Pharmacological Principles of General Anesthetics, Sedatives, etc. (Week 3, Mod 8)
1/22
Earn XP
Description and Tags
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
23 Terms
What are the psychotropic drug classifications based on increasing unresponsiveness?
1) Tranquilizer
2) Neuroleptic
3) Sedative
4) Hypnotic
What are the 2 amino acid pathway receptors that are targets for consciousness-altering drugs, and what kind of drug targets each receptor?
1) Glutamate ‘NMDA’ receptor
Ketamine (General Anaesthetic/Analgesic)
2) GABAA receptor
Benzodiazepines (sedative, antiepileptic, anxiolytic)
Several general anaesthetics
What are the 3 Monoamine pathway receptors that are targets for consciousness-altering drugs, and what kind of drug targets each receptor?
1) Alpha2-adrenoceptor
Sedative/analgesic
2) Noradrenaline/5-HT (Serotonin) degradation/reuptake
Monoamine Oxidase Inhibitors
Tricyclic antidepressants
Selective serotonin reuptake inhibitors (SSRIs)
3) Dopamine D2 receptors
Sedative/tranquilizers
Antiemetic drugs
What is one thing in particular about the pharmacokinetics of these drugs that you need to keep in mind?
THEY CAN CROSS THE BLOOD BRAIN BARRIER
Are either small, non-polar molecules or they get through via transporters
Describe the NMDA receptor… what neurotransmitter usually binds to it? What is its function normally?
Glutamate receptor = NMDA receptor
Excitatory receptor
Ion channel with many binding sites
Glutamate binds to binding site, opening the channel and resulting in an influx of sodium -> action potential
Describe the mechanism of action of ketamine on the NMDA receptor…
Inhibits the excitatory action of the receptor by being either a competitive receptor antagonist, or as a physical channel blocker
What are the 5 features of ketamine as an anesthetic? What will you see in the patient?
Sensory loss with analgesia
Increased muscle tone
Eyes open ± slow nystagmus
Active reflexes incl. laryngeal/pharyngeal reflexes
Less profound CVS & respiratory depression
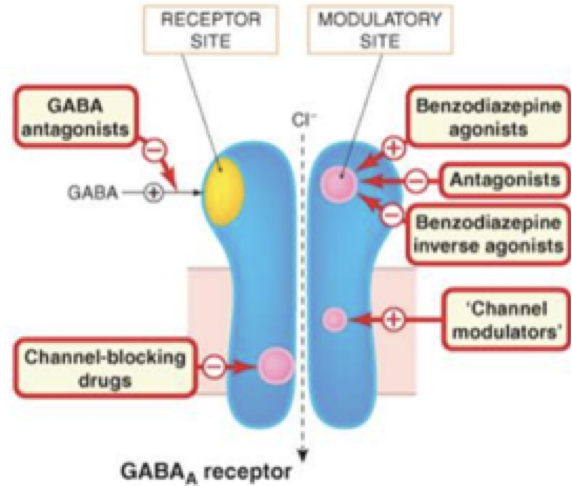
Describe the GABA a receptor… what neurotransmitter usually binds to it? What is its function normally?
GABA binds to the GABA receptor
Is the MAIN INHIBITORY transmitter / channel in the CNS
GABA receptor is a ligand-gated Cl- channel; when GABA binds, opens to allow Cl- to flood into the cell, resulting in a hyper polarization
Responsible for mediating fast inhibitory synaptic responses
What receptor is the MOST important target for general anesthetic drugs?
GABA is the MOST important target for GA drugs
Describe the mechanism of action of general anesthetics on the GABA a receptor…
Work by ENHANCING the inhibitory function of the receptor
Bind to an allosteric site on the receptor, which allows for a larger, more frequent current of Cl- to enter the cell
What are the pharmacodynamics of general anesthetics that target the GABA receptor? What do they cause (both good, and bad)?
Cause sedation at the CNS
BUT cause significant depression of the CVS / RESP
Describe the mechanism of action of benzodiazepines (BZPs) on the GABA a receptor?
Has a SPECIFIC binding site on the receptor that it binds to (BZP binding site)
Has agonists, antagonists, and inverse agonists
What we usually use when using BZPs is the agonist… enhances the function of the GABA receptor
Uses as a sedative / premedicant (also an anticonvulsant)
What are the pharmacodynamics of BZP’s? (both desired and side effects)
CNS: primarily anxiolytic action
muscle relaxation
CVS/RESP: minimal depression
Describe the function of the alpha-2 adrenoceptor… what is its function normally?
