Motor Speech Disorders Final
1/101
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
102 Terms
Info about non-speech tx tasks
-Strength needed to produce speech; strong tongue ≠ more accurate articulation
-Training one part of sequence does not lead to integrated behavior
-Limited evidence to support neuromusclar treatments for speech
What should be done in place of non-speech tx tasks?
-Focus on end product and making tx simpler
1. Not focusing on the sequence -> better outcomes
-Motor learning principles
What are the motor learning principles?
-Lots of repetitions
-Intense practice
-Simple
What are the 5 components of speech production?
-Respiration: breathing
-Phonation: vocal fold vibration
-Resonance: Nasality
-Articulation: shaping air stream
-Prosody: melody patterns, stress, intonation, etc.
What are the speech disorder classifications
-Speech components involved
-Severity
-Perceptual characteristics
-Confirmatory signs: speech system (e.g., lingual) and non-speech (e.g., impaired gait, writing)
What do we want from tx?
A partnerships w/ our pts to see what it is they will want to do
What are three areas EBP is combined in?
-Clinical decision-making
-Client's preferences
-Published literature
Describe dysarthria
-Neurologic speech disorder w/ abnormalities in strength, speed, range, steadiness, tone or accuracy of movements required for control of the respiratory, phonatory, articulatory and prosodic aspect of speech production
What causes dysarthria
-Central/peripheral nervous system abnormalities
How is dysarthria reflected in the voice
-Weakness
-Spasticity
-Incoordination
-Involuntary movements
-Excessive/reduced/variable muscle tone
Describe the Assessment of Intelligibility of Dysarthric Speech
-Single word and sentence level % of intelligibility
-Can calculate WPM
-Need unfamiliar listeners to transcribe utterances
-Speech intelligibility test
Describe Dysarthria Impact profile
-48 item questionnaire on the psychosocial impact of dysarthria from speaker's perspective; 5 point rating
-5 sections:
1. Effect on pt
2. Accepting dysarthria,
3. How pt feels other reacts to their speech
4. How dysarthria affects comm.
5. Dysarthria relative to other concerns
Describe Apraxia of speech (AOS)
-Praxis = plan/program of motor movement
-Neurologic speech disorder that reflects an impaired capacity to plan sensorimotor commands necessary for speech
-Deficit in ability to accurately produce sequential speech movement
-Impaired motor planning for the intentional movements needed for speech
What are the clinical characteristics of AOS
-Slow rate of speech
-Speech-sound errors
-Errors that are relatively consistent in type (i.e., distortion) and location (i.e. within a word)
-Disturbed prosody
What are the characteristics of severe AOS
-Reduced variability of articulatory characteristics
-Few meaningful utterances and automatic speech not better than volitional
-Singing: appropriate melody/tune, appropriate # of syllables, but only single consonants and few vowels
How do you define a syllable
-One vowel sound w/ any corresponding consonant sounds that surround it
-The placement of consonants often determines the sound of the vowel
Describe Nonverbal Oral Apraxia (NOVA) and limb apraxia
-NOVA: deficit in ability to sequence nonverbal, voluntary movements of tongue/lips/jaw and other associated structures; unrelated to speech production
-Limb apraxia: inability to sequence movements of arms/legs/hands/feet during voluntary action
Describe AOS vs dysarthria
-AOS: motor planning deficit; difficulties typically limited to articulation and prosody
-Dysarthria: motor execution deficit; difficulties often include respiration/phonation/resonance along w/ articulation/prosody
Describe primary progressive apraxia of speech (PPAOS)
-May be the only/most important clinical sign of neurodegenerative disease
-Speech is sole impairment to start
-Core features:
1. Slow rate
2. Artic disturbances
3. Distorted sound substitutions
4. Segmentation of syllable in multisyllabic words
-Pt. know what they want to say but do not come out right
What are the subtypes of PPAOS
-Phonetic: artic distortions, sound additions, subsitutions/distortions
-Prosodic: slow segmented speech, inter-word segmentation, intra-word segmentation
-Pts. can have both types
-Dysarthria can be present BUT cannot be more severe than AOS @ presentation
Describe Apraxia Battery for Adults 2nd Edition
-Variety of tasks
1. Single syllable words that start and end w/ the same sound
2. Words of increasing length
3. Multisyllabic complex sentences
-Looks @ aspects of NVOA
Do apraxia assessments always work?
