Gram positive bacterial pathogens
1/28
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
29 Terms
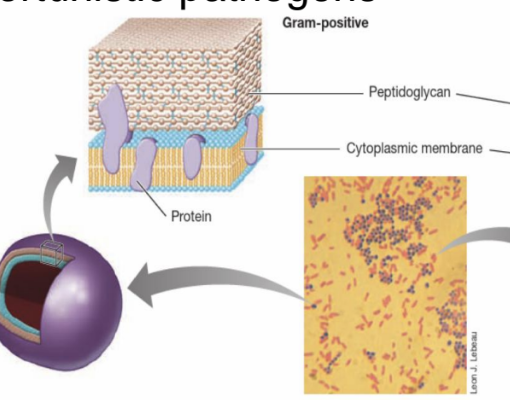
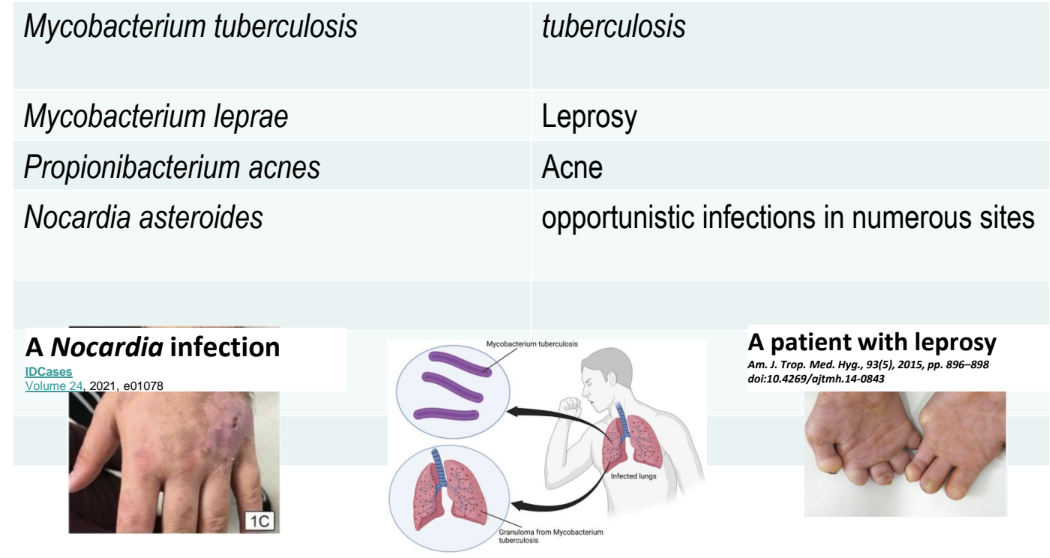
(review) What is Gram-Positive Bacteria
Bacteria that stain purple, thick peptidoglycan, no OM when Gram-stained and can include opportunistic pathogens.
2 major groups:
Low G + C (guanine-cytosine) bacteria,
High G + C bacteria
when did anti-biotic resistance begin?
