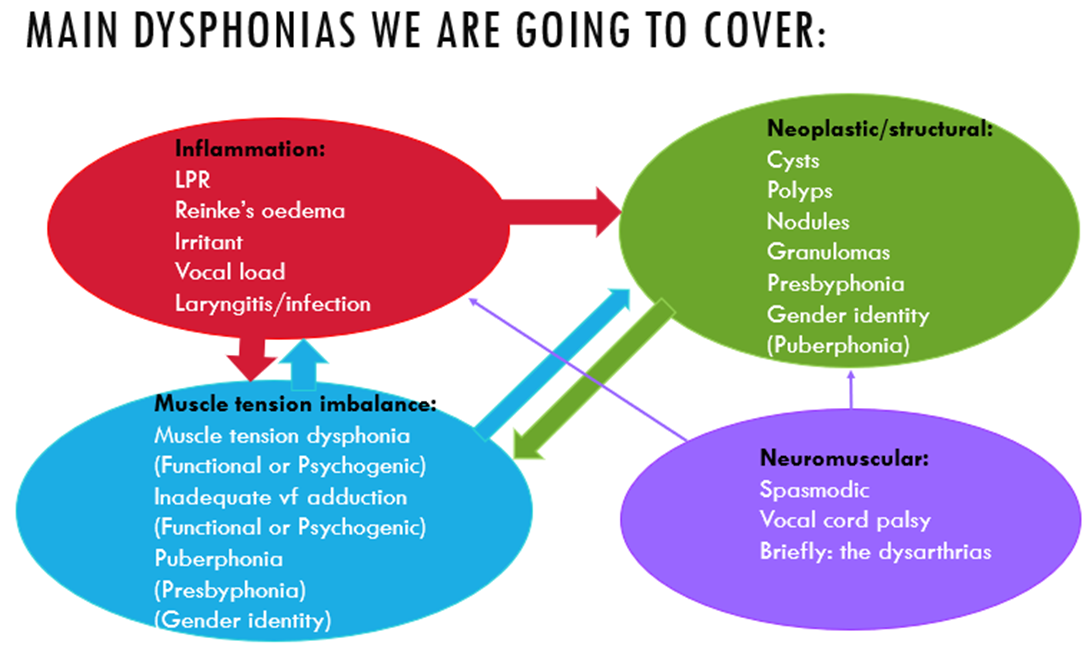
How can muscle tension imbalance be further subdivided?
Functional and psychogenic
THEN functional into…
Hyperfunctional, normal, Hypofunctional

Features of hyperfunctional. Discuss vocal folds and describe voice
Vocal folds:
Over-adduction
A-P compression
Ventricular involvement
Arytenoid squeeze Cricothyroid or hypothyroid tension
Larynx held higher than natural position
Voice is:
Strained, tight
harsh and rough
pitch breaks/ reduced pitch range
voice breaks
squeak
can be aphonic (no voice) or diplophonic (producing 2 pitches at once)
can be breathy (recruitment/ over-adduction of other structures can prevent proper vf vibration)
Features of hypofunctional (muscle tension dysphonia). Describe vocal folds and voice
Vocal folds:
Gap on phonation (without arytenoid squeeze)
poor adduction
generalised reduced recruitment of relevant muscles
bowing
Voice:
Weak
breathy
quiet
rough
pitch breaks/ reduced pitch range
voice breaks
can be aphonic (no voice) or diplophonic (2 pitches at same time)
can be implications for swallowing
What McGlashan categories does hyper and hypofunctional voice disorders fall into?
Inflammatory
Structural
Neuromuscular
Muscle tension dysphonia
What therapy techniques span both hyper and hypofunctional voice disorders?
Voice care/ hygiene
Diaphragmatic breathing
Common hyperfunctional voice disorders
Muscle tension dysphonia (muscle tension imbalance)
Polyps (neoplastic/ structural)
Nodules (neoplastic, structural)
Hyperfunctional voice disorder: Polyps (neoplastic/ structural)
• Growth, usually on one of the vocal folds (unilateral)
• Usually soft and fluid-filled, like a blister
• Usually as a result of vocal misuse and/or vocal load
• There may be a contact lesion on the other vocal fold (from rubbing against the polyp)
• Usually presents weak voice, hoarse (rough), may have voice or pitch breaks, problems with pitch and volume, vocal fatigue, weak (asthenic) voice, may be breathy due to air escape where VFs cannot meet properly
• Perceptual assessment often reveals limited breath support, poor voicing/projection technique
• Sometimes visible discomfort e.g. hard swallow/throat clear/cough/touching neck post voicing
• Including a projection task is very useful in perceptual assessment
• Usually treated with microphonosurgery

Hyperfunctional voice disorder: Nodules (neoplastic/ structural)
• Occur bilaterally (on both vocal folds) in a symmetrical position
• Usually occur at the anterior 1/3 point of the true vocal folds (midline of the vibratory portion of the folds)
• Start small and soft; get bigger and harder over time if vocal behaviour not treated
• Usually a result of voice misuse and/or vocal load; specifically forceful contact of the vocal folds. The presence of the nodules can perpetuate this, as more effort is required to initiate and sustain voicing
• Usually presents with a voice that is weak, hoarse (rough), may have voice or pitch breaks, problems with pitch and volume, voice often worse at higher pitch, vocal fatigue, weak (aesthenic) voice, can be some pain after speaking
• Perceptual assessment often reveals limited breath support, hard attack and poor voicing technique
• Sometimes visible discomfort e.g. hard swallow/throat clear/cough/touching neck post voicing)
• Including a projection task is very useful in perceptual assessment
• Rarely seen in males (but not unheard of)
• Very common in professional voice users, loud individuals and party-goers
• May require microphonosurgery if hardened

Hyperfunctional voice disorder: Muscle tension dysphonia (muscle tension imbalance)
Muscle tension can occur as either a primary or secondary phenomenon.
