3.3.4.1 mass transport in animals
1/109
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
110 Terms
how is blood forced through blood vessels?
by contraction of the muscular chambers of the heart
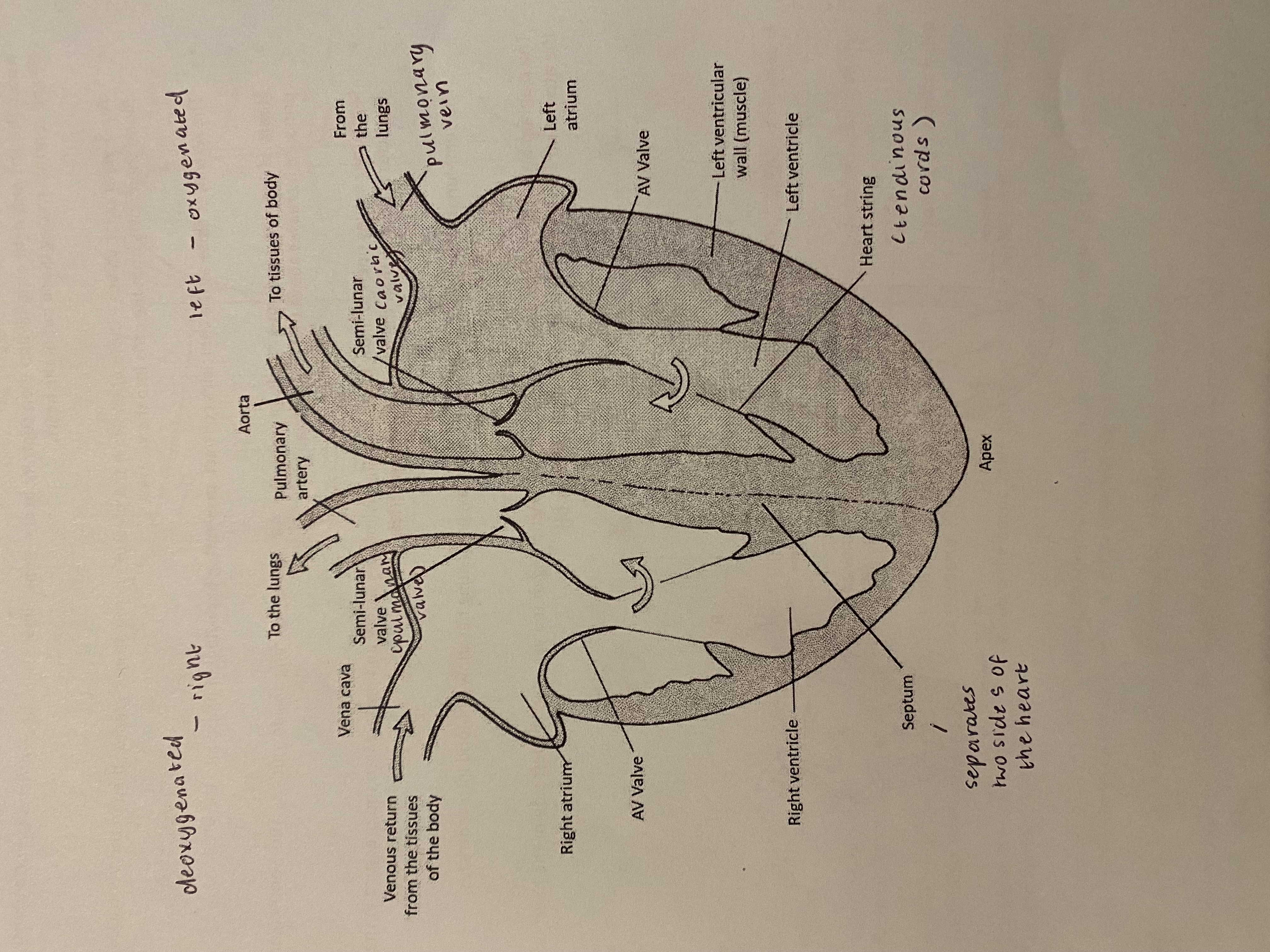
briefly outline the structure of the heart
the heart has right and left sides, each having an atrium + a ventricle
define:
a. atria
b. ventricles
a. thin muscular walls receiving low pressure blood returning to the heart in veins
b. thick muscular walls that contract to move blood at high pressure into arteries
give the roles of the right atrium + ventricle
right atrium — receives deoxygenated blood from the body (except the lungs) via the vena cava
right ventricle — contracts to move deoxygenated blood into the pulmonary artery leading to the lungs
give the roles of the left atrium + ventricle
left atrium — receives oxygenated blood from the lungs via the pulmonary veins
left ventricle — contracts to move oxygenated blood into the aorta leading to the rest of the body
state a difference between the structure of the left + right ventricle & explain why
left ventricle has a much thicker muscular wall than the right ventricle
when it contracts it produces a greater pressure, as it has to pump blood a greater distance ie to all parts of the body
whereas the right ventricle only supplies blood to the lungs
outline the purpose of heart strings/tendinous cords
they prevent the AV valves ‘turning inside out’ or inverting as the ventricular pressure increases above that in the atria
veins bring blood…. whilst arteries bring blood…
veins — to the heart
arteries — away from the heart
what do valves prevent?
