Clinical Oncology - Gastrointestinal: Colorectal Cancer
1/72
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
73 Terms
Describe the epidemiology of colorectal cancer
Third most common cancer in men and women, and second leading cause of cancer related death in the US
What sex is colorectal cancer more common in?
Men
What is the common age of diagnosis?
More than 90% of cases occur in those 55 years old and older, however, the incidence rate is increasing in those younger than 50 years old
Why have death rates for colorectal cancer been declining?
Due to early detection and better treatment
What is one of the main etiological factors in colorectal cancer?
Diet high in animal fat and low in fibre
How does fibre play a role in reducing risk for colorectal cancer?
Fibre can dilute fecal contents and increase fecal bulk, so there is faster removal, minimizing exposure of epithelial lining to carcinogens
What are other risk factors for colorectal cancer?
Obesity, smoking, alcohol, type 2 diabetes, minimal physical activity, chronic ulcerative colitis, familial adenomatous polyposis (FAP), Lynch syndrome/hereditary nonpolyposis colorectal cancer (HNPCC), family history
What is chronic ulcerative colitis?
Inflammation of bowel wall and ulcerations. Usually occurs in rectum and sigmoid colon, but can spread to rest of colon.
What is familial adenomatous polyposis (FAP)?
Growths that arise from mucosal lining and protrude into bowel lumen. It causes hundreds of polyps in the bowel and if left untreated, always turns to colorectal cancer.
What is Lynch syndrome?
Frequent occurence of colorectal cancer in families without polyposis. Usually causes right sided colon cancers at a younger age. They have higher risk for second cancer of colon, and adenocarcinoma of breast, ovary, endometrium, pancreas.
What is a major factor in colorectal cancer that determines treatment and prognosis?
If lesion is located retroperitoneal or intraperitoneal
What are the divisions of the colon?
Cecum, ascending colon, hepatic flexure, transverse colon, splenic flexure, descending colon, sigmoid colon, rectum
What sections of the colon are located intraperitonealy?
Cecum, transverse colon, sigmoid colon
Describe intraperitoneal organs
Organs are covered by the peritoneum and have a complete mesentery and serosa; they are freely mobile
Describe lesions that are located intraperitonealy
It can be surgically removed with adequate margins unless tumour is adherent or invades adjacent structures. Treatment failure or recurrence is likely due to peritoneal seeding.
What sections of the colon are located retroperitonealy?
Ascending and descending colon, hepatic and splenic flexures
Describe retroperitoneal organs
Lack true mesentery and serosal layer on posterior and lateral portion
What location of colorectal lesions are likely to spread more often?
Lesions that are located retroperitonealy, as they lack a mesentery and serosal layer - early spread and invasion of soft tissues, kidneys and pancreas is common
Which section of the rectum is retroperitoneal?
Lower two thirds
Which section of rectum is covered by peritoneum?
Upper lateral and anterior surfaces
What are the layers of the large bowel?
Mucosa
Submucosa
Muscularis propria
Serosa *not all segments of colon have serosa; formed by visceral peritoneum
What is the mucosa?
Inner lining of digestive tract and forms lumen of bowel, and it has two supporting layers - the lamina propria and muscularis mucosa
What is the submucosa?
It is rich in blood vessels and lymphatics
What is the muscularis propria?
