Mandibular Anesthesia Part 1
1/86
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
87 Terms
what is the largest branch of the trigeminal n.?
MANDIBULAR DIVISION (V3)
MANDIBULAR DIVISION (V3) exits via the _______ and enters the _____
Exit via Foramen Ovale and enter the Infratemporal Fossa
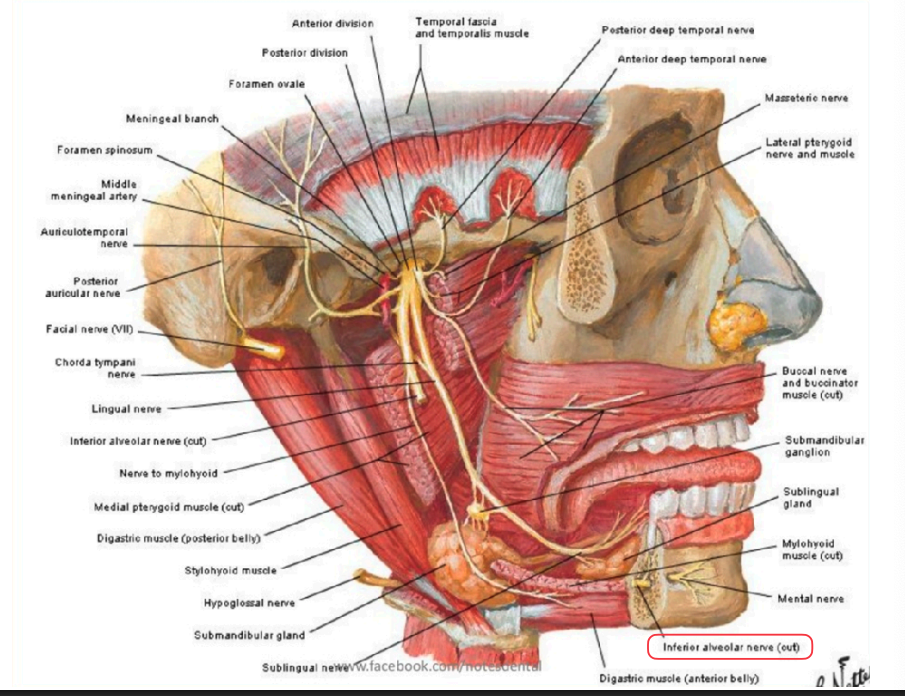
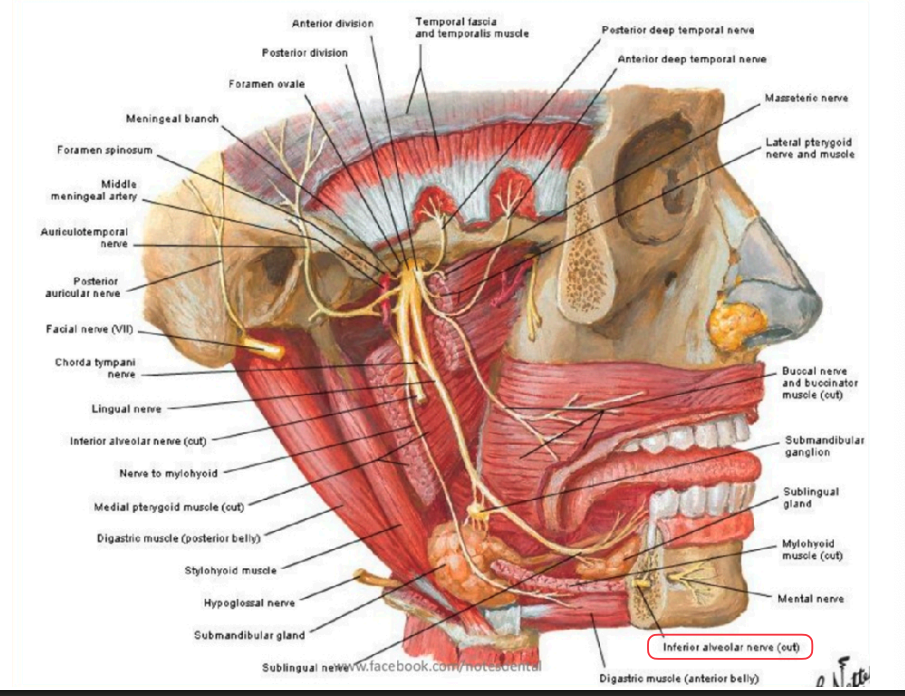
V3 is a large sensory root that innervates what areas/structures?
Skin on lower 3rd of the face, lower lip
Skin of temporal region
Mandibular dentition and gingiva
Anterior 2/3rd of the tongue (general sensation)
V3 has a small motor root as well that innervates what structures?
muscles of mastication
V3 also carries nerve fibers from other nuclei including…?
Autonomic fibers for salivary glands (CN VII)
Special sensory taste fibers (CN VII)
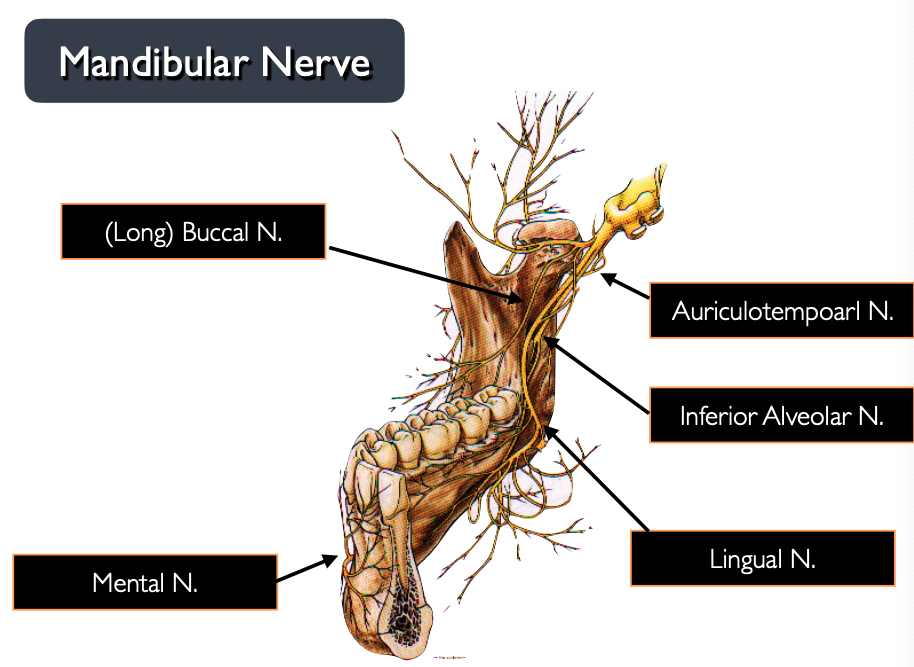
what branches make up the anterior division of V3?
Motor:
Masseter N.
Deep Temporal N
Medial Pterygoid N.
Lateral Pterygoid N.
