OB33: Introduction to Radiology OB34: Radiological Science
1/134
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
135 Terms
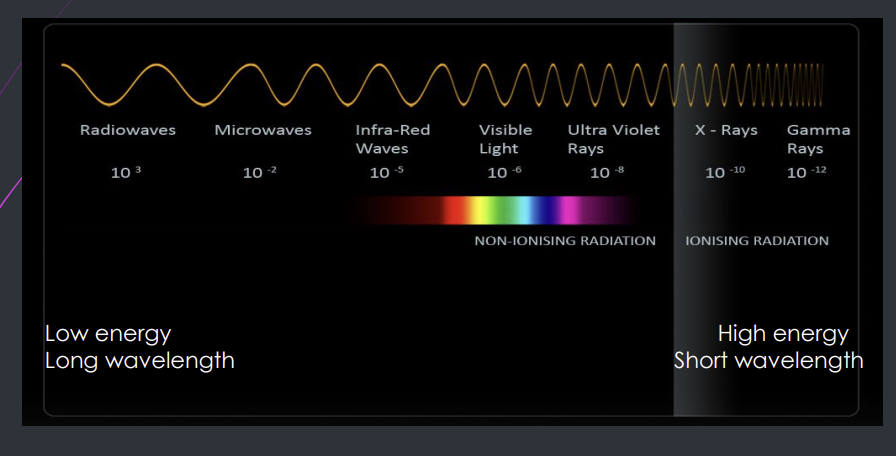
Where will you find x rays and describe its energy, frequency and wavelength
electromagnetic spectrum
high energy
short wavelength
high frequency
who discovered X rays?
wilhelm conrad roentgen
What does ionisation mean?
the process by which atom or a molecule acquire a negative or positive charge by gaining or losing electrons
What does ionising radiation mean?
radiation that caries sufficient amount of energy to detach electrons from atoms
Why are X rays and gamma rays in the ionising radiation category?
they are energetic enough to free electrons from atoms causing ionisation
What are X rays?
packet of energy, each packet is called a photon
Each x-ray beam is made from?
millions of individual photons
What is the speed of photons?
constant speed of light in a vacuum
How do X-rays travel?
straight line
Can X rays be detected by humans?
no
How are X-rays produced?
high speed energetic electrons bombard the target material and are brought to rest by sudden deceleration which results in emission of X rays photons
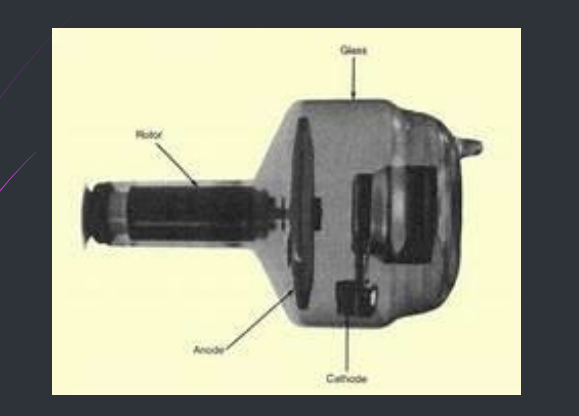
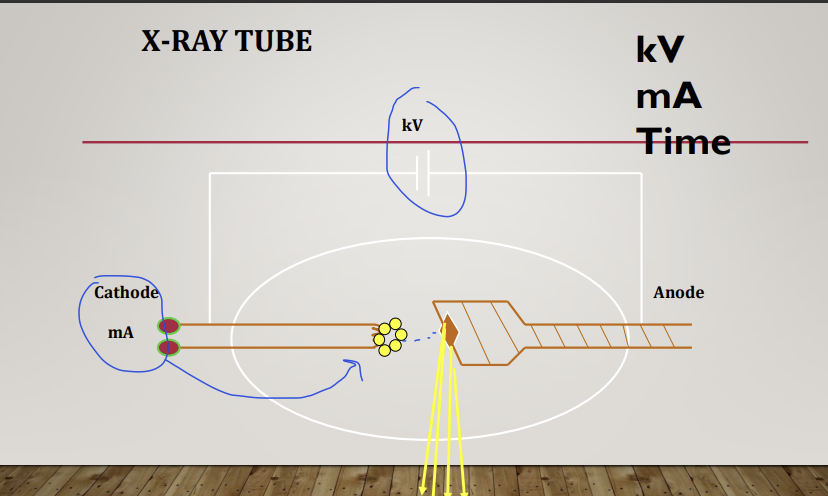
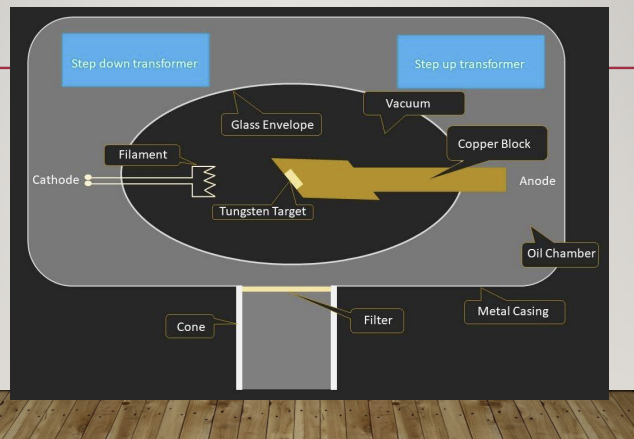
What is this?
an x ray tube
What two principle elements does an x ray tube contain?
cathode (-) and anode (+)
What provides the source of electrons?
cathode
What does the anode act as?
a target for electrons and releases X rays
What happens in an x ray tube?
filament which is made of tungsten is heated - on the cathode , requires a small voltage
electrons are emitted by the hot filament
negatively charged electrons travel to the anode which is + (deceleration)
a high voltage is used to accelerate the electron movements between the cathode and anode (Kv)
this produces a tube current mA - the flow of electrons from cathode to the anode
What is the anode role?
the anode consists of the target which is a small piece of tungsten set into the angled face of a copper block to allow efficient removal of heat
it converts hight energy electrons into x ray photons - due to deceleration
99% is converted to heat while only 1% is converted to Xray
So what is found at the cathode and anode?