It’s always been present as bacteria have evolved over time to resist naturally occurring anti-biotic compounds / organisms
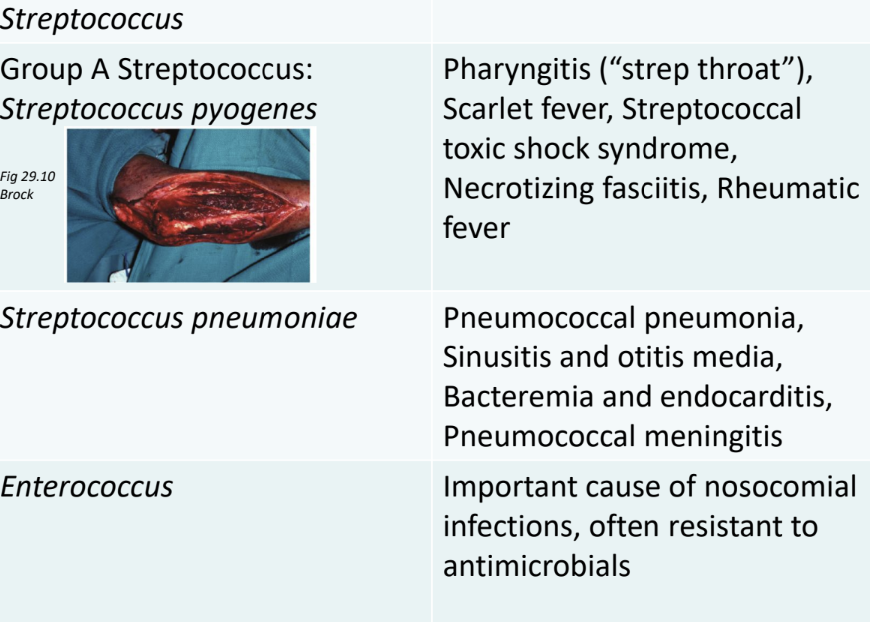
what do Group A Streptococci such as S. pyogenes cause?
Group A Streptococci (GP) such as S. pyogenes cause a range of infections including strep throat, scarlet fever, and skin infections.
They can also lead to more severe conditions like rheumatic fever and necrotizing fasciitis.
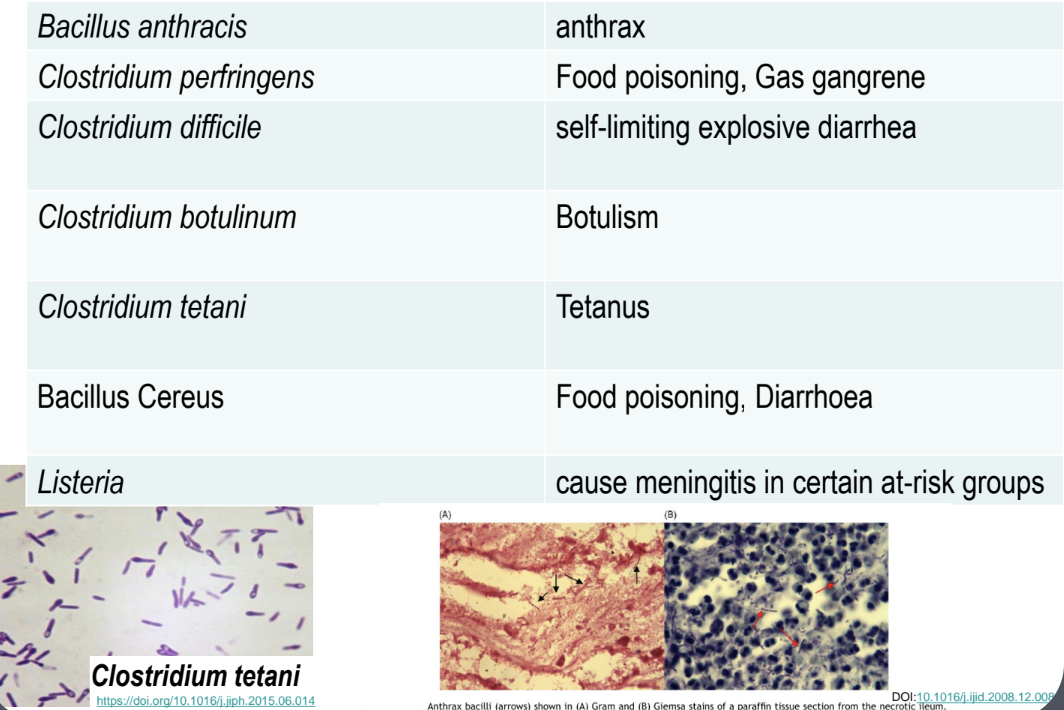
what are some examples of Gram + pathogens?
what are some defining features of Staphylococcus?
