7.3 - The Kidneys
1/31
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
32 Terms
The Urinary System
The system is composed of the kidneys, ureters, bladder and urethra that is responsible for the excretion of wastes.
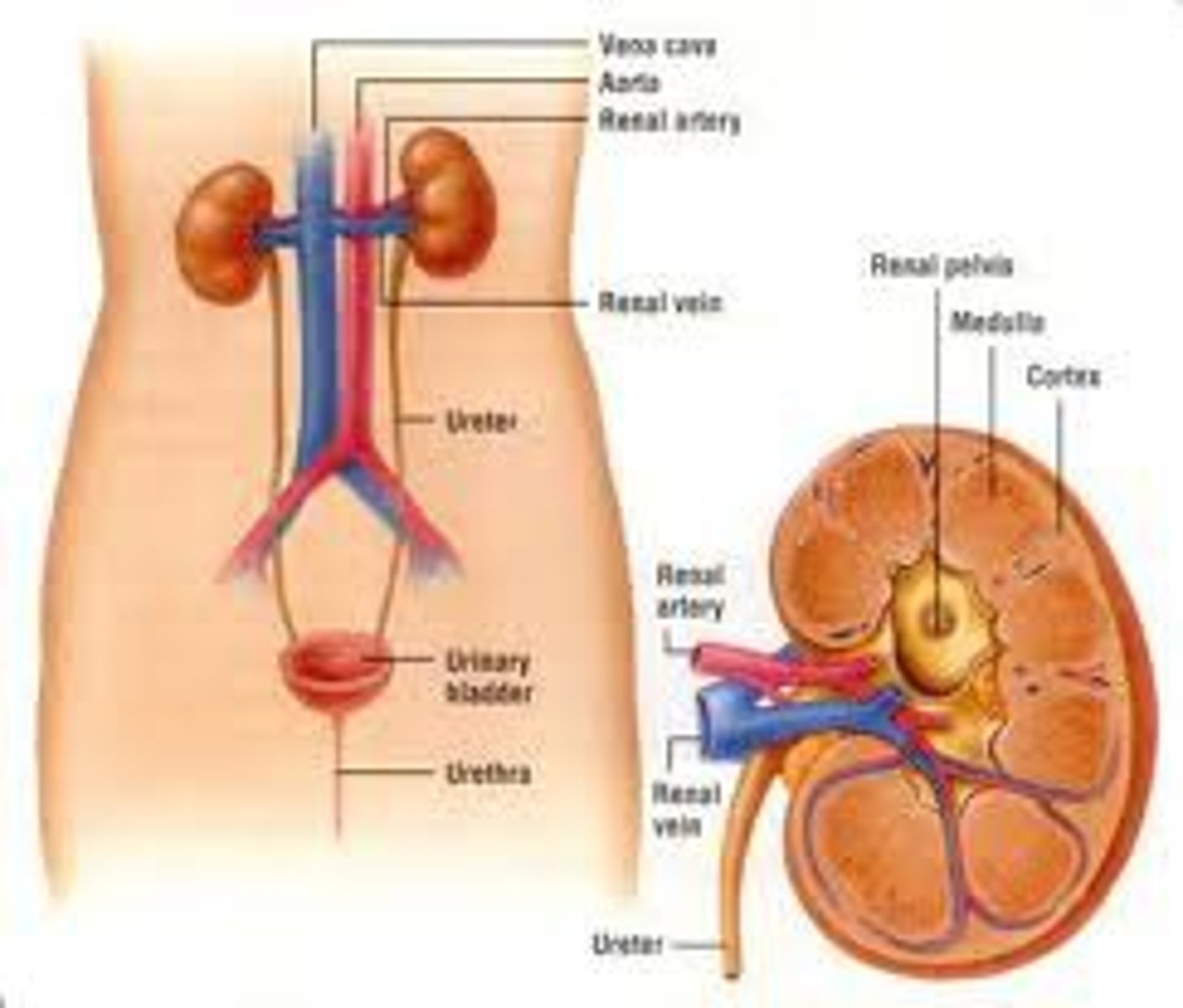
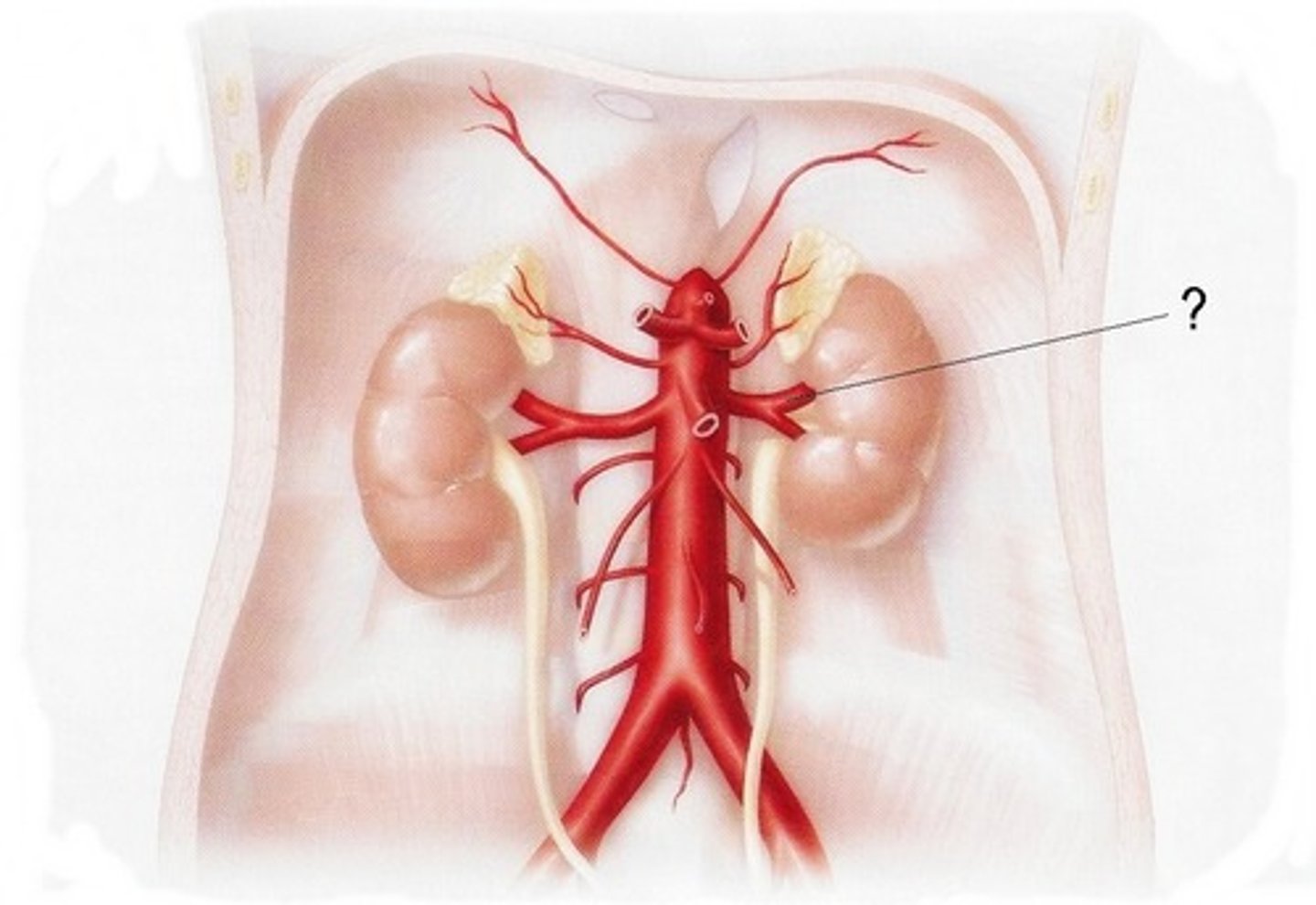
The Kidneys
- reddish brown, bean shaped structure that is formed by millions of nephrons and collecting ducts.
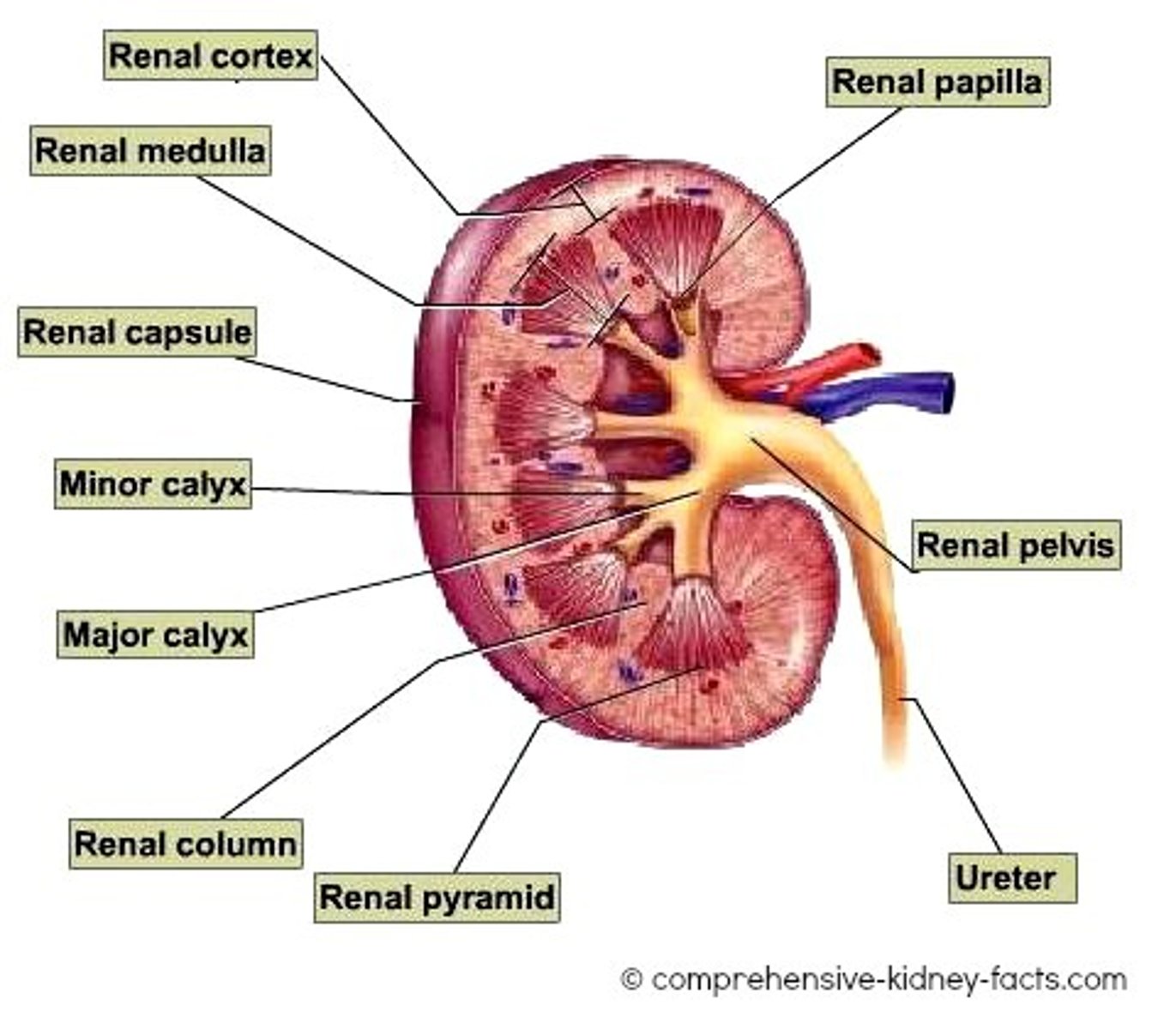
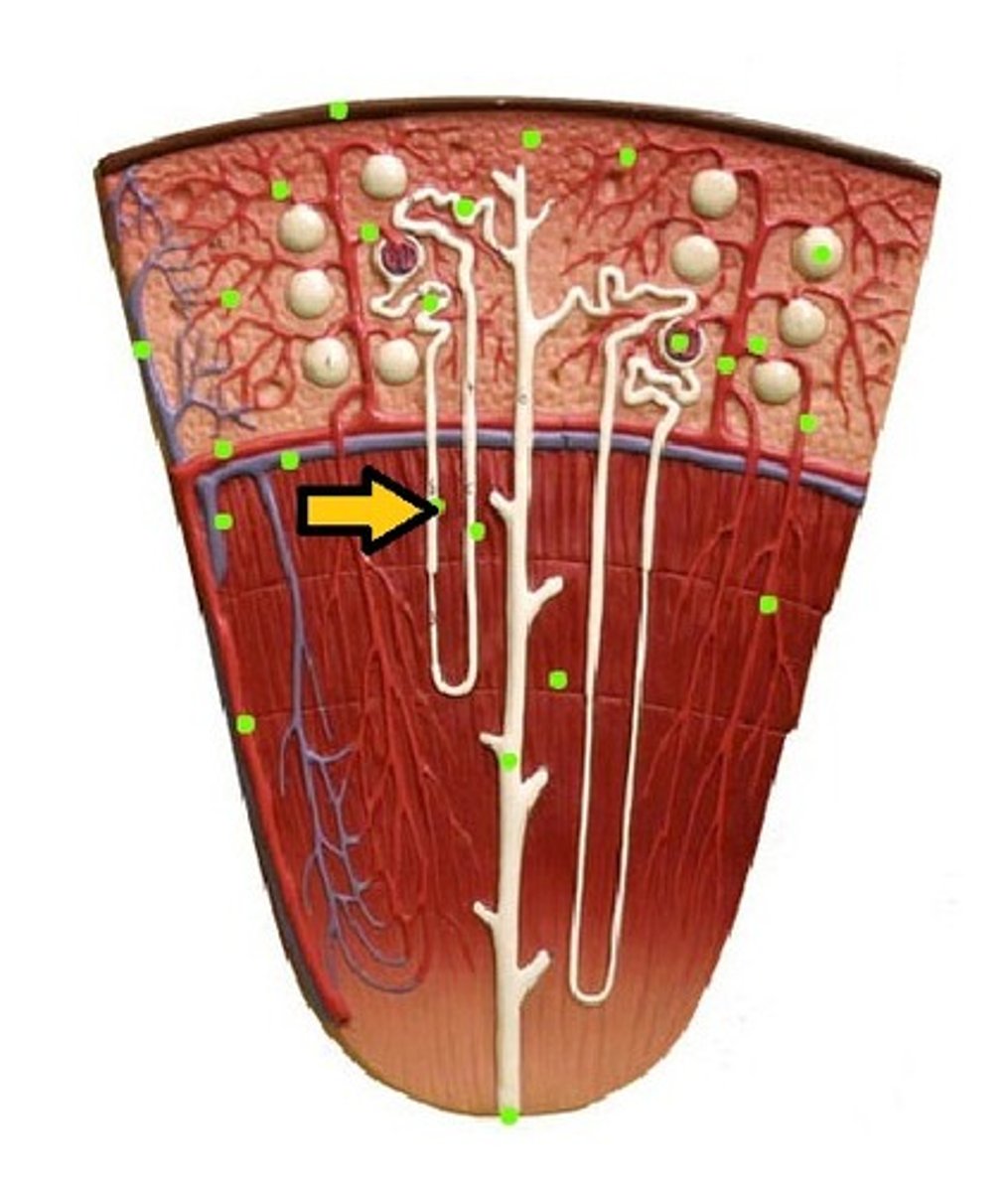
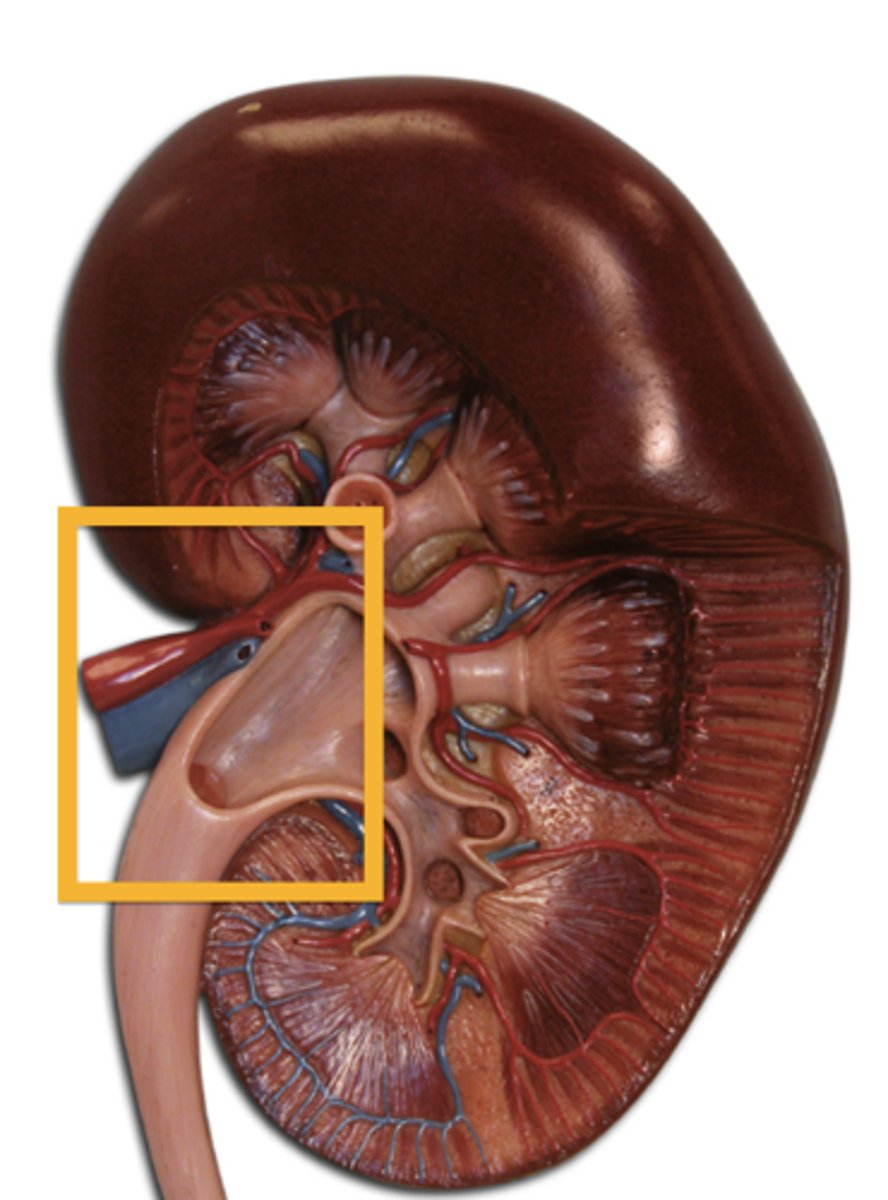
Structure of the Kidney
Renal capsule: Surrounds the kidney
Renal Cortex: Outer part of the kidney contains the top half of the nephron
Renal Medulla: The Inner part of the kidney, which consists of the bottom half of the nephron.
Renal Pyramid: Cone-shaped structures within the medulla
Renal columns: It separates the renal pyramids and is where blood vessels lie.
Renal pelvis: It funnels urine into the ureter.
Renal Hilum: Where vessels enter and leave the kidney.
Ureter: Carries urine to the bladder
Bladder: An organ in the pelvis that stores urine.
Urethra: A muscular tube that connects the bladder to the outside of the body, serving as the pathway for urine to exit the urinary system.
Nephron
- A microscopic functional unit of the kidney
- The role of the nephron is to: Form urine, remove waste from blood and regulate blood composition.
- Around 1.2 million in each kidney -> Increasing the SA for each process.
