Intergumentary system
1/143
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
144 Terms
intergumentary system
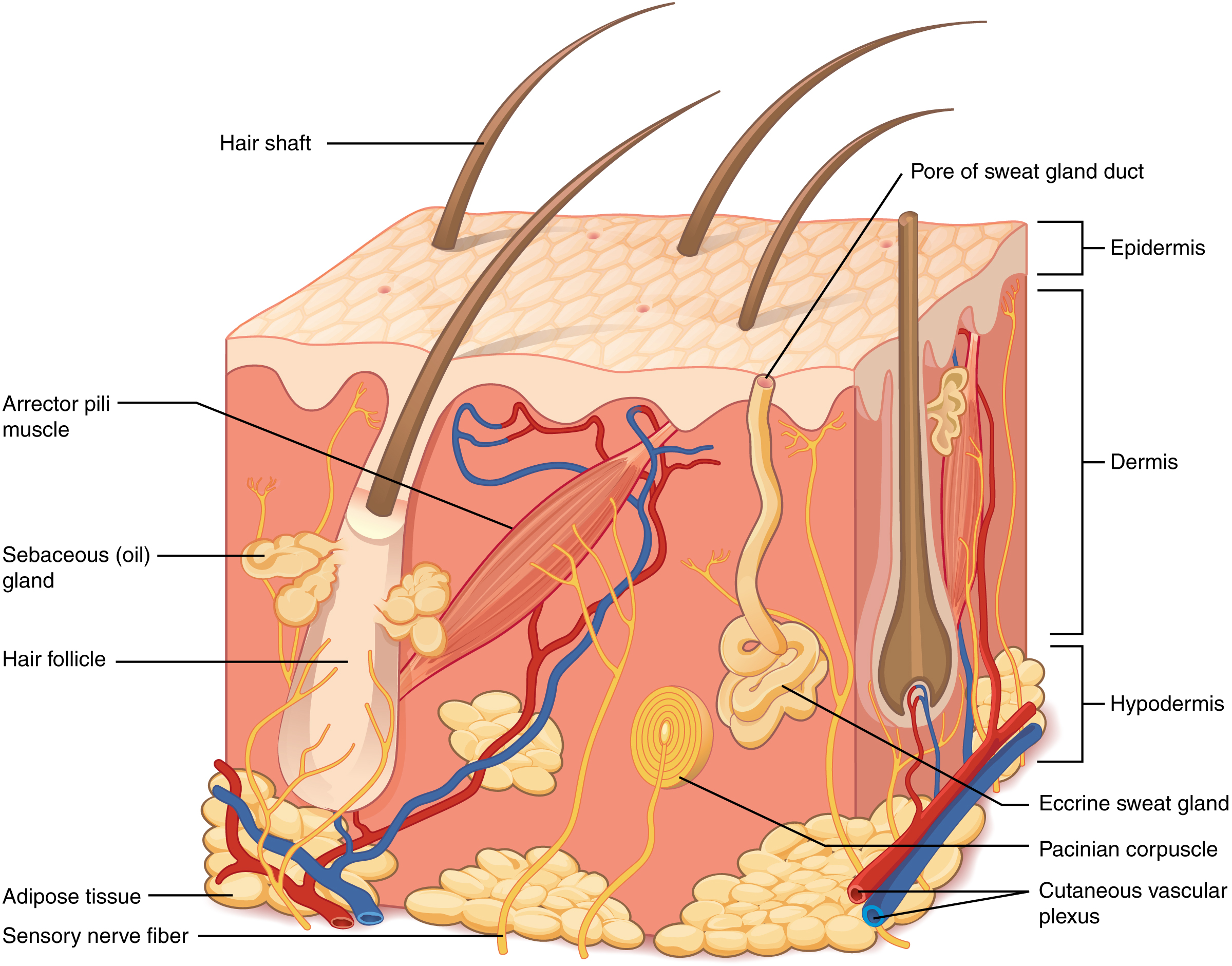
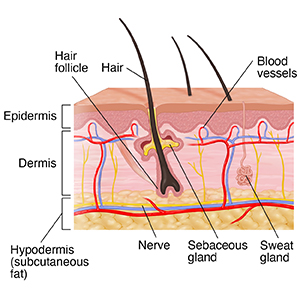
The integumentary system consists of skin, hair, nails, and associated glands
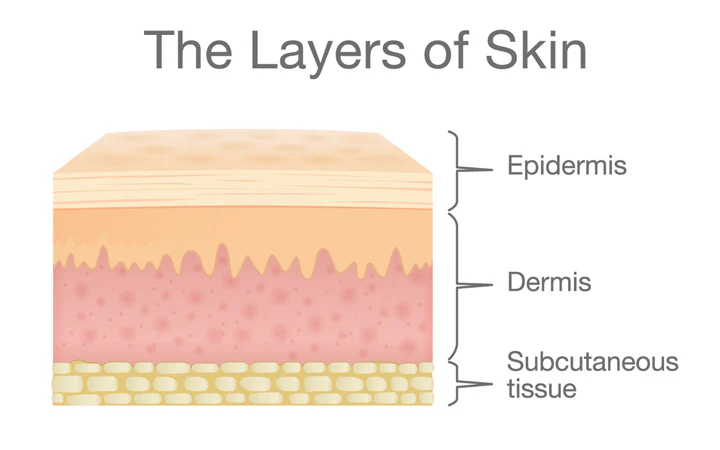
The skin (integument) is body's largest and heaviest organ. Consists of two layers:
Epidermis: made up of stratified squamous epithelium
Dermis: is a deeper connective tissue laver
Hypodermis– not part of the skin but usually studied with it
Skin is a cutaneous membrane, which is a type of epithelial membrane. The word cutaneous means "relating to the skin".
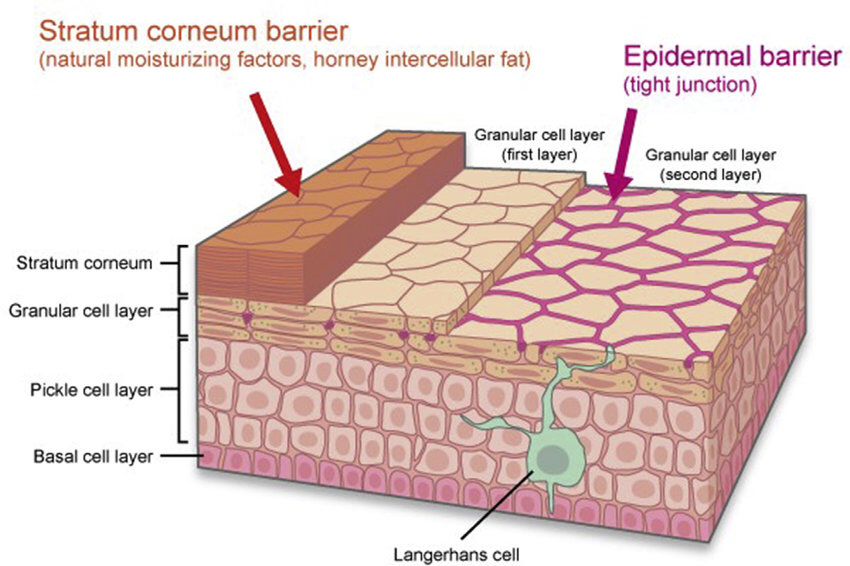
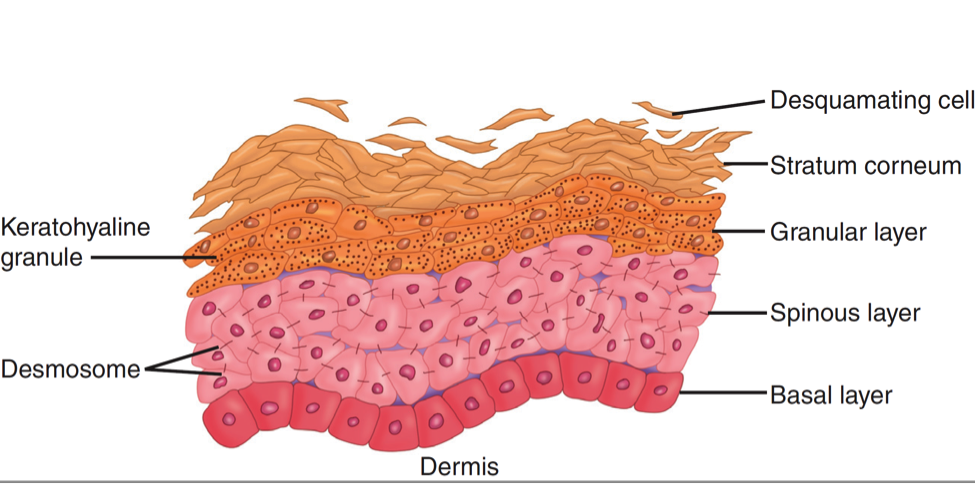
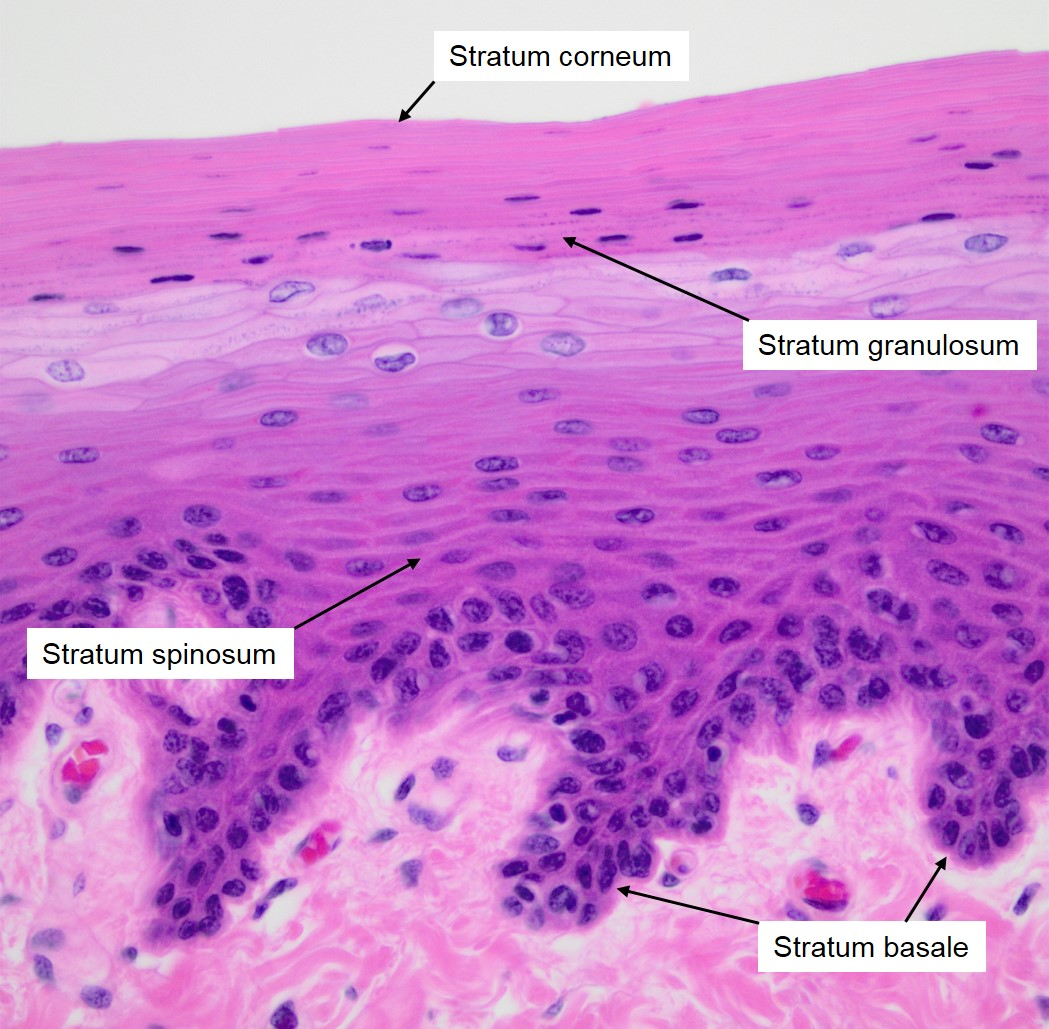
what are the layers of the epidermis
stratum basale, stratum spinosum, and stratum granulosum layers
what cells are dead in the epidermal layer
stratum corneum, stratum lucidum
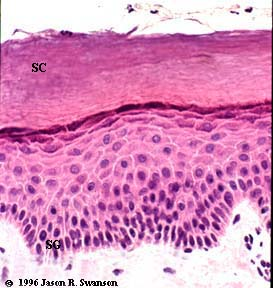
The epidermal water barrier
It's located in the stratum corneum (SC), the outermost layer of the epidermis.