– Gram-positive cocci, nonmotile, facultative anaerobes
— Catalase positive
– Grape-like clusters
– Salt-tolerant i.e can tolerate salt on human skin
--Tolerant of desiccation
– Survive on environmental surfaces
What is the difference b/w Staphylococcus aureus and Staphylococcus epidermidis?
S. aureus: A virulent strain of Staphylococcus that can cause a variety of infections depending on the site.
S. epidermidis: apart of normal skin microbiome is a coagulase-negative strain generally less virulent and often associated with opportunistic infections, particularly in immunocompromised individuals.
what are the 3 disease categories of staphylococcus?
1. Noninvasive
Food poisoning
Due to ingestion of enterotoxin-contaminated food
2. Cutaneous
Various localised skin conditions *due to use of coagulase
Scalded skin syndrome, impetigo, folliculitis
3. Systemic
Variety of infections when bacteria invade deeper tissues eg bacteremia, pneumonia, endocarditis, osteomyelitis.
what are the 3 main mechanisms of how Staphylococcus become pathogenic?
1. Evading phagocytosis
2. Production of enzymes i.e coagulase, staphylokinase
3. Production of toxins
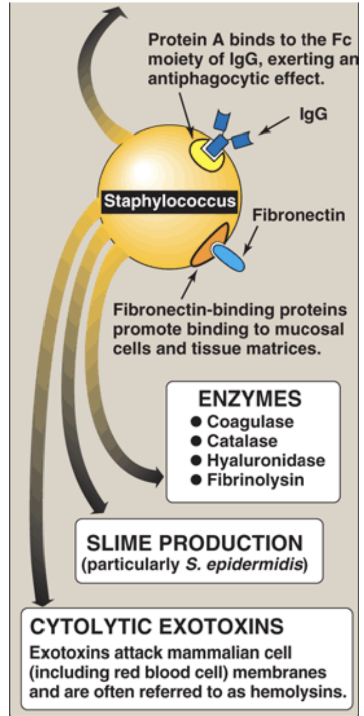
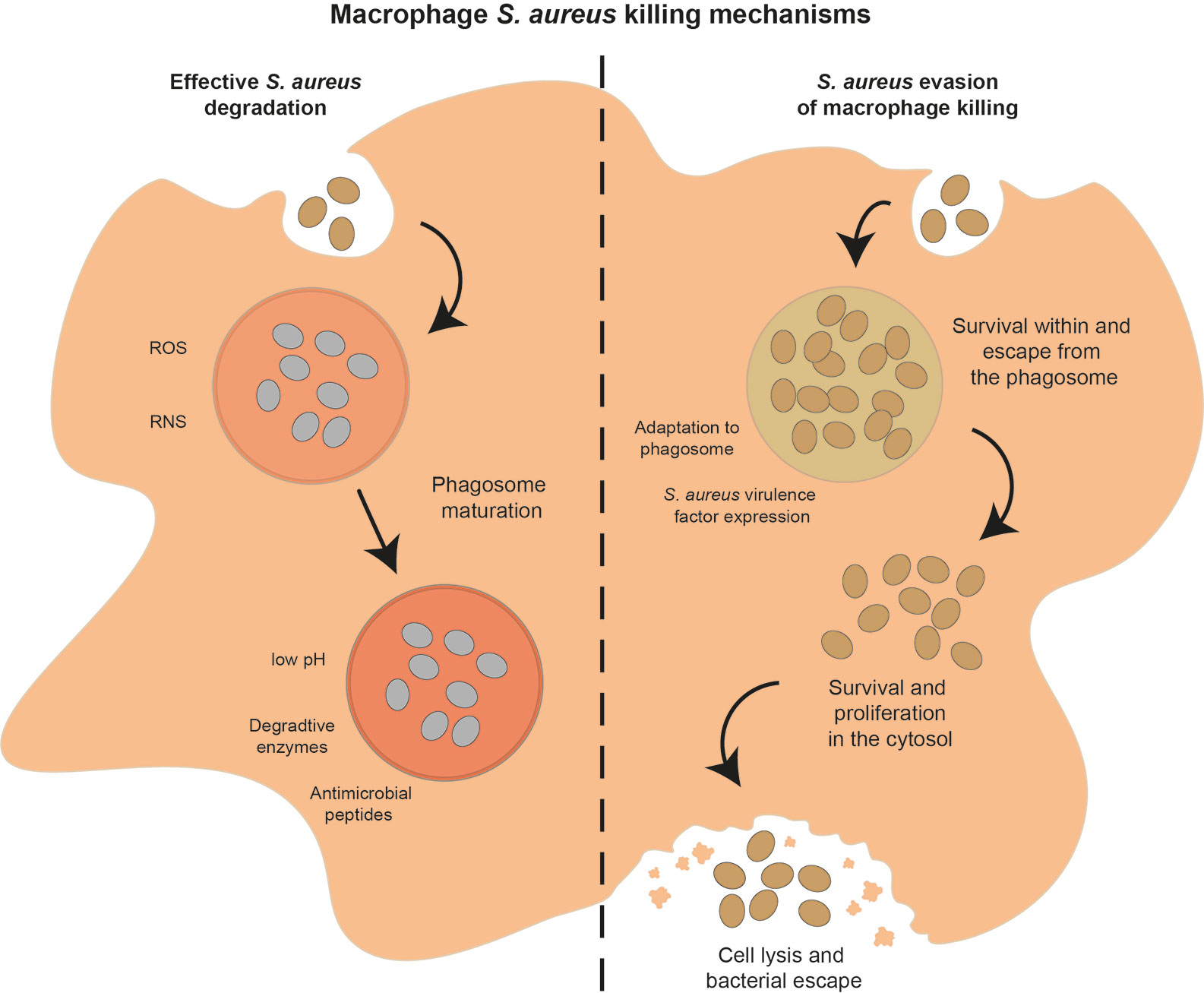
how do staphylococcus evade phagocytosis?
