Week 4: Stages & Phases of Labor
1/70
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
71 Terms
What is Labor?
function of the patient by which the products of conception (fetus, amniotic fluid, placenta and membranes) are separated and expelled from the uterus through the vagina to the outside world
True Labor
cervix: softens, effaces, dilates, moves anteriorly
contractions: longer, stronger and closer together; worsen w/ activity; continue despite position change or comfort measures
regular contraction pattern
pain location: lower back radiating to lower abdomen
False Labor
cervix: little to no change, posterior position
contractions: intensity doesn’t increase; interrupted w/ meds, walking or position change
irregular contraction pattern
pain location: back or upper fundal area
Contractions from the [blank] help push the baby out
top bottom
Contractions from the [blank] keeps the baby in
sides
What contraction pattern indicates its time to go to the hospital?
contractions every 5 min, lasting >60 seconds for >1 hr
What Maternal Factors Lead to Labor Onset?
Stretching of uterine muscles releases prostaglandins
Pressure on cervix triggers oxytocin (Ferguson reflex)
Increased estrogen and decreased progesterone ratios enhance UC
In labor initiation, a decrease in prostaglandins allows for…
increase in oxytocin which stimulates UCs
Ferguson Reflex
A positive feedback reflex during labor in which pressure from the fetal head on the cervix, vagina, or pelvic floor stimulates oxytocin release from the posterior pituitary. Causes stronger UCs, which further increase fetal pressure and oxytocin release until birth.
