Cardio PES
1/70
Earn XP
Description and Tags
incomplete
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
71 Terms
Diaphoresis
profuse sweating
(unrelated to temperature or activity)
may indicate MI or shock
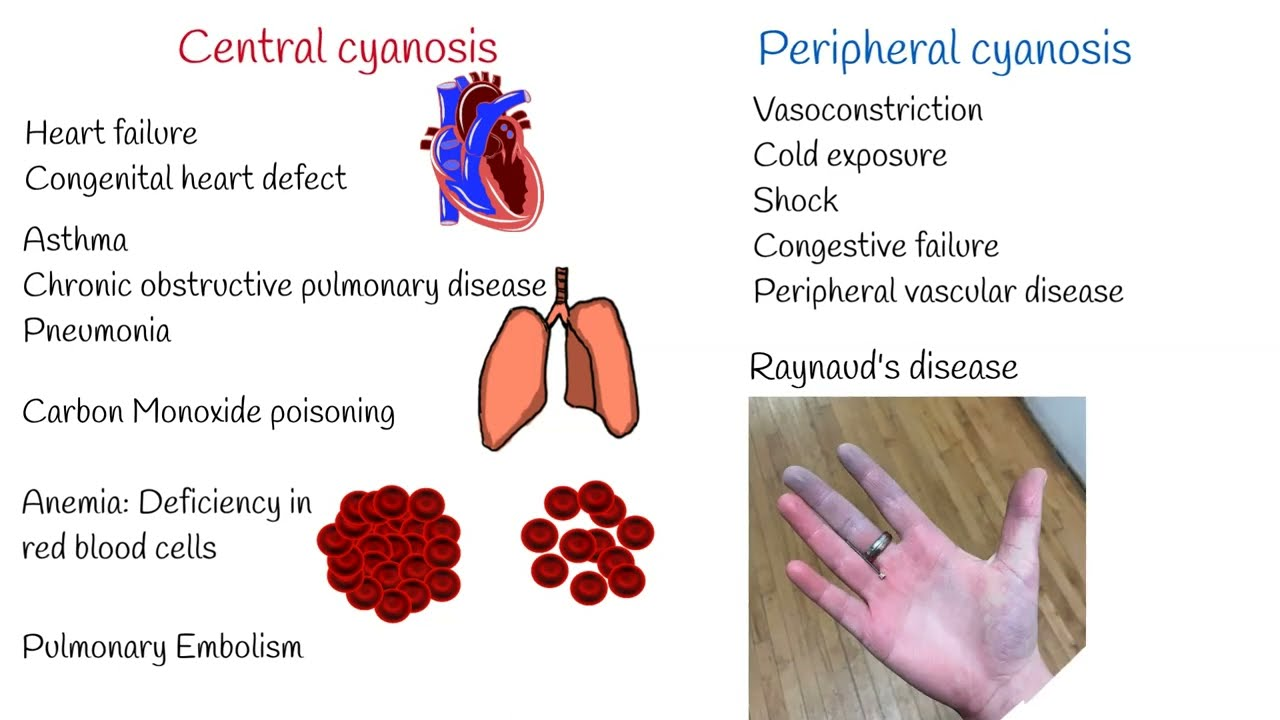
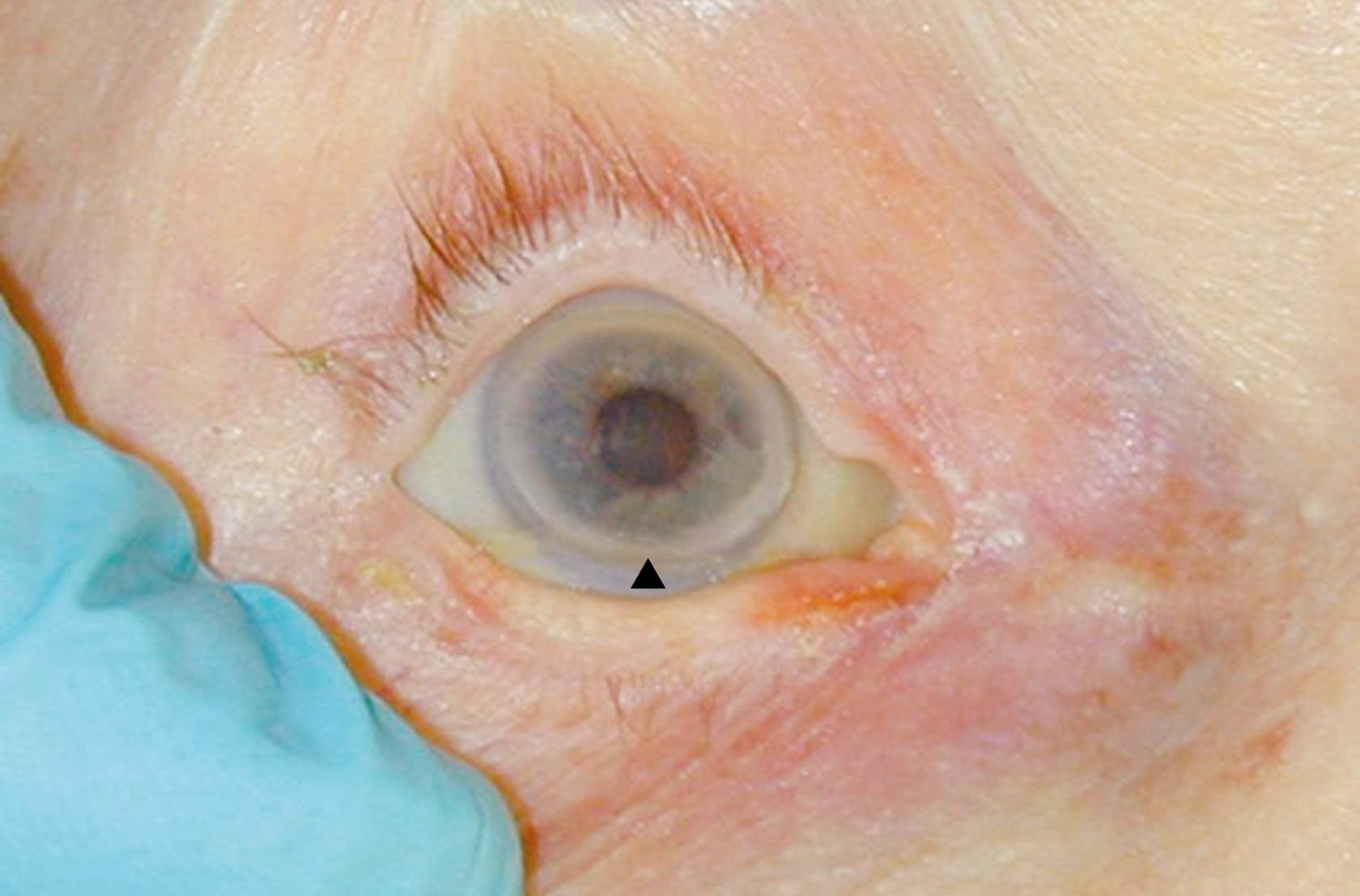
Cyanosis signs
either peripheral or central:
Central cyanosis:
bluish lips, tongue (especially the underside), and oral mucous membranes (use a light)
causes:
cyanotic congenital heart disease with right-to-left shunt
respiratory disease e.g. COPD and pulmonary embolism
high altitude + resultant decreased inspired oxygen concentration
polycythaemia (increased hematocrit and/or hemoglobin concentration)
haemoglobin abnormalities
Peripheral cyanosis
bluish discoloration of the hands, nail beds and feet
causes:
All causes of central cyanosis cause peripheral cyanosis
exposure to the cold
reduced cardiac output
arterial or venous obstruction
can reflect poor oxygenation, reduced perfusion, or anaemia
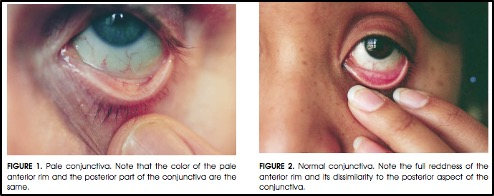
Pallor
pale conjunctiva, nail beds, and palmar creases
can reflect poor oxygenation, reduced perfusion, or anaemia
male risk factor
Earlier Coronary Artery Disease (CAD) risk
obesity risk factor
Coronary Artery Disease (CAD) risk
ethnic background risk factor
South Asian, Indigenous Australians, Pacific Islanders have higher Coronary Artery Disease (CAD) risk
GTN spray
Common nitrate used in angina
Suggests known ischaemic heart disease

down syndrome cardiac relation
50% of patients will have a cardiac defect
most often an atrioventricular septal defect
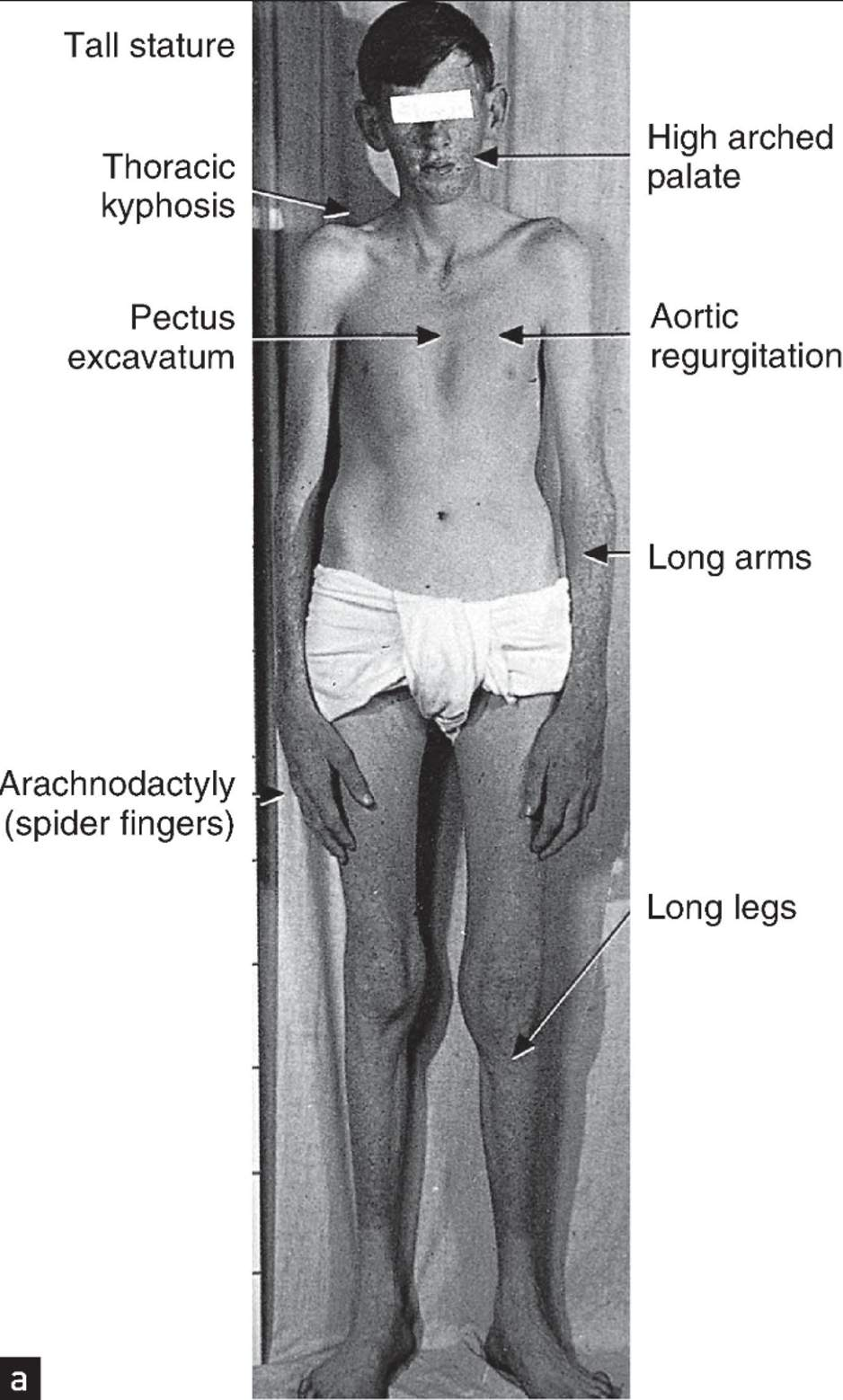
marfan syndrome cardiac relation
Check for:
High arched palate
tall stature
long limbs
long fingers
Associated with:
aortic dilatation with risk of dissection
mitral valve prolapse
aortic regurgitation
Turner syndrome cardiac relation
50% of patients will have a major cardiac defect e.g.
