Clinical Disorders of Calcium and Phosphorus
1/8
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
9 Terms
What are the two forms of circulating calcium
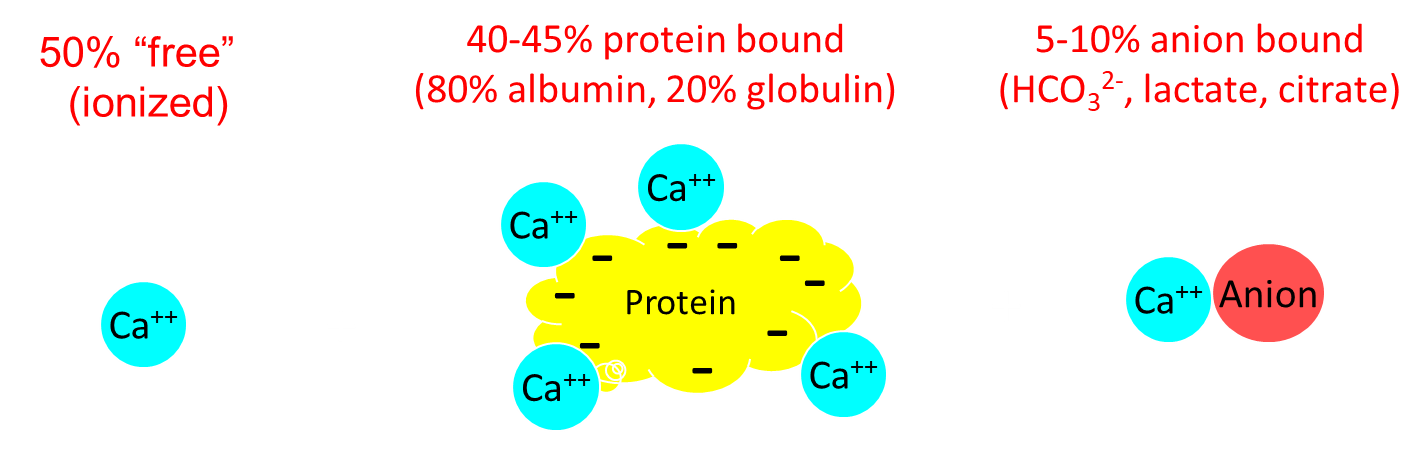
Calcium is split evenly between freely circulating and calcium bound to albumin
1) The freely circulating calcium is what is used for muscle contraction, nerve function, and blood coagulation
2) The calcium that is bound to albumin is the main part of our total calcium that fluctuates
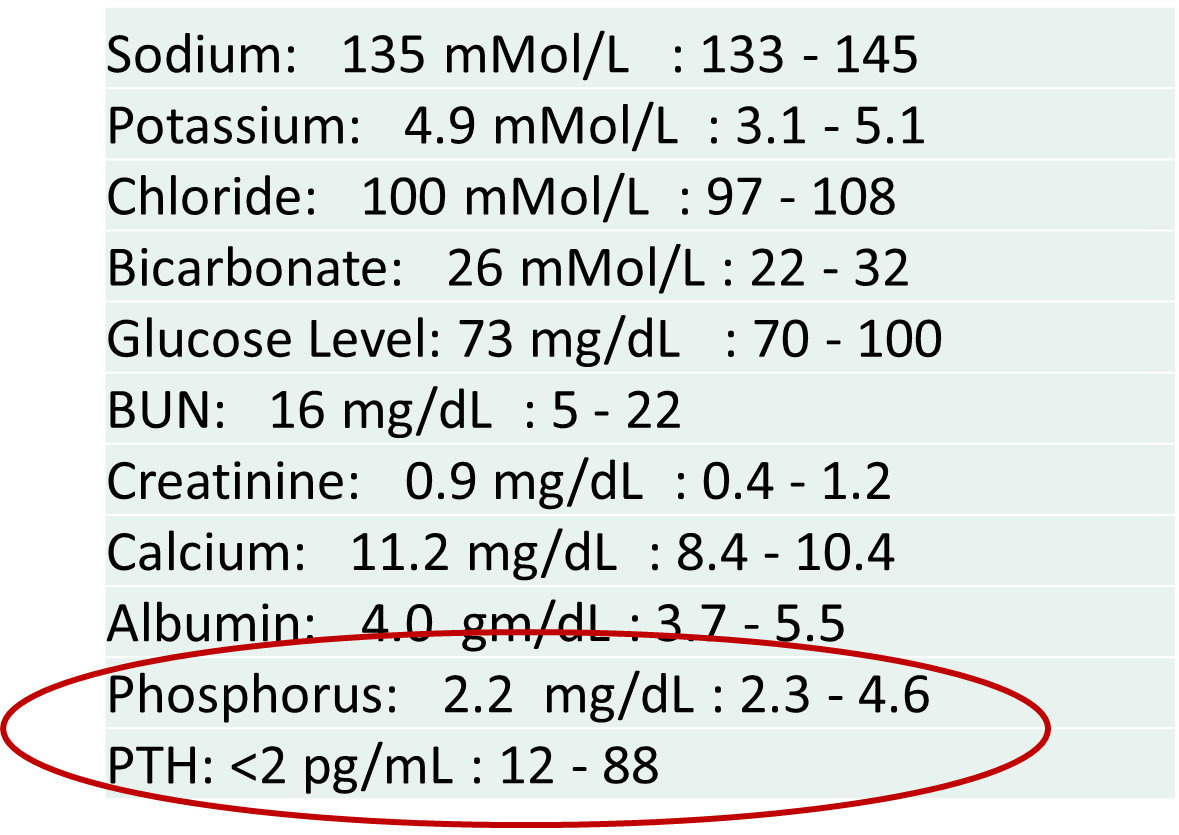
What is Primary Hyperparathyroidism?
