CR05 - CO and the Cardiac Cycle
1/56
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
57 Terms
What is cardiac output (CO)?
The amount of blood pumped from each ventricle in 1 min, expressed in L/min.
What factors affect cardiac output?
Heart rate
Contractility
Preload
Afterload
What is end-diastolic volume (EDV)?
Volume in the ventricle before ejection (at the end of diastole). It is preload dependent.
What is end-systolic volume (ESV)?
Volume remaining in the ventricle after ejection (at the end of systole). It is contractility-dependent.
What is the equation for stroke volume?
SV = EDV - ESV
What is the equation for cardiac output?
CO = SV * HR
CO = (EDV - ESV) * HR
What 2 factors determine cardiac output?
CO is a function of HR and SV.
What is HR determined by?
The rate of depolarization of autorythmic cells (rate of phase 4 depolarization).
What slows HR?
Parasympathetic innervation.
What speeds up HR?
Sympathetic innervation and epinephrine from the adrenal medulla.
What is SV determined by?
The force of contraction in the ventricular myocardium.
What is SV influenced by?
Contractility and the length-tension relationship of muscle fibers.
Which factors affect contractility?
Sympathetic innervation and venous return.
What factors influence the length-tension relationship of muscle fibers?
It varies with venous return, which is aided by the skeletal muscle pump and the respiratory pump.
What factors affect EDV?
Filling pressure (increased preload → increased CO)
Filling time (increased HR → decreased filling time)
Ventricular compliance (increased compliance → increased volume)
What factors affect ESV?
Afterload (increased afterload → decreased CO)
Contractility (positive inotropes → increase CO)
Which factors have no effect on CO?
Sleep, moderate changes in environmental temperature.
What factors increase CO?
Anxiety and excitement, eating, exercise, high environmental temperature, pregnancy, epinephrine, histamine
What factors decrease CO?
Sitting up or standing from lying position, rapid arrhythmia, heart disease
What is the ejection fraction (EF)?
It is a measurement, expressed as a percentage, of how much blood the LV pumps out with each contraction.
What is EF an indicator of?
Contractility/heart efficiency.
What is the equation for EF?
EF = SV/EDV
(fraction of EDV that is ejected in one stroke)
What is the normal range for EF?
0.55-0.65 or 55%-65%.
What happens during diastole?
Events associated with ventricular relaxation and filling.
What happens during systole?
Events associated with ventricular contraction and ejection.
How is the duration of the cardiac cycle related to HR?
The duration of the cardiac cycle is the reciprocal of heart rate.
HR = 1/cardiac cycle.
What always precedes mechanical contraction in the heart?
Electrical activation.
What are the phases of diastole?
Isovolumetric relaxation (valves are closed after systole)
Filling (AV valves open)
Rapid ventricular filling
Decreased ventricular filling (diastasis)
Atrial systole (additional filling with atrial contraction)
What are the phases of systole?
Isovolumetric contraction (valves close after diastole)
Ejection (semilunar valves open)
Rapid ventricular ejection
Decreased ventricular ejection
What is phase 1 of valve activity?
Inflow phase: the inlet valve is open (for filling), and the outlet valve is closed.
What is phase 2 of valve activity?
Isovolumetric contraction: both valves are closed with no blood flow (after filling has occured).
What is phase 3 of valve activity?
Outflow phase: The outlet valve is open (for ejection), and the inlet valve is closed.
What is phase 4 of valve activity?
Isovolumetric relaxation: Both valves are closed with no blood flow (after ejection).