- Each has a complex network of blood capillaries -> Increasing efficiency of processes

Nephron Structures
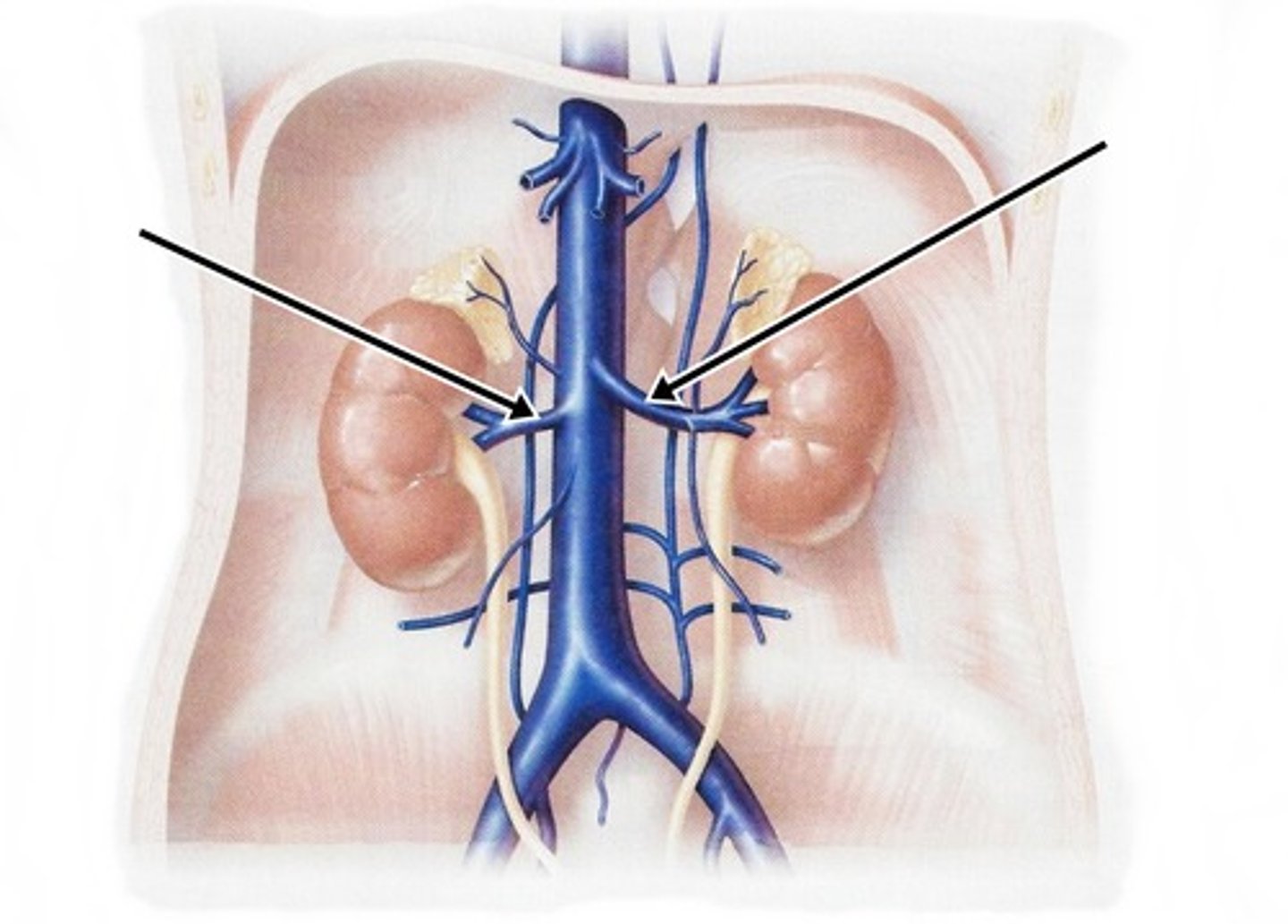
- Renal Artery and Renal Vein
- Afferent Arteriole and Efferent Arteriole
- Peritubular Capillaries
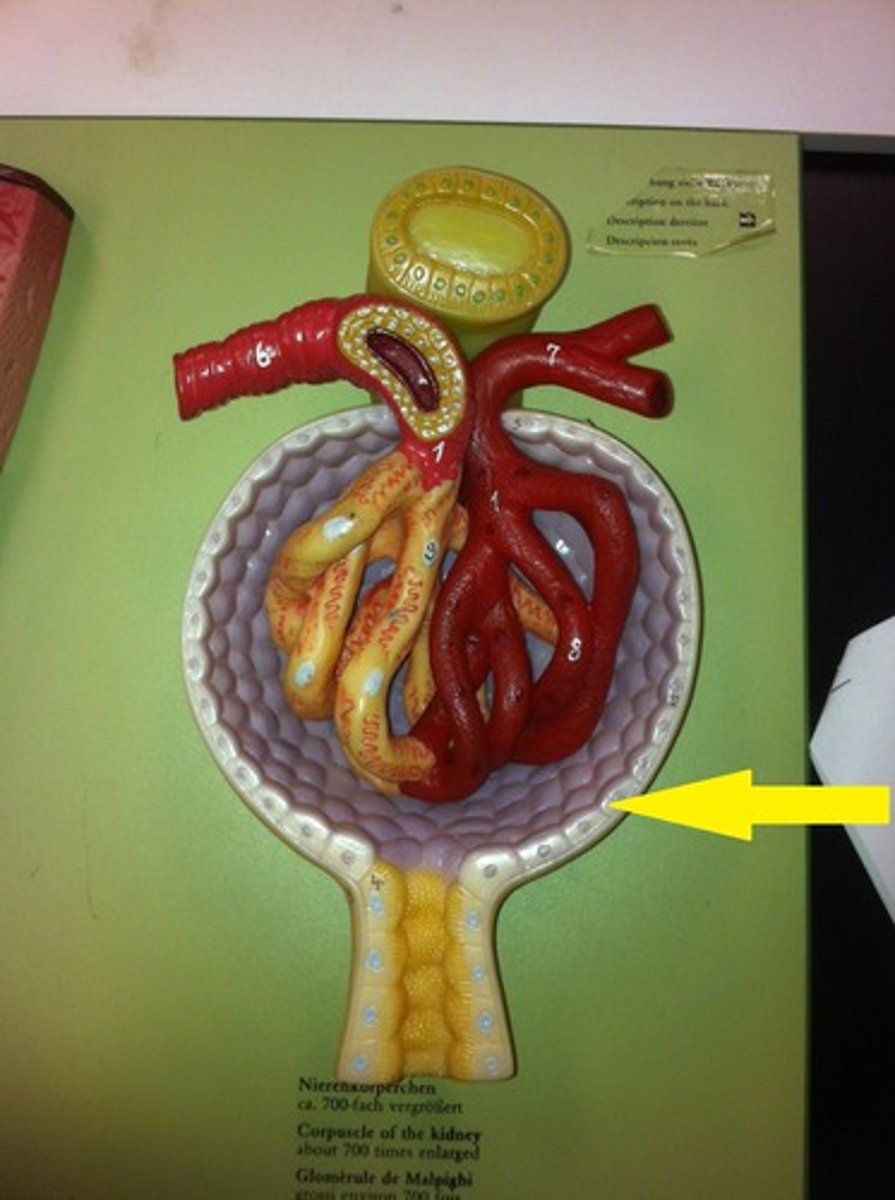
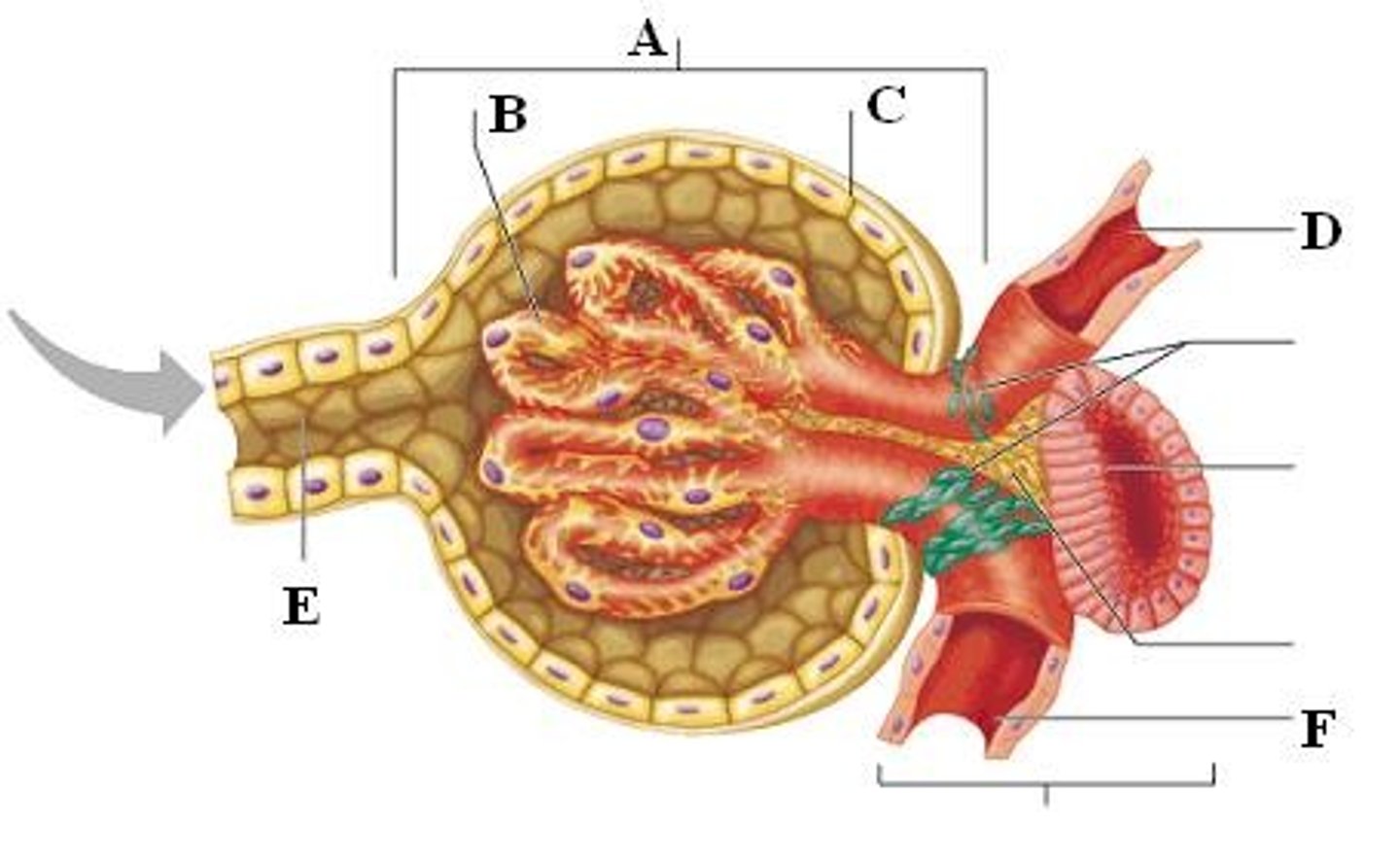
- Renal Corpuscle (Glomerulus and Glomerular Capsule)
- Proximal convoluted tubule
- Descending Limb, Loop of Henle, and Ascending Limb
- Distal convoluted tubule -> Collecting Duct -> Renal Pelvis
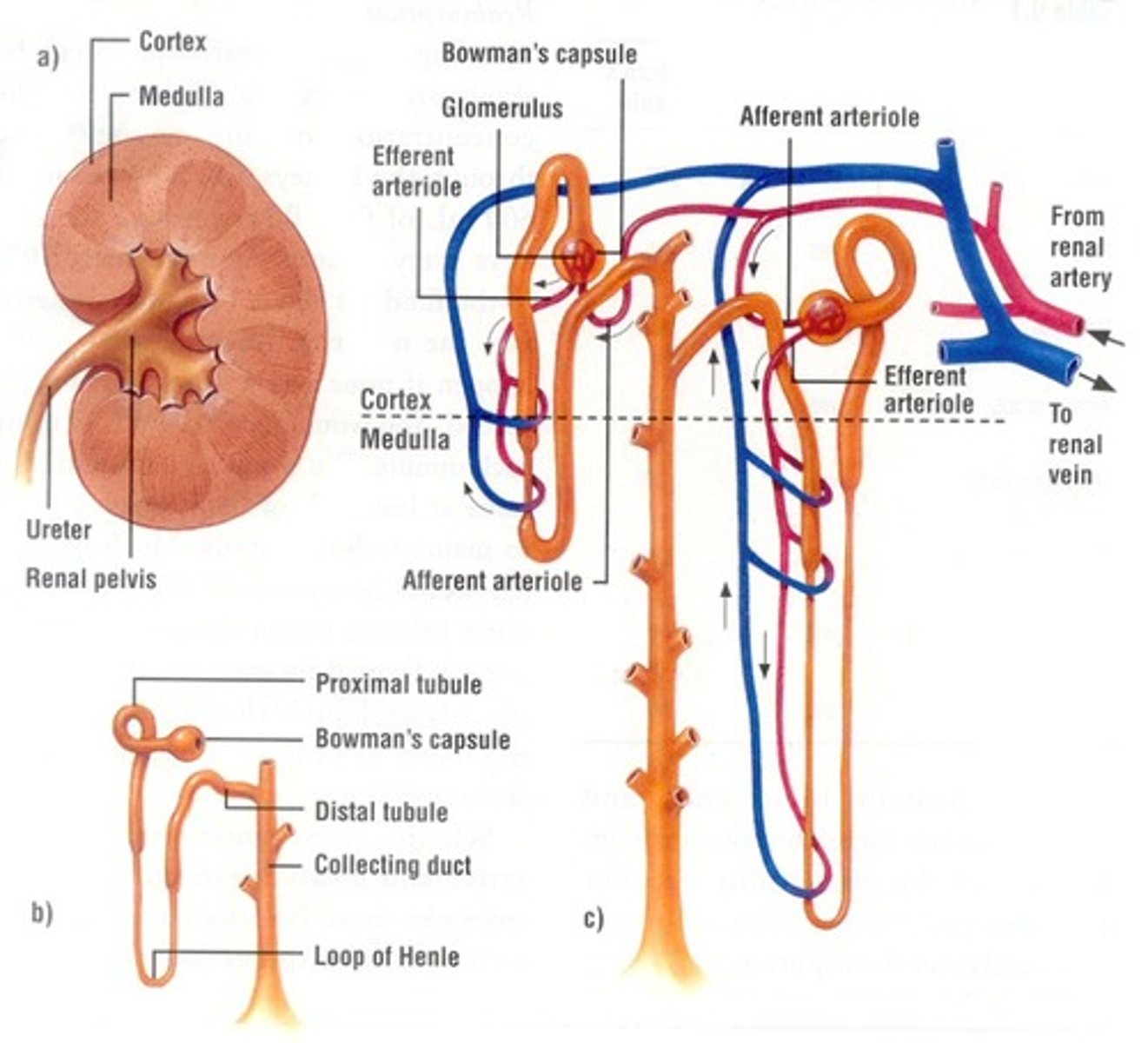
The Structures of the Nephron - Renal Artery