What Fetal Factors Lead to Labor Onset?
Placental aging & deterioration stimulates UCs
Fetal cortisol production reduces progesterone formation and increases prostaglandin
Prostaglandins from fetal membranes stimulate uterine contractions.
Episiotomy
surgical incision made in the perineum during the second stage of labor to enlarge the vaginal opening and facilitate delivery
Uterus: Active Portion
contracts and helps push baby out
Uterus: Passive Portion
typically lower uterine section; stretches to help the baby come out
List the 5 P’s of Labor
Powers → strength of uterine smooth muscles
Passage → bony boundaries, the cervix and pelvis
Position of patient in labor
Psyche → patient’s emotional state determines response to labor and physiologic functioning
Passengers → fetus & placenta; affected by size, presentation, position, flexion
Effect of Maternal Cortisol on the Labor Process
moderate increase can help w/ labor progession; excessive maternal cortisol related to stress, anxiety, or fear can slow labor progression by slowing cervical dilation, ineffective contractions and causing vasoconstriction
Powers → Uterine Contractions
Force generated by the myometrium that dilates the cervix; most effective when consistent frequency & adequate intensity
Powers → Frequency
The time from the start of one contraction to the start of the next
Powers → Duration
The time from the beginning to the end of one contraction.
Powers → Intensity