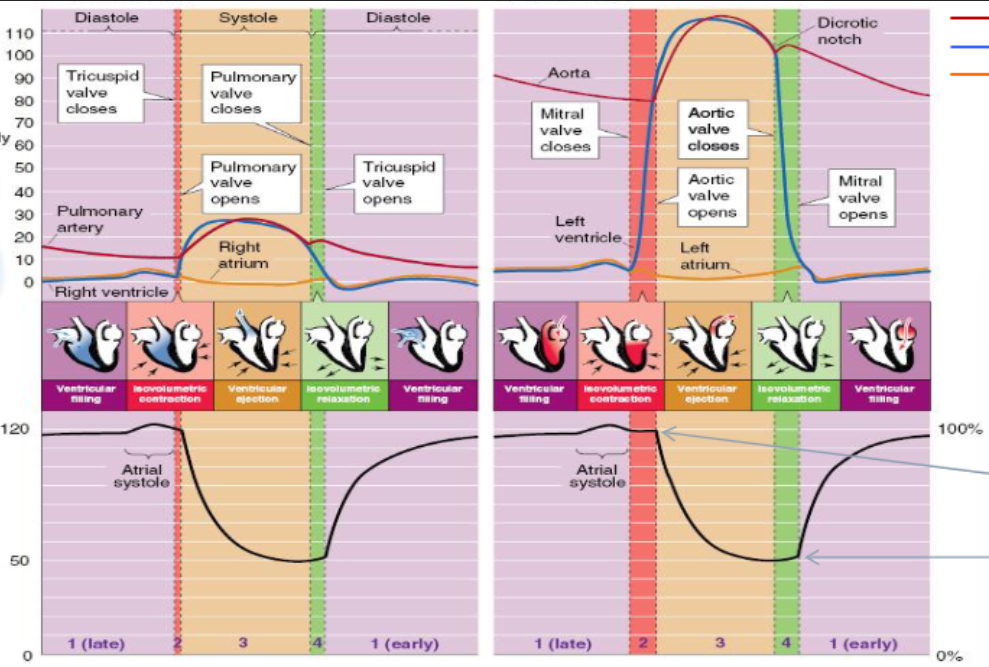
What is Wigger’s diagram?
A diagram outlining the pressure and volume changes of the heart chambers throughout the cardiac cycle.
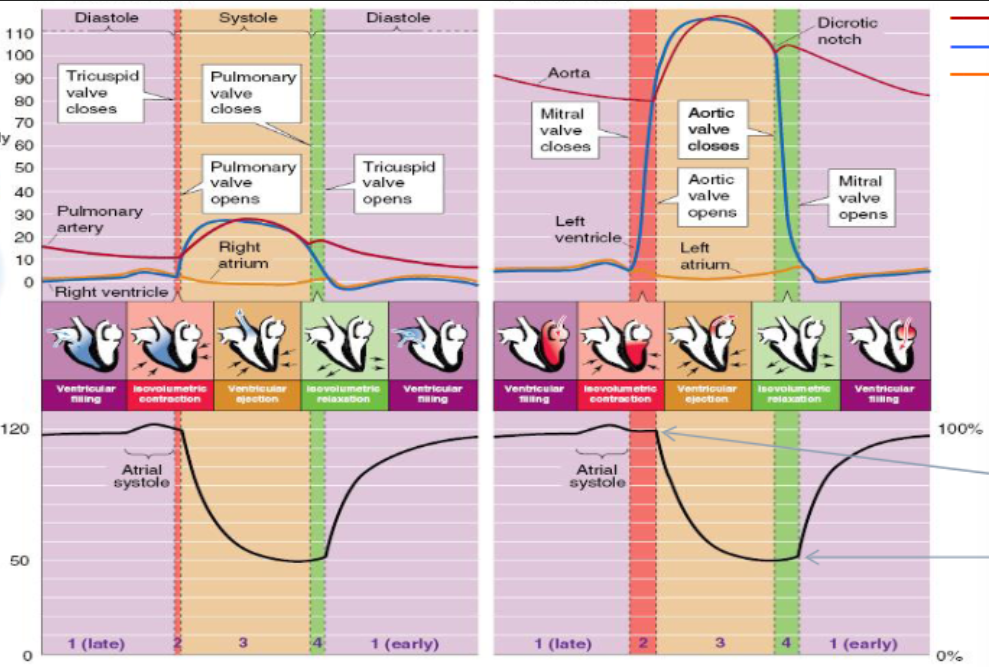
Which ventricle has a higher pressure profile during systole?