the back flow of the blood
what does the septum do?
it separates the two sides of the heart
the left side of the hearts pumps….. whilst the right side of the heart pumps….
left → oxygenated
right → deoxygenated
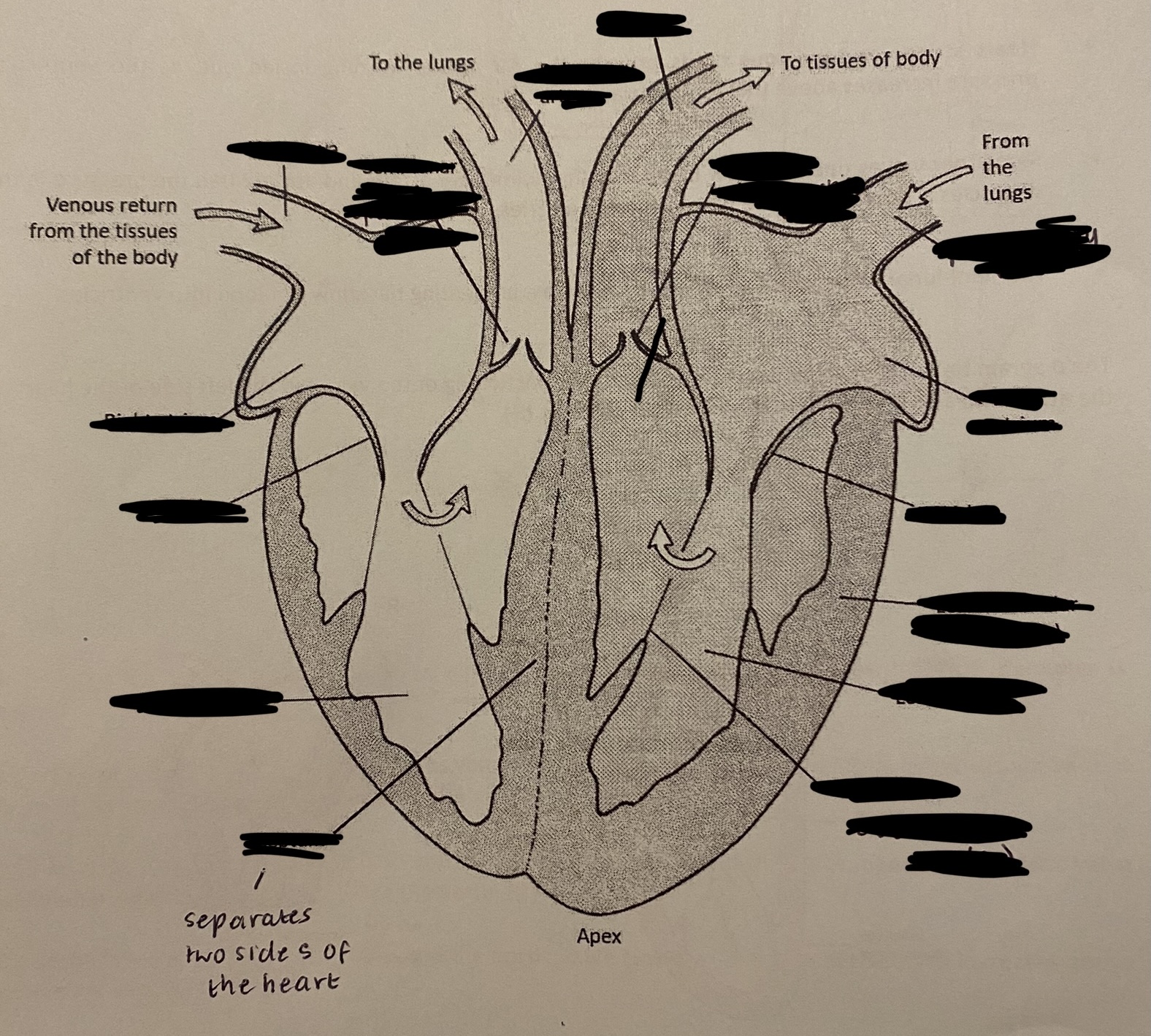
label the diagram
briefly describe the movement of the atria + ventricles during the cardiac cycle
the left + right atria fill + then contract at the same time
then the ventricles simultaneously fill + contract forcing blood out of the heart
where are atrioventricular valves found?
between the atrium + ventricle
when do atrioventricular valves open? and when do they close? mention what happens when they open + close
they open when the pressure in the atria is greater than in the ventricles
blood then flows from the atria into the ventricles
the AV valves close as the ventricles contract, preventing back-flow of blood into the atria
what prevent the AV valves from ‘turning inside out’?
heart strings or tendinous cords
what are the two semi-lunar valves?
aortic valve
pulmonary valve
when + why to semilunar valves open + close?
they open to allow blood into the pulmonary artery + aorta when the pressure in the ventricles is greater than the pressure in the arteries
the semi-lunar valves close as the ventricles relax, preventing back flow of the blood into ventricles
during one heart beat, what changes occur?
