Ex phys final
1/90
Earn XP
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
91 Terms
PO2 throughout the body
in alveoli→ 105
lungs to systemic arteries→ 100
systemic veins→ about 40
PCO2 throughout body
in capillaries→ 40
Lungs to systemic arteries→ 40
Systemic veins→ 46
temperature’s affect on hemoglobin curve
warmer temps make O2 unload easier
warm muscles are muscles in use
cold muscles are muscles at rest
pH affect on hemoglobin curve
lower pH makes O2 unload easier
lower pH, aka more hydrogen atoms, aka more CO2 used means muscle needs O2
respiratory control center
medulla and pons
control rate/depth of breathing
unconscious control
influenced by chemoreceptors
heart rate regulation
autonomic→ parasympathetic slows heart
hormonal→ cortisol (and GH) and T4 increase HR
cardiac cycle
systole- aka contraction normally takes 1/3 of cycle
with exercise, this is 0.2 sec
diastole, aka relaxation normally takes 2/3 of cycle
with exercise, this is .13 sec
SV values (EDV, ESV, SV)
EDV- 120 ml/beat
ESV- 70 ml/beat
SV- at rest, 80 ml/beat
HR influences
(temp, neural, hormone)
Temp: direct relationship. Inc temp inc. HR
Neural: Sympathetic stim increases, parasympathetic decreases HR
Hormones: catecholamines, and thyroid hormones inc HR
SV influences
preload- End-diastolic volume
sympathetic stimulation
afterload- mean arterial blood pressure
preload influences
venous return
venoconstriction of non-working muscle
skeletal muscle pump
respiratory pump
Frank-starling mechanism
sympathetic stimulation on SV
increased sympathetic stimulation will increase cardiac contractility
including better calcium handling
E/NE and thyroid hormones will also increase contractility
afterload affect on SV
if it is high, MABP will increase the pressure of the aorta, making the L ventricle have to work harder to push blood to the body
hypertension:( damages the heart)
Mean arterial BP (definition and formula)
the average pressure in arteries
MABP= CO * TPR
MABP= Diastolic BP plus 1/3 pulse pressure
pulse pressure
difference between SBP and DBP
mean arterial BP, short and long term regulation
Short term:
chemical and baroreceptors signal to SNS
SNS will inc stimulation to vasoconstrict or decr stimulation to vasodilate
Long term:
kidneys control blood volume and therefore BP
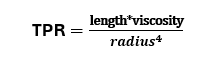
TPR regulation
length- you can really only change this by changing weight
viscosity of liquid- aka hematocrit. This can be changed by RAAS or aldosterone
radius of vessel- controlled be frequency of SNS stimulation
local factors can vasodilate or vasoconstrict
alpha 1 receptors vasoconstrict
angiotensin II vasoconstricts
Blood pressure “formula”
BP = CO * TPR
assumptions of submax testing:
after 110, Hr increases linearly
every intensity of exercise has an O2 consumption rate
with incremental exercise, each level has its own steady stae
submax tests can be used in conjunction with HR max to predict the power output/exercise capacity
CV changes with exercise
bloodflower redistribution (more to muscles, less to GI tract)
inc CO
improved a-vO2 dif
blood redistribution is controlled by:
vasoconstriction:
myogenic stretch reflex
sympathetic stimulation to non-working tissue
Vasodilation
local factors from working muscles produce H+, CO2, NO which all signal for local dilation
Fick equation
VO2= CO * a-vO2 difference
basically amount of O2 used is amount of blood pumped times the amount of O2 taken up by blood
O2 demand during incremental exercise
increases much higher than at rest
will inc with every intensity
CO change with incremental exercise
CO will dramatically inc until it reaches the need, then inc slowly
SV response to incremental exercise
SV will inc rapidly, then plateau around 40% VO2 max
in highly trained individuals, they train their heart to pump efficiently so that SV doesn’t plateau
for 99.9% of population, all CO increase after 50% VO2max comes from HR
a-vO2 difference response to incremental exercise
changes a lot early/low intensity, increases slowly after about 50% VO2max
inc is due to a high amount of O2 taken up for oxidative phosphoryation
BP response to incremental exercise
SBP increases. Vasoconstriction to the rest of the body requires inc in BP
DBP doesn’t really change→ this would decr filling time and EDV
criteria for meeting VO2 max
plateau in VO2 despite inc work rate
RER is over 1.15 (ratio of gases used)
HR in final stage is within 10 bpm of HRmax
(high blood lactate, RPE of 17+, HR doesn’t inc with work rate)
double product
Hr *SBP
inc linearly with intensity
indicates myocardial O2 consumption
stroke work
SV * mean systolic pressure
aka the amount of work the L ventricle has to do to push out blood
arm vs leg exercise (HR and BP)
BP is higher bc there is more inactive muscle tissue (aka legs)
