3.4.1 Mass Transport in Animals
1/33
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
34 Terms
Haemoglobin
Group of chemically similar molecules found in many different organisms
Has a quaternary structure - four polypeptide chains with haem group per polypeptide
Describe the role of red blood cells and haemoglobin in oxygen transport
red blood cells contain lots of Hb
(No nucleus and bioconcave - more space for Hb, high SA:V and short diffusion distance)
Hb associates with oxygen at gas exchange surfaces where partial pressure of oxygen (pO2) is high
This forms oxyhaemoglobin which transports oxygen
(Each can carry four oxygen molecules, one at each haem group)
Hb dissociates from / unloads oxygen near cells/ tissues where pO2 is low
Describe the structure of haemoglobin
protein with a quaternary structure
Made of 4 polypeptide chains
Each chain contains a Haem group and an iron ion (Fe2+)
Describe the loading, transport and unloading of oxygen in relation to the oxyhemoglobin dissociation curve
Areas with low pO2 - respiring tissues:
Hb has a low affinity for oxygen
So oxygen readily unloads Hb
So % saturation is low
Areas with high pO2 - gas exchange surfaces:
Hb has a high affinity for oxygen
So oxygen readily loads Hb
So % saturation is high
Explain how the cooperative nature of oxygen binding results in a S-shaped (sigmoid) oxyhemoglobin dissociation curve:
binding of first oxygen changes tertiary structure of haemoglobin
This uncovers the haem group binding sites, making further binding of oxygen easier
Describe evidence for the cooperative nature of oxygen binding
at low pO2 as oxygen increases there is slow increase in % saturation of Hb with oxygen
(When oxygen is binding)
At higher pO2, as oxygen increases there is a rapid increase in % saturation of Hb with oxygen
(Showing it has got easier for oxygen to bind)
What is the Bohr effect?
Effect of CO2 concentration on dissociation of oxyhemoglobin → curve shifts to the right
Explain the effect of CO2 concentration on the dissociation of oxyhaemoglobin
increasing blood CO2 e.g. due to increased rate of respiration
Lowers blood pH (more acidic)
Reducing Hb’s affinity for oxygen as tertiary structure changes slightly
So faster unloading of oxygen to respiring cells at given pO2
Describe evidence for the Bohr effect
At given pO2 % the saturation of Hb with oxygen is lower
Explain the advantage of the Bohr effect (e.g. during exercise)
More dissociation of oxygen → faster aerobic respiration → more ATP produced
Explain why different types of haemoglobin can have different oxygen transport properties
different types of Hb are made of polypeptide chains with slightly different amino acid sequences
Resulting in different tertiary structures
So they have different affinities for oxygen
Explain how organisms can be adapted to their environment by having different types of haemoglobin with different transport properties
Curve shifts to the left - Hb has higher affinity for O2
more O2 associates with Hb more readily
At gas exchange surfaces where pO2 is lower
E.g. organisms in low pO2 environments - high altitudes, underground, or foetuses
Curve shifts to the right - Hb has a lower affinity for O2
more O2 dissociates from Hb more readily
At respiring tissues where more O2 is needed
E.g. organisms with high rates of respiration/ metabolic rate (may be small or active)
Describe the general pattern of blood circulation in a mammal
Closed double circulatory system - blood passes through heart twice for every circuit around the body
deoxygenated blood in the right side of the heart pumped to lungs; oxygenated blood returns to left side