It has two muscle layers - circular and longitudinal for peristalsis
Describe the lymphatics of the right colon
Follows superior mesenteric nodes, including ileocolic and right colic nodes
Cecum & Appendix: cecal
Ascending Colon: ileocolic, right colic, middle colic
Hepatic Flexure: right and middle colic nodes
Transverse Colon: middle colic nodes
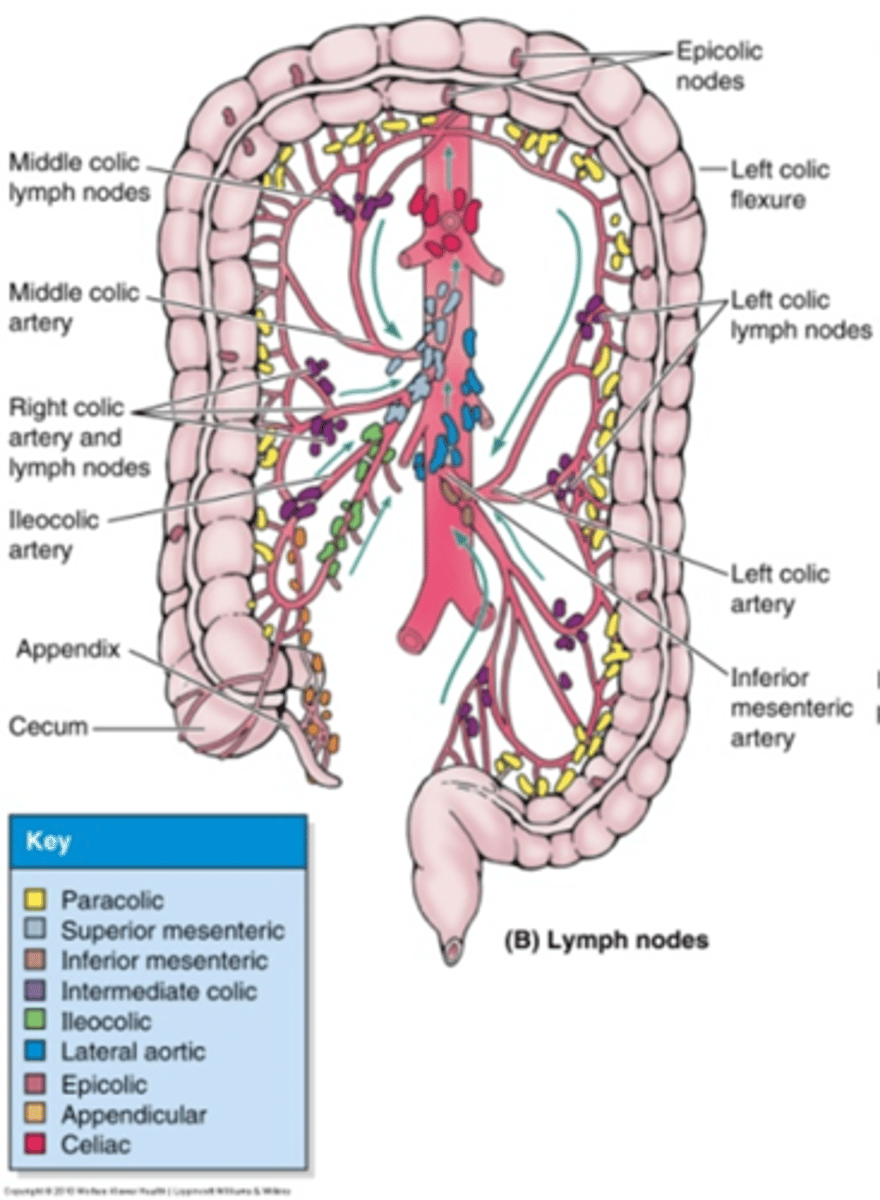
Describe the lymphatics of the left colon
Splenic Flexure: middle and left colic
Descending Colon: left colic, inferior mesenteric, sigmoid
Sigmoid Colon: sigmoidal, superior hemorrhoidal, superior rectal, inferior mesenteric
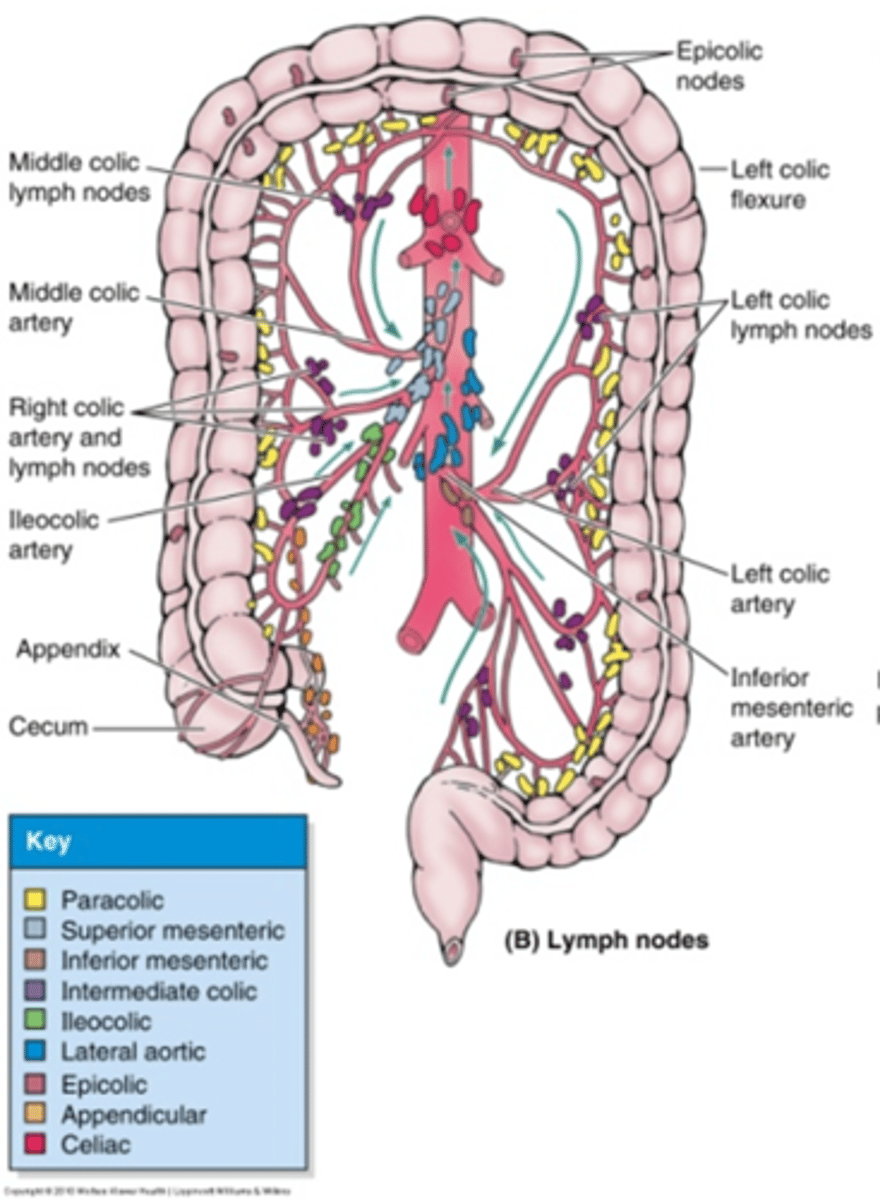
Describe the lymphatics of the rectum
Upper rectum drains to inferior mesenteric lymph nodes. Middle and lower rectum drain to internal iliac lymph nodes. Other lymph nodes at risk of involvement include perirectal, lateral sacral, and presacral nodes.
Low rectal lesions that extend to anal canal can drain to inguinal nodes.
Invasion of vagina or prostate can result in spread to external iliac nodes.
What is the clinical presentation of rectal cancer?
Usually have hematochezia (rectal bleeding). Other signs and symptoms include changes in bowel habits, diarrhea, constipation, change in stool caliber.
What signs and symptoms may be present in a lesion in the rectal valve?
Pencil thin stools, constipation or diarrhea
What can indicate locally advanced rectal cancer?
