Operative - (on written exam 3) Liners and Bases
1/80
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
81 Terms
T or F: the pulp has no way of protecting itself from damage caused by irritants
FALSE
- The pulp has inherent defense mechanisms to limit damage from irritants
specialized cells located at the outermost layer of the dental pulp, forming a continuous layer along the predentin-pulp boundary are known as
odontoblasts
what extends a cellular process into a corresponding dentinal tubule?
odontoblasts
what cells are responsible for the production and modification of the dentin matrix, including collagen fibers as long as a tooth remains viable?
odontoblasts
what materials have traditionally beenused to protect the pulp and support restorations?
bases and cavity liners
T or F: there is no risk of pulpal irritation associated with most dental procedures
FALSE
- Most restorative procedures introduce some degree of pulpal irritation
what is the natural protector of the pulp?
dentin
the following is the role of what tooth substance?
buffers cariogenic acids and insulates the pulp from thermal changes during cavity preparation
dentin
what is the most effective way to maintain pulpal health?
Preserving as much natural tooth structure as possible is more critical for pulpal health than simply replacing lost structure with liners or bases
what group has a higher risk of pulp exposure? Why?
young patients
- Due to the larger pulp chamber and thinner overlying dentin, especially in deep carious lesions
what consequence of aggressive caries removal can quickly lead to pulp exposure?
minimal remaining dentin thickness
