Creams, ointments and topical preparations
1/51
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
52 Terms
What does topical mean?
Applied to any external body surface for a localised effect
E.g. eye, nasal mucosa, skin, scalp
What label goes on all topical formulations?
“For external use only”
Why do we give treatment locally to the skin?
To enhance barrier function of the skin
Targeted delivery to specific layers of the skin
e.g. fungal infections are in the outermost part of the skin
e.g. for eczema need to deliver drugs deeper into the skin
Fewer side effects with topical preparation compared with oral delivery
How do topical formulations improve skin’s barrier function?
Sunscreens protect against UV radiation
Antibiotics for abrasions protect against infection
Emollients (preparations that add moisture) improve dry skin conditions
Moisturisers protect against drying atmospheric conditions
Barrier creams prevent exposure of the skin to harsh chemicals
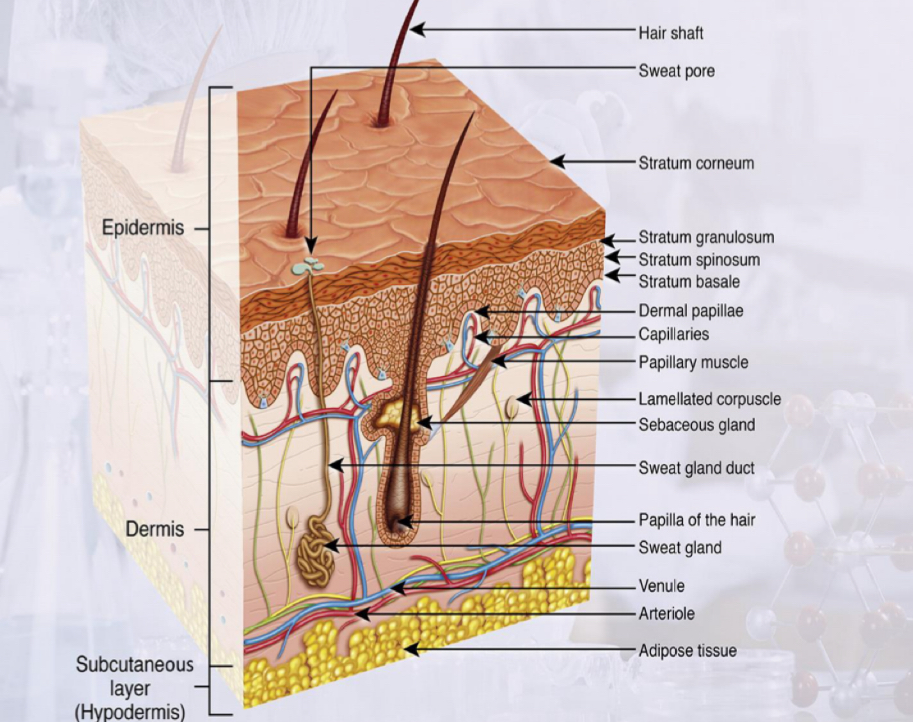
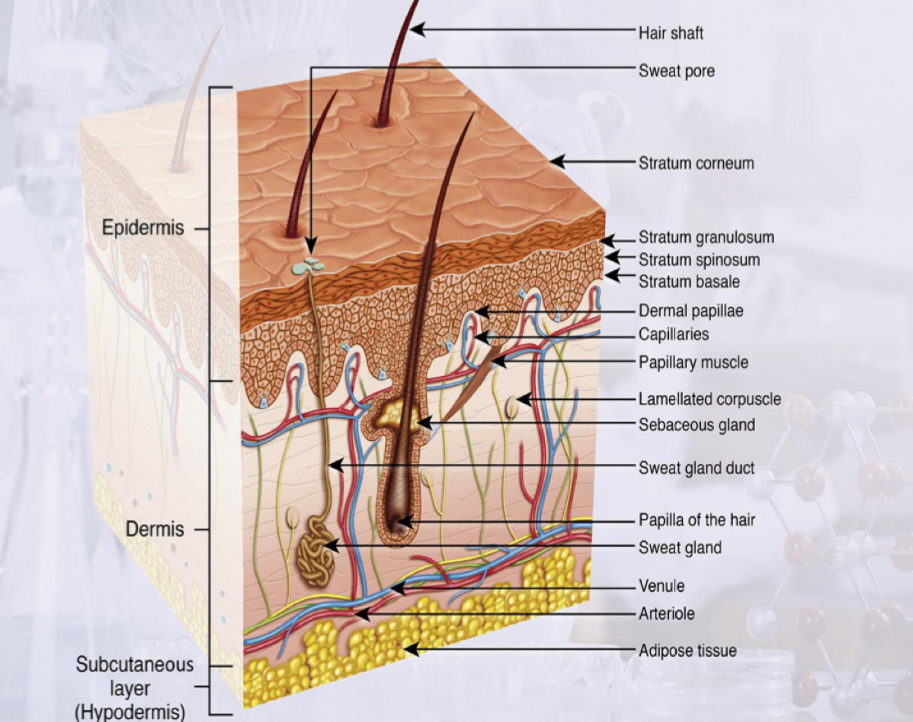
Describe the 3 main layers of the skin
Epidermis
Dermis
Subcutaneous layer (hypodermis)
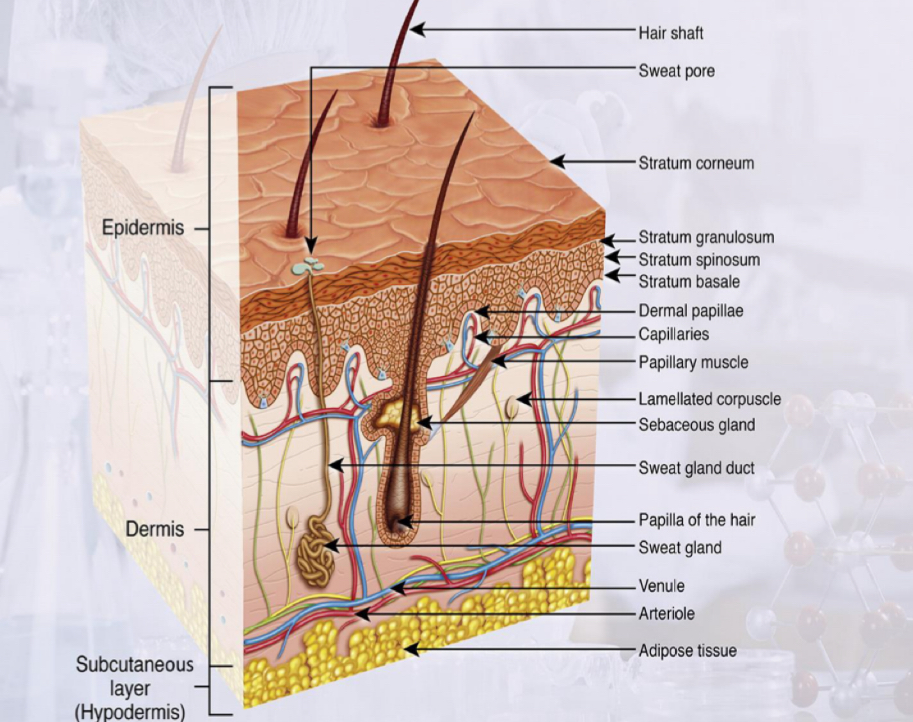
Describe where different components of the skin are located in each of the layers
Stratum corneum is the outer layer of the epidermis
Skin cells begin life in the stratum basale layer of the epidermis
Blood vessels are present in the dermis but not the epidermis
Sweat glands, hair follicles and sebaceous glands originate in the dermis
Subcutaneous layer is fatty tissue and acts as a cushion for the skin
What topical dosage form should you select for application to the skin, depending on which layer of the skin needs treating?
Skin surface = on the skin
Stratum corneum = in the skin
Viable epidermis = deeper in the skin
Dermis = underneath the epidermis
Skin appendages = hair, sweat glands, sebaceous glands, nails
Example of when we would need to treat the stratum corneum
Fungal infections present
What do we have to make sure about the formulation if treating the epidermis or dermis?
The formulation must allow the drug to cross the stratum corneum
AKA there must be percutaneous absorption of the drug
Types of topical dosage forms
Semisolids e.g. ointments, pastes, creams, lotions, gels
Topical solutions
Soaps / shampoos
Tinctures (alcoholic solutions)
Powders
Aerosols / foams
Topical patches
What is an occlusive topical formulation?