Inhibits the release of neurotransmitters presynaptically when stimulated; activated by endogenous norepinephrine and epinephrine, but are a typical target for sedatives and analgesic agents
ALSO causes post-synaptic inhibition of smooth muscle relaxation
Results in vasoconstriction
Describe the mechanism by which noradrenaline induces a contraction on smooth muscle via alpha 1 and alpha 2 adrenoceptors…
Alpha-1 mediated pathway…
Induces a contraction in smooth muscle when noradrenaline binds
Is the PRIMARY pathway to induce a contraction
Alpha-2 mediated pathway…
When noradrenaline binds, inhibits adenylate cyclase (enzyme that produces cAMP)
cAMP INHIBITS CONTRACTION, causing relaxation of smooth muscle
Since cAMP is inhibited, contraction isn’t inhibited; instead, enhances contraction of muscle by secondary means
Describe the specificity exhibited by alpha-2 AGONISTS for their alpha-2 adrenoceptor… what does this mean in terms of its effects and/or side effects?
Alpha-2 agonists are PREFERENTIAL for alpha 2 receptors, but CAN stimulate alpha 1 receptors at smooth muscle
Essentially, we use alpha 2 agonists for sedation at the CNS. Its primary target is the alpha 2 adrenoreceptors at the pre-synaptic level to inhibit neurotransmitter release, inhibiting signals for wakefulness / pain
HOWEVER, still have a 1620:1 (or 260:1 or 160:1) chance of those agonists acting on the ALPHA 1 RECEPTORS of smooth muscle within the autonomic nervous system
Causes peripheral nervous system side effects
Describe the pharmacodynamic actions (the sedative / analgesic effects) of alpha 2 agonists…
PRIMARILY used as a sedative, but has the added benefit of analgesic effects (potent, but shorter lived than sedation)
Sedation
dose-dependent (not at higher serum concentrations)
mild sedation to deep sedation
Analgesia
potent analgesic action, dose dependent and shorter than sedation
central action: spinal & supraspinal
spinal: receptors are located densely in laminae I & II of dorsal horn of spinal cord
supraspinal: receptors located in PAG, LC, NRM - associated with pain information processing
What are the effects that alpha 2 agonists can have on the CVS? Respiratory system? GIT?
CVS
hypertension (bp increase) -> hypotension / normotension
marked bradycardia
Respiratory
mild to moderate depression: cat, dog, horse
ruminants - arterial hypoxaemia
GIT
vomiting in some species, generally GIT motility is depressed (not as extreme compared to opioids)
What are 2 medicines that are considered to be dopamine antagonists? What is their general mechanism of action?
Dopamine antagonists:
Phenothiazines (acepromazine)
Butyrophenones (azaperone and fluanisone)
Mechanism of action:
Dopamine transmission is EXCITATORY in the CNS, especially in movement and behavior
Antagonists are NON-SELECTIVE; cause a REDUCTION in activity at the basal ganglia, limbic system, etc.
Most phenothiazines affect other receptor systems, causing a wide range of peripheral effects (effects the ANS)
Describe the pharmacodynamics of phenothiazines… both the desired effect, and the side effects in the periphery
DESIRED:
CNS – tranquilliser
SIDE EFFECTS: come from anti-adrenergic or anti-cholinergic effects
CVS - Arterial hypotension (10-20% decrease ABP) *** can be problematic in hypovolemic patients
Peripheral vasodilatation (α adrenergic blockade)
Central actions, medulla (decreased sympathetic outflow)
Mild tachycardia
Anti-arrhythmic action
Respiratory - generally minimal
GIT (anti-emetic)
Decrease gastrointestinal smooth muscle activity (anti-muscarinic action)
Delayed gastric emptying
Decrease gastro-oesophageal sphincter tone
What are the 2 main targets for inhibiting adrenergic (noradrenaline) transmission at the synapse?
1) Monoamine oxidase
Breaks down noradrenaline within the synapse; stopped by MAO inhibitors
2) Neuronal epinephrin transporter (NET)
Takes transmitted noradrenaline in the synaptic cleft and transfers it back into the synapse; stopped by tricyclic antidepressants
What 2 monoamine pathways are involved in depression?
NORADRENALINE
SEROTONIN
What 3 classes of mood-altering drugs act on adrenergic transmission? Describe their mechanisms of action
Tricyclic antidepressants
block noradrenaline and 5HT (serotonin) reuptake into the synapse
Increases the availability of noradrenaline and serotonin
Monoamine oxidase inhibitors (MOAI)
increase stores of noradrenaline and 5HT in the synapse
Selective serotonin reuptake inhibitors (SSRIs)
block 5HT reuptake SELECTIVELY