coarctation of the aorta
bicuspid aortic valve
Turner Syndrome signs
short stature
webbing of the neck
stocky build
shield-like chest
lack of breast development and cubitus valgus in female patients
hydration status
fluid overload:
can be a sign of cardiac failure
e.g. bilateral ankle swelling due to peripheral oedema
could also be renal failure or excessive IV drug use
dehydration:
sunken eyeballs
a ‘moribund’ appearance (i.e., look very unwell)
altered consciousness
heart rate
normal resting: 60-100 beats per minute
bradycardia: <60
tachycardia: >100
radio-radial delay
inequality in timing or volume of the pulse
can occur with:
coarctation of the aorta
aortic dissection
subclavian artery stenosis
radio-femoral delay
suggestive of coarctation of the aorta
heart rhythm categories
regular
regularly irregular
irregularly irregular
respiratory rate
12-20 breaths per minute
blood pressure ranges
Diastolic: 60-90mmHg
Systolic: 90-140mmHg
oxygen saturation
normal: 95-100% (room air)
Hypoxaemia: <92%
temperature range
36.1 - 37.9oC
fever could signify
infection (e.g. endocarditis, pericarditis, pneumonia)
peripheral perfusion of hands
well perfused: warm and pink, normal CRT
shut down: cold and pale, reduced CRT
capillary refill time (CRT)
apply pressure to the nail bed, pressing over the top of the fingernail until it turns white
Release the pressure and count the number of seconds it takes for the colour to return to the nail bed
Colour should return in less than 2 seconds
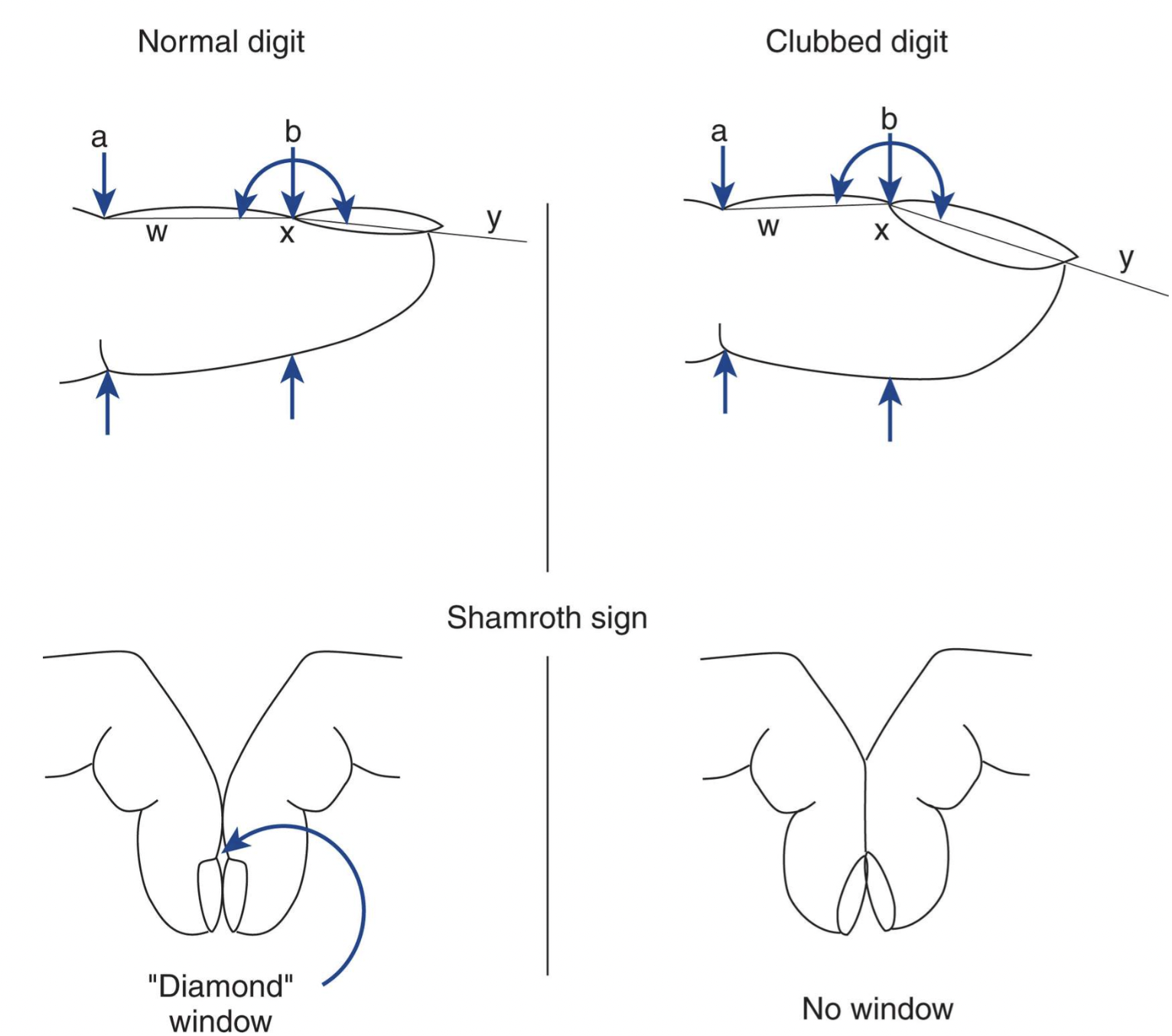
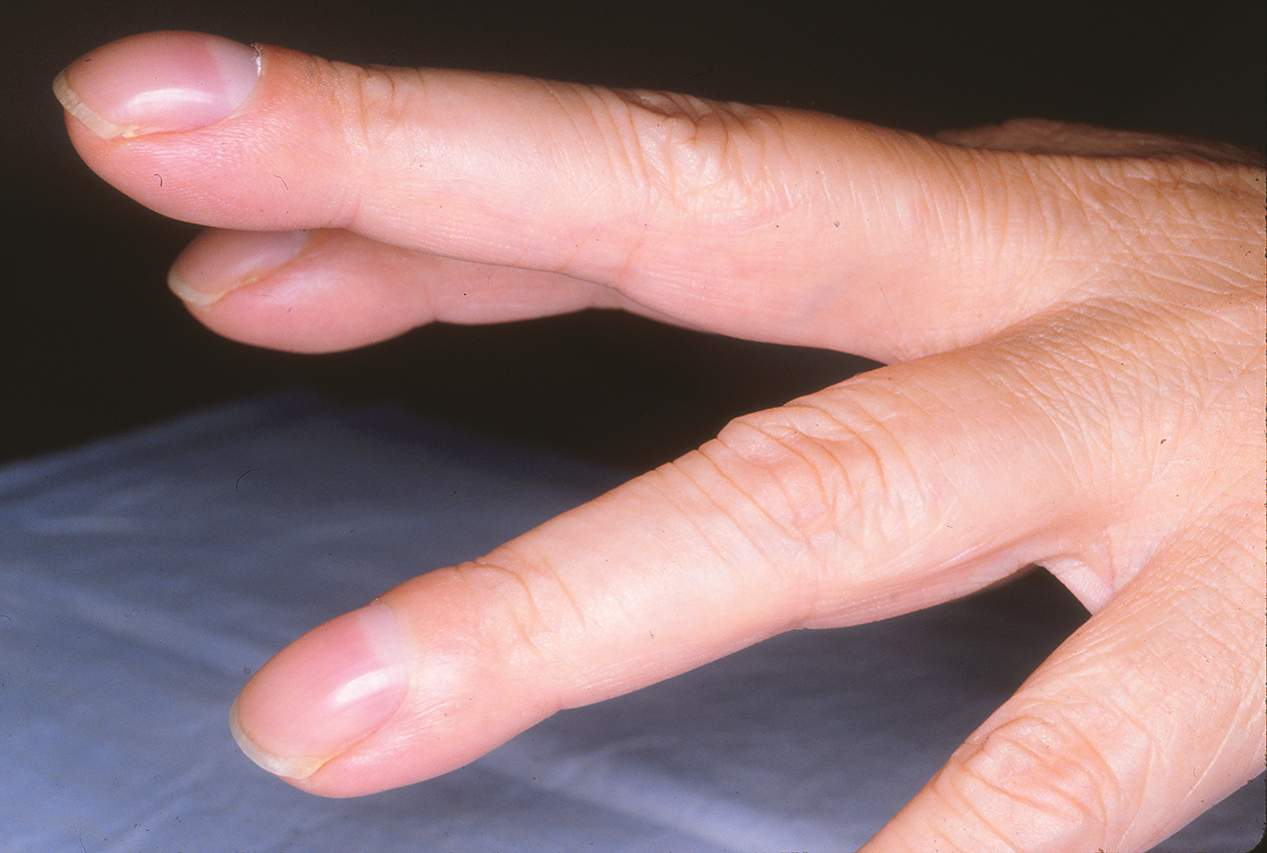
clubbing
loss of normal hyponychial angle:
the angle between the nail bed and the cuticle increases and rounds out
nails curve downwards
Schamroth’s sign:
Ask the patient to place the dorsal surfaces of the terminal phalanges of index back-to-back.
Normal: A small diamond-shaped window of light is visible between the nails.
Positive Schamroth’s Sign: No window — the space is obliterated due to the nails being more convex and the tissues swollen, indicating clubbing.