in older patients, what lowers the risk of pulp exposure? How/Why?
Secondary and tertiary dentin formation reduces the size of the pulp chamber and thickens the dentin walls
between younger and older patients, who has the more predictable margin for excavation?
older patients
- But also reduced pulp vitality and reparative capacity
between younger patients, who has the higher chance of pulp vitality and reparative capacity?
younger patients
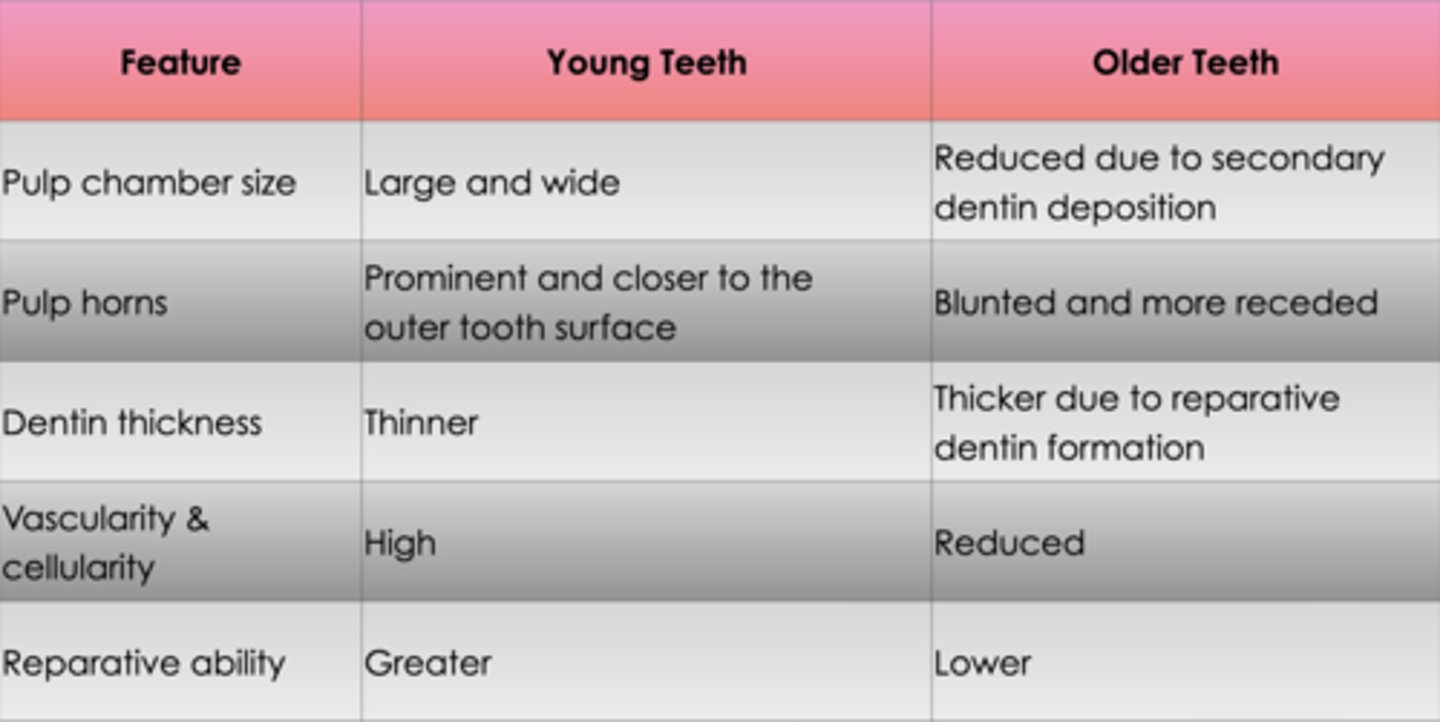
compare tooth physiology/composition between young teeth and older teeth
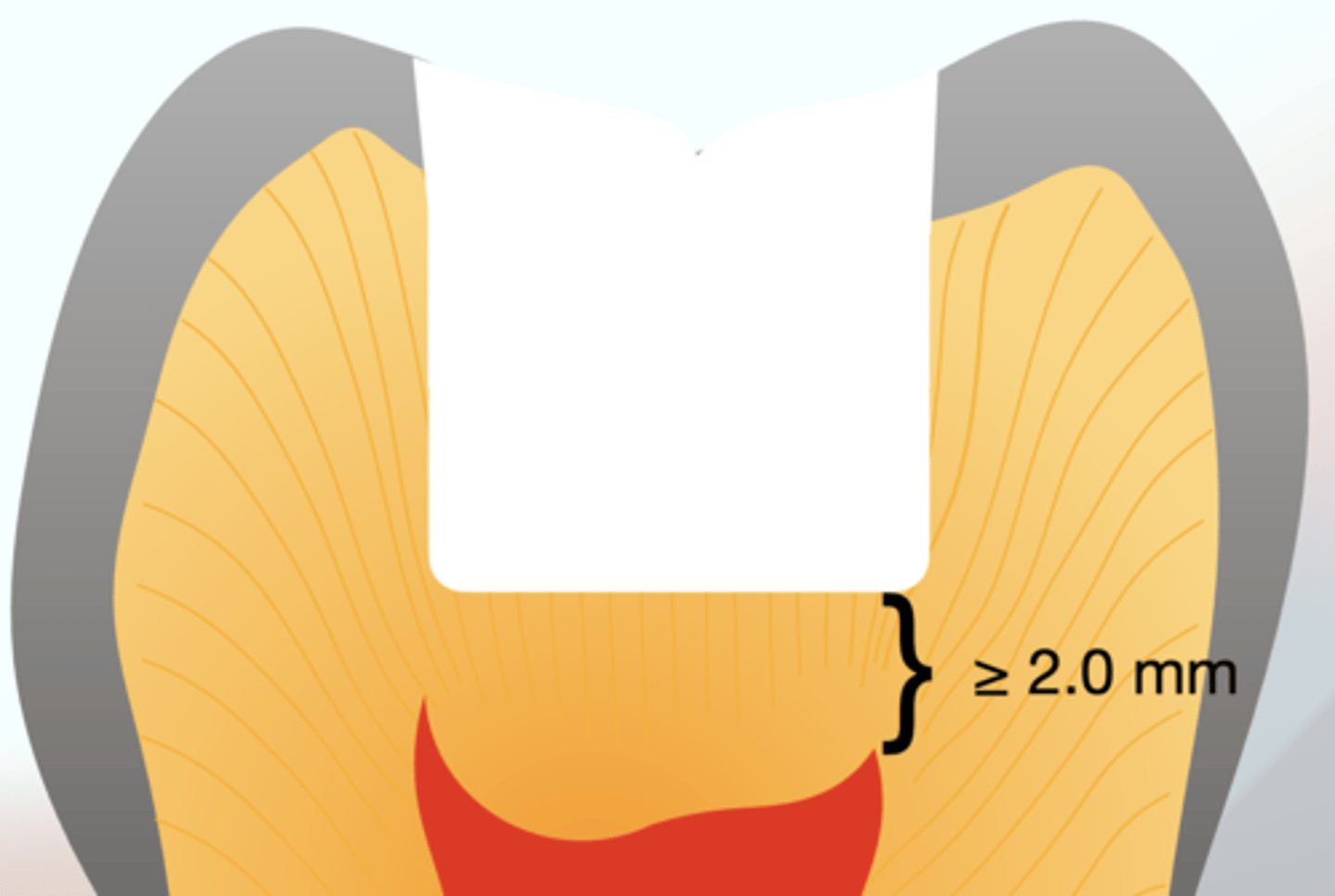
what remaining dentin thickness (RDT) generally results in little to no pulpal reaction
greater than 2.0mm
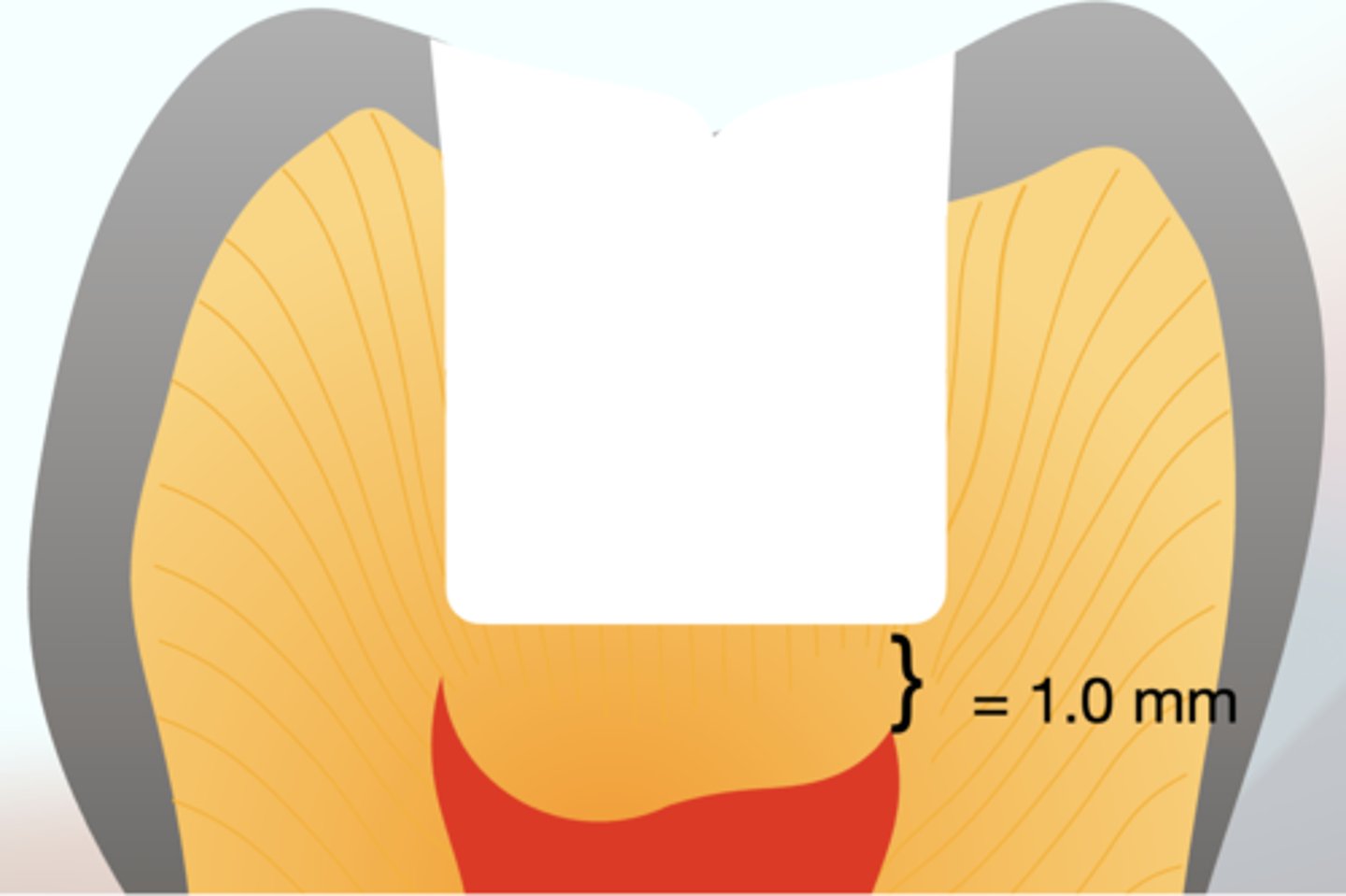
what remaining dentin thickness (RDT) provides about a 90% reduction in toxin impact?
1 mm of dentin
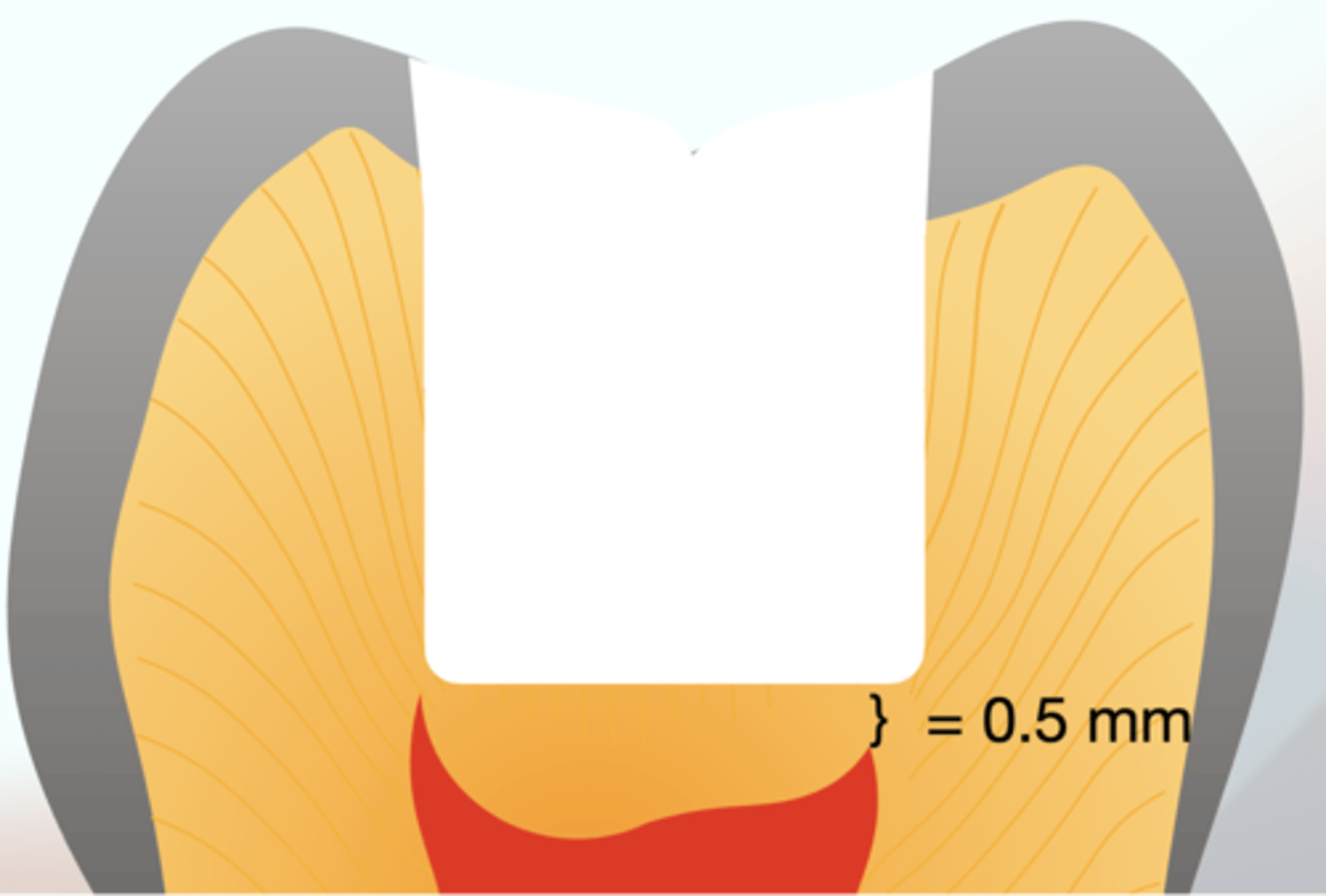
what remaining dentin thickness (RDT) reduces the effect of toxic substances by approximately 75%?
0.5 mm of dentin
how does the pulp respond to irritants (from caries or restorative procedures)?
inflammation
what is the primary culprit of pulpal inflammation?
bacterial invasion
T or F: only advanced dentinal caries elicit a pulpal response
FALSE
- Even early enamel caries, especially those that progress rapidly, can lead to a mild pulpal response due to increased permeability of enamel.
as caries penetrate deeper, what happens to the pulp?
the severity of pulpal inflammation increases
what can happen once bacteria reach the pulpal chamber?
severe inflammation or even pulpal necrosis can occur
what does the pulp do in response to offense by caries?