-Typical testing may be too difficult/frustrating for persons w/ severe AOS
Describe the Colorado Motor Speech Framework
-Not specific to AOS or dysarthria
-Looks @ various aspects of MSD
-Free online
What are two measures that help distinguish if people w/ L MCA stroke have AOS
-Words of increasing length (thick/thickening) on ABA-2
-Pairwise variability of index for strong-weak words
1. have weak onset and 2nd syll is a long vowel for max contrast (banana, tomato, potato)
-People w/ AOS have difficulty producing longer words and controlling timing of vowels in polysyllabic words
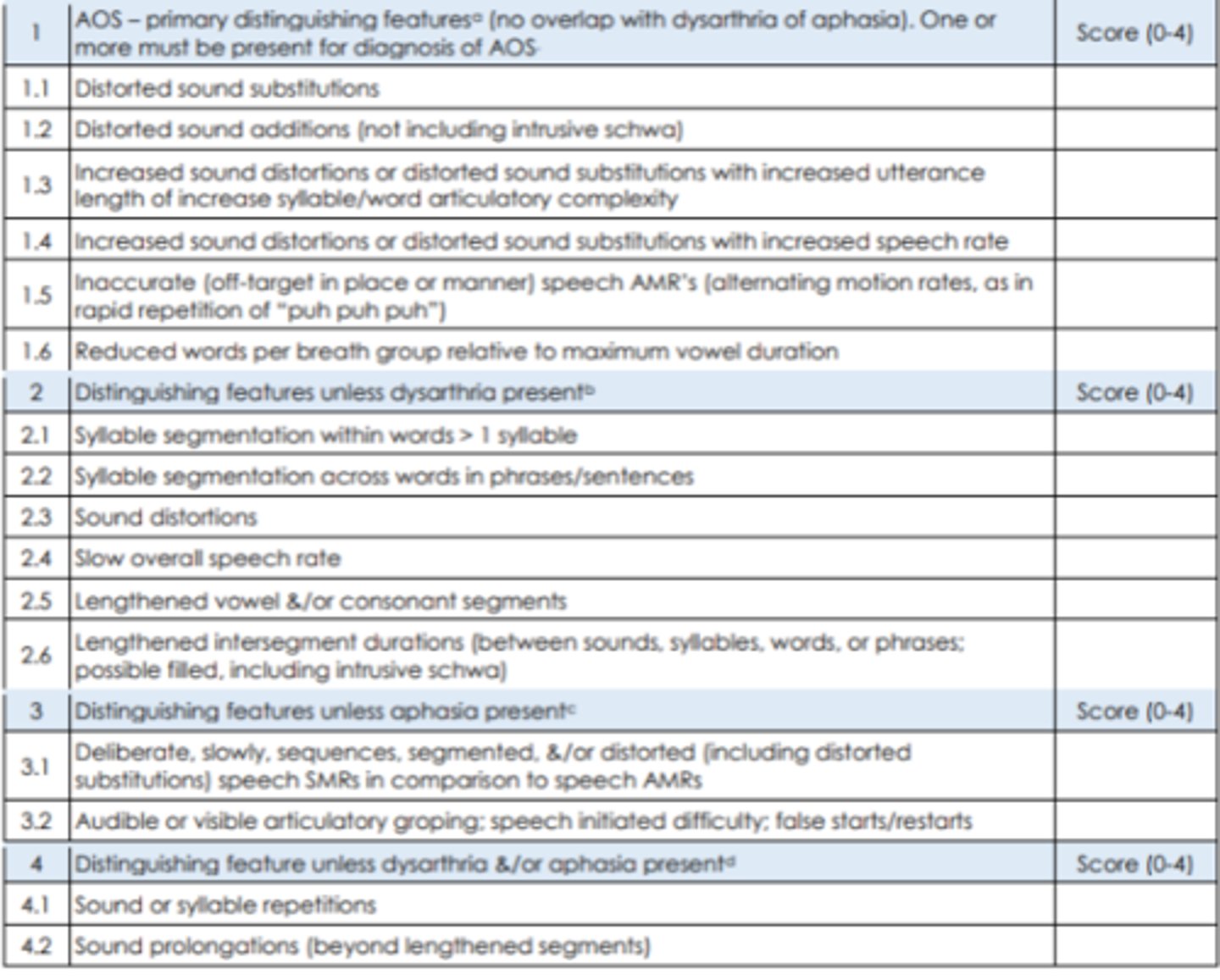
Describe the Apraxia of Speech Rate Scale
-16 item rating scale
-Designed to quantify AOS diagnosis:
1. Presence/absence
2. Relative frequency
3. Severity of characteristics
-Need to have a score of 8 or above and at least 1 of the first 6 items in order to have AOS dx
What assessments should be done if MSD is suspected
-Cranial Nerve Exam
-Motor Speech Exam
-5 Components of speech: artic, respiration, phonation, resonance and prosody
-Look @ structures at rest/sustained pose/during motion
-Look @ ROM/symmetry/steadiness/loudness/strength/weakness (loudness is perceptual, intensity is measurable)
-Speech vs. non-speech functions
-Assess speech in w/e capacity they possess
What speech tasks does Mayo do for assessment
-Connected speech: reading, picture description, conversation, monologue
-Repetition: single words, sentences
-Evaluate pt as a whole in their life/community per WHO's International Classification of Functioning (ICF)
What are some considerations when assessing for MSD
-Identify linguistic features that are differentially affected depending on the language is essential for best treatment
-Culturally responsive treatment includes SLP's clinical knowledge/experience and pt's lived experiences
-Cultural humility
-Use interpreters
What are the main types of AOS treatment?