linked with cyanotic congenital heart disease
splinter hemorrhage
most commonly trauma related
can be a peripheral sign of infective endocarditis due to:
Microemboli (tiny clots or infected material from heart valves) traveling through circulation
or
Vasculitis (immune complex deposition) causing damage to capillaries

tobacco staining
sign of smoker
risk factor for ischaemic heart disease and peripheral vascular disease

xanthomata
lipid deposits under the skin suggests hyperlipidaemia → risk factor for ischaemic heart disease and peripheral vascular disease
typically seen over extensor tendons such as on the back of the hand (wrist) or the elbows

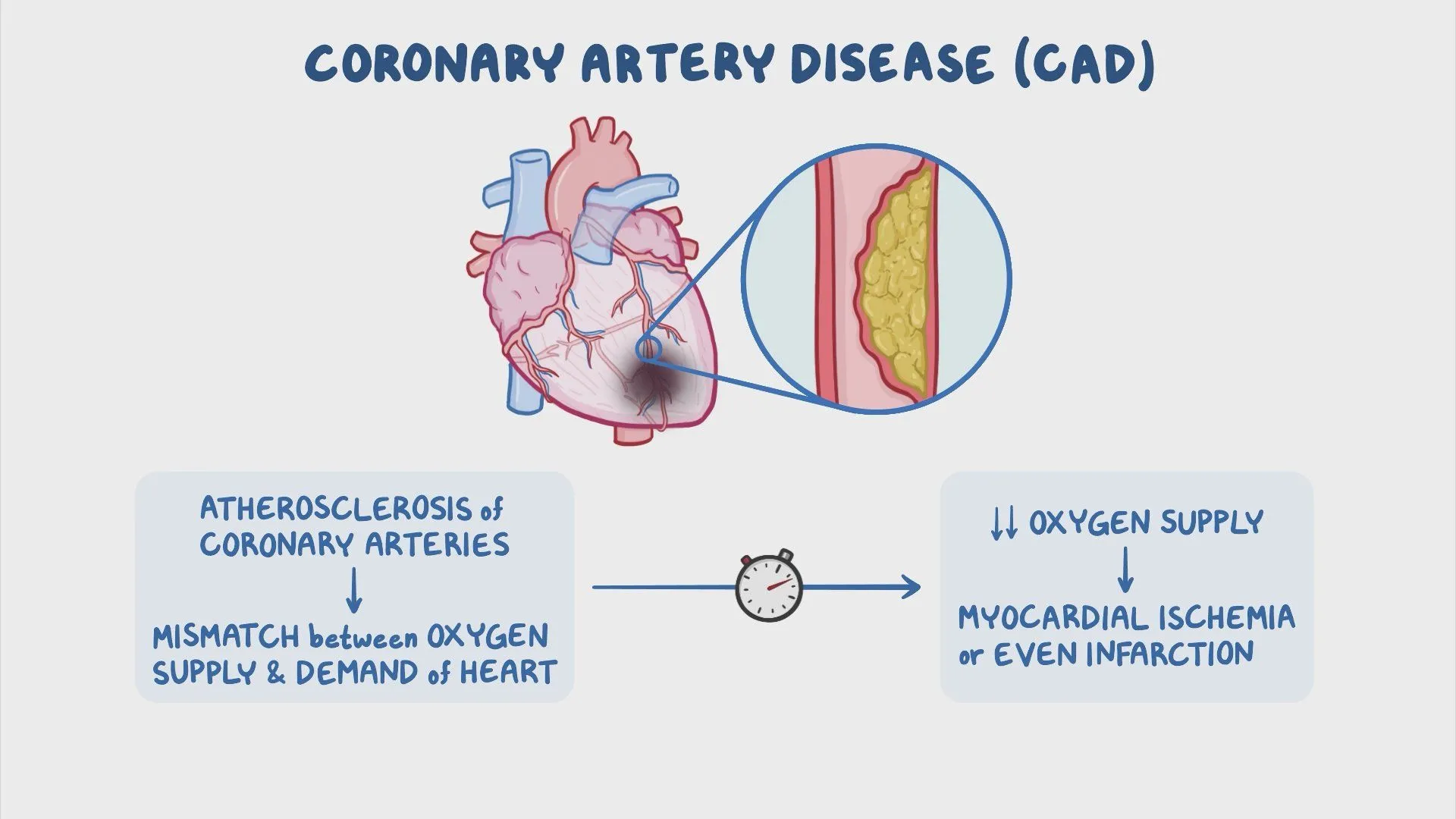
ischaemic heart disease
Also called Coronary Artery Disease (CAD)
reduced blood flow to the heart muscle (myocardium) occurs due to narrowing or blockage of coronary arteries
usually from atherosclerosis
Pathophysiology:
Atherosclerosis → Plaque buildup in coronary arteries
↓ Blood supply to myocardium → Myocardial ischaemia
Can be stable or acute
Clinical Presentations:
Stable Angina: Chest pain on exertion, relieved by rest
Unstable Angina: Chest pain at rest or minimal exertion
Myocardial Infarction (MI): Prolonged ischaemia → Heart muscle damage
Silent ischaemia (especially in diabetics)
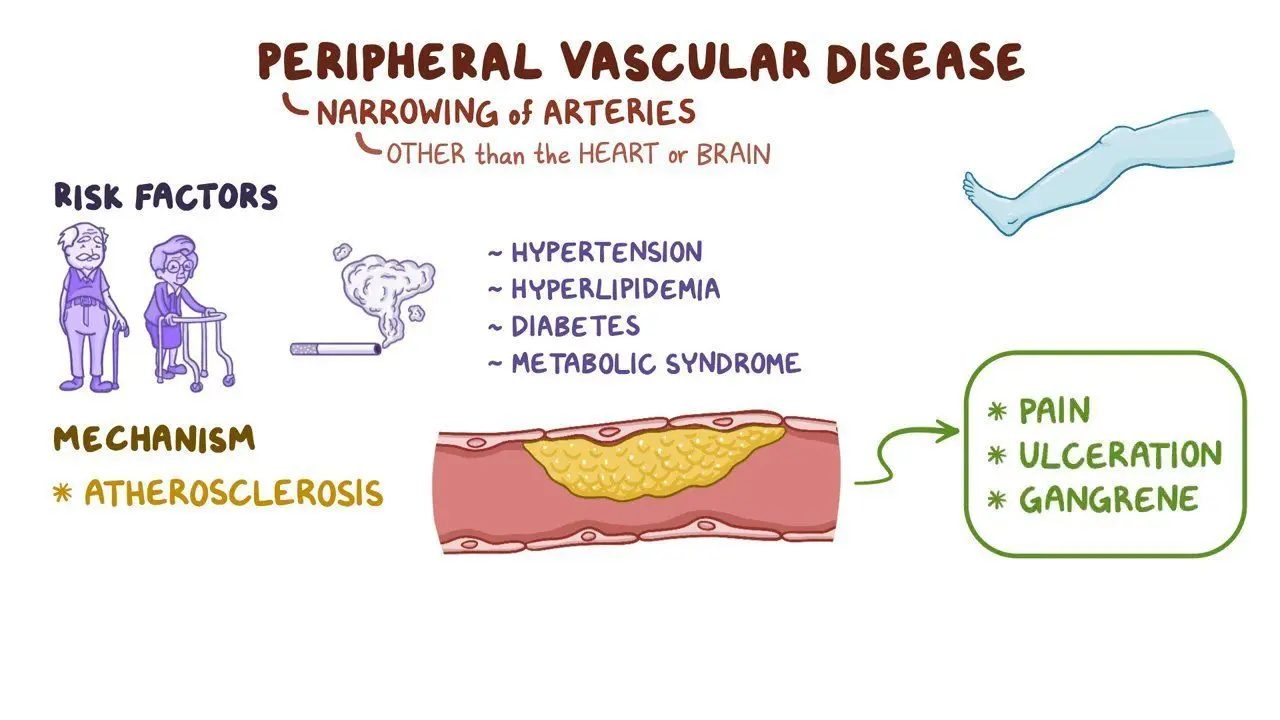
peripheral vascular disease
Also called Peripheral Arterial Disease (PAD)
arteries supplying the limbs, especially the legs, become narrowed or blocked
due to atherosclerosis
results in poor circulation
Pathophysiology:
Atherosclerosis in peripheral arteries
↓ Blood flow to limbs, especially during exercise
→ Ischaemic muscle pain
Clinical Presentations:
Intermittent claudication:
Cramping leg pain during walking
relieved by rest
Critical limb ischaemia:
Pain at rest
non-healing ulcers
gangrene
Diminished pulses:
cool or pale skin
poor wound healing
angina
chest pain or discomfort caused by reduced blood flow to the heart muscle
symptom of CAD
Stable angina:
most common type
occurs predictably: usually during exertion or emotional stress
relieved by rest or medication.
Unstable angina:
more serious type
follows an irregular pattern
not relieved by rest or medication
can be a sign of a more severe heart problem and may precede a heart attack.
Variant angina (Prinzmetal's angina):
occurs at rest due to a spasm in the coronary arteries (myocardial vessel vasospasm), which can reduce blood flow to the heart
Symptoms of Angina:
Chest pain or discomfort that may feel like squeezing, tightness, or pressure.
Pain or discomfort that may radiate to the neck, jaw, arms, shoulders, or back.
Feeling of indigestion, heartburn, or nausea.
Shortness of breath, fatigue, or dizziness
Osler’s nodes
tender palpable nodules
rare, peripheral signs of infective endocarditis
noted on the finger pulps or thenar/hypothenar eminences
thought to be due to:
Septic Microemboli (tiny clots or infected material from heart valves) traveling through circulation
or
Vasculitis (immune complex deposition) causing damage to capillaries


Janeway lesions
non-tender, late peripheral sign of infective endocarditis
found on the palms or finger pulps and are thought to be septic emboli
rarely seen in western cultures due to advances in medical treatment

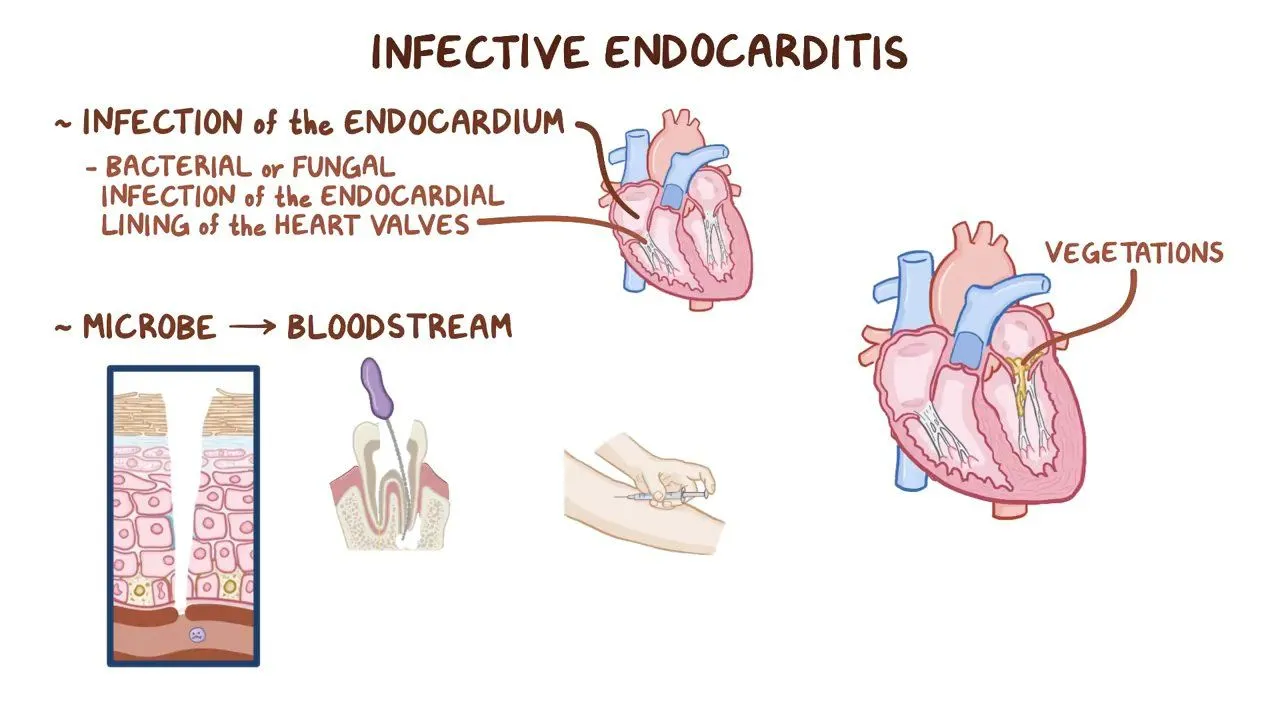
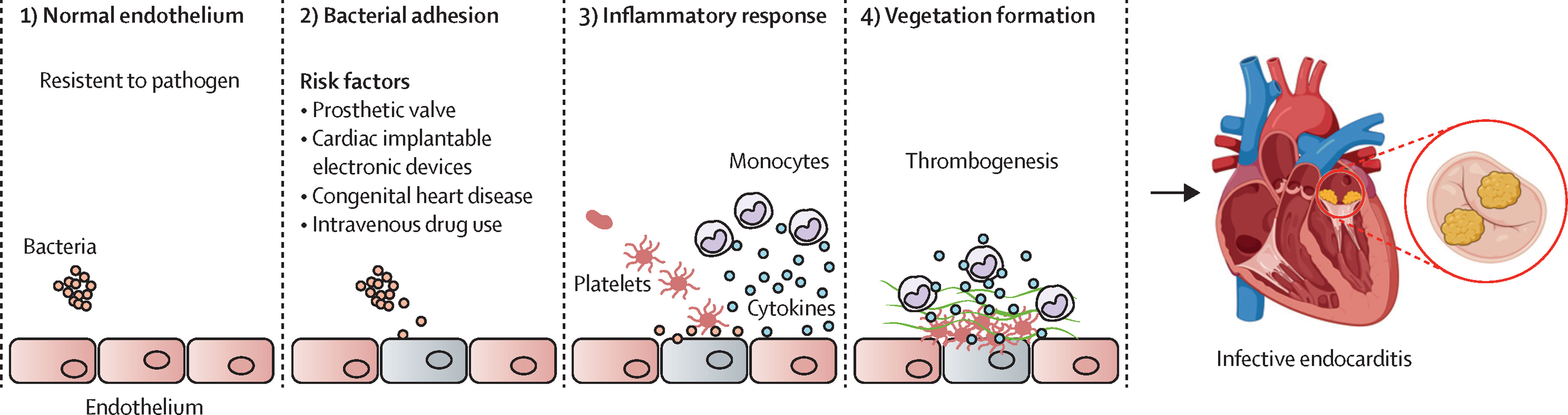
infective endocarditis pathogenesis
Endothelial Damage
Damaged endothelium exposes collagen and tissue factor, promoting platelet-fibrin thrombus formation
Bacteremia
Microorganisms (bacteria or fungi) enter the bloodstream via:
Dental procedures
Poor gingival health
IV drug use
Surgery
Infected devices (e.g., catheters, prosthetic valves)
Vegetation Formation
Bacteria adhere to the thrombus → form infected vegetations composed of fibrin, platelets, and microorganisms
These vegetations are protected from immune cells, allowing bacteria to multiply
Destructive and Embolic Effects
Vegetations can destroy valve tissue
→ regurgitation or heart failure
Septic Microemboli (tiny clots or infected material from heart valves) can break off
→ travel to skin, brain, kidneys, etc.