- Carries blood to the kidneys
- Carries 1/4 of the blood from the heart, 1/8 to each kidney
- Efficient filtration -> 1.2L/ minute
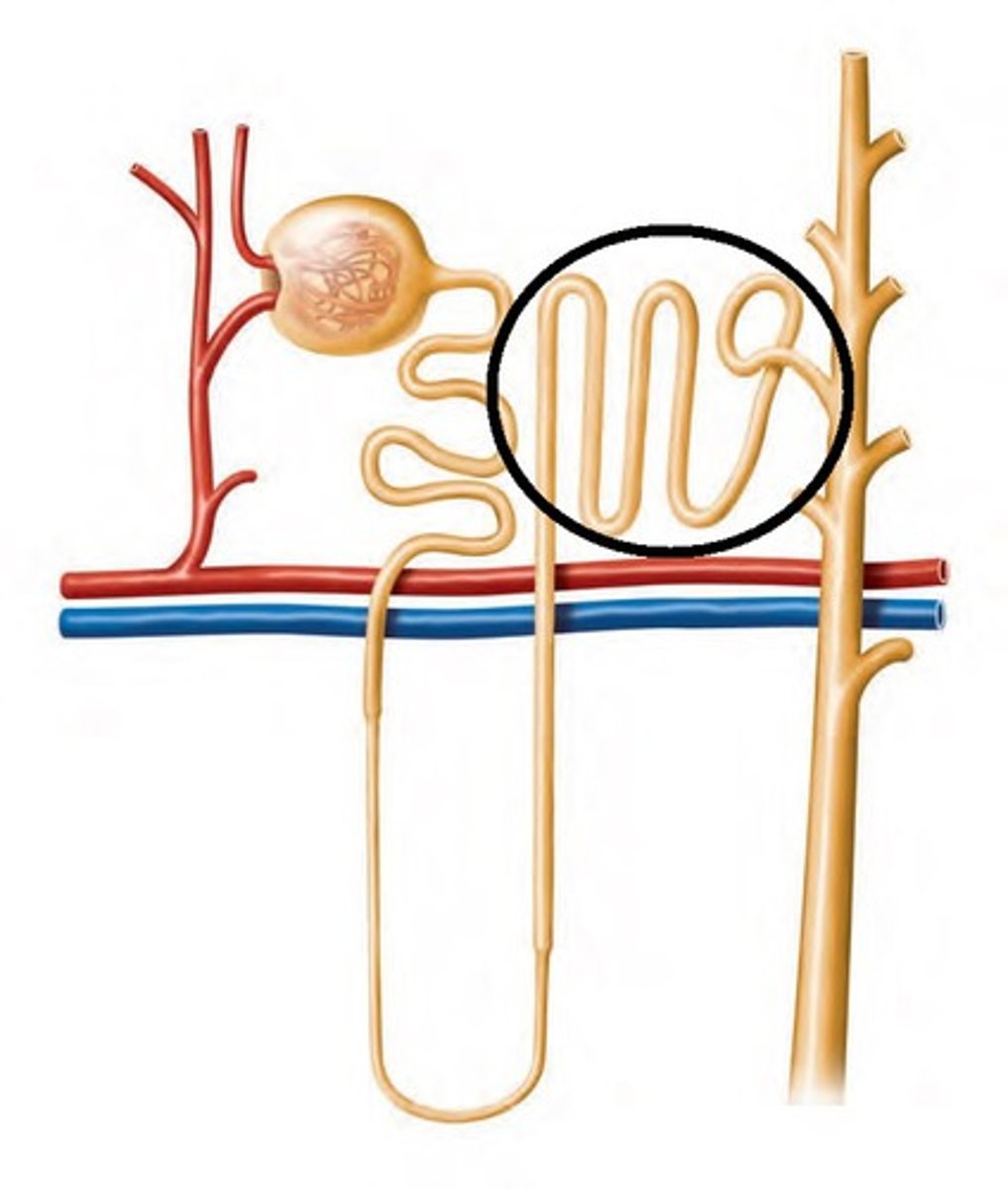
The Structures of the Nephron - Afferent arteriole
- Carries blood from the renal artery to the glomerulus
- Has a wider diameter so more blood can be delivered.
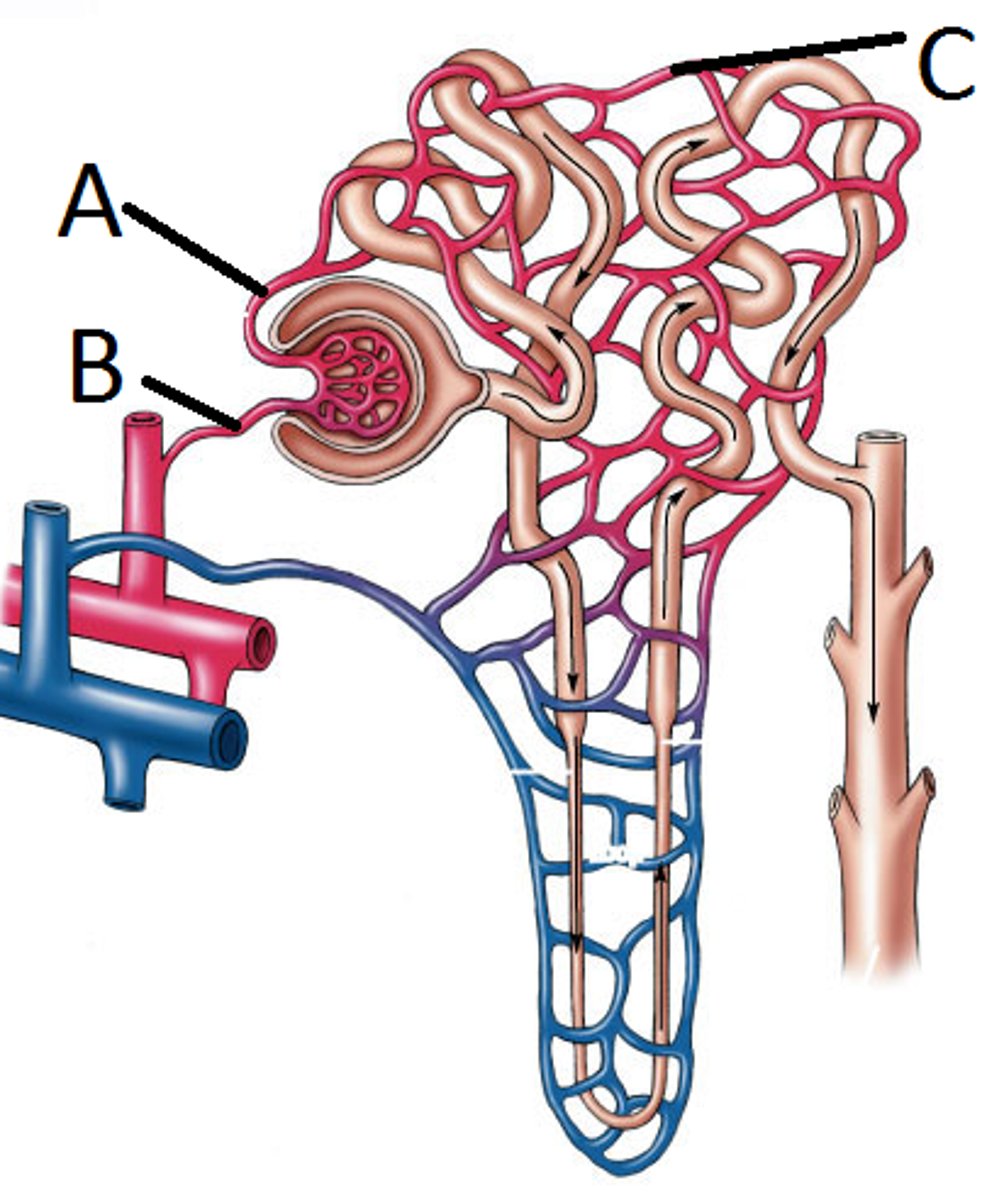
!(B) IN THE DIAGRAM!
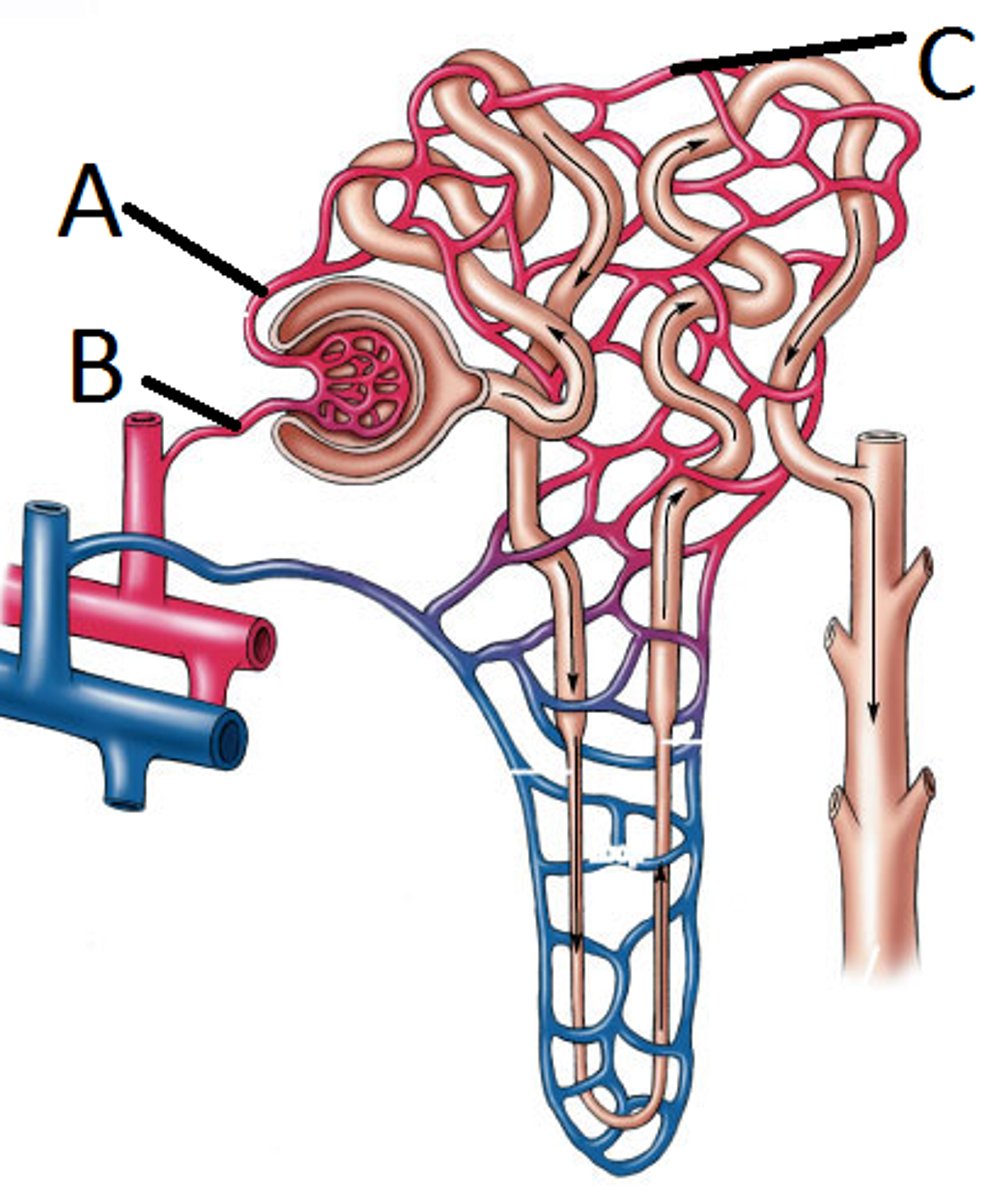
The Structures of the Nephron - Glomerulus
- Network of capillaries
- 1 cell-thick wall -> shorter distance for the transport of materials to the glomerular capsule.