cathode - tungsten filament to emit electrons through thermionic emission when heated - requires a small voltage
anode - tungsten acts as a target where high energy electrons strike and rapidly decelerate producing X rays
What is the role of the copper?
efficient removal of heat,
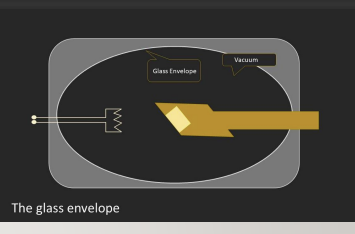
What is the purpose of a vacuum chamber?
the high energy electrons are negatively charged and air particles can scatter the electrons away from the target, so a vacuum is used to remove obstruction e.g nitrogen and oxygen so this lets the electrons travel in a straight line
What are 3 important factors in producing X-rays?
kV - voltage
mA - current
Time
What are the 2 main types of collision with the tungsten atom at the anode?
x-ray producing collisions
heat producing collisions
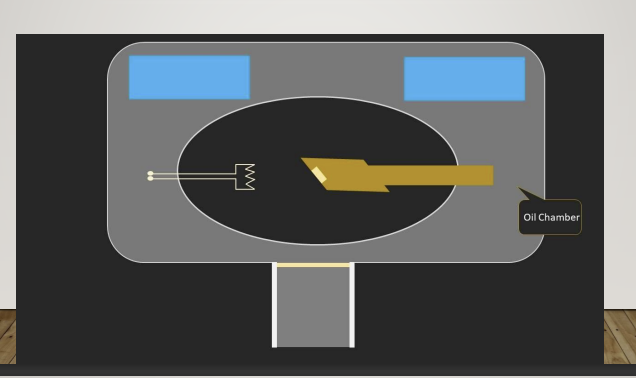
6 What is the oil chamber?
a significant amount of heat is generated along with X ray - oil will remove most of this heat with the aide of the copper block in the anode
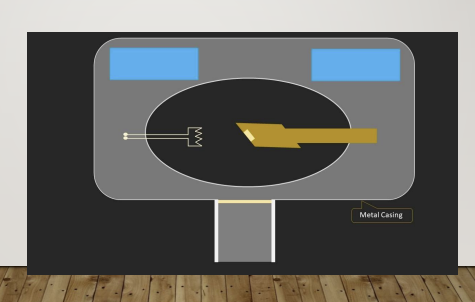
6 What is the metal casting?
this is the outer component of the tube within the x ray machine - lead - prevents leakage , you want it directed at the teeth
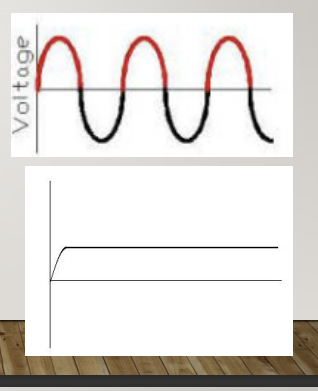
6 What is the main supply to the X ray machine? the magnitude of the voltage?
what type of current this is and why this is a problem? how is this overcome?
240 V is the main supply to the X ray machine
this is an alternating current, so half the cycle is positive and the other half is negative, for X-ray production, only the positive half can be used to ensure the electrons from the filament are drawn to the target
rectification is used to alter it from a alternating current to a direct current AC-DC
the rectifier eliminates the negative half , making the voltage work at its peak
AC produces X-rays during the half cycle, but low energy is unusable
DC - constant steam of radiation means all of it is useful
6 Why does the 240 V supply to the x ray machine need to be modified?
High voltage across the X ray tube head - to accelerate the electrons via a step-up transformer
low voltage to heat the filament via the step-down transformer -
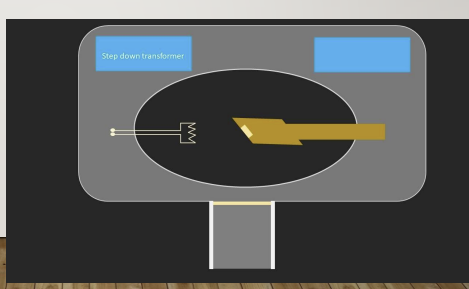
6 Why do we need a step down transformer?
step-down transformer reduces the voltage reaching the filament to protect it from burning up reduced from 110 or 220 to only 10 Volts