Thick vs thin skin
skin is classified as thick or thin based on epidermis
Thick skin is found in areas where there is a lot of abrasion- fingertips, palms and the soles of your feet. Has sweat glands, but no hair follicles or sebaceous glands
Thin skin covers rest of the body; has hair follicles, sebaceous glands, and sweat glands

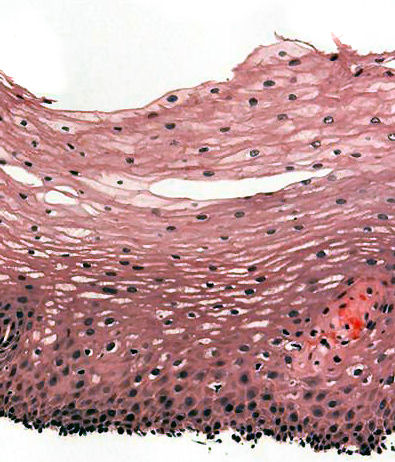
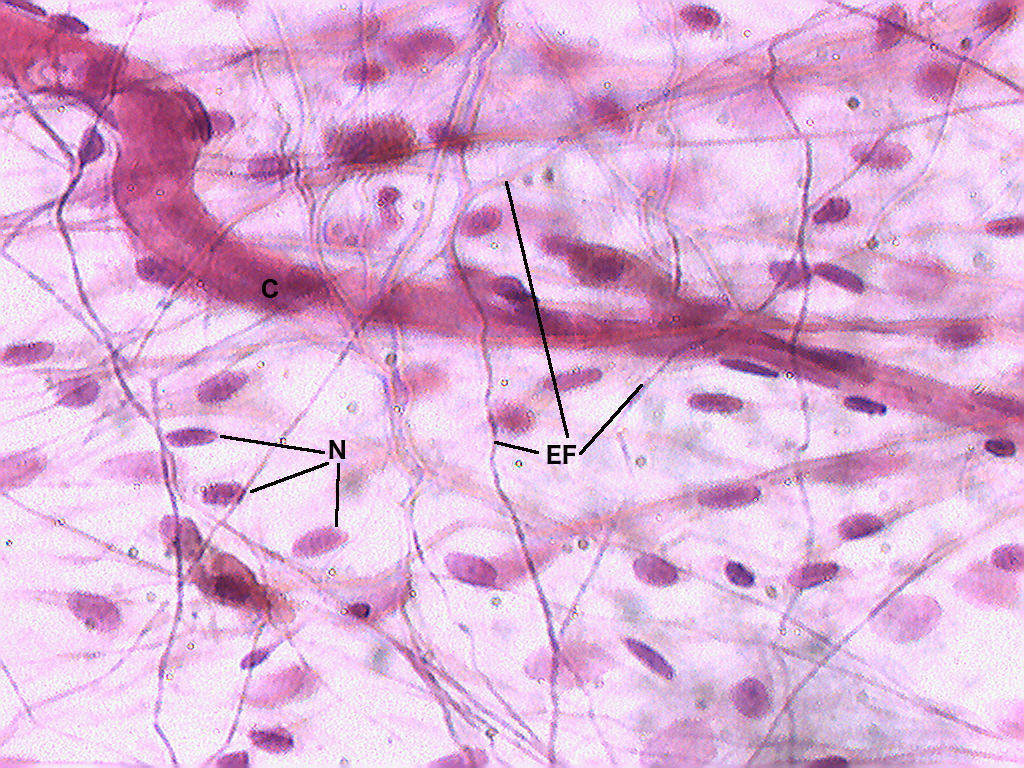
thin skin histology
Thin skin actually has a thicker dermis than thick skin, which makes thin skin easier to suture, if it gets damaged. Thin skin also has fewer eccrine/merocrine sweat glands.
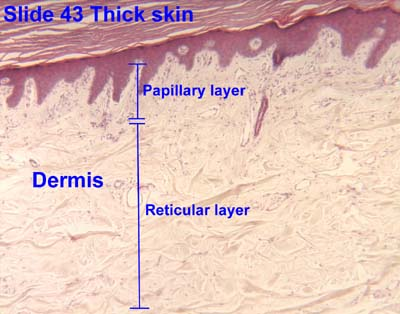
thick skin histology
Thick skin has a thinner dermis than thin skin, and does not contain hairs, sebaceous glands, or apocrine sweat glands.
Thick skin is only found in areas where there is a lot of abrasion - fingertips, palms and the soles of your feet.
where is the layer of the epidermis where cells begin to lose their nuclei and immortalize
The layer of the epidermis where cells begin to lose their nuclei is the stratum granulosum
layers of the epidermis
Stratum (layer) corneum: Up to 30 layers of dead, scaly, keratinized cells (corneocytes.) Resists abrasion, penetration, regulates water loss
Stratum lucidum: Thin, pale layer found only in thick skin. Layer composed of “lucid ghost cells”
Stratum granulosum: 3-5 layers of flat, living keratinocytes with protein granules that will eventually lose their organelles and move up to form the stratum corneum.
Stratum spinosum: Several layers of living keratinocytes joined by desmosomes (sticky proteins) and tight junctions
Stratum basale: Single layer of stem cells and keratinocytes resting on the basement membrane, along with melanocytes and tactile cells.
Can lemurs get some bamboo?
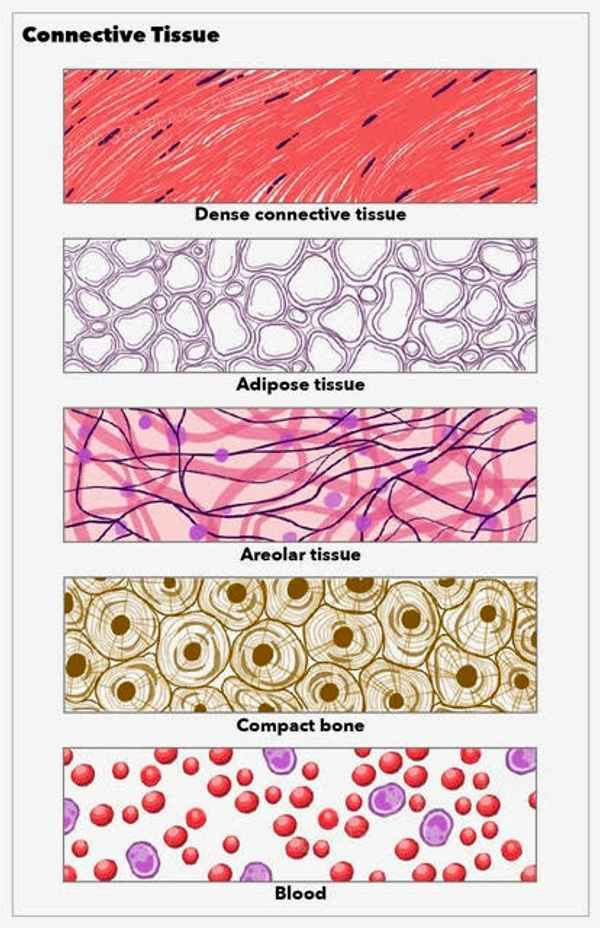
dermis
The dermis is a type of connective tissue, which is a non-epidermal type of tissue that connects things together in the body.
Composed mainly of collagen (a protein)
Well supplied with blood vessels, sweat glands, and nerve endings; houses hair follicles, nail roots
Muscles of facial expression attach to dermis
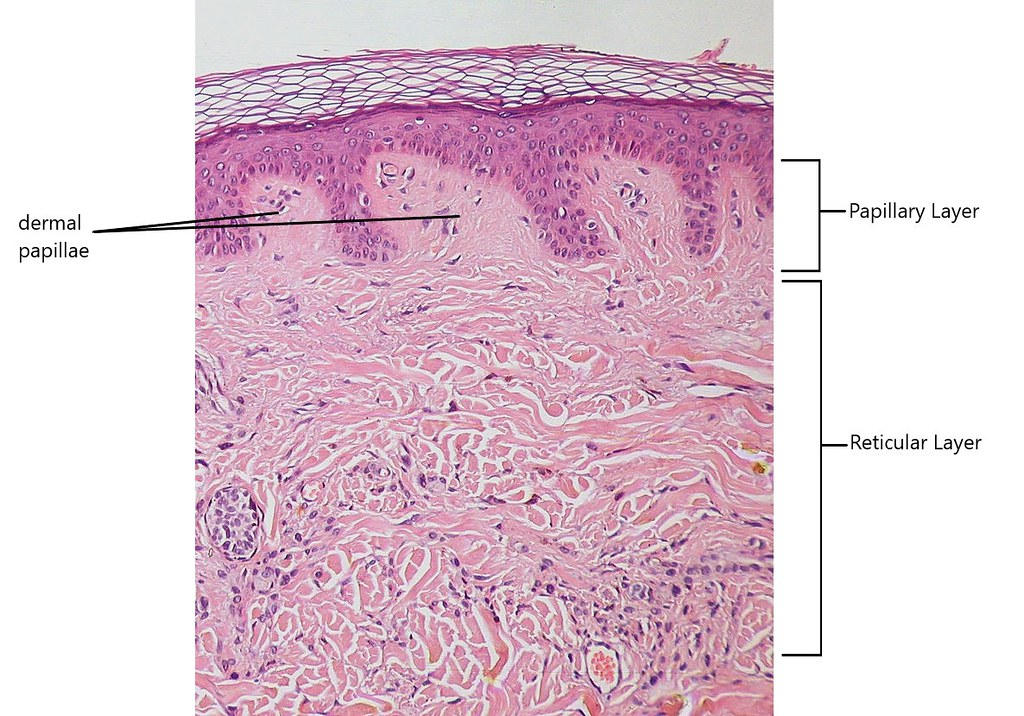
Dermis has two layers: papillary and reticular
what are the dermal layers
Papillary layer
composed of thin, smaller collagen
Thin zone of areolar (connective) tissue in and near the dermal papillae
Allows for mobility of leukocytes and other defense cells
Rich in small blood vessels
Reticular layer:
composed of thick, larger collagen bundles
Deeper, thicker layer of dermis
Composed of dense irregular connective tissue
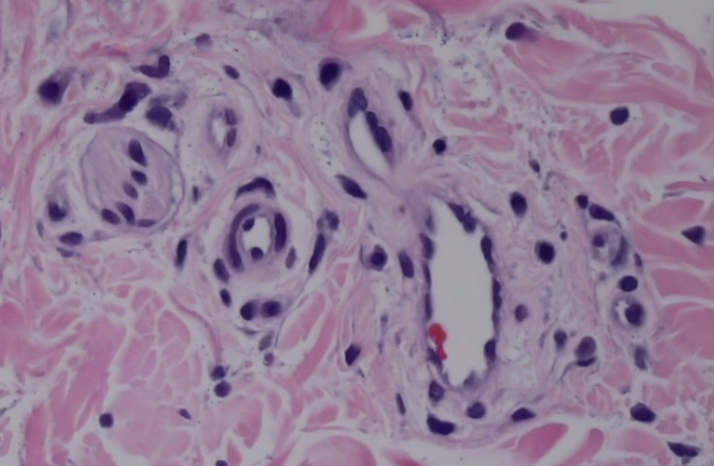
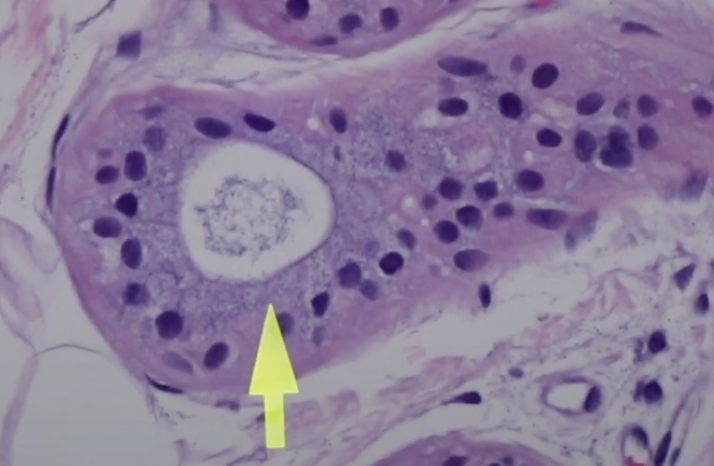
rete ridges
wavy microstructures that connect the epidermis and dermis in the skin
Rete ridges are made up of epithelial cells that extend into the dermis, the connective tissue beneath the skin.