Tenesmus, which is spasms of rectum accompanied with desire to empty bowel
What can occur with tumours extending posteriorly?
Pain the buttock or perianal area
What are signs and symptoms of colon cancer?
Dark or black coloured stools, changes in bowel habits, diarrhea or constipation
What are signs and symptoms of a lesion in the left colon?
It is similar to rectal cancer; blood in stool, change in stool caliber, obstructive symptoms, abdominal pain
What are signs and symptoms of a lesion in the right colon?
Abdominal pain, often accompanied by an abdominal mass
What is the screening for colorectal cancer?
Age: 50 years old
Fecal occult blood test or fecal immunochemical test every 1 to 2 years
Fecal immunochemistry test-DNA every 3 years
Sigmoidoscopy, CT colonography, double contrast barium enema every 5 years
Colonoscopy every 10 years
*Colonoscopy should follow any positive test results
What is the most common pathology of colorectal cancer?
Adenocarcinoma (90-95%)
Describe the direct and lymphatic spread of colorectal cancer
Direct: radial manner into bowel wall
Lymphatic: occurs if tumour invades submucosa; 50% of patients have nodal involvement at time of diagnosis
What is another method of spread besides direct extension, lymphatics, and via blood?
Peritoneal seeding, which is caused when tumour grows through bowel wall and onto peritoneal surface, resulting in tumour cells shedding into abdominal cavity
What are the common sites of distant spread?