Protein A coats the cell surface which interferes with humoral immune responses
• Inhibits complement cascade
Bound coagulase allows for fibrin clots hide the bacteria from phagocytic cells
Synthesize polysaccharide slime layers (capsules)
• Inhibit leukocyte chemotaxis and phagocytosis
• Enables attachment of Staphylococcus to surfaces
what are the 5 main enzymes of staphylococcus?
Cell-free Coagulase
Staphylokinase
Hyaluronidase
Lipases
B-lactamase
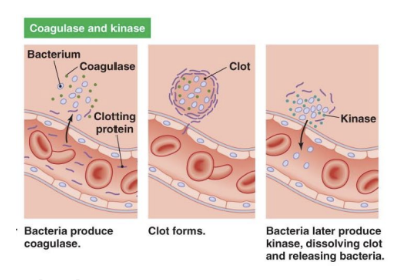
what does cell-free coagulase and staphylokinase do?
Converts fibrinogen to fibrin, facilitating the formation of blood clots.
This process helps the bacteria evade the host's immune response by cloaking themselves in fibrin.
Dissolves fibrin threads in blood clots – Allows S. aureus to free itself from clots
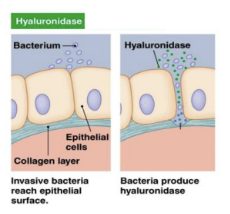
what do Hyaluronidase do?
Breaks down hyaluronic acid
– Enables the bacteria to spread between cells
Exofoliative toxins
Cause skin cells to separate and slough off produced by certain Staphylococcus species, leading to skin conditions such as impetigo and scalded skin syndrome.
Enterotoxins
Toxins produced by certain bacteria, affect the stomach lining such as Staphylococcus aureus, stimulate symptoms of food poisoning.