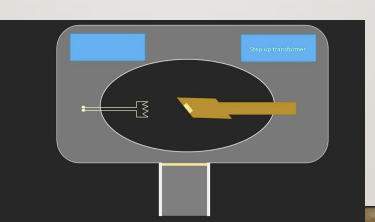
6 What is the new voltage when using the step up transformer?
step up transformer increases the voltage of the tube
typically increase the voltage up to 70000 volts
Kv setting determines the voltage of the tube
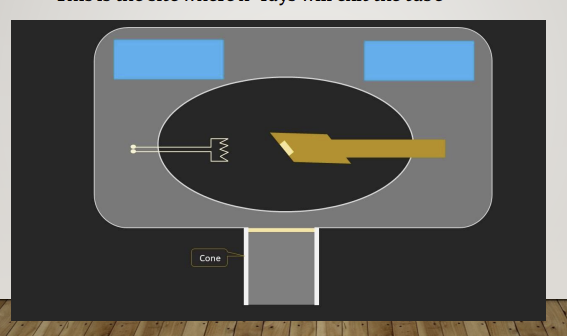
6 What is the cone?
this is the site where X rays will exit the tube
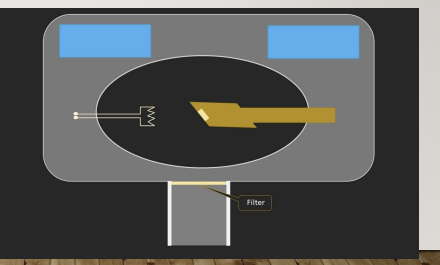
6 What is the filter and what is it made from?
made from aluminium and it is responsible for removing low energy photons
these can get stuck in the tissue and cause problems
6 sum up what features are present in an X-ray tube
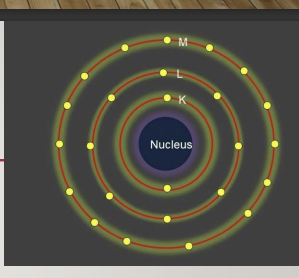
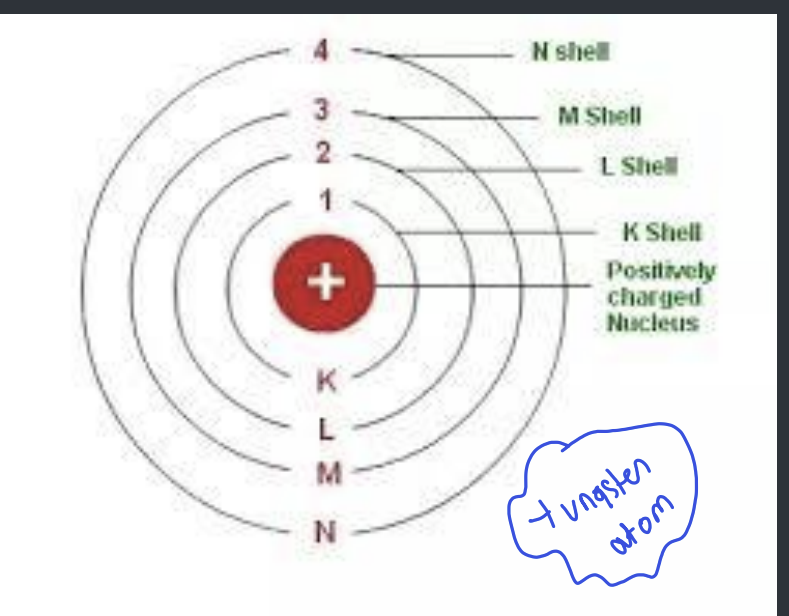
6 Describe this structure of the atom?
how many electrons are found at k and its position means what?
the nucleus is positively charged
the orbiting electrons are negatively charged
electrons circle in a number of orbits K,L,M
K shells have the fewest electrons , and the highest binding energy as they are closest to the nucleus - this means that ejecting them from their orbit requires more energy compared to ejecting an M shell electron
What is the atomic number of H and Lead and why is this important?
the atomic number is the number of orbiting electrons in an atom
1 for hydrogen as it has a single orbiting electron and 82 for lead making it a good material for absorbing radiation
What are 2 types of collisions with the tungsten atom at the anode?
X ray producing and heat producing collisions
What are 2 main types of X-ray producing collisions?
continuous spectrum
characteristic spectrum
explain continuous spectrum?
the incoming electron passes near the nucleus of the atom - slowed down and deflected by the nucleus producing bremsstrahlung radiation (as the nucleus is positively charged causing rapid deceleration) therefore they lose large amount of energy in the form of x-rays
when the incoming electrons penetrate the outer electron shells and pass close to the nucleus of the tungsten atom, the electrons are dramatically slowed down and deflected by the nucleus - rapid deceleration of bombarding electrons
also called bremsstrahlung radiation = braking radiation = continuous X rays
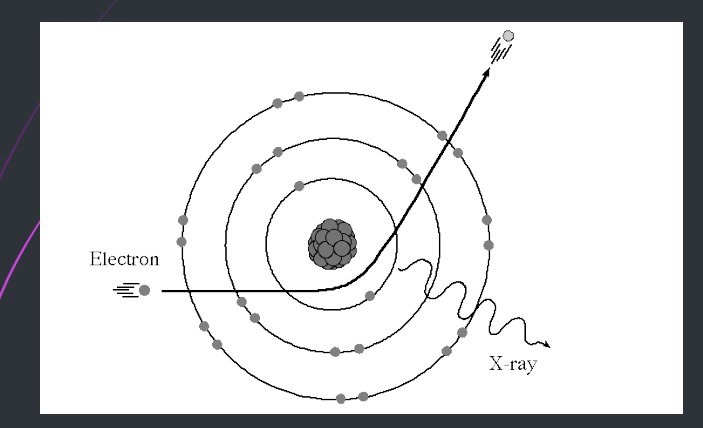
What is characteristic spectrum?
K shell have the largest amount of energy as they are closer to the nucleus which is positively charged, if the incoming electron collides with an inner shell and displaces it into a higher energy level - excitation. If it displaces the electron from the atom - higher energy electrons replace this vacancy, it is ionisation which causes a large loss of energy - x rays
the energy level or shells are specific to any particular atom and that’s why it is called characteristic spectrum
When the incoming electrons collide with an inner shell of tungsten electrons (K shell), if they displace these K shell electrons from the atom - ionisation, if they displace these K-shell electrons to an outer shell - excitation
this causes a large loss of energy and subsequent emission of X rays
If the k shell is the closest what does this mean about the binding energy?
it is the highest
So what is important of the high energy electrons that is bombarding the tungsten atoms in the characteristic spectrum?
must have sufficient energy to displace the K shell tungsten electrons
What is the combined spectrum?
continuous and characteristic
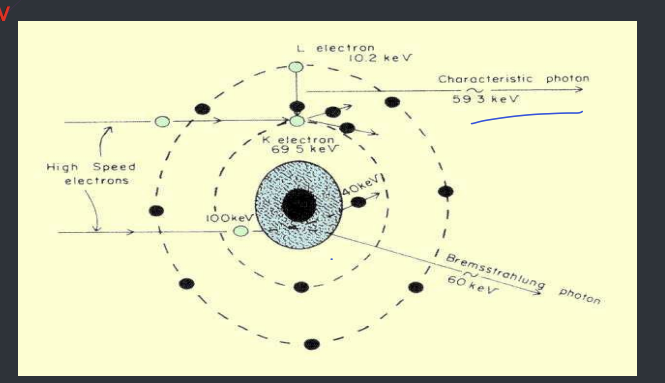
What is critical voltage?