Oxygenated blood in left side of heart pumped to rest of body; deoxygenated returns to right
Suggest the importance of the double circulatory system:
prevents mixing of oxygenated / deoxygenated blood
(So blood pumped to body is fully saturated with oxygen for aerobic respiration
Blood can be pumped to body at higher pressure (after being lower from lungs)
(Substances taken to / removed from body cells quicker/ more efficiently)
Draw a diagram showing the general pattern of blood circulation in a mammal, including the names of key blood vessels
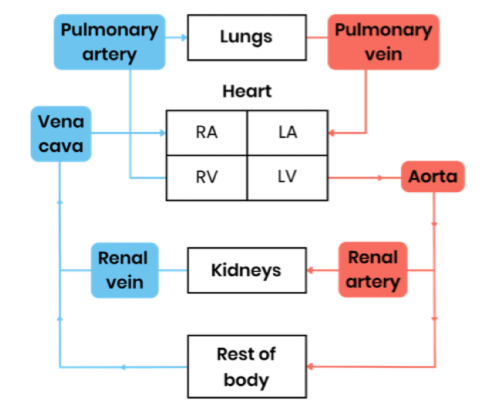
Name the blood vessels entering and leaving the heart and lungs
vena cava - transports deoxygenated blood from respiring body tissues → heart
Pulmonary artery - transports deoxygenated blood from heart → lungs
Pulmonary vein - transports oxygenated blood from lungs → heart
Aorta - transports oxygenated blood from heart → respiring body tissues
Name the blood vessels entering and leaving the kidneys:
renal arteries - oxygenated blood → kidneys
Renal veins - deoxygenated blood to vena cava from kidneys
Name the blood vessels that carry oxygenated blood to heart muscle
Coronary arteries - located on surface of heart, branching from aorta
Label a diagram to show the gross structure of the heart
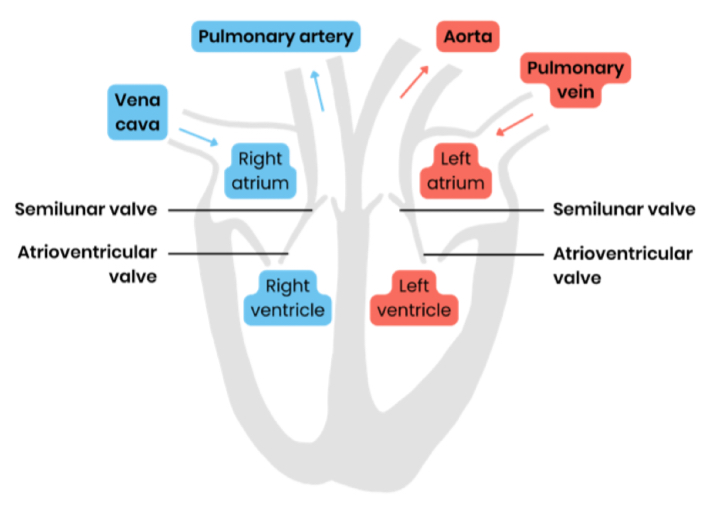
Suggest why the wall of the left ventricle is thicker than that of the right
thicker muscle to contract with greater force
To generate higher pressure to pump blood around entire body
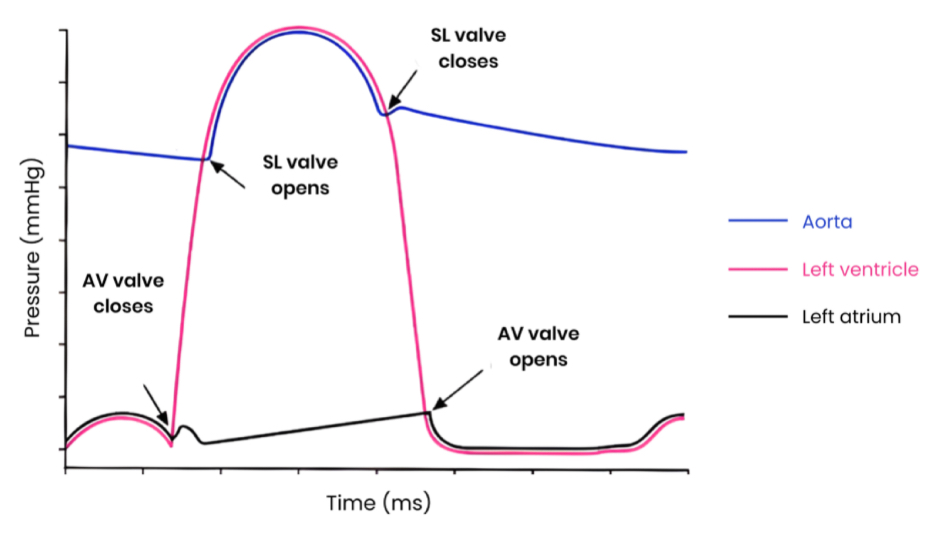
Explain the pressure + volume changes and associated valve movements during the cardiac cycle that maintain a unidirectional flow of blood (atrial systole)
atria contract
So their volume decreases, pressure increases
Atrioventricular valves open when pressure in atria exceeds pressure in ventricles
Semilunar valves remain shut as pressure in arteries exceeds pressure in ventricles
So blood pushed into ventricles
Explain the pressure + volume changes and associated valve movements during the cardiac cycle that maintain a unidirectional flow of blood (Ventricular systole)
ventricles contract
So their volume decreases, pressure increases
Atrioventricular valves shut when pressure in ventricles exceeds pressure in atria
Semilunar valves open when pressure in ventricles exceeds pressure in arteries
So blood pushed out of heart through arteries
Explain the pressure + volume changes and associated valve movements during the cardiac cycle that maintain a unidirectional flow of blood (Diastole)
atria + ventricles relax
So their volume increases, pressure decreases
Semilunar valves shut when pressure in arteries exceeds pressure in ventricles
Atrioventricular valves open when pressure in atria exceeds pressure in ventricles
So blood fills atria via veins and flows passively to ventricles
Explain how graphs showing pressure or volume changes during the cardiac cycle can be interpreted e.g. to identify when valves are open/ closed
Semilunar valves are closed:
pressure in (named) artery higher than in ventricle
To prevent backflow of blood from artery to ventricles
Semilunar valves open:
when pressure in ventricle is higher than in (named) artery
So blood flows from ventricle to artery
Atrioventricular valves closed:
pressure in ventricle higher than atrium
To prevent backflow of blood from ventricles to atrium
Atrioventricular valves open:
when pressure in atrium is higher than in ventricle
So blood flows from atrium to ventricle
How can heart rate be calculated from cardiac cycle data?