Occlusive means the formulation prevents water movement out of the body
So an occlusive preparation increases skin hydration and moisture by ‘locking in’ the water present in the body
Enhances skin barrier as forms a shield on skin
Good for dry skin
However, bad for infected skin
What are ointments?
What are the 2 types of ointments for the skin?
Semisolid preparations intended for external application to the skin or mucous membranes
2 types:
Hydrocarbon ointments which aren’t water soluble
Water soluble
Hydrocarbon ointments
What are the most common oils used?
Soft paraffin is the most common ingredient
Liquid paraffin or hard paraffin is used to thin or thicken the formulation as needed
Hydrocarbon ointments
Soft paraffin hydrocarbon ointments
What 2 types of soft paraffin can be used?
Yellow petrolatum Vaseline (petroleum jelly)
White petrolatum (white petroleum jelly) » has been bleached to remove yellow colour
Hydrocarbon ointments
What other oils can be used in hydrocarbon ointments?
Vegetable oils from plant sources e.g. castor, olive, coconut
Synthetic oils e.g. silicone oils » used as water repellants
Isopropyl myristate » semisynthetic, similar properties to vegetable oil
Hydrocarbon ointments
What can cetostearyl alcohol be used for?
Thickening vegetable oils used in hydrocarbon ointments
Hydrocarbon ointments
Properties of hydrocarbon ointments
Occlusive » forms a physical barrier on the surface of the skin, reducing water loss by preventing evaporation
Emollient » hydrate skin due to moisture accumulation
Skin hydration keeps skin supple
Difficult to remove » cannot be removed with just water
Greasy
Good if drug not stable in water
Hydrocarbon ointments
Example of products
Simple ointment » hard paraffin, soft paraffin, wool fat, cetostearyl alcohol
Plantibase » liquid paraffin gelled with polyethylene
Emulsifying ointment » soft paraffin, liquid paraffin, emulsifying wax
Water soluble ointments
What can water soluble ointments be made from?
Why is this useful?
Polymers e.g. macrogol ointment AKA polyethylene glycol ointment
We can control the length of the polymer to produce whatever type preparation we want
e.g. longer chain polymer = higher melting point of ointment
Can mix short and long chain polymers to produce different ointments with different melting points
Water soluble ointments
Properties of water-soluble ointments
Water soluble
Washable
Non-greasy
Not as occlusive as hydrocarbon ointments so they do not lock water in as well
Water soluble ointments
Examples of products with water soluble ointment bases
Bactroban ointment
» contains mupirocin composed of macrogol 400 and macrogol 3350
» treats skin infections
Iodosorb ointment
» consists of iodine in a macrogol ointment base
» used for wound management
Pastes
What are pastes?
Ointments which have 20-50% solid material
So they are stiffer than ointments
Pastes
What do pastes do?
Provide a good protective barrier as water impermeable
Prevent dehydration
Prevent nappy rash (absorb ammonia from break down of urine)
Pastes
What is nappy rash paste made of?
What are its properties?
Zinc oxide, starch, white petrolatum
Has drying and protective properties
Creams
What are creams
Creams have 2 phases, oil and water
Can either be o/w or w/o
Not as stiff as ointments
Creams
What must creams contain?
Emulsifiers » to keep the droplets suspended
Preservatives » to stop contamination as water is present in creams
Creams
What is the most common formulation of creams containing drugs?
o/w creams
Creams
Advantages of using creams for topical application
Good patient acceptability
Spreads easily
Not as occlusive as ointments » lightweight and lets the skin breathe
For o/w creams, water evaporates to leave a thin film on the skin
Creams
Examples of w/o emulsifiers
Wool fat AKA lanolin » pale, yellow sticky material composed of fatty acid esters of cholesterol and other sterols
Wool alcohols AKA lanolin alcohols » has more cholesterol and less impurities than wool fat
Hydrous wool fat AKA hydrous lanolin » 7 parts wool fat and 3 parts water, softer than wool fat and wool alcohols
Beeswax » contains fatty acid esters and long chain alcohols
Calcium soaps » produced by mixing fatty acid with lime water
Synthetic surface active agents » low HLB
Creams
Examples of o/w emulsifiers
Emulsifying waxes
Emulsifying wax BP » contains sodium laurel sulphate and CSA (1:9)
Cetrimide emulsifying wax BPC » contains cetrimide and CSA (1:9)
Cetromacrogol emulsifying wax BPC » contains cetomacrogol 1000 and CSA (8:2)
Each wax contains cetostearyl alcohol (CSA) and a surface active agent
Synthetic surface active agents » high HLB
Lotions
What are lotions?