The caries process stimulates the formation of reparative dentin and reactive dentin sclerosis, both of which help bolster the natural protective barrier provided by dentin
T or F: only high speed instruments induce pulpal inflammation
FALSE
- High- and low-speed rotary instruments can induce pulpal inflammation due to friction and desiccation
what are key factors to minimizing adverse effects of rotary instruments on pulpal response?
▪ Water spray is critical to prevent excessive heat buildup
--- Use adequate air-water coolant spray.
▪ Friction control reduces thermal damage ---Light pressure & sharp burs minimize trauma.Diamond burs generate more heat than carbide burs.
▪ Deep cavity preparations & full-coverage restorations increase pulpal necrosis risk
---Preserve as much tooth structure as possible
inflammation increases what sensation in the pulp, affecting nerve endings?
intrapulpal pressure
what theory theory explains non-inflammatory sensitivity due to fluid movement in dentinal tubules?
hydrodynamic theory
what does the hydrodynamic theory explain?
non-inflammatory sensitivity due to fluid movement in dentinal tubules
initial concerns about metallic restorations causing ______ _______ led to cavity base placement.
thermal shock
which restorations are more prone to sensitivity?
deeper restorations with higher dentinal tubule density
what has been traditionally places beneath restorations to reduce thermal conductivity?
base or liner no thicker than 0.75 mm
A base or liner no thicker than 0.75 mm has traditionally been placed beneath restorations to reduce thermal conductivity; however, in the case of amalgam restorations, what must be considered?
thicker bases may compromise their mechanical strength