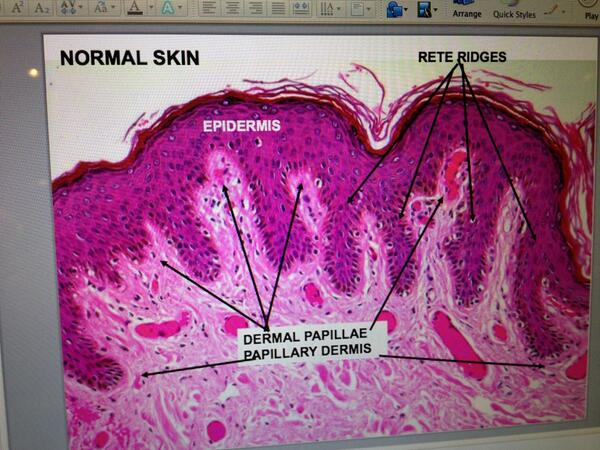
what are in between/under rete ridges
the papillary dermis— each invagination are dermal papilla
significance of the blood vessels in dermal papillae for the epidermis
Since the epidermis lacks blood vessels, it relies on diffusion from capillaries in the dermal papillae for oxygen and nutrients. This sustains basal keratinocytes, which continuously divide and replace old skin cells. When the epidermis is damaged (e.g., from cuts or burns), the dermal papillae enhance regeneration by:
Delivering oxygen and glucose for cellular metabolism.
Providing growth factors that stimulate keratinocyte proliferation.
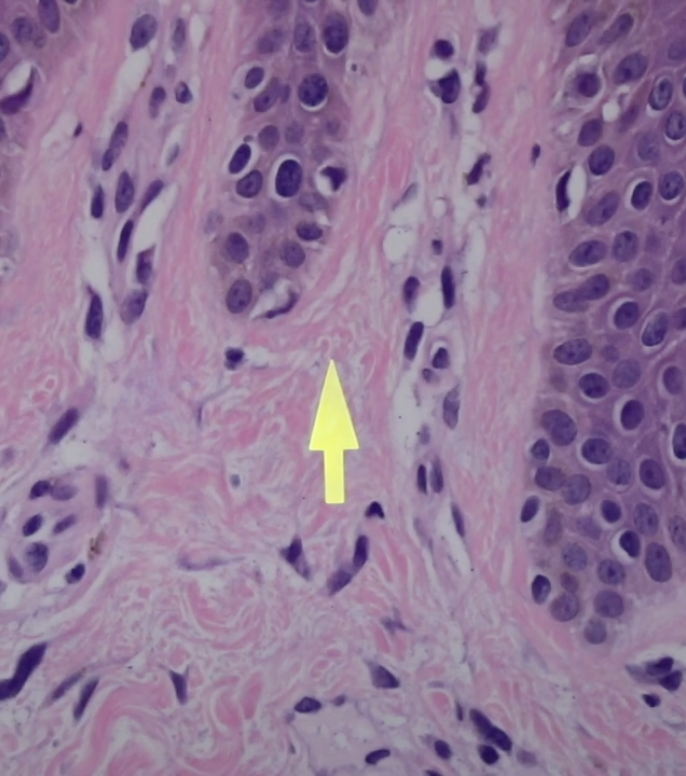
what protein fibers compose most of the soft tissue and bone around the body
collagen, stained pink
what are the principal functions of the integumentary system
protection
water retention
thermoregulation
vitamin d synthesis
cutaneous sensation
"Penguins Wear Tuxedos Very Classily"
how many layers of epithelial cells does the epidermis have
4 or 5
dis- prefix meaning
apart
avascular meaning
no blood vessels
what is the body’s largest organ?
the skin.
name the different layers of the skin
epidermis
dermis
hypodermis/subcutaneous tissue
histo- prefix meaning
tissue
ana- prefix meaning
apart
epi- meaning
above
reticular dermis
main supporting structure of the skin- thickest layer (excluding fat)

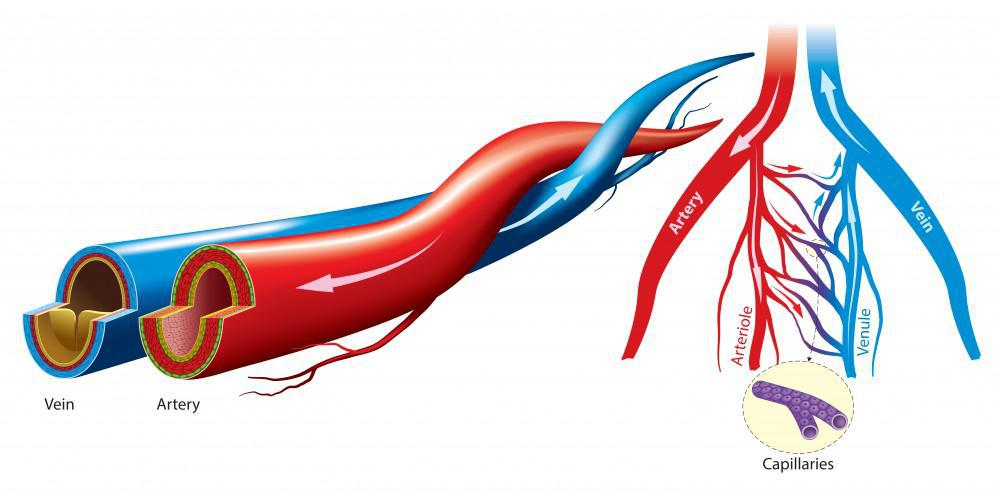
how to recognize a vascular channel/vein
white space
lined by a thin single layer of endothelial cells
how to recognize sweat glands
white space/circle with goo in the middle (sweat)
lined by epithelium
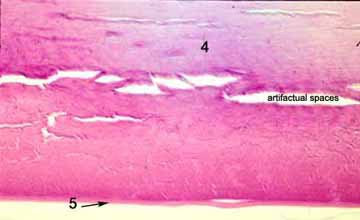
artifactual space
an empty space or other alteration in a tissue sample that is not normally present
could be fat cells deprived of lipids
poor sample preparation
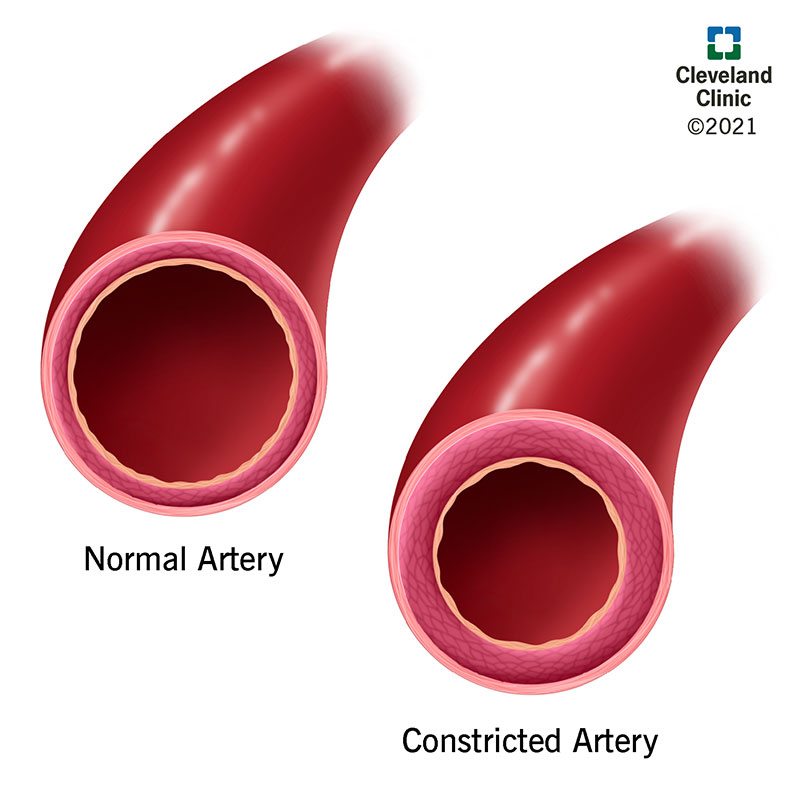
veins vs arteries histology
Veins:
Carry blood towards the heart.
Low pressure, thinner walls.
Have valves to prevent backflow.
Typically carry deoxygenated blood (except pulmonary veins).
Arteries:
Carry blood away from the heart.
High pressure, thicker walls.
No valves (except at heart).
Typically carry oxygenated blood (except pulmonary arteries).