→ infarctions or abscesses
Immune complexes can deposit in tissues
→ vasculitis, glomerulonephritis
infective endocarditis clinical features
Splinter hemorrhages
Linear nailbed bleeding (septic microemboli or immune complexes (vasculitis))
Osler nodes
Tender, palpable nodules on finger pulps or thenar/hypothenar eminences (septic microemboli or immune complexes (vasculitis))
Janeway lesions
Non-tender lesions on palms or finger pulps (septic microemboli)

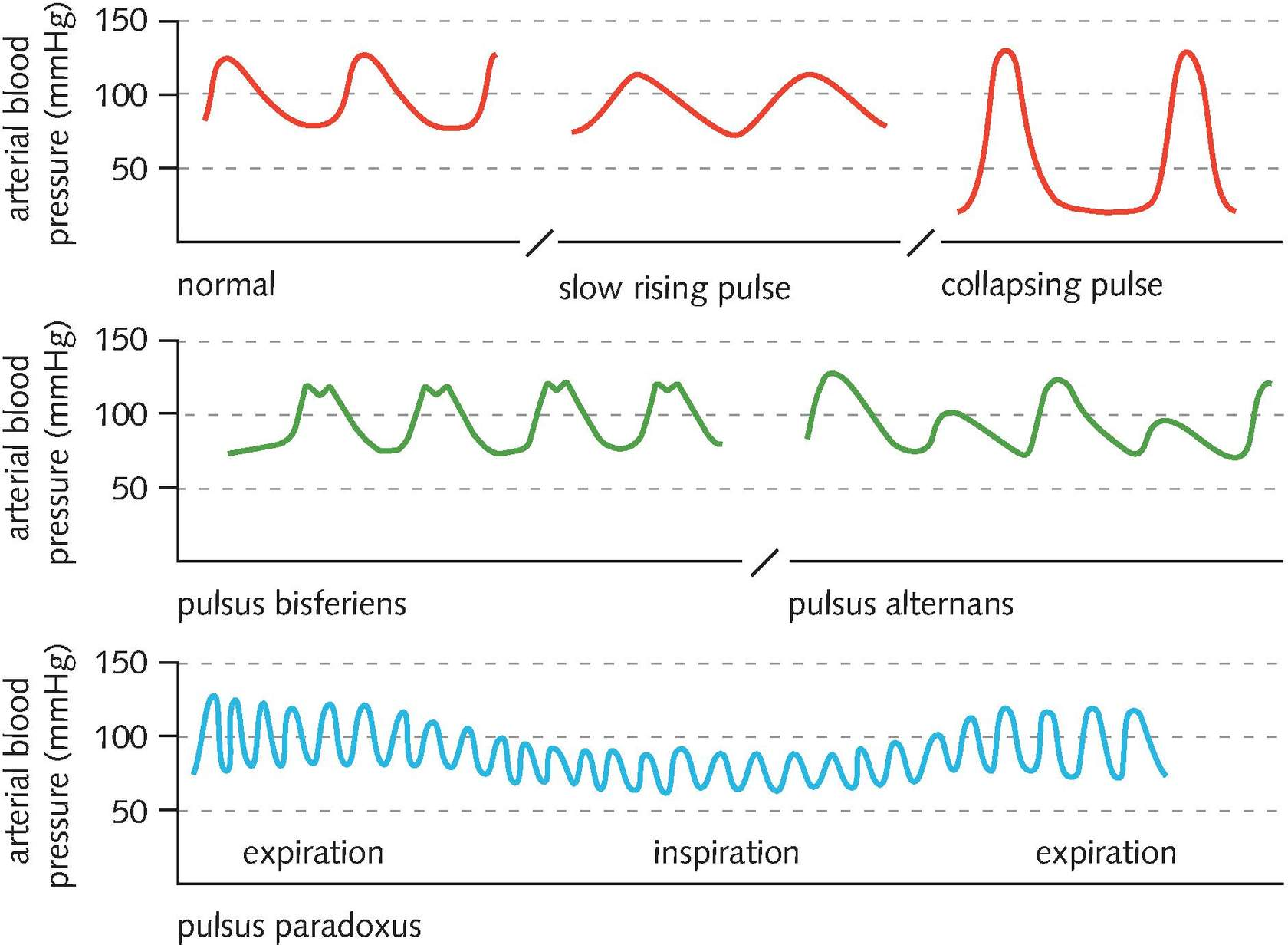
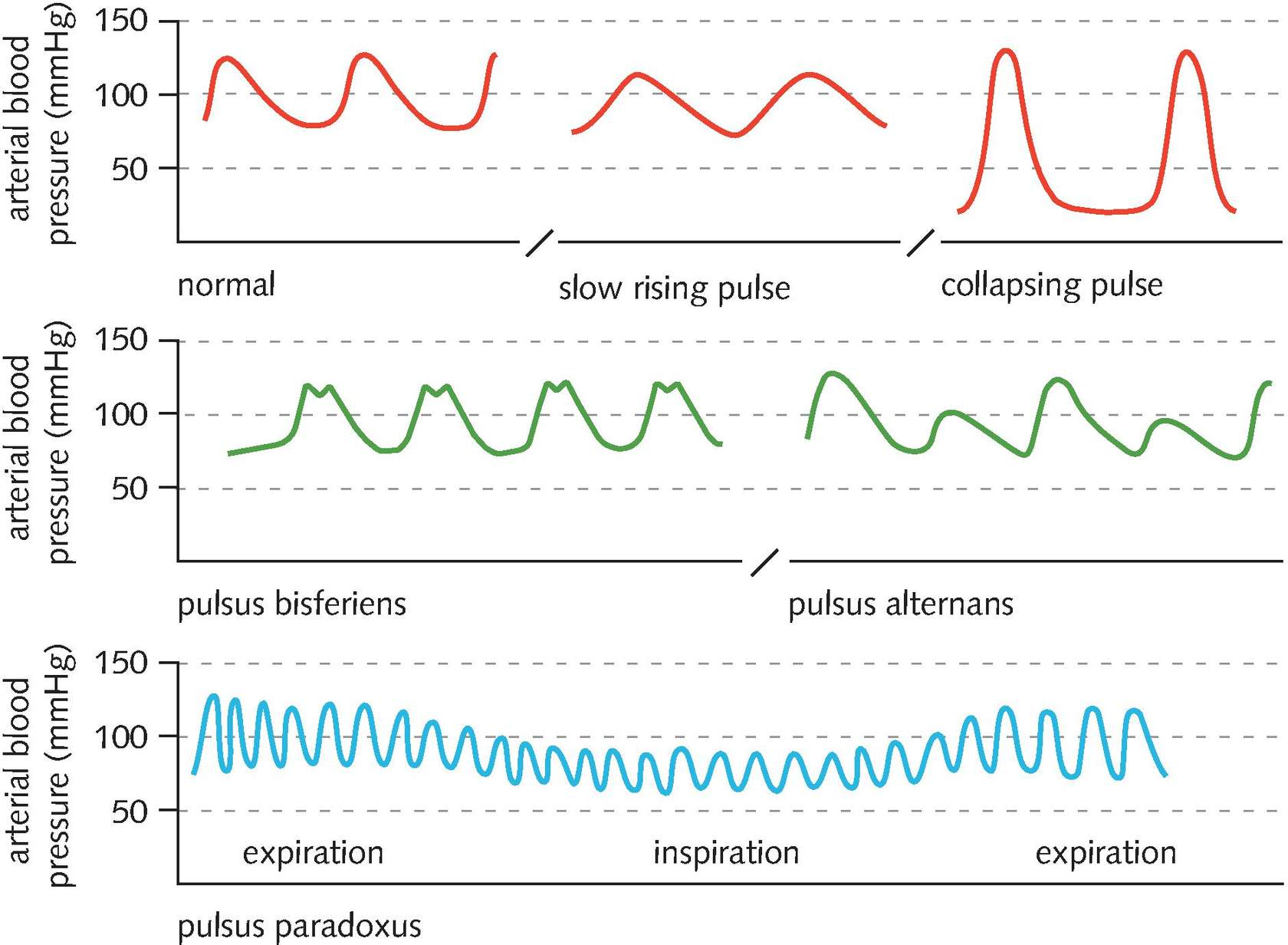
blood pressure
normally there is a small, non-palpable drop in systolic blood pressure on inspiration
If this drop is palpable, it is called pulsus paradoxus
>10mmHg drop in systolic pressure during inspiration may indicate pericardial tamponade or severe asthma
The pulse pressure is defined as the systolic pressure minus the diastolic pressure
A wide pulse pressure is a sign of aortic regurgitation (80-100mmHg)
A narrow pulse pressure is a sign of aortic stenosis (less than 25% of the systolic pressure)
An average pulse pressure is approximately 40mmHg
scleral jaundice
yellowing of the sclera (the white of the eye)
e.g. in cardiovascular disease can signify cardiac failure associated with hepatic congestion
signs of anemia
conjunctival pallor
tachycardia
systolic murmur
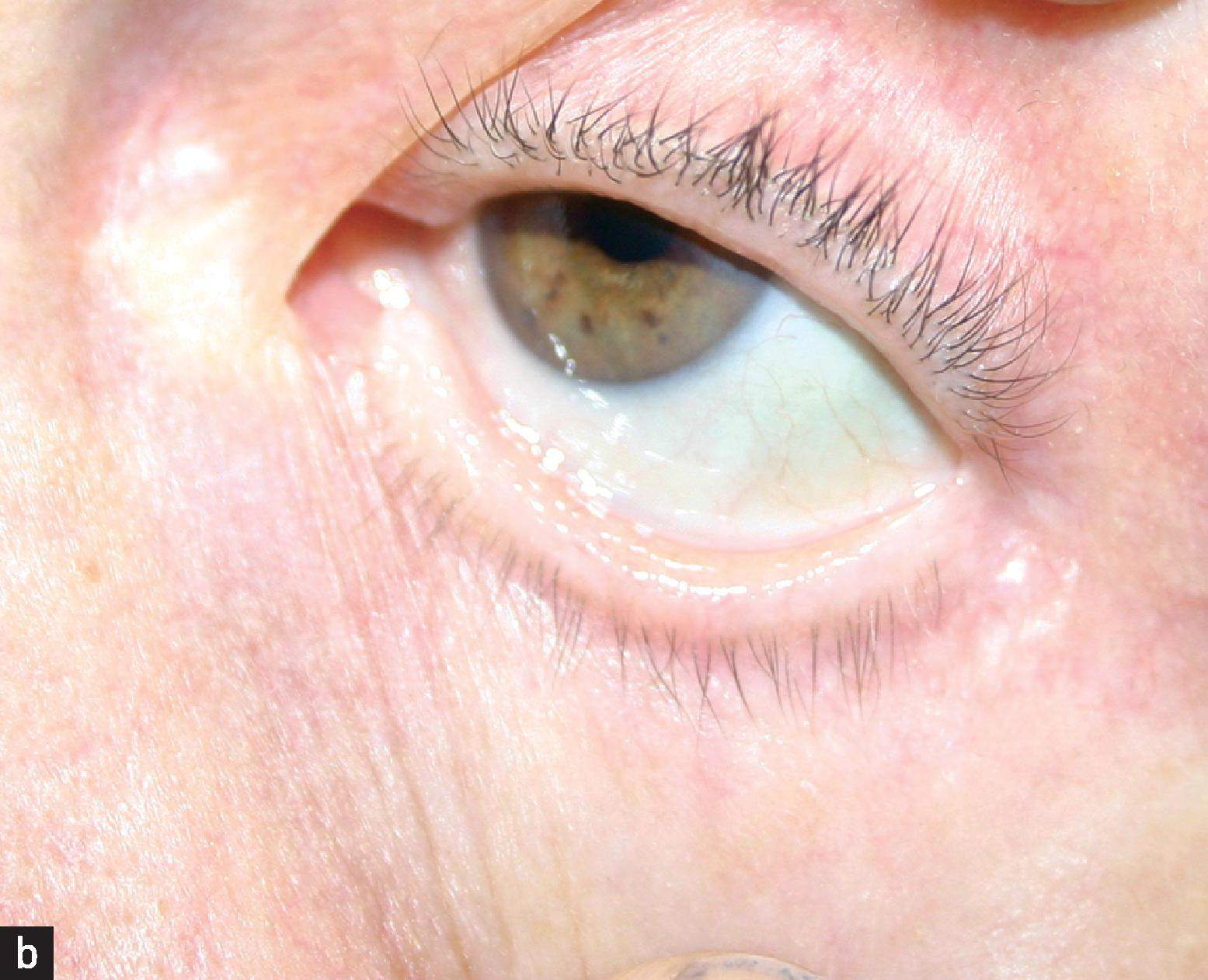
xanthelasma
seen near the upper inner eyelid
yellow-orange cholesterol deposits under the skin
sign of hyperlipidaemia in young patients (normal for old)

corneal arcus
grey/white ring around the iris
sign of hyperlipidaemia in young patients (normal for old)
Gingival health and dentition
check for signs of gum disease or infection
Poor gingival health = entry route for bacteria causing infection endocarditis
Angular stomatitis
inflammation at the edges of the mouth
may be present in iron and/or vitamin B deficiencies

mucosal petechiae
small red-purple haemorrhages on the oral mucosa, often seen on the palate
sign of infective endocarditis

collapsing pulse
Rapid upstroke, higher volume, fast downstroke (i.e. rises and falls quickly)
Occurs with:
physiological states:
fever
exercise
pregnancy
hyperdynamic circulation:
anaemia
thyrotoxicosis
large arteriovenous fistula
commonly associated with aortic regurgitation
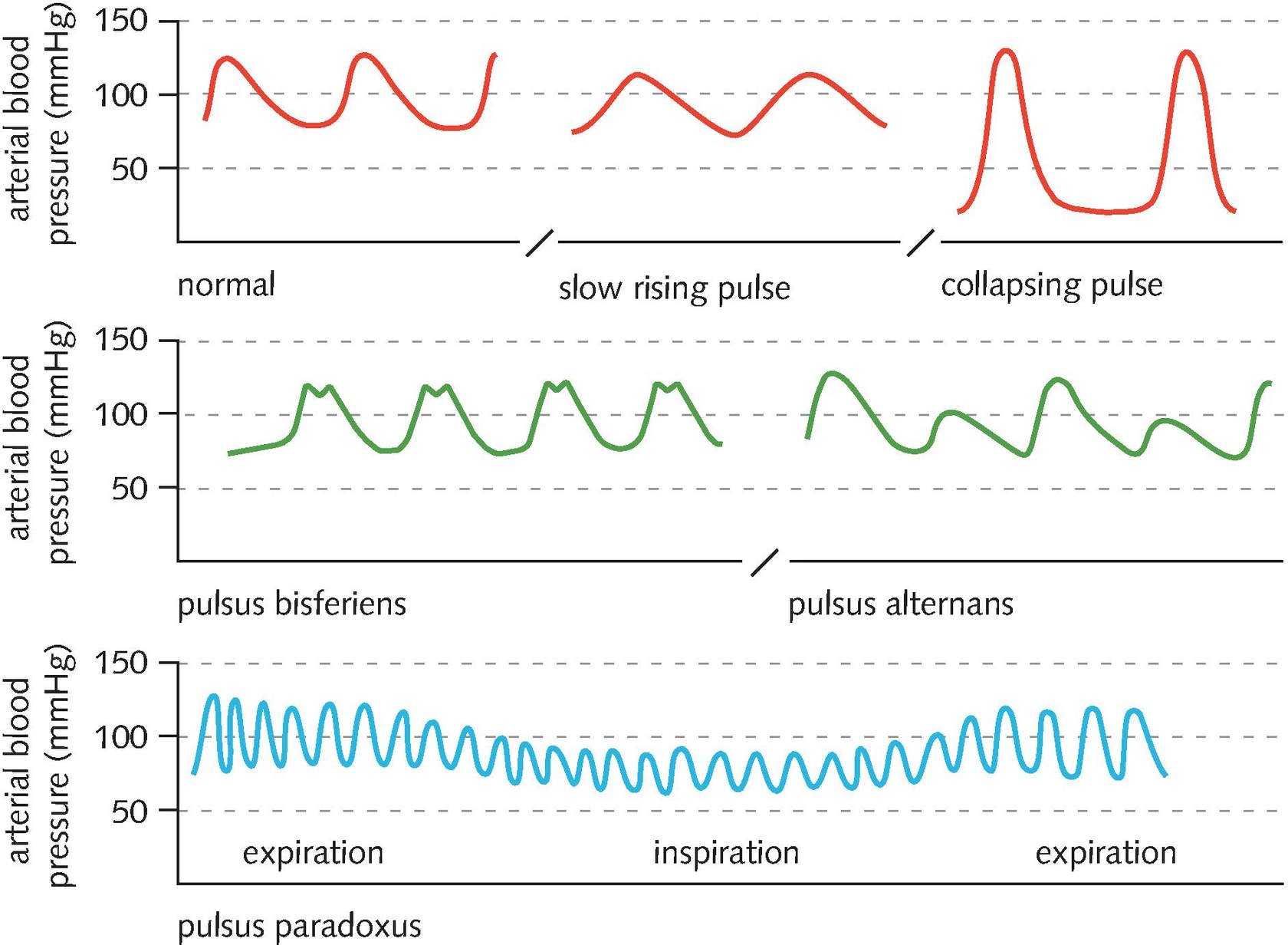
bifid pulse
can feel two separate peaks (a double impulse) during systole
Occurs with:
co-existing aortic stenosis and aortic regurgitation
hypertrophic obstructive cardiomyopathy (HOCM)
(pulsus bisferiens)
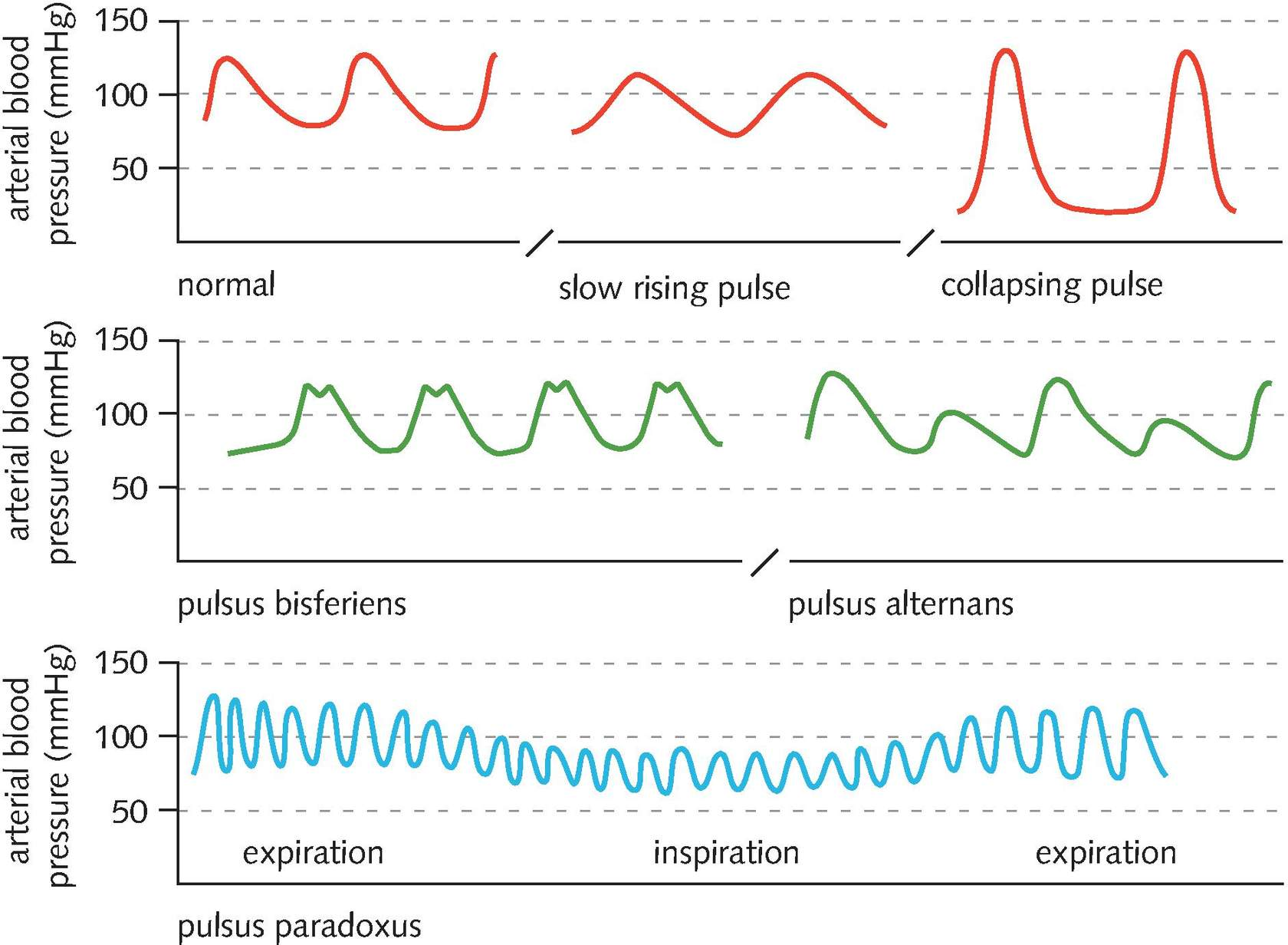
plateau pulse
Slow-rising or anacrotic (small volume, slow-rising)
Occurs in aortic stenosis
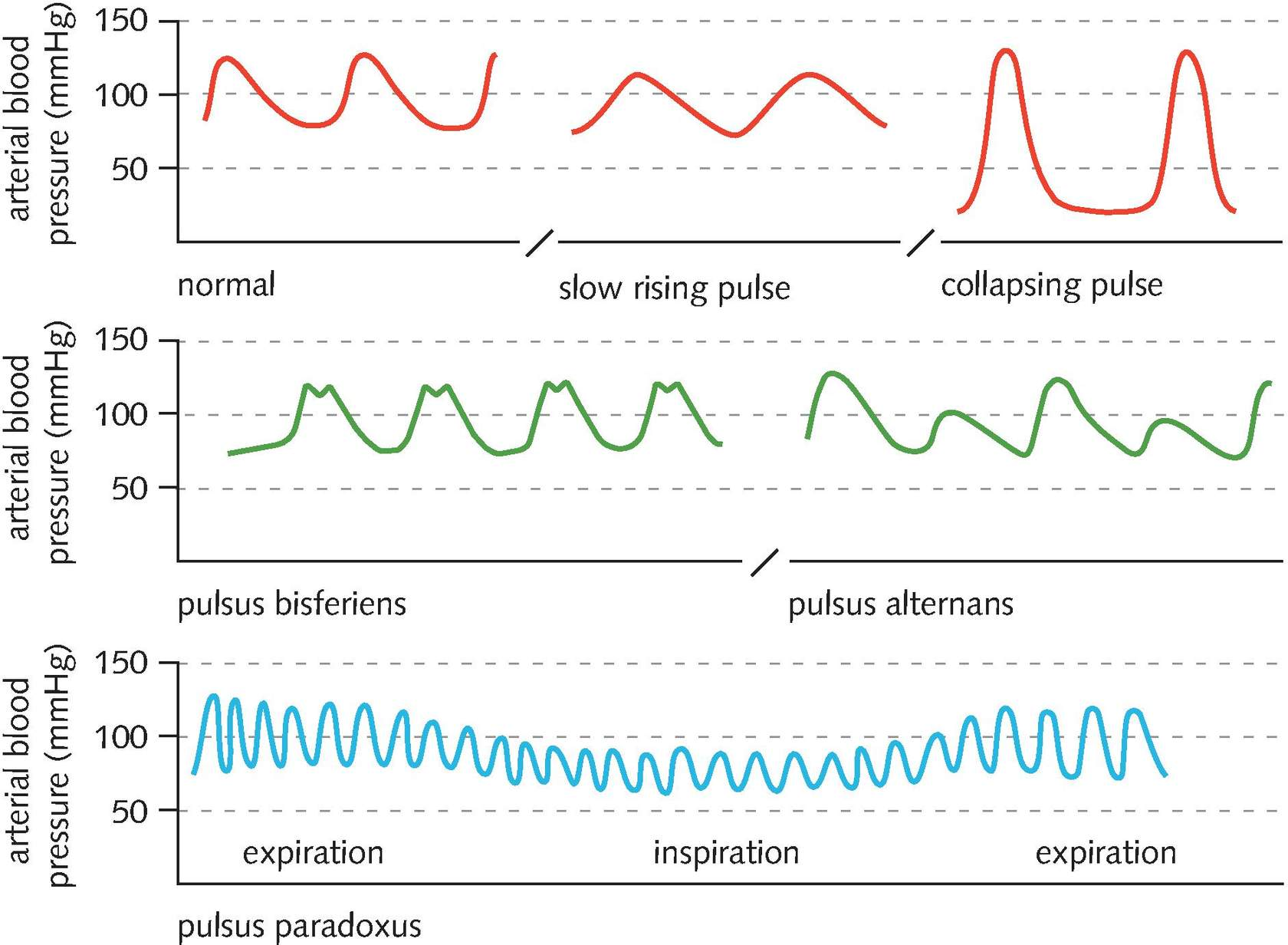
pulsus alternans
Alternating strong and weak beats
Can be caused by left ventricular failure