Sensory:
(Long) buccal N
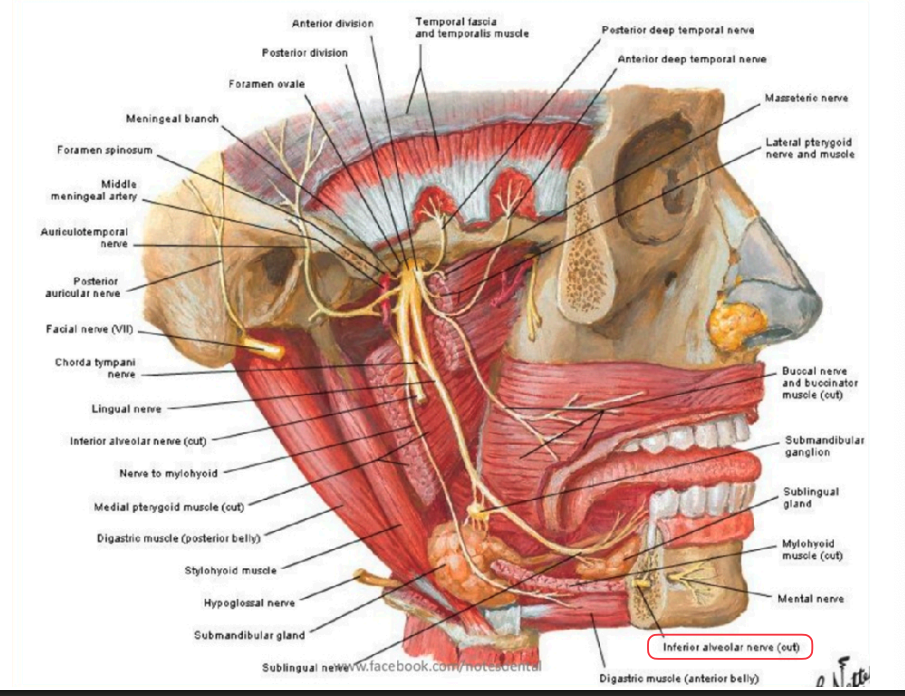
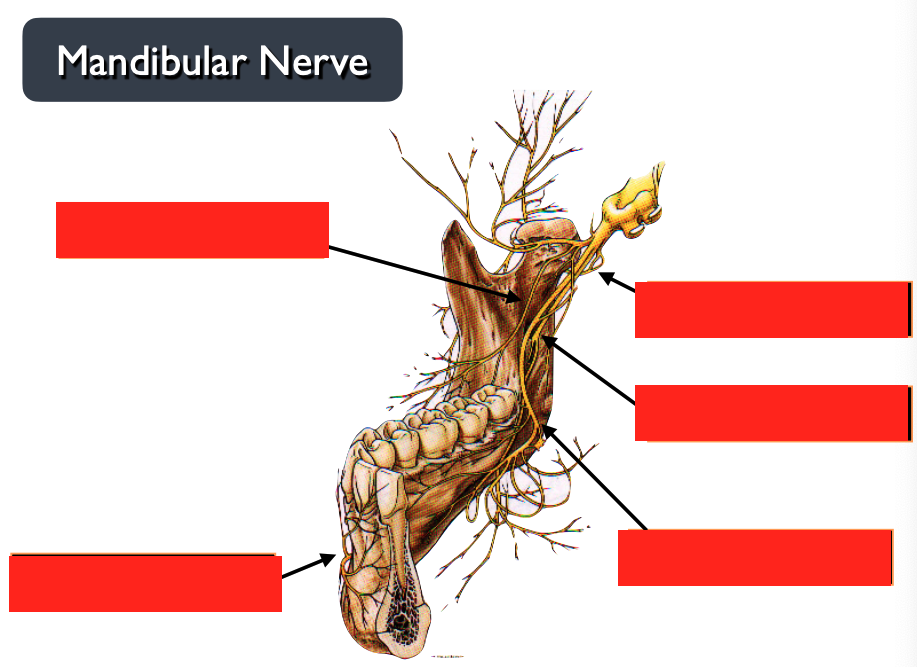
what branches make up the posterior division of V3?
Sensory
Auriculotemporal N.
Lingual N.
Inferior Alveolar N.
Mental N.
Incisive N.
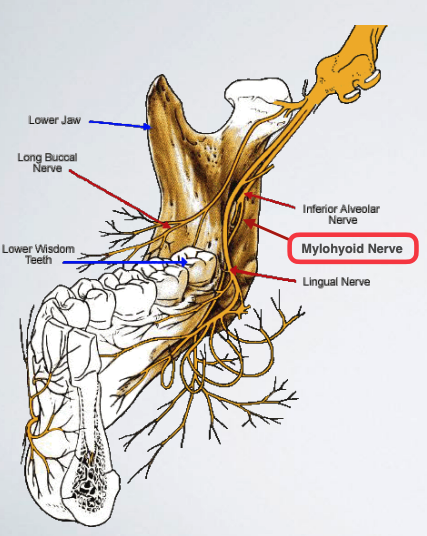
Mylohyoid N.
Motor:
Mylohyoid N.
what is the main nerve of interest (branch of V3) when we’re talking mandibular dental anesthesia?
inferior alveolar n.
what structures are innervated by the medial pterygoid n.?
Medial Pterygoid Muscle
Palate: Tensor veli palatini
Ear: Tensor tympani
what structures are innervated by the masseteric n.?
masseter m.
what structures are innervated by the deep temporal n.?
temporalis m.
what structures are innervated by the lateral pterygoid n.?
lateral pterygoid m.
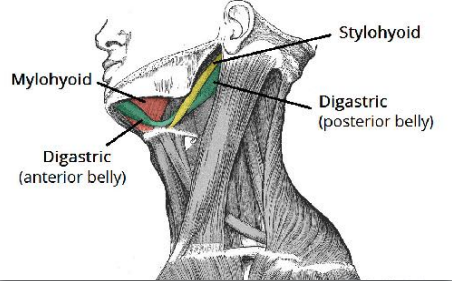
what structures are innervated by the mylohyoid n.?
mylohyoid m.
anterior belly of digastric
what structures/regions are innervated (sensory) by sensory root of V3>?