- Permeable membrane -> increase efficiency for the transport of materials. Although large structures like erythrocytes, leukocytes and proteins cannot pass.
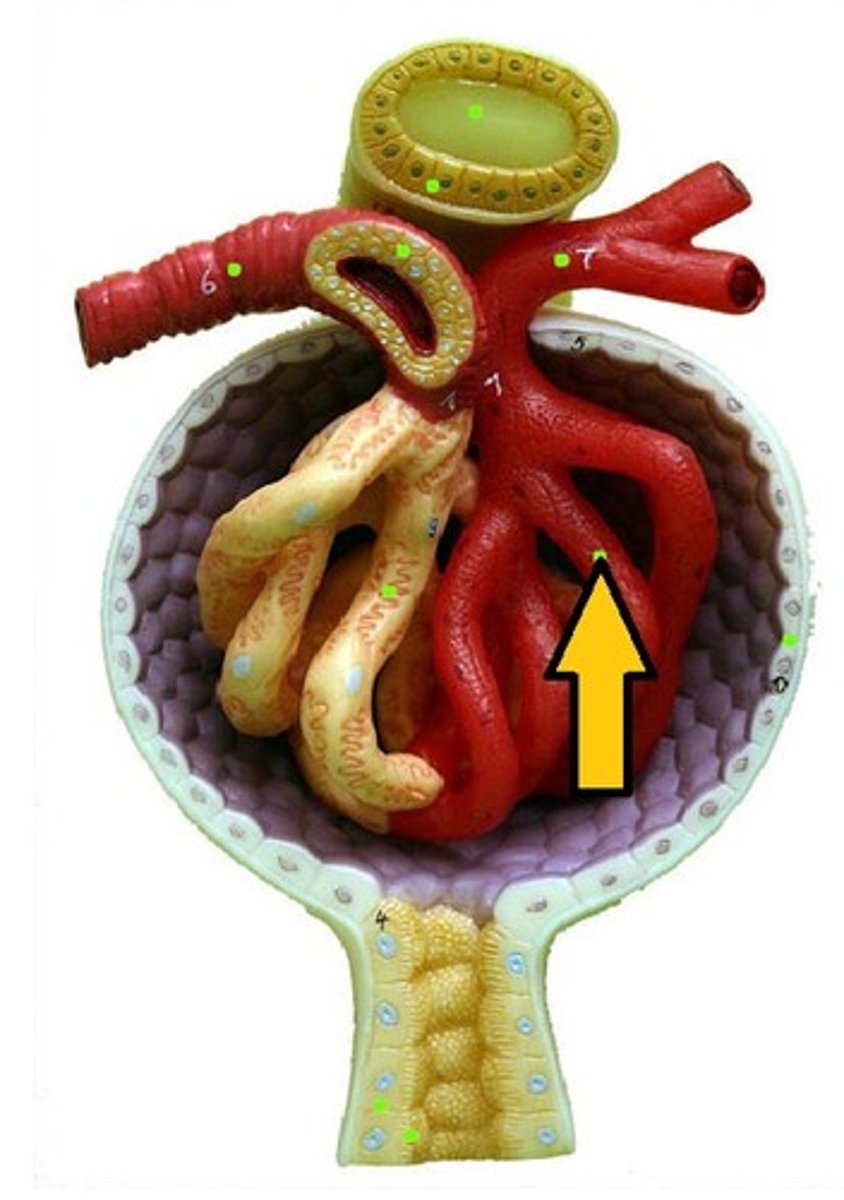
The Structures of the Nephron - Efferent arteriole
- Carries blood away from the glomerulus to the peritubular capillaries.
- Narrower diameter so less blood can be removed -> Increases the blood pressure in the glomerulus.
!(A) IN THE DIAGRAM!
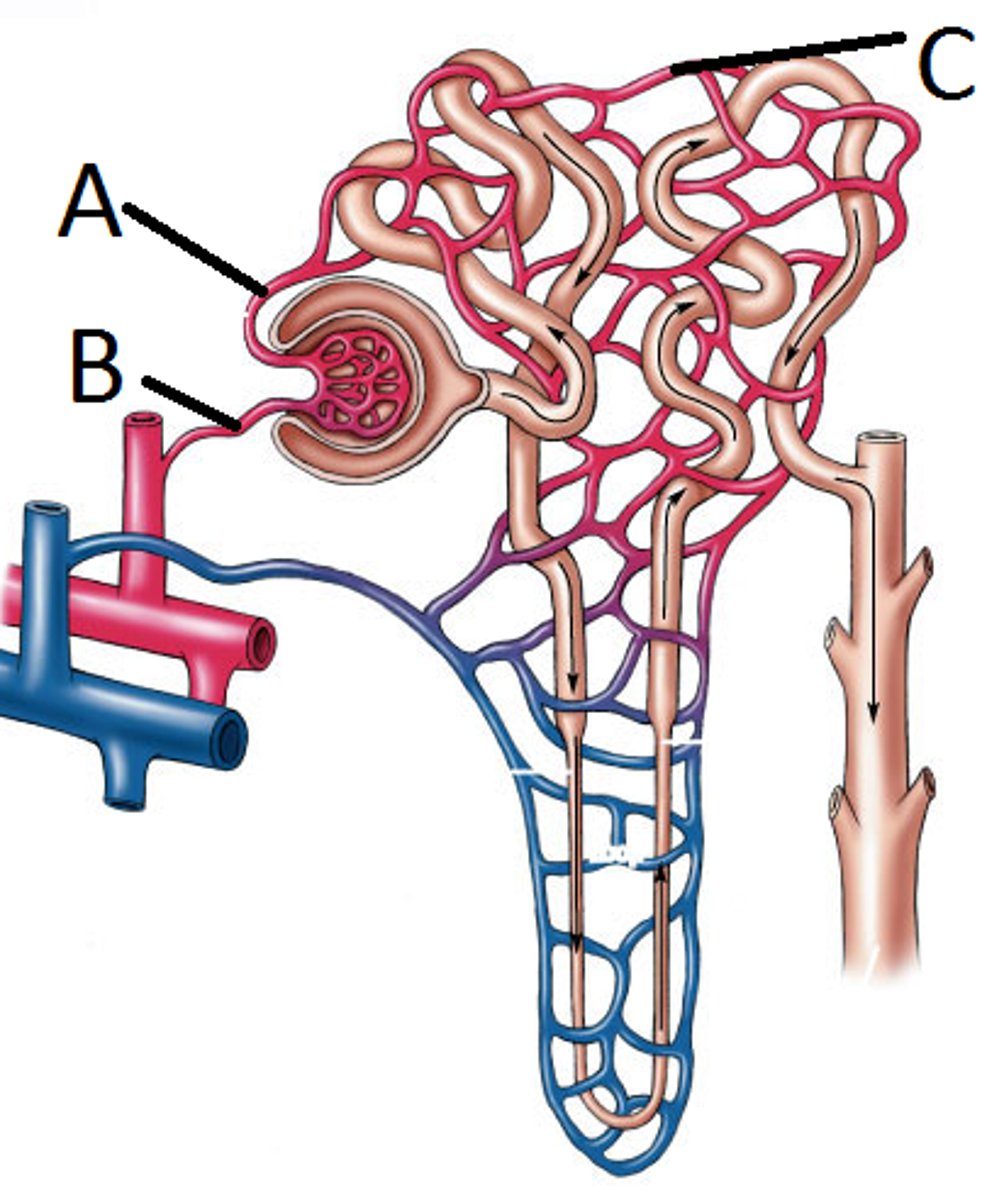
The Structures of the Nephron - Peritubular Capillaries
- Secondary capillary network from efferent arteriole to renal venules.
- Surrounds the renal tubule and collecting duct -> increases surface area + less distance
!(C) IN THE DIAGRAM!
The Structures of the Nephron - Glomerular Capsule
- Expanded sac that surrounds the glomerulus.
- 1 cell-thick wall -> Short distance for transport of materials
- Fluid inside is called filtrate
The Structures of the Nephron - Proximal convoluted tubule
- A winding tube, carrying filtrate to the Loop of Henle.
