O2 transport and Regulation (Lectures 29,30,31)
1/64
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
65 Terms
Ventilation-Perfusion Matching (V/Q)
Refers to coordination between amount of air (ventilation) reaching the alveoli and the amount of blood (perfusion) flowing
Sequence of oxygen movement
Atmospheric O2
Affected by altitude, humidity
Alveolar O2
Affected by lung compliance, airway resistance
Plasma O2
Affected by factors affecting diffusion (membrane thickness, excess liquid)
HbO2
Each step determines next/one way
What is responsible for O2 and CO2 pressure gradients?
Us living and existing is responsible for driving pressure gradients with use of O2 and production of CO2
O2 vs CO2 pressure gradient
O2 gradient from alveoli to tissue that drives oxygen movement
CO2 gradient is opposite as higher pressure in tissue and lower in alveoli since CO2 is waste production of metabolism
What enters the pulmonary capillary (conducting airway) and what leaves?
O2 enters
CO2 leaves
What blood comes from right heart and what blood goes to left heart?
Mixed venous blood from right heart (pretty equal PVO2 and PVCO2)
Systematic arterial blood to left heart (PaO2=100, PaCO2=40)
Steps for Gas Exchange
Oxygen needs to reach alveoli
Oxygen needs to diffuse across
Oxygen needs to reach blood
Alveolar Gas Exchange influenced by
O2 reaching the alveoli
Composition of inspired air
Alveolar ventilation: affected by rate and depth of breathing, airway resistance, lung compliance
Gas diffusion between alveoli and blood:
By surface area
By diffusion of distance: affected by barrier thickness and amount of fluid
Adequate perfusion of alveoli
Total peripheral resistance (TPR) is regulated by arteriolar radius, which is regulated by
Local control
Reflex control
Local control of arteriolar radius is regulated by
Myogenic responses
Paracrines
a. Metabolic - O2, CO2
b. Signal molecules - NO
c. Immune cells - Histamine
Reflex control of arteriolar radius is regulated by
neural
Sympathetic on arterioles (norepi on alpha)
hormonal
epi on beta2
angiotensin II
ADH (vasopressin)
ANP
In peripheral and systemic system, local factors of O2 and CO2 affect arterials by:
If low O2 and high CO2 in peripheral tissue = hints at lots of metabolizing
This is sensed by arterioles —> vasodilate —> get more oxygen to supply skeletal muscle
If high O2 and low CO2 in peripheral tissue = hints at low metabolizing
This is sensed by arterioles as body does not want to waste O2 —> vasoconstrict
Goal of systemic and peripheral system managing O2 and CO2 arteriolar radius is to:
Optimize tissue oxygenation
In pulmonary system, local factors of O2 and CO2 affect arterials by:
If low O2 and high CO2 —> pulmonary arterioles vasoconstricts —> why waste in not ventilated area, go to lungs that are well ventilated
If high O2 and low CO2 —> pulmonary arterioles vasodilates —> enough oxygen in body, go divert blood in areas that are oxygen rich
Goal of pulmonary system managing O2 and CO2 arteriolar radius is to:
Optimize gas exchange
Lungs do not want to waste perfusion to poorly ventilated areas
What is ideal ventilation/perfusion matching (V/Q)?
0.8
Avg aleolar ventilation (air flow) = 4 L/min
Takes into account of dead space
Avg perfusion (blood flow) = 5 L/min
4/5 = 0.8
PAO2 =
PaO2 =
PAO2 = alveolar oxygen pressure
PaO2 = arterial oxygen pressure
For gas exchange to be effective, what must happen between blood flow and air flow?