Primary Hyperparathyroidism is a disease of the parathyroid gland triggering autonomous secretion of parathyroid hormone
1) Patients will present with stones, groans, bones, thrones, and psychiatric overtones
→ Nephrolithiasis due to high urine calcium
→ Constipation
→ Bone pain and osteoporosis
→ Mental status changes
→ polyuria
2) Patients will have high urine calcium and high serum calcium with high parathyroid hormone levels
→ patients will also have low phosphate levels due to inhibition of phosphate reabsorption
3) Treated with surgery most of the time
→ can also be treated with calcium receptor agonists like Cinacalcet
What is Familial Hypocalciuric Hypercalcemia?
Familial Hypocalciuric Hypercalcemia is a congenital disorder caused by loss of function mutation at the calcium sensing receptors located on the chief cells and the kidney
→ leads to a low urine calcium with a high serum calcium
→ parathyroid hormone is often high normal to slightly elevated
1) This disease often presents very similarly to primary hyperparathyroidism but is seen most often in younger patients as opposed to older patients
→ low urine calcium is the main distinguisher
What is Hypercalcemia due to Granulomatous and Lymphomatous Disease?
Hypercalcemia due to granulomatous or lymphomatous disease is high serum calcium levels due to excess extrarenal production of active vitamin D (calcitriol/1,25-dihydroxy-vitamin D)
1) Often seen in patients with Sarcoidosis, Lymphomas, or Tuberculosis
→ patients will have elevated calcium and phosphorus with low parathyroid hormone levels
What is Hypercalcemia of Malignancy?
Hypercalcemia of Malignancy is caused by a tumor that secretes PTHrP or Parathyroid Hormone Related Peptide
1) PTHrP can mimic the action of PTH, leading to rapid increases in serum calcium, low phosphorus levels, and low PTH
→ disease process will mimic PTH on labs, but PTH will be abnormally low
→ is often rapid onset and will be in a patient that has a known malignancy
What is the most common causes of secondary hyperparathyroidism?
Chronic Kidney Disease is the most common cause of secondary hyperparathyroidism, which presents with decreasing calcium reabsorption and increased phosphate reabsorption due to impaired activity of the kidney
1) CKD will cause secondary hyperparathyroidism due to the inability of the kidneys to respond to PTH
→ patients will also have decreased 1,25-dihydroxyvitamin D production
→ patients will have very high phosphate levels with low calcium levels
2) Patients with Secondary Hyperparathyroidism are often treated with vitamin D supplementation
→ their phosphate levels will be regulated
→ Cinacalcet, the calcium mimetic, can also be introduced, in order to reduce levels of parathyroid hormone
What is Primary Hypoparathyroidism?