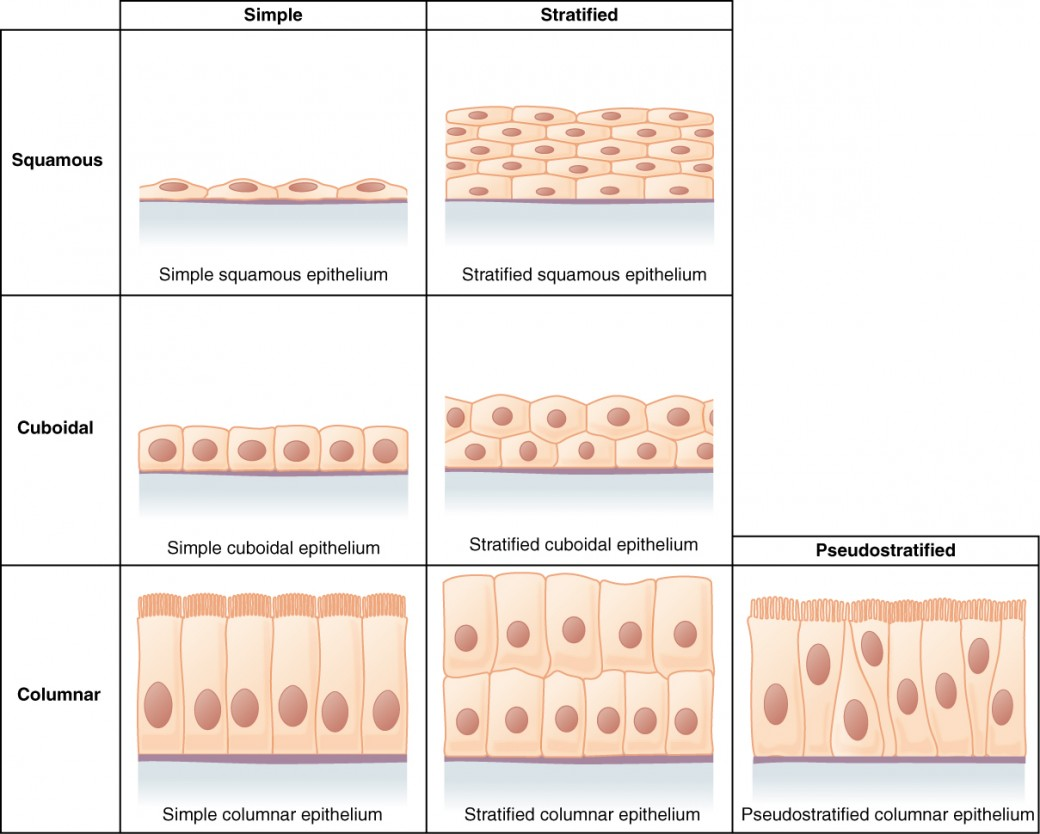
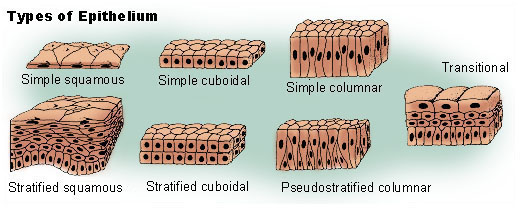
what type of tissue is the epidermis made up of
stratified squamous epithilium that contains layers of cells called keratinocytes
what tissue is the stratum basale made up of
cuboidal to columnar stem cells resting on the basement membrane that separates the epidermis from the dermis.
what cells make up the nail plate
Onychocytes are the main structural cells that make up the hard, visible portion of the nail (the nail plate). They are produced in the nail matrix, undergo keratinization, and are then layered tightly to form the nail plate.
Onychocytes are formed through a process called keratinization, where living cells from the nail matrix harden and die as they become filled with keratin, a structural protein. Once fully keratinized, the cells are no longer metabolically active.
Nail Growth: The nail plate itself (composed of onychocytes) is pushed forward by new, living cells produced in the nail matrix. These new cells eventually undergo keratinization, replacing the older, dead onychocytes.
desmosomes
protein complexes that act as adhesive junctions between cells. They are responsible for maintaining the structure and strength of tissues
Keratinocytes in all layers are linked to each other via desmosomes which connect intracellularly to intermediate filaments.
desmosomes in adjacent cells are linked via integral membrane proteins from a large family of genes called cadherins. In skin, desmosomes primarily contain a type of cadherin called desmoglein
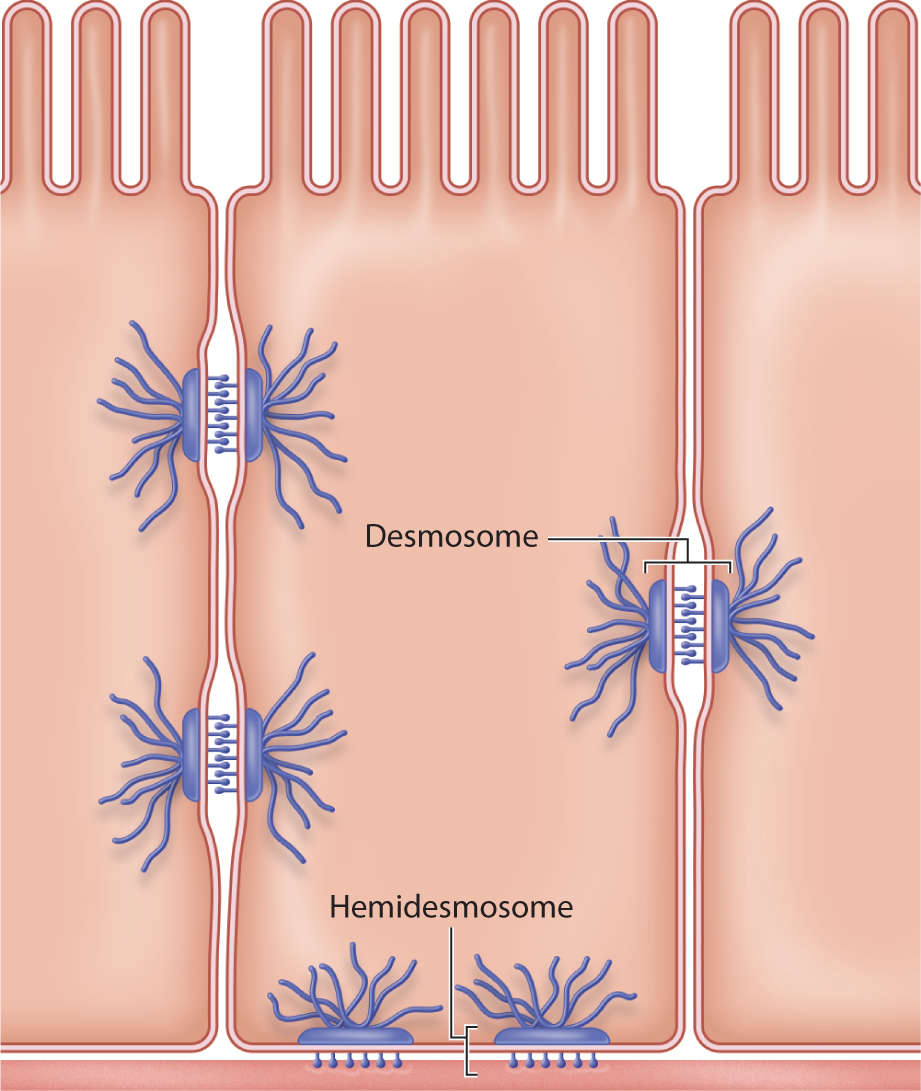
stratum basale
the deepest layer of the epidermis, the outer layer of the skin.
It consists of a single row of cuboidal or columnar cells called keratinocytes.
Keratinocytes are attached to the underlying basement membrane by hemidesmosomes.
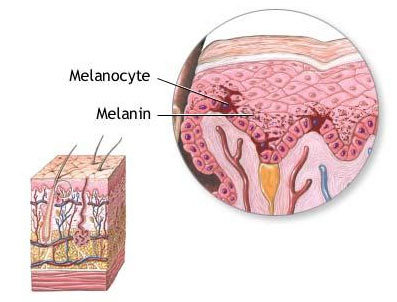
Melanocytes, which produce melanin (skin pigment), are also present in the stratum basale.
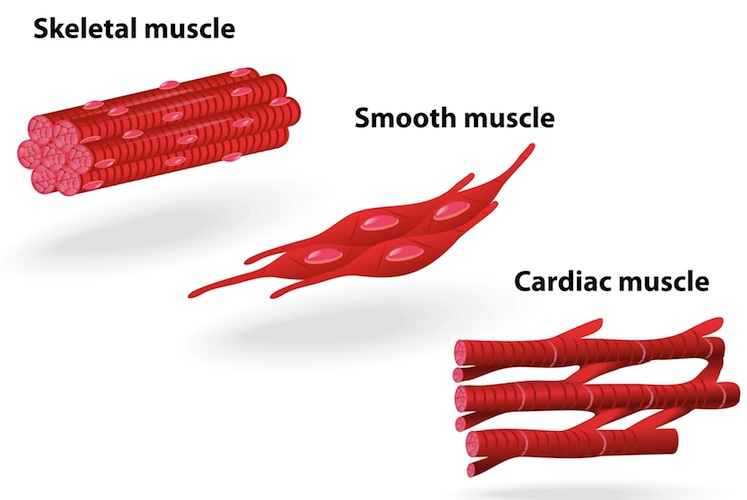
Tissues
tissues are groups of cells working together to carry out a particular task within the body.
they can provide protection, support, movement, and communication, depending on the type of tissue
four main types: epithelial, connective, muscle, and nervous tissue
Hypodermis/subcutaneous tissue
layer of connective tissue beneath the skin
Contains more areolar and adipose tissue than the dermis
Pads body and binds skin to underlying tissues
Common site of drug injection due to many blood vessels
Energy reservoir
Thermal insulation
Thicker in women, thinner in infants, elderly
Keratinocytes role
Protection: Keratinocytes produce keratin, a tough, fibrous protein that provides mechanical strength to the skin and acts as a water-resistant barrier.
Waterproofing: As keratinocytes mature and move to the surface of the skin, they undergo a process called keratinization, where they become filled with keratin. This process makes the skin impermeable to water, preventing excessive water loss from the body.
Immune Defense: They are involved in the immune response. Keratinocytes can detect invading microorganisms and release signaling molecules to initiate an inflammatory response, in collaboration with immune cells like Langerhans cells (dendritic cells in the skin).
Keratinocytes Structure
Keratinocytes are polygonal or cuboidal when deep in the epidermis, and as they move upward, they flatten out.
Location: These cells are found in the epidermis, specifically in the stratum basale (the deepest layer) and move upward through the layers of the epidermis.
Keratinization Process keratinocytes
Mitosis: New keratinocytes are formed in the stratum basale and begin to divide and migrate upwards.
Keratin Production: As they move into the stratum spinosum, they start to produce keratin, which toughens and waterproofs them.
Cell Death: By the time they reach the stratum corneum, keratinocytes are fully keratinized and dead, forming a protective barrier.
Melanocytes role
Pigmentation: Melanocytes produce melanin, which gives the skin, eyes, and hair their color. The type and amount of melanin determine an individual's skin tone.
UV Protection: Melanin absorbs UV light and dissipates it as heat, helping to protect the skin from the harmful effects of UV radiation, such as DNA damage, sunburn, and skin cancer. This protective function is especially important in preventing damage to keratinocytes, which make up the majority of the skin.
types of melanin
Eumelanin: This type of melanin is dark brown or black and is primarily responsible for darker skin tones.