The amount of voltage required to displace an electron from inner shell (K-shell) of a tungsten atom can not be less than 69.5 kV
combined spectrum - if the X-ray equipment operates above 69.5 Kv the final spectrum will be the addition of the continuous and characteristic spectrum (now you get ionisation in addition to excitation/)
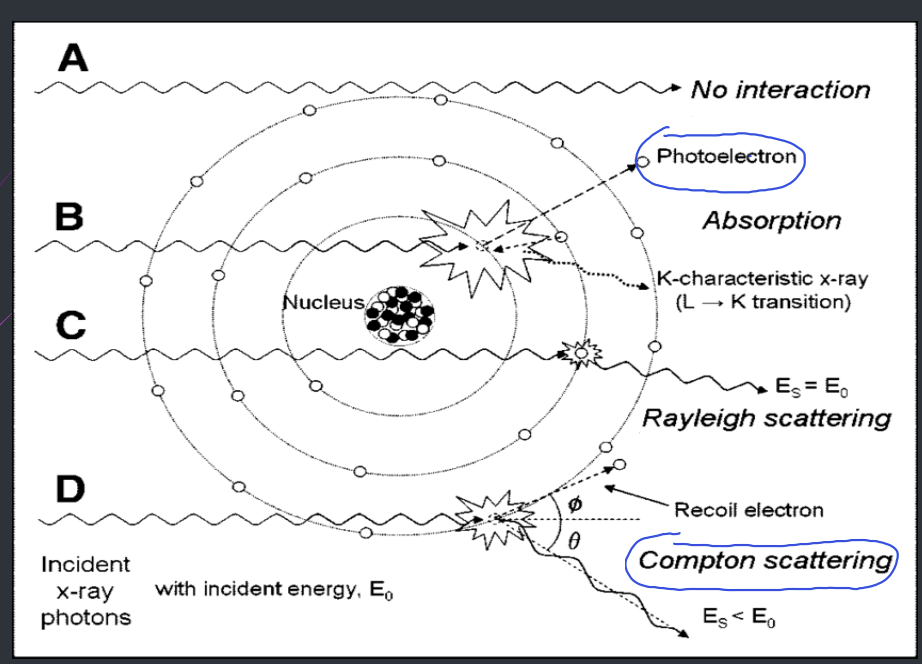
what does scattering mean?
change in direction of a photon with or without loss of energy
What does absorption mean?
deposition of energy = removal of energy from the atom
What does attenuation mean?
reduction in the intensity of the main x-ray beam caused by absorption and scattering
What are the possible fates of X rays when they interact with matter such as patient’s tissue? (4)
scatter without any change, pure scatter - unmodified or Rayleigh scattering
Photoelectric effect (pure absorption) ! - only one’s we need to know
Compton effect - (scatter + absorption) ! - only ones we need to know
pair production - (pure absorption)
How is heat produced in the x-ray tube?
incoming electrons - changes in direction by the outer-shell tungsten electrons
small loss of energy in the form of heat
if collide with an outer shell tungsten electrons, cause either excitation or ionisation
so some loss of energy in the form of heat
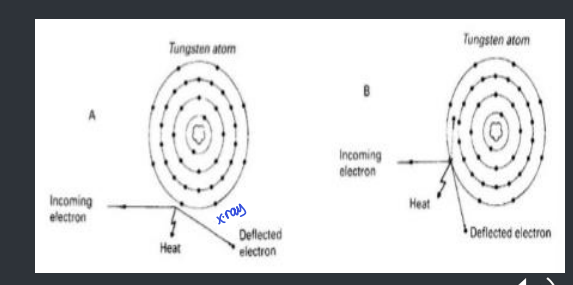
99% of energy is converted to?
heat, so heat producing collisions are the most common interaction s
1% of energy is converted to?
x-ray
How is heat removed? (2)
surrounding oil and copper block
so target is not damaged
Why do we use x rays in dentistry? (7)
check the developing dentition
caries diagnosis
periodontal assessment (bone level)
endodontics
pathology
trauma
implant dentistry

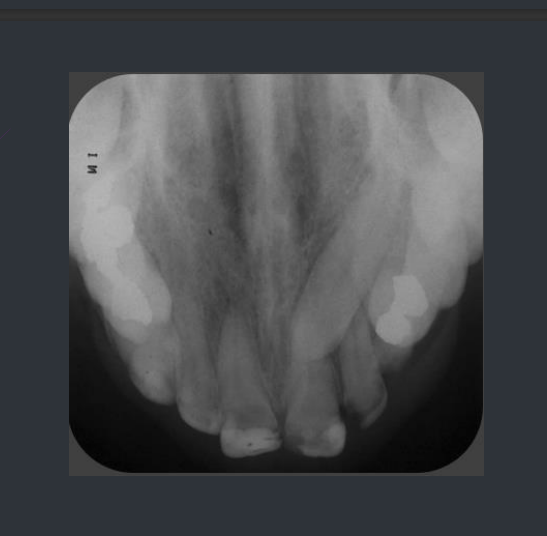
what type of radiograph is this?
bite wing, caries detection and common

What type of radiograph is this?
periapical , pathology of the apex of the tooth/endodontic treatment

What type of radiograph is this?
dental panoramic tomography
What type of radiograph is this?
open standard occlusal, check for trauma, unerupted tooth/buccal or lingual
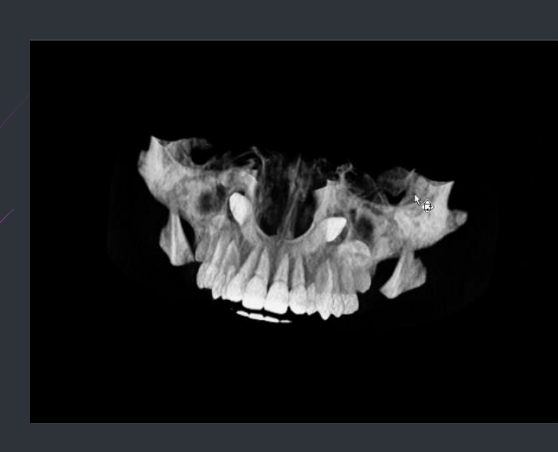
What is this?
cone beam CT - 3D image
What does biological effect mean?
the radiation damage to the cell and tissue of human body
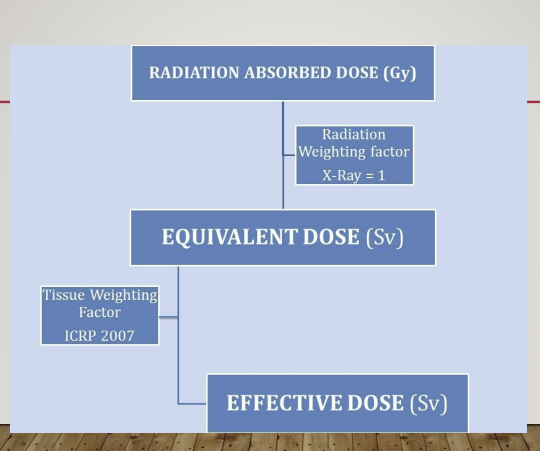
(after 88skip for now) What is Radiation absorbed dose (D)?