Strength of contractions
30-50mmHg per UC necessary for effective labor or >200 mmHg total in 10 min
no more than 5 UCs in 10 min (>280 mmHg)
impacted by pain/fear
Powers → Measuring Methods
Palpation → always confirm w/ palpation ensuring cervix is resting between each UC
Intrauterine pressure catheter (IUPC) → measures mmHg; associated w/ infection, trauma and uterine perforation
External toco → measures frequency & duration NOT intensity
Tachysystole
>5 contractions in 10 min
Hypertonus
Contractions lasting longer than two minutes
Passage and Passenger → Cephalopelvic Disproportion (CPD)
Mismatch between fetal head and maternal pelvis that prevents vaginal delivery; should be reassessed as labor progresses
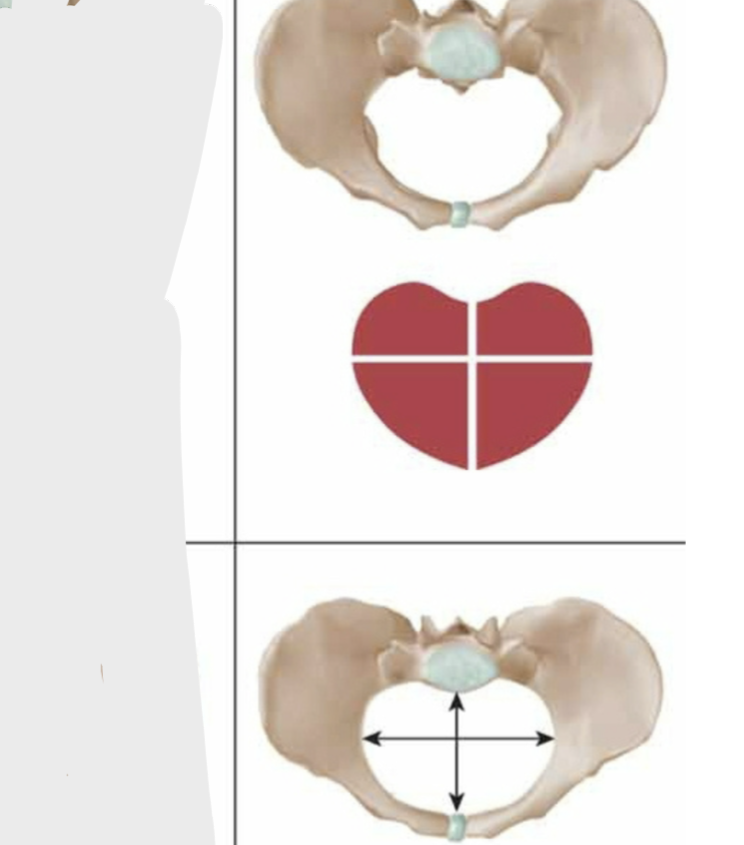
Pelvic Anatomy: Gynecoid
Most favorable pelvis for childbirth; round or transverse oval shape and adequate diameters
favorable for vaginal birth
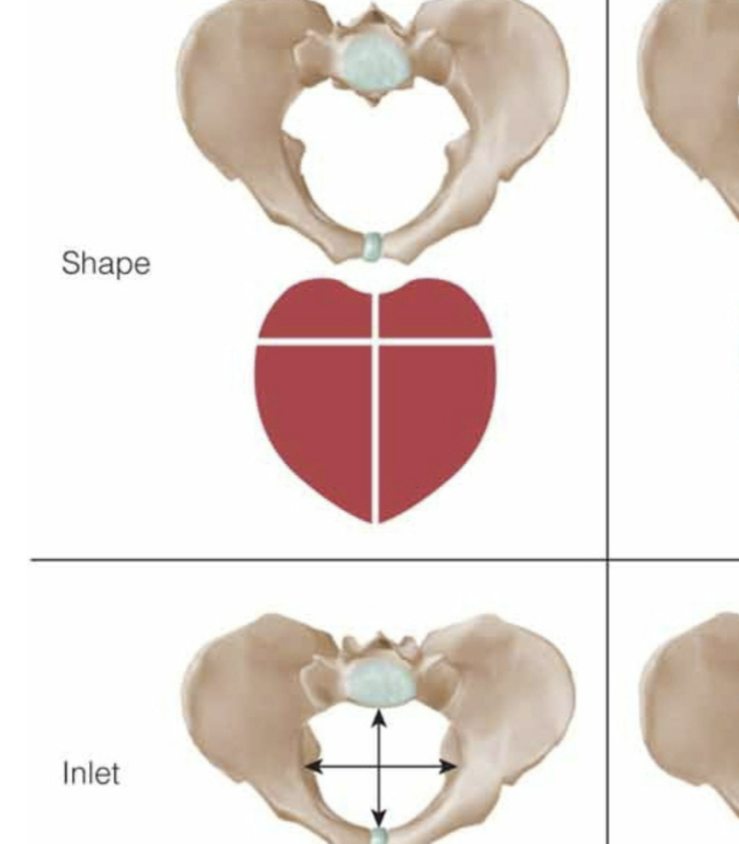
Pelvic Anatomy: Android
pelvis adequate for 20% of assigned males at birth; heart or wedge-shaped; reduced in all diameters; arrest of labor common
not favorable for vaginal birth
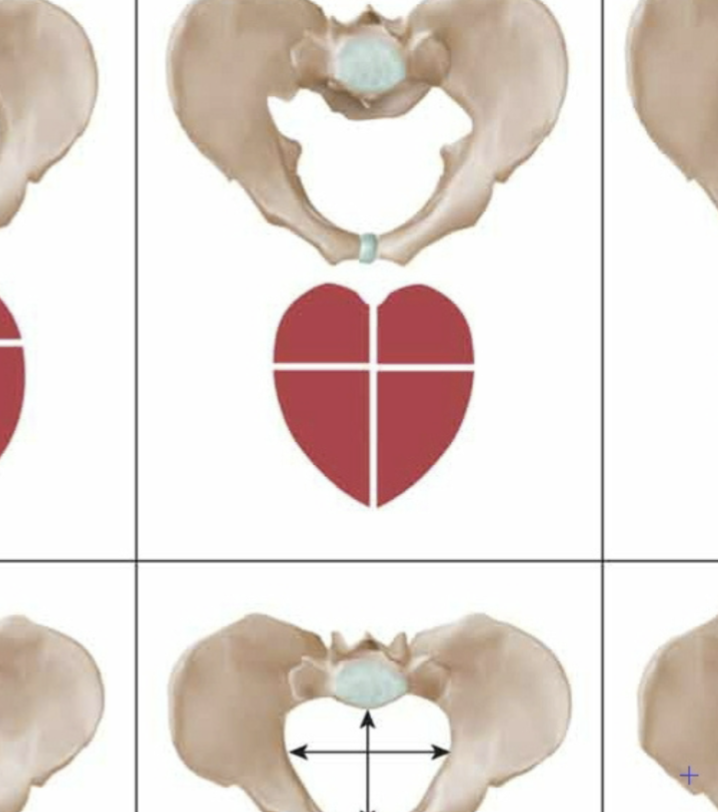
Pelvic Anatomy: Anthropoid
ape like pelvis w/ incidence of 25%; long antero-posterior oval shape; OP presentation is common (sunny-side up)
favorable for vaginal birth
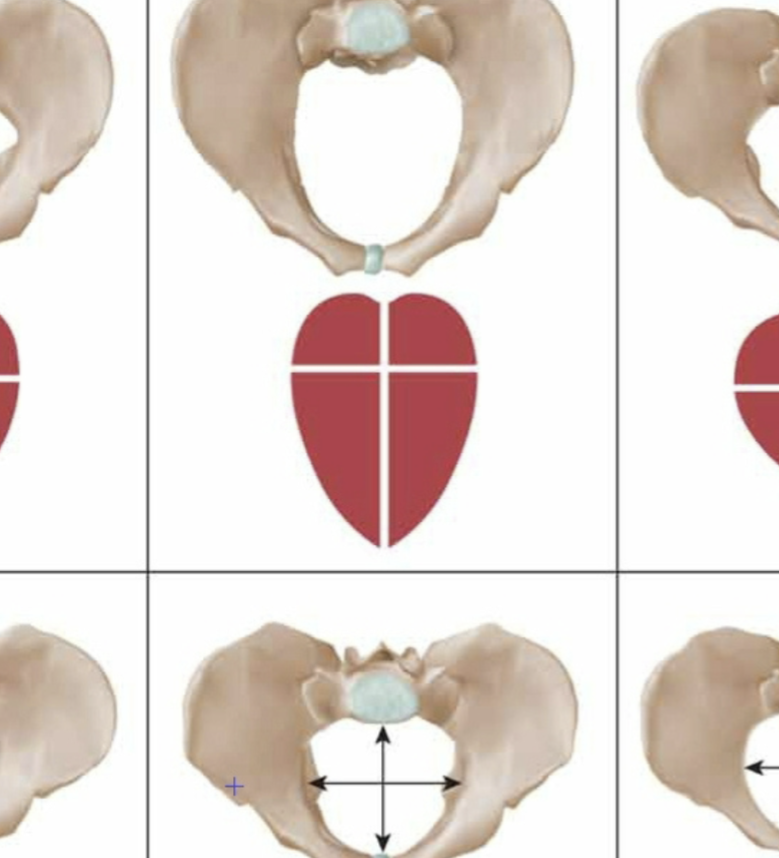
Pelvic Anatomy: Platypelloid
flat w/ incidence of 5%; transverse oval shape; delay of descent at inlet common; c/s common
not favorable for vaginal birth