Primary Hypoparathyroidism is a disorder resulting in a deficiency in parathyroid hormone secretion
1) Patients will have low parathyroid hormone levels with low calcium levels
→ the disease is diagnosed by measuring these levels twice over a period of greater than 2 weeks
2) Most often caused by surgical excision of the gland, but the next three most common are:
→ Autoimmune disease
→ Genetic Conditions
→ Idiopathic
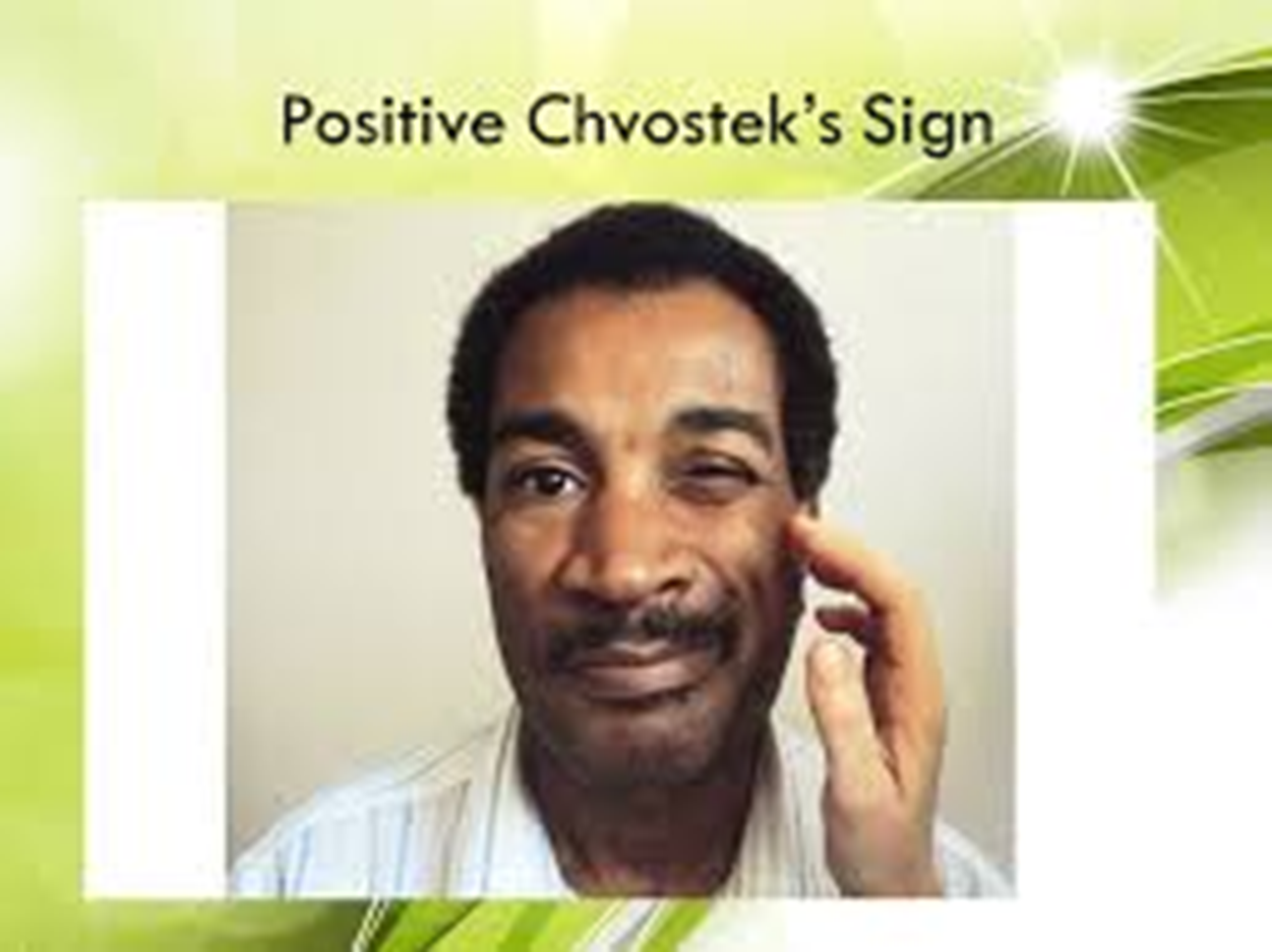
3) Patients will present with symptoms consistent with low calcium levels
→ muscle cramping and tetanus (positive Chvostek’s and Trousseau’s sign)
→ patients may have a higher bone mineral density because calcium is not being taken from the bone
4) Patients long term will have an increased risk of calcifications due to treatments leading to elevated phosphorus
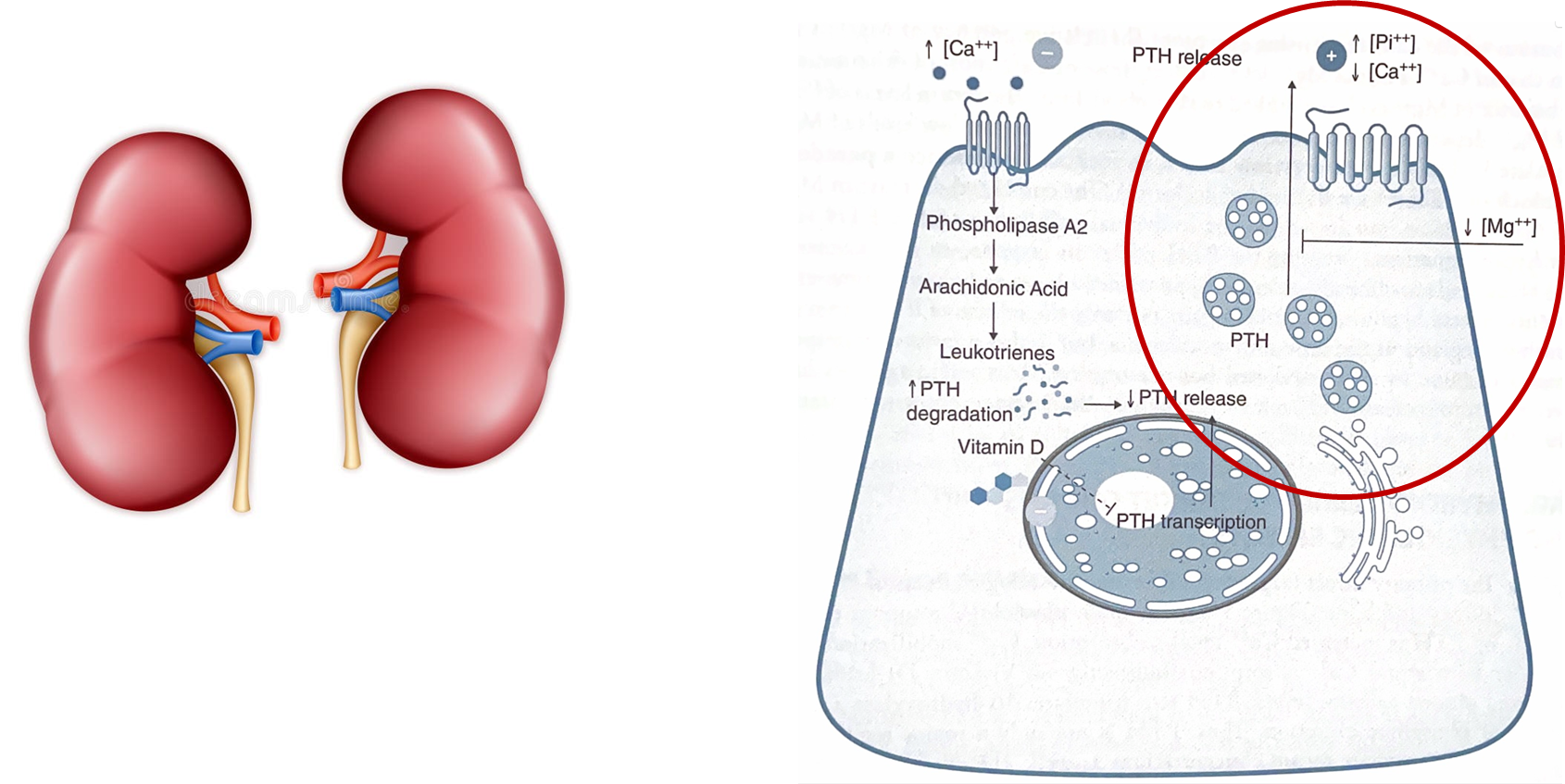
How does magnesium affect calcium levels?
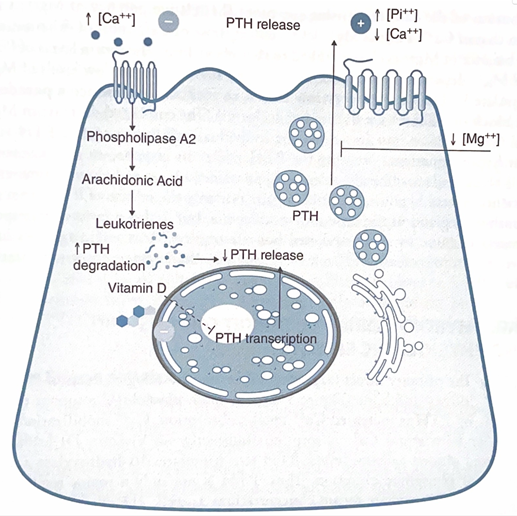
Magnesium can affect our parathyroid hormone levels based on its levels
1) Hypermagnesemia
→ magnesium is a divalent cation similar to calcium
→ magnesium can bind to the calcium sensing receptors and decrease PTH secretion
2) Hypomagnesemia
→ magnesium is a required cofactor in the pathway for PTH release
→ low magnesium will lead to a decrease in PTH secretion
What is Osteomalacia and what are the two most common genetic causes?

Osteomalacia or Rickets is a disorder of defective bone mineralization, often caused by Vitamin D deficiency or phosphorus deficiency.
→ patients have low phosphorus, low calcium, high alkaline phosphate, with normal PTH
→ alkaline phosphate levels are increased due to increased activity of osteoblasts
1) The most common hereditary form is due to X-linked hypophosphatemia caused by a mutation that prevents FGF-23 degradation
→ elevated levels of FGF-23 levels leads to increased phosphate excretion resulting in inadequate bone mineralization
2) The second most common hereditary cause is ADHR or autosomal dominant hypophosphatemia rickets
→ causes increased production of FGF23 resulting in increased phosphate excretion
3) Patients are often bow-legged and has soft-fontanelles in kids
→ often have Looser zones or areas of pseudofractures on bones in adults, looks like translucent bands