Heart rate (beats per minute) = 60 (seconds) / length of one cardiac cycle (seconds)
Describe the equation for cardiac output
Cardiac output (volume of blood pumped out of heart per min) = stroke volume (volume of blood pumped in each heart beat ) x heart rate (number of beats per minute)
Explain how the structure of the arteries relates to their function
(Function - carry blood away from heart at high pressure)
Thick smooth muscle tissue - can contract and withstand blood pressure
Thick elastic tissue - can stretch as ventricles contract and recoil as ventricles relax, to reduce pressure surges / even out blood pressure
Thick wall - withstands high pressure / prevents bursting
Smooth / folded endothelium - reduces friction / can stretch
Narrow lumen - increases / maintains high pressure
Explain how the structure of arterioles relates to their function
(Function - division of arteries to smaller vessels which can direct blood to different capillaries / tissues)
thicker smooth muscle layer than arteries
(Contracts → narrows lumen (vasoconstriction) → reduces blood flow to capillaries)
(Relaxes → widens lumen (vasodilation) → increases blood flow to capillaries)
Thinner elastic layer → pressure surges are lower (as further from heart/ ventricles)
Explain how the structure of capillaries relates to their function
(Function - allow efficient exchange of substances between blood and tissue fluid (exchange surface))
wall is a thin (one cell) layer of endothelial cells - reduces diffusion distance
Capillary bed (large network of branched capillaries) - increases surface area for diffusion
Small diameter/ narrow lumen - reduces blood flow rate so more time for diffusion
Pores in walls between cells - allow larger substances through
Explain how the structure of veins relates to their function
(Function - carry blood back to heart at lower pressure)
Wider lumen than arteries - less resistance to blood flow
Very little elastic and muscle tissue - blood pressure lower
Valves - prevent backflow of blood
Explain the formation of tissue fluid
At the arteriole end of capillaries
Higher blood / hydrostatic pressure inside capillaries (due to contraction of ventricles) than tissue fluid (so net outward force)
Forcing water (and dissolved substances) out of capillaries
Large plasma proteins remain in capillary
Explain the return of tissue fluid to the circulatory system
At the venule end of capillaries
Hydrostatic pressure reduces as fluid leaves capillary (also due to friction)
(Due to water loss) an increasing concentration of plasma proteins lowers water potential in capillary below that of tissue fluid
Water enters capillaries from tissue fluid by osmosis down a water potential gradient
Excess water taken up by lymph capillaries and returned to circulatory system through veins
Suggest and explain causes of excess tissue fluid accumulation
Low concentration of protein in blood plasma:
water potential in capillary not as low → water potential gradient is reduced
So more tissue fluid formed at arteriole end / less water absorbed at venule end by osmosis
Lymph system may not be able to drain excess fast enough
(Think Kwashiorkor)
High blood pressure (e.g. caused by high salt concentration) → high hydrostatic pressure
increases outward pressure from arteriole end AND reduces inward pressure at venule end
So more tissue fluid formed at arteriole end / less water absorbed at venule end by osmosis
Lymph system may not be able to drain excess fast enough
What is a risk factor? Give examples for cardiovascular disease
an aspect of a person’s lifestyle or substances in a person’s body / environment
That have been shown to be linked to an increased rate of disease
Examples - age, diet high in salt or saturated fat, smoking, lack of exercise, genes