Bases and cavity liners have traditionally been used to do what?
protect the pulp and support restorations
what is an endodontic treatment aimed at preserving the vitality of the pulp?
pulp capping
what conditions must be met for a successful pulp capping outcome?
✓The pulp must be vital with no history of spontaneous pain.
✓Pain elicited by thermal stimuli should not persist after stimulus removal.
✓Periapical radiographs should show no signs of periradicular pathology.
✓The restoration must effectively seal the site to prevent bacterial contamination.
when is indirect pulp capping preferred over direct pulp capping?
when the following conditions are met:
✓The pulp must be vital with no history of spontaneous pain.
✓Pain elicited by thermal stimuli should not persist after stimulus removal.
✓Periapical radiographs should show no signs of periradicular pathology.
✓The restoration must effectively seal the site to prevent bacterial contamination.
T or F: indirect pulp capping requires no further monitoring after placment
FALSE
- pulp vitality should be monitored for several months, especially in cases involving abutment teeth for prosthetic restorations
when is direct pulp capping indicated?
Used when pulp exposure occurs due to trauma, caries,or mechanical factors
when is direct pulp capping more successful?
when the exposure is mechanical rather than carious, as carious exposures introduce bacterial contamination, leading to inflammation and reduced healing potential
what is the goal of direct pulp capping?
promote healing, induce reparativedentin formation, and avoid root canal therapy
what must be done after placing a direct pulp cap?