For gas exchange to be effective, blood flow (perfusion) must “match” air flow (ventilation
If one alveoli becomes underventilated:
Decrease in PAO2 and increase in PACO2
Pulmonary arteriole constricts in hypoxia
Don’t want to send blood to poor ventilated area —> redirect blood elsewhere
If one alveoli is well ventilated:
Increase in PAO2 and decrease in PACO2
Pulmonary arterioles dilate in hypoxia
Want to send body there to pick up oxygen
Total pulmonary ventilation (TPV) equation
TPV = Respiratory rate (RR) x Tidal volume
Avg RR = 12 - 18 br/min (about 15 br/min)
Avg TV/breath = 500 mL/br
Avg TPV = 6-9 L/min
Low V/Q Defects
V lower than normal, Q not changing
Perfusion (Q) is being wasted
COPD (bronchitis or emphysema), pulmonary edema (liquid in alveoli)
Body senses low ventilation as O2 is not reaching arterioles
Means ventilation is issue —> oxygen not able to each alveoli
High V/Q Defects
V is not changing, Q lower than normal
Ventilation (V) being wasted
Emphysema *
Means perfusion is an issue → oxygen not able to reach blood
V/Q = 0
Shunt: no ventilation
Airwway obstriction, pneumonia
V/Q = infinite
Q = 0
Pulmonary embolism: clot from another place in the body which had lodged its way into lungs, capillaries, or bigger vessels
Dead space
Low Ventilation Disorders:
High ventilation Disorders
Low Ventilation: Airway obstruction, Pneumonia, Obstructive Lung Disorder (Asthma, Bronchitis), Restrictive Lung Disorder
High Ventilation: Emphysema
Low perfusion disorders:
High perfusion disorders:
Low perfusion disorders: low cardiac output, pulmonary embolism
High perfusion disorders: N/A
The lower the V/Q ratio…
the closer the outflowing blood composition gets to mixed venous blood, aka true shunt
The higher the V/Q ratio….
the closer the outflowing blood composition gets to alveolar gas
Gas Composition | Bronchioles | Pulmonary Arterioles | Systemic Arterioles |
PCO2 increases | |||
PCO2 decreases | |||
PO2 increases |
| ||
PO2 decreases |
Gas Composition | Bronchioles | Pulmonary Arterioles | Systemic Arterioles |
PCO2 increases | Dilate | Constrict | Dilate |
PCO2 decreases | Constrict | Dilate | Constrict |
PO2 increases | Constrict | Dilate | Constrict |
PO2 decreases | Dilate | Constrict | Dilate |
O2 diffuses across from ___ into ___ into ___
alveoli —> plasma blood —> RBCs where O2 binds to hemoglobin
Total Blood oxygen (TBO) =
O2 dissolved in plasma (PaO2) about 2% + O2 bound to hemoglobin (HbO2) about 98%
Why does our body use O2 bound to hemoglobin and not dissolved O2?
Oxygen is not very soluble in liquid → poor at delivering good amount of oxygen to tissues
Hemoglobin
Composed of 4 chains (2 light and 2 heavy)
Each chain has heme group where oxygen binds to
One hemoglobin can bind up to 4 oxygen molecules
If you do not have hemoglobin:
rely on dissolved oxygen for means of delivering oxygen to their tissue
Normal amounts of oxygen reaching alveoli
Low O2 carrying capacity
Equation of HbO2
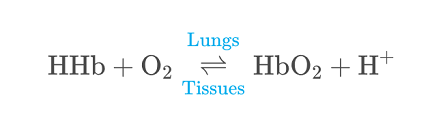
reversible reaction in order to offload oxygen to give to tissues
Relationship between partial pressure of oxygen (PO2) and amount of hemoglobin saturated with oxygen
Directly related
More oxygen around, more hemoglobin that is going to have oxygen bound to it
P50
PO2 that corresponds to 50% saturation of hemoglobin
Does PO2 every reach 100%?
No, max is 98%
The oxygen hemoglobin disassociation curve shows what shape
S shape (sigmoidal) due to cooperative binding
cooperative binding: as more O2 binds to Hb, it increases affinity of Hb to O2
Why is Cooperative binding evolutionary/biologically advantageous and get selected for?
Hemoglobin is at 75% saturation when it returns to lungs, posessing the highest affinity to O2 - perfect for O2 binding to Hgb at the lungs
When there is less O2 bound, Hgb’s affinity to O2 decreases, so more O2 will unbind
Perfect for when you need to offload O2 quickly
PO2 of arterial blood
PO2 at mixed venous pressure/at rest
PO2 of arterial blood = 100 mm Hg
PO2 at mixed venous pressure/at rest = 40 mm Hg
Factors changing affinity of Hb
Metabolic byproducts
CO2 (byproduct of cellular respiration)
pH (H+ byproduct of CO2 breakdown)
Temperature (byproduct of muscle movement)
2,3 BPG (byproduct of metabolism)
How to unload O2?