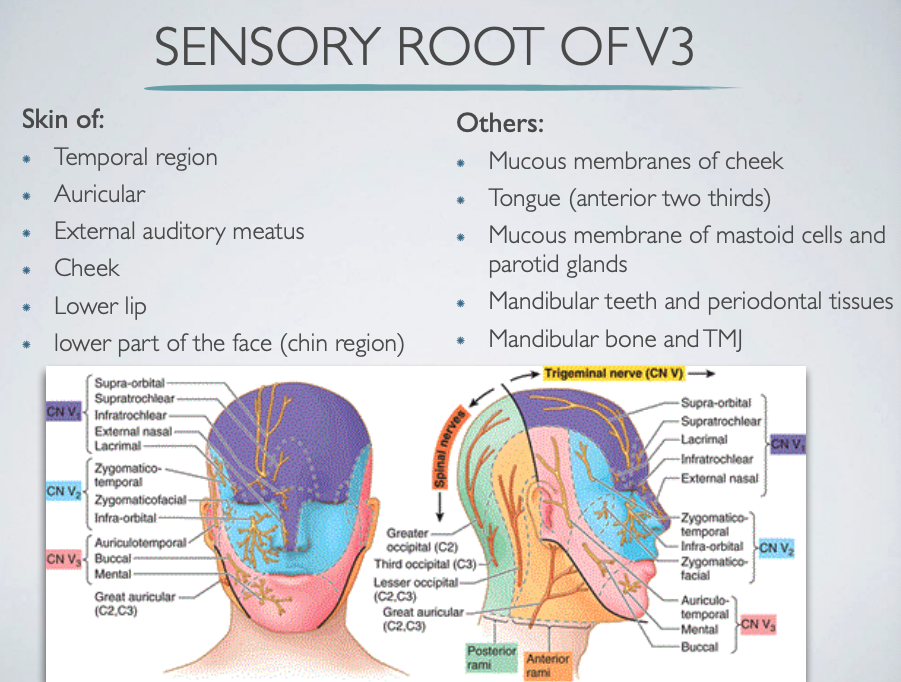
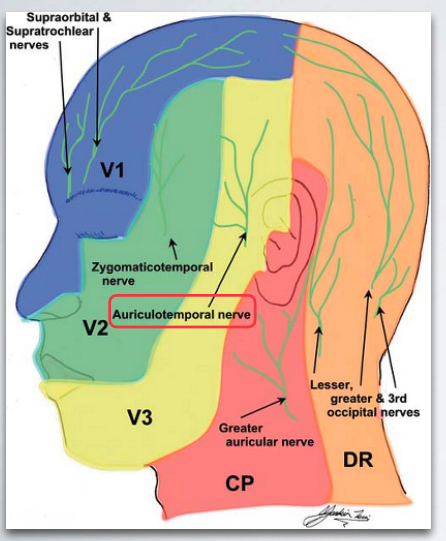
auriculotemporal n. supplies sensory innvervation to…?
External auditory meatus
Skin of anterior aspect of temple
Skin of the auricle
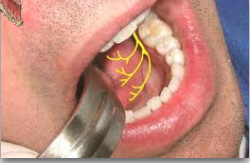
long buccal n. provides sensory innvervation to …?>
Buccal gingival tissue of the molars to the second premolar region
Skin of the cheek

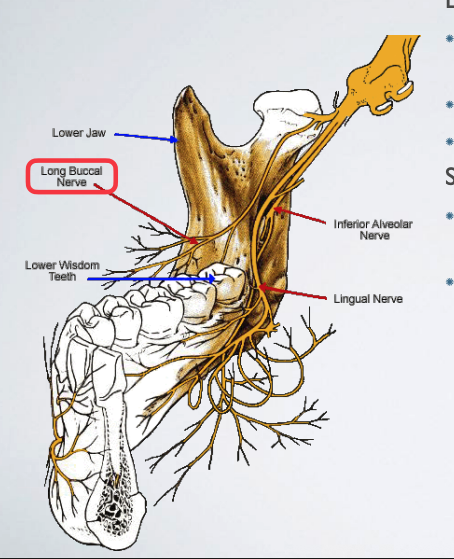
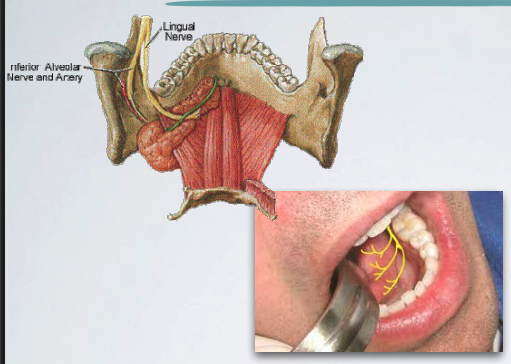
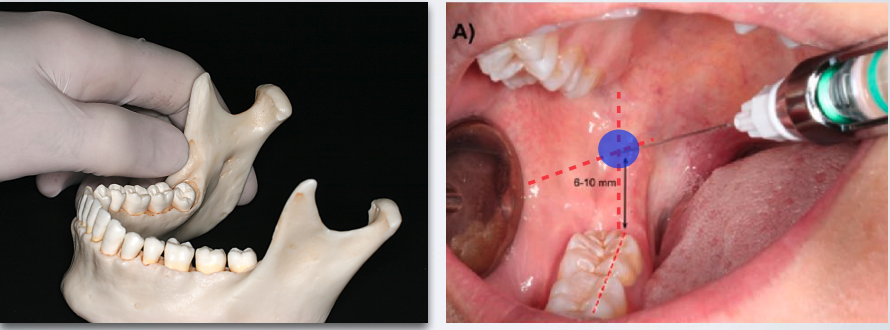
what nerve is indicated in this image?
long buccal n.
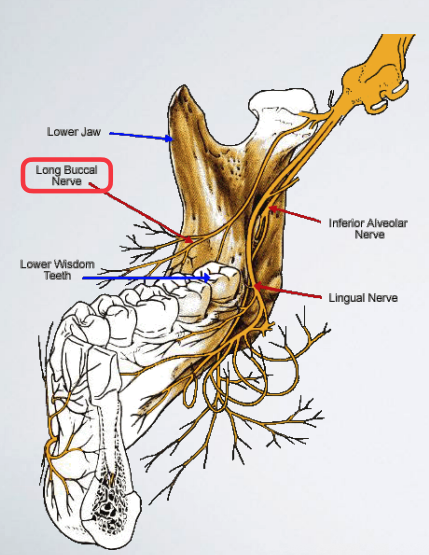
describe the location of long buccal n.
Runs from the medial side and cross the anterior border of the ramus
Runs anterior to inferior alveolar nerve
Enters the cheek
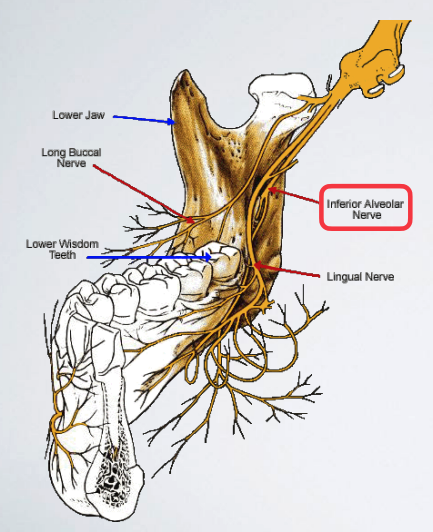
inferior alveolar n. provides sensory innervation to …/
Mandibular dentition to midline
Lingual hard and soft tissue
Buccal gingiva anterior to mandibular first molar
what terminal branches come off of inferior alveolar n./
mental n.
incisive n.