Liver, the most common, via portal vein
Lung, via a tumour embolus into inferior vena cava
What is the treatment of choice in colorectal cancer?
Surgery, in which the tumour, an adequate margin, and lymphatics are removed
Describe the treatment for stage 1 colon cancer
Surgery
What is involved in surgery for colon tumours?
Right or left hemicolectomy, which involves removal of large segment of bowel, adjacent lymph nodes, immediate vascular supply
Describe the treatment for stage 2 colon cancer
Surgery, followed by chemotherapy for high risk colon cancer, T4 lesions, spread to lymph nodes or blood vessels, obstruction, perforation, etc
Describe the treatment for stage 3 colon cancer
Surgery, and is usually followed by chemotherapy
Radiation therapy is not a common treatment because colon cancer usually does not spread locally - if it spreads, it is more likely to distant organs
What surgical procedures are common in rectal cancer?
Lower anterior resection (LAR) and abdominoperineal resection (APR)
Describe the lower anterior resection procedure
Removal of tumour plus a margin and adjacent lymph nodes. The bowel is re-anastomosed, so a colostomy is not necessary.
Used in colon and upper and middle rectal cancers
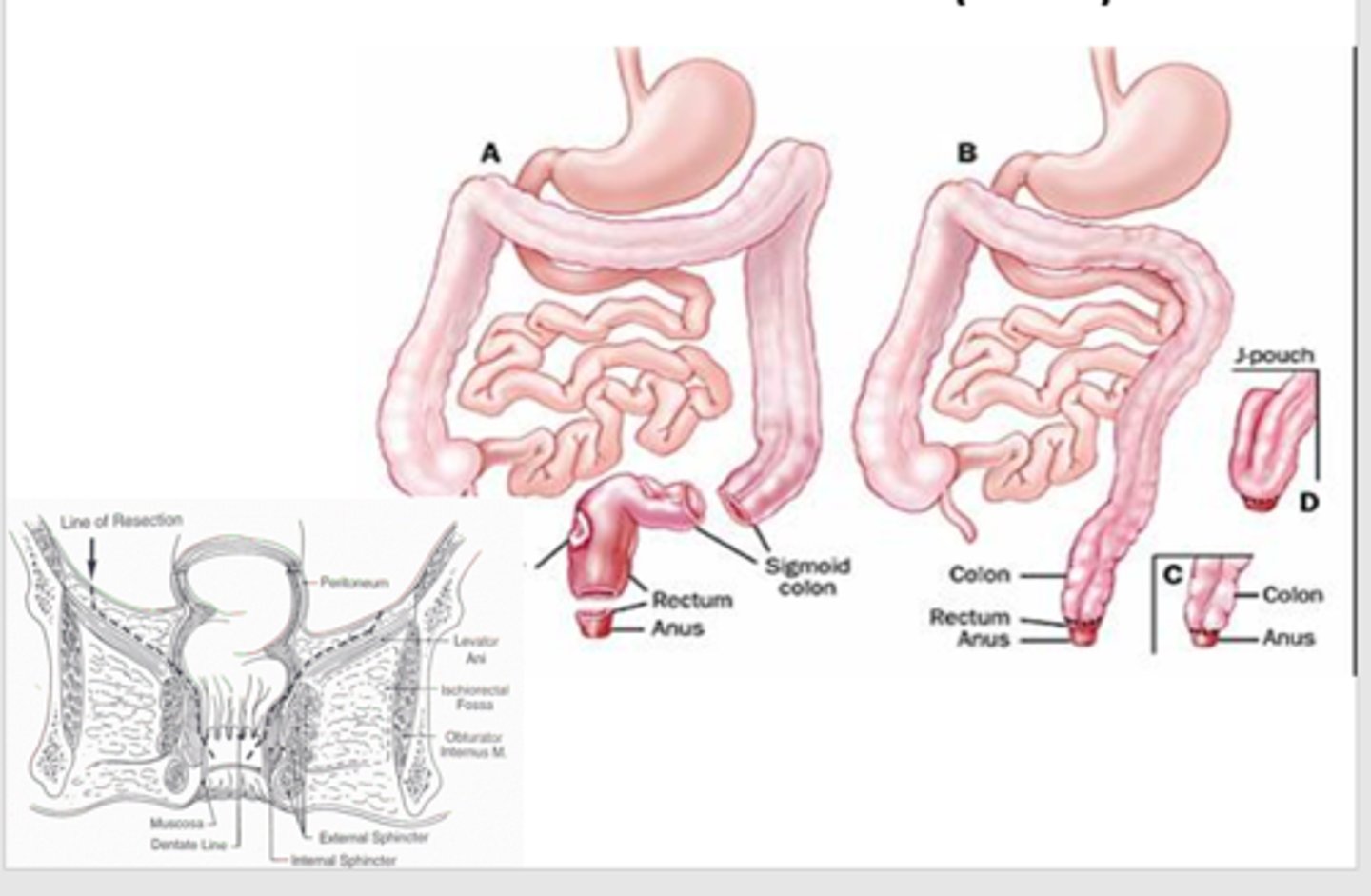
When is the abdominoperineal resection (APR) procedure done?