volumes + pressures in the heart chambers change
and so does the pressure in the aorta
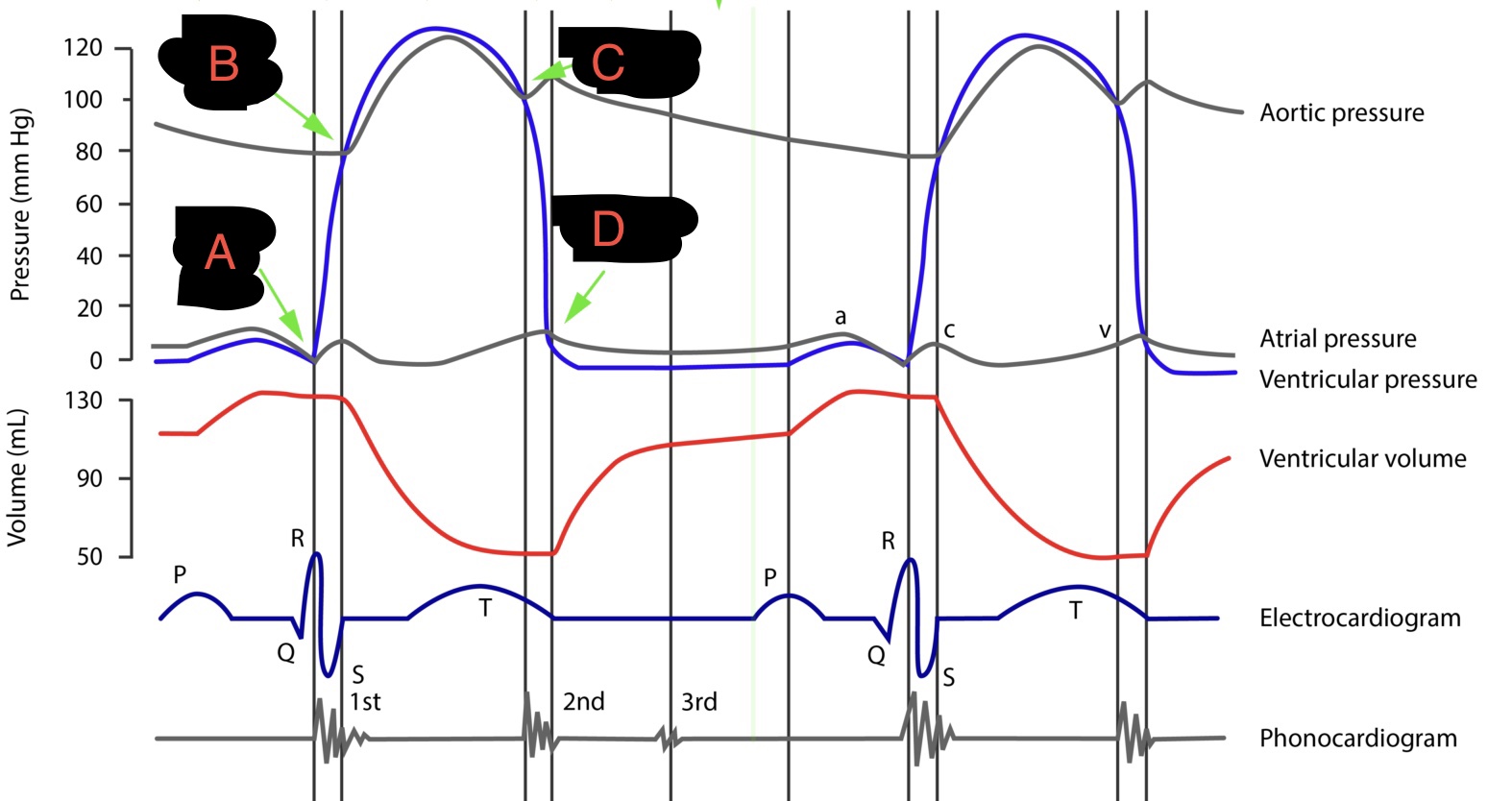
this diagram shows the changes on the left side of the heart.