-Articulatory-Kinematic: focus on articulatory movements
1. some approaches: motor learning, imagined production, integral stimulation, script training
-Rate/rhythm control: focus is prosody and includes pacing tasks
-Multi-modal training: combine gesture and visual
-AAC
-Person w/ AOS can benefit from behavioral tx
Describe motor learning information
-Neurons of the "mirror system neurons" believed to be a way w learn new motor actions; 1st we observe, then we try
-This system, including Broca's area, is activated when looking @ pictures of lip postures indicating vowel sound production during imitation/free production
What are the motor learning tenets for developing a motor program
-Focus on learning, retention, and generalization vs. performance
-Drill is essential
-Instruction improves performance by providing a model of the motor skll
-Self-learning and self-detection are valuable
-Feedback is essential
-Specificity of training is needed
-Practice schedule influences acquisition and retention
Describe motor learning principles
-Motor learning theory: different approaches should be used based on stage learning and the final outcome
-Practice schedule: blocked vs random; include variability and complexity
-Feedback: knowledge of performance (KP) and knowledge of results (KR)
-Frequency feedback: reducing KR can lead to better retention; delayed feedback leads to better retention
-Specificity of training: the more similar the action is to the activity, the more likely it will generalize to other contexts; begin treatments w/ whole words/expressions vs. phonemes
-Prep the pts.: more difficulties early on but more durable, longer-lasting outcomes; set them up to have as high accuracy as possible in a typical session
-Stimuli: work least complex to most complex
-Non-words: takes away language demands that might get in the way of making progress
What's the difference between knowledge of performance (KP) and knowledge of results (KR)
-KP: provides specific info on how to correct an incorrect pattern
-KR: indicates accuracy levels
What is the 4 point rating scale for self-reflection
-+1 Bad: I didn't do it
-+2 Hard, I tried it
-+3 Good, I fixed it
-+4 Easy, I got it
What are the motor learning principles included in systematic review on AOS
-Practice: massed vs. distributed, blocked vs. random
-Targets: simple vs. complex
-Feedback: KP vs. KR, high vs. low frequency, immediate vs. delayed
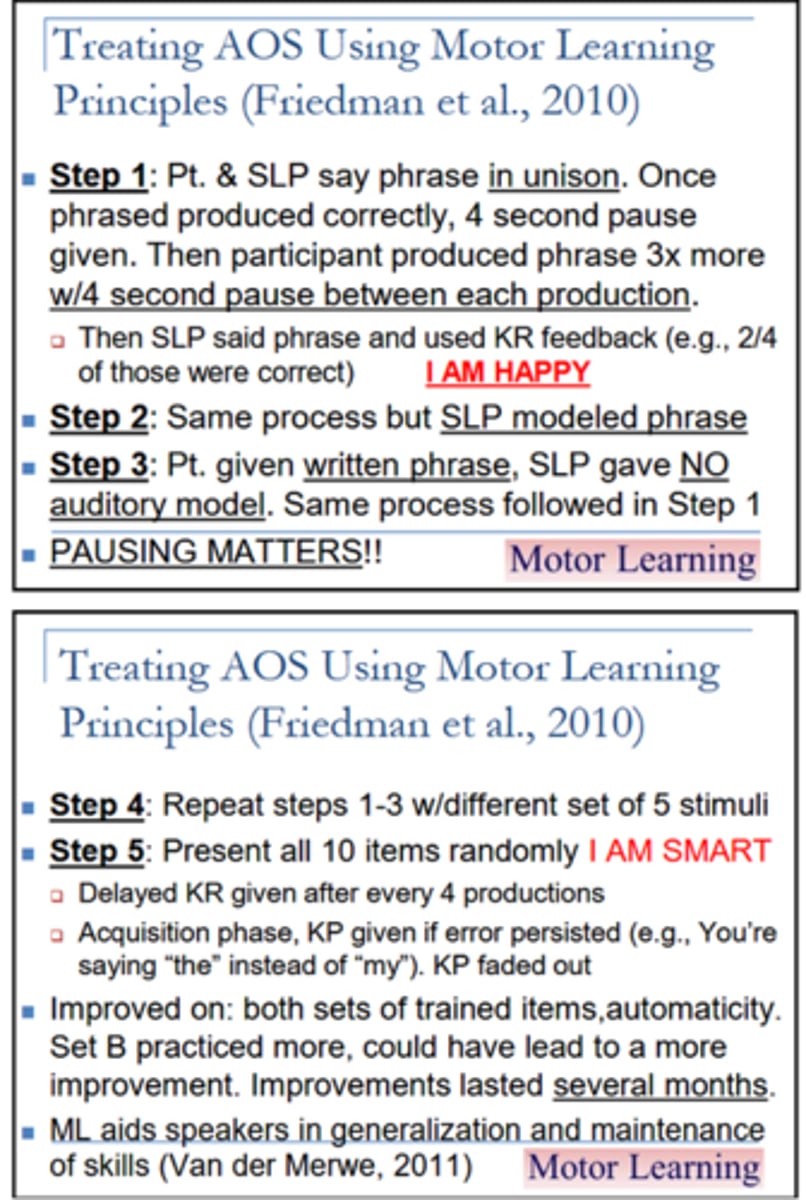
Example of Treating AOS using Motor Learning Principles
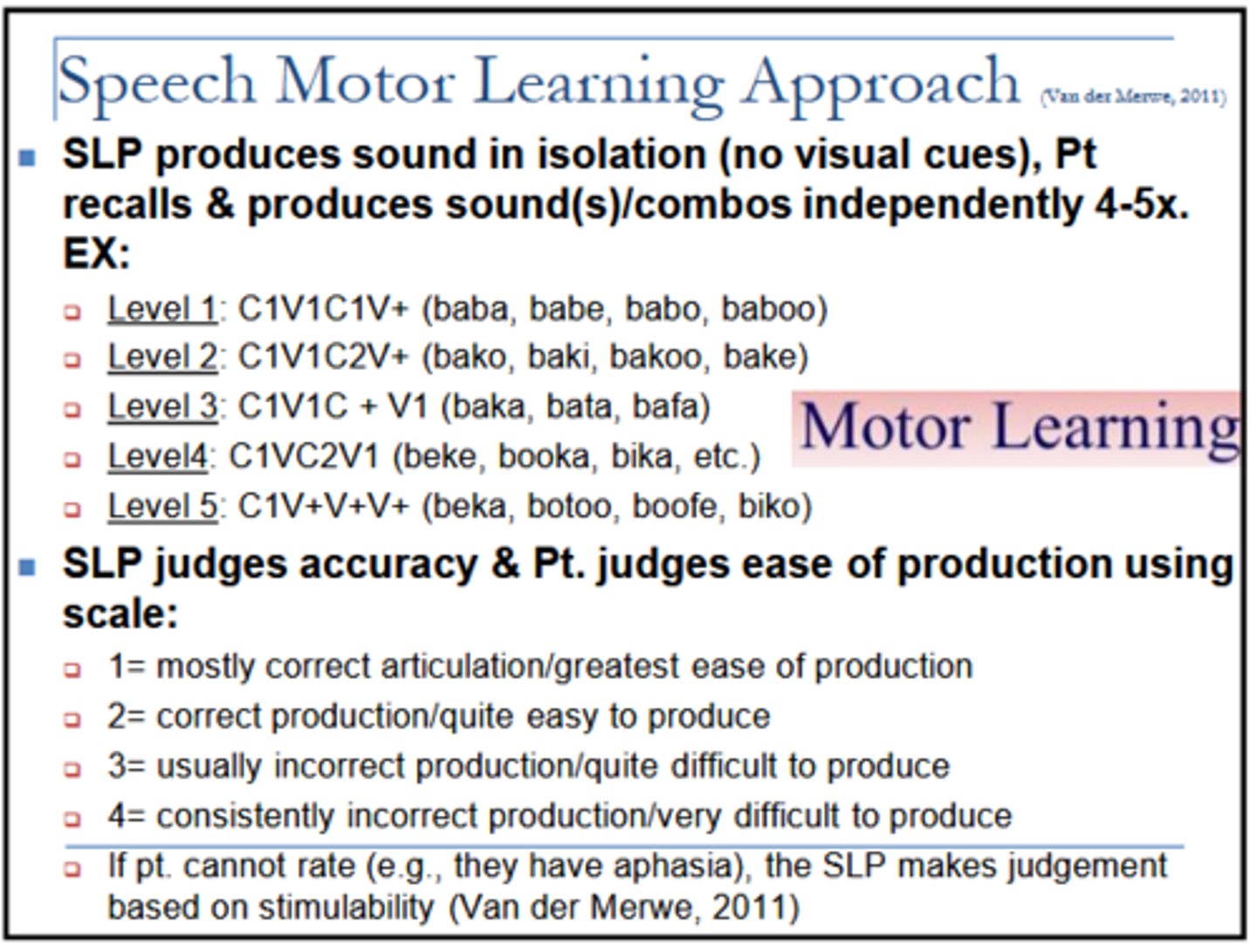
Speech Motor Learning Approach Scale
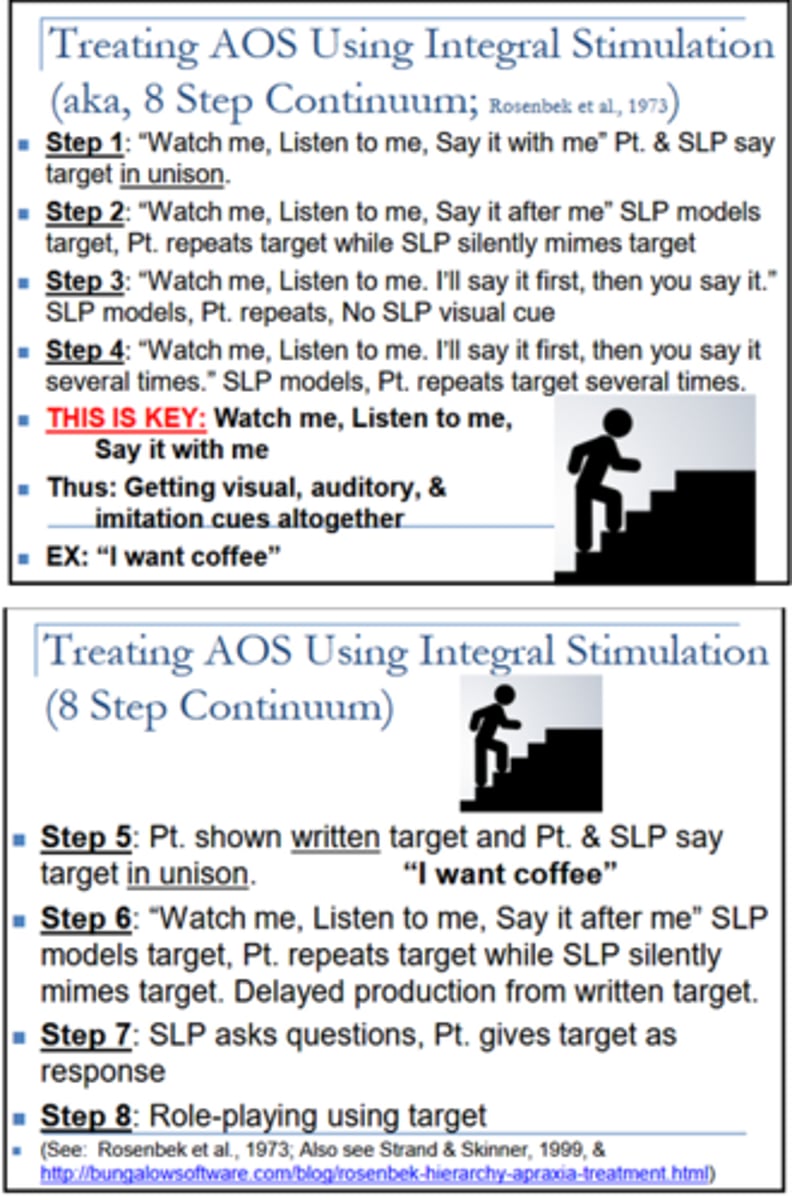