A well-sealed restoration must be placed to prevent future bacterial infiltration.
what are consequences of uncontrolled pulpal bleeding in a capping procedure?
• Indicate a higher level of pulpal inflammation, reducing healing potential.
• Compromise the bacterial seal necessary for successful pulp capping
what are common hemostatic agents used in pulp capping?
• Water or saline - Least harmful to pulp tissues.
• Sodium hypochlorite (0.12%-5.25%) - Highly effective for both hemostasis and disinfection but can be caustic.
• Chlorhexidine - Strong antibacterial properties but less effective at controlling hemorrhage
when is an indirect pulp capping procedure recommended
when a deep caries lesion is encroaching on the pulp in a tooth with no history of spontaneous pain and a normal response to vitality tests
what dentin should be removed and what dentin should be left in an indirect pulp cap?
Soft, wet carious dentin should be removed, leaving only dry, fibrous, moderately resistant dentin near the pulp.
what is critical for success of an indirect pulp cap?
a well-sealed restoration
what are thin layers (≤0.5 mm) placed in dental preparations to provide therapeutic benefits such as fluoride release, dentinal sealing through adhesion, and antibacterial action that promotes pulpal health?
cavity liners
what is the goldstandard of direct pulp capping materials?
calcium hydroxide
why has calcium hydroxide long been used as a liner?
due to its pulpal compatibility and ability to assist in reparative dentin formation
the traditional belief of calcium hydroxide has been that it stimulates dentin formation, what does recent research suggest?