describe what is happening during the cycle, specifically the four points at A,B,C + D
initially the left atrium contracts, blood flows into the left ventricle, the atrioventricular valve is open
A - the left ventricle contracts, its volume decreases + the pressure inside increases above that in the atrium, closing the AV valve
B - the pressure in left ventricle increases above that in the aorta, opening the aortic valve (semilunar) + blood flows into the aorta
C - left ventricle relaxes + aortic valve closes as pressure in aorta increases above that in the ventricle
D - as the ventricle relaxes, the pressure inside ventricle falls below that in the atrium, the AV valve opens, allowing blood to flow into the ventricle
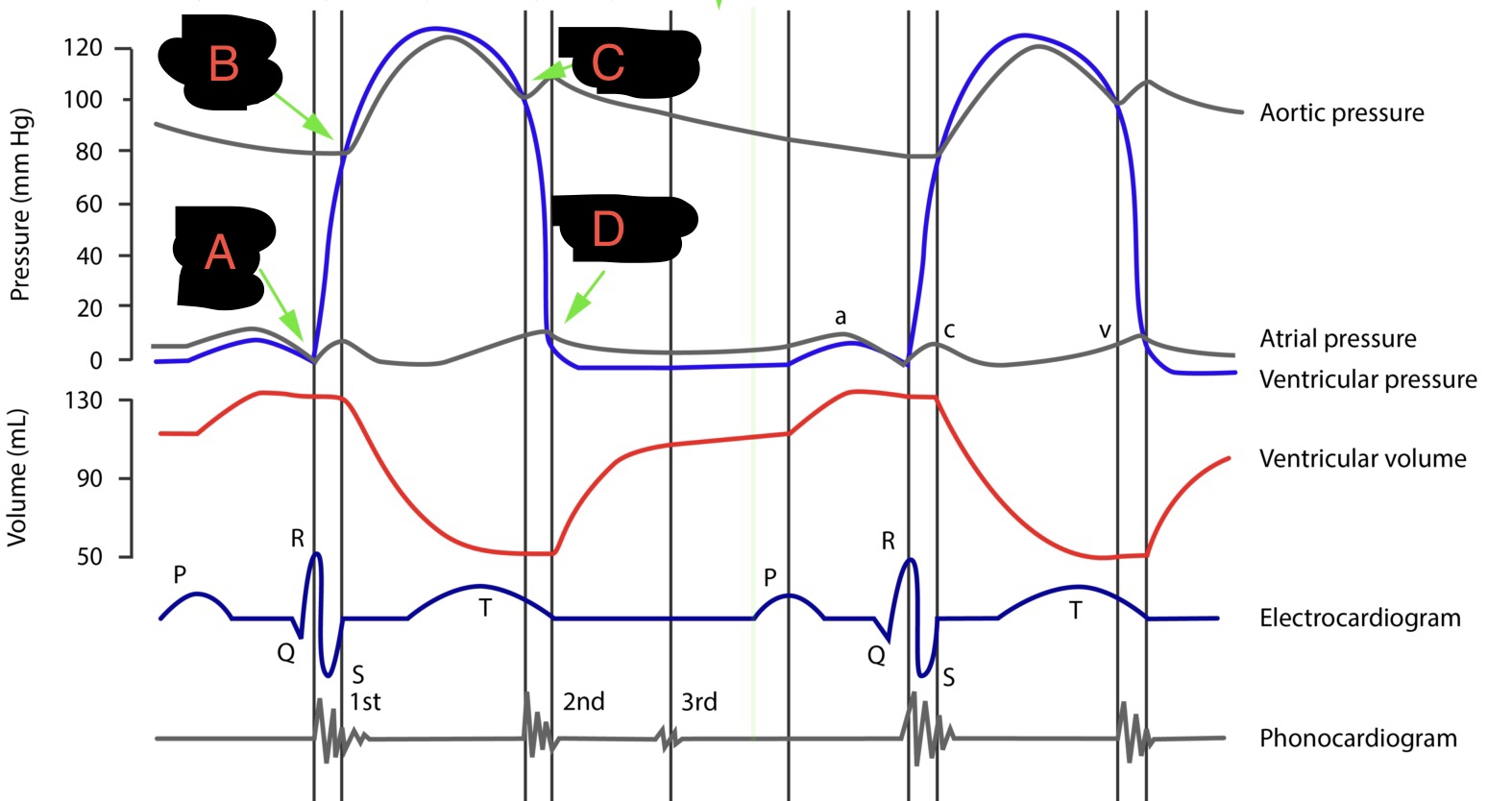
how can you determine heart rate from a graph like this?
divide 60 seconds by the length of one cardiac cycle
(heart rate = 60/one cardiac cycle)
what is cardiac output?
the volume of blood pumped out of one ventricle per minute
how do you calculate cardiac output? give the units of the equation
cardiac output = stroke volume x heart rate
cm³ min⁻¹
what is stroke volume?
the volume of blood expelled from the left ventricle of heart per contraction (beat)
what is heart rate?
the number of contractions (beats) per minute
what happens during exercise regarding our blood rate?
the rate at which venous blood returns to the heart increases
explain what happens due to this increased blood flow to the heart during exercise
it causes the cardiac muscle to contract more strongly, pumping out an increased volume of blood per beat (ie stroke volume increases)
the heart rate also increases during exercise
what happens to the heart muscle + the ventricles due to regular exercise? which results in…
regular exercise causes the heart muscle to produce stronger contractions + the ventricles to be larger in size + volume
this leads to an increased stroke volume + as a result there is a reduction in the resting heart rate
a number of factors increase the risk of _________ disease
cardiovascular (ie diseases of the heart and/or of the blood vessels)
give 6 factors that increase the risk of cardiovascular disease
smoking
high blood pressure
high blood cholesterol levels
prolonged stress
genetic factors
lack of exercise
what is a risk factor?
anything that increases the chance of getting a disease
what does the circulatory / cardiovascular system consist of?
the heart + blood vessels
in mammals there is a ________ circulatory system
double
describe the double circulatory system in mammals
blood is pumped from the heart (right ventricle) to the lungs + returns to the heart (pulmonary circulatory system) before being pumped (left ventricle) to the rest of the body (systemic circulatory system)
name the artery entering + the vein entering the:
a. right ventricle
b. liver
c. kidneys
d. left ventricle
a. pulmonary artery + vena cava
b. hepatic artery + hepatic vein
c. renal artery + renal vein
d. aorta + pulmonary vein
where do the coronary arteries branch off + what is their role?
they branch off from the aorta
they supply oxygen + glucose to the heart muscle
describe the systemic circulatory system (blood vessels of the body)
aorta
large arteries
small arteries
arterioles
capillaries
venules
small veins
large veins
vena cava
capillaries are the only vessels that are _______
permeable
describe the pressure + speed changes as blood is carried through the systemic circulatory system
arteries carry blood very rapidly under high pressure
as blood flows into arterioles + then the capillary beds, resistance to the flow of the blood increases
this causes the blood pressure + rate of flow to fall
blood flows into the venules + veins and back to the heart under low pressure
where + how do arteries carry blood?