- 1 cell-thick wall -> More efficient transport of materials
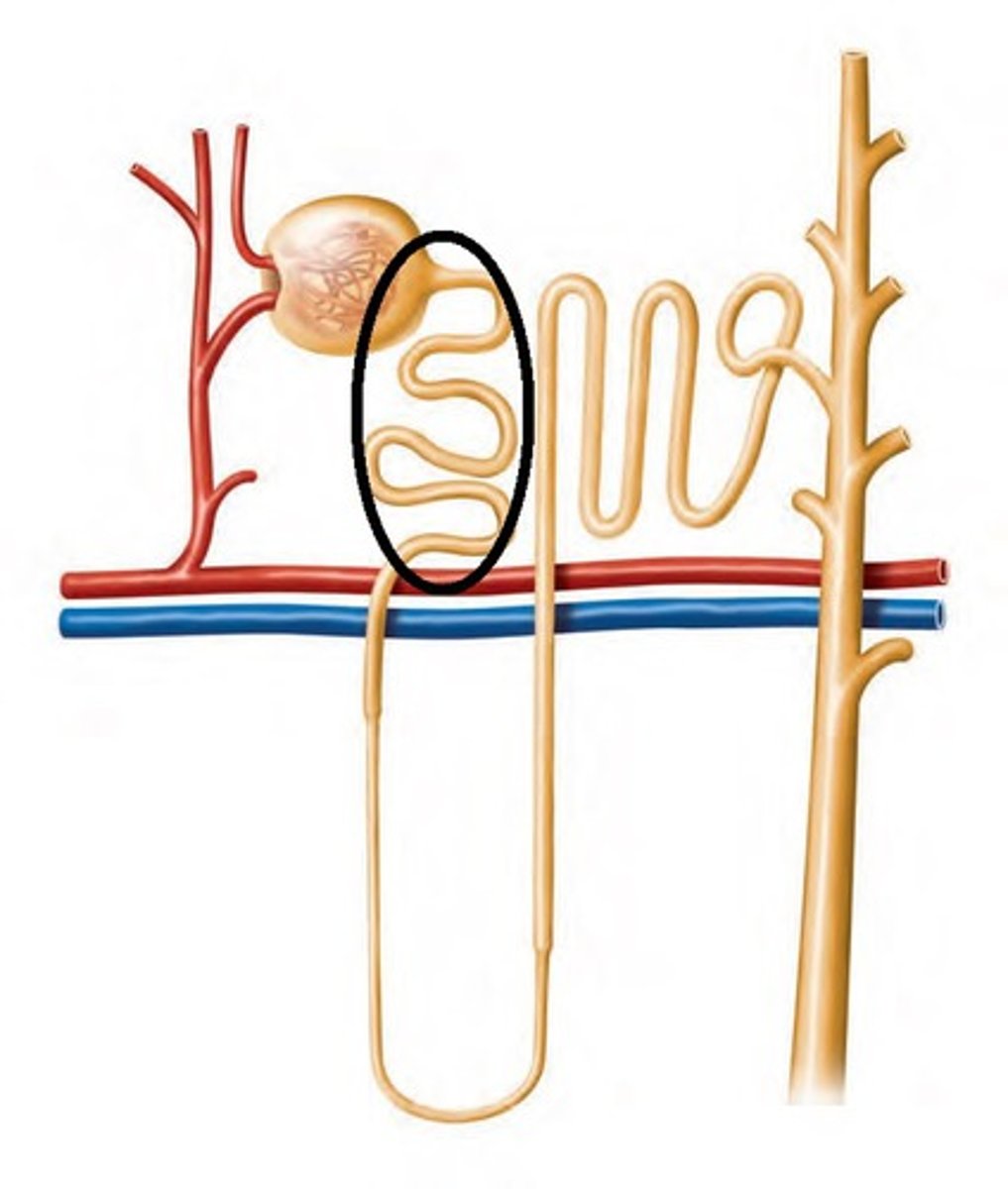
The Structures of the Nephron - Loop of Henle
- Tube carrying filtrate to the distal convoluted tubule
- Long bend -> Large surface area
- 1 cell-thick wall
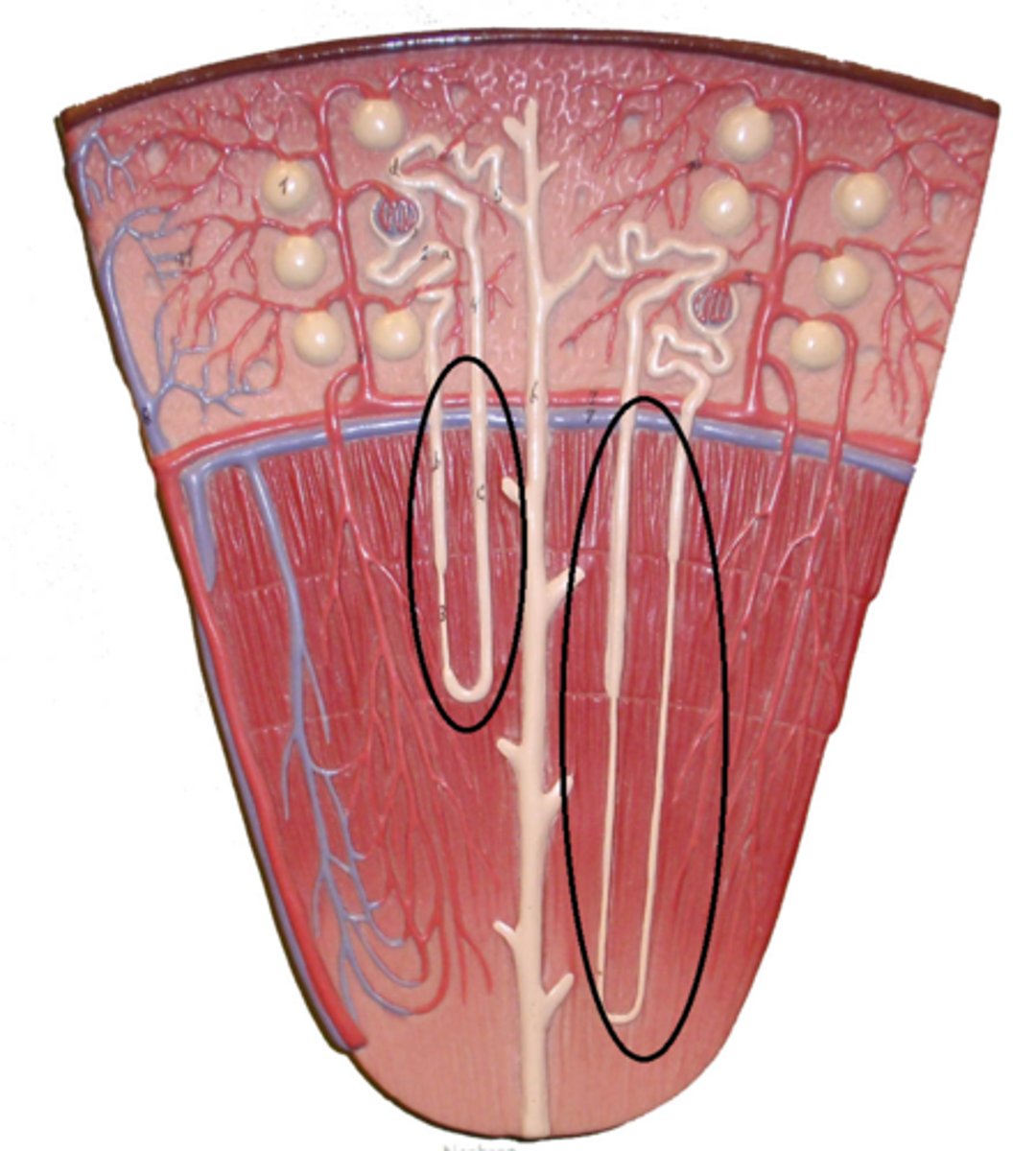
The Structures of the Nephron - Loop of Henle: Descending Limb
- Large number of aquaporins -> More efficient transport of water out of the filtrate.
- Making the filtrate hypertonic
The Structures of the Nephron - Loop of Henle: Ascending Limb
- Few aquaporins -> More efficient transport of NaCl out of the filtrate.
- Making the filtrate hypotonic
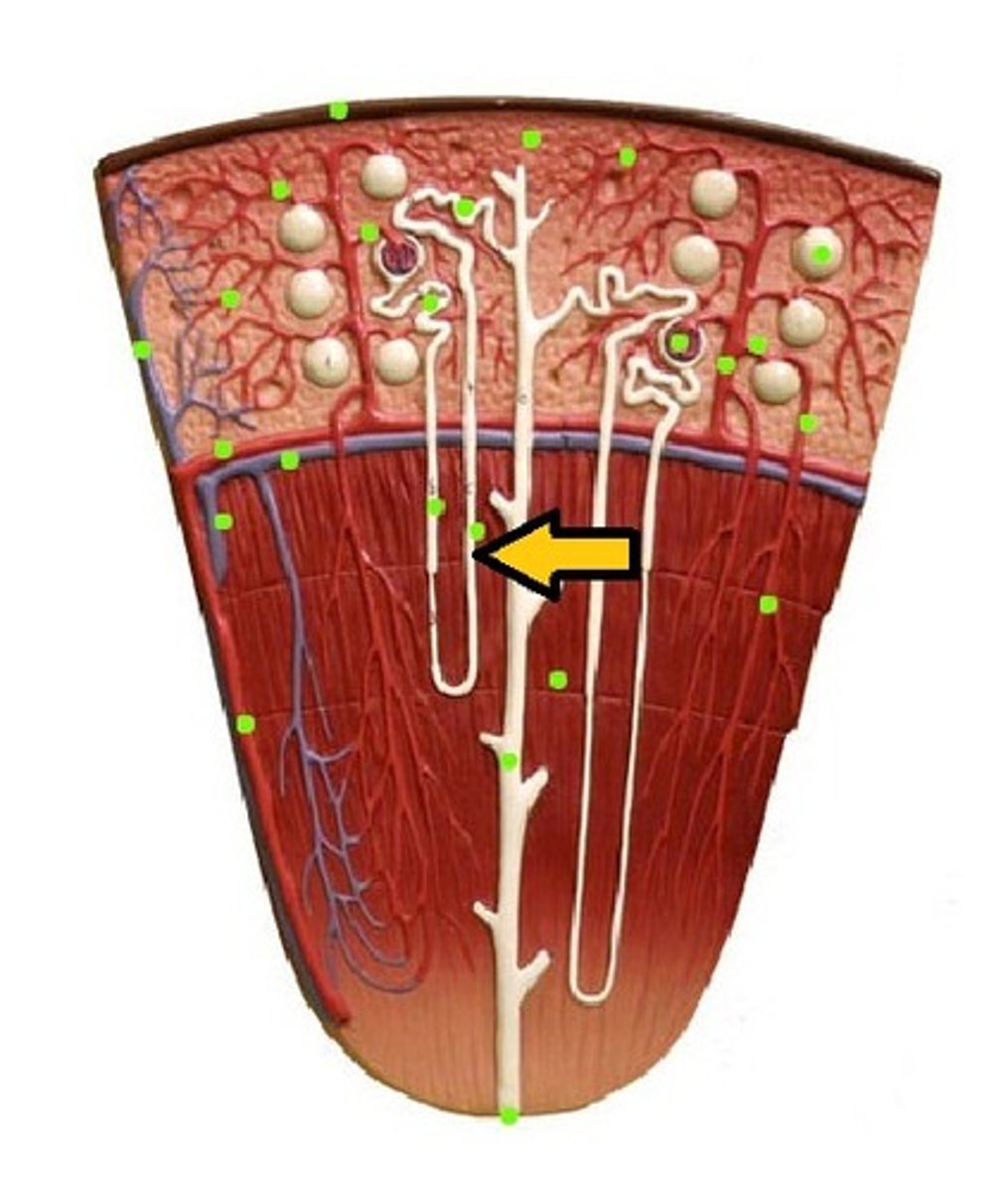
The Structures of the Nephron - Distal Convoluted Tubule
- A winding tube carrying filtrate to the collecting duct. -> Winding = Large surface area
- 1 cell-thick wall
The Structures of the Nephron - Renal Vein
- Carries blood away from the kidney
The Structures of the Nephron - Collecting duct
- DCT from many nephrons connected, delivering filtrate, now called urine.