carotid pulse volume categories
strong
weak and 'thready'
normal

carotid pulse character categories
Collapsing pulse
Bifid pulse (pulsus bisferiens)
Plateau pulse
Pulsus alternans
JVP
jugular venous pressure
reflects right atrial pressure
visible in around 50% of people
elevated JVP can indicate:
right heart failure
fluid overload
say: “I’m looking at the base of the neck between the two heads of the sternocleidomastoid”"
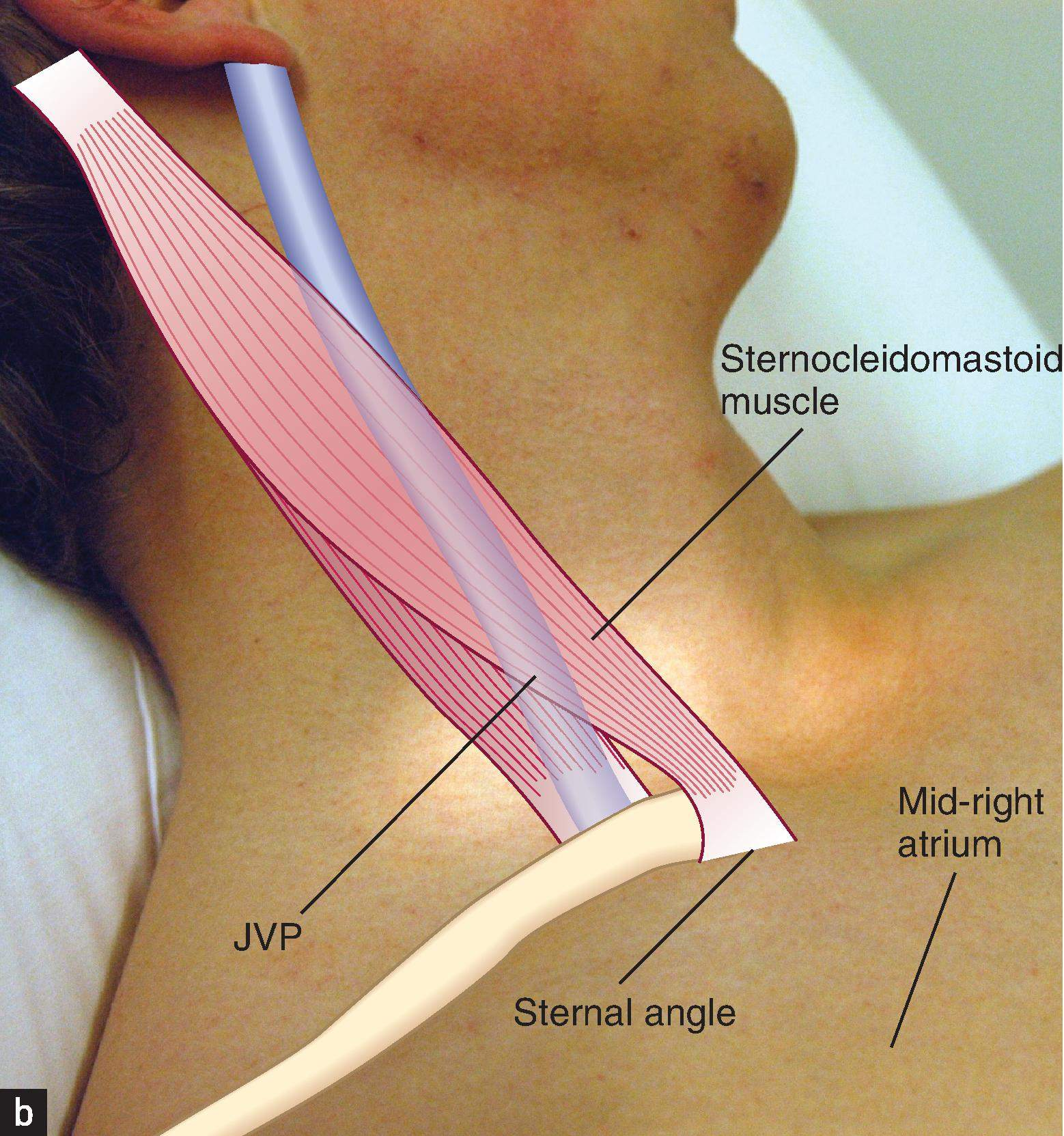
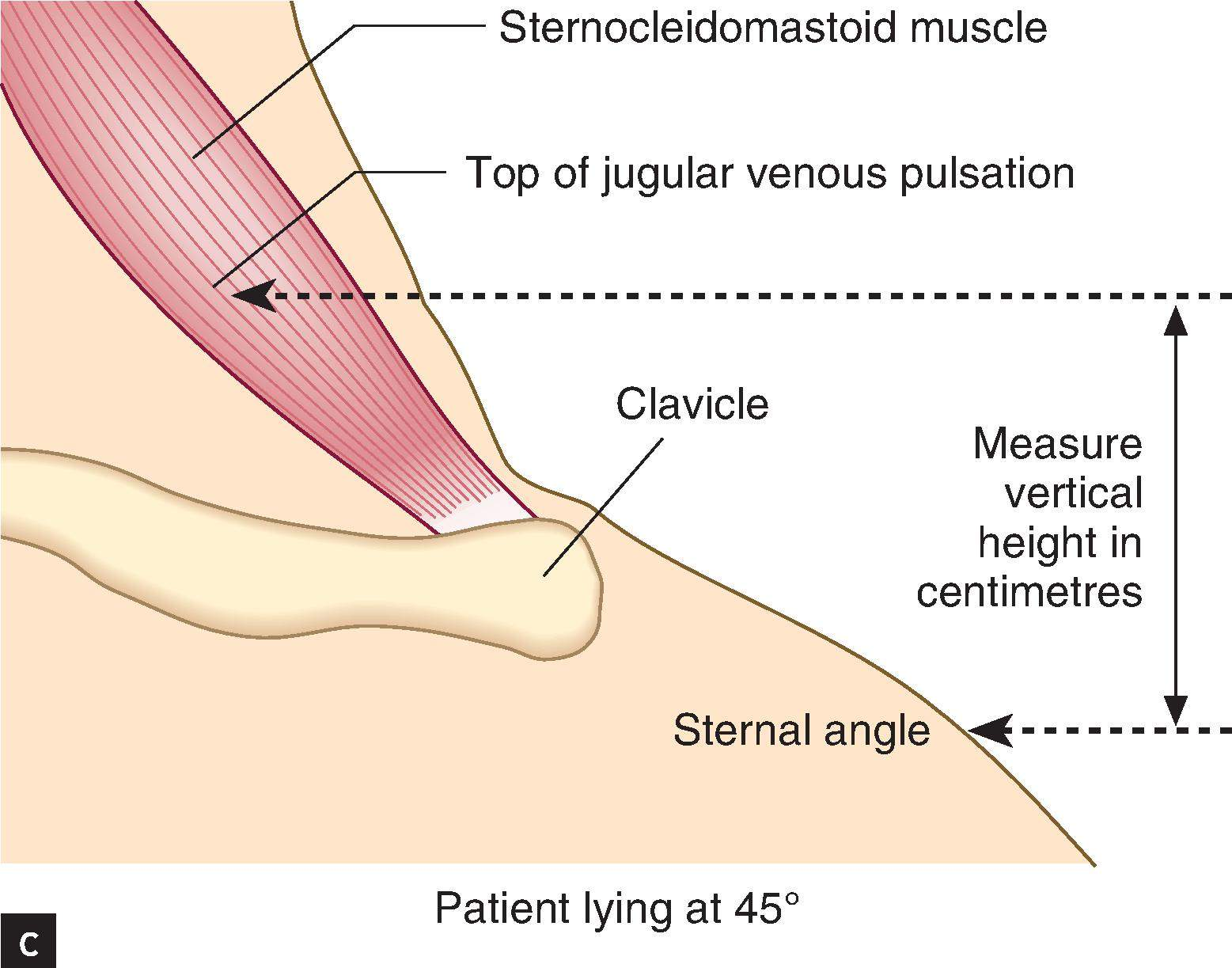
how to measure JVP
patient is positioned at a 45° angle with their head supported on a pillow
Ask the patient to turn their head away from you slightly
Look at the base of the neck for a double pulsation
say: “I’m looking at the base of the neck between the two heads of the sternocleidomastoid”
then:
Identify the highest point of the pulsation up the internal jugular vein and draw an imaginary horizontal line across to vertically above the sternal angle (Angle of Louis)
Measure or estimate the vertical distance between this point and the sternal angle
A normal JVP height is 3cm or less
then:
abdominojugular reflux test:
ask whether the patient has any abdominal pain
compress over the centre of the abdomen firmly, using the flat of your hand
hold for 10 seconds while watching the JVP
abdominal pressure increases venous return to the right atrium
it is normal for the JVP to rise transiently
should return to normal within a few seconds as the compliance of the right heart and vessels adapts to the increased volume
A positive (bad) test is when the JVP remains elevated at > 4 cm for the full 10 seconds that you maintain pressure
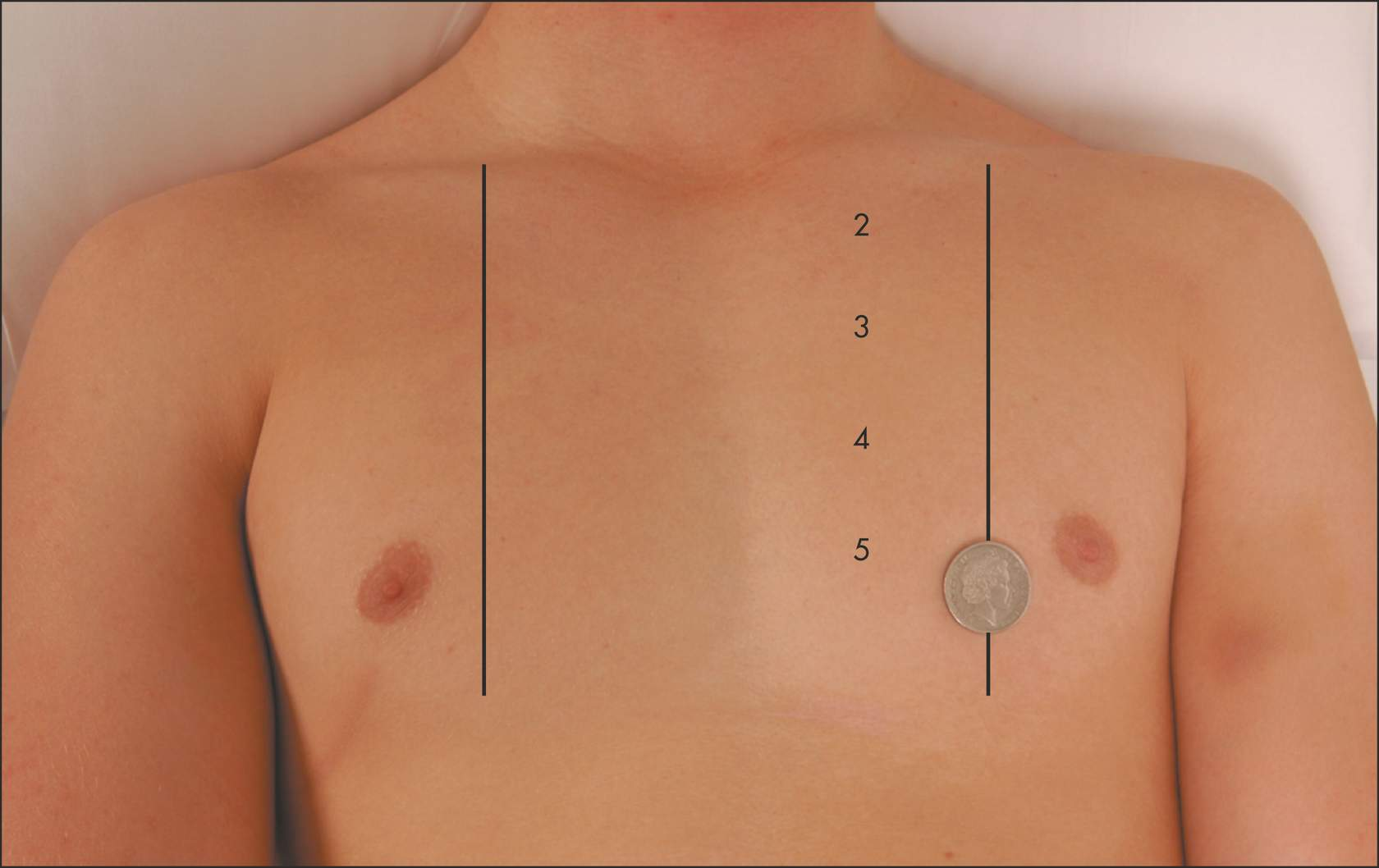
types of visible pulsatations
Apex of the heart (coin)
in a thin person
in cardiac conditions that cause a forceful apex beat
A right ventricular impulse may be seen in the 3rd, 4th or 5th intercostal spaces at the left sternal edge
in right ventricular hypertrophy
Over the pulmonary artery at the left 2nd intercostal space
if severe pulmonary hypertension is present
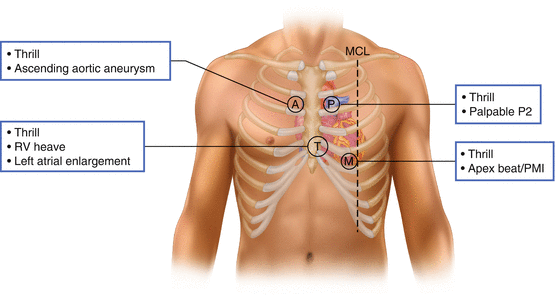
apex beat palpation
5th left intercostal space (demonstrate counting out the rib spaces)
the tips of all the fingers of the right hand flat on the chest (palpable in 50% patients)
roll the patient into the left lateral position
Identify:
whether or not it is palpable
normal position, or is it displaced left or right
e.g. left displacement in volume overload in mitral regurgitation
character:
A forceful or pressure-loaded 'heaving' apex beat
in left ventricular hypertrophy
Causes:
hypertension
aortic stenosis
A volume-loaded 'thrusting' apex beat (displaced laterally and inferiorly)
in left ventricular dilatation
Causes:
mitral regurgitation
dilated cardiomyopathy