how can it be measured
what are the units
This is energy absorbed in tissues from an exposure to a radiation beam. This does not take into effect the radiation type or the tissues exposed. In other words, this is pretty useless number from a clinical or a practical point of view unless we get to know: 1. Type of radiation and its weighting factor 2. Type of tissues exposed and their weighting factor
amount of energy absorbed from the radiation beam per unit mass of tissue
using a dosimeter
milli-gray mGy
D
(after 88skip for now) What is the equivalent dose HT ?
units
formula
it is a dose quantity calculated for individual organs/absorbed dose for an organ
sieverts Sv
equivalent does = radiation absorbed dose (D) x radiation weighing factor WR in a particular tissue
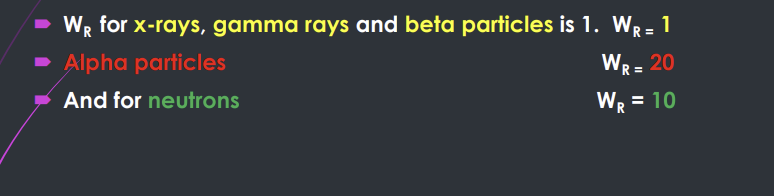
(after 88 skip for now) What is the radiation weightings factor WR ?
radiation weighting factor represents the biological effects of different radiations on different tissues
alpha particles penetrate only a few mm in tissue and lose all their energy and are absorbed totally - very damaging
X rays penetrate much further, lose some of their energy and are only partially absorbed
alpha particles are more damaging - absorbed completely
WR for X-rays, gamma and beta - 1, aloha - 20 neutrons - 10
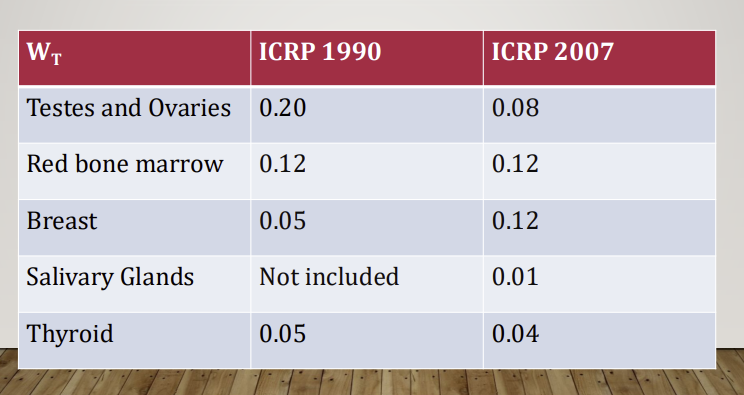
(after 88skip for now) What is tissue weighting factor WT?
the relative measure of the risk to specific tissue to develop non-deterministic effects following radiation exposure
it takes into account the variable sensitivity of tissues to ionising radiation
The International Commission on Radiological Protection (ICRP) has allocated each tissue a numerical value, known as the tissue weighting factor(WT) • The greater the risk of the tissue being damaged by radiation-the higher the tissue weighting factors.
(after 88skip for now) What is the ICRP?
international commission on radiological protection, they allocated each tissue a numerical value as each tissue is susceptible to different extents - Tissue weighting factor
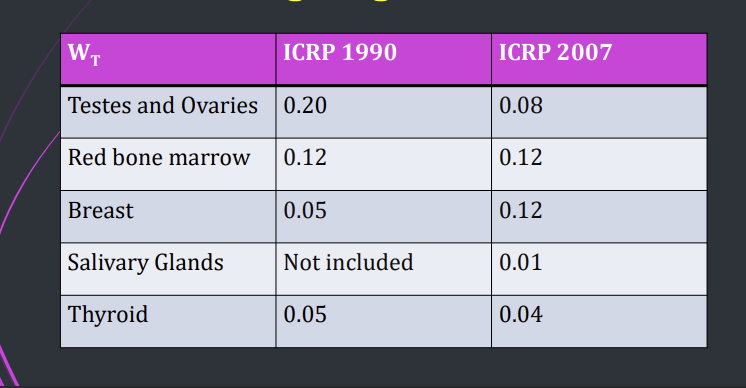
(after 88skip for now) What organs are more suceptible?
(after 88bskip for now) What is the effective dose?
when the simple term dose is applied loosely, it is the effective dose E
by converting all doses to an equivalent whole body dose, different parts of the body can be compared together
because some parts of the body are more sensitive to radiation than others
• This takes into account the tissues being exposed. • Different tissues react differently to radiation, for example, bone marrow has a higher tissue weighting factor at 0.12 when compared to salivary glands at 0.01.
(after 88bskip for now) How can you make a panoramic X ray more safer?
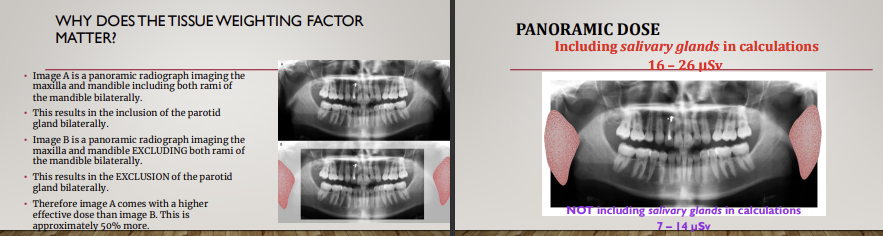
What is the relationship between radiation absorbed dose, radiation weighted factor, equivalent dose, tissue weighted factor and effective dose?