E.g., can occur on its own, or someone may develop a muscle tension dysphonia to compensate for laryngitis, nodules, etc. Often the pattern of tense voicing becomes learned, and even once the primary cause (e.g. laryngitis) has gone, the individual continues to voice in this way.
It is characterised by excessive squeezing, tension or compression on the cartilages and soft tissues within and directly surrounding the larynx.
Common patterns include:
1. Anterior-posterior (AP) compression (top and bottom)
2. Phonation with (or squeeze of) the false (ventricular) vocal cords- ‘plicae ventricularis’
3. Hyper-adducted arytenoids, causing posterior gap
Regarding cause of muscle tension dysphonia (muscle tension imbalance), how can it be categorised?
Functional/ behavioural or psychogenic
Describe psychogenic muscle tension dysphonia (muscle tension imbalance) and cause
Emotional strain, anxiety or trauma manifests in tension in the larynx/neck/shoulders.
Voice:
tight, strained, creaky, effortful, can be rough, voice or pitch breaks, problems with pitch or volume, vocal fatigue, asthenic (weak) voice, pain or discomfort when speaking, tightness in neck/larynx, squeezing sensation, globus sensation.
Perceptual assessment often reveals significant tension in the neck and shoulders, often visible SCMs on phonation, pushing/squeezing/forcing behaviours. May also have visible/audible tension in face, jaw, tongue etc and/or larynx may be held in unnaturally high position.
2 main types:
Conversion (Classical Freudian Hysterical Conversion)
Cognitive Behavioural Conversion
Psychogenic muscle tension dysphonia: Conversion (classical Freudian hysterical conversion) type vs Cognitive Behavioural Conversion
Conversion/ Classical Freudian Hysterical Conversion:
Suppressing traumatic event they are unaware of
Rare and often resistant to voice therapy
Help of psychology/ counselling will maximise likelihood of improvement and is first recommended line of treatment
Cognitive Behavioural Conversion
They know they are suppressing something and know the nature of their stress e.g., divorce
Most common type and responds well to voice therapy.
Name all 4 hyperfunctional voice disorders
Muscle tension dysphonia lateral compression (coming in from the sides)
Polyp
Nodule
Muscle tension dysphonia anterior-posterior compression (top and bottom)
What are the two types of compression that can occur in muscle tension dysphonia?
Muscle tension dysphonia lateral compression (coming in from sides)
Muscle tension dysphonia anterior-posterior compression (top to bottom squeeze)
Principles of therapy for hyperfunctional voice
• Relaxation
• Exercises for the release of constriction and tension
• Semi-occluded vocal tract therapy (SOVT)
Laxvox
• Resonant voice therapy (RVT)
• Soft onset
• (also voice care and diaphragmatic breathing as fundamental underpinnings)
• Need to think about how you move into more speech-like exercises as therapy progresses
Hyperfunctional voice therapy: Semi-occluded vocal tract therapy (SOVT) or LaxVox
Phonating into a tube/straw submerged in water creates back pressure that relieves tension from the vocal folds while engaging the core breath support. Creating pressure above the vocal folds to partially negate the pressure from below, as such voicing becomes easier with better position and shape of vocal folds.
The more tight the voice, the thinner or longer straw you use
The more breathy the voice, the wider or shorter straw you use
Hyperfunctional voice therapy: resonant voice therapy
Improve vocal quality and reduce strain by teaching individuals to produce a voice that resonates forward, enhancing vocal health and efficiency.
Hyperfunctional voice therapy: soft onset
Starting speech with a gentle, soft onset of sound, rather than a sudden or abrupt onset.