away from the heart
at high blood pressure
what does the aorta have a large amount of?
of elastic tissue
explain what happens when the left ventricle contracts and when relaxes in regards to the aorta
when left ventricle contracts the aorta stretches due to its elasticity
when left ventricle relaxes the artery wall recoils due to its elasticity + forces blood to the body tissues
what is the advantage of the elasticity of the arteries?
it helps to provide a smooth flow of blood + maintain a relatively high pressure when the ventricle relaxes
*side note— elastic tissue does not contract + relax, elastic tissue stretches + recoils to smooth out blood flow
outline the process of the movement of blood out of the arteries
elastic tissue in wall stretches
most blood forced out when ventricle contracts
remaining blood forced out when ventricle relaxed due to elastic recoil of aorta
give 4 features of arteries
they have a thicker wall + a smaller lumen (inner cavity) than veins + contain more elastic fibres + smooth muscle fibres
do not possess valves except for the aorta + pulmonary artery
transport blood at a higher pressure than veins
carry oxygenated blood except for the pulmonary artery
what is different about the aorta + larger arteries near the heart + why?
they contain a higher ratio of elastic fibres to smooth muscle fibres
to withstand the high blood pressure + to help smooth out blood flow
how are arterioles different to main arteries?
they do not have to withstand the very high pressure found in main arteries
describe the proportion of smooth muscle + elastic fibres in arterioles
they possess a higher proportion of smooth muscle than elastic fibres
how do arterioles control the flow of blood to different tissues/organs?
by contraction or relaxation of the smooth muscle in their wall
describe how contraction + relaxation of the smooth muscle in arterioles controls the flow of blood? + why do they do this?
contraction of the smooth muscle causes narrowing (vasoconstriction) of the arteriole, reducing blood flow to the capillaries → to minimise heat loss (eg when cold)
relaxation of the smooth muscle causes widening (vasodilation) of the arteriole, increasing blood flow to the capillaries → to maximise heat loss (eg when hot)
in what conditions to veins carry blood to the heart?
under low pressure
give 3 ways veins differ from arteries
the walls of veins are thinner than arteries
the walls contain less elastic fibres + smooth muscle
the lumen is larger than in arteries
because veins have a larger lumen than arteries, this means what?
that even at a low pressure, blood flows back to the heart at the same rate that it leaves along the arteries
how is venous return achieved?
by the contraction of the skeletal muscles that surround veins
when they contract they compress the veins + push
why does the skeletal muscles need to contract?
the pressure in veins is too low for blood to return to the heart (especially against gravity) so contraction of skeletal muscles squashes veins + pushes blood along with them
what do the semi-lunar valves in veins do?
they are present to prevent back flow → the low pressure in veins means that blood could flow backwards
how are capillaries adapted so a short diffusion pathway is present for the exchange of substances with the tissues? (give 3 ways)
the walls of capillaries are one endothelial cell thick
no cells are very far from a capillary
capillaries have a very small diameter + red blood cells are squeezed flat against the capillary giving short diffusion pathways
how else are capillaries adapted for efficient exchange of substances? (as well as providing a short diffusion pathway)
gaps/pores between the endothelial cells increase the permeability of the capillary
there are very large numbers of capillaries + they’re highly branched, giving a large surface area of exchange with the tissues
the total cross-sectional area of capillaries is very high, producing a large frictional resistance, reducing the rate of blood flow + allowing more time for the exchange of substances
what does blood consist of?
liquid blood plasma with suspended blood cells + dissolved substances
what is the role of the blood capillaries?
to supply the cells with oxygen, glucose, amino acids etc
and remove waste products of metabolism eg carbon dioxide + urea
the exchange of substances through the capillaries happens via what?
via the tissue fluid which surrounds the body cells
arterioles divide to produce…
a large number of capillaries which supply all body tissues
explain the process that takes place to form tissue fluid (refer to hydrostatic + osmotic pressure)
at the arteriole end of a capillary the hydrostatic (blood) pressure is still high due to the contraction of the left ventricle
the high blood pressure (which forces water out) is greater than the osmotic pressure of the blood (which draws water in) → therefore filtration of blood plasma occurs
water + small molecules eg glucose, amino acids + ions pass through the permeable capillary wall (endothelial layer)
the blood cells + plasma proteins remain in the capillary
the filtered plasma forms tissue fluid which surrounds the body cells
what happens once tissue fluid is formed around the body cells?
oxygen, glucose, minerals etc (nutrients) diffuse into the body cells + carbon dioxide, urea + other metabolic waste diffuse out
explain the process that takes place to reabsorb some of the tissue fluid
volume of blood decreases due to the loss of fluid
this loss of fluid + high frictional resistance cause a reduction in the blood pressure as blood flows through the blood capillaries
the large plasma proteins which remain in the blood reduce the water potential of the blood plasma
this means that the osmotic pressure is greater than the blood pressure (as there is a reduced hydrostatic pressure at the venule end of the capillaries)
therefore some of the water from tissue fluid is reabsorbed by osmosis into the blood down a water potential gradient
this process is too slow to reabsorb all the filtered plasma, so what happens alongside it?