HR is higher bc of more sympathetic stimulation (to stimulate for vasoconstriction)
alveolar type 1 cell
simple squamous, is the lining of the alveoli
alveolar type 2 cell
this type of cell secretes pulmonary surfactant, which prevents the alveoli from collapsing
equation for flow of gas
flow = (Palveolar- Patmophere)/resistance
change volume→ pressure changes→ get flow
ways O2 can exist in plasma
hemoglobin- 98%
dissolved in plasma- 1.5%
ways CO2 can exist in plasma
on hemoglobin- 30%
dissolved in plasma- 10%
mixed in as bicarbonate- 60%
P50
partial pressure necessary to keep 50% of hemoglobin saturated with O2
things that inc HB’s affinity for oxygen
(mean it holds on to O2, muscle doesn’t need it)
decr temp
decr PCO2
inc pH (more alkaline/basic)
things that decr Hb’s affinity for oxygen
(make it easier for O2 to leave, mean tissue needs O2)
high temp
low pH (CO2 production, more acidic, more H+)
Hering-bruer inflation reflex
prevents lungs from over-inflating
stretch receptors in (intercostals???) stop inhalation
sensors that affect pO2, pCO2, pH of blood
peripheral chemoreceptors (in the aortic arch and carotid bodies, which supply blood to the body and brain)
central chemoreceptor (in the medulla oblongata, directly senses ECP’s pH)
Neural controllers of breathing
medulla oblongata is the leader/pace-setter (inspiration via phrenic n and intercostals)
RR is modified by the pons (inhibitory, fine tuning)
P wave on EKG
atrial depolarization
QRS complex on EKG
ventricular polarization and atrial repolarization
ST segment and T wave on EKG
ventricular repolarization
IRV
inspiratory reserve volume
the amt that can be inspired after a normal inspiration
ERV
expiratory reserve volume
the amt that can be expired at end of normal expiration
VC
vital capacity
max volume inspired/expired in one breath
TV + IRV + ERV
RV
reserve volume
amount left after ERV/max exhalation
there is some amt of air needed in lungs to prevent them from collapsing
TLC
total lung volume/capacity
the amount of air in the lungs after a full inspiration
VC + RV
FVC, FEV1
forced vital capacity
VC but inhaled and exhaled forcefully
FEV1- amt air forcefully expired in1 sec
FECV1/FVC
ratio of amt of air blown out in 1 sec to amt of air you can forcefully blow out
you want to get 80% or more out to be normal
PEF (test)
peak expiratory flow- highest flow rate of air during max exhale
done after surgery to clear CO2 from lungs and inc RR
MVV
max ventilatory volume
amt of air breathed in during sustained voluntary effort
minute ventilation (Ve)
TV * RR
amt expired each minute
usually 70% of MVV
pCO2 on ventilation
CO2 drives ventilation!!!!!!
inc in this increases Ve
inc in pO2 decreases Ve
Ve change (rest→exercise)
Ve will inc rapidly with onset, then inc steadily
pO2 and pCO2 remain unchanged relatively bc of this increase right away
ventilatory response to exercise (trained vs untrained)
trained- ventilation is less frequent at rest and at any intensity of a submax exercise
better CV shape (SV inc, HR can relax with the same CO)
body is better at utilizing O2
change in aerobic capacity of locomotor muscles
untrained- ventilation is more frequent at rest and at any submax intensity of exercise
ventilatory threshold
where your RR inc disproportionately to the O2 consumption
this illustrates the shift from aerobic to anaerobic respiration (and inc CO2 production)
untrained occurs around 50% VO2max
trained occurs higher, maybe 75% VO2 max
myoglobin O2 affinity
much higher than hemoglobin, even at low pO2
allows for Mb to “store” O2 as a reserve
shuttles O2 from cell membrane to mitochondria
types of non-steroid hormones
peptide-
hydrophilic, made in ER and golgi/stored in vescicles. enter blood as “free hormone”
Amine hormone-
aka catecholamines and thyroid hormones
(Prostaglandins) a third type of hormone
ADH
from posterior pituitary
to kidneys
prevents water loss by resorbing Na+
inc BP
inc with exercise
GH
from anterior pituitary
to all cells
inc use of fats/FFA as an energy source
decr use of carbs as a fuel
“supports” actions of cortisol
Inc with exercise
Thyroid hormones
from thyroid
to whole body
inc HR and contractility
inc FFA mobilization
“mimic” the affects of catecholamines in this way
inc with exercise
no chronic adaptations to exercise
insulin
from pancreas
to whole body
inc glucose uptake
decr BG
decr with exercise
glugagon
from pancreas
to whole body
decr glucose uptake
inc BG
inc protein and fat use for fuel
influenced by catecholamines
inc with exercise
catecholamines
from adrenal medulla
to whole body
inc HR and contractility
decr glucose uptake→ MAINTAIN BG
inc glycogenolysis in liver and lipolysis
vasoconstriction
inc with exercise
decrease with training for same exercise-→ progressive overload!