that its antibacterial properties help reduce inflammation, indirectly supporting healing
- Additionally, it may release growth factors from dentin, further aiding pulpal recovery.
T or F: Dycal is moisture tolerant
FALSE
- Dycal is not moisture-tolerant and requires a dry field for proper placement. It does not adhere well to moist tooth structures, and exposure to saliva or blood can result in washout or displacement
conventional calcium hydroxide liners have poor physical properties, including high solubility, which can lead to:
• Material degradation, compromising long-term effectiveness.
• Bonding resin contamination, increasing marginal leakage.
at what remaining dentin thickness is calcium hydroxide indicated?
less than 0.5 mm
- can be used as an indirect or direct pulp cap
why should calcium hydroxide liners ALWAYS be covered with an RGMI base?
to seal the area and preventing the etchant (applied later) from dissolving the liner
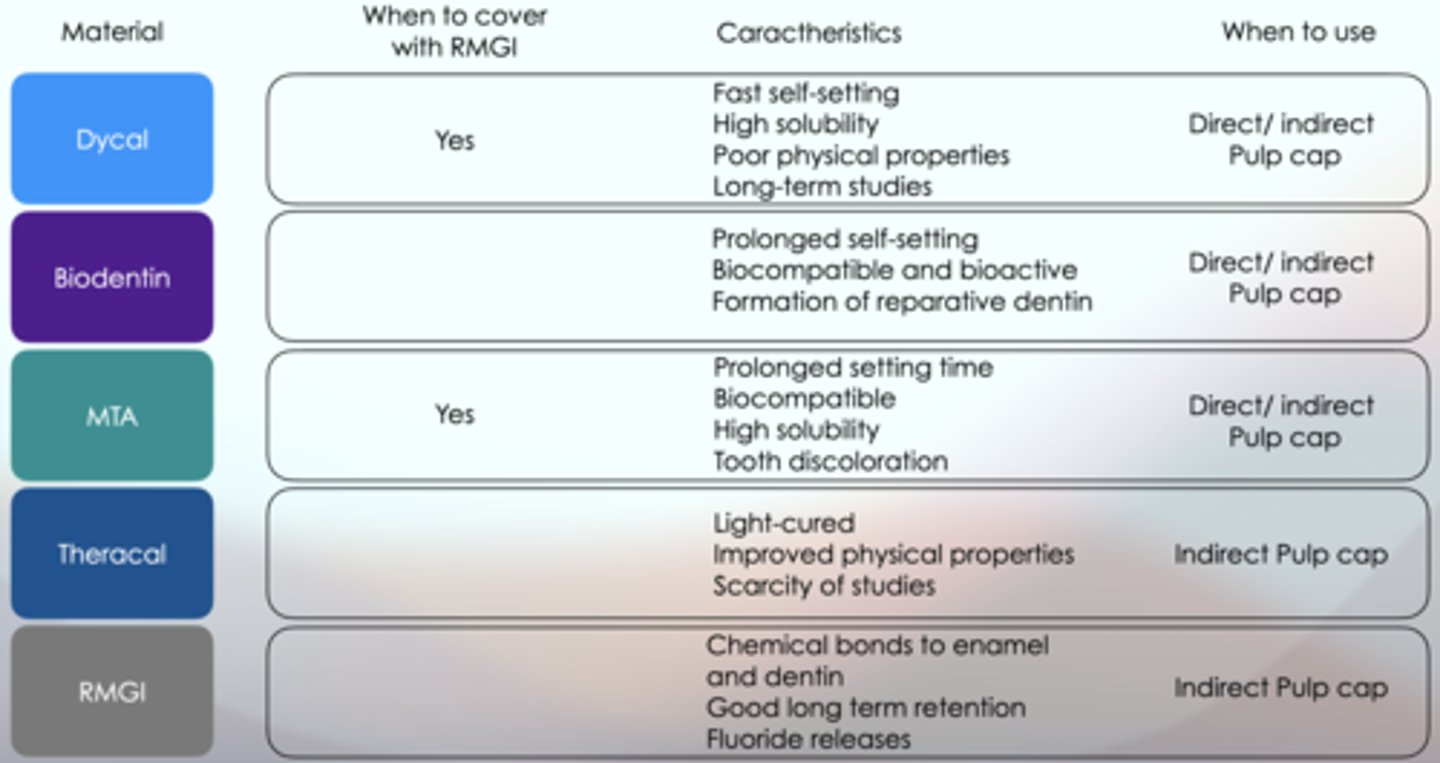
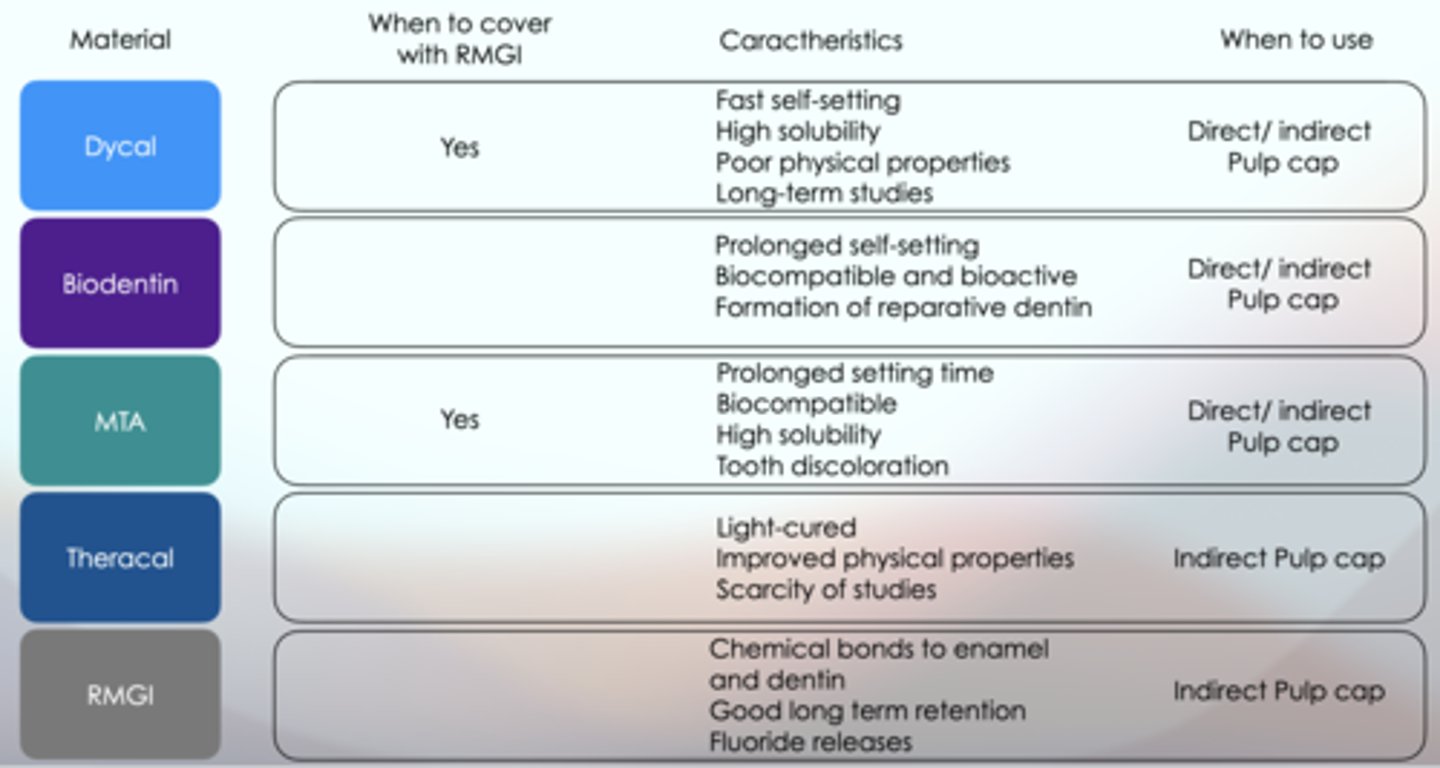
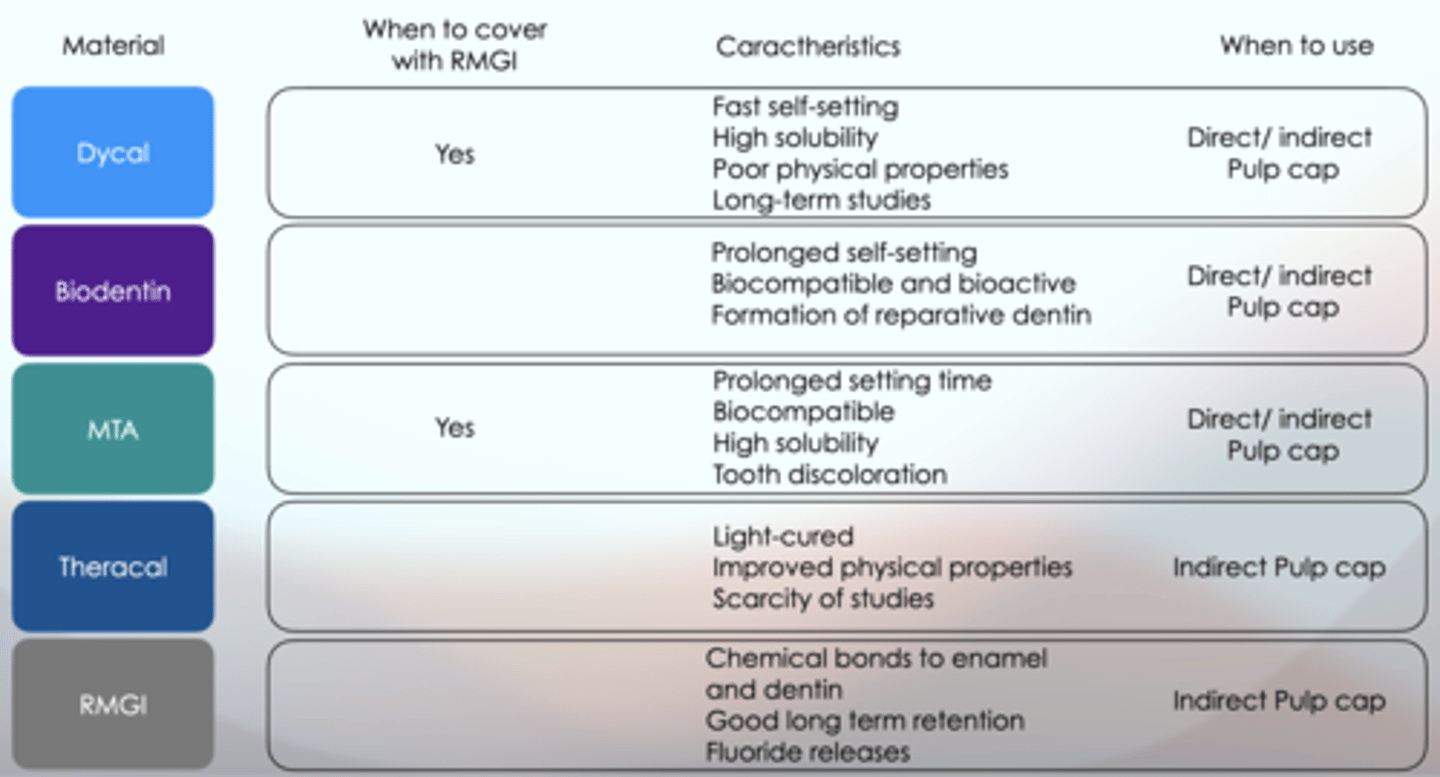
which liners discussed should ALWAYS be covered with an RGMI base?
which liner is a light-cured resin-modified calcium silicate-filled liner, that performs as a barrier and protectant of the dental-pulpal complex?
TheraCal
the following describes which liner?
Calcium release stimulates hydroxyapatite and secondary dentin bridge formation and the alkaline pH that it generates promotes healing and apatite formation
TheraCal
TheraCal and Dycal are both liners but one is more tolerant to moisture than the other. Which is more tolerant to moisture?