Pheomelanin: This type is yellow to red and is primarily responsible for lighter skin tones and red hair.
Melanin Distribution
Melanin Transfer: Once synthesized in the melanosomes, melanin is transferred from the melanocytes to nearby keratinocytes, where it accumulates to provide pigmentation and UV protection.
Skin Color: The amount of melanin transferred and its type influence an individual’s skin color. People with darker skin have more melanin, particularly eumelanin, while those with lighter skin have less melanin, particularly pheomelanin.
where are melanocytes found
Melanocytes reside in the stratum basale and have their dendritic processes extending between keratinocytes in the basal layer and sometimes into the stratum spinosum.
The melanocytes and keratinocytes work together to protect the skin from environmental damage. While melanocytes produce melanin for UV protection, keratinocytes help form the skin barrier that holds moisture and prevents pathogen entry.
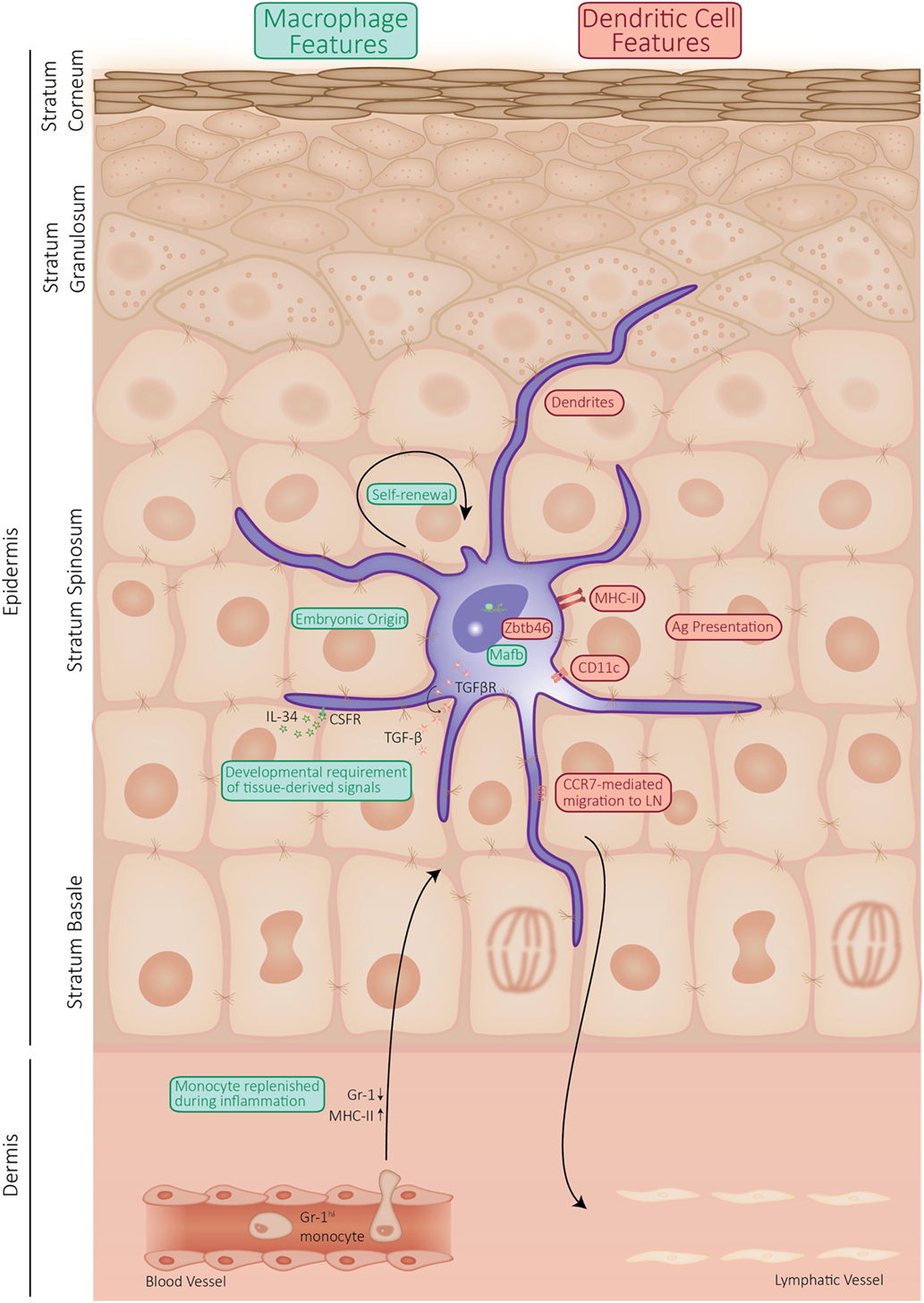
Langerhan’s cells location
found in the stratum spinosum layer of the epidermis, although they can also be present in other parts of the skin and mucous membranes. They are dispersed throughout the epidermis, making them well-positioned to detect pathogens or foreign substances.
Langerhan’s cells function
Langerhans cells are key to maintaining the immune integrity of the skin. By recognizing pathogens and initiating an immune response, they help prevent infections from reaching deeper layers of the skin or entering the bloodstream.
When Langerhans cells detect pathogens or danger signals, they release cytokines that can influence keratinocytes, triggering inflammation or changes in the epidermal layer.
In addition to pathogens, Langerhans cells can also respond to allergens. They are involved in allergic reactions, particularly in conditions like contact dermatitis, where the skin reacts to allergens like poison ivy or nickel.
Function merkel cells
Mechanoreceptors for steady pressure and texture.
Detect fine tactile sensations (e.g., texture, pressure, vibration).
Merkel Disks form synapses with sensory nerve fibers to transmit signals to the brain.
Important for fine tactile discrimination (e.g., reading Braille).
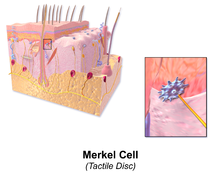
merkel cells location
Stratum basale of the epidermis (mainly in hairless skin like fingertips, palms, soles).
Evolutionary explanation for skin colors
Darker skin evolved in regions with high UV exposure (e.g., Africa, South Asia) to protect against DNA damage, folate degradation, and skin cancer.
Lighter skin evolved in regions with low UV exposure (e.g., Europe, Northern Asia) to allow better vitamin D synthesis in low sunlight conditions.
Intermediate skin tones are seen in populations from mixed or moderate UV exposure regions.
skin receptors
The skin contains specialized receptors that are sensitive to various forms of stimuli. These receptors allow us to perceive touch, temperature, pain, and pressure. They are primarily located in the epidermis and dermis, but some are also found deeper in the hypodermis.
Mechanoreceptors, Thermoreceptors, Nociceptors
mechanoreceptors
These receptors are sensitive to mechanical pressure or distortion of the skin. They help us detect touch, vibration, and pressure.
Merkel Discs (or Merkel Cells)
Meissner’s Corpuscles
Pacinian Corpuscles
Ruffini Endings:
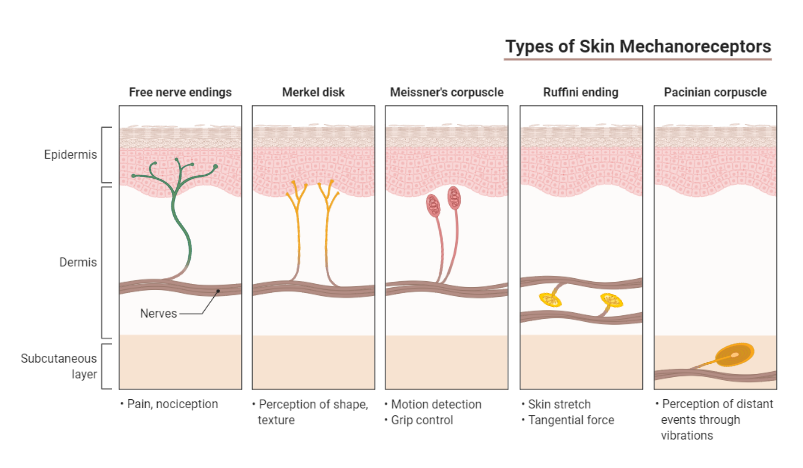
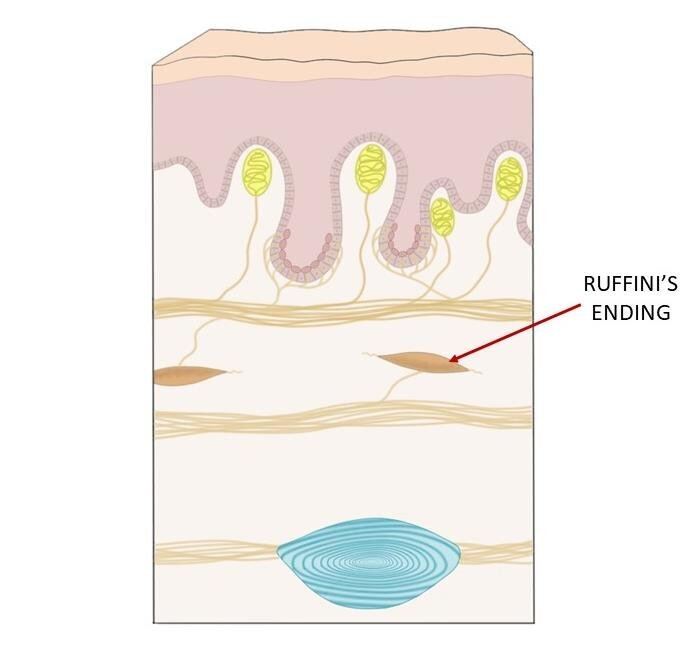
Ruffini Endings:
Stimulus: Stretching, skin deformation, sustained pressure.
Location: Deep dermis and hypodermis, particularly in the skin over joints and the back of the hand.
Structure: Spindle-shaped, and encapsulated.
Function: Detect skin stretch and proprioception (sense of body position).
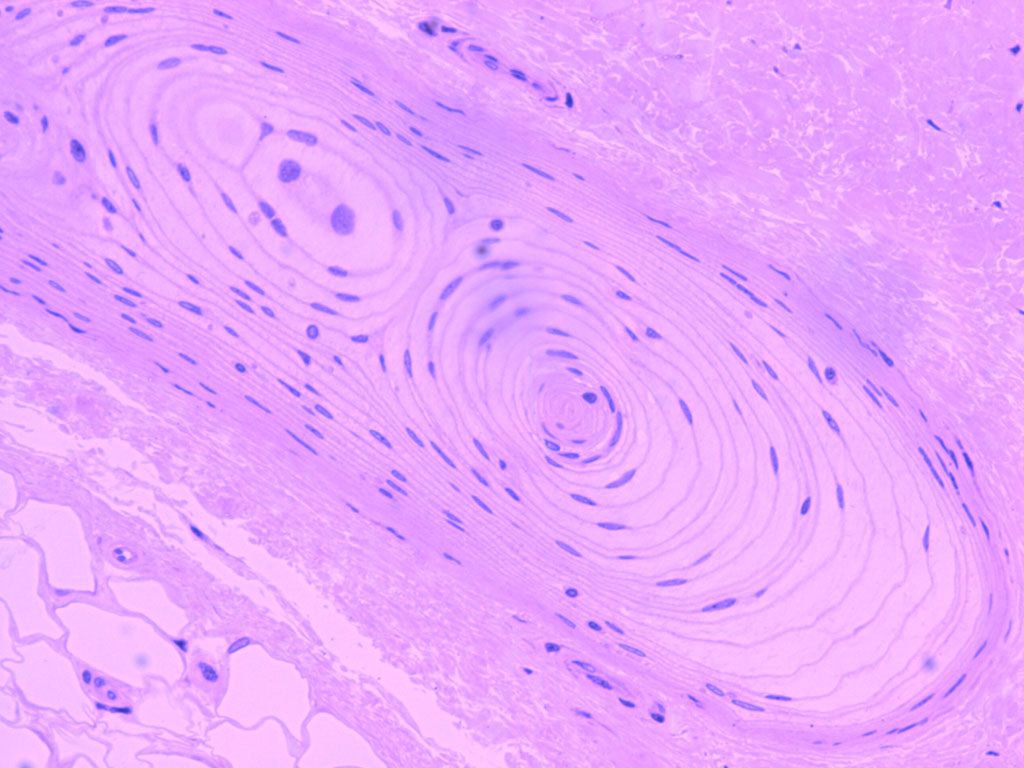
Pacinian Corpuscles:
Stimulus: Deep pressure, high-frequency vibration.