some of the tissue fluid enters lymph capillaries
lymph capillaries join to form…. + eventually return…
lymph vessels
return the tissue fluid to the blood
give 3 differences between blood plasma, tissue fluid + lymph
blood plasma contains large plasma proteins whilst tissue fluid does not
there are more white blood cells in lymph than in tissue fluid
more CO₂ in tissue fluid than blood plasma
how is oxygen carried?
combined with haemoglobin
in red blood cells
what is haemoglobin? include its role
an iron containing pigment, which loosely + reversibly combines with oxygen to form oxyhaemoglobin
haemoglobin is a _____ with a ______ structure
protein
quaternary
what type of pigment is haemoglobin?
a respiratory pigment
describe the structure of a haemoglobin molecule?
each molecule consists of four haem units + four polypeptide chains
it has a _______ structure because…
quaternary
it has more than one polypeptide chain
explain how many oxygen molecules one haemoglobin molecule can transport
each haem unit can combine with one oxygen molecule so one haemoglobin molecule can transport four oxygen molecules
what is the partial pressure of oxygen?
the concentration of oxygen
define affinity
the attraction of haemoglobin (Hb) for oxygen
how does affinity change?
depending on the conditions eg on the partial pressure of oxygen, of carbon dioxide, on pH + temp
what is oxygen dissociation?
when oxygen detaches from haemoglobin
explain the process of the association of oxygen in the lungs
blood entering the lung capillaries is deoxygenated
alveoli contain a high conc of O₂ (there is a high ppO₂) due to ventilation
this provides a concentration gradient for the diffusion of oxygen through the epithelium of alveolus + endothelium of capillary
the oxygen enters red blood cells + associates (combines) with haemoglobin to form oxyhaemoglobin
this is because haemoglobin has a high affinity for oxygen due to the high pp
what happens to the oxygen after being combined with haemoglobin?
its carried away by the blood, maintaining a concentration gradient
explain the process of the disassociation of oxygen in the body tissues
in the body tissues respiration uses oxygen + therefore there is a low ppO₂
oxyhaemoglobin releases oxygen (O₂ dissociates from haemoglobin) which diffuses into the respiring cells
this happens due to haemoglobin’s low affinity for oxygen (due to the low ppO₂)
what is haemoglobin ideally suited for?
for the transport of oxygen from the lungs to the body tissues
why is haemoglobin ideally suited for the transport of oxygen from the lungs to the body tissues?
it has a very high affinity for oxygen + quickly loads (associates with) oxygen (becomes 96% saturated) in the lungs where the partial pressure of oxygen is high
at low partial pressure of oxygen in the tissues, haemoglobin dissociates (unloads) some of its O₂ to the respiring cells
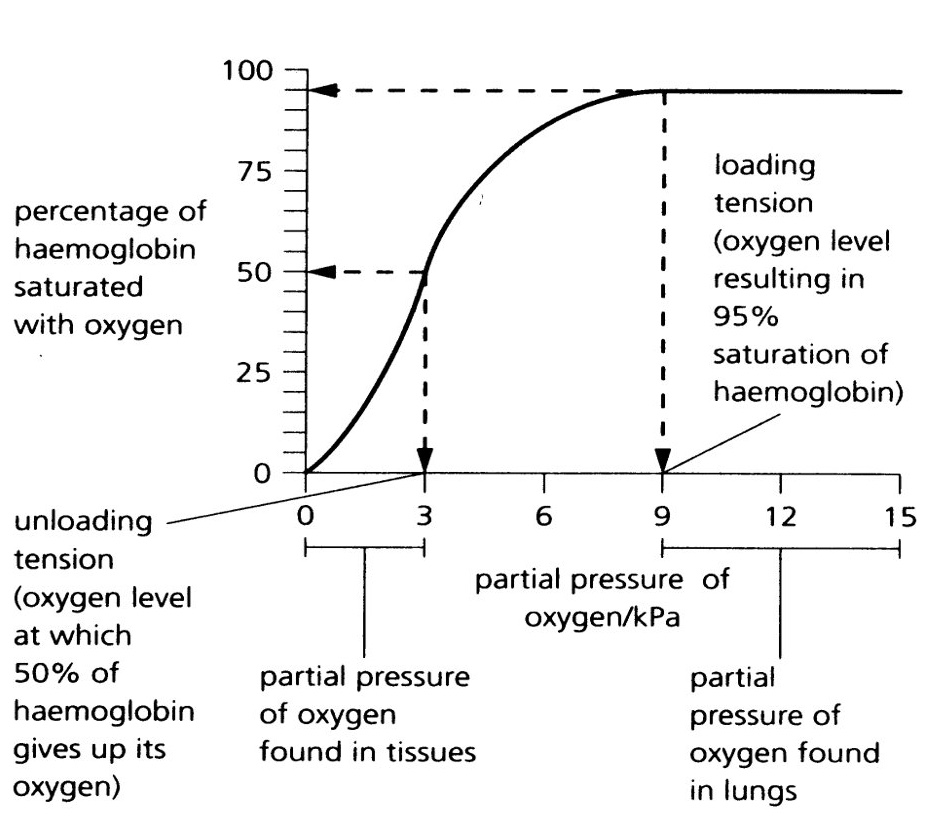
what does the oxyhaemoglobin dissociation curve show a relationship between?