Hyper and Hypofunctional voice therapy: diaphragmatic breathing
Using the diaphragm to facilitate expansion of the lungs to improve breath support and strength
What to think about before starting a therapy session
• Hold a mirror up to yourself and your working environment:
• Factors outside the room before the person entered your clinic room today (long queue at the desk, bad traffic, noisy or stressful waiting area, called in on time etc)
• Feeling in the room (lighting, smell, sounds, privacy)
• Seating arrangements (comfort of the seats, formality of the seating)
• Availability and positioning of drinking water, mirror, diagrams etc.
• Think about your own modelling of desirable behaviours:
• Posture and relaxation
• Rate of speech
• Volume of speech
• Quality and tone of your own voice (as professional voice users we should all be carrying out vocal warm-up prior to starting our working day!)
• Taking regular breaks within the session to sip water, resume resting breathing patterns, reflect on each exercise etc.
• Be mindful; calm and unrushed
exercises for a client to relax
• Progressive relaxation/ meditation/mindfulness (body scanning, tighten and soften – lots of great apps or this or can be therapist-led). Often a good starter.
• Shoulder rolls backward/forward
• Shoulder raise and drop down
• Head tilts (ear to shoulder), chin to chest
• Lifting head, as if by a string
• Shoulders back and down
• Inhale bringing arms up, exhale and swoop down
• Self-massage
• Some patients already attend yoga/pilates/ meditation/ Tai Chi etc or may wish to consider something like this
How to get client to release constriction of face
Aim: To reduce habitual tension in articulators and/or larynx
• Chewing (exaggerated)
• Voiceless bilabial or lingual trills
• Facial massage (self)
• Tongue massage of cheeks
• Tongue out sweeping (licking lips)
• Tongue out stretching
• Wow-wow-wow/ meow
How to get client to release constriction of larynx
Aim: To reduce habitual tension in articulators and/or larynx
• Volitional yawn/ yawn-sigh/ supressed yawn
• Laryngeal manipulation or Laryngeal Manual Therapy
Hyperfunctional voice therapy: semi occluded voice tract therapy (SOVT)
Aim: To facilitate healthy VF vibration by equalising supraglottic and subglottic air pressures.
• Translated: more resistance in upper vocal tract (e.g. mouth) helps relaxed phonation
• Might include:
• Voiceless and voiced lip trills (horse and shiver/phone)
• Voiceless and voiced lingual trills (purr and rolled ‘r’)
• (Voiceless and voiced velar trills)
• Voiceless and voiced alveolar and postalveolar fricatives (s/z, sh/dj)
• Extension of these into CV, words, phrases etc
Hyperfunctional voice therapy: Laxvox
Aim: To facilitate healthy VF vibration by equalising supraglottic and subglottic air pressures.
• Translated: more resistance in upper vocal tract (e.g. mouth) helps relaxed phonation
• Involves: Using a silicon tube (35 cm length, 9-12mm diameter) and glass/bottle of water. End of tube placed approx. 2cm under water surface. Neutral posture and soft face essential.
• Includes:
• Blowing bubbles into water. Continual, pulses, small to large, etc
• Phonating through the tube – hhhhoooo
• Experimenting with pitch – glides, songs etc, e.g. happy birthday
Hyperfunctional voice therapy: resonant voice therapy
• Aim: Utilise nasal resonance for improved depth/richness of sound, amplification and therefore reduction of laryngeal effort
• Might include:
• Hum on /m/ or /n/ or ‘ng’ (velar nasal), aiming for vibration in lips/mouth and ideally into nose/forehead
• Moving in and out of nasal resonance
• Pitch glides/intonation with resonance
• ‘M’ onset words – mmmmmummy, mmmmmoney, mmmmmore mmmmmilk, mmmminnie mmmouse has mmmmmany mmmmmminnions etc
• Chant voice
Hyperfunctional voice disorder therapy: soft onset
• Aim: Reduce the forceful banging together of the vocal folds on initiation of phonation; bring vfs together gently for smooth onset of voicing
• Might include:
• Breathy onset phonation e.g vowels – hhhhhhee, hhhhhhhhhoooo, hhhhhhaaaa
• Reduce the exaggeration gradually of the ‘h’ or contract between with and without ‘h’
• Into words, phrases, pitch glides etc – hhhhhow hhhhhappy hhhhhis Hhhhhharry?
• Smooth transitions during passages then in connected speech
Hyperfunctional voice disorder therapy: other approaches/ therapy
• Accent Method
• The Estill Voice Programme
• Lessac-Madsen Resonant Voice Therapy
• The above approaches require specific training and I suggest looking at them in turn, but bearing in mind that they fundamentally use elements of the therapy types listed above, to different degrees.
• Laryngeal manipulation is an osteopathic technique used in some voice clinics, pioneered by Jacob Lieberman. Laryngeal Manual Therapy is a slightly gentler technique with similar aims.