- Carries urine to renal pelvis
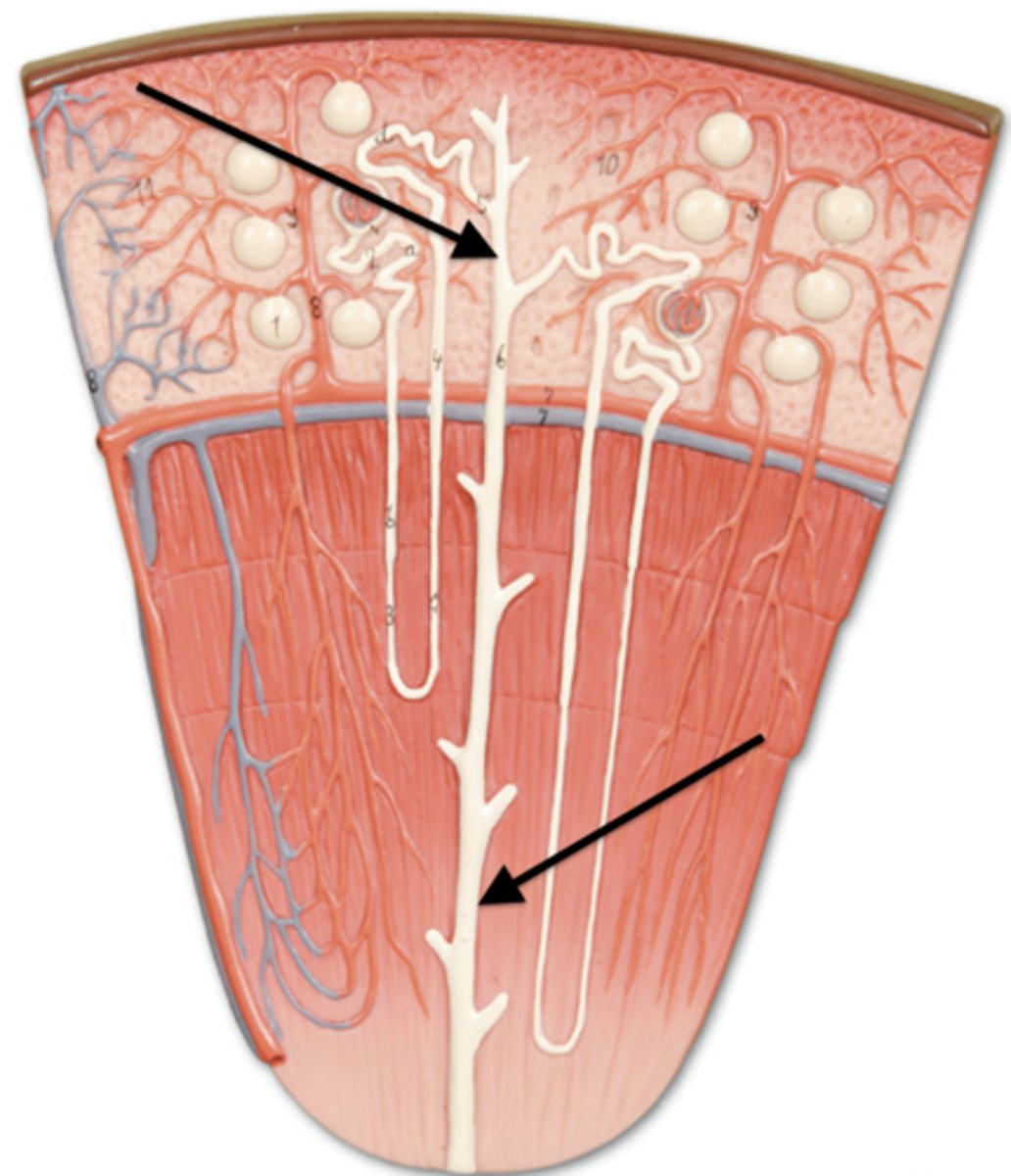
The Structures of the Nephron - Renal Pelvis
- A funnel-shaped chamber on the concave side of the kidney.
- Channels urine to the ureter
State how the renal artery, renal vein and ureter differ by the substances they carry.
- The renal artery carries unfiltered blood into the kidney.
- The renal vein carries filtered blood out of the kidney.
- The ureter carries urine away from the kidney.
The Formation of Urine
1. Glomerular Fitration
2. Selective Reabsorption
3. Tubular Secretion
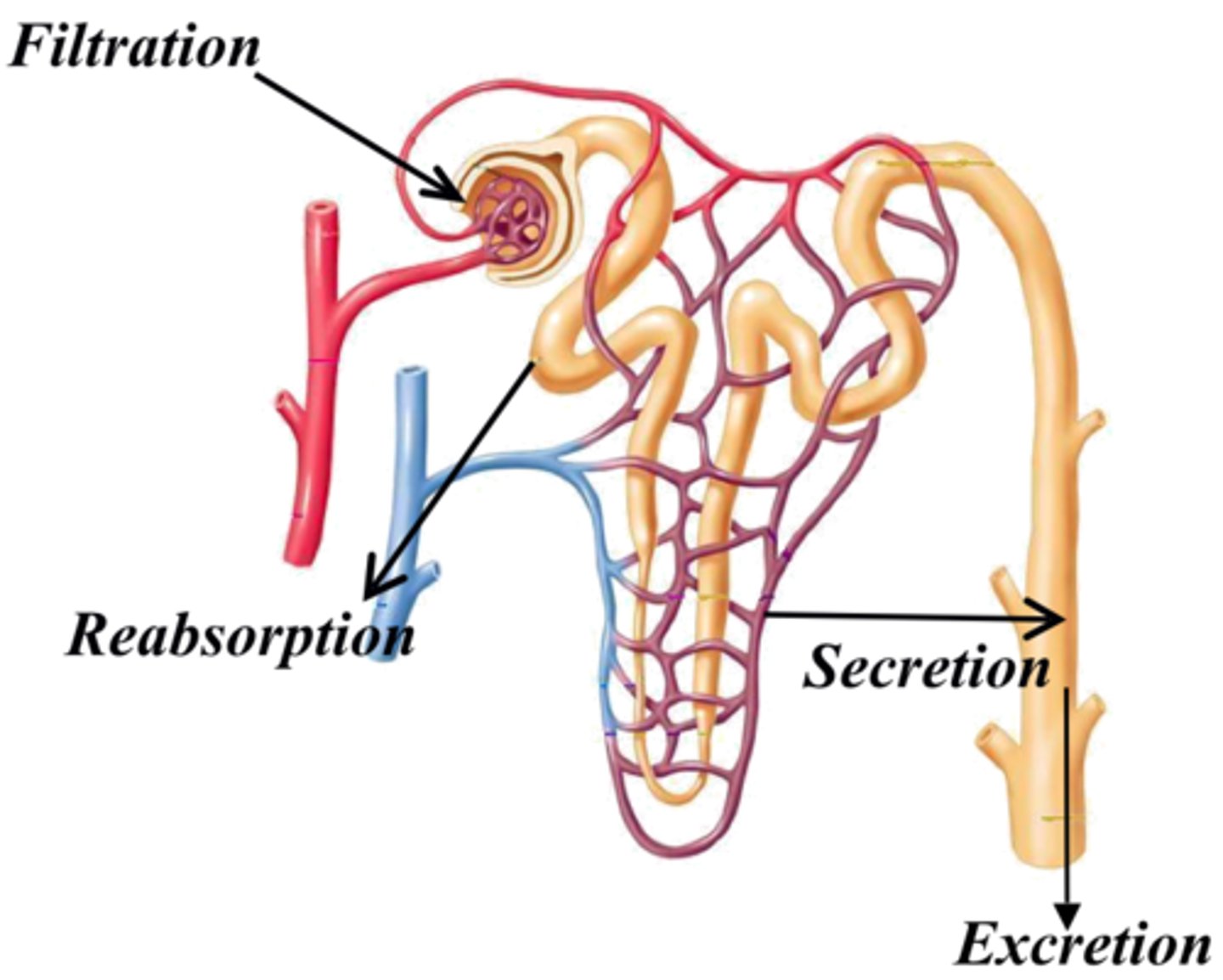
Glomerular Filtration (Blood -> Nephron)
- Occurs in the renal corpuscle (glomerulus + Glomerular Capsule).
- High pressure in the glomerulus pushes water and small molecules out of the blood into the capsule.
- Large molecules like proteins and blood cells stay in the blood.
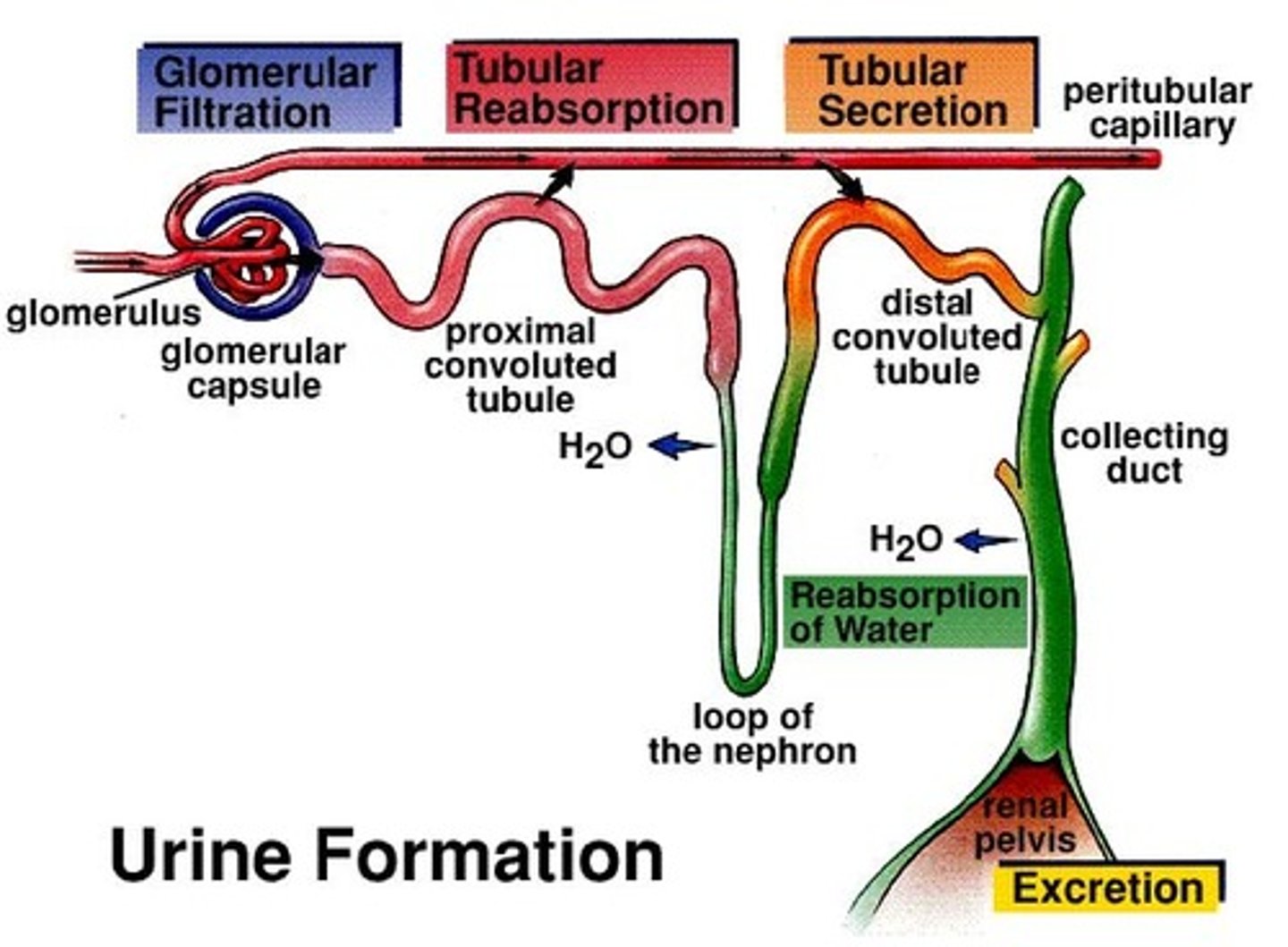
Tubular/ Selective Reabsorption (Nephron -> Blood)
- Happens along the renal tubule, specifically: The proximal convoluted tubule, the descending limb, the ascending limb, and the distal convoluted tubule.