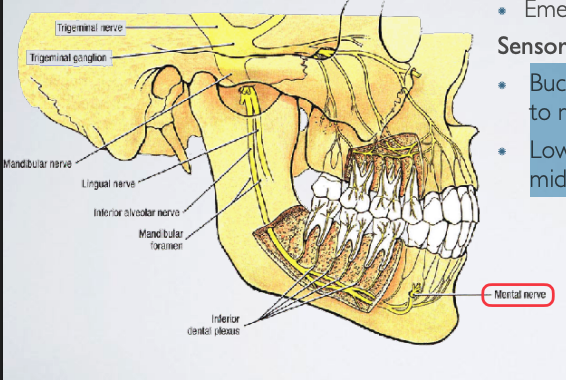
mental n. is a terminal branch of which nerve?
inferior alveolar n.
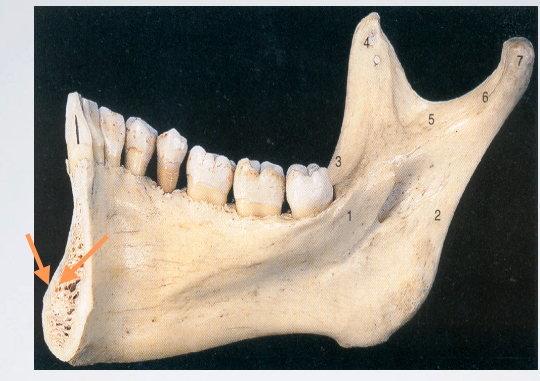
mental n. emerges from which foramen?
mental foramen
mental n. provides sensory innvervation to…?
Buccal gingiva from second premolars to midline
Lower lip and skin of the chin to midline

which nerve is displayed here?
mental n.
incisive n. is a terminal branch of which nerve?
inferior alveolar n.
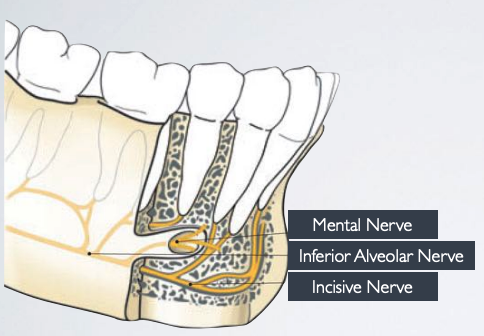
where is the invisive n. located?
remains within mandibular canal
incisive n. provides sensory innervation to what areas?
Buccal mucosa anterior to mental foramen from second premolar to midline
Lower lip and skin of chin to midline
Dental pulps of premolars, canine, lateral and central incisors
mylohyoid n. provides motor innervation to what muscles?
mylohyoid m. and anterior belly of digastric m.
mylohyoid n. provides sensory innervation to what structures?
mandibular dentition (accessory innervation)
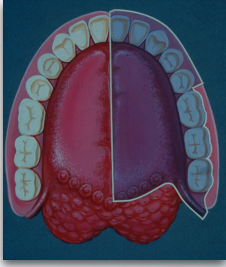
lingual n. provides sensory innvervation to what structures/regions?
Lingual gingiva of lower dentition
Mucosa of floor of the mouth
Anterior two thirds of the tongue (general sensation)
the lingual n. communicates with what other nerve?
chorda tympani (facial n.)
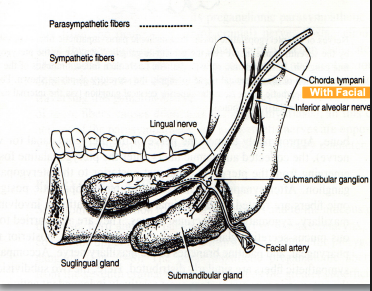
lingual n. communicates with chorda tympani to provide what type of innervation to what structures?
Parasympathetic fibers to the submandibular/ sublingual gland
Special taste sensory fibers to taste buds on the anterior two thirds of the tongue
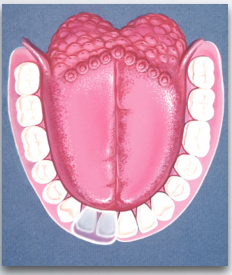
what nerve is depicted here?
lingual n.
what is the problem with mandibular anesthesia, in adults?
the density of the cortical plate of the mandibular bone
It precludes the successful administration of supraperiosteal anesthesia
which injection technique is indicated for Pupal and buccal soft tissue anesthesia for a limited area (single tooth)?
SUPRAPERIOSTEAL INJECTION
what are contraindications for SUPRAPERIOSTEAL INJECTION?
Infection
Dense bone covering the apices of teeth
what nerve is anesthetized with SUPRAPERIOSTEAL INJECTION?
Large terminal branches of the dental plexus
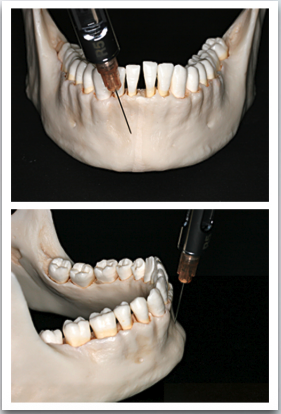
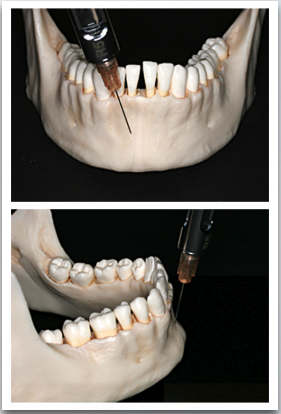
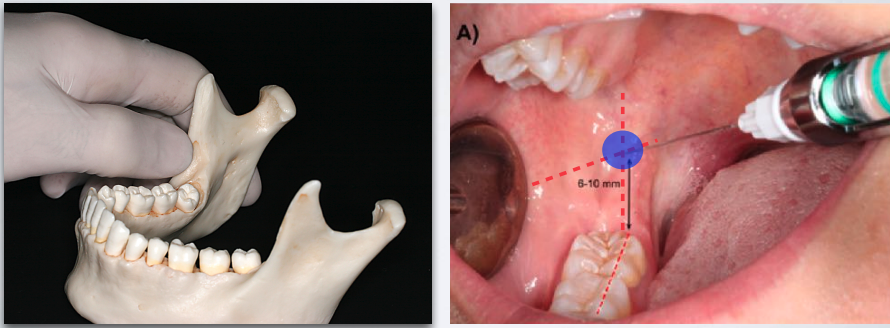
which injection technique?
SUPRAPERIOSTEAL INJECTION
SUPRAPERIOSTEAL INJECTION
what are 3 different techniques for INFERIOR ALVEOLAR NERVE BLOCK?
Standard/Classic/Halstead Technique
Gow-Gates Mandibular technique
Akinosi “closed mouth” technique
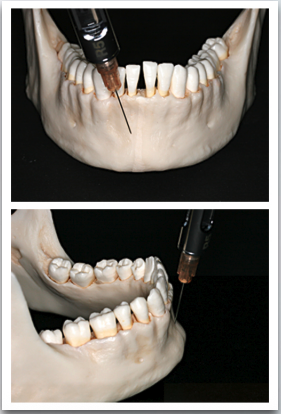
which injection technique?