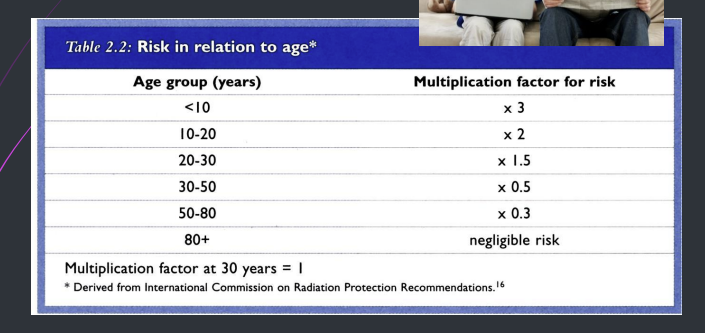
(after 88skip for now) What is the risk in relation to age?
much higher in age range from 0 to 20
(after 88skip for now) What is the collective effective dose or collective dose?
unit
effective dose E x population
man sv
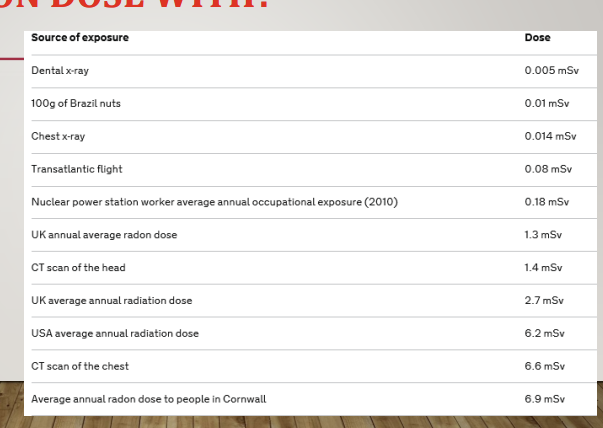
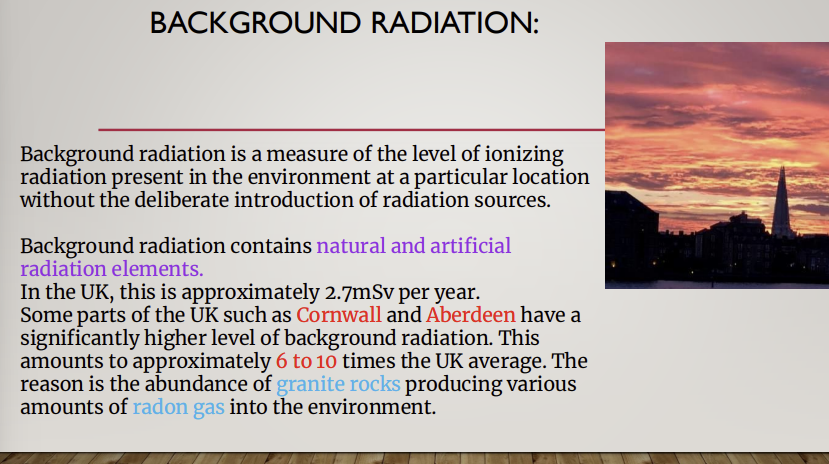
(after 88skip for now) What are sources of radiation not due to x ray taking?
natural background radiation - about 2.7 MSV per year
from earth atmosphere
gamma radiation from rocks/soil
ingestion f radioisotopes in certain foods
artificial background radiation
from nuclear explosions, radioactive waste
medical and dental diagnostic radiation
radiation from occupational exposure
(after 88skip for now) why does background radiation occur?
(after 88skip for now) how can you compare radiation and flying?

What are biological effects of x rays?
damage to cells and tissue
the biological effects are classified into? (3)
somatic deterministic effects
somatic stochastic
genetic stochastic
What are stomatic deterministic effects?
they are the damaging effects to the body that will definitely result from a specific high dose of radiation
the severity of the effect is proportional to the dose received
so the higher the dose, the higher the severity of the effect
usually occurs at higher levels of radiation, unlikely seen in relation to dental X ray examinations
in most cases, the threshold dose exists, and below this , there will be no effect
What are 2 types of somatic deterministic?
acute and chronic
What is acute somatic deterministic?
large dose of radiation delivered in a short time
effects are seen just after exposure - within 24 hours
immediate health problems such as nausea, vomiting, skin burns, redness of skin
What is chronic somatic deterministic?
occurs after months or years of taking exposure
may lead to death
e.g nurse holding the film lost her digits - obliterative endarteritis
single large dose and see effects after a long time- cataracts
can cause genetic mutation e.g inability to conceive

What are stomatic stochastic (non-deterministic)?
may develop - occur by chance
their development is random and depends on the cause of chance or probability
these damaging effects may be induced when the body is exposed to any dose of radiation
e.g leukaemia, certain tumours
so there is no threshold
is there a safe dose?
no safe dose with stochastic, every exposure has a chance of effects. The lower the exposure the lower the probability of damage, not related to the magnitude of the dose either, but probability increases with the increase of the dose
What are genetic stochastic effects? (4)
genetic non-deterministic effects involves a genetic cell, any some level might initiate the process required to produce this effect
congenital abnormality
mental retardation
death of an unborn child
increase mutation rate
rare in dentistry as the X ray beam from dental X ray examination is unlikely to reach the reproductive organs
0 The biological effects depends on? (4)
quality of radiation
quantity of radiation
received dose of radiation
exposure conditions
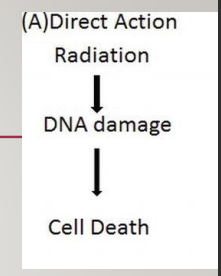
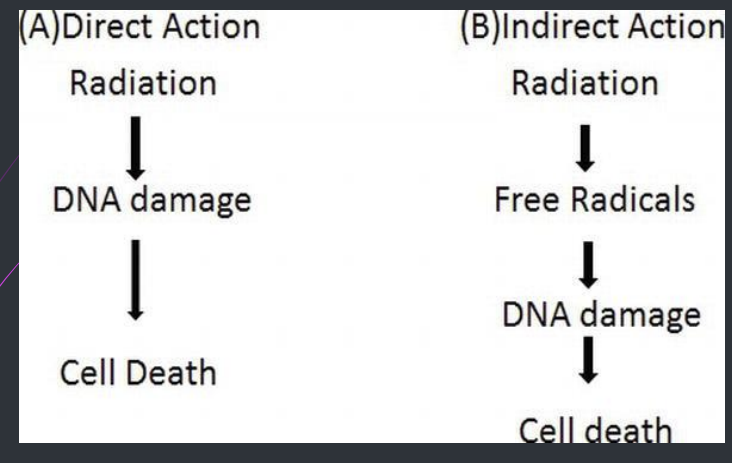
How can x rays cause damage?