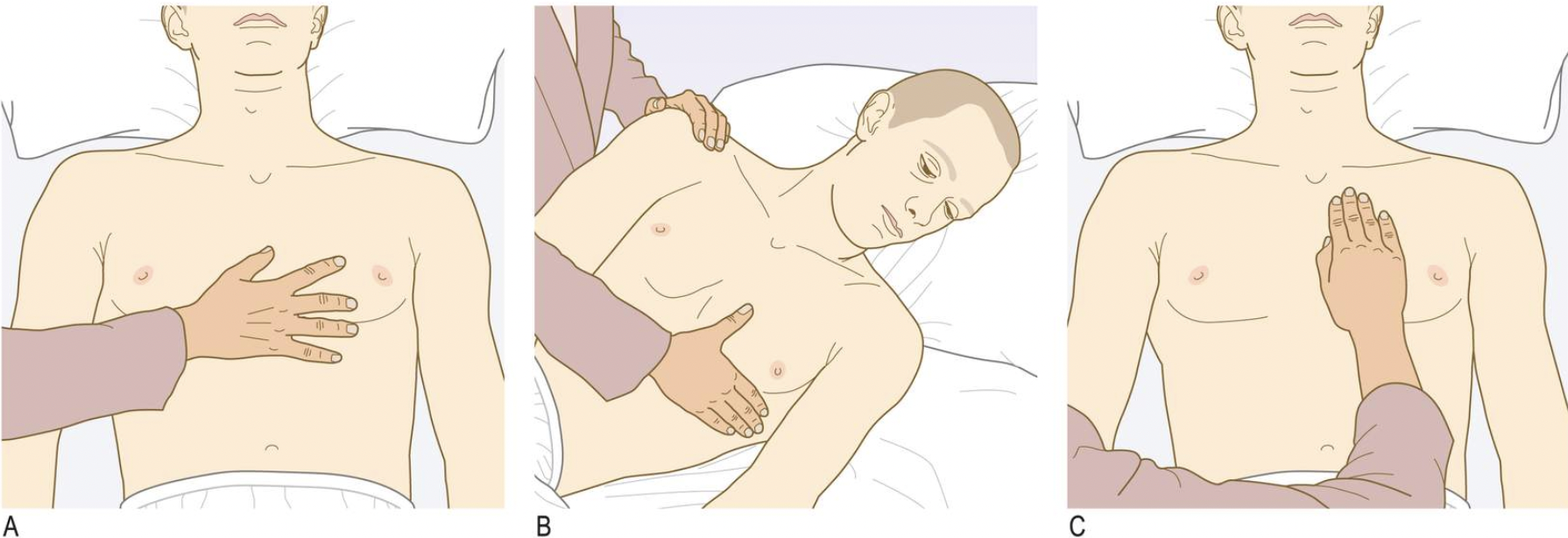
tricuspid palpation
Sit the patient forward
use the heel of the hand flat to palpate over the left sternal edge
Identify:
heaves (or ‘parasternal impulse’)
in right ventricular hypertrophy
pulmonary hypertension
chronic lung disease: chronic hypoxia leading to constriction of the pulmonary vasculature
left heart failure causing congestive cardiac failure
if the patient is thin
place your fingers flat on the chest (A)
identify:
thrills (palpable murmur that feels like a rapid vibration under your fingers)
suggests severe valve disease
useful for murmur grading
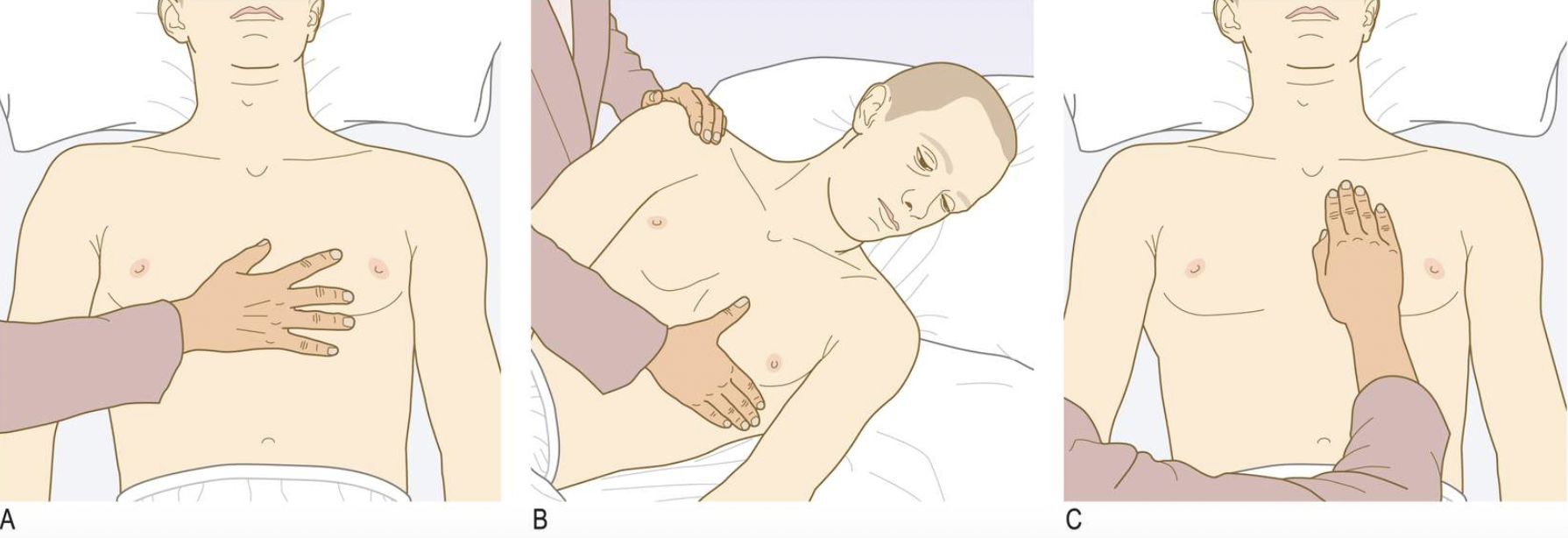
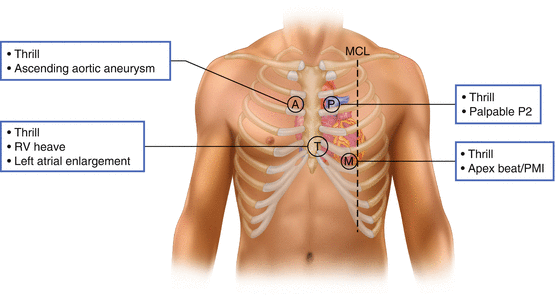
mitral palpation
after palpating for the apex beat, with patient rolled to their left side
feel with the flat of your hand (with fingers extended) (B)
identify:
thrills (palpable murmur that feels like a rapid vibration under your fingers)
suggests severe valve disease
useful for murmur grading
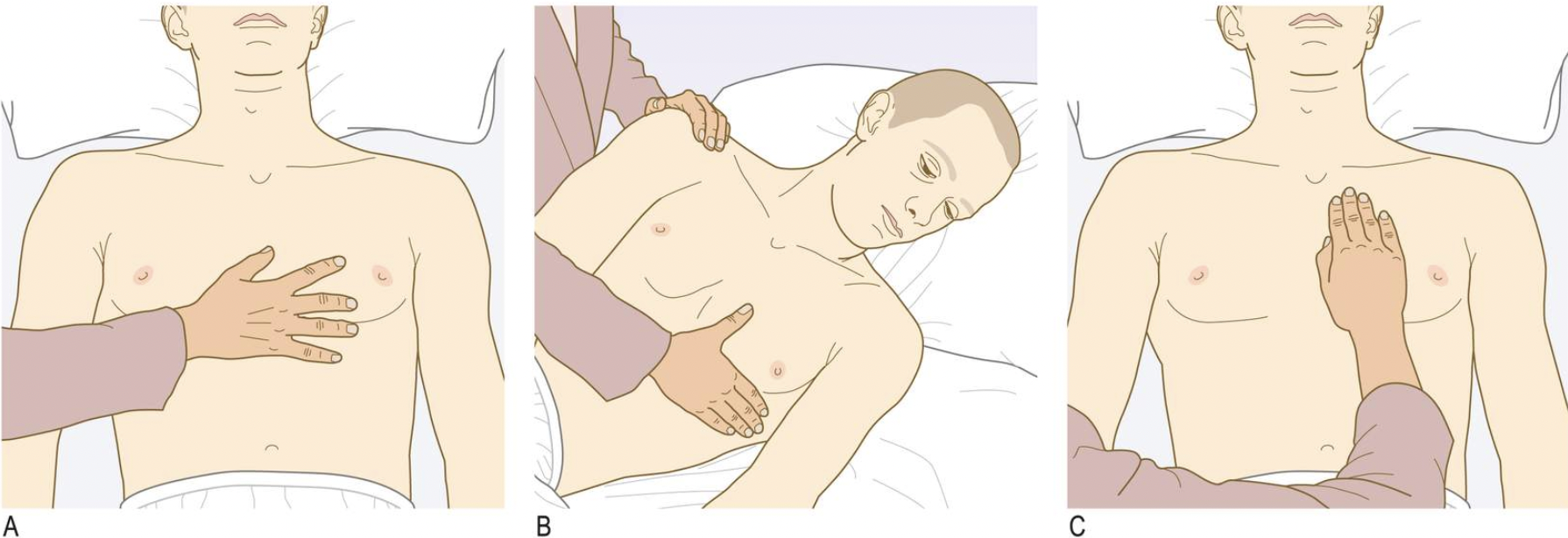
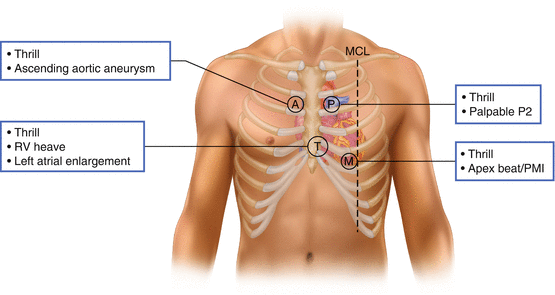
aortic and pulmonary palpation
with the patient sitting forward
feel with the flat of your hand (with fingers extended) over the aortic and pulmonary areas (base of the heart) (C)
identify:
thrills (palpable murmur that feels like a rapid vibration under your fingers)
suggests severe valve disease
useful for murmur grading
splitting
clearly heard gap in the second heart sound (S2, closure of aortic and pulmonary valves)
significant delay between aortic valve closure and pulmonary valve closure
normal: on deep inspiration
pathological: right bundle branch block (abnormal conduction)
third heart sound (S3)
unexpected heart sound heard shortly after S2 (during early diastole)
heard:
with the bell (low pitched)
over the apex (patient left lateral position/side) or the left sternal edge
can occur:
in healthy individuals (especially younger patients)
or
where there is high cardiac output
or
left ventricular failure and dilatation
fourth heart sound (S4)
unexpected heart sound heard shortly before S1 (late diastole)
heard:
with the bell (low pitched)
over the apex (patient left lateral position/side) or the left sternal edge
can occur in high pressure states such as:
aortic stenosis
hypertension
murmurs
additional heart sounds due to turbulent blood flow (stenosis or regurgitation (??))
if identified, describe:
Timing (during systole or diastole)
Location (over which area it is loudest)
Radiation (whether it can be heard anywhere else)
Effect of inspiration/expiration (right-sided are louder on inspiration, left-sided on expiration)
Effect of the Valsalva manoeuvre (murmurs of HOCM and mitral valve prolapse get louder on Valsalva, the rest get quieter)
Whether a thrill is present (represents more turbulence/louder murmur)