INFERIOR ALVEOLAR NERVE BLOCK
INFERIOR ALVEOLAR NERVE BLOCK
what nerves are anesthetized with INFERIOR ALVEOLAR NERVE BLOCK?
Inferior alveolar nerve.
Incisive nerve and mental nerve
Lingual nerve (very commonly)
what areas are anesthetized with Inferior alveolar nerve block?
All mandibular teeth to midline and surrounding periodontium and alveolar
Buccal and labial soft tissue anterior to mandibular 1st molar (served by mental nerve)
All lingual soft tissue, floor of the mouth, anterior two thirds of the tongue
what are some contraindications for Inferior alveolar nerve block?
Infection/acute inflammation in area of injection
Patient who might bite either the lip or tongue (young pediatric or special needs patients)
what are advantages to Inferior alveolar nerve block?
One injection provides a wide area of anesthesia (useful for quadrant dentistry)
Bony contact
which injection technique is inidcated for procedures on multiple mandibular teeth in one quadrant?
INFERIOR ALVEOLAR NERVE BLOCK
which injection technique is inidcated when buccal (anterior to 1st molar) and lingual soft tissue anesthesia is required?
INFERIOR ALVEOLAR NERVE BLOCK
a disadvantage to INFERIOR ALVEOLAR NERVE BLOCK include lower success rates compared to maxillary anesthesia. what are some reasons why?
Density of bone
Anatomical variations
Greater distance to target area
what is the success rate of inferior alveolar nerve blocks?
80-85%