Passenger → Fetal Lie
Relationship of the fetal spine to the maternal spine
longitudinal, transverse, or oblique
Fetal Presentation
The part of the fetus entering the birth canal first
cephalic → head first
breech → feet first
shoulder
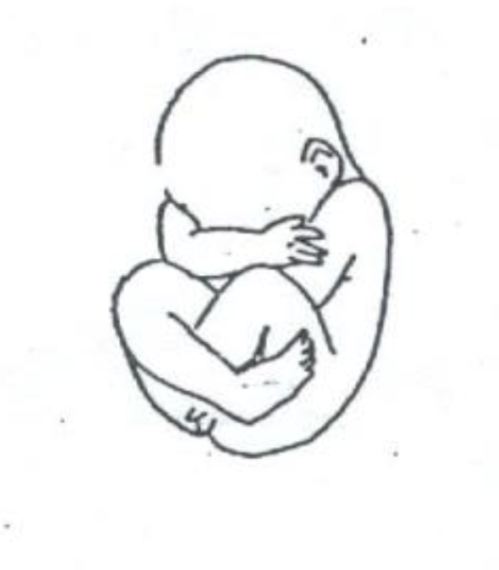
Fetal Presentation → Cephalic Vertex
most common and ideal presentation for vaginal birth; head fully flexed, with the chin tucked to the chest; allows the smallest diameter of the fetal head to pass through the pelvis
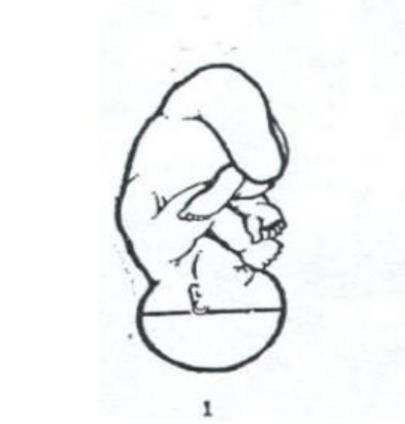
Fetal Presentation → Cephalic Military OR Sinciput
can still deliver vaginally; head is neutral aka “looking straight”; diameter is wider making descent slower/more difficult
Fetal Presentation → Cephalic Brow
cannot deliver vaginally; fetal head is partially extended, with the forehead (brow) presenting first; may require C-section
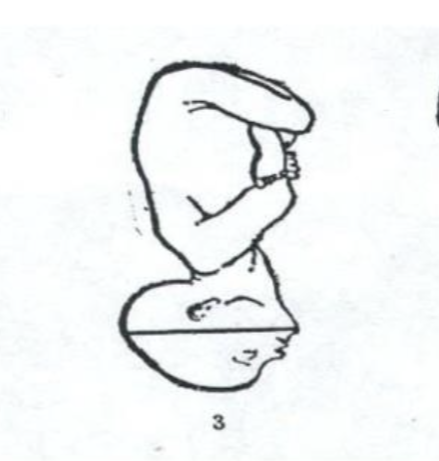
Fetal Presentation → Cephalic Face
vaginal delivery may be possible if chin is anterior; fetal head is fully extended, with the face as the presenting part; may require C-section if mentum posterior

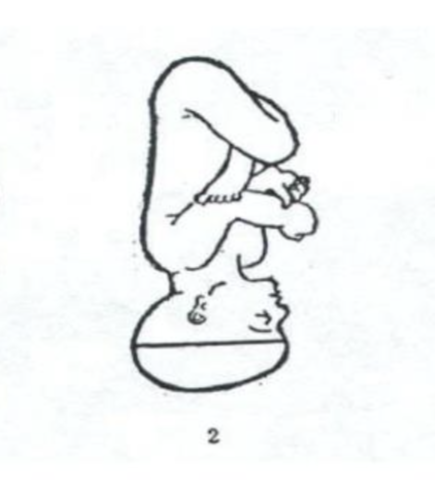
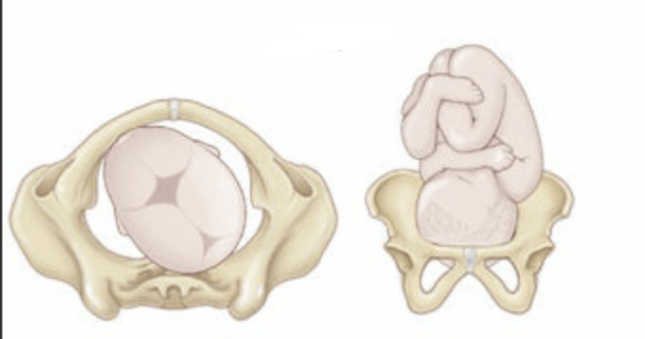
Fetal Presentation → Breech Complete
vaginal delivery sometimes possible; fetus is flexed at both hips and knees, sitting “cross-legged”; risk of umbilical cord compression and birth injury
Fetal Presentation → Breech Frank
vaginal delivery possible but c/s recommended; hips are flexed and knees extended, so the feet are near the head; buttocks are presenting; most commo