- Useful substances are selectively reabsorbed from the filtrate back into the blood.
Facultative Reabsorption
- The amount of water reabsorbed is controlled by hormones depending on the body's needs.
Examples of the Substances involved in Tubular/ Selective Reabsorption at specific points in the Nephron: (2)
Descending Limb:
-> Water (mostly)
-> Not permeable to salt (Cannot leave the filtrate) -> filtrate becomes hypertonic -> increasing concentration gradient.
Ascending Limb:
-> Increase in solutes
-> Not permeable to water (Cannot leave the filtrate)
-> Mostly Na+ and Cl-
Examples of the Substances involved in Tubular/ Selective Reabsorption at specific points in the Nephron: (1)
Proximal Convoluted Tubule:
-> Glucose
-> Amino Acids (most)
-> Water
-> Ions: Na+, Cl-, K+, Ca2+ HCO3+
Distal Convoluted tubule:
-> Some Na+, Cl- and water.
-> Depending on the body, regulatory concentrations will be different.
Collecting Duct:
-> Water
-> Urea
Tubular Secretion (Blood -> Nephron)
- It occurs mainly in the proximal convoluted tubule and the distal convoluted tubule.
- Adds substances from the blood into the filtrate.
- Removes unwanted materials from the body and helps regulate blood pH. (Blood pH 7.35-7.45)
Examples of the Substances involved in Tubular Secretion at specific points in the Nephron:
Proximal convoluted tubules:
-> H+ -> regulates pH
-> NH4+ (Ammonium)
-> Creatinine
-> Drugs
Distal convoluted tubule:
-> H+
-> K+
-> NH4+
-> Drugs (Penicillin)
Collecting Duct:
-> H+ and K+
Ascending and Descending Limb:
-> No secretion
How is the glomerulus well suited to its function of filtration?
- It has high blood pressure, created by the afferent arteriole being wider than the efferent arteriole, which forces more fluid out of the blood.
- The blood is filtered through only two thin layers, one from the capillary wall and one from the capsule wall, allowing easy passage of small molecules.
- The walls are differentially permeable, which means small molecules like water and ions can pass through, but large molecules like red blood cells and proteins cannot.
- The large surface area of the glomerulus allows for more filtration at once.
- Over a million nephrons are present per kidney, this results in a large volume of filtrate being produced.
How is the nephron wall suited for it's function?
- The glomerular capsule and capillaries are only one cell thick, allowing for easy diffusion of substances.
- The tubule has many folds and a long loop, giving it a large surface area for reabsorption and secretion.
- Each kidney has over a million nephrons, which means there's a huge total surface area available to efficiently reabsorb useful substances and remove wastes.
- The constant flow of blood helps maintain a concentration gradient, which aids in the efficient movement of substances across the nephron wall.
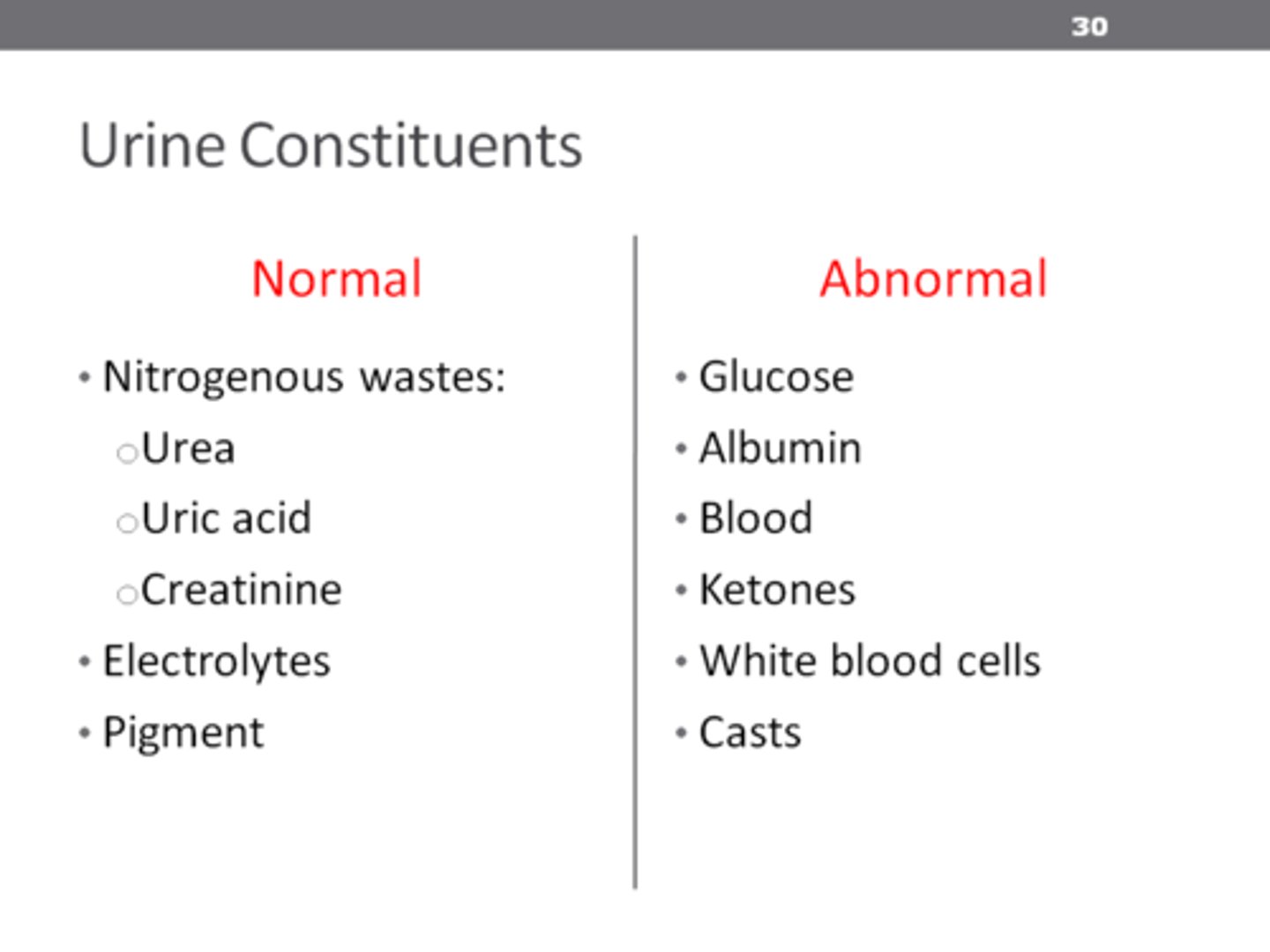
Components in Urine
- Water (96%)
- Nitrogenous wastes (2%)
-> Urea
-> Uric Acid
-> Creatinine
- Various Ions (1.5%)
- Other/ Bile pigments (0.5%)
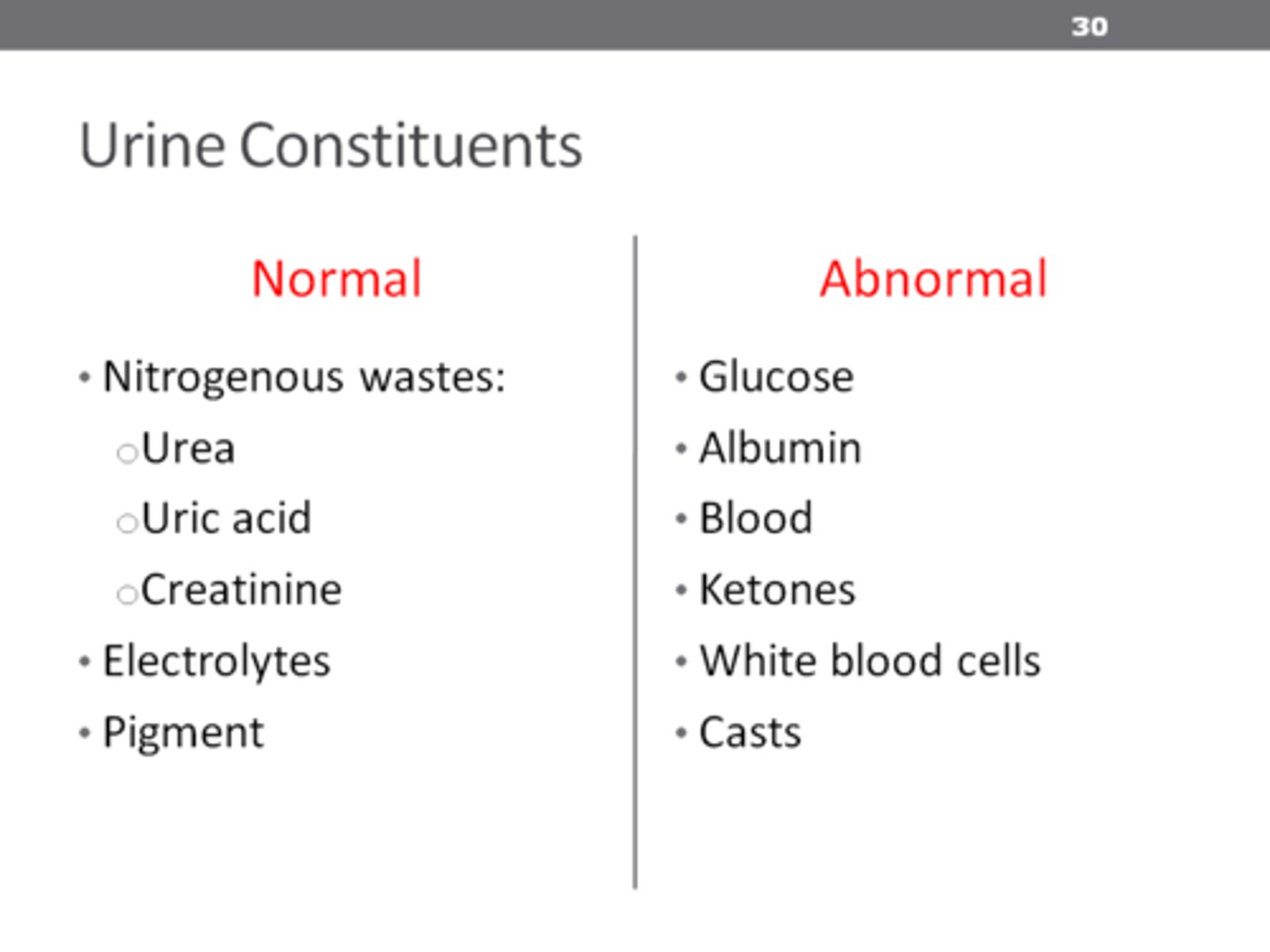
Components that should NOT be in Urine
- Leukocytes -> Too big to enter the glomerulus
- Erythrocytes -> Too big to exit the glomerulus
- Plasma Proteins -> Too big to exit the glomerulus
- Glucose -> Is fully absorbed