TheraCal LC is moisture tolerant and radiopaque for placement under restorative materials and cements
what is a significant limitation concerning TheraCal?
the scarcity of clinical studies available in the literature,which restricts our ability to draw definitive conclusions regarding long-term outcomes, efficacy, and comparative performance in real-world settings
at what remaining dentin thickness is use of TheraCal indicated?
less than 0.5 mm
Does TheraCal have to be covered with an RMGI base?
NO
What liners can be used as a direct AND indirect pulp cap?
- Dycal
- Mineral Trioxide Aggregate (MTA)
- BioDentin
MTA success may be attributed to...
its calcium hydroxide release and its capacity to provide a sealat the pulp exposure site
what liner discussed is comparable to calcium hydroxide?
mineral trioxide aggregate (MTA)
- MTA has gained interest as a direct pulp capping agent, as it shares similarities with calcium hydroxide (Human studies show comparable or superior performance to calcium hydroxide), including antibacterial properties, biocompatibility, and bioactive dentin matrix protein release
advantages of using MTA:
✓Biocompatible silicate cement with antibacterial properties.
✓Provides a better seal than calcium hydroxide and promotes pulpal healing.
disadvantages of using MTA:
๏High solubility
๏Prolonged setting time
๏Tooth discoloration (in gray MTA)
๏Higher cost
which liner is a bioactive, tricalcium silicate-based dental material developed as a dentin substitute for various restorative and endodontic procedures. It is designed to mimic the properties of natural dentin and promote healing of the dental pulp?