Fetal Presentation → Breech Footling
c/s required; one or both hips and knees extended; single or both feet present first; high risk for cord prolapse and fetal injury
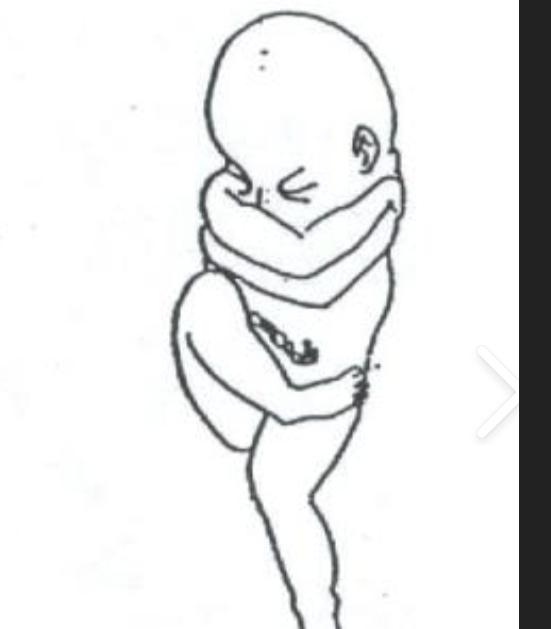
Fetal Presentation → Attitude
Degree of flexion or extension of the fetal body parts (ideal is full flexion)
Fetal Presentation → Position
The relationship of a fetal reference point (occiput, sacrum, mentum) to the maternal pelvis (e.g., ROA, LOA
Assessing Fetal Position → Anterior Fontanelle
Diamond-shaped, larger, soft area; closes by 18 months
Assessing Fetal Position → Posterior Fontanelle
Triangle-shaped, smaller area; closes by 6-8 weeks
Assessing Fetal Position → Occiput
back part of the fetal skull; point of reference when assessing fetal position specifically which way the baby is facing in the mother’s pelvis when the baby is in a cephalic (head-down) vertex presentation
Assessing Fetal Position→ LOA (Left Occiput Anterior)
back of the baby’s head (occiput) is pointing toward the mother’s left front side
Baby’s Face: the mother’s right back side
most common and ideal position for vaginal birth
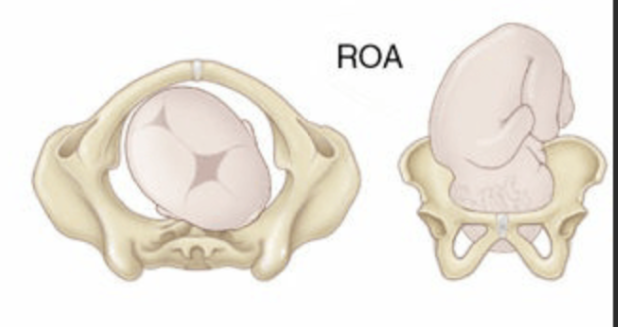
Assessing Fetal Position→ Right Occiput Anterior
back of the baby’s head is pointing toward the mother’s right front side
Baby’s Face: the mother’s left back side
favorable position for vaginal birth
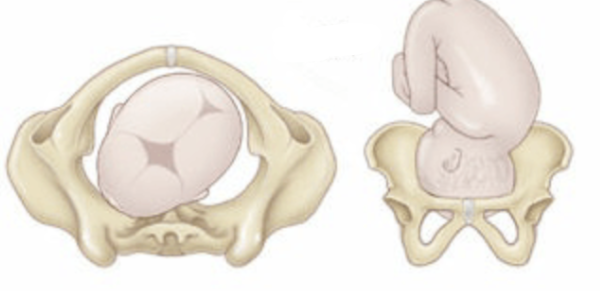
Assessing Fetal Position→ Left Occiput Posterior
back of the baby’s head is pointing toward the mother’s left back side.