The LV, because it pumps blood to the systemic circulation which has higher pressure than the pulmonary circulation.
What are the events of the cardiac cycle?
Atrial systole
Isovolumetric ventricular contraction
Rapid ventricular ejection
Reduced ventricular ejection
Isovolumetric ventricular relaxation
Ventricular filling (rapid and reduced/diastasis)
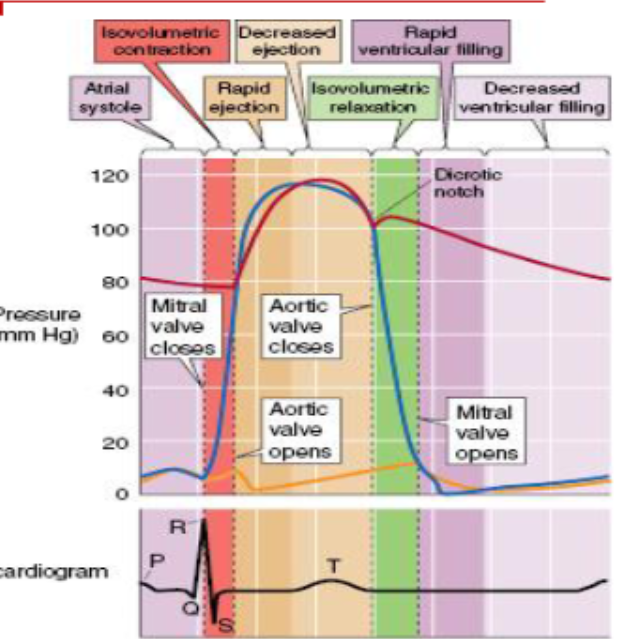
Which phase follows the P wave?
Atrial systole.
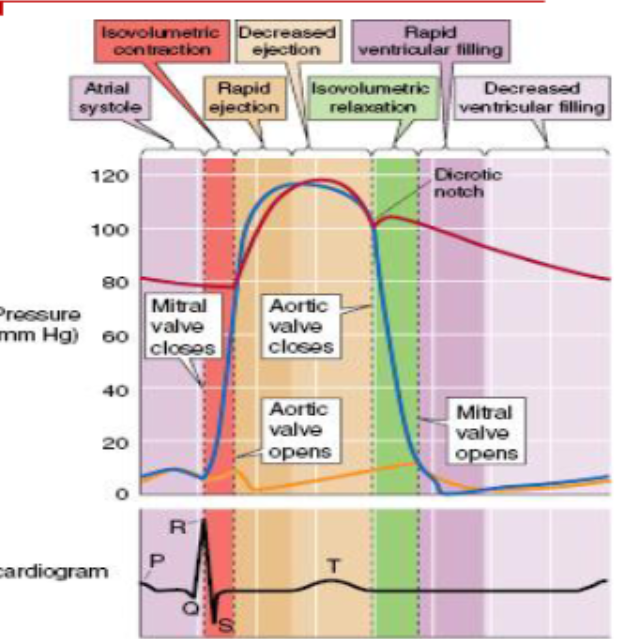
Which phase follows the QRS complex?
Isovolumetric contraction, rapid ejection, and then decreased ejection (later on).