Treating AOS using integral stimulation (8 step continuum)
Treating AOS: sound production treatment
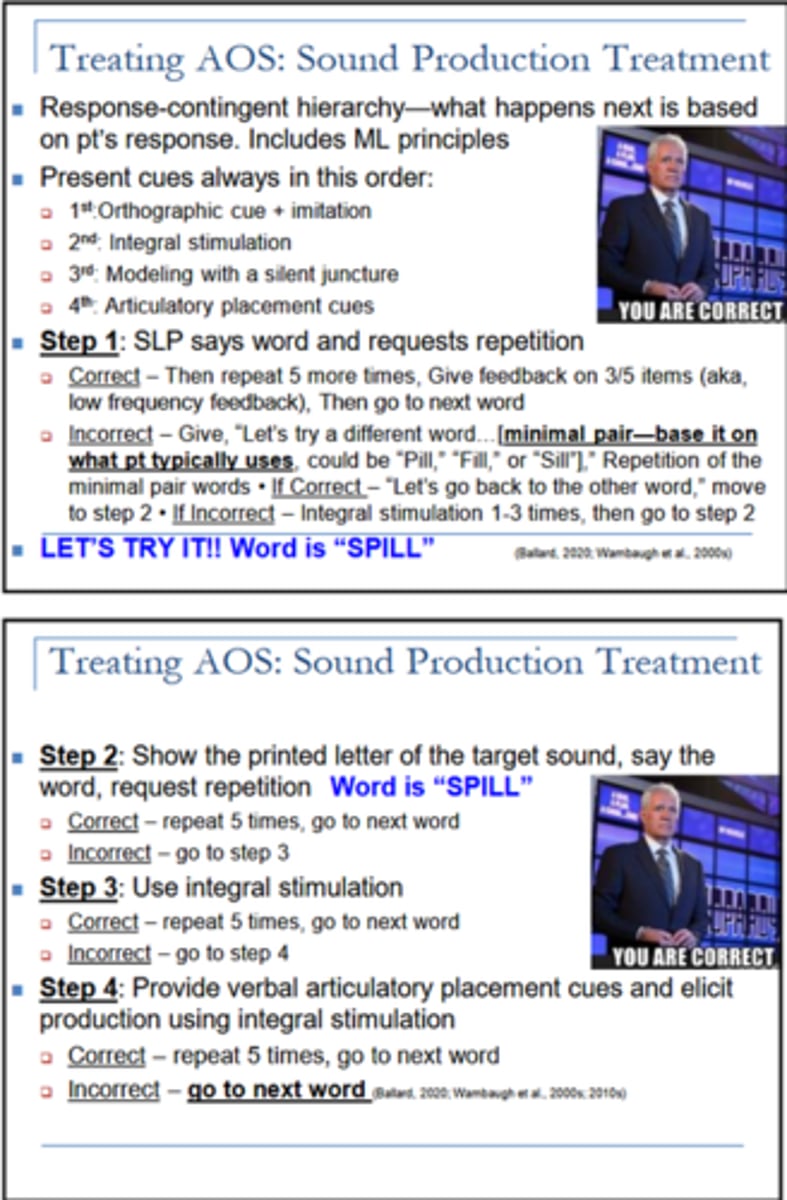
Describe Repeated Practice for treating AOS
-Target where pt. was 0-40% at baseline
-Repeat target 5x after single verbal model with:
1. minimal feedback on productions
2. 15 productions per target, per session
3. small blocks of randomized presentation
-Can do at home
Treating AOS w/ rate/rhythm control
Describe Perceptual Assessment of Respiration
Listen to:
-Loudness: if loudness appropriate, respiratory support likely to be Ok; reduced loudness may indicate respiratory problems. Keep constant mouth-mic distance. Listen to:
1. overall loudness
2. Consistency of loudness
3. Stress patterns
-Breath patterns & phrasing: where are pauses, are they appropriate
Describe Respiratory impairments and associated speech changes
-Impairments
1. reduced inspiratory capacity
2. reduced expiratory pressure
3. reduced control: checking action, involuntary movements
-Speech changes
1. reduced overall loudness
2. loudness decay
3. excessive loudness variation
Describe supporting respiratory function
-Postural adjustments: sitting upright/standing typically better than lying supine, avoid excess flexion (trunk/abdomen and neck)
-External supports: expiratory boards
Describe inspiratory muscle training
-diaphragm is primary target (belly breathing)
-Discourage excess use of accessory muscles (shoulder breathing)
-Goal to establish strong, quick inspiration followed by slow, controlled exhalation
Describe controlled expiration (inspiratory checking)
-Can be combined w/diaphragmatic breathing
-Focus on quick, strong inhalation
-Followed by slow, steady exhalation
Describe Expiratory Muscle Strength Training (EMST)
-Pressure threshold trainer
-Resistance set t 75% max expiratory pressure
-Rules of 5s
1. 5 reps
2. 5 times per day
3. 5 times per week
-4-8 weeks
What's the difference between the breather and pressure threshold trainer
-Breather: cheaper, creates resistance based on airflow; flow-dependent
-Pressure threshold trainer: using a spring-loaded valve to provide resistance once a set pressure is met; pressure dependent
Describe respiration treatment phrase grouping
-Targets strategic pauses for inhalation
-Phrase length selected according to:
1. respiratory support
2. syntactic boundaries
Describe resonance treatment resonatory impairments
-Impairments:
1. velar weakness
2. slowness of velar elevation
3. reduced control: incoordination, involuntary movements
-Associated speech challenges:
1. hypernasality
2. nasal emission
3. weak articulatory contacts
4. hypnasality