Biodentin
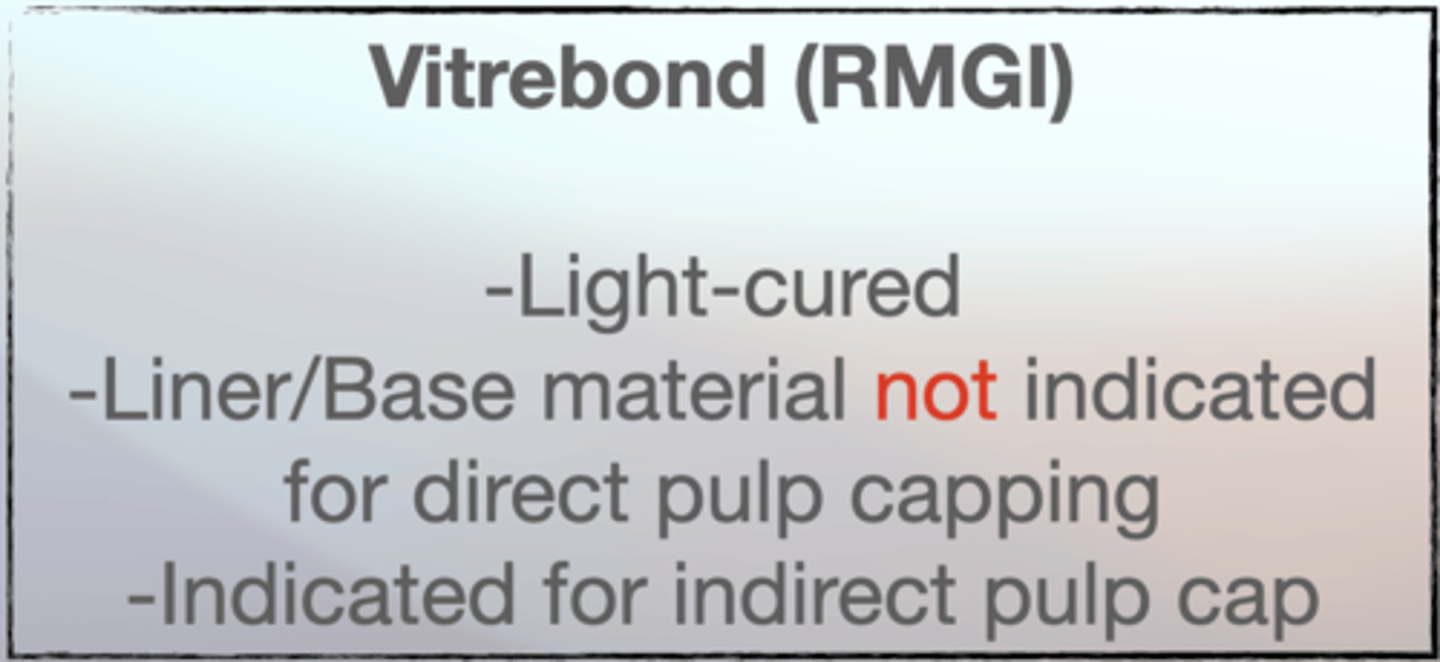
which liners discussed can ONLY be used as an indirect pulp cap?
- TheraCal
- RMGI
what liners does the following describe?
- powder component primarily consists of tricalcium silicate, dicalcium silicate, calcium carbonate, and zirconium oxide, while its liquid contains calcium chloride and a water-reducing agent.
- This composition contributes to its biocompatibility and bioactivity, allowing it to induce the formation of reparative dentin and support pulp vitality.
BioDentin
what liners are widely used due to their chemical bond to tooth structure and fluoride release, which helps prevent recurrent caries (fluoride is released during the acid-base reaction and then to the oral cavity over time but not indefinitely)?
Glass ionomer
T or F: once fluoride release diminishes from glass ionomer liners, there is no further fluoride release benefit
FALSE
- Though fluoride release diminishes over time,"recharge" with fluoride when exposed to fluoride, contributing to long-term anticariogenic effects
• However, not all clinical trials have confirmed the ability of GIC to prevent secondary caries.
• Some studies also suggest that GIC may not be more effective than other non-fluoridated materials like composites
What liners MUST be covered with an RGMI base?
- DyCal
- MTA
what is the remaining dentin thickness for resin-modified glass ionomer liners?
between 0.5 and 1.5mm
Vitrebond:
what are dentin-replacement materials mainly used to block undercuts or reduce the volume of restorative material. They are not primarily for pulpal protection but provide structural support
cavity bases
the following are characteristic of what base?
✴Excellent mechanical properties and modulus of elasticity.
✴Provides both cavity base and liner functions.
✴Offers restoration support and fluoride release.
✴Compatible with resin composite material.
glass ionomer
remaining dentin thickness range for glass ionomer base
0.5-1.5 mm
remaining dentin thickness range for zinc oxide-eugenol base
0.5-1.5 mm
the following are characteristics of what base?
✴Historically used for their thermal insulation properties.
✴Zinc phosphate cement offers excellent physical properties.
✴Their use has declined due to concerns about pulpal health and the emergence of fluoride-releasing materials.
✴Eugenol, a component of the base, has been reported to interfere with the polymerization of resin composites,potentially compromising the bond strength between the composite and dentin.
which base discussed has been known to interfere with polymerization of resins?
Zinc Oxide-Eugenol (ZOE)