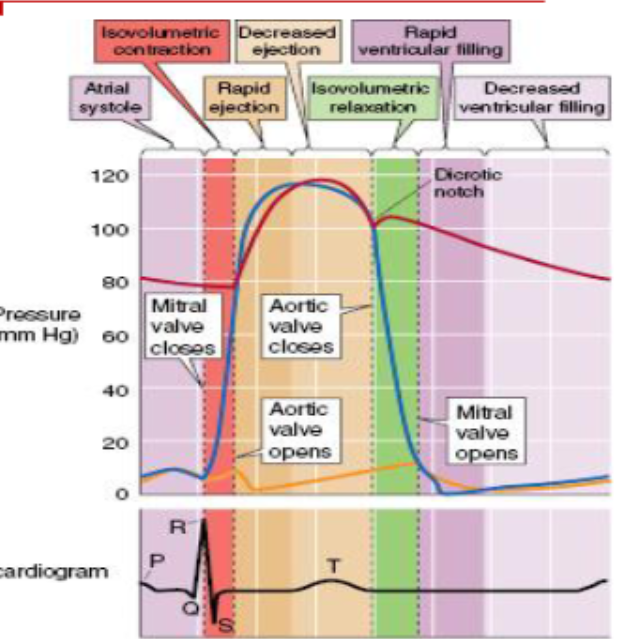
Which phase follows the T wave?
Isovolumetric relaxation.
What causes the S1 heart sound?
Closure of the AV (tricupsid and mitral) valves (onset of systole).
What causes the S2 heart sound?
Closure of semilunar (aortic and pulmonary) valves.
What causes the S3 heart sound?
Diastolic filling.
What causes the S4 heart sound?
Atrial contraction.
Which heart sounds are irregular/should not be heard in healthy patients?
S3 and S4; you should not normally be able to hear atrial contraction and diastolic filling unless there is a volume overload or regurgitation.
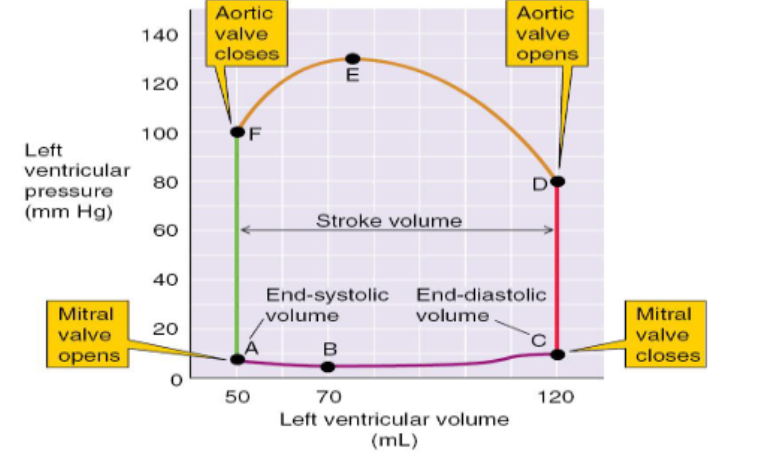
What does a ventricular pressure-volume loop show?
The change in pressure of a ventricle as it changes in volume.
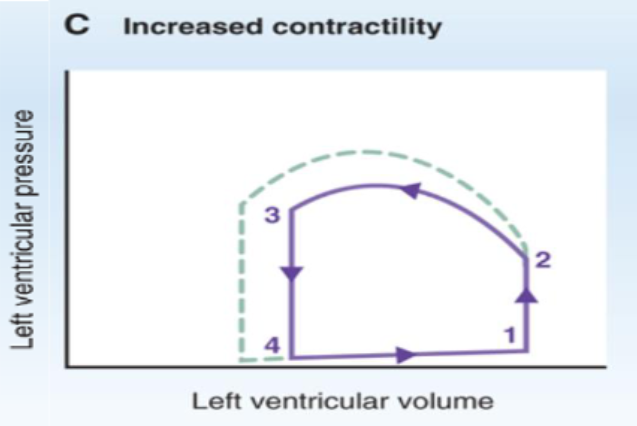
How does increased contractility affect a PV loop?
Increased contractility decreases ESV which increases SV.