Baby’s Face: mother’s right front (up toward her belly button).
Baby is “sunny side up.”
Causes back labor (intense lower back pain)
Labor may be longer or require position changes to help baby rotate anteriorly.
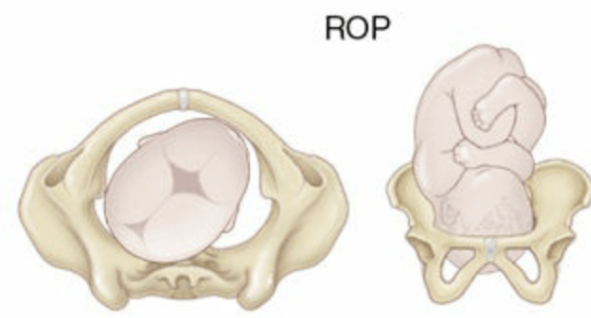
Assessing Fetal Position→ Right Occiput Posterior
back of the baby’s head is pointing toward the mother’s right back side.
Baby’s Face: the mother’s left front side.
leads to back pain and slower labor
rotates to anterior position during labor, but may need maternal repositioning to assist.
Fetal Cardinal Movements Order
this is in the most ideal scenario:
Engagement → Descent → Flexion → Internal Rotation → Extension → External Rotation (Restitution) → Expulsion
Fetal Station → Engagement
when the widest diameter of the presenting part has passed the inlet, usually station 0; comes after floating; rate at which this occurs dependent on number of previous deliveries
if head not engaged, cord prolapse can occur
Fetal Station → Floating
presenting part is out of pelvis and freely moveable in inlet; comes before engagement; stations -3 to -2
Fetal Station → Descent
head moves deeper into pelvis; comes after engagement; stations +1 tp crowning
How Does Psyche Impact Labor?
fear related to past experiences (own or others); emotional readiness; stress; unwanted pregnancy and more all impact the labor process in a negative or positive way; as nurse you listen, educate, support
Nurs Interventions of 5 P’s → Powers
facilitate effective uterine contractions
Nurs Interventions of 5 P’s → Passage
minimize risk of infections, complications, etc
Nurs Interventions of 5 P’s → Position
facilitate maximum pelvic capacity
Nurs Interventions of 5 P’s → Passengers
facilitate fetal cardinal movements with position changes
Nurs Interventions of 5 P’s → Psyche
minimize anxiety & fear associated w/ labor; maximize coping strategies knowledge & understanding
Physical Assessment → Initial Admit
Complete Systems Assessment: review of systems, urinary protein + glucose (GDM, preeclampsia), Leopold’s to determine fetal position (ultrasound, SVE), fundal height, signs of preeclampsia, signs of domestic abuse/support
Evaluate for Risk Factors: review H&P (prenatal), prior OB hx, current pregnancy info
Ask about Labor Symptoms & Fetal Status: O2 status of patient/fetus, assessment of labor tolerance
Physical Assessment → Ongoing
frequency dependent on labor progression, signs & symptoms but generally speaking:
General assessment → hydration (I&Os q4hr), vitals (including FHR pattern + pain)
Abdominal → contraction pattern, confirm uterine relaxation, pain NOT associated w/ contractions
Vaginal → bleeding, discharge, ROM (time, color, odor), cervical exam (dilation, effacement, fetal station)
Emotional → ongoing
How often should vitals be checked when in active labor?