Decreases Hb affinity to O2 —> right shift
Running away from tiger aka increased metabolic state where you are using lots of O2
Increase CO2
Low pH (increase H+)
Increase 2,3 BPG
Area below graph ahs gotten smaller which means less oxygen bound hemoglobin
Higher PCO2, higher P50
How to tightly bind o2?
Increase Hb affinity to O2 —> left shift
Decrease CO2
Higher pH (decrease H+)
Decrease temperature
Decrease 2,3 BPG
Area below graph has gotten bigger which means more oxygen bound to hemoglobin
Lower PCO2, lower P50
If you are running away from a tiger, do you want O2 bound more tightly to Hgb?
No, you want it to be loose and unloading oxygen
Effects of anemia
Reduction in hemoglobin
Decrease in hemoglobin = decrease in HbO2
TBO decreased as same PaO2 but HbO2 decrease
You always equilibrate same amount of
oxygen in your plasma (PaO2) even if less more more hemoglobin
Effects of carbon monoxide poisoning
Extremely fatal as brain not getting oxygen supplied
Displaces oxygen off of iron in heme group
Binds to heme group with very high affinity (200-300 times more than oxygen)
Increases affinity of Hb for O2 that is bound
Shifts curves in both directions
Influences amount of oxygen bound to hemoglobin
Sits at 50% saturation
Effects of altitude
At sea level
PAO2 = 100 mm Hg
PO2 = 160 mm Hg
As you get higher in altitude, values declines
Decreased O2 (dissolved oxygen)
Immediate response to attitude (hypoxia)
Hyperventilation: chemoreceptor reflex activated at plasma PO2 = 60 mm Hg
Systemic arteriolar dilation (low O2 thinks metabolizing a lot) and cerebral edema (collection of fluid in brain)
Increased sympathetic output
Pulmonary arteriole constriction (hypo ventilated) area) —> HAPE
Long term response to altitude (hypoxia)
Increased erythropoietin (EPO) —> RBC synthesis (increase RBCs)
Increase # mitochondria and mitochondria enzymes
Increased myoglobin (muscle form of Hb)
Angiogenesis (making more vascular/arterioles)
Initially decrease in plasma oxygen and increase in Hb
Breathing is dependent on
skeletal muscles which do not contract spontaneously, but rely on somatic motor neuron/pacemakers in RCC in pons and medulla
Influences of rate of breathing
Carotid and aortic chemoreceptors detected by CO2, O2, and H+
Integrated in medulla and pons
Emotions and voluntary control
Respiratory neurons in medulla
control inspiratory and expiratory muscles
Neurons in the pons
interact with medullary neurons to influence ventilation
DRG (Dorsal Respiratory Group)
D for Diaphragm and DRG
In medulla
Regulates muscles for quiet inspiration
NTS receives sensory information from peripheral chemo and mechanoreceptors through vagus and glossopharyngeal nerves (X and IX)
Output from DRG goes via the phrenic nerves to the diaphragm and via intercostal nerves to intercostal muscles
VRG (Ventral Respiratory Group)
V for VRG and Very forced breathing
Active during forced inspiration and expiration
Innervate muscles of larynx, pharynx, and tongue
Inappropriate relaxation of muscles constrictive to obstructive sleep apnea
Pre Botzinger complex
Part of VRG
Contains spontaneously firing neurons which are pacemakers in RCC for respiratory rhythm
Medulla vs Pons function for respiration
Medulla: initiates respiration
Pons: modulates respiration
Chemoreceptor reflex function for respiration
modulates respiration
detects CO2, O2, and H+
Peripheral (carotid/aortic) chemoreceptors
Detects CO2, O2, and H+
Central (medullary) chemoreceptors
Detects only H+ in CSF
Plasma levels of O2 need to be ___ in order to trigger chemoreceptor reflex
below 60 mm Hg
Steps for how chemoreceptors detect hypoxia
Low PO2 (PO2 drops below 60 mm Hg)
K+ channels close
Cell depolarizes
Voltage gated Ca2+ channels open
Ca2+ floods in
Exocytosis of neurotransmitters
Activates afferent fibers of CN IX
Sends signal to medullary respiratory centers
Ventilation increases