direct or indirect damage
What is direct damage?
the incoming high-energy electrons hit DNA and RNA within the cells
directly disrupting the molecular structre
weak bonds between the nucleic acids break
inability to pass on the information and/or abnormal replication
cell damage or cell death may occur
if radiation hits somatic cells result in?
radiation induced malignancy
affects DNA and hence chromosomes - results in induced malignancy
if radiation hits reproductive stem results in?
radiation induces congenital abnormalities
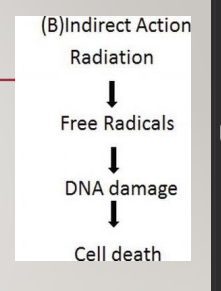
What is indirect damage?
as cells are made up of 75% water, radiation is likely to hit water, causing water molecule to ionise
it is the water molecule that are most likely to be ionised by incoming high energy X rays photons
positive ions break up forming free radicals which damage cells
they are highly reactive and unstable and combine with each other, forming hydrogen peroxide and hydroperoxyl - damage DNA
Difference between direct and indirect damage?
Due to the damaging effects of ionising radiation, what is put in place?
safety legislation to minimise the risks to radiation workers and to the patients
What are 3 principles for radiation protection according to ICRP? (international commission on radiological protection)
justification
optimisation
limitation
What are the main aims of radiation protection according to ICPR?
(international commission on radiological protection)
prevent the deterministic effects - should never happen in dentistry
limit the probability of stochastic effects
Describe justification
the benefit to the patient from the exposure should outweigh the detriment
• The availability and findings of previous radiographs •
The specific objectives of the exposure in relation to the history and examination of the patient •
The total potential diagnostic benefit to the individual •
The radiation risk associated with the radiographic examination •
The efficacy, benefits and risk of available alternative techniques having the same objective but involving no, or less, exposure to ionizing radiation.
any dental exposures must be clinically justified
Describe optimisation
all exposures shall be kept as low as reasonably practicable
taking economic and socio factors into account
It is necessary to reduce patient doses to as low as reasonably practicable consistent with the intended purpose
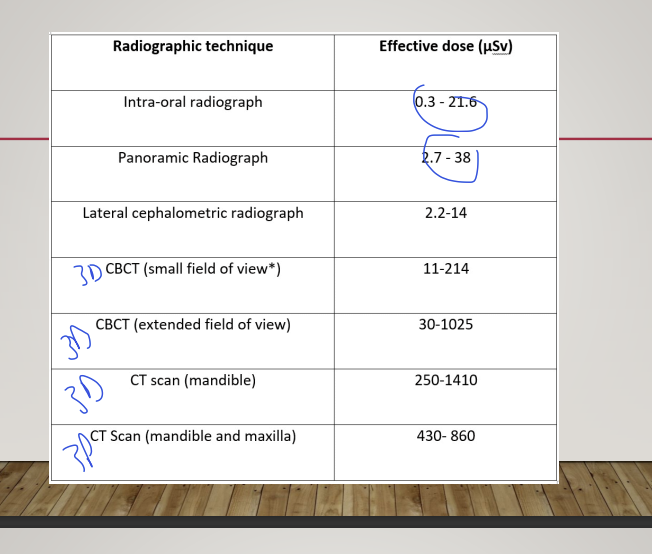
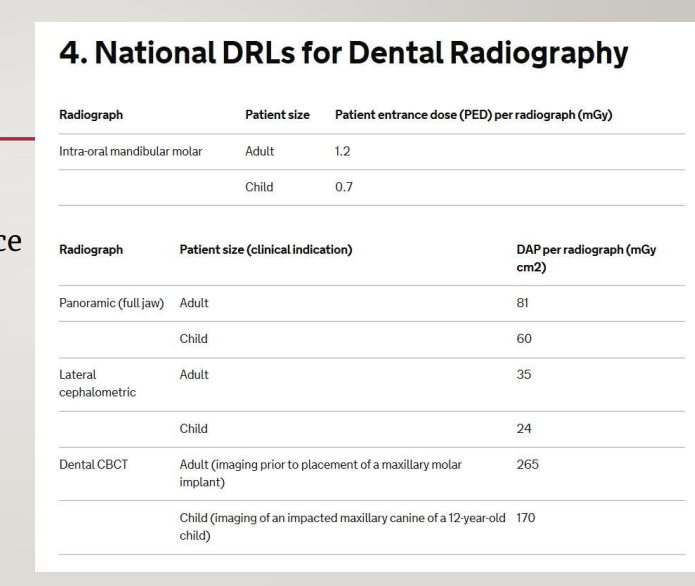
Compare the effective dose of radiographic techniques
Ct is not used in dentistry
Describe limitation
the dose equivalent to individuals shall not exceed the limits recommended by the ICRP
divided the population into patients, radiation worker and general public
Describe the dose limits for patients
no set dose limit, The number, type and frequency of the radiographs requested or taken (selection criteria) are the responsibility of the clinician.