q1hr
Frequency of Fetal Assessment w/ EFM → Low Risk w/o Oxytocin
latent phase (<4cm): q1hr
latent phase (4-5cm): q30min
active phase (>6cm): q30min
2nd stage (passive fetal descent): q15min
2nd stage (active pushing): q15min
Frequency of Fetal Assessment w/ EFM → w/ Oxytocin OR Risk Factors
requires closer monitoring b/c process isn’t 100% natural
latent phase (<4cm): q15-30min
latent phase (4-5cm): q15min
active phase (>6cm): q15min
2nd stage (passive fetal descent): q15min
2nd stage (active pushing): q5min
Hyperventilation in Labor
common w/ anxiety; can occur using relaxation breathing techniques; results in respiratory alkalosis
symptoms: lightheadedness, dizziness, tingling of fingers, spasms in hands/feet, numbness
nurs interventions: replace bicarb ions by rebreathing CO2 (breathing into cupped hands or paper bag)
Lab Values → Platelets & WBCs
platelets → decreased at term due to hemodilution and increased consumptions
WBCs → increase during labor (~25,000) b/c body experiencing trauma
Stages of Labor → 1st (Latent Phase)
cervix dilated 0-6cm; contractions (mild to moderate) transitioning from irregular to regular (q5-30min, lasting 30-45 seconds); longest phase
maternal response: excited, talkative, eager; may be anxious about the start of labor
nurs interventions: assist w/ positioning, monitor maternal/fetal status, integrate support persons (doula, family, etc), implement pain management, monitor I&Os, implement infection prevention measures
Stages of Labor → 1st (Active Phase)
cervix dilated 6-10cm; contractions (moderate to strong) (q2-5min, lasting 45-60 seconds)
maternal response: serious, focused, and less talkative; may feel anxious or fatigued
nurs interventions: assist w/ positioning, monitor maternal/fetal status, integrate support persons (doula, family, etc), implement pain/comfort management, monitor I&Os, implement infection prevention measures; prepare for delivery
Stages of Labor → 2nd
cervix dilated 10cm; contractions (strong) (q2-3min, lasting 60-90 seconds); ends w/ delivery of baby
maternal response: intense focus on pushing; may feel relief when allowed to push; sense of control alternates with fatigue
nurs interventions: encourage rest during latent phase, optimize oxygenation (open glottis pushing, side-lying, push every other UC), monitor FHR, prepare for newborn care + skin-to-skin contact, resuscitation equipment ready
Stages of Labor → 3rd
known as delivery of placenta
nurs interventions: facilitate bonding (skin to skin), observe for signs of placental separation, monitor for increased bleeding (hemorrhage), inspect placenta for abnormalities
Stages of Labor → 4th
known as recovery/postpartum phase (1-4hr); focus on maternal stabilization, bonding and initiation of breastfeeding
nurs interventions: monitor VS/fundus/lochia (Q15 min for 1 hr, Q30 min × 2 until stable), QBL (weigh pads, 1mg = 1mL), oxytocin (IV/IM) for hemorrhage prevention, fundus should be firm and midline at or below umbilicus; assess bladder function, encourage voiding, evaluate perineum using REEDA, assess/manage pain, monitor for signs of hemorrhage or infection
Signs of Placental Separation
Gush of blood, lengthening of cord, change in shape of fundus
Shiny Schultz: fetal side of the placenta
Dirty Duncan: maternal side of the placenta
QBL for Hemorrhage
≥ 500 mL
What Reflex Might be Suppressed due to Pitocin
Ferguson reflex
Open-Glottis Pushing Technique
Encourages exhalation during pushing to maintain oxygenation and reduce maternal/fetal hypoxia compared to Valsalva pushing; can lead to low APGARs
discourage breath-holding
limit pushing to 3x per contraction for 6-8 seconds each