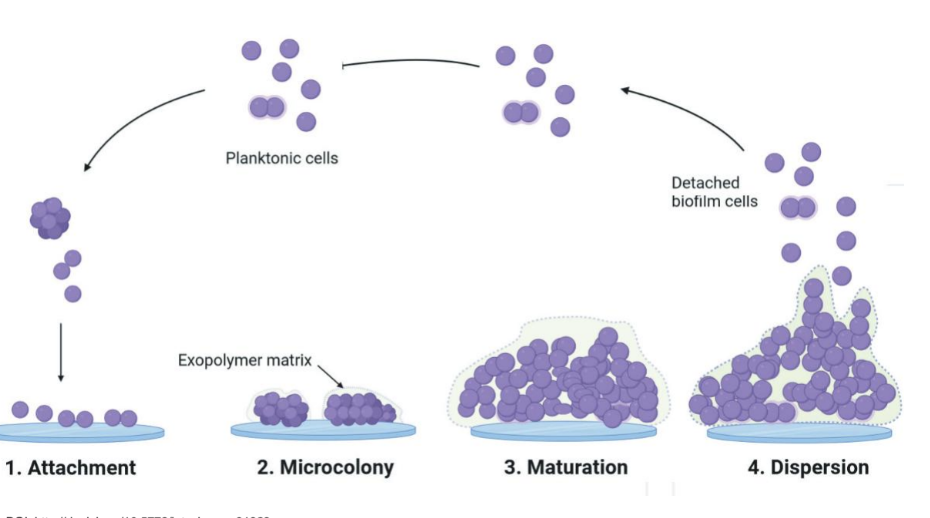
What are the general steps of biofilm formation?
Initial attachment of bacteria to a surface.
Microcolony formation as bacteria multiply
Maturation of biofilm structure.
Dispersion of cells to colonize new surfaces.
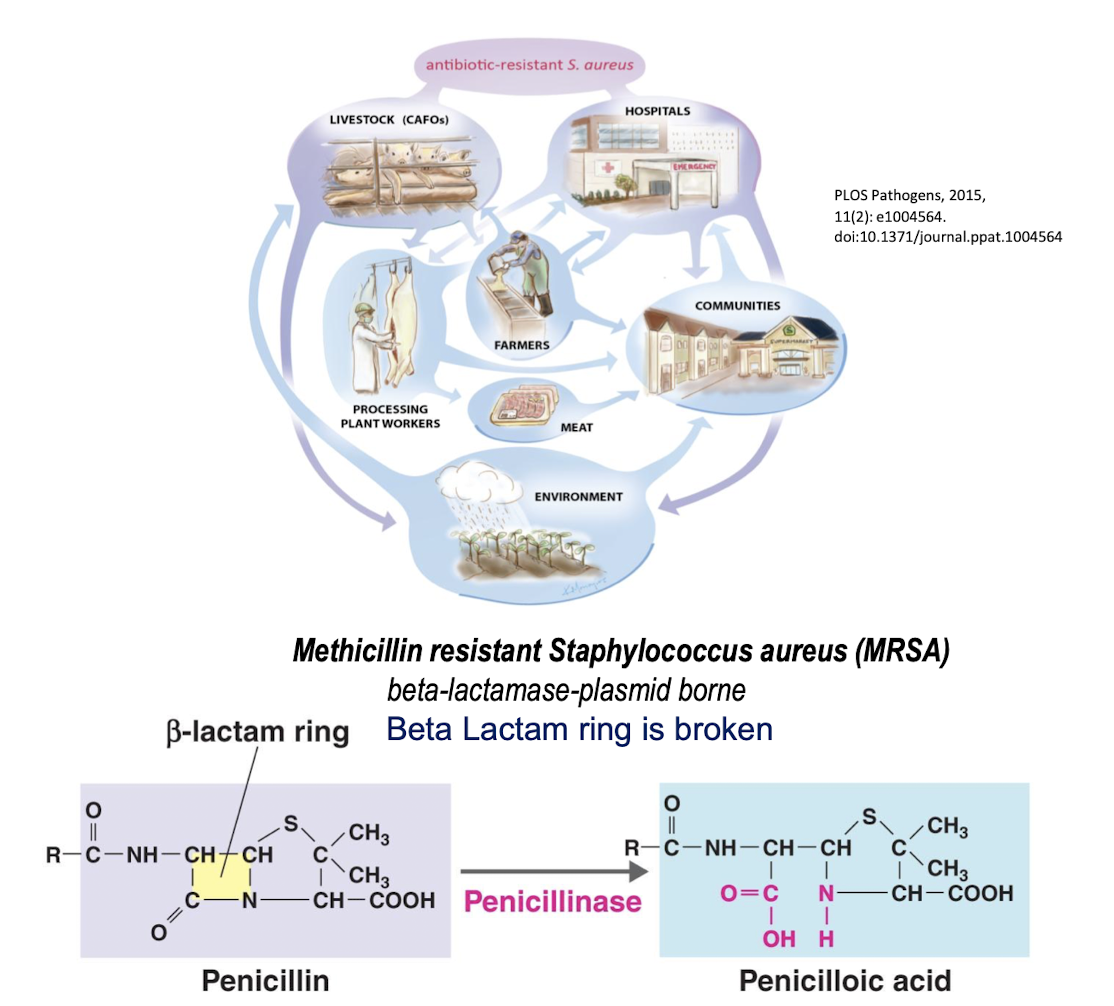
Methicillin-resistant Staphylococcus aureus (MRSA)
A strain of Staphylococcus aureus that is resistant to ALL methicillin and other beta-lactam antibiotics