pericardial friction rub (probably not assessed)
inconsistent crunching sound which may occur in systole or diastole and may come and go
sometimes seen in pericarditis and is due to inflamed pericardial surfaces moving over each other
Auscultation steps
With the patient supine at 45°
Listen with the bell over the mitral area [for mitral stenosis, S3 or S4]
Palpate the carotid pulse simultaneously to identify S1 and S2
Ask the patient to roll to the left
mitral area [for mitral stenosis, S3 or S4]
Ask the patient to return to supine at 45°
Change to the diaphragm
mitral area [for mitral regurgitation]
in the axilla [for the radiation of mitral regurgitation]
tricuspid area [for any tricuspid murmurs]
Left sternal edge to the pulmonary area [for any aortic murmurs]
Pulmonary area [for any pulmonary murmurs]
Aortic area [for any aortic murmurs]
Change to the bell
Listen over both carotids [for radiation of aortic stenosis and for carotid bruit]
Ask the patient to hold their breath
Listen over both carotids [radiation of aortic stenosis (bilateral) or carotid bruit (unilateral or bilateral)]
Dynamic manoeuvres - Leaning Forward & Inspiration/Expiration
Dynamic manoeuvres - Valsalva manoeuvre
![<ul><li><p><span style="font-size: inherit; font-family: inherit"><strong>With the patient supine at 45°</strong></span></p><ul><li><p>Listen with the <strong>bell</strong> over the mitral area [for mitral stenosis, S3 or S4]</p></li><li><p>Palpate the carotid pulse simultaneously to identify S1 and S2</p></li></ul></li><li><p><span style="font-size: inherit; font-family: inherit"><strong>Ask the patient to roll to the left</strong></span></p><ul><li><p>mitral area [for mitral stenosis, S3 or S4]</p></li></ul></li><li><p><span style="font-size: inherit; font-family: inherit"><strong>Ask the patient to return to supine at 45°</strong></span></p><ul><li><p>Change to the <strong>diaphragm</strong></p></li><li><p>mitral area [<em>for mitral regurgitation</em>]</p></li><li><p>in the axilla [<em>for the radiation of mitral regurgitation</em>]</p></li><li><p>tricuspid area<strong> </strong>[<em>for any tricuspid murmurs</em>]</p></li><li><p>Left sternal edge to the pulmonary area<strong> </strong>[<em>for any aortic murmurs</em>]</p></li><li><p>Pulmonary area [<em>for any pulmonary murmurs</em>]</p></li><li><p>Aortic area [<em>for any aortic murmurs</em>]</p></li><li><p>Change to the <strong>bell</strong></p></li><li><p>Listen over both carotids [<em>for radiation of aortic stenosis and for carotid bruit</em>]</p></li></ul></li><li><p><span style="font-size: inherit; font-family: inherit"><strong>Ask the patient to hold their breath</strong></span></p><ul><li><p>Listen over both carotids [<em>radiation of aortic stenosis (bilateral) or