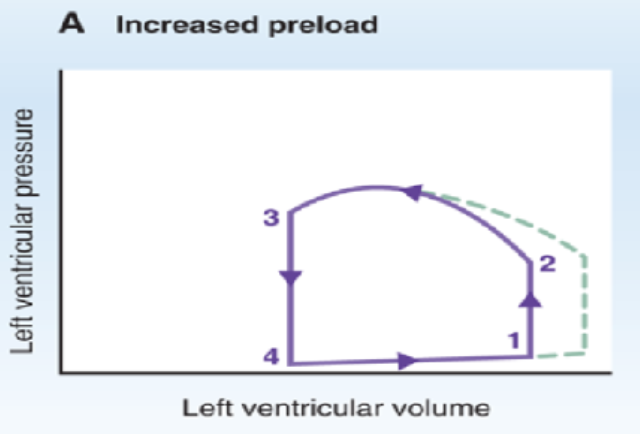
How does increased preload (EDV) affect a PV loop?
Increased preload increases EDV which increases the SV.
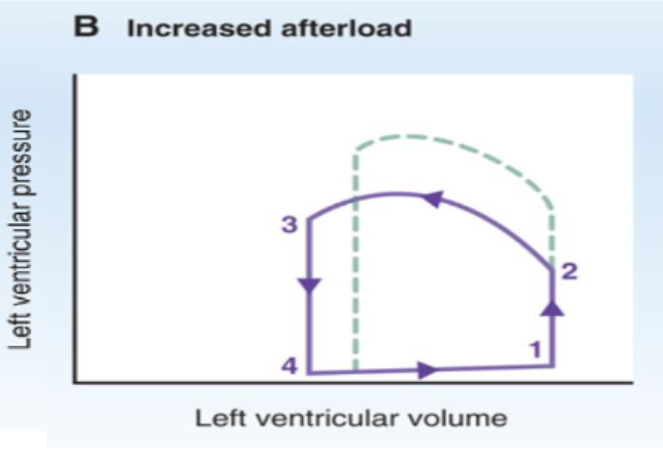
How does increased afterload (aortic pressure) affect a PV loop?
Increased afterload increases ESV, which decreases the SV.
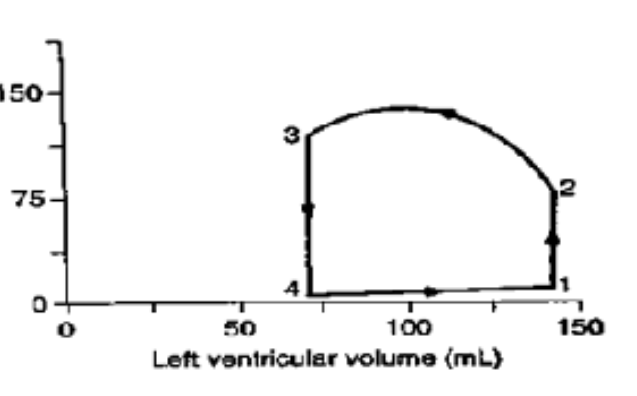
Where does isovolumetric contraction occur on a PV loop?
1 → 2
At which point does the aortic valve close on a PV loop?
3
Where can you find ESV and EDV on a PV loop?
ESV = volume at point 4, EDV = volume at point 1.
EDV - ESV = SV
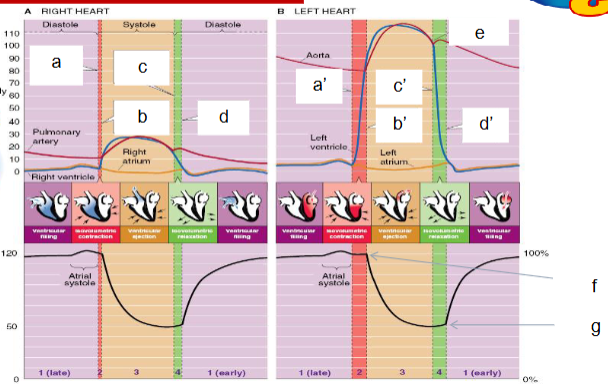
What does a indicate?
Tricupsid valve closes.
