How to use glucocorticoids
1/29
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
30 Terms
What role has cortisol evolved to have in mammals?
defence against stress
levels become very high to protect against starvation and disease (things that make us unwell)
What factors cause variation in how much cortisol an individual makes?
age, sex, breed, activity
external temperature, exercise
subclinical disease
How much more potent is prednisolone than cortisol?
5x more potent
What are the effects of cortisol?
metabolism
water and electrolyte homeostasis
immunity and inflammation
What are the effects on blood glucose metabolism?
increased gluconeogenesis
inhibit glycogen synthesis
decrease peripheral blood glucose utilization
point is to preserve glucose for your brain
What specific metabolisms does it effect?
fat metabolism- lipolysis, inhibits leptin secretion
protein metabolism- proteolysis
calcium metabolism- mobilizes calcium from bone, increases calcium excretion
bone, muscle, and CNS metabolism
What is the effect of glucocorticoids on electrolytes?
increase sodium re-absorption
increase potassium secretion
type 2 receptor (GR) effects
want to increase water retention
What is the effect on water?
if you said increase water retention, you’re a stupid head!!! I know the last card said increase water retention but forget that!
it actually increases GFR so increases flushing out of abnormalities to protect from disease
increased ANF (atrial natriuretic factor) receptors
What immunity and inflammation cells do they effect?
white blood cells- affect distribution and function, lymphocyte apoptosis
cytokines- suppression, NFkappaB
Should you vaccinate while on steroids?
YES!
they need it more now because they are immunocompromised
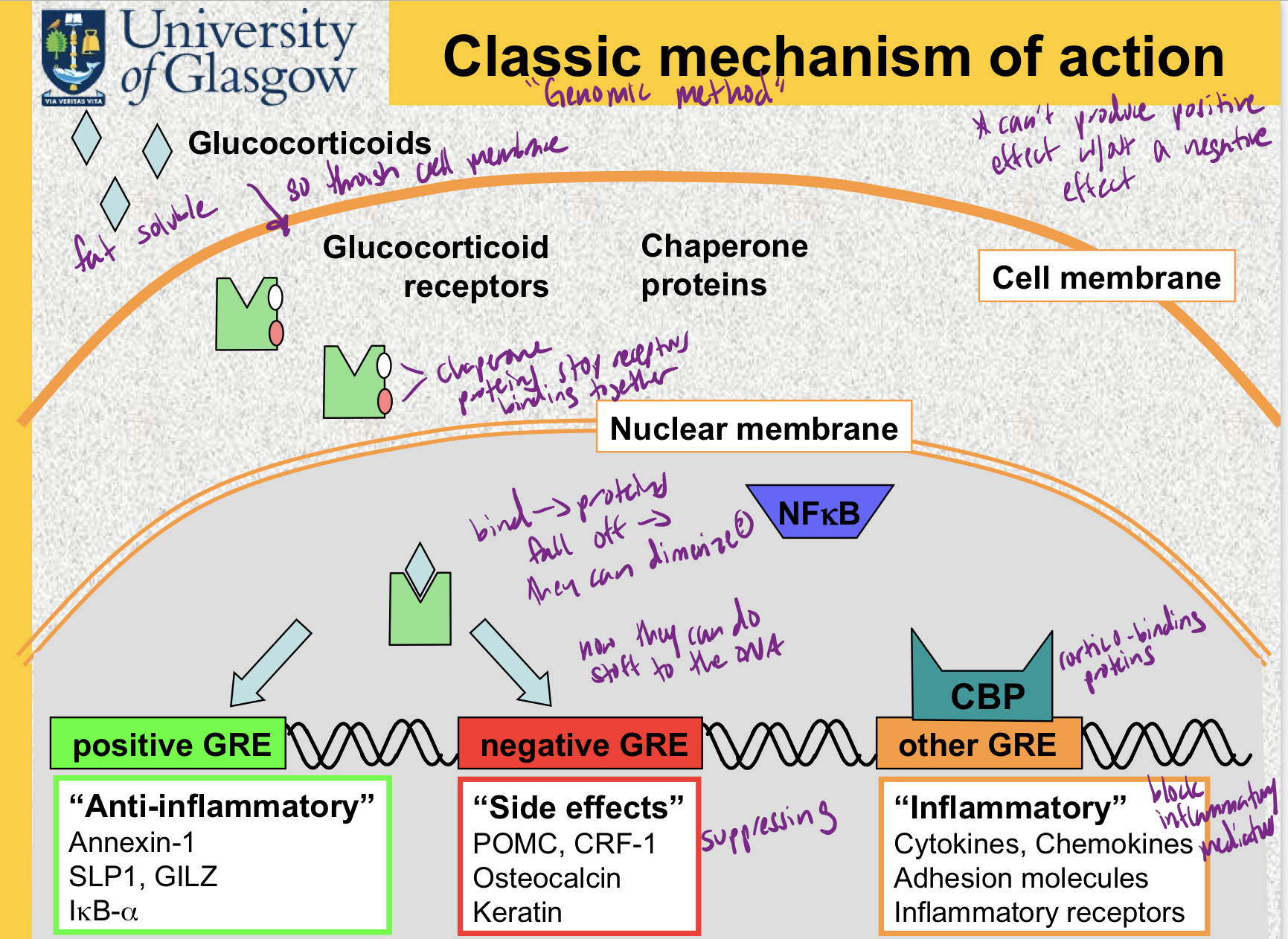
What are the steps in the genomic mechanism of action?