Breaks down the B-lactam ring in Penicillin into Penicilloic acid by penicillinase
what are some features of Clostridia and some examples?
Gram-positive, anaerobic, endospore-forming bacillus
Ubiquitous in soil, water, and gastrointestinal tracts of animals and humans –
*Endospores allow for survival in harsh conditions – eg: C. perfringens , C. difficile – C. botulinum – C. tetani
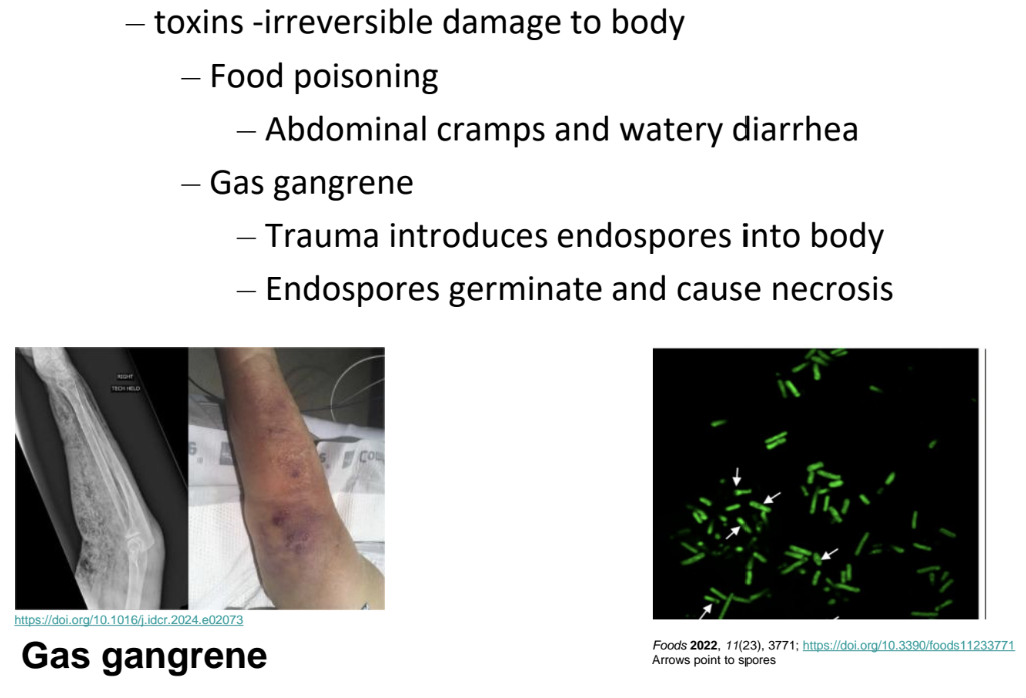
what does Clostridium perfringens cause?