what is the positive aspiration rate of inferior alveolar nerve blocks?
10-15%
what are some disadvantages of inferior alveolar nerve block?
lower success rate
wide area (unnecessary for localized procedures)
lingual and lower lip anesthesia (uncomfortable)
inadqequate/partial anesthesia
due to inadqequate/partial anesthesia, what supplementary injections may be needed with inferior alveolar nerve blocks?
buccal nerve block or supraperiosteal injections
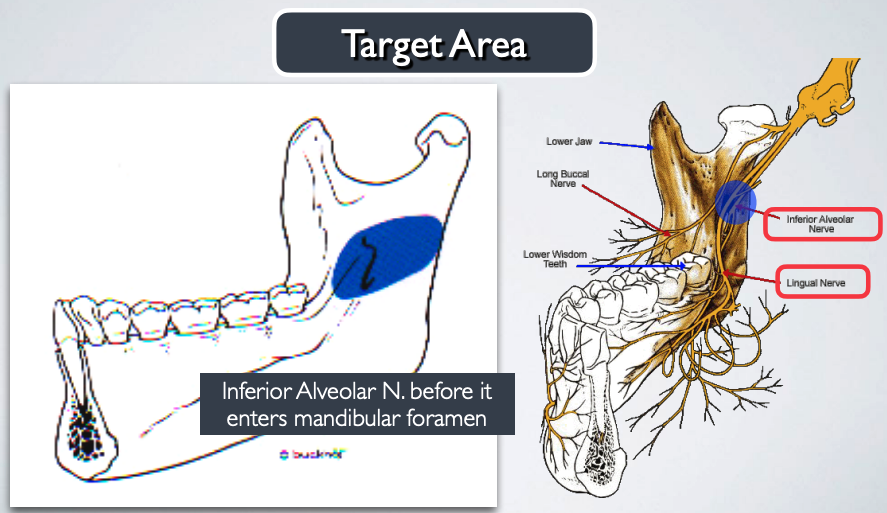
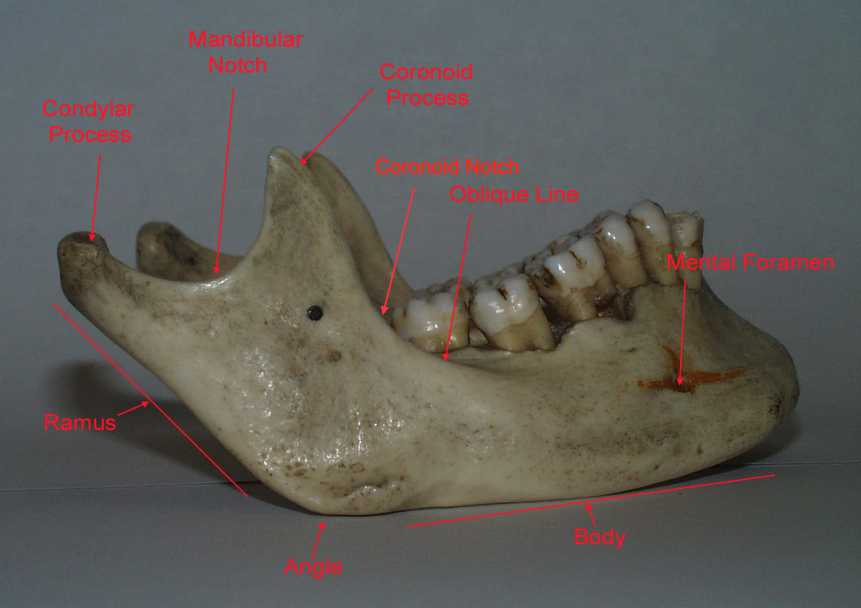
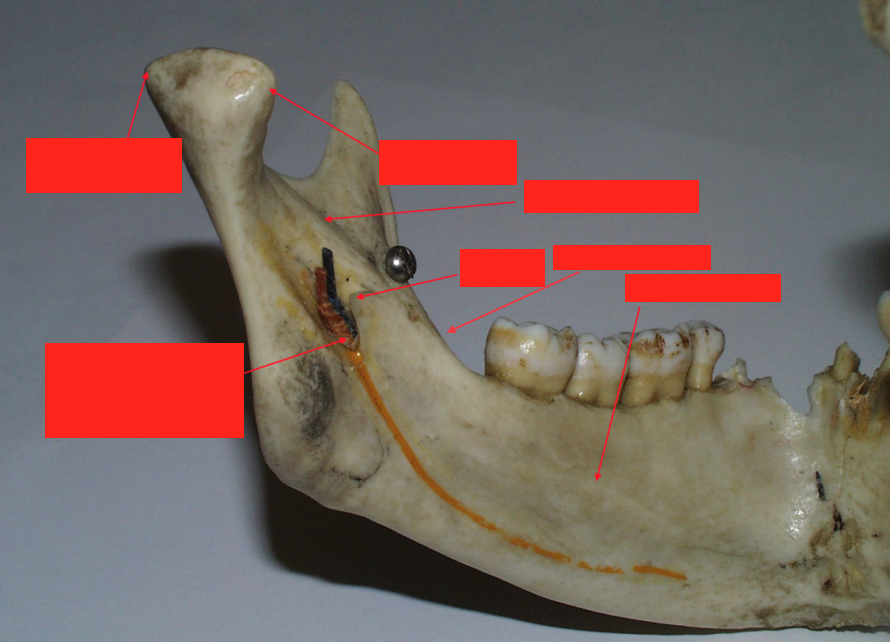
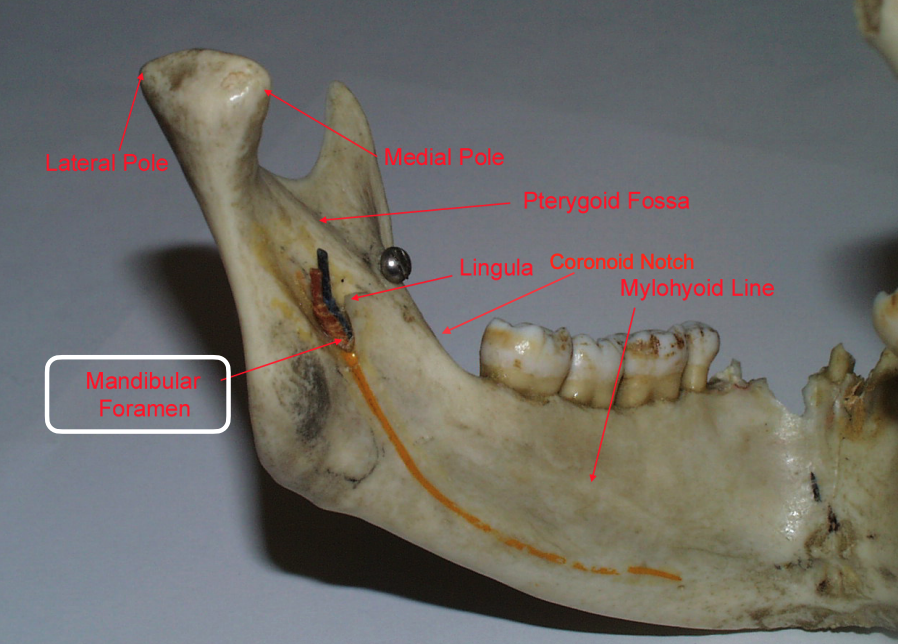
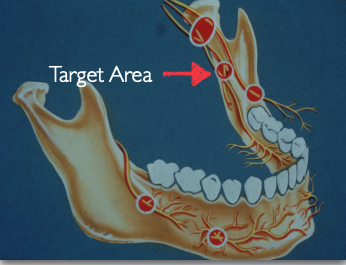
target area for which nerve block?
inferior alveolar nerve block before it enters mandibular foramen
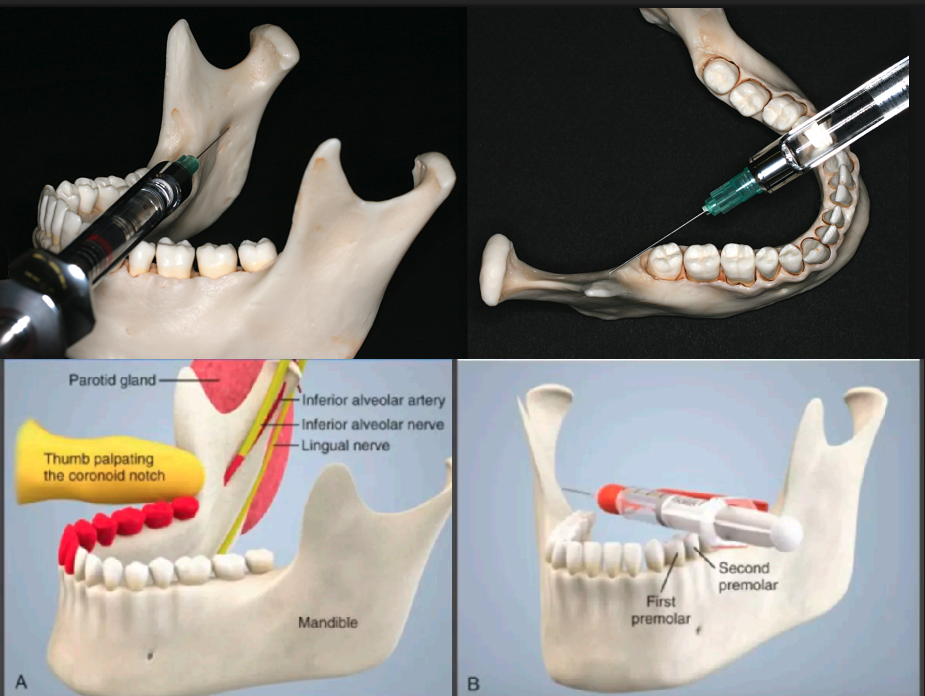
what is the standard/classic technique for inferior alveolar nerve block?
1. Find the landmarks
2. Establish the height of injection
3. Determine the direction of injection
what anatomical landmarks do we use during standard/classic technique for inferior alveolar nerve block?
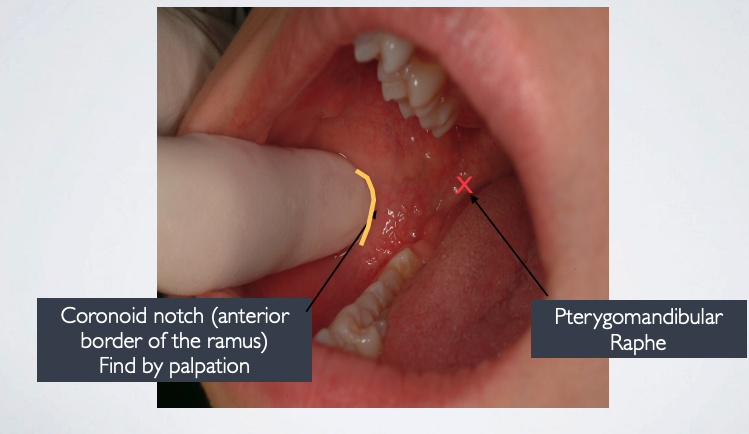
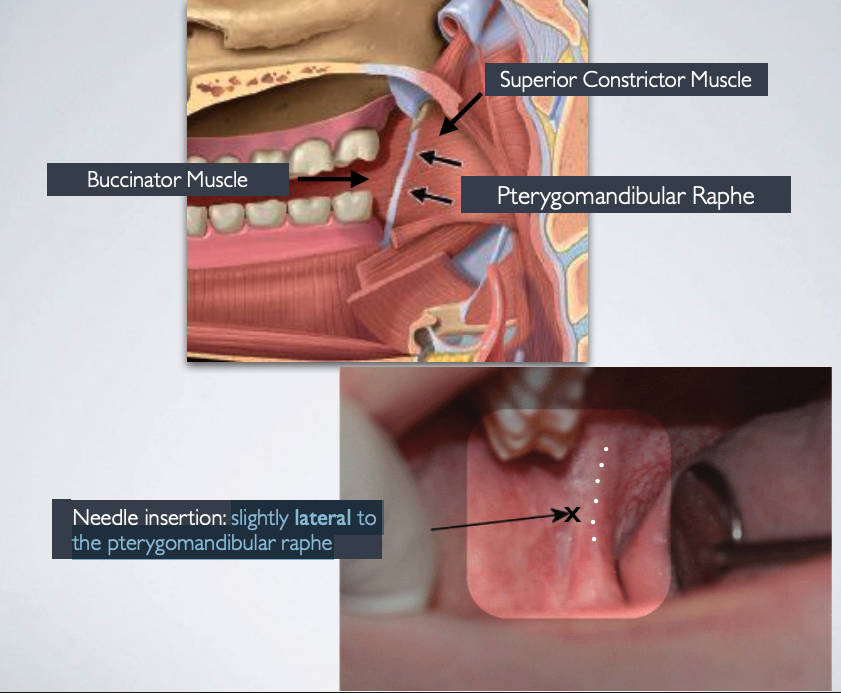
where should the needle be inserted during standard/classic technique for inferior alveolar nerve block?
slightly lateral to the pterygomandibular raphe
describe how to establish the height of injection during standard/classic technique for inferior alveolar nerve block?