between the concentration of oxygen carried by haemoglobin + the partial pressure of oxygen in the surrounding environment (eg in lungs or body tissues)
what shape does the oxyhaemoglobin dissociation curve have?
it has a characteristic S (sigmoid) shape
explain why the oxyhaemoglobin dissociation curve has a S (sigmoid) shape?
a molecule of oxygen binds to one of th four haem units
this cause a slight change in the tertiary structures of the other haem units / quaternary structure of the haemoglobin
this increases their affinity for oxygen as this uncovers the binding sites of the next haem units → allowing the second oxygen molecule to bind more easily + the third even more easily
briefly describe what happens when oxygen dissociates
by the same process as association, the ability of haemoglobin to lose oxygen increases (its affinity for oxygen decreases) as fewer oxygen molecules are bound
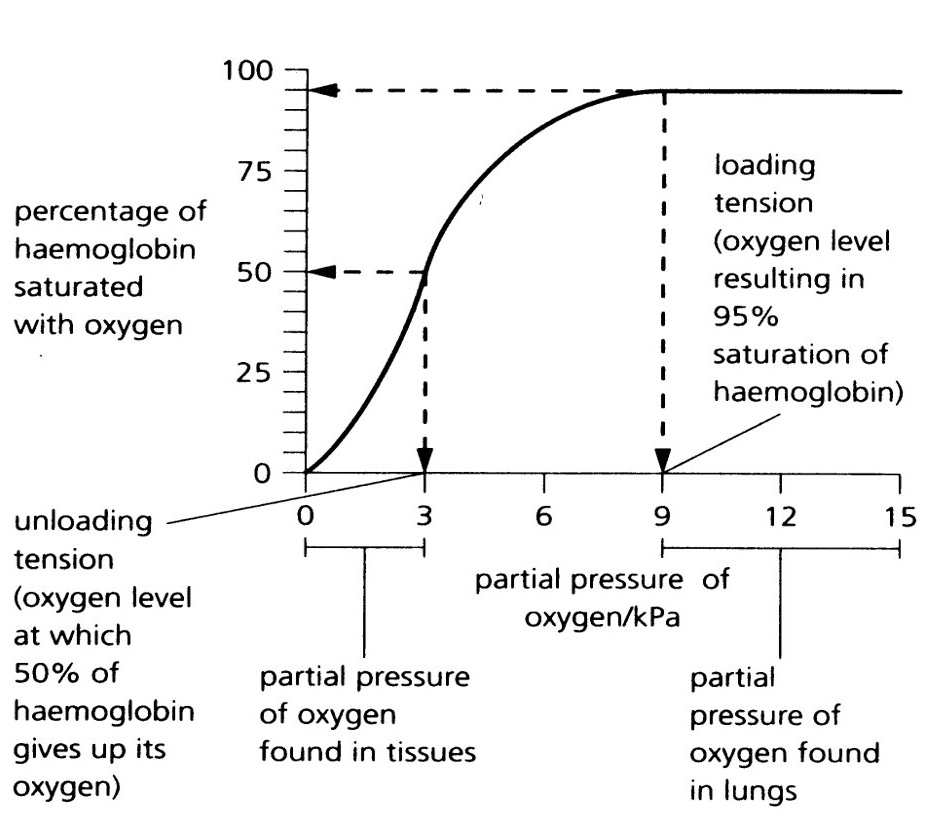
what is the Bohr effect?
the effect of CO₂ on haemoglobin
where does the Bohr effect occur?
only occurs in tissues, usually during exercise
it does not occur in the lungs
what happens during exercise regarding the cells?
muscle cells respire more rapidly, producing larger concentrations of CO₂
explain what the Bohr effect is due to
due to the decrease in pH produced as carbon dioxide dissolves in the blood plasma to form an acid (carbonic acid)
describe the Bohr effect (explain the graph)
the change in pH in the tissues changes the quaternary structure of haemoglobin + lowers the affinity of haemoglobin for oxygen
therefore the O₂ dissociation curve moves to the right
haemoglobin releases more oxygen to respiring tissues
why is the Bohr effect give a physiological advantage to the body?
it ensures that haemoglobin releases more oxygen to the most active cells for the increase of respiration taking place
describe the effect temperature has
an increase in temp also causes the O₂ dissociation curve to shift to the right
so more O₂ is released to cells
more heat is released when respiration increases
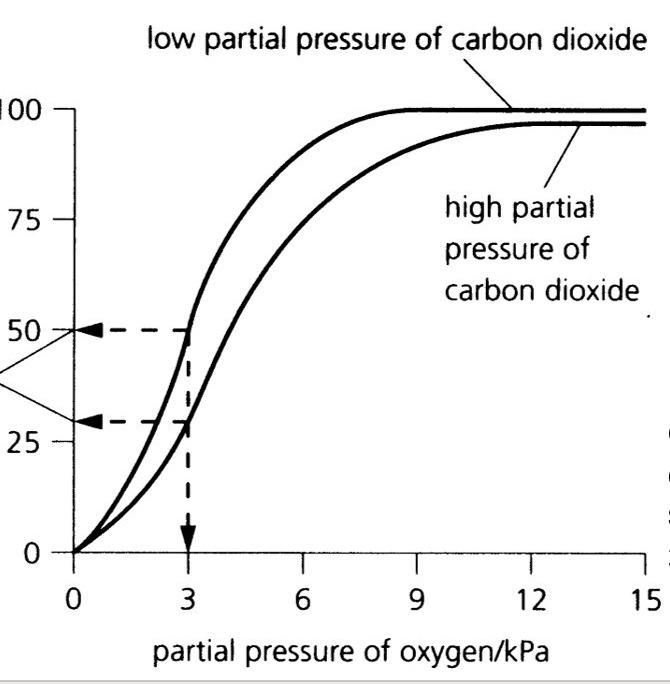
many animals are adapted to their environment by…
possessing different types of haemoglobin with different oxygen transport properties
the type of haemoglobin organisms possess is related to what?