aldosterone (mineralocorticoid)
from adrenal cortex
to kidneys
resorbs Na+, inc fluid retention
inc BP
inc with exercise
cortisol (glucocorticoid)
from adrenal cortex
to whole body
prevent glucose uptake in body
inc gluconeogenesis in liver
inc FFA mobilization
decr/not produced with low intensity exercise, inc with higher intensity exercies
renin
from kidneys
to liver
inc water resorption
inc BP
increase vasoconstriction
how BG is maintained
glycogenolysis in liver
lipolysis in liver
FFA mobilization in liver
preventing CHO uptake in muscle tissues
beta adrenergic receptor effects
beta 1 has no E/NE preference
beta 2 MUCH prefers E
beta1→ inc hr, glycogenolysis, lipolysis
beta2→ inc bronchodilation, vasodilation
alpha adrenergic receptor effects
both slightly/equally prefer E/NE
alpha1→ vasoconstriction
alpha2→ opposes actions of beta receptors
leptin
hormone that influences appetite
from hypothalamus
inc insulin sensitivity and FA oxidation
too high concentration activates SNS, CV remodeling, heart failure
adiponectin
inc insulin sensitivity and has FA oxidation
too much inc coronary heart disease/myocardial hypertrophy risk
too little causes visceral fat accumulation/hyperglycemia
change in appetite hormones w increased fat mas
MORE leptin
Less adiponectin
leads to T2D and low-grade inflammation
fatty pancreases→ more beta cells→ more insulin-hyperinsulinemia
too much leptin→ decr receptors→ leptin resistance→ hyperinsulinemai
TSH inc→ hyperthyroidism→ inc in fat mass → HP axis inc cortisone chronically
ghrelin is decr→ decr growth hormone → decr lipid mobilization→ inc food uptake→ hypogonadism/hyperandrogenism
hormone signaling that would mobilize fat mass is blocked
testosterone
from testes
anabolic (promotes tissue rebuilding/performance enhancements)
promotes masculine characteristics
Estrogen/Progesterone
released from ovaries
establish and maintain reproductive fn
lack of estrogen can cause osteoporosis/athletic dysmenorrhea
FSH/LH/estradiol change with exercise
overload
effect of training when body is exercised at lvl above what it is used to
adaptations from endurance training
inc in VO2 (from SV and a-vO2 dif)
inc SV (inc preload, decr afterload, inc contractility)
inc a-vO2 dif (venous O2 changes, muscle blood flow, capillary density, mitochondrial #/size)
other adaptations/metabolic changes with endurance exercise
(aerobic enzymes, lactate Dehydrogenase form, IM fatty acid stores, FFA uptake ability, enzymes for lipolysis)
inc aerobic enzymes
lactate Dehydrogenase shifts to H-form (makes more lactate than pyruvate)
inc IM fatty acid stores and glycogen
inc FFA uptake ability
inc enzymes for lipolysis
acute CV response to exercise
inc in: HR, SV, CO, MABP, blood flow to working muscles
at 95% of RM1, you can see up to 320/350mmHg for BP and 170bpm
be v careful with valsalva, this can cause reactive hyperemia
chronic CV response to exercise
decr RHR, (individual)
resting MABP is lower
inc in SV, mostly due to change in lean muscle mass
general adaptation syndrome
body gets “stressed” from resistance training and will compensate to this stress w minimal fatigue
this is good stress and how we see adaptation
overreaching
intentionally training excessively, which leads to short term decrements
you are out for a day or two to recover
can be used intentionally to get out of plateaus
overtraining
when the body is way way over-stressed from workouts and this causes long-term decreases in performanve
can last weeks-6 months
can extend to ending athletic careers
exercise and immunity
immune system is transiently suppressed for 3-72 hrs post workout
if someone is overtrained/lacks sleep/additional stressors→ immune response is even worse
Detraining
2 days→ we see initial atrophy due to decr protein synthesis
little later, inc protein resorption
Strength drops around 2 weeks
we see 7-12% change/loss of strength
you can regain muscle quicker when working out bc of neural “set point”
age-related muscle change
10% of muscle mass is lost 25-50
40% of muscle mass is lost 50-80
loss of fast fibers and gain in slow fibers
due to reduced PA
regular training can improve strength/endurance but can’t eliminate this phenomena
metabolic syndrome
type 2 diabetes, dyslipidemia, obesity, hypertension