Practical 2: Acute inflammation and Sepsis
1/25
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
26 Terms
Acute inflammation
Activation
Recognition of damage
Mast cell release of histamine
Release of fibrinogen
Conversion of fibrinogen to fibrin
Recruitment of neutrophils
Activation of acute inflammation
PAMPS/DAMPS + PRR
Recognition of damage
Triggers mast cell recruitment to tissues
Mast cell release of histamine
Histamine is vasoactive amine triggering vasodilation and increased vascular permeability to release plasma proteins
Release of fibrinogen
Fibrinogen is one of the most important proteins to be released from the blood into tissues.
Conversion of fibrinogen to fibrin
Formation of fibrin through thrombin action forms part of the coagulation cascade.
Fibrin creates a meshwork within the tissues which the WBC are recruited from the vascular system and be used for diapedesis.
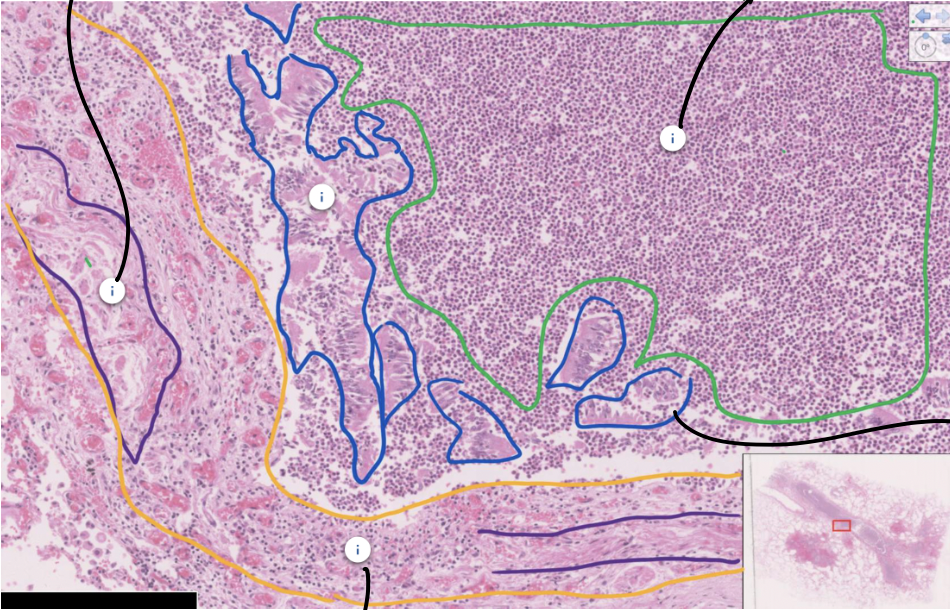
Acute pneumonia
Acute inflammation occurring in the lung with neutrophils accumulating in the bronchi and alveoli as a result of a bacterial infection.
Inflammation spreading from the bronchi and bronchioles (bronchopneumonia) into the surrounding alveolar tissue (lobar pneumonia).
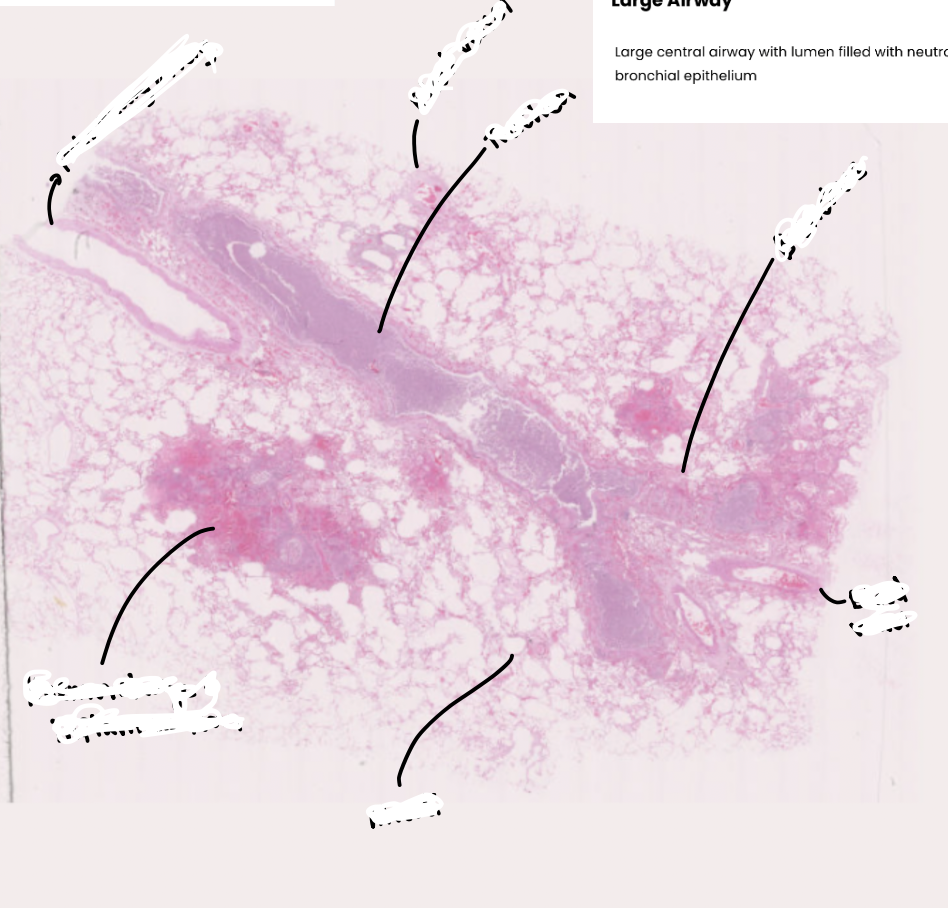
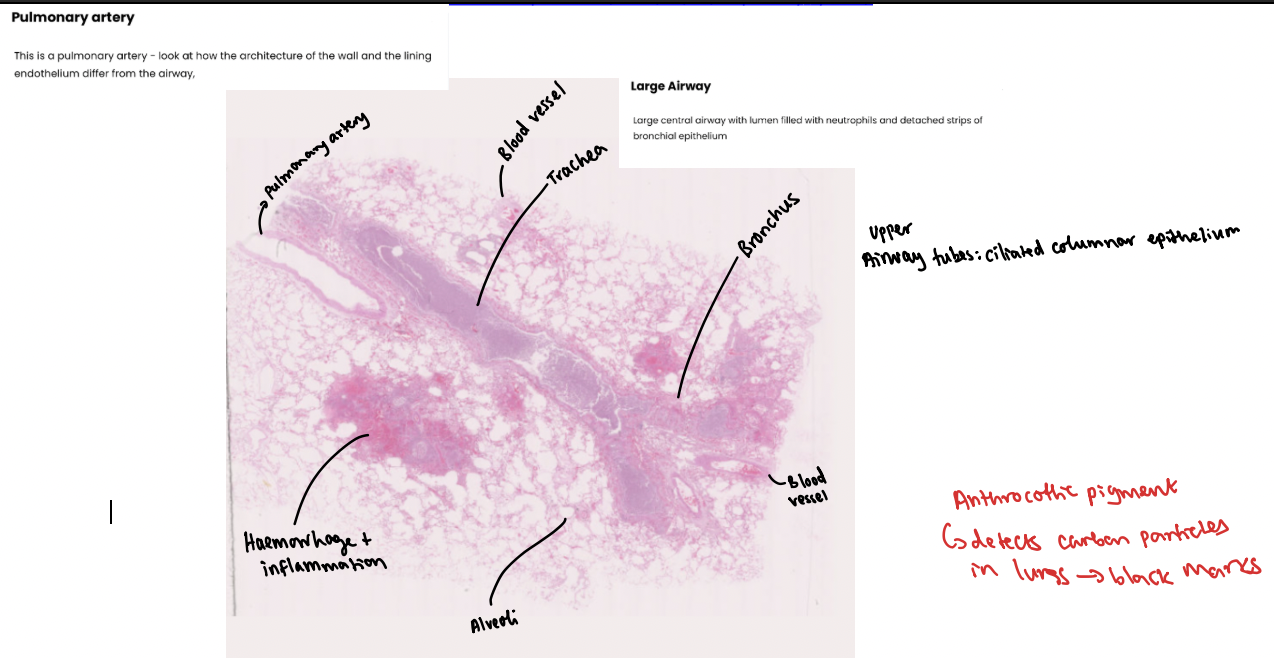
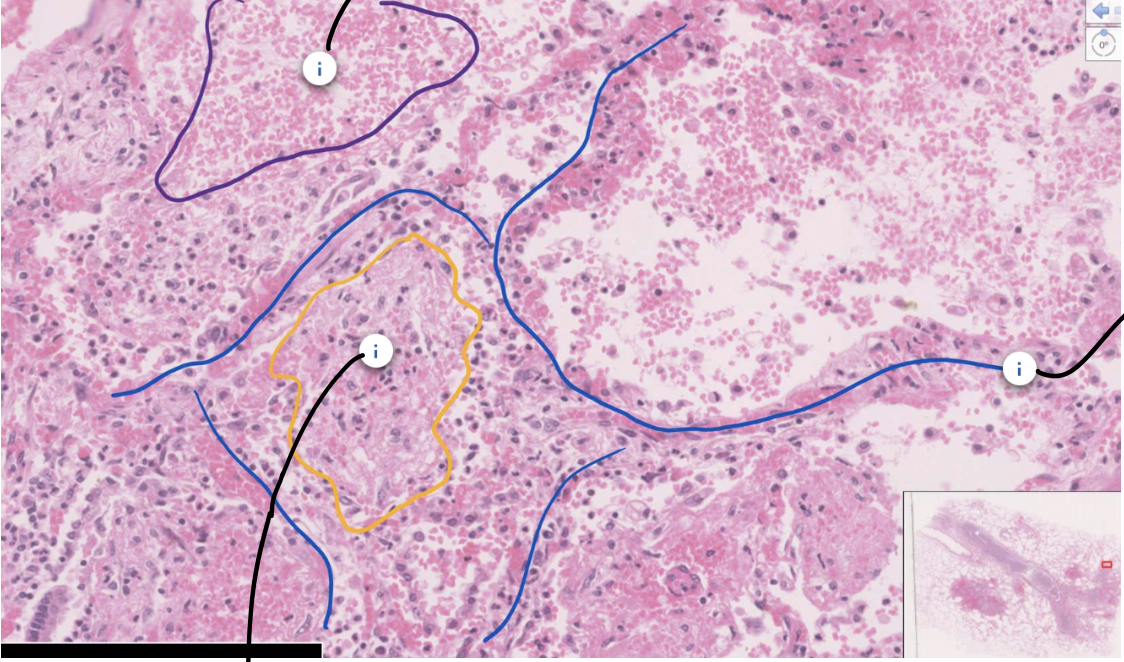
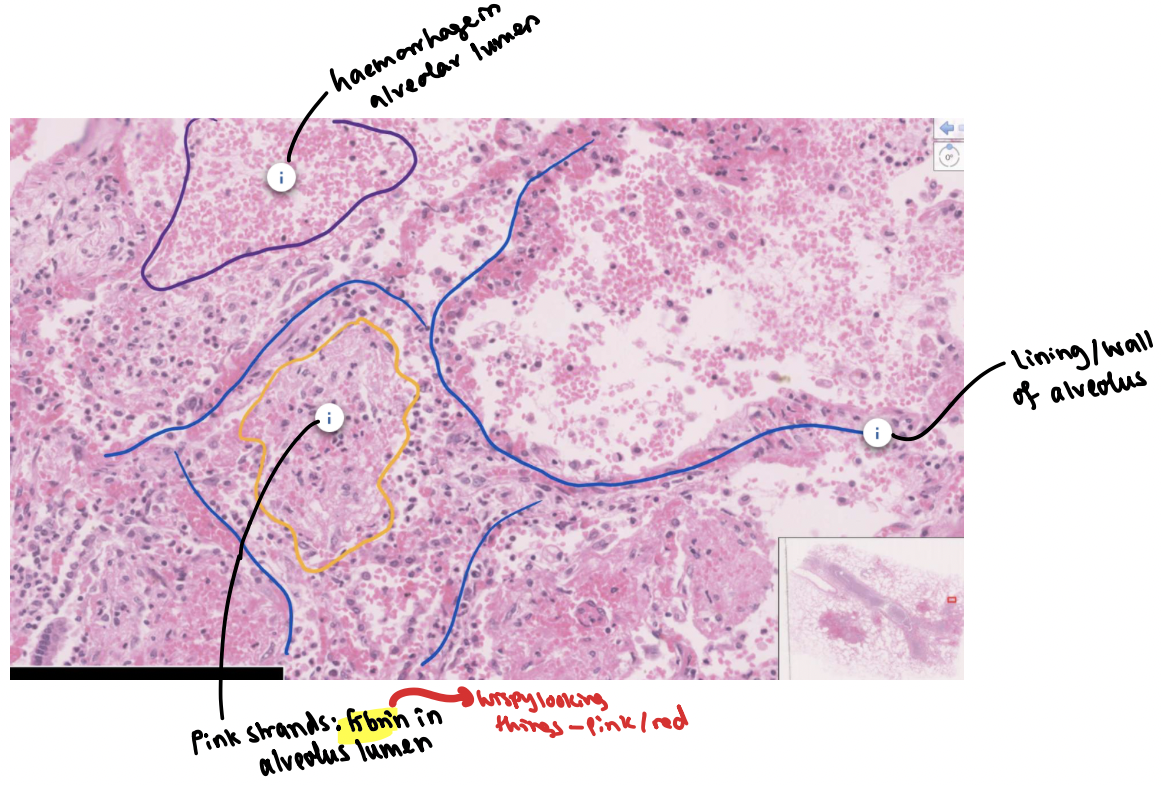
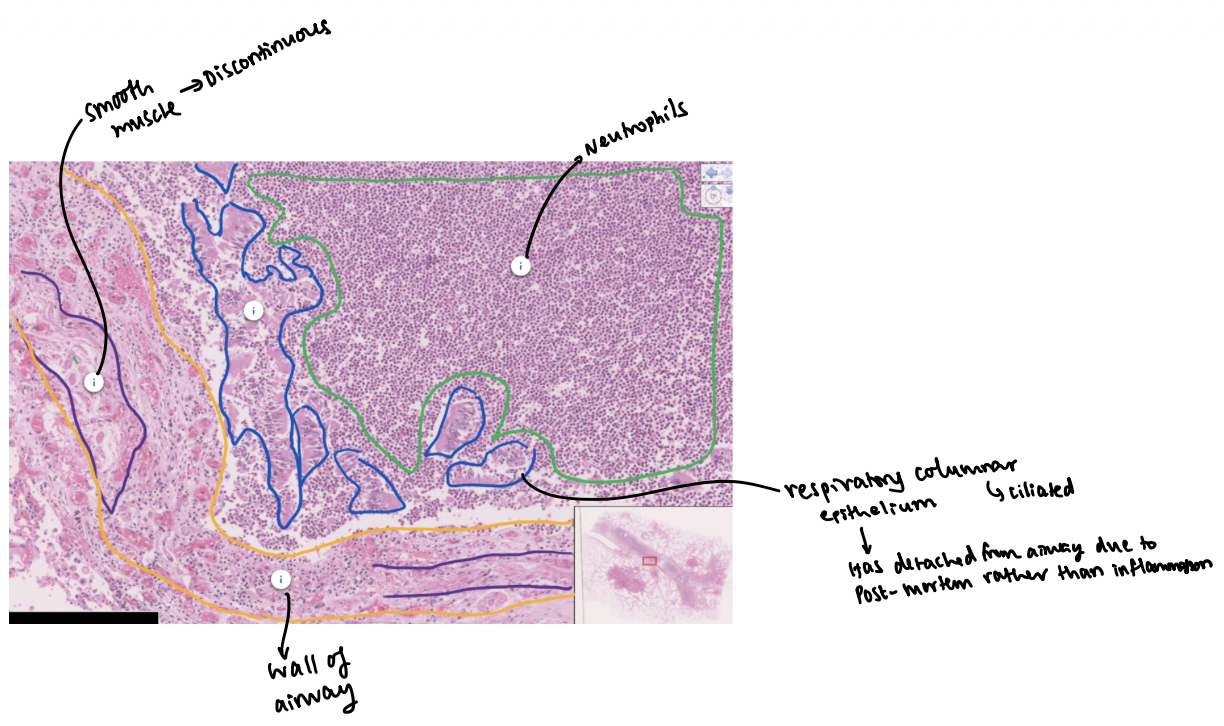
Why might there be haemorrhage in the alveoli around the inflamed areas?
Lung tissue has compliance and inflammation disturbs this and this therefore leads to shearing effect which damages the lining to cause haemorrhage.
Clinical signs of acute pneumonia
-Shortness of breath: dyspnoea
The presence of neutrophils in the bronchi and alveoli reduce the amount of lung available for gas exchange which can reduce the oxygen concentration and lead to a feeling of breathlessness.
-Cough with green sputum
The presence of neutrophils within the bronchi and alveoli leads to irritation which causes cough. The green colour to the sputum is from the neutrophil granules.
-Increased respiratory rate (tachypnoea)
A reduction in the oxygen levels leads to an increase in the rate of breathing to improve oxygenation.
Infiltrate
can be used to describe a collection of white blood cells in tissue e.g. a neutrophil-rich infiltrate.
Exudate
refers to fluid that has left blood vessels and entered tissues during inflammation. Strictly the fluid needs to have a high level of protein - fluid leaving the vasculature without protein is termed a transudate.
When neutrophils are present in the fluid, it can be referred to as a neutrophil-rich exudate.
air bronchograms
Increased white shadowing which (with careful inspection) contains slightly darker channels.
Reflect air in the airways in tissue which has lost most of the air within it due to fluid containing neutrophils.
What is the total lymphocyte count at the start of a viral infection?
Less than healthy range due to cytokine effects drawing lymph into tissues.
What happens to CRP in bacterial infections?
Raised CRP in bacterial rather than viral infections due to the use of complement against bacterial.
Cytokine released in fever
IL-I beta
TNF-alpha
IL-6
IFN-gamma
These trigger the hypothalamus to reset the body thermostat to 1-4 degrees higher.
What is the effect of septic shock on BP,HR and RR?
BP decrease
HR increase
RR increase
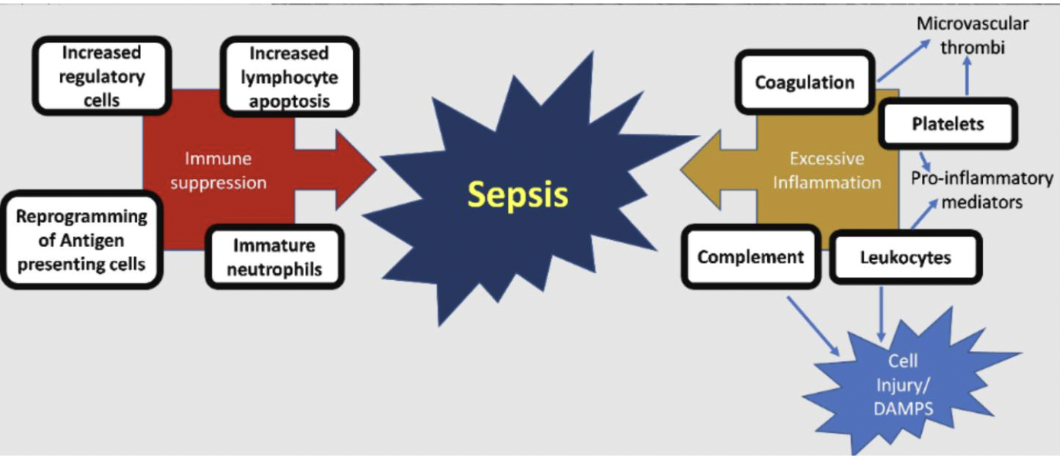
Sepsis
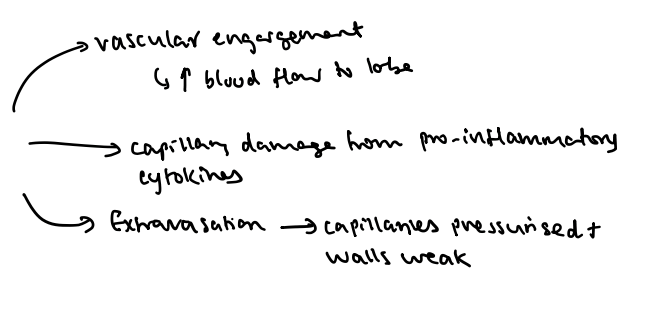
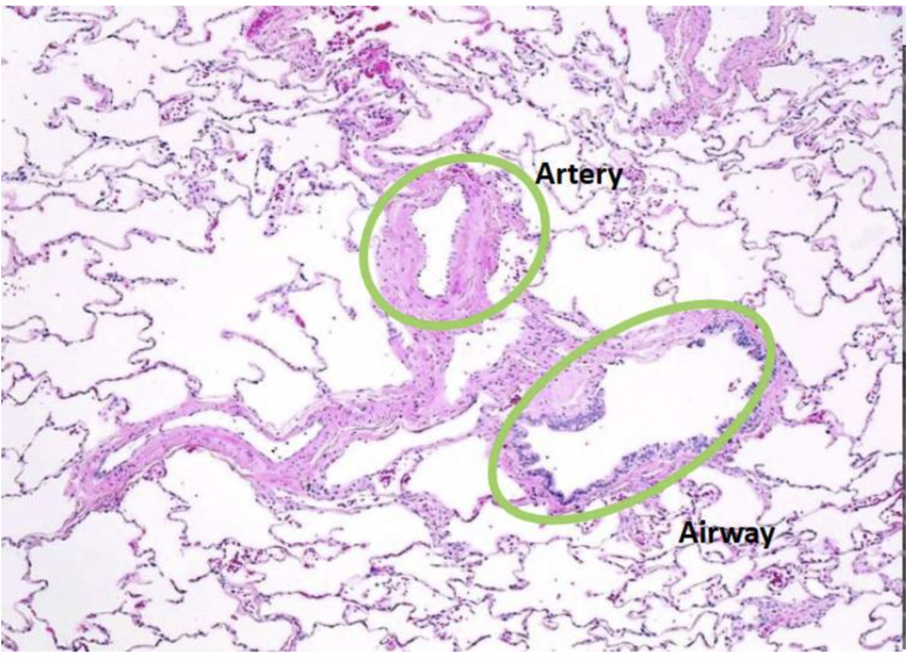
Differences between artery and airway histology
Airways have more visible epithelial lining than artery endothelium
Surrounding smooth muscle tissue is thicker relative to lumen than airway
What scale calculates how alert a patient is
ACVPU
A - Alert
C - Confused
V - Voice (only responds to voice)
P - Pain (only responds to pain)
U - Unconscious
Why is it NOT a good idea (infact a REALLY REALLY BAD idea) to suddenly try and give such patients a very large amount of oxygen (even if their sats are lower)?
CO2 Narcosis
They will initially look pinker and "better," but they will soon become:
Somnolent (very sleepy)
Confused
Comatose
VQ mismatch
What is CO2 narcosis?
Brain central chemoreceptors monitor CO2 levels so when these rise we breathe more.
In COPD, CO2 is always high so brain will ignore this high level and become densesitised rendering central receptors futile so the peripheral chemoreceptors become main regulators.
Peripheral chemoreceptors monitor oxygen levels (hypoxic drive).
Therefore if we flood the system with oxygen the peripheral chemoreceptors will assume there is plenty oxygen so will stop sending signals to the brain to breathe so RR drops and this stops blowing off CO2 and blood becomes toxic
What happens to V/Q in COPD when oxygen is given?
Hypoxic Pulmonary Vasoconstriction: In a COPD lung, some parts are "dead" or broken. The body is smart: it constricts the blood vessels in those broken areas to divert blood to the "good" parts of the lung where oxygen is available.
Reversing the Protection: When you give 100% O2, those constricted vessels in the "dead" parts of the lung suddenly relax (vasodilate) because they sense oxygen.
The Disaster: Blood starts flowing back into the broken, non-ventilated parts of the lung. This blood picks up zero oxygen and fails to drop off any CO2. This is called "increasing dead-space ventilation," and it causes CO2 levels in the blood to skyrocket.
COPD scale
Scale 1 is standard, Scale 2 is used for patients who have hypercapnic respiratory failure (respiratory failure with chronically elevated CO2 levels typically due to Chronic Obstructive Pulmonary Disease which is caused in turn most commonly by smoking).
You would tend to keep a hypercapnic patient with O2 sats of 88-92% routinely.