Location: Deep dermis and hypodermis, often found in palms, soles, and external genitalia.
Structure: Large, onion-shaped, and encapsulated with many concentric layers.
Function: Detect deep pressure and vibration.
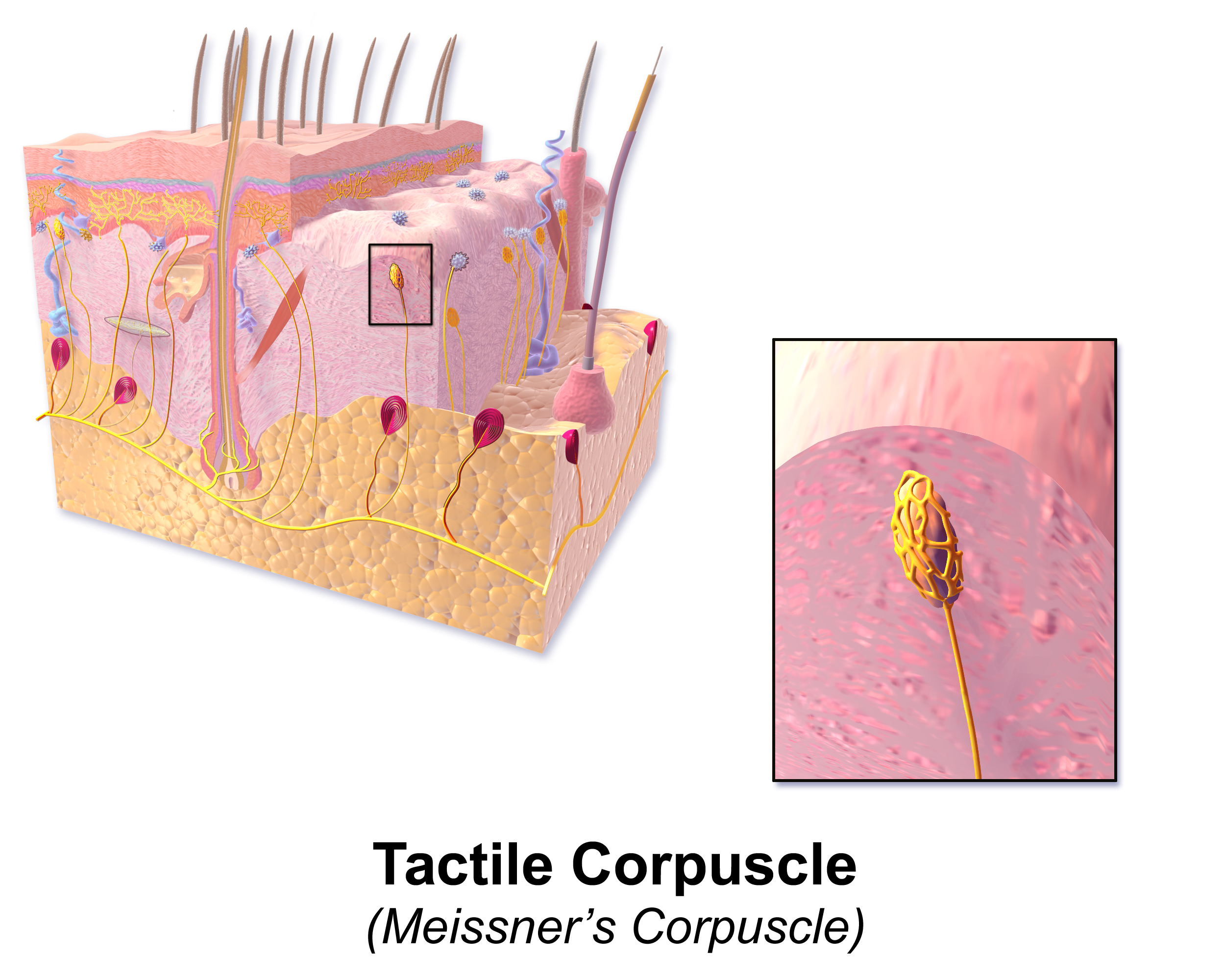
Meissner’s Corpuscles:
Stimulus: Light touch, flutter, and low-frequency vibrations.
Location: Dermal papillae (upper dermis), especially in hairless skin (fingertips, lips, palms).
Structure: Small, oval-shaped, and encapsulated.
Function: Responsible for detecting fine, rapid touch and vibrations (important for grip and texture detection).
Thermoreceptors
specialized sensory neurons that detect changes in temperature. They play a crucial role in maintaining body temperature homeostasis. Thermoreceptors are primarily located in the skin, particularly in the dermis and epidermis. There are two types of thermoreceptors: hot and cold
what type of membrane is the skin
The skin is classified as a cutaneous membrane. This means it is a type of epithelial membrane, specifically referring to the skin as a tissue structure.
what type of tissue is the epidermis made out of
stratified squamous epithelial tissue. This means it is a multilayered epithelium composed of flat, tile-like cells that are stacked on top of each other.
what is the primary cell of the epidermis
The principal cells of the epidermis are keratinocytes.
The basal cells or "stem cells" of the epidermis are undifferentiated, proliferating cells that migrate upwards through all the five layers in a process known as keratinization. It takes about 30 days for the cells to migrate from the basal layer to cross the stratum corneum where they are finally shed.
the water-proofing protein found in the epidermis is
Keratin is a fibrous protein that is the primary component of the epidermis, the outermost layer of skin. It forms a waterproof barrier that protects the skin from moisture loss. Keratin is also found in hair and nails.
Epithelial Tissue
Covers and protects body surfaces (e.g., skin, mucous membranes)
Forms glands (e.g., sweat glands, salivary glands)
Types include squamous, cuboidal, columnar, and transitional.
Connective Tissue
Supports and binds other tissues
Includes bone, cartilage, tendons, ligaments, blood, and adipose tissue
dermis is made up of connective tissue called dense irregular connective tissue.
Muscle Tissue
Contracts to produce movement
Types include skeletal, cardiac, and smooth
Nervous Tissue:
Transmits and receives electrical impulses and Includes neurons and glial cell
tissue definition
a group of similar cells that work together to perform a specific function within an organism, often with an extracellular matrix surrounding them, representing a level of organization between individual cells and a complete organ
essentially, tissues are made up of cells with a shared structure and function that cooperate as a unit
what type of tissue composes the hypodermis
loose connective and adipose tissue (fat cells), with the connective tissue forming a network that holds the fat lobules together; essentially, it's a loose, areolar connective tissue with a high concentration of fat cells.
Acts as a fat storage area, provides insulation, and cushions the body by absorbing shock.
arrector pili muscle contraction
When arrector pili muscles contract, they cause hairs to stand on end, creating the phenomenon known as "goosebumps"
occurs in response to cold temperatures or strong emotions like fear, as these muscles are stimulated by the sympathetic nervous system
essentially, they pull the hair follicle upright, trapping a layer of air against the skin for some insulation.
The main purpose of erect hair in humans is not significant for thermoregulation but is more of a vestigial response.
effects of aging on the epidermis
Thinning: The epidermis becomes thinner, leading to more fragile skin that is prone to tearing and bruising.
Decreased Cell Turnover: Keratinocyte turnover slows, which causes slower wound healing and duller skin appearance.
Reduced Barrier Function: The skin’s ability to retain moisture diminishes, contributing to dryness.
effects of aging on dermis
Loss of Collagen & Elastin: Collagen (providing strength) and elastin (providing elasticity) production decreases, resulting in wrinkles and sagging skin.
Reduced Vascularization: Fewer capillaries in the dermis mean reduced blood flow, which impairs thermoregulation and healing.
effects of aging on hair
Graying: Melanocyte function declines, leading to less melanin production and gray or white hair.
Hair Thinning: Hair follicle density decreases, causing overall hair thinning.
Slower Growth: Hair growth slows with age due to reduced follicular activity.
Hair Loss: Androgenic alopecia (pattern baldness) is common with age, especially in men.
effects of aging on nails
Thickening or Brittle Nails: Nails can become thickened, brittle, and prone to splitting or ridging due to reduced circulation and keratin production.
Slower Growth: Nail growth slows with age, making it harder for nails to recover from damage.
Pigmentation Changes and aging on the skin
Age Spots (Lentigines): Sun exposure and aging cause hyperpigmented spots, especially on areas frequently exposed to the sun.
Hypopigmentation: Some areas may develop depigmented patches due to melanocyte loss.
freckles
A freckle is caused by an overproduction of melanin, the pigment responsible for skin color, within the integumentary system, primarily triggered by exposure to ultraviolet (UV) radiation from sunlight, which stimulates melanocytes to produce more melanin, resulting in visible brown spots on the skin, especially in people with lighter skin tones
it's a localized increase in melanin production due to sun exposure within the skin's pigment cells.
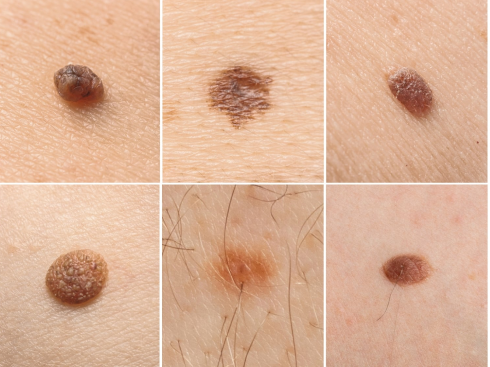
mole/congenital nevi
A mole is caused by a cluster of cells called melanocytes growing together in the skin, which are the cells responsible for producing melanin, the pigment that gives skin its color
this essentially creates a small, localized growth within the integumentary system (skin) where these melanocytes are concentrated instead of being evenly distributed throughout the skin.
They can happen anywhere on the body. Moles can also happen in adulthood, but only moles that are present at birth are considered birthmarks.
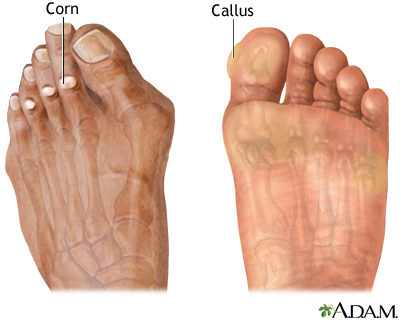
scaly skin
Scales are a visible peeling or flaking of outer skin layers. These layers are called the stratum corneum.

Calluses
calluses form when The skin's outermost layer, the epidermis, becomes more active in response to repeated injury
The epidermis produces more cells, which mature and thicken the skin
The thickened skin protects underlying tissues
often form in the hands and feet
macular stain
common, flat, pink or red birthmarks that typically appear on the face, neck, or scalp. They are also known as "stork bites" or "angel kisses."

Hemangioma
A common vascular birthmark.
Hemangiomas become visible within the first few weeks or months of life and continue to grow rapidly for about 6 to 9 months. Then, they gradually lose this red color and also shrink. They are called strawberry patch hemangiomas.

Cafe-au-lait spots
These are usually oval-shaped and light brown or black. Typically these birthmarks fade with age and are not a problem.
birthmarks
discolored or raised areas of skin that are present at birth or appear shortly after. They are caused by an overgrowth or undergrowth of pigment cells (melanocytes) or blood vessels.
Vascular birthmarks:
These are caused by blood vessels and can appear as red, pink, or purple marks. Examples include hemangiomas (strawberry marks) and stork bites.
Pigmented birthmarks:
These are caused by pigment cells and can appear as brown, black, or tan marks. Examples include moles, freckles, and café-au-lait spots.
Other types:
Some birthmarks do not fit into these categories, such as Mongolian spots (blue-gray marks that usually fade with age) and port-wine stains (flat, red marks that can be permanent).
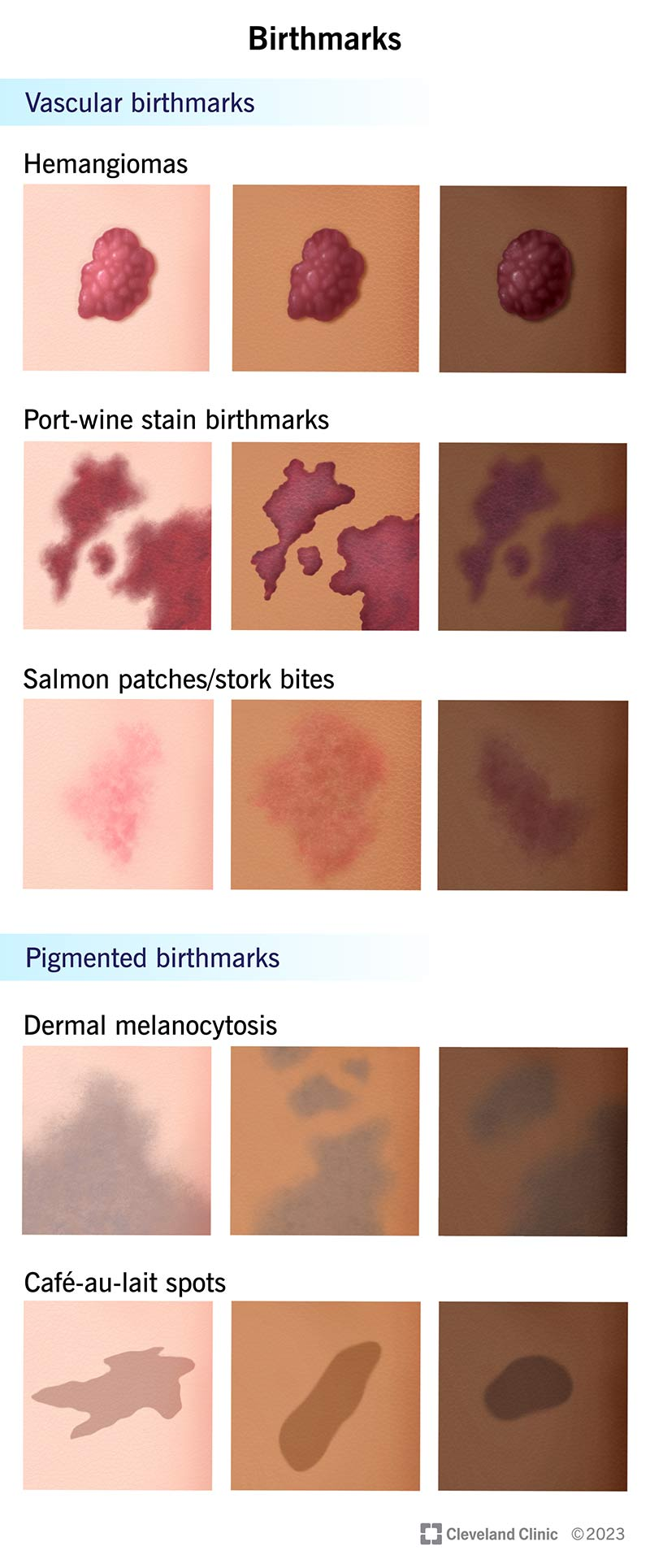
mongolian spots
These are blue or blue-gray spots on the lower back or buttocks. They are most common in babies with darker skin

what are fingerprints
Fingerprints are the pattern of the epidermal ridges on fingers. They consist of friction ridge units that can be characterised by patterns (arrangement of ridges) and minutiae (small specific details such as bifurcations and ridge endings).
how do fingerprints arise
Fingerprints develop during early fetal life. They undergo various phases, of which crucial events occur by the early weeks of the second trimester.
why do fingerprints occur?
Ridge formation is due to mechanical forces and skin growth differences, leading to compression and buckling.
The nervous system plays a role by influencing ridge patterns as they form.
Ridges develop on sensory nervous tissue grids, guided by specialized cells like Merkel cells and Meissner corpuscles.
This process results in both primary and secondary ridge patterns with interconnected formations.
first step of vitamin d synthesis
SKIN
UV-B Radiation Activation
When your skin is exposed to UV-B rays from sunlight, 7-dehydrocholesterol (a cholesterol derivative in the epidermis) absorbs the UV light.
This triggers a chemical reaction, converting 7-dehydrocholesterol into pre-vitamin D3.
Thermal Isomerization
Over a few hours, pre-vitamin D3 is converted into cholecalciferol (vitamin D3).
The skin releases cholecalciferol into the bloodstream.
2nd step of vitamin D synthesis
LIVER
Hydroxylation (First Step of Activation)
calcidiol is created
Calcidiol is the main circulating form of vitamin D and a marker for vitamin D status in the blood.
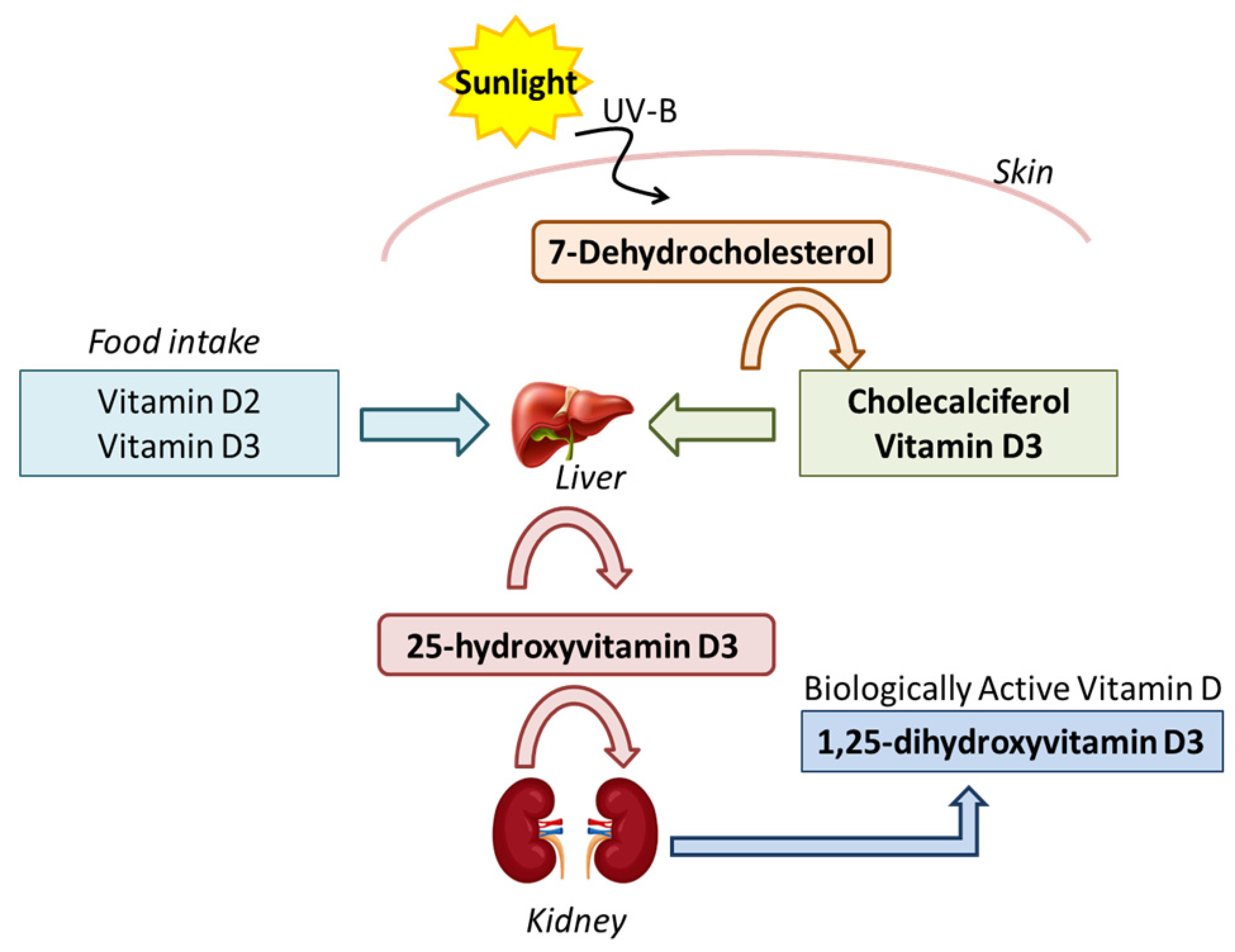
3rd step of vitamin d synthesis
Kidneys
Hydroxylation (Second Step of Activation)
In the kidneys, another enzyme called 1-alpha-hydroxylase adds another hydroxyl group to calcidiol, converting it into 1,25-dihydroxyvitamin D (1,25(OH)2D), also known as calcitriol.
Calcitriol is the active form of vitamin D.
4th step in vitamin D synthesis
Calcitriol travels through the bloodstream to various organs, where it binds to the vitamin D receptor (VDR) in the following tissues:
Intestines:
Calcitriol stimulates calcium and phosphate absorption in the small intestine to help maintain healthy bones.
Bones:
When calcium levels are low, calcitriol promotes the release of calcium from bones to maintain blood calcium levels.
Kidneys:
Calcitriol reduces calcium excretion by increasing calcium reabsorption in the kidneys.
Immune System:
Calcitriol modulates the immune system, promoting antimicrobial activity and reducing excessive inflammation.
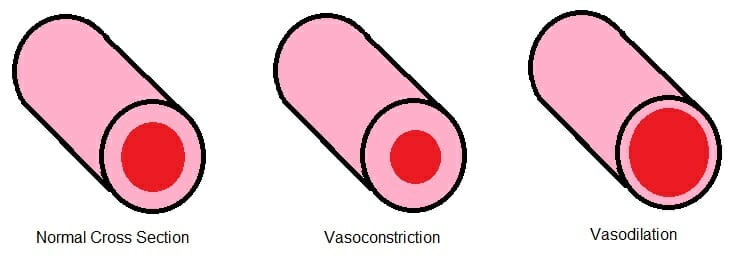
vasoconstriction
Narrowing of blood vessels due to smooth muscle contraction
Increases blood pressureReduces blood flow
Conserves body heat by limiting blood flow to the skin
Occurs in response to cold, stress, or norepinephrine
Vasodilation
Widening of blood vessels due to smooth muscle relaxation
Decreases blood pressure
Increases blood flow
Releases body heat by increasing blood flow to the skin
onychocytes
cells that make up the nail plate. They are keratinized epithelial cells that form in the nail matrix. The keratin in onychocytes gives nails their strength and rigidity.
nail function
protection, sensation, and helping with fine motor skills
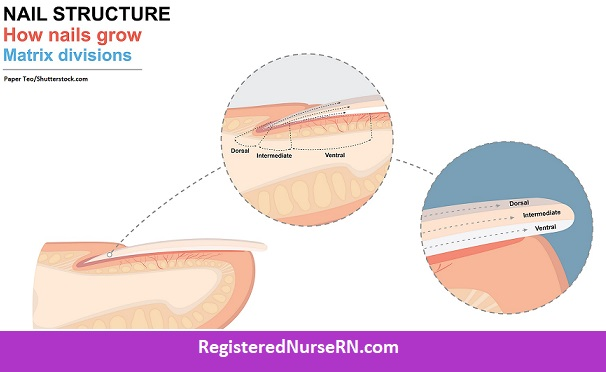
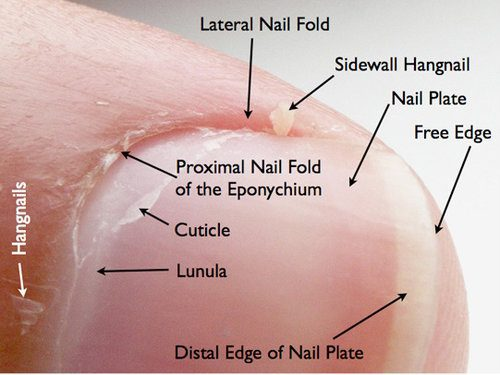
nail plate
The nail plate is composed of layers of keratinized cells. These cells are produced in the nail matrix, located beneath the cuticle, and as they grow, they harden and push toward the fingertip, forming the nail plate.
It is translucent and appears pink due to the underlying blood vessels in the nail bed. The nail plate's free edge extends beyond the fingertip.
The plate itself can be divided into three main layers: a dorsal layer (top), an intermediate layer (middle), and a ventral layer (bottom).
Function: The primary function of the nail plate is to protect the tips of fingers and toes from injury. It also aids in fine motor functions, like picking up small objects, by providing support and stability to the fingertip.
Nails grow at an average rate of about 0.1 mm per day, with the new cells in the nail matrix constantly pushing older cells out toward the fingertip.
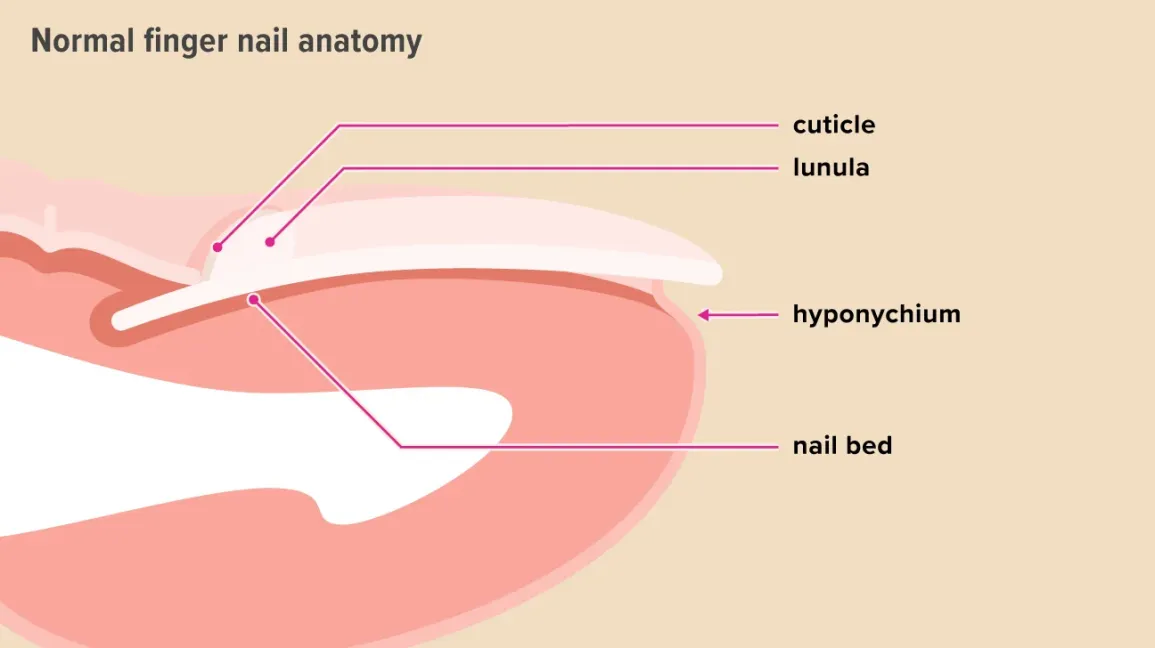
nail bed
the skin beneath the nail plate that provides support and nourishment for the growing nail.
he nail bed consists of layers of skin similar to the epidermis and dermis. It is rich in blood vessels, which give the nail bed a pinkish appearance due to the underlying capillaries.
It extends from the cuticle area at the base of the nail to the free edge of the nail, where the nail plate meets the fingertip.
Function: The nail bed serves as a foundation for the nail plate. It provides nutrients and oxygen to the nail cells from the underlying blood vessels, supporting nail growth. It also helps to anchor the nail plate, preventing it from detaching.
Nervous System: The nail bed is sensitive due to the presence of nerve endings, contributing to tactile sensation in the fingertips.
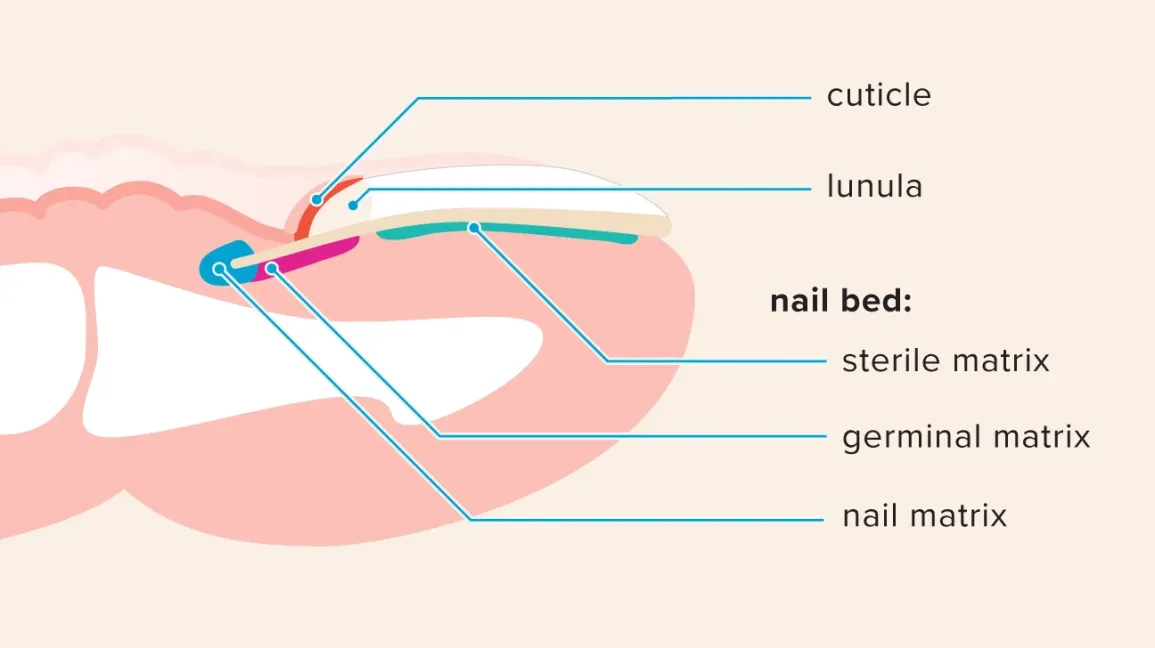
cuticle nail
The cuticle is the thin, dead, transparent tissue produced by the eponychium, and it extends onto the base of the nail plate. Note: You may also see the eponychium referred to as the cuticle of the nail (or even the proximal fold in some texts or illustrations), but these are technically different.
Protection: The cuticle serves as a barrier, preventing bacteria, fungi, and other pathogens from entering the area where the nail grows.
Nail Growth Support: It helps in protecting the newly growing nail as it emerges from the nail matrix (the tissue under the base of the nail that produces new cells). The cuticle also helps anchor the nail to the nail bed.
Prevents Infection: By forming a seal around the nail, the cuticle prevents infections that could affect the nail matrix and hinder nail growth.

lunula
The lunula’s name means “little moon” (think lunula = lunar), and this is actually the distal end of the germinal matrix, which is not translucent like the nail’s body, so it has a different color.

Hyponychium
The hyponychium is the epithelial tissue just under the free edge of the nail and distal to the nail bed.
Remember, the prefix “hypo” means “under”, so it’s under the “little claw.”
The hyponychium is rich in white blood cells and forms a seal between the nail plate and nail bed to defend against germs. The onychodermal band is present where the hyponychium joins the nail bed.
eponychium
The eponychium is the thin layer of tissue on the ventral surface of the proximal fold that covers, seals, and protects the nail’s matrix and root.
The prefix “epo” or “epi” means “over” or “upon”, and again “nychium” refers to nail/claw, so this is over or upon the nail at its root.
The eponychium produces the cuticle.
Nail folds
folds of skin that surround the sides and base of the nail plate.
Purpose: They protect the nail matrix and help anchor the nail plate.
Types:
Proximal nail fold: The skin at the base of the nail, covering the nail root.
Lateral nail folds: The skin on the sides of the nail plate.
Germinal matrix:
found under the skin and originates behind (proximal to) the nail’s root.
The germinal matrix causes most of the nail’s growth by creating new cells that migrate forward. These cells eventually flatten and lose their nuclei in the process.
This germinal matrix can extend all the way to the proximal part of the nail’s body and and is sometimes visible as the lunula.
free edge
The free edge is the distal-most part of the nail that you have to trim with fingernail clippers. It often has a white appearance as it grows out, because this part of the nail is no longer attached to the underlying nail bed, which is what gives the nail body its pinkish color.

Nail Bed (Sterile Matrix)
The nail bed (or sterile matrix) is the area found between the lunula of the nail matrix and the hyponychium, and this tissue allows for the attachment of the nail body (plate).
The dermis and epidermis of the nail bed often form into longitudinal ridges, and sometimes you can see small vertical ridges on the nail plate itself. These ridges can be normal.
However, deeper ridges or horizontal ridges in the nails could indicate an underlying health issue.