Liquids that contain insoluble solids which need to be suspended
Contain more water and are less stiff than creams
Lotions
Why are lotions good topical formulations?
Low viscosity so spread easily and are easy to apply
Dry on skin quickly after application
Lotions
What are the components of calamine lotion?
Where does the pink colour of calamine lotion come from?
Calamine, zinc oxide (solids)
Glycerol » helps to keep the skin moisturised
Phenol » antibacterial agent
Bentonite » a clay which helps to keep the solids suspended in the lotion
Water
Pink colour comes from the iron oxide in calamine
What are liniments?
A lotion with oils
Similar viscosity to lotions but rubbed in with pressure
May contain methyl salicylate or other materials which act to relieve pain and stiffness
What are powders?
Give an example
Applied to the skin for a surface effect
E.g. drying
E.g. lubricating
E.g. for antibacterial or antifungal action
Made of fine particle size powders
E.g. Daktarin powder
What are tinctures / paints?
Give an example
Alcohol based solutions
Used for pre-operative disinfection
E.g. iodine tincture
Gels
What are gels?
Gels are a dispersion of liquid within a solid where the solid is the continuous phase and the liquid is the disperse phase
Usually transparent or translucent
Require a gelling agent
Gels
Examples of natural gelling agents
Tragacanth
Pectin
Alginate
Gels
Examples of synthetic gelling agents
Synthetic polymers e.g. carbomer, cellulose
Gels
What do gelling agents do?
Forms a cross-linked network in the liquid
Allowing the dispersion of the liquid within the solid
Gels
What are hydrogels?
Gels which are mostly water
Formed by a hydrophilic polymers gelling in water
Gels
What are carbomer gels?
Known for their stability, meaning they maintain their consistency and properties over time with minimal degradation
Made up of carboxy vinyl polymers » in water, they form a low viscosity dispersion with an acidic pH
When the dispersion is neutralised by adding an alkali, a gel is formed
Types of neutralising agents:
Triethanolamine » used when formulation is water-based
Diisopropranolamine » used when formulation contains alcohol
Gels
Examples of topical gels
Ibugel
Isotrexin gel
What are topical patches?
Example?
Hydrogel with a backing layer
E.g. Lidocaine to treat postherpetic neuralgia
What are collodions?
Example?
Sticky liquid which dries to a film
Used as a skin protectant
» applied to skin to close small wounds, abrasions, cuts
» keeps medications in contact with skin
E.g. Salactol to treat warts
What is the best topical formulation for sunscreens and why?
Sunscreens must stay largely on skin surface
So ointments too occlusive
Gels, sprays, creams and lotions preferred
What is the best topical formulation for anti-fungal drugs and why?
Fungal infections reside in the stratum corneum
So anti-fungal drugs must be localised on the outer layers of the skin not in deeper layers
So ointment not appropriate
Gels, sprays, creams and lotions preferred
What is the best topical formulation to treat inflamed skin and why?
Inflamed skin associated with problems in skin barrier
Ointments preferred
What is the difference between transdermal delivery and topical delivery?
Transdermal delivery aims to get the drug into the bloodstream whilst topical delivery does not
Transdermal delivery avoids problems associated with oral delivery e.g. break down in stomach and gut
What is a transdermal patch?
Examples of drugs administered by patch and the corresponding transdermal patch name
Adhesive patch placed on the skin to deliver medicine all the way through the skin and into the bloodstream
Drugs administered via patch:
Fentanyl » Transiderm-nitro
Nicotine » Nicotinell
Nitroglycerine » Durogesic
Estradiol » Estraderm
Testosterone
Examples of transdermal gels
Testogel
Oestrogel
Limitations of transdermal patches or transdermal gels
The skin is a good barrier and large amounts of drug cannot permeate
Maximum attainable flux across the skin important to make sure not to exceed maximum daily dose