5. alternating resonance
Describe resonance treatment velopharyngeal exercise
-non speech exercises
1. examples: horn-blowing, straw sucking
2. no evidence for carryover to speech tasks
-speech exercise
1. continuous positive airway pressure (CPAP)
2. Overloads the velopharyngeal musculature during speech tasks
Describe speech based resonatory treatment
-emphasis on appropriate oral/or nasal resonance
-may incorporate augmented feedback
-may incorporate progressive difficulty
Describe resonance treatment prosthetic management
-Palatal lift
1. assessment/implementation in collaboration w/ prosthodontist
2. will be most helpful for speakers w/ isolated hypernasality/nasality disproportionate to other features
-Behavioral intervention usually still needed
-Differs from Obturator: Obturator fills a cleft wheres life is for velar elvation in the absence of motor control
Describe phonation treatment phonatory impairments
-impairments
1. hypo-adduction
2.hyper-adduction
3. reduced flexability
4. reduced stability
-associated speech changes
1. strained voice
2. breathiness
3. reduced loudness
4. monopitch/monoloudness
5. tremor
6. flutter
Describe phonation treatment reducing laryngeal strain
-direct speaker's attention to somatosensory aspects of muscle tension
-some aspects of laryngeal strain may not respond to behavioral approaches
-excess laryngeal tension may result from poor respiratory support/poor coordination w/ respiration
Describe phonation treatment laryngeal exercise
-Increasing medical compression (adduction)
1. push-pull
2. grunt
3. cough
-Increasing pitch range/control
1. pitch glides/steps
2. pitch matching
MSD treatment considerations
-Most research done in adults w/ PD because most have hypokinetic dysarthria
-Pt may need language-independent and language specific speech treatment
Describe language independent treatment approach
-Most notable speech characteristics of dysarthria are neurological so they present the same in all languages; ST strategies are universal
Describe language specific treatment approach
-Some treatments can vary across language
-Ex: tonal languages may require more focus on intonation to improve intelligibility
Describe Lee Silverman Voice Treatment (LVST LOUD)
-Targets respiratory, articulatory, laryngeal and prosodic subsystems
-Loudness therapy incorporates coordination of respiration and phonation
-"Talk with effort"
-Intense: 4 days/weeks x 4 weeks x1 hour/day plus daily HW
1. Daily exercises
2. Hierarchy Exercises
3. Homework
4. Shaping techniques
-Counteracts underlying neurological deficits by increasing amplitude of speech production
Describe the research on LSVT LOUD