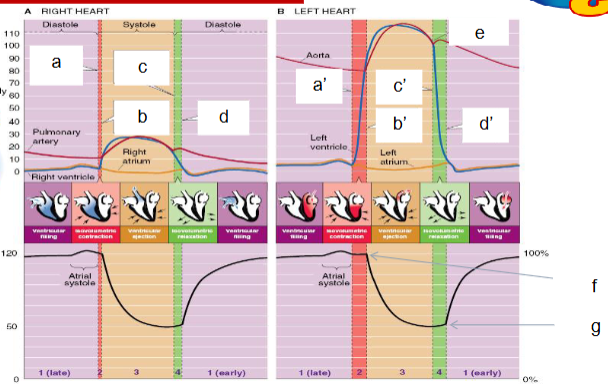
What does b indicate?
Pulmonary valve opens.
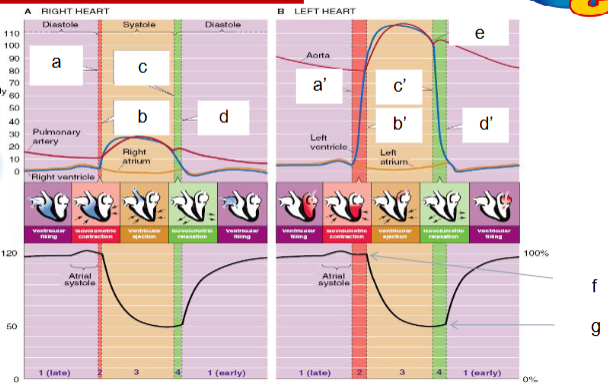
What does c indicate?
Pulmonary valve closes.
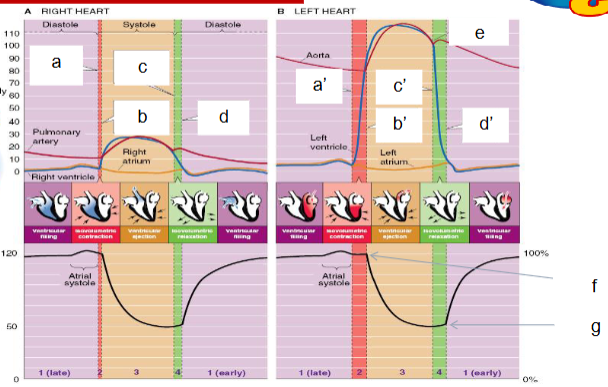
What does d indicate?
Tricupsid valve opens.
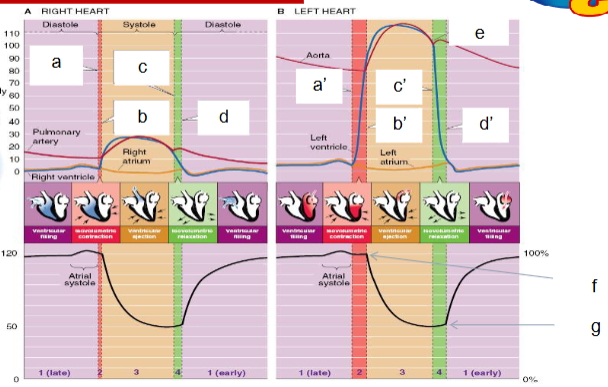
What does f indicate?
The LV end diastolic volume.
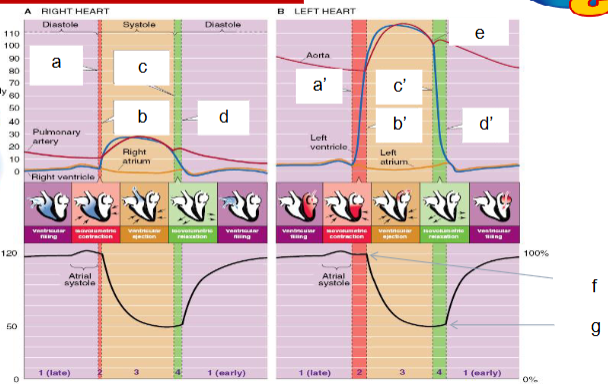
What does g indicate?
The LV end systolic volume.