Place thumb at the coronoid notch, parallel to the plane of occlusion
The imaginary line begin at the midpoint of the notch and terminate at the deepest part of the pterygomandibular raphe
Place finger in the coronoid notch (greatest concavity on anterior border of the ramus)
Continue the imaginary line to the deepest part of the pterygomandibular raphe.
Needle insertion lies 3/4th of the anteroposterior distance of this line

In most patients, the imaginary line that lies on the coronoid notch and deepest part of pterygomandibular line lies ____ mm above the mandibular occlusal plane (during standard/classic technique for inferior alveolar nerve block)
6-10
during standard/classic technique for inferior alveolar nerve block, needle tipe should be slightly _____ to mandibular foramen
superior
what is the average depth of insertion during standard/classic technique for inferior alveolar nerve block?
20-25 mm
how do you determine the direction of injection during standard/classic technique for inferior alveolar nerve block?
Come in from the contralateral side between the premolar area
Slowly advance until bone is contacted
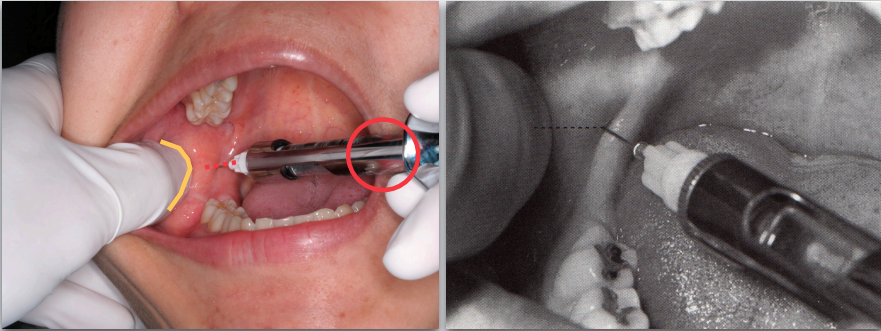
which injection technique?
standard/classic technique for inferior alveolar nerve block
what should you do if bone is contacted too soon during standard/classic technique for inferior alveolar nerve block?
Withdraw slightly
Angulate the needle tip more posteriorly (syringe barrel more anteriorly)
Re-advance to correct depth (20-25 mm)
if bone is contacted too soon during standard/classic technique for inferior alveolar nerve block, what might have went wrong?
Needle tip is located too anteriorly
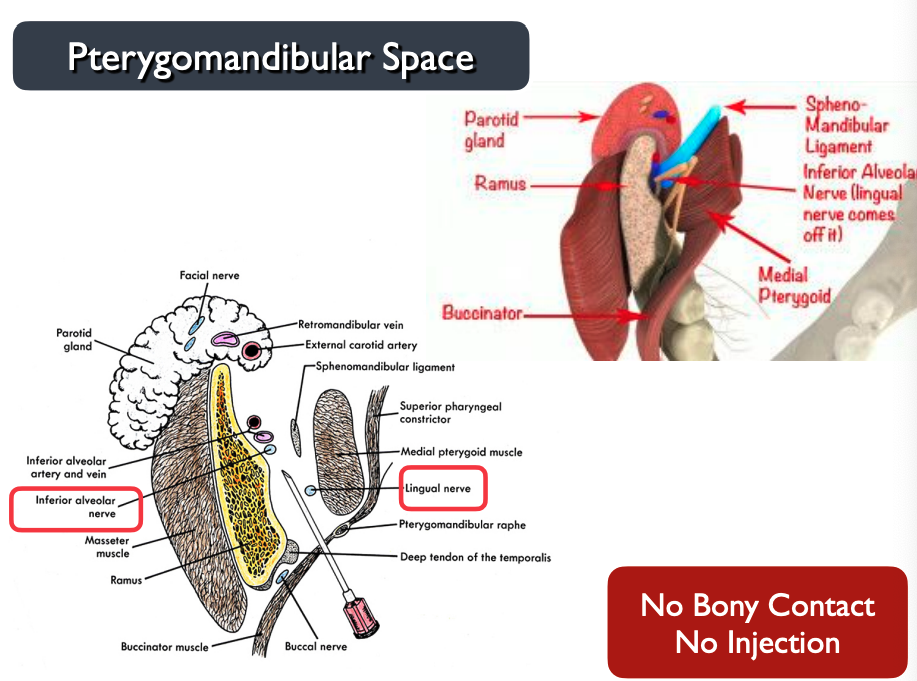
what should you do if there is no bony contact during standard/classic technique for inferior alveolar nerve block?
Withdraw slightly
Angulate the needle tip more anteriorly (syringe barrel more posteriorly)
Re-advance to correct depth (20-25 mm)
if there is no bony contact during standard/classic technique for inferior alveolar nerve block, what might have went wrong?