to the environment or way of life of the organism
which organisms possess haemoglobin with a higher affinity for oxygen?
organisms living in environments where the oxygen concentration is low
eg
in the mud
at the bottom of polluted rivers
at high altitudes
describe the oxyhaemoglobin dissociation curve for these organisms (ones that live in low O₂ conditions)
the curve for these organisms is further to the left when compared to organisms living in areas of higher oxygen concentration
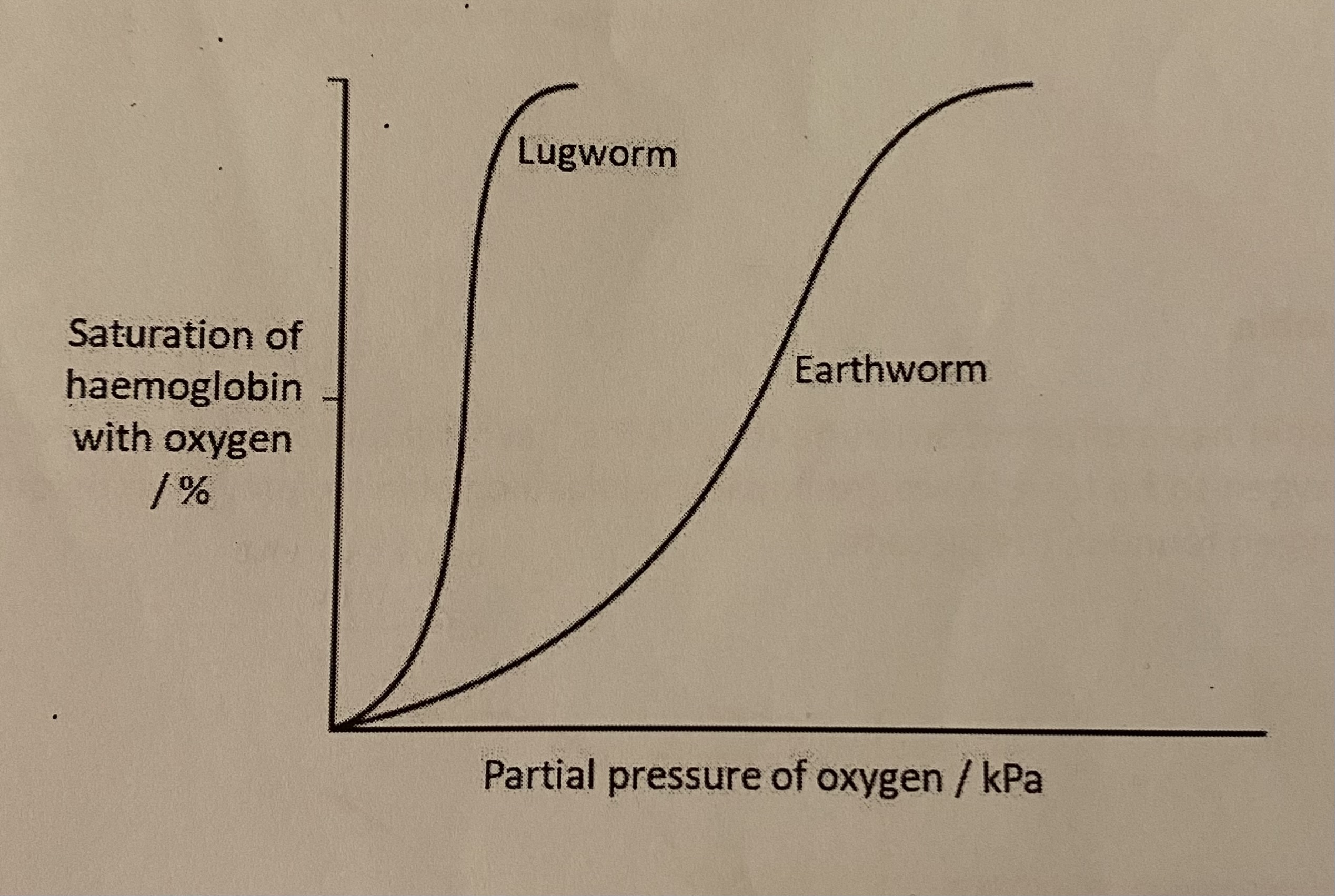
describe how the loading of oxygen in the lugworm than in the earthworm
the haemoglobin of lugworm has a higher affinity for oxygen + will load more oxygen than earthworm at the low partial pressures of oxygen which are present in its surrounding environment