use selection criteria for dental radiography - faculty of general practice of the royal college of surgeons of England
2nd part of the lecture :Dose reduction techniques are divided into? (4)
equipment
clinical decision
practical techniques
diagnostic interpretation
explain equipment for dose reduction techniques
install the dental x ray machine correctly and should be tested by a medical physicist, checked regularly every 1 to 3 years
X-ray equipment should function between agreed parameters usually 60-90kV and 7 to 12 mA
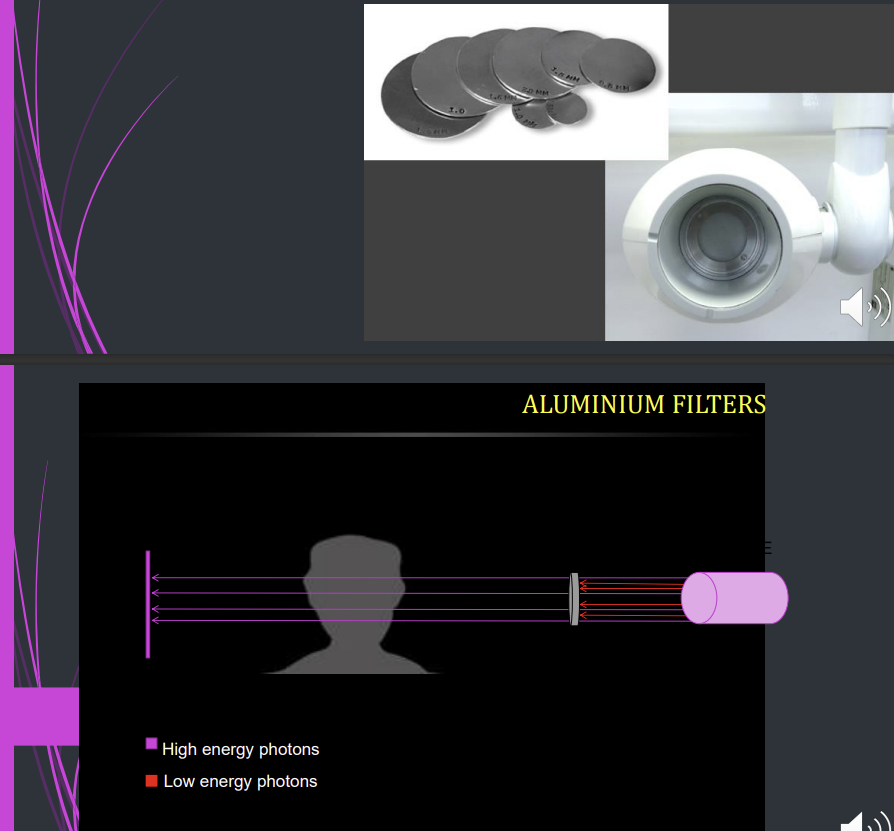
What is aluminium filtration?
is used to remove harmful low energy x rays - soft x ray as they don’t pass through the tissue but are absorbed
1.5 mm below 70 kV
2.5 mm above 70 kV
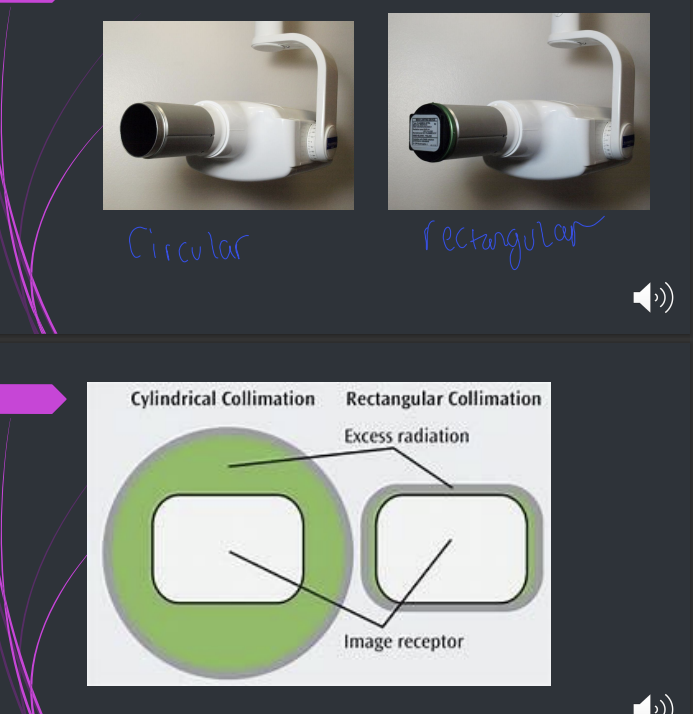
What is collimation?
a metallic barrier with an aperture in the middle which is used to reduce the size and shape of the X ray beam and therefore reducing the volume of irradiated tissue in the patient
it minimises scattering radiation, sharper image and better contrast
diaphragm, round, rectangular and slit
rectangular collimator is more effective, 50% more reduction
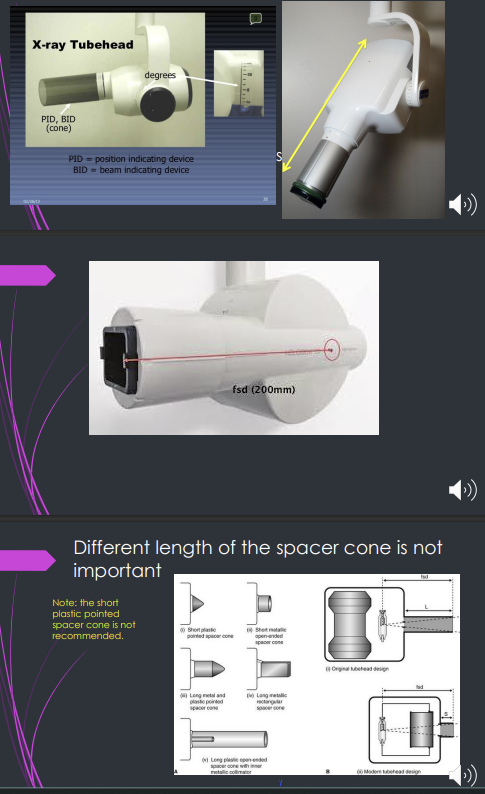
What is the beam indicating device BID or the spacer cone?
it is a device for indicating the direction of the beam, setting the ideal distance from the focal spot on the target
200mm for operating above 60 Kv
100 mm for operating 60 Kv or below
it is the length of the focal spot to skin distance
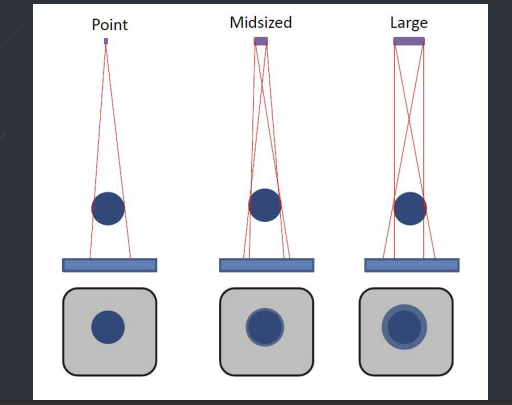
the focal spot or the source of the x ray should ideally be what?
ideally be a point source to reduce blurring of the image - penumbra effect