carotid bruit (unilateral or bilateral)</em>]</p></li></ul></li><li><p><span style="font-size: inherit; font-family: inherit"><strong><em>Dynamic manoeuvres - Leaning Forward & Inspiration/Expiration</em></strong></span></p></li><li><p><span style="font-size: inherit; font-family: inherit"><strong><em>Dynamic manoeuvres - Valsalva manoeuvre</em></strong></span></p></li></ul><p></p>](https://knowt-user-attachments.s3.amazonaws.com/6462789f-e349-4f30-a66a-a1732492eb77.png)
leaning forward inspiration and expiration
Ask the patient to lean forwards and breathe all the way in and hold then all the way out and hold
[To help differentiate between right sided murmurs (louder on inspiration) and left sided murmurs (louder on expiration)]
Tip: Right Inspiration, Left Expiration (RILE)
Listen over the aortic area with the diaphragm [for any aortic murmurs]
Listen over the left sternal edge (Erb's Point) with the diaphragm [for radiation of aortic regurgitation]
Valsalva maneuver
Ask the patient to take a deep breath in, then pinch their nose and try to pop their ears like on a plane [to accentuate the murmur of HOCM, mitral valve prolapse]
Listen over the left sternal edge (Erb's Point) with the diaphragm [for mid-systolic murmur of HOCM which gets louder on Valsalva]
Listen over the mitral area with the diaphragm [for late-systolic murmur of mitral valve prolapse which gets louder on Valsalva]
![<p><span style="font-size: inherit; font-family: inherit"><strong>Ask the patient to take a deep breath in, then pinch their nose and try to pop their ears like on a plane [to accentuate the murmur of HOCM, mitral valve prolapse]</strong></span></p><ul><li><p>Listen over the left sternal edge (Erb's Point) with the <strong>diaphragm</strong> [<em>for mid-systolic murmur of HOCM which gets louder on Valsalva</em>]</p></li><li><p>Listen over the mitral area with the <strong>diaphragm</strong> [<em>for late-systolic murmur of mitral valve prolapse which gets louder on Valsalva</em>]</p></li></ul><p></p>](https://knowt-user-attachments.s3.amazonaws.com/46149d95-278a-406a-bbdf-864c6bdd8ccd.png)
carotid bruit
swooshing sound over carotid artery
may indicate plaque buildup in the carotid artery
HOCM
hypertrophic obstructive cardiomyopathy
heart muscle thickens, particularly in the septum, causing a blockage of blood flow
posterior back examination
Inspect for any scars and any obvious deformities of the chest wall or spine
Palpate for sacral oedema:
press over the sacrum gently for 5-10 seconds
allows any fluid to be pushed out of the way
After releasing the pressure, look and feel for a pit in the area (pitting oedema)
fluid will accumulate at the sacrum in patients who spend a lot of time in bed
Pitting oedema: sign of cardiac failure or fluid overload