For lower third (distal 5 cm) rectal lesions
Describe the abdominoperineal resection (APR) procedure
Anterior incision is made in abdominal wall to make a colostomy, and a perineal incision is made to resect rectum, anus, and lymphatics. The pelvic floor is reconstructed with a mesh, peritoneum or omentum.
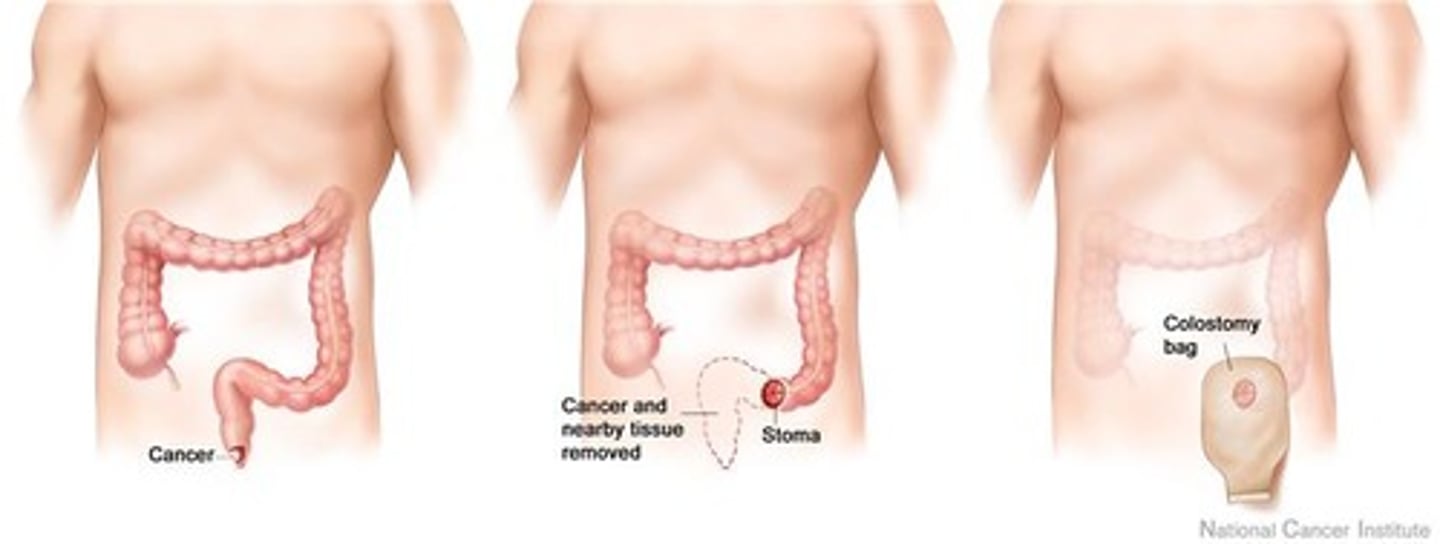
In an abdominoperineal resection (APR), why is reperitonealization of the pelvic floor important?
It displaces the small bowel superiorly, reducing the amount of small bowel in the treatment field, which minimizes side effects in post-op patients
Describe the treatment for stage 1 rectal cancer
Surgery
Describe the treatment for stage 2 and 3 rectal cancer
Surgery
Radiation therapy is almost always offered, either alone or with chemotherapy; may be before or after surgery
Chemotherapy may be offered alone after surgery, or with radiation therapy before or after surgery
*Chemoradiation + Surgery (most common) OR Surgery + Chemoradiation
RT + Surgery OR Surgery + RT
Surgery + Chemotherapy
What is an advantage of post-operative radiation therapy in rectal cancer?