-Has better outcomes in loudness than LSVT ARTIC or being untreated
-Adaptable to telepractice
-Successful in other dx
-Challenging w/o practice partner
-
Describe phonation treatment Speak Out
-Speak w/ intent
-12 sessions, 40-45 mins per session
-Pt works on series of speech, voice and cognitive exercises
-Pay for training; do not have to pay annual/biannual fees
-Use voice amplification to gain extra acoustic info
-Cheaper than LSVT LOUD
-Can conserve energy; loud may be too much effort for some
Describe phonation treatment coordinating respiration and phonation
-Potential targets
1. lung volume at onset of phonation
2. Initiating phonation at top of exhalation
3. Phrase grouping (ceasing phonation before respiratory support wanes)
4. Rapid inhalation between phrases
Describe articulation treatment articulatory impairments
-Impairments
1. Weakness/fatigue
2. Reduced range of motion
3. Reduced speed
4. Reduced coordination
5. Involuntary movements
-Associated speech changes
1. Articulatory imprecision
2. Slow rate
Describe articulation treatment supporting articulatory function
-Velopharyngeal support
-Jaw Support (bite block)
-Sensory tricks (hyperkinetic dysarthria-dystonia)
-Traditional articulatory therapy
-Articulation therapy using MLT
Describe articulation treatment Nonspeech OM exercise/articulatory exercise
-Candidates for exercise: detectable weakness primary contributor to articulatory imprecision
-Tongue strengthening programs
-Not every pt who's weak has weakness as main prob; dysarthria doesn't mean they're weak
Describe strength training principles
-Overload and progression:
1. Overload: tax muscles beyond typical functioning=increase motor unit recruitment
2. Progression: systematic overload
-Intensity
-Recovery: allow recovery between sessions but avoid reversal
1. Tongue strengthening: 3-7 days/week
2. respiratory muscles strengthening: 3-5 days/week
-Reversibility: use it or lose it
-Specificity of training
Describe strength training w/ dysarthria
-Limited support
-Most caution against emphasizing strength training over speech directed tx
-Acknowledge potential benefit for specific pts
Describe articulation treatment articulatory treatments
-Exaggerated articulation
-Alternative place/manner voicing
-Coordination of complex phonetic sequencing
-Vowel space matters: helps differentiate vowels from each other; increases intelligibility
-Visual phonics: gesture/symbol based cuing system
Describe prosody treatment speaking rate
-Slower rate allows more time for aritculatory placements and speech precision
-Increasing overall speaking rate is almost never an appropriate target (even for slow rate)