Needle tip located too posteriorly
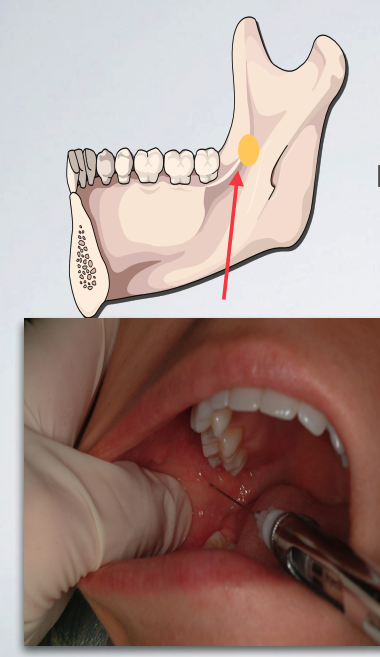
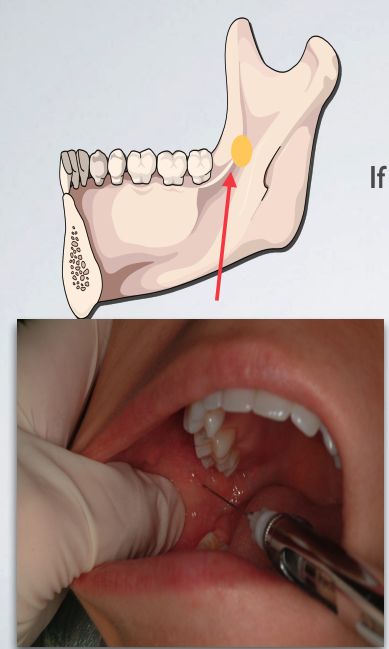
INCORRECT technique (standard/classic technique for inferior alveolar nerve block)
needle tip located too anteriorly
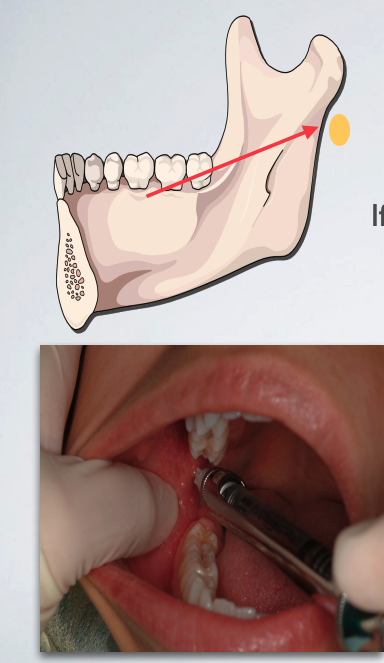
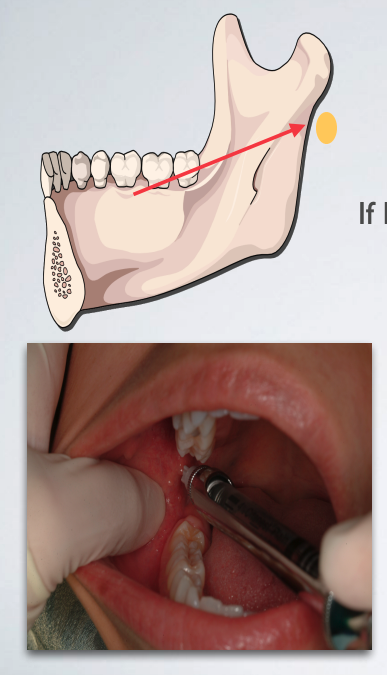
INCORRECT technique (standard/classic technique for inferior alveolar nerve block)
needle tip located too posteriorly
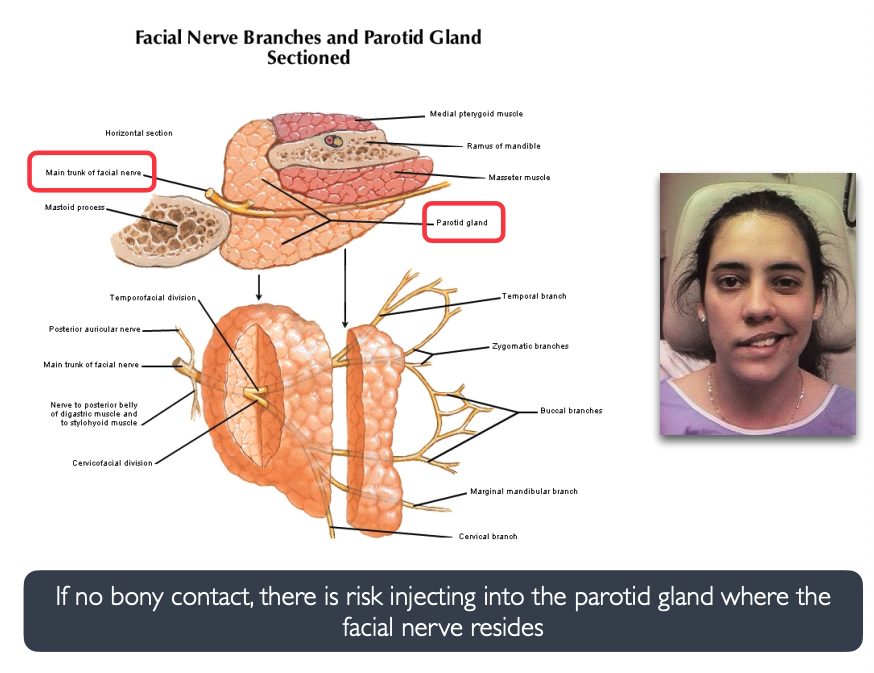
what might happen if you inject too far posteriorly during standard/classic technique for inferior alveolar nerve block?
parotid gland is right behind inferior alveolar nerve → anesthetize facial nerve → facial paralysis
what is the proper operatgor position for STANDARD INFERIOR ALVEOLAR NERVE TECHNIQUE?
7 o’clock right side, 11 o’clock left
what is the proper needle size for STANDARD INFERIOR ALVEOLAR NERVE TECHNIQUE?
25 or 27 gauge long
what is the proper needle target for STANDARD INFERIOR ALVEOLAR NERVE TECHNIQUE?
Mandibular sulcus just superior to the mandibular foramen and behind the lingula
what is the proper bevel orientation for STANDARD INFERIOR ALVEOLAR NERVE TECHNIQUE?
Not as critical
what is the proper insertion point for STANDARD INFERIOR ALVEOLAR NERVE TECHNIQUE?
Medial to deep tendon of the temporalis m and just lateral to the pterygomandibular raphe and at height approximating an imaginary line bisecting the thumbnail placed in deepest concavity of coronoid notch
what is the proper insertion path for STANDARD INFERIOR ALVEOLAR NERVE TECHNIQUE?
Through the mucosa and buccinator muscle, from the opposite premolars, parallel to occlusal plane and towards the mandibular sulcus
what is the proper insertion depth for STANDARD INFERIOR ALVEOLAR NERVE TECHNIQUE?
20 -25 mm (and 10 mm for the lingual nerve)
what is the proper anesthetic volume for STANDARD INFERIOR ALVEOLAR NERVE TECHNIQUE?
1.3 to 1.8 mL ( and 0.3 to 0.5 mL for lingual)
what are signs/symptoms of a successful inferior alveolar nerve block?
tingling/numbness of lower lip (mental n.)
tingling/numbness of tongue (lingual n.)
t/f: tingling/numbness of lower lip is a reliable indicator of pulpal anesthesia depth
false. Mental nerve - good indication but not a reliable indicator of plupal anesthesia depth
t/f: Tingling or numbness of tongue may be present without anesthesia of the inferior alveolar nerve
true
which injections would you administer prior to preparing #28 for DO restoration? #30 extraction?
#28 → something + mental nerve block
#30 → something + long buccal
(double check)
when performing standard inferior alveolar nerve injection, you did not contact bone once the needle was inserted to proper depth. what do you do next?
withdraw
redirect
reangulate
patient experienced difficulty moving unilateral facial muscles after your LA injection, which nerve was inadvertently anesthetized? how did this occur?
facial n.
didn’t contact bone because injected too far posteriorly into parotid gland