Pathological information of tumour extent and nodal involvement is available, which helps in determining if adjuvant treatment is needed
What is a disadvantage of post-operative radiation therapy in rectal cancer?
Can have hypoxia (more radioresistant) due to disrupted blood supply from surgery
When is pre-operative chemoradiation done in rectal cancer?
Locally advanced rectal cancers (T3, or N1/2)
What is the goal of pre-operative radiation therapy in rectal cancer?
Preservation of sphincter. Chemoradiation shrinks tumour so LAR is done instead of APR, sparing a colostomy.
What are the advantages of pre-operative radiation therapy in colorectal cancer?
Down staging of tumour reduces risk of seeding during surgery
Increased radiosensitivity of oxygenated cells in nonoperative pelvis
Increase in local control
Less acute side effects
What are disadvantages of pre-operative radiation therapy in colorectal cancer?
No pathological tumour staging (T)
Can affect post-surgical healing due to side effects of radiation
Where do most recurrences occur in rectal cancer?
Posterior pelvis; metastases to internal iliac and pre-sacral nodes
Which nodes are included in the radiation fields for rectal cancer and why?
Internal iliac and pre-sacral nodes, as they are not resected during a standard surgery
How is small bowel dose reduced?
Patient positioning, bladder filling, dosimetric weighting, gantry arrangements
Why is small bowel more easily reduced in pre-operative than post-operative radiation therapy?
In post-operative radiation, the rectum and peritoneum are removed, which allows small bowel to be displaced more inferiorly
What doses are used for colorectal cancer?
Colon: 5040 cGy/28#
- 4500 cGy/25# to nodes
- Boost: 540 cGy/3#
Rectum (N-): 2500 cGy/5# followed by surgery in 1 week
Rectum (N+): 5040 cGy/28#
- 4500 cGy/25# to nodes
- Boost: 540 cGy/3#
- Surgery 5 to 12 weeks if pre-op
What radiation therapy conventional techniques were used for colorectal cancer?
3-Field: no anterior field to reduce dose to small bowel
4-Field: used when anterior structures, such as vagina and prostate are involved or at risk of involvement
Describe the field borders of radiation therapy for colorectal cancer
Superior: 1.5 cm superior to S1/L5 or up to L4/5 to para-aortic nodes
Inferior: include obturator foramen; 3 to 5 cm beyond tumour (pre-op) or below most distal extent of dissection (post-op)
Lateral: 2 cm lateral to pelvic brim, encompassing iliac lymph nodes
Posterior: 1.5-2 cm behind sacrum
Anterior: anterior edge of femoral heads to ensure coverage of internal iliac nodes; if anterior structure (prostate or vagina) is involved, field includes pubic symphysis for external iliac nodes
What is the dose-limiting structure for the treatment of ascending and descending colon?
Kidney and small bowel
What is an advantage and disadvantage of VMAT?
Advantage: sparing more healthy tissue, dose conformity to PTV
Disadvantage: more tissues are exposed to low dose radiation
What can be done prior to CT Sim/treatment in colon cancers to reduce dose to dose-limiting structures?
Contrast studies to assess kidney function and localization to ensure adequate sparing of at least 1 kidney
What are the acute side effects of radiation for colorectal cancer?
Diarrhea, abdominal cramps, bloating, proctitis, bloody or mucus discharge, dysuria, leukoplakia, thrombocytopenia
What are chronic side effects of radiation for colorectal cancer?
Persistent diarrhea, increased bowel frequency, proctitis, fistula, urinary incontinence, bladder atrophy
What are the most common long-term complications for radiation for colorectal cancer?
Damage to small bowel that results in enteritis, adhesions and obstruction
How can surgeons work with radiation oncologists to limit dose to surrounding structures?
Place clips to highlight tumour bed, which allows radiation oncologist to outline area at risk instead of requiring a more generous treatment volume
What foods should patients experiencing enteritis avoid? What are recommended foods?
Avoid: whole grains, fried and fatty foods, milk products, raw vegetables
Recommended: white bread, bananas, apples, cooked vegetables
What reactions may occur with the 3-field radiation technique in colorectal cancer?
Skin reactions on perineum, such as erythema to moist desquamation