-Reducing speaking rates improves intelligibility (even in patients w/ normal/slow rate
-Speakers w/ hypokinetic dysarthria often have rapid rate + may have difficulty reducing rate
Describe prosody treatment rate reduction strategies
-Pacing board/hand tapping
-Metronome
-Stopping between each word briefly (not between syllables)
-Delayed auditory feedback
-Indirect strategies: increased loudness, clear speech
-Contrastive stress drill and verbal repair
Describe intelligibility treatment
-Slow rate by separating words (not syllables)
-Clear speech (speak like someone is HOH)
-Shorten utterances to key words
-Speech supplementation: gestures, facial expressions)
Describe comprehensibility treatment
-Communicative exchange not only speech and responsibility of speaker: improve communicative context w/o focusing only on speech
Give examples of speaker comprehensibility treatment
-Face listener
-Cue topic
-Signal topic change
-Use predictable sentence types + words
-Gestures, facial expressions, amplification
-Writing
-Don't assume they know what you know, even if its common sense
Give examples of listener comprehensibility treatment
-Reduce background noise
-Face speaker
-Look for turn-taking signals
-Watch for topic changes
-Take advantage of cues/devices
-Seek clarification
Describe comprehensibility treatment techniques
-Glossing: listener repeats word as soon as its heard; speaker stops only when listener incorrectly repeats a word and repair strategies are employed
-Amplification
-Environmental changes: eliminate background noise, good lighting, speak in same room
-AAC
-Expect ppl to need various techniques
Describe dysarthria treatments at On With Life
-Imitation
-Speech strategies
-Vocal amplitude exercises
-OM exercises
-Biofeedback for motor planning: record/self asses, use mirror
-Voice resistance: EMST/breather
-Facial massage/stretching
-CPAP protocol
-Home exercises
Describe flacid dysarthria
-Weakness
-Hypotonia: saggy/floppy
-Atrophy
-Fasciculations: twitches
-Progressive weakness w/ use
-Pts perceptions and complaints
Describe documenting flaccid dysarthria
-NOMS and level of severity
-Level of intelligibility DN necessarily match the NOMS
-Can document intelligibility based on:
1. Familiar vs. unfamiliar listener
2. Known vs. unknown context
3. Single words vs. longer utterances
Describe treatment options for flaccid dysarthria
-Must match what you documented w/ what you did in therapy
-Increased intelligibility: overarticulation, clear speech
-Improve prosodic variation by working on pitch range exercises + contrastive stress drills
-Increase breath support to:
1. increase loudness
2. improve intelligibility
3. lengthen phrases
-Velar exercises
Describe spastic dysarthria
-Produced by damage to bilateral direct and indirect activation pathways of CNS
1. lesions in the UMN
2 Difficulty w/ fine, discrete movements (button shirt, zip pants, etc.)
-Spasticity slows everything down
-Imprecise articulation, harsh/strained voice
-Slow rate
-Short phrases
Describe etiologies of spastic dysarthria
-CVA
1. Single BS stroke because left+ rght UM pathways are in close proximity
2. Single cerebral hemispheric CVA not typically the cause
-TBI
-Degenerative disease
-Multi-infarct dementia (vascular dementia)
-Neoplasm
-Gliobastoma multiforme affecting both hemispheres
Give examples of what bilateral damage can lead to
-Loss/reduction in ability to facilitate fine/discrete motor movements
-Muscle tone
-Reflexes: Babinski, snout
-Overactivity
-Drooling: muscles tighten/ DN move easily, not swallowing as much
-Reduced ROM
Describe vocal function exercises
-Used to strength/balance the laryngeal musculature
-Create a balance among airflow, laryngeal muscular effort and tone placement
-Can be used to indirectly address onset of vocal fold vibration and laryngeal area tension
-Do softly but not breathy
1. sustain the /i/ as long as possible
2. glide from lowest note to highest on word "knoll" and vice versa
Describe ataxic dysarthria and cerebellar damage
-Damage to the cerebellum + it's control circuit
1. including vermis which connects the hemispheres @ the midline, affecting force, timing and online regulation
-Ataxia: poor muscle control
-Gait and standing
-Occular problems: nystagmus
-Hypotonia
-Dysmetria: inability to control ROM
-Dyssynergia: decomposition of movement; errors in sequence and speed
-Tremor
Describe ataxic dysarthria
-Many aspect of OM exam can be WNL
-Speech reflects:
1. Irregular articulatory breakdowns
2. AMRS irregular and uneven
3. Excess and equal stress
4. Slow ROS
5. Prolonged phonemes
6. Telescoping syllables: simplify bc its too effortful to say all syllables
7. Paradoxical movements: reduce vital capacity
-Cluster symptoms: artic inaccuracy, prosodic excess, phonotory-prosodic insufficiency
Describe treatment options for ataxic dysarthria
-Improve respiratory control by encouraging slow + controlled exhalation
1. Immediate speech upon exhalation
-Reduce ROS to allow more time for articulator movement
-Improve stress and intonation by using contrastive stress drills and pitch range exercises
-Target articualtion using traditional articulation/possibly motor learning tasks
Describe clear speech
-Speakers modify habitual speech to enhance intelligibility for a listener
-Overarticulation + slowed speech are central to this technique
-Tends to be 5-8 dB louder than conversational speech
-Persons s/p CVA/TBI w/ dysarthria improved single word/conversational speech intelligibility w/ technique
-1 hour x 4x/week x 1 month
Describe hypokinetic dysarthria
-Hypokinetic= reduced movement
-Basal Ganglia activities strongly associated w/ actions of Indirect Activation Pathways-muscle tone
-Neurotransmitters: Acetylcholine (ACh) and dopamine (DA)
-Parkinson's Disease: idiopathic vs. med-induced
-Speech: low volume, monopitch, reduced stress, tremulous vocal qualty, pallialia (invalid repetition of own words)
Describe drug-induced Parkinsonism
-Onset: within 3 hours
-Reversible: months to years
-Risk factors: advanged age, dementia, female, pre-existing PD
-Tremor may not be present
Describe signs of Parkinson's Disease
-Resting tremor
-Bradykinesia: generalized slowness of movement
-Akineasia: loss of voluntary muscle movement
-Rigidity
-Disturbances/reduced postural reflexes
-Kyphosis: excessive outward curve of spine
-Strength
-Mask-lik face
-Gait
-Writing
-Sensory impairments
Describe how normal pressure hydrocephalus gets confused for Parkinson's Disease
-Gait problems
-Mild dementia
-Incontinence
-Not from "old age"
-NPH does not have tremors like PD
Describe recording hypokinetic dysarthria
-NOMS
-Level of severity
-Level of intelligibility does not have to match NOMS rating
Describe treatment options for ataxic dysarthria
-Reduce ROS
-Traditional articulatory techniques
-Increase ROM of laryngeal muscles to improve vocal quality
-LSVT Loud
-Parkinson's voice project
-Clear and loud speech
Describe deep brain stimulation
-Good candidates:
1. PD symptoms for at least 5 yrs
2. On/off fluctuations w/ or w/o dyskinesia
3. Good response to PD meds
4 Tried other PD meds w/o benefit
5. PD symptoms that interfere w/ ADLs
-Placed in globus pallidus or subthalamic nucleus (basal ganglia)
-Impaired speech production may result from activation
-Mood disorders possible post-surgery
Describe hyperkinetic dysarthrias
-Hyperkinetic=abnormal/excessive involuntary movements (dyskinesias)
-Damage to basal ganglia in control circuit
-Every hyperkinetic disorder has own movement pattern
-Level of intelligibility does NOT capture social consequences
-Normal involuntary movement vs abnormal involuntary movements
-Chorea vs. dystonia
Describe sampling hyperkinetic dysarthria
-Voice stoppages
-Sudden forced, involuntary inhalation/exhalation
-Jerky
-Prolonged intervals
-Inappropriate silences
-Loudness variations
-Transient breathiness
-Irregular articulatory breakdowns
-Pt. perceptions and complaints
-Etiologies
Describe treatment options for hyperkinetic dysarthria
-Sensory tricks + relaxation techniques to minimize effects of involuntary movement
-Botox
-Use of easy onset to lessen involuntary movements that affect larynx during speech
-Respiratory (strengthening/control), phonatory (glottal adduction), and OM exercises for lip/tongue ROM and resistance led to improved CN exam
1. Intelligibility, comprehensibility + naturalness not measured
Describe upper motor neuron dysarthria
-UMNs damaged that carry impulses to Cranial + Spinal nerves that supply speech muscles
-Typically mild and temporary
-Often accompanies aphasia, AOS or other comm dis
-May be only comm disorder/sign of neurologic damage
-Reflects unilateral UMN weakness in face + tongue
-Mild hypsernasalty, slow rate, slow/irregular AMRs, imprecise artic, strained/harsh voice
Give examples of mixed dysarthrias etiologies
-ALS: spastic-flaccid
1. When rate of speech is slowed to 120 WPM, reduction in intelligibility is imminent
2. Can have AOS, but uncommon
-MS: spastic-ataxic most common
1. LSVT might address rate, low volume
-Brain tumor: depends on where tumor is/what its doing