*endospores are only produced under certain conditions, NEVER by GN
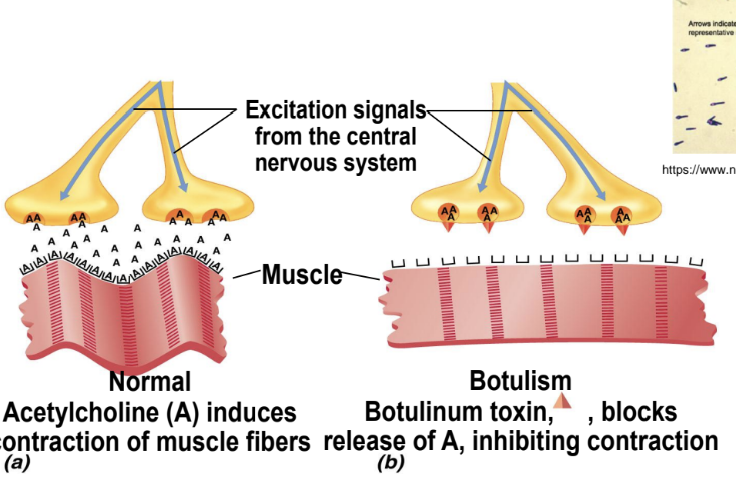
Clostridium botulinum + botulism
The bacterium that produces botulinum toxin, leading to botulism and paralysis, used for cosmetic purposes in small doses and as a treatment for various medical conditions.
Anaerobic, endospore-forming, Gram-positive bacillus
Common in soil and stagnant water
Botulism results when the endopsores germinate and produce botulism toxins
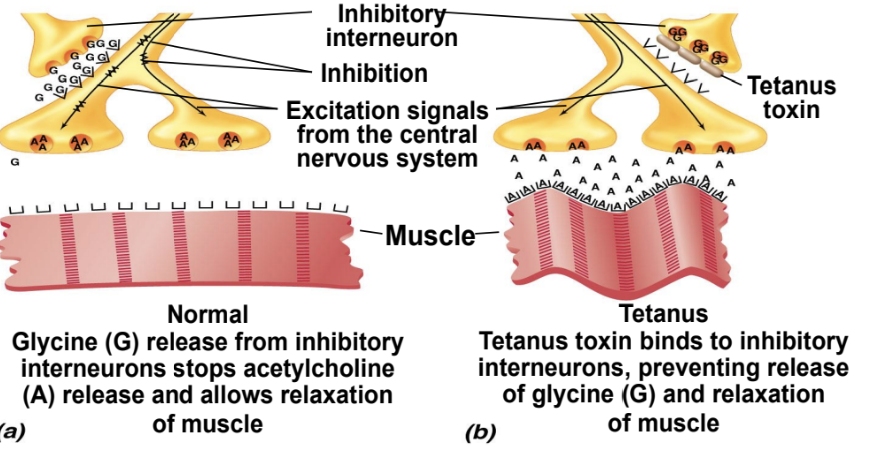
What is Clostridium tetani?
– Ubiquitous in soil, dust, and GI tract of animals and humans
– Tetanus results when endospores germinate and produce tetanus toxin
Mechanism:
Clostridium difficile
– Common member of the intestinal microbiota
– Opportunistic in patients taking broad-spectrum antimicrobial drugs
Minor infections causes self-limiting explosive diarrhea
– Serious cases: Pseudomembranous colitis
– Life-threatening

A disease caused by Clostridium difficile, following broad spectrum antibiotic treatment, leading to severe diarrhea and colitis.
- Produces enterotoxins that damage intestines
• Increasingly more common in community-acquired diarrhea
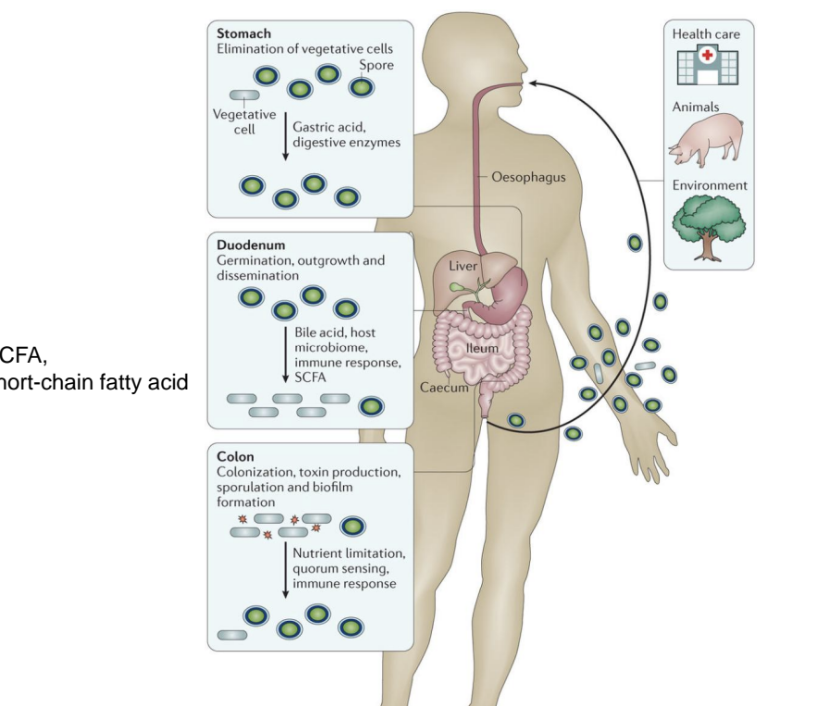
what is the life cycle of C. difficle
Contraction from healthcare settings, animals, the environment
Spore formation by elimination of vegetative cells, survive gastric acid and digestive enzymes
Germination, outgrowth and dissemination in the duodenum
Colonisation in the colon, toxin production and inflammation
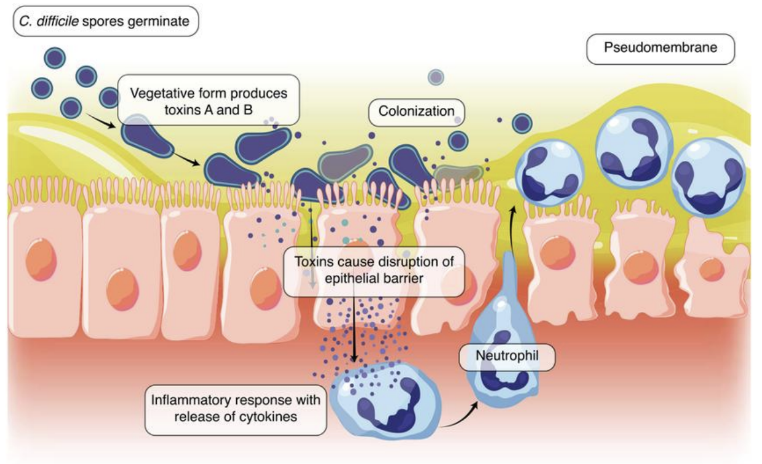
how does C. difficile cause disease in the large bowel?
Production of toxins A and B, which damage intestinal epithelial cells, leading to inflammation, diarrhea
Formation of pseudomembranes where mucous and cellular debris are expelled into the lumen, resulting in symptoms associated with pseudomembranous colitis.
Diagnosis, treatment, and prevention of Clostridium difficile
Discontinue causative antimicrobial drug to resolve minor infections
Serious cases treated with antibiotics treatment (selected carefully)
Prevention- proper hygiene to limit nosocomial infections