What is different about the non-genomic mechanisms of action?
cytoplasmic receptors- direct changes in metabolism
membrane receptors
direct interactions with cell membranes
it’s very fast
Which mechanism of action explains why the changes can be permanent?
chromosomal
deacetylation of histone
but this is slow
What determines the duration of action?
which esters, carriers, and prodrugs are added
Which steroid can’t cats have?
they can’t convert prednisone to prednisolone
Plasma levels of prednisolone is a waste of time, so what is a more effective way to measure the anti-inflammatory effect?
you can measure how much HPA suppression which is relative to the anti-inflammatory affect
For prednisolone, what diseases should you use a reduced dose?
if the patient has hypoalbuminemia
liver problems
maybe consider if you should be using it all
You should have a plan! What elements should be included?
starting dose
length of initial course (2 weeks is good starting point)
recheck points
method (parameters) on monitoring
likely dose reductions
What is important to tell clients before starting steroids?
why you are using it (disease and why it will work)
expected improvements
side effects (if the drug is working, they will have them)
time course
need for rechecks
What is the starting course for maintenance (ie for Addison’s)?
prednisolone 0.08 mg/kg/day
What is the starting course for an anti-inflammatory disease ie atopic dermatitis?
0.5-1.0 mg/kg q 24 h PO
What is a starting course for an immunosuppressive disease ie IMHA?
2 mg/kg q24h PO
cats double?
What is a starting course for anti-neosplastic ie cutaneous lymphoma?
20-40mg/m² q24 PO
What is a starting dose for anti-insulin ie insulinoma?
0.5-1.0 mg/kg q24h PO
What is the risk when doing a longer course of steroids?
can become dependent after 4 weeks
HPA is suppressed → dependent on steroids, if you take away → addison’s
also adrenals will atrophy after 6 months on steroids
If at first you don’t succeed, try, try again, right?
NO! stope, think, try something new
if it does not work in 5 days, change the drug, change the dose, try something else
When should you reduce doses?
for some diseases you can do direct observations ie measure platelets for IMTP (immune mediated thrombocytopenia)
for others you have to use surrogate markers ie measure CRP (c-reactive protein) for inflammation for SRMA (steroid- responsive meningitis-arteritis)
very hard for pemphigus
bottom line is adjust according to objective parameters such as PCV, platelet counts and acute phase proteins but if you can’t then you should adopt the ALARA principle (as low as reasonably achievable)
What should you do if you need to stop suddenly ie you need to take the patient to sx?
put on prednisolone 0.1 mg/kg a24h PO
There are some slides that talk about ADST, aka alternate day steroid treatment. He talked about some doses, I don’t know if we need to know it. Technically he said this whole lecture would be difficult to test on so could be a waste of time
I think his point was there isn’t proof that it’s effective? And that it’s not ‘safer’ to the adrenals
Alright, what are the golden rules of steroid therapy?
use enough, but no more, to control clinical signs
if not working soon, try something else
once signs controlled, start tapering doses
only switch to ADST when signs controlled
use other treatments to help reduce doses
monitor the animal individually
do not use as ‘preventative’ or ‘speculative’ treatment
do no